Supplemental Digital Content is available in the text.
Keywords: intubation, remote intubation, scoping review, teleguidance, tele-intubation
Abstract
OBJECTIVES:
Teleguidance facilitated intubation has recently reemerged during the coronavirus disease 2019 pandemic as a strategy to provide expert airway management guidance and consultation to practitioners in settings where such expertise is not readily available onsite or in-person. We conducted a scoping review to provide a synthesis of the available literature on teleguidance facilitated intubation. Specifically, we aimed to evaluate the feasibility, safety, and efficacy of teleguidance facilitated intubation given existing technology.
DATA SOURCES:
A librarian-assisted search was performed using three primary electronic medical databases from January 2000 to November 2020.
STUDY SELECTION:
Articles that reported outcomes focused on implementing or evaluating the performance of teleguidance facilitated intubation were included.
DATA EXTRACTION:
Two reviewers independently screened titles, abstracts, and full text of articles to determine eligibility. Data extraction was performed using customized fields established a priori within a systematic review software system.
DATA SYNTHESIS:
Of 255 citations identified, 17 met eligibility criteria. Studies included prospective investigations and proof of technology reports. These studies were performed in clinical and simulation environments. Five of the prospective investigations that examined time to intubation and intubation success rates. Multiple different commercially available and noncommercial teleconference software systems were used in these studies.
CONCLUSIONS:
There is a limited body of literature evaluating the feasibility, safety, and efficacy of teleguidance facilitated intubation. Based on the studies available that examined a variety of technologies within simulation and clinical environments, teleguidance facilitated intubation appears to be feasible, safe, and efficacious. Given the exponential growth in the use of telemedicine technology during the coronavirus disease 2019 pandemic and the evidence supporting teleguidance facilitated intubation, there is a need to critically evaluate the most effective mechanisms to integrate and optimize these technologies across diverse practice settings.
Endotracheal intubation is a critical life-saving procedure, but many rural and remote settings do not have access to experienced airway providers. Both technical and nontechnical skills are required to reliably and safely secure a patient’s airway. A hallmark of critical care training is learning to supervise and coach junior trainees or other providers through a successful intubation without resorting to hands-on intervention. Similarly, clinicians working in tele-critical care practices are likewise accustomed to assisting other providers in performing procedures remotely. Thus, teleguidance technology may be a viable alternative for providing expert airway management consultation and guidance to remote providers who need to perform intubation but are not experts in airway management. While tele-observation, telemedicine, and teleguidance are not new technologies in clinical practice with the first published case from 1974 (1), they have reemerged as invaluable tools during the coronavirus disease 2019 (COVID-19) pandemic to provide large numbers of patients with expert level care while reducing patient and provider exposure and decreasing the need for personal protective equipment (2).
The topic of teleguidance facilitated intubation (TFI) has not been rigorously reviewed in the literature. Here, we perform the first scoping review of the literature involving TFI to elucidate: 1) the feasibility of use and barriers to implementation in clinical practice and 2) whether patient safety, complications, and measures of intubation success (i.e., first-pass success, time to intubation) are improved with its use. A scoping review was chosen in this setting due to the emerging nature of this technology and the limited body of published research.
METHODS
This scoping review was conducted by a research team with expertise in anesthesiology, critical care, medical education, telemedicine, and systematic review methodology. This review adhered to the review methodology outlined by Grant and Booth (3) and the checklist for Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (4). Covidence systematic review software (Melbourne, VIC, Australia) was used for all stages of the review process, including title and abstract screening, full-text review, and data extraction. For the purpose of this scoping review, we considered teleguidance, tele-observation, and telemedicine to be synonymous terms. We defined teleguidance as the use of video and audio telecommunications technology to facilitate procedural guidance of a provider performing an intubation by a supervisor who was not physically present in the location where the procedure was being performed.
Research Questions
TFI was defined as the use of audio-visual telecommunication technology to provide remote guidance for the performance of endotracheal intubation. The aim of this scoping review was to summarize the published literature regarding: 1) the feasibility of TFI and barriers to implementation within clinical practice and 2) examine overall patient safety, complications, and examine whether measures of intubation success (i.e., first-pass success, time to intubation) are improved with TFI.
Search Strategy
A librarian-assisted search was performed on November 10, 2020, using three widely used electronic databases: PubMed, Web of Science, and Excerpta Medica dataBASE. The databases were selected as they are comprehensive covering a wide range of clinical disciplines. The following key words were used in the literature search: teleguidance, intubation, teleprocedures, telemedicine, telehealth, procedures, teleintubation, remote intubation, remote supervision. The selected key words were searched individually in each database. The search was limited to articles published between January 2000 and November 2020 to coincide with the development of the relatively new field of telemedicine. Reference lists of included articles were reviewed, and hand searches of relevant appearing references were performed to identify other literature not captured by the electronic database search.
Inclusion and Exclusion Criteria
Articles were included if they: 1) reported outcomes of a research study, quality improvement effort, or program aimed at implementing, or evaluating TFI; 2) the study was conducted in the operating room, ICU, emergency department, prehospital, or simulation settings; and (3) involved adults. Articles published in languages other than English were excluded. We also excluded reviews, commentaries, editorials, abstracts, and conference proceedings that did not provide original data necessary to address the questions sought in our review.
Data Abstraction
Two reviewers (B.S.L., E.A.B.) independently screened titles and abstracts of identified articles to determine eligibility. The same two reviewers then performed full-text review in duplicate, with conflicts resolved by an independent third reviewer (M.G.C.). Reviewers customized data extraction fields in Covidence to align with the aims of the review; a trial of 10 references were used in a pilot run and both reviewers (B.S.L., E.A.B.) agreed unanimously on inclusion and exclusion. Two reviewers tested extraction fields for consistency and fidelity to project aims (B.S.L., E.A.B.). The same two reviewers independently extracted data from articles for insertion into required fields. Extracted data were compared between reviewers for consensus prior to finalizing the extraction forms. The following data were extracted from included articles: year and country of publication, project aim, design, setting, key components of the intervention, implementation strategies, challenges/barriers to implementation, and clinical/implementation outcomes. Outcomes extracted included time to intubation (as reported), intubation success, technology feasibility, ease of use, and user satisfaction. Studies were classified based on study design and setting, allowing differentiation between simulation-based studies, clinically based studies, and proof of technology from prospective or retrospective designs. The study question, number of participants and their level of training, video conferencing software, airway equipment used, and outcome and results were also extracted.
RESULTS
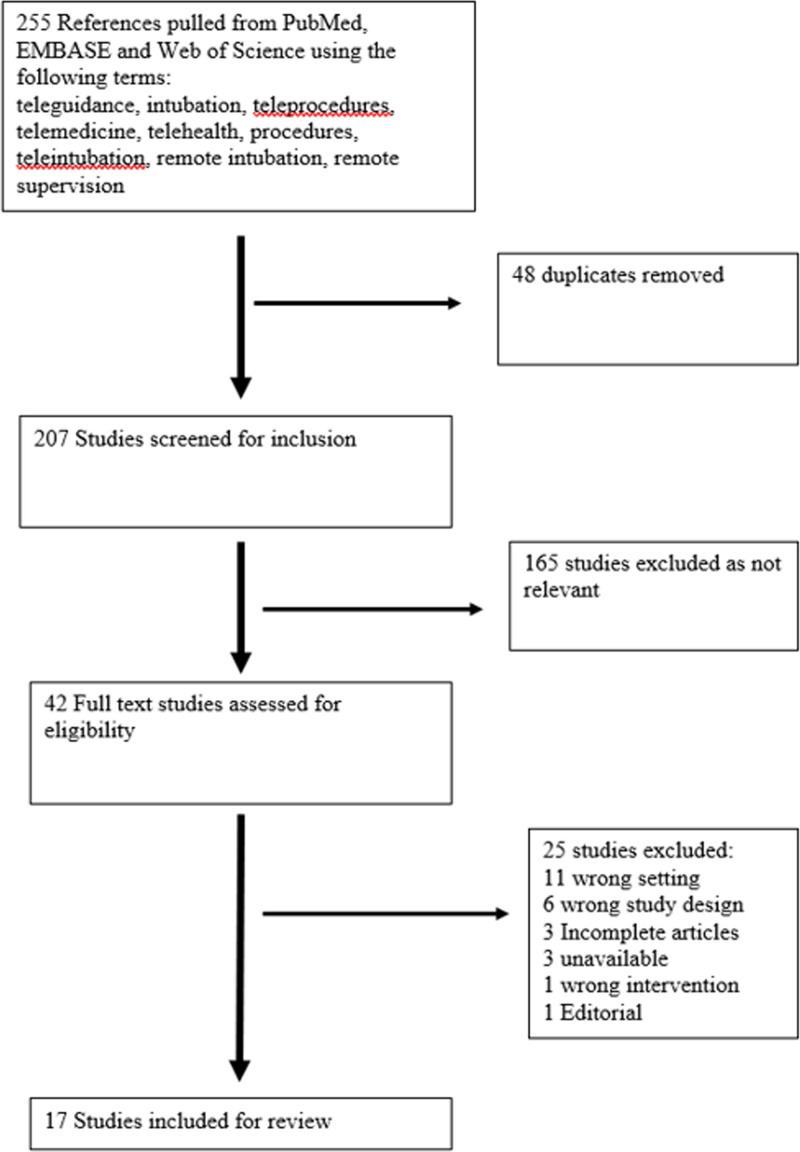
The combination of search terms with selection criteria and limits yielded 255 studies. Of these articles, 48 duplicates were removed, leaving 226 studies for title and abstract screening (Fig. 1). Of these, 165 were excluded for not meeting initial inclusion criteria (i.e., title or abstract indicated nonadult population, noncritical care setting, or literature review), a subsequent 25 were excluded after screening, resulting in 17 articles that were included in the final review.
Figure 1.
Study extraction and inclusion diagram. EMBASE = Excerpta Medica dataBASE.
Characteristics of Included Studies
Supplemental Table 1 (http://links.lww.com/CCX/A858) summarizes the characteristics of the 17 articles that met inclusion criteria including year of publication, study type and setting, study design, equipment used, and primary outcome evaluated. The articles included five prospective trials (5–9), one prospective observational study (10), and 11 proof of technology demonstrations (11–21). The included studies were published as early as 2006 (17) to as recently as 2020 (18). Of these 17 studies, seven were conducted by the same principal investigator and all seven of these had coauthors affiliated with the U.S. military (6, 11–16). A research group in the United States conducted three of the remaining studies (9, 19, 21) and two of the studies were performed by a research group in South Korea (7, 8).
Twelve of the studies were conducted in a simulation environment (5, 6, 8, 9, 11–16, 18, 20) and five were performed in clinical environments (7, 10, 17, 19, 21). Only three of the 11 proof of technology demonstrations were performed in a clinical environment (17, 19, 21). Of the prospective simulation studies, randomization of participants was performed in four cases (5, 8, 9, 16) and method of participant allocation was not reported in one (6). The single prospective clinical study randomized participants to TFI versus on-scene supervision (7).
The average number of participants for simulation studies, including proof of technology demonstrations, was 18.6, with the three largest prospective simulation trials having 50 (5), 48 (9), and 46 (6) participants each. The average number of patients for clinical studies was 50. The only prospective clinical study had 25 patients (7). The largest study in the clinical environment had 206 patients (10).
Five studies were performed in a clinical environment, three were proof of technology studies (17, 19, 21); All reported that the technology was feasible for remote supervision of intubation. The one clinically based randomized trial reported no difference in time to intubation or success rate of intubation of emergency department patients when performed by novice operators (emergency medicine residents) with in-person or remote supervision (7). One observational study showed a 71% first-pass success rate for intubations teleguidance (no comparison was available for the success rate of intubations not performed with teleguidance) (10).
All of the simulation-based prospective trials included a measure of time to intubation as an outcome (5–9, 16). Time to intubation was measured very heterogeneously and was not reported in the clinical studies. In the one prospective clinical trial, time to intubation was defined as beginning from when the laryngoscope was picked up to confirmation via auscultation, and success was determined by end-tidal Co2 monitoring at the discretion of the supervising attending (7). For the two prospective studies that compared tele-presence to no supervision, one study found that TFI had a faster time to intubation (5, 7) and one reported a higher success rate of intubation and faster time to intubation with TFI (5). All four of the prospective studies that compared in person supervision to telepresence reported no difference in time to intubation (6, 8, 9, 16), and one of these four studies also reported no difference in intubation success rate (8). One simulation study did not provide a statistical analysis (16).
Adverse events were not widely reported in the reviewed studies. The one prospective clinical study reported no difference in frequency of esophageal intubation and no difference in complication rate between teleguidance and on-scene supervision (7). The one observation study, which did not have a control group, and in which only 31% of users used teleguidance prior to their first intubation attempt reported an adverse outcome rate of 24%. Adverse events were associated with increasing number of intubation attempts, the most frequent adverse event was hypoxia (18%), followed by hypotension (6%), cardiac arrest following intubation occurred in 2.4% of patients (10).
Seven of the studies used noncommercially available videoconferencing software (Supplemental Table 1, http://links.lww.com/CCX/A858), while the remaining studies used a variety of commercially available videoconferencing software including Skype, Apple FaceTime, Tango, Google glasses, Adobe Connect, Vidyo link, and Microsoft Net Meeting. Among the commercially available software systems used, all are currently available except for Microsoft Net Meeting (17). One study that compared video quality for TFI between three different brands of videoconferencing software (Apple FaceTime, Skype, and Tango) found that while all three video services provided adequate fidelity to supervise intubations, Apple FaceTime was rated as having the highest video and audio quality (19). The type of videolaryngoscope used in the studies varied with Storz C-Mac the most prevalent (53%), followed by Glidescope (23.5%) (Supplemental Table 1, http://links.lww.com/CCX/A858). Two of the twelve simulation studies used direct laryngoscopy with telehealth glasses that afforded the supervising physician a first-person point of view (5, 18).
Only three studies assessed user responses to the technology or reported technical issues that were encountered during use. One study that surveyed users of telehealth glasses for TFI reported that the technology was “bulky and uncomfortable,” “distracted from the learning,” and had other technical issues. Another study evaluated educational value of the TFI (rated 9.5/10) and reported that 11 of 12 users had no issues obtaining the laryngoscope view or hearing the guidance provided (18). A similar study surveyed users regarding quality of imaging and reported that the average rates were 7/9 for video and audio quality and 7.8/9 for overall quality (20). Two studies evaluated surveyed users as to whether they would use the technology again and both had high ratings for continued use of TFI (19, 20).
DISCUSSION
Teleguidance for medical procedures is a growing technology and an active field of investigation (22–27). The majority of published literature has focused on proof of technology demonstrations that allude to the benefits that might be achieved with clinical use. While limited, we believe that the body of literature allows us to begin to answer the study questions regarding feasibility, safety, and efficacy of TFI and suggests avenues of future investigation. Many of the studies reviewed were small simulation-based proof of concept studies, the small size of these studies limits the conclusions that can be drawn from them. The prospective simulation studies using airway trainers and randomization of participants provide reassurance to the robustness of the results and the one prospective clinical trial was of moderate size. Overall, the quality of the studies is mixed but provides an adequate starting point for this review.
Is TFI Feasible Given Existing Technology and What Are the Barriers to Implementation?
The studies selected to answer this question span both the clinical realm and simulation environment. These studies demonstrate that TFI is feasible given the technology available at the time that the studies were performed (5–9, 11–15, 20, 21). While limited fidelity of the video and audio technology was reported in three studies, the majority did not indicate this as being a barrier to successful implementation (12, 19, 20). Ergonomic challenges with tele-glasses were discussed in one study and did present a distraction and a potential limitation for implementation of this technology for TFI (18). While technological limitations were infrequently reported in the studies, it is important to recognize that the majority of the TFI systems evaluated were customized setups that are not commercially available. The lack of availability of these systems without customization poses a barrier for users looking for “off the shelf” technology ready to implement within their own clinical environments.
A challenge in all of the studies examined was seamless integration of the video laryngoscope imaging with the videoconferencing software. However, even without full integration of these devices, the studies demonstrated that available technology was able to provide a view of a video laryngoscope screen as well as bidirectional communication supporting the feasibility of TFI. It is important to recognize that the majority of studies used technology more than 5 years old and that telemedicine technology has advanced markedly since that time especially during the COVID-19 pandemic. Based on the authors’ clinical experience direct supervision of inexperienced operators performing intubations outside of the operating room, we believe that the ideal TFI system should not only integrate of video laryngoscopy with videoconferencing but would also provide visualization of the larger clinical environment. This additional visualization (via camera) should allow for hemodynamic monitoring and visualization of patient positioning and intubator technique. While tele-glasses technology (e.g., Google Glass) is appealing because of the point-of-view images provided from the standpoint of the intubator, they lack crucial environmental information that can be important for optimizing intubating conditions (28).
Does TFI Improve Patient Safety and Intubation Efficacy?
While the available literature is limited, studies indicate that TFI appears to improve patient safety with no additional complications reported beyond those that are reported with in person supervision of intubation (7). In the observational study of TFI performed in the emergency department (10), there was no control group without TFI for comparison, and the rates of hypotension and hypoxia were lower than reported studies in similar environments with in person supervision (29, 30). The benefit of TFI in this study was further supported by the findings that adverse events were associated with increasing number of intubation attempts and a decreased rate of complications when a teleconsultation was performed prior to the first intubation attempt (10).
Consideration of the comparison groups used in the evaluations studies is important for evaluating the efficacy of TFI. Studies that compare TFI to in-person supervision provide information regarding the comparability of the two methods of oversight, while studies that compare TFI to no supervision evaluate the added value of the technology compared with no oversight at all. Two studies performed in a simulation environment indicated that time to intubation and success rate with TFI were no different than with in-person supervision (6, 9), and these findings were confirmed in a study performed in the clinical setting (7). The existing body of literature does not allow determination of superiority when comparing teleguidance to in-person supervision. The heterogeneous nature of the technology used and outcomes selected make comparison across studies difficult. For novice operators performing intubation in simulation environments, TFI was demonstrated in two studies to have a faster time to intubation and higher first-pass success rate when compared with not having any supervision at all (5, 8). A reduced rate of complications seen in the observational study when TFI was used prior to first intubation attempt also supports these findings (10). Teleguidance could also be valuable in the setting of failure to intubate; the virtual airway expert could direct a novice through a difficult airway algorithm. This virtual role has been suggested as a component of a pediatric-specific difficult airway response team (28). Teleguidance could also be used to guide performance of a surgical airway. This use of teleguidance for this indication has not been reported, but there are examples of using teleguidance to facilitate other emergent surgical procedures (31) and even damage control laparotomies (27). Extrapolating from the TFI literature, teleguidance could help improve outcomes and decrease complications during a difficult airway situation.
Limitations
Our scoping review has a number of limitations. The number of published studies that have evaluated TFI is limited, and they were performed in a small number of environments by only a few investigators. Study selection was limited to available articles contained within three major medical databases. Studies that may be available in the gray literature including technical reports, proceedings, and theses were not examined. Finally, only articles published in English were included.
There are limitations to the studies themselves, which may impact the findings. The proof of technology studies are small, single center and often employed customized equipment. The efficacy studies were limited by small study size, single-center evaluation, and lack of blinding. Adverse events were only reported in two studies (7, 10) and which might represent area source of publication bias that could impact conclusions regarding safety of the technologies. None of the studies examined the role of telemedicine in the setting of the difficult airway or if failure to intubate occurred while using TFI.
Future Directions
Given the advances in telemedicine over the last decade, there is a need to reevaluate TFI that incorporates recent technology. There is a need to fully integrate video laryngoscopy, telecommunication technology with imaging of the clinical environment. Evaluations of this integrated TFI technology first be trialed in a simulation environment with novice intubators and then in randomized controlled studies within clinical environments where experts in emergency airway management are immediately available. Objective measures of intubation success (e.g., first-pass success rate, time to successful intubation) should be collected together with feedback from users regarding challenges and areas for improvement. Practical measures of use including portability, time to setup, troubleshooting, and disinfection should also be evaluated. Robustness of the technology under actual clinical conditions in a variety of diverse environments will be essential to establishment of a successful platform for a wide range of users.
CONCLUSIONS
Based on the available literature included in this scoping review TFI appears to be a feasible, safe, and effective approach when in person supervision is unavailable. TFI appears valuable both for novice operators and may serve as an “expert consult” for trained providers. Widespread implementation of a robust TFI technology has the potential to improve patient safety and outcomes in many existing clinical environments where airway management experts are not immediately available 24/7. Teleguidance may be valuable as an educational tool providing trainees graded autonomy while ensuring an appropriate degree of supervision. While much work remains to further develop, critically evaluate, and integrate TFI into clinical care, TFI holds great promise for improving upon the existing practice for critically ill patients.
Supplementary Material
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccejournal).
All authors identified and screened studies for inclusion, extracted the data, wrote, and reviewed the article.
The authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Gravenstein JS, Berzina-Moettus L, Regan A, et al. : Laser mediated telemedicine in anesthesia. Anesth Analg 1974; 53:605–609 [PubMed] [Google Scholar]
- 2.Gibson LE, Low SA, Bittner EA, et al. : Ultrasound teleguidance to reduce healthcare worker exposure to coronavirus disease 2019. Crit Care Explor 2020; 2:e0146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grant MJ, Booth A: A typology of reviews: An analysis of 14 review types and associated methodologies. Health Info Libr J 2009; 26:91–108 [DOI] [PubMed] [Google Scholar]
- 4.Tricco AC, Lillie E, Zarin W, et al. : PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med 2018; 169:467–473 [DOI] [PubMed] [Google Scholar]
- 5.Pérez Alonso N, Pardo Ríos M, Lasheras Velasco J, et al. : Randomized clinical simulation trial of a Google Glass telemedicine application to assist orotracheal intubation. Emergencias 2016; 28:235–238 [PubMed] [Google Scholar]
- 6.Berg BW, Beamis EK, Murray WB, et al. : Remote videolaryngoscopy skills training for pre-hospital personnel. Stud Health Technol Inform 2009; 142:31–33 [PubMed] [Google Scholar]
- 7.Cho J, Chung HS, Choa M, et al. : A pilot study of the tele-airway management system in a hospital emergency department. J Telemed Telecare 2011; 17:49–53 [DOI] [PubMed] [Google Scholar]
- 8.Chung HS, Choa M, Kim SY, et al. : A comprehensive telemedicine system for remote guidance of emergency airway management. J Telemed Telecare 2007; 13:29–32 [Google Scholar]
- 9.Prescher H, Grover E, Mosier J, et al. : Telepresent intubation supervision is as effective as in-person supervision of procedurally naive operators. Telemed J E Health 2015; 21:170–175 [DOI] [PubMed] [Google Scholar]
- 10.Van Oeveren L, Donner J, Fantegrossi A, et al. : Telemedicine-assisted intubation in rural emergency departments: A national emergency airway registry study. Telemed J E Health 2017; 23:290–297 [DOI] [PubMed] [Google Scholar]
- 11.Abadia de Barbara AH, Nicholas Iv TA, Del Real Colomo A, et al. : Virtual simulation training using the Storz C-HUB to support distance airway training for the Spanish Medical Corps and NATO partners. Stud Health Technol Inform 2012; 182:1–9 [PubMed] [Google Scholar]
- 12.Boedeker BH, Bernhagen M, Miller DJ, et al. : The combined use of Skype and the STORZ CMAC video laryngoscope in field intubation training with the Nebraska National Air Guard. Stud Health Technol Inform 2011; 163:83–85 [PubMed] [Google Scholar]
- 13.Branecki C, Boedeker B, Schwedhelm M, et al. : Use of transatlantic telebroncoscopy to confirm proper endotracheal tube placement during a simulated Chemical, Biological, Radiological or Nuclear or Explosive (CBRNE) Event. Presented at: 2014 Science and Information Conference. London, United Kingdom, August 27–29, 2014 [Google Scholar]
- 14.Irizarry D, Boedeker BH, Bernhagen M, et al. : Telementoring for airway management between a far forward special operations location to a major medical center using inexpensive telemedicine solutions. Stud Health Technol Inform 2012; 173:212–214 [PubMed] [Google Scholar]
- 15.Walker MI, Walker RB, Morgan JS, et al. : The use of virtual training to support insertion of advanced technology at remote military locations. Stud Health Technol Inform 2011; 163:688–690 [PubMed] [Google Scholar]
- 16.Zeger WG, Branecki CE, Nguyen TT, et al. : A description of teaching methods using an on-site instructor versus a distant site instructor to train laryngoscopy to medical students in Hanoi, Vietnam, from Omaha, Nebraska, by video communication. Int J Emerg Med 2015; 8:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cone SW, Gehr L, Hummel R, et al. : Remote anesthetic monitoring using satellite telecommunications and the internet. Anesth Analg 2006; 102:1463–1467 [DOI] [PubMed] [Google Scholar]
- 18.Foronda CL, Crenshaw N, Briones PL, et al. : Teaching and learning the skill of intubation using telehealth glasses. Clin Simul Nurs 2020; 40:31–35 [Google Scholar]
- 19.Mosier J, Joseph B, Sakles JC: Telebation: Next-generation telemedicine in remote airway management using current wireless technologies. Telemed J E Health 2013; 19:95–98 [DOI] [PubMed] [Google Scholar]
- 20.Sibert K, Ricci MA, Caputo M, et al. : The feasibility of using ultrasound and video laryngoscopy in a mobile telemedicine consult. Telemed J E Health 2008; 14:266–272 [DOI] [PubMed] [Google Scholar]
- 21.Sakles JC, Mosier J, Hadeed G, et al. : Telemedicine and telepresence for prehospital and remote hospital tracheal intubation using a GlideScope™ videolaryngoscope: A model for tele-intubation. Telemed J E Health 2011; 17:185–188 [DOI] [PubMed] [Google Scholar]
- 22.Aminoff H, Meijer S, Arnelo U, et al. : Telemedicine for remote surgical guidance in endoscopic retrograde cholangiopancreatography: Mixed methods study of practitioner attitudes. JMIR Form Res 2021; 5:e20692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baribeau Y, Sharkey A, Chaudhary O, et al. : Handheld point-of-care ultrasound probes: The new generation of POCUS. J Cardiothorac Vasc Anesth 2020; 34:3139–3145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brinne Roos J, Bergenzaun P, Groth K, et al. : Telepresence-teleguidance to facilitate training and quality assurance in ERCP: A health economic modeling approach. Endosc Int Open 2020; 8:E326–E337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Adachi T, Sato A, Kuroki K, et al. : Audiovisual telesupport system for cardiovascular catheter interventions: A preliminary report on the clinical implications. Catheter Cardiovasc Interv 2020; 95:906–910 [DOI] [PubMed] [Google Scholar]
- 26.Burckett-St Laurent DA, Cunningham MS, Abbas S, et al. : Teaching ultrasound-guided regional anesthesia remotely: A feasibility study. Acta Anaesthesiol Scand 2016; 60:995–1002 [DOI] [PubMed] [Google Scholar]
- 27.Kirkpatrick AW, McKee JL, McBeth PB, et al. : The Damage Control Surgery in Austere Environments Research Group (DCSAERG): A dynamic program to facilitate real-time telementoring/telediagnosis to address exsanguination in extreme and austere environments. J Trauma Acute Care Surg 2017; 83(1 Suppl 1):S156–S163 [DOI] [PubMed] [Google Scholar]
- 28.Dalesio NM, Lester LC, Barone B, et al. : Real-time emergency airway consultation via telemedicine: Instituting the pediatric airway response team board! Anesth Analg 2020; 130:1097–1102 [DOI] [PubMed] [Google Scholar]
- 29.Smischney NJ, Demirci O, Diedrich DA, et al. : Incidence of and risk factors for post-intubation hypotension in the critically ill. Med Sci Monit 2016; 22:346–355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Casey JD, Janz DR, Russell DW, et al. ; PreVent Investigators and the Pragmatic Critical Care Research Group: Bag-mask ventilation during tracheal intubation of critically ill adults. N Engl J Med 2019; 380:811–821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kirkpatrick AW, McKee JL, Netzer I, et al. : Transoceanic telementoring of tube thoracostomy insertion: A randomized controlled trial of telementored versus unmentored insertion of tube thoracostomy by military medical technicians. Telemed J E Health 2019; 25:730–739 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.