Summary:
Endoscopic-assisted or robotic nipple-sparing mastectomy (E-NSM or R-NSM) with direct-to-implant breast reconstruction is becoming an increasingly popular surgical treatment for breast cancer patients. However, existing surgical methods such as traditional two-dimensional endoscopic-assisted or robot-assisted surgery are time-consuming and expensive. A new innovative three-dimensional videoscope system is efficient but needs special instruments; additionally, the incision over the extramammary region near the anterior axillary line is still too invisible. This study took place from May 2020 to April 2021. This technique is suitable for patients with small- to moderate-sized breasts (C cup size and below; grade 0 to grade I ptotic breasts). We have now performed 30 procedures, including eight bilateral reconstructions. The average operative time (including axillary operation) of a unilateral reconstruction is 179 ± 40.96 minutes, and for bilateral reconstruction, it was 271 ± 45.29 minutes. The median follow-up time was 9.93 months. For the complications, only one patient presented with a mild depigmentation of the nipple and one patient presented with local cellulitis but recovered after oral administration of antibiotics. All patients were satisfied with their postoperative aesthetic outcome. We present a new surgical technique of E-NSM with direct-to-implant subpectoral breast reconstruction to achieve better results.
Takeaways
Question: We intend to present a new surgical technique for E-NSM with direct-to-implant subpectoral breast reconstruction to achieve better results.
Findings: We present a brand-new surgical approach to E-NSM with direct-to-implant subpectoral breast reconstruction with the concept of “HUAXI Hole 1,” which is recommended for young patients without breast ptosis. This new surgical technique has noteworthy advantages like no visible scar on either breast or body trunk, no need for special instruments, short operative time, financial friendliness, and easiness to learn and generalize.
Meaning: This new method for E-NSM with direct-to-implant subpectoral breast reconstruction could be the first choice of treatment for patients with indications of NSM who do not have breast ptosis.
INTRODUCTION
Endoscopic-assisted nipple-sparing mastectomy (E-NSM) or robotic nipple-sparing mastectomy with direct-to-implant breast reconstruction is becoming a new surgical treatment trend, which has had increasing demands and provides better cosmetic outcomes for breast cancer patients.1-3 Subpectoral breast implant reconstruction through a transaxillary approach is feasible and is being used more commonly.4 However, existing surgical methods such as the traditional two-dimensional endoscopic-assisted or robot-assisted surgery, are time-consuming and expensive.5–7 A new innovative three-dimensional video system is efficient but needs special instruments; additionally, the incision over the extramammary region near the anterior axillary line is still too invisible8 when compared with the incision at the highest axillary natural fold. After 2 years of study, here we present a brand-new surgical approach for E-NSM with direct-to-implant subpectoral implant breast reconstruction, which is recommended in young patients without breast ptosis or in patients who need a bilateral reconstruction.
MATERIALS AND METHODS
This study took place from May 2020 to April 2021. This technique is suitable for patients with small- to moderate-sized breasts (C cup size and below; grade 0 to grade I ptotic breasts). The median age of the patients was 44.88 years ranging from 24 to 56 years, and the median body mass index was 21.75 ranging from 17.58 to 30.18 kg/m2.
SURGICAL PROCEDURE
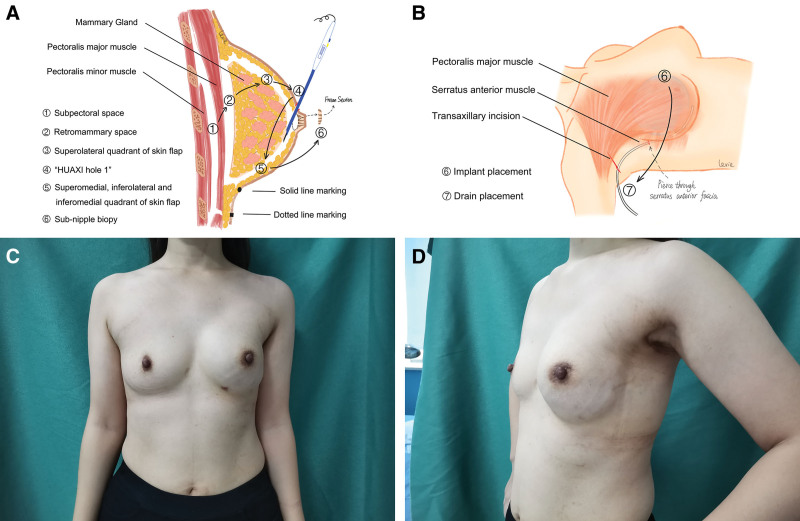
The patient laid in the supine position with the ipsilateral arm abducted at 90 degrees. An approximately 5–7 cm mark at the highest axillary natural fold, a solid line mark at the inframammary fold (IMF) and a dotted line mark at 1.5 cm below the IMF were made. Then axillary lymph node dissection or a sentinel lymph node biopsy was performed manually by an electric scalpel, if needed. Under direct vision and by using an electric scalpel, a 5 cm range of dissection of the posterior space of the pectoralis major and a 2 cm range of dissection of the retromammary space were performed to build an endoscopic working space. Next, the lapprotector, wrapped by the opening end of a sterile surgical glove (#6), was placed as the endoscopic port. Two bladeless trocars (Aesculap EJ701R, EJ751R) were inserted into two fingerholes of the glove, which created entries for the coagulation hook (Aesculap GK372R+GK384R) and the endoscope (KARL-STORZ). During the endoscopic procedure, insufflation with carbon dioxide (CO2) with the air pressure kept at 10–12 mm Hg was used to maintain the patency of the surgical air cavity. After endoscopic setup, the subpectoral space was dissected by using a coagulation hook, from the parasternal line and running medially to the dotted line that was marked inferiorly and to the serratus anterior fascia laterally using the coagulation hook. It should be noted that the serratus anterior fascia was lifted along with the pectoral major muscle to later cover the implant. Next, the medial and inferior attachment points of the pectoralis major were transected along the dotted lines using an ultrasonic knife (Ethicon Endo-Surgery HAR36) to avoid bleeding. The retromammary space was dissected inferiorly to the solid line (IMF) (it was important not to dissect beyond the IMF; therefore, the cut end of the pectoralis major was still attached to the IMF spot) using the coagulation hook due to the loose tissue. It was important that this dissection was performed underneath the pectoralis major fascia considering the oncological safety and to avoid damaging the serratus anterior fascia for the coverage of the implant. Next was the skin flap dissection. The superolateral quadrant of the skin flap was dissected under direct vision. The dissection of the nipple areolar complex region was performed under direct vision for small breasts but was performed under endoscopic vision for large breasts. At the superolateral margin of the areola (“HUAXI Hole 1”), a 5 mm incision named after our center, was made for inserting the electric scalpel (Peng’s electric dissector, Shuyou SY-IIA-2) into the air cavity, and then the remaining quadrant of the skin flap was dissected under endoscopic vision. The mammary gland was then excised via a transaxillary incision. Then, a subnipple biopsy for frozen sections was performed by taking specimens under the nipple areolar complex under direct vision, which determined whether the nipple areolar complex should be spared or excised. One drain was subsequently placed through the transaxillary incision. The implant was then inserted via the trans-axillary incision. The drain was removed when there was less than 30 mL of discharge for 3 consecutive days. After the surgery, the patients continuously wore postsurgical compression shapewear for 3 months. A schematic diagram of the surgical process is shown in Figure 1A, B and Supplemental Video. The postoperative results are shown in Figure 1C, D. (See Video [online], which displays E-NSM with direct-to-implant subpectoral breast reconstruction.)
Fig. 1.
Schematic diagram of surgical process and postoperative results. A, Surgical process (Part 1). B, Surgical process (Part 2). C, Postoperative results (front view, left reconstruction). D, Postoperative results (lateral view, left reconstruction).
Video 1. Endoscopic-assisted nipple-sparing mastectomy.This video displays endoscopic-assisted nipple-sparing mastectomy with direct-to-implant subpectoral breast reconstruction.
RESULTS
We have now performed 30 procedures, including eight bilateral breast reconstructions. The average surgical time (including axillary operation) of a unilateral reconstruction was 179 ± 40.96 minutes, and the average operative time for a bilateral reconstruction was 271 ± 45.29 minutes. The median follow-up time was 9.93 months. With regard to the complications, only one patient had a mild depigmentation of the nipple, and one patient developed a local cellulitis but recovered after oral antibiotics. No other complications (such as hemorrhage, ischemia, or necrosis) occurred. All of the patients were very satisfied with the postoperative aesthetic results.
DISCUSSION
Comparing with our operative time, the mean operative time was 347 minutes for the long blade light retractor method (including axillary operation).9 Robot-assisted mastectomy with implant breast reconstruction takes approximately 150 minutes without auxiliary operations and 351 minutes with auxiliary operations.5,10 Robot-assisted surgery also significantly increases the financial burden. Research has shown that the robot-assisted group’s surgery costs $3732 more than the surgery would cost in the endoscopic-assisted group.6, 11
Our new surgical technique achieves better results because of three strengths. First, we changed the dissection order of the layers. We have taken advantage of the tension formed by CO2 insufflation, which makes the breast a tent-like structure to dissect the subpectoral space fascia. The retromammary space and subcutaneous tissue are then dissected by utilizing insufflation tension combined with gravity of the pectoralis major muscle and mammary gland. Second, we introduced the concept of “HUAXI Hole 1,” through which we could insert the longest Peng’s electric dissector, allowing surgeons to easily reach the superomedial, inferiomedial, and inferiolateral quadrants. The strength of “HUAXI Hole 1” lies in the fact that it is not only convenient and efficient but also helps protect the skin flaps from being disturbed. Additionally, it compares favorably to 3D E-NSM and R-NSM in terms of cost.8 Furthermore, the incision of “HUAXI Hole 1” is so small (5 mm) that it leaves almost no visual scar on the breast, and there is a well-hidden transaxillary incision in the highest axilla, which improves the patients’ cosmetic needs compared with other techniques. Third, our procedure enables greater surgical vision and improved surgical efficiency without the need for retraction-type instruments, thereby overcoming problems such as tunnel vision of using retractors and dissectional difficulties from mammary glands falling after subcutaneous dissociation. Although the skin lift system solves the retractor difficulty, uneven forces on the dissectional layer still leads to poor surgical vision, dissectional difficulties, a prolonged operative time, and unsatisfactory surgical performance.
There are barriers to implementing this innovative surgery more broadly. The first is the learning curve and the familiarity with the surgical process. In our experience, approximately five surgeries could allow a surgeon to master this new technique as long as they have already mastered endoscopic surgeries. The second is that this new surgical technique is not indicated for patients with grade II and above ptotic breasts. In our opinion, if patients have indications of NSM and do not have breast ptosis, this new method could be the first choice of treatment. We believe our new method will provide benefits for many patients and we hope that it will become one of the routine options for breast reconstruction.
Footnotes
Published online 10 December 2021.
Drs. Zhang and Lee contributed equally to this work.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. This study was supported by grants from projects of the Science and Technology Department, Sichuan province, China under grants 2019YFH0146 and 2020YFS0199 and from Health Commission of Sichuan Province under Grant Research Project on Healthcare in Sichuan Province (2019-107).
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Leff DR, Vashisht R, Yongue G, et al. Endoscopic breast surgery: where are we now and what might the future hold for video-assisted breast surgery? Breast Cancer Res Treat. 2011;125:607–625. [DOI] [PubMed] [Google Scholar]
- 2.Angarita FA, Castelo M, Englesakis M, et al. Robot-assisted nipple-sparing mastectomy: systematic review. Br J Surg. 2020;107:1580–1594. [DOI] [PubMed] [Google Scholar]
- 3.Yang HJ, Ko G, Kim JH, et al. Implant delivery technique for prepectoral reconstruction after endoscopic-assisted nipple-sparing mastectomy. Plast Reconstr Surg Glob Open. 2021;9:e3623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Troilius C. Total muscle coverage of a breast implant is possible through the transaxillary approach. Plast Reconstr Surg. 1995;95:509–512. [DOI] [PubMed] [Google Scholar]
- 5.Toesca A, Peradze N, Galimberti V, et al. Robotic nipple-sparing mastectomy and immediate breast reconstruction with implant: first report of surgical technique. Ann Surg. 2017;266:e28–e30. [DOI] [PubMed] [Google Scholar]
- 6.Ahn SJ, Song SY, Park HS, et al. Early experiences with robot-assisted prosthetic breast reconstruction. Arch Plast Surg. 2019;46:79–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Toesca A, Invento A, Massari G, et al. Update on the feasibility and progress on robotic breast surgery. Ann Surg Oncol. 2019;26:3046–3051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lai HW, Chen ST, Mok CW, et al. Single-port 3-dimensional videoscope-assisted endoscopic nipple-sparing mastectomy in the management of breast cancer. Plast Reconstr Surg Glob Open. 2019;7:e2367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Franceschini G, Visconti G, Garganese G, et al. Nipple-sparing mastectomy combined with endoscopic immediate reconstruction via axillary incision for breast cancer: a preliminary experience of an innovative technique. Breast J. 2020;26:206–210. [DOI] [PubMed] [Google Scholar]
- 10.Park HS, Lee J, Lee DW, et al. Robot-assisted nipple-sparing mastectomy with immediate breast reconstruction: an initial experience. Sci Rep. 2019;9:15669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lai HW, Chen ST, Tai CM, et al. Robotic- versus endoscopic-assisted nipple-sparing mastectomy with immediate prosthesis breast reconstruction in the management of breast cancer: a case-control comparison study with analysis of clinical outcomes, learning curve, patient-reported aesthetic results, and medical cost. Ann Surg Oncol. 2020;27:2255–2268. [DOI] [PubMed] [Google Scholar]