Abstract
Limited data are available on changes in metabolic parameters in transgender youth on testosterone therapy in comparison with cisgender females. Data from 42 transgender males on testosterone therapy were retrospectively analyzed. Body mass index (BMI) and lipid profile changes were compared with BMI-matched females. There was a significant increase in BMI over time in the transgender males as compared with the cisgender females, and a decrease in high-density lipoprotein in the transgender males after starting testosterone therapy. Longitudinal prospective studies with cisgender controls are needed to better define effects of testosterone therapy in adolescents.
Keywords: adolescent, BMI, cholesterol, testosterone, transgender
Introduction
With expanding availability of and access to transgender care for youth, the number of transgender adolescents seeking medical transition is increasing.1 Recent studies have shown that about 1.8% of adolescents identify as transgender, representing an increase for the past decade.2 As transgender youth continue to experience higher rates of mental health concerns, including suicidality, gender-affirming therapies remain an important aspect of care in this population as these have been shown to improve mental health and well-being.3,4
Gender-affirming therapies may begin with pubertal suppression soon after the onset of puberty, followed by testosterone or estradiol.5 Although changes in metabolic parameters and myocardial infarction risk have been shown in adults taking testosterone,6,7 the cardiometabolic effects of gender-affirming hormones in pediatric populations remain unclear. Specifically, adult studies have shown an increase in cardiovascular risk factors such as an increase in triglycerides, low-density lipoprotein cholesterol (LDL-C), body mass index (BMI), insulin resistance, and blood pressure, as well as a decrease in high-density lipoprotein (HDL) after initiation of testosterone; however, longer-term studies show variable results on rates of actual cardiovascular events.6–8
Current clinical practice guidelines recommend counseling transgender youth and families about potential cardiometabolic effects of testosterone.5 However, recent studies demonstrate conflicting results on BMI changes and lipids after starting testosterone,9–13 and it remains unknown whether these changes are solely influenced by testosterone exposure or whether differences in diet and physical activity in a population with a higher incidence of mental health disorders14 also play a role. Furthermore, many studies have lacked a comparison group. To address this gap, this retrospective study examined changes in BMI and lipids in adolescent transgender males receiving testosterone, using a comparison group of BMI-matched cisgender female adolescents.
Methods
An IRB-approved retrospective study was conducted at a large Midwestern pediatric academic center with a multidisciplinary program serving transgender and gender-diverse youth. Transgender males (14–21 years) taking testosterone from 2014–2018 were eligible, and 53 were identified. Of these, 42 were seen at least twice and, therefore, included in assessment of BMI changes. Twenty-eight had lipid panels drawn, and 18 had laboratories both pre- and post-testosterone, with an average of 15.6 months between laboratory draws. Testosterone cypionate dosing started at 50 mg intramuscularly (IM) monthly and subsequently increased to 50–150 mg IM every other week.
Our Primary Care database was used to compile a comparison cohort of cisgender females (14–21 years) seen in our 13 primary care centers, without any chronic conditions such as attention deficit hyperactivity disorder, asthma, or conditions managed by our subspecialty clinics. BMI was calculated using age, sex assigned at birth, height and weight at time of visit, and is presented as a percentile. The 2000 Centers for Disease Control and Prevention (CDC) Growth Charts15 were used to calculate percentiles (where 5 to <85%ile is normal weight, 85 to <95%ile is overweight and ≥95%ile is obese). BMI z-scores were also calculated to help with differentiation at higher BMI percentiles. Initial BMIs of cisgender females were matched to the pre-testosterone BMIs of the transgender male cohort, and a random number generator used these matched patients to create a 2:1 match of cisgender females to the transgender males. Race and ethnicity were both classified as race within the electronic medical record.
Mean values with standard deviations were calculated to evaluate change in BMI of transgender male adolescents while on testosterone, as well as change in BMI for a similar time interval of the cisgender females. Both short- and long-term follow-ups were evaluated, with short-term follow-up assessing changes in BMI between each clinic visit, and long-term follow-up assessing changes in BMI between first and final follow-up clinic visits. A Shapiro–Wilk test was used to determine if continuous data had a normal distribution. Normally distributed independent data were evaluated with either a Student's t-test or paired t-test and nonparametric data with a Mann–Whitney U or Wilcoxon rank sum. Categorical variables (race/ethnicity) were compared using a Fisher's exact test.
Results
The transgender cohort had a mean age of 16.6 years (range 14–19 years) and was majority white, with bi-/multiracial subjects being the second most common race represented. The cisgender cohort had a mean age of 15.5 years (range 14–21 years) and was majority black/African American, with white subjects as the second most common racial group (Table 1).
Table 1.
Demographics and Baseline Characteristics
| Transgender males (n=42) | Cisgender females (n=82) | p | |
|---|---|---|---|
| Age at baseline (years) | 16.6±1.3 | 15.5±1.8 | 0.003 |
| Race/ethnicity | 0.0001 | ||
| White | 37 (88) | 19 (23.1) | |
| Black | 2 (5) | 40 (48.8) | |
| Latinx/Hispanic | 0 | 10 (12.2) | |
| Bi-/multiracial | 3 (7) | 3 (3.7) | |
| Asian | 0 | 6 (7.3) | |
| Not recorded | 0 | 4 (4.9) | |
| BMI | |||
| BMI percentile | 79 (63, 99) | 93 (71, 99) | 0.6 |
| BMI z-score | 1.4 (0.32, 2.3) | 1.5 (1.4, 1.6) | 0.6 |
| n=28 | n=26 | ||
|---|---|---|---|
| Lipids (mg/dL) |
|
|
|
| Total cholesterol |
156±30 |
166±30 |
0.7 |
| LDL-C |
87±29 |
97±26 |
0.5 |
| HDL |
45 (39, 59) |
44 (38, 54) |
0.4 |
| Triglycerides | 90 (69, 111) | 92 (63, 170) | 0.7 |
Values are mean±standard deviation if normally distributed, median (25, 75%ile) if not normally distributed, or n (%).
BMI, body mass index; HDL, high-density lipoprotein; LDL-C, low-density lipoprotein cholesterol.
There was a significant change in BMI percentile and z-score measured both between each visit, as well as for the entire follow-up period in the transgender male cohort after starting testosterone. Time between visits was an average of 4.9 months (range 0.5–17.7) and 5.0 months (range 0.8–21.0) for the transgender and cisgender cohorts, respectively, and an average total follow-up time of 10.8 months (range 2.6–25.7) and 12.7 months (range 1.0–27.1), respectively. The transgender group had an increase in BMI of +1.28 percentiles from visit to visit, and of +3.29 percentiles from baseline through final follow-up, whereas the cisgender group showed an opposite trend of a decrease in BMI of −0.70 percentiles from visit to visit and of −1.77 percentiles from baseline through final follow-up. BMI z-scores showed similar trends. In the transgender group, there was an increase in BMI z-score of +0.08 from visit to visit, and of +0.20 through the entire follow-up period. Conversely in the cisgender group, there was a BMI z-score decrease of −0.01 from visit to visit, and of −0.05 through the entire follow-up period. The difference in BMI percentiles and z-scores was significant when comparing the transgender and cisgender cohorts for both short- and long-term follow-up periods (Table 2). Of note, when comparing the prevalence of obesity in our transgender and cisgender cohorts (both 26.2%), we found it to be higher than that cited nationally (20.6%).16
Table 2.
Change in BMI Over Time in Transgender Males and Cisgender Females
| Mean change in BMI (%ile) | Mean change in BMI (z-score) | Time interval (mean, months) | p | |
|---|---|---|---|---|
| Transgender males (n=42) | ||||
| Short-term follow-up | 1.28 | 0.08 | 4.9 | 0.004 |
| Long-term follow-up | 3.29 | 0.2 | 10.8 | 0.002 |
| Cisgender females (n=82) | ||||
| Short-term follow-up | −0.7 | −0.01 | 5 | 0.004 |
| Long-term follow-up | −1.77 | −0.05 | 12.7 | 0.001 |
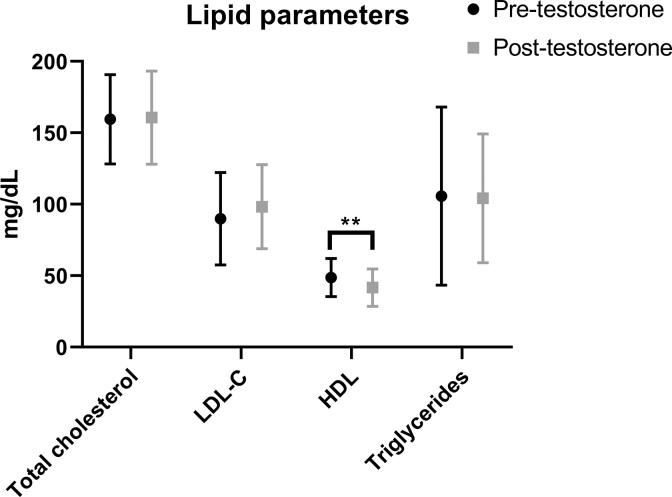
There were no significant differences between baseline lipid parameters between transgender males and cisgender females. Transgender males had a significant decrease in HDL (p<0.01) after testosterone exposure, with no changes in other lipid parameters (Fig. 1).
FIG. 1.
Lipid panels in transgender males before and after starting testosterone (n=18). **p<0.01. HDL, high-density lipoprotein; LDL-C, low-density lipoprotein cholesterol.
Discussion
We found a significant increase in BMI percentiles and z-scores in the transgender males after starting testosterone, as compared with the BMI-matched cisgender females for both shorter- and longer-term follow-up periods. This suggests that exogenous testosterone administration in adolescents who were assigned female at birth may lead to increased body mass over time. The smaller changes in BMI from visit to visit during a shorter follow-up period, as compared with the larger increase in BMI when examined for a longer follow-up period suggests that this may be an ongoing change with possible cumulative effect over time. These data highlight the need for longer-term studies to capture the full effects of testosterone therapy in this group. In addition to the increase in BMI over time, we also observed a decrease in HDL values in the transgender cohort after testosterone initiation. This is consistent with adult data showing a decrease in HDL after starting testosterone, as well as increases in BMI and LDL-C.17 This is important, as some adult literature suggests that lower HDL concentrations may correlate with an increased risk of coronary artery disease.18
Limited studies have examined metabolic changes after initiation of hormone therapy in transgender youth, generally without a comparison group. Similar to our findings, Jarin et al. found a significant decrease in HDL and increase in BMI in transgender adolescents on testosterone.10 Likewise, Sequeira et al. found a significant rise in BMI after 6 months of testosterone therapy, although noted that this effect lost significance 12 months after initiation.11 Olson-Kennedy et al. also found a significant decrease in HDL after starting testosterone in adolescent and young adult transgender males, although they noted an increase in triglycerides,9 which were stable in our study. A more recent study also found a lower HDL, as well as higher aspartate transaminase level in transgender males taking testosterone as compared with cisgender females.19 In addition, this study showed differences in body composition between transgender males on testosterone versus cisgender females, with a lower percentage body fat and more lean body mass in the transgender group, underscoring the need for further investigation of these parameters and their long-term implications.19 This finding of increased lean body mass after testosterone initiation has also been noted by Klaver et al.20
We attribute the notable racial differences between cisgender and transgender groups in our study to differences in the populations seen at our center for gender concerns versus primary care services, as well as a higher overall prevalence of overweight and obesity in the African American and Latino American communities16 (given that our comparison cohort was matched by starting BMI). Compared with national data describing BMI trends in American adolescents, our transgender male cohort had a higher prevalence of obesity than average for their age group, with 26.2% obesity rate as compared with 20.6% nationally.16 This could have implications in expected BMI trajectories for each cohort based on population data. In addition, given that the BMI-matched cisgender cohort was on average 1.1 years younger than the transgender group, one might expect that group to have an overall faster rate of weight gain, as standard CDC growth charts show a progressive slowing of weight gain between ages 14 and 17 years in cisgender females. Conversely, our data show that the slightly older transgender male group actually demonstrated more weight gain for the time period measured. Despite this racial discrepancy and limitations related to retrospective study design, small sample size, single site data collection, and variable length of follow-up, our use of a BMI-matched cisgender comparison group adds important information about implications of hormonal therapy for transgender youth. Further studies should investigate how possible changes in eating patterns, physical activity, long-term psychological benefit from hormones, and other medications prescribed could impact this increasing BMI trend as well.
Given that only retrospective and cross-sectional data are currently available, larger longitudinal prospective studies are needed to better define effects of testosterone therapy in transgender and gender-diverse adolescents. This would allow practitioners to provide more comprehensive counseling about gender-affirming hormone therapy to these youth and their families, and potentially refine guidelines for laboratory monitoring and diet/lifestyle interventions in those on testosterone. Since a decrease in HDL and increase in BMI appear to be the most consistent findings across studies, long-term clinical implications of these changes should be studied in this population. Although cardiometabolic outcomes remain poorly understood, there is evidence supporting improved mental health outcomes with medical transition that includes gender-affirming hormones.14 Long-term improvement in mental health may ultimately impact BMI changes differently as well. As such, it is critical to weigh any potential cardiometabolic risk of testosterone against potential psychosocial benefit given the morbidity and mortality associated with anxiety and depression in transgender adolescents.14
Abbreviations Used
- BMI
body mass index
- CDC
Centers for Disease Control and Prevention
- HDL
high-density lipoprotein
- IM
intramuscularly
- LDL-C
low-density lipoprotein cholesterol
Author Disclosure Statement
A.V., A.B., G.C., J.I., S.L., L.N.: No competing financial interests exist. N.N.: Previously consulted for Antares Pharma, Inc.
Funding Information
A.V. received funding through National Institutes of Health/National Institutes of Diabetes and Digestive and Kidney Diseases (5T32DK063687-17). N.N. received funding through the National Institutes of Health/National Institute of Child Health and Human Development (K12 HD 057022).
Cite this article as: Valentine A, Nokoff N, Bonny A, Chelvakumar G, Indyk J, Leibowitz S, Nahata L (2021) Cardiometabolic parameters among transgender adolescent males on testosterone therapy and body mass index-matched cisgender females, Transgender Health 6:6, 369–373, DOI: 10.1089/trgh.2020.0052.
References
- 1. Chen M, Fuqua J, Eugster EA. Characteristics of referrals for gender dysphoria over a 13-year period. J Adolesc Health. 2016;58:369–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Johns MM, Lowry R, Andrzejewski J, et al. . Transgender identity and experiences of violence victimization, substance use, suicide risk, and sexual risk behaviors among high school students—19 states and large urban school districts, 2017. MMWR Morb Mortal Wkly Rep. 2019;68:67–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Thoma BC, Salk RH, Choukas-Bradley S, et al. . Suicidality disparities between transgender and cisgender adolescents. Pediatrics. 2019;144:e20191183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Connolly MD, Zervos MJ, Barone CJ, et al. . The mental health of transgender youth: advances in understanding. J Adolesc Health. 2016;59:489–495. [DOI] [PubMed] [Google Scholar]
- 5. Hembree WC, Cohen-Kettenis PT, Gooren L, et al. . Endocrine treatment of gender-dysphoric/gender-incongruent persons: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2017;102:3869–3903. [DOI] [PubMed] [Google Scholar]
- 6. Nota NM, Wiepjes CM, de Blok CJM, et al. . Occurrence of acute cardiovascular events in transgender individuals receiving hormone therapy. Circulation. 2019;139:1461–1462. [DOI] [PubMed] [Google Scholar]
- 7. Maraka S, Singh Ospina N, Rodriguez-Gutierrez R, et al. . Sex steroids and cardiovascular outcomes in transgender individuals: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2017;102:3914–3923. [DOI] [PubMed] [Google Scholar]
- 8. Dutra E, Lee J, Torbati T, et al. . Cardiovascular implications of gender-affirming hormone treatment in the transgender population. Maturitas. 2019;129:45–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Olson-Kennedy J, Okonta V, Clark LF, Belzer M. Physiologic response to gender-affirming hormones among transgender youth. J Adolesc Health. 2018;62:397–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jarin J, Pine-Twaddell E, Trotman G, et al. . Cross-sex hormones and metabolic parameters in adolescents with gender dysphoria. Pediatrics. 2017;139:e20163173. [DOI] [PubMed] [Google Scholar]
- 11. Sequeira GM, Kidd K, El Nokali NE, et al. . Early effects of testosterone initiation on body mass index in transmasculine adolescents. J Adolesc Health. 2019;65:818–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Stoffers IE, de Vries MC, Hannema SE. Physical changes, laboratory parameters, and bone mineral density during testosterone treatment in adolescents with gender dysphoria. J Sex Med. 2019;16:1459–1468. [DOI] [PubMed] [Google Scholar]
- 13. Klaver M, de Mutsert R, van der Loos M, et al. . Hormonal treatment and cardiovascular risk profile in transgender adolescents. Pediatrics. 2020;145:e20190741. [DOI] [PubMed] [Google Scholar]
- 14. de Vries AL, McGuire JK, Steensma TD, et al. . Young adult psychological outcome after puberty suppression and gender reassignment. Pediatrics. 2014;134:696–704. [DOI] [PubMed] [Google Scholar]
- 15. Kuczmarski RJ, Ogden CL, Guo SS, et al. . 2000 CDC Growth charts for the United States: methods and development. Vital Health Stat 11. 2002;246:1–190. [PubMed] [Google Scholar]
- 16. Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of obesity among adults and youth: United States, 2011–2014. NCHS Data Brief. 2015;219:1–8. [PubMed] [Google Scholar]
- 17. Velho I, Fighera TM, Ziegelmann PK, Spritzer PM. Effects of testosterone therapy on BMI, blood pressure, and laboratory profile of transgender men: a systematic review. Andrology. 2017;5:881–888. [DOI] [PubMed] [Google Scholar]
- 18. Emerging Risk Factors Collaboration, Di Angelantonio E, Sarwar N, et al. . Major lipids, apolipoproteins, and risk of vascular disease. JAMA. 2009;302:1993–2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nokoff NJ, Scarbro SL, Moreau KL, et al. . Body composition and markers of cardiometabolic health in transgender youth compared with cisgender youth. J Clin Endocrinol Metab. 2020;105:e704-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Klaver M, Dekker M, de Mutsert R, et al. . Cross-sex hormone therapy in transgender persons affects total body weight, body fat and lean body mass: a meta-analysis. Andrologia. 2017;49:1–11. [DOI] [PubMed] [Google Scholar]