Abstract
Purpose: This study aims to describe health inequities experienced by transgender Hispanic (TH) individuals in the United States.
Methods: This retrospective case–control study used the Behavioral Risk Factor Surveillance System (BRFSS) data from 2014 to 2018. Propensity score matching and logistic and negative binomial regression were used to compare TH survey respondents with other relevant populations across the following outcomes: health care access, health risk factors, self-reported chronic conditions, and perceived health status.
Results: Relative to transgender White (TW) respondents, TH respondents (n=414) were less likely to report having health insurance (odds ratio [OR]: 0.35, p<0.001), a regular provider (OR=0.40, p<0.001), and were more likely to report cost barriers to care (OR=1.85, p<0.001) and HIV risk factors (OR=2.41, p<0.001). Similar results were found when comparing outcomes with cisgender White respondents. TH respondents reported fewer days of poor health (rate ratio [RR]=0.67, p<0.001), activity limited days (RR=0.64, p=0.011), and were less likely to report depression (OR=0.44, p<0.001) than TW respondents. Relative to cisgender Hispanic (CH) respondents, TH respondents experienced more cost barriers (OR=1.56, p=0.003), higher HIV risk (OR=3.38, p<0.001), and more activity limited days (RR=2.93, p<0.001).
Conclusion: Our results demonstrate that TH individuals may be less likely to have access to health care and have poorer health-related quality-of-life when compared with either CH or TW individuals. It is vital that additional research further elucidate the challenges faced by this multiply marginalized population including racism and transphobia. Further health care solutions should be responsive to the unique challenges of the TH population at the individual and institutional level.
Keywords: intersectionality, health inequities, BRFSS, Hispanic, epidemiology, transgender
Introduction
Transgender individuals and members of racial/ethnic minority groups belong to marginalized populations that experience severe health inequity in the United States. Members of these groups are subjected to oppression in the form structural racism1 and transphobia,2 which coalesce to limit socioeconomic resources and drive poor health outcomes. For transgender individuals, these inequities include mental health disorders, such as anxiety, depression, suicidality, substance use disorder,3–5 and HIV,5,6 among others. For racial/ethnic minorities, these inequities include asthma,7 cardiovascular disease,8 and diabetes,9 among others. Specifically, prior studies have shown that the prevalence of asthma in the United States is highest among Puerto Ricans compared with other racial/ethnic groups.10 Similarly, the prevalence of diabetes is higher among Hispanics than non-Hispanic Whites, although there is considerable variation between Hispanic subpopulations, with prevalence estimates as low as 10.2% among South Americans and as high as 18.3% among Mexican Americans.11 However, cardiovascular disease shows a different trend with prevalence of coronary heart disease, stroke, and related risk factors, smoking and hypertension, being lower among Hispanics than non-Hispanic Whites.12,13
Given that individuals carry multiple social identities, it is important for investigators to have a systematic approach to study how experiences related to these identities may shape health. Intersectionality is an important theoretical framework that allows us to contextualize individuals with multiple marginalized social identities (transgender, racial/ethnic minority) within the complex social inequalities that precipitate worse health outcomes. In the last decade, there has been an effort to incorporate intersectionality in framing research on marginalized populations,14,15 and recent efforts have been focused on using intersectionality to refine quantitative methods.16,17
Currently, there are a paucity of studies that specifically center health outcomes of individuals at the intersection of marginalized racial/ethnic groups and gender minorities. Our previous work has addressed this knowledge gap and characterized health inequities specifically faced by transgender Black individuals and demonstrated more limited health care access, increased self-reported cardiovascular disease prevalence, and worse perceived health status among the transgender Black population compared with both cisgender Black and transgender White (TW) populations in the United States.18 As with the transgender Black population, much of the current literature centering transgender Hispanic (TH) individuals has been focused on HIV and other sexually transmitted diseases or is limited to regional and health system constrained cohorts.19,20 The present study extends our work on intersectional transgender health by addressing health outcomes of the TH population and comparing health inequities relative to the cisgender White (CW) and cisgender Hispanic (CH) populations and the TH population using data from the Behavioral Risk Factor Surveillance System (BRFSS), a Centers for Disease Control and Prevention (CDC) national health survey in the United States.
Methods
The BRFSS is the largest continuous health survey system in the world. The survey is administered in partnership with all states and territories in the United States, via landline and cell phone, and is available in English and Spanish. The system captures information on sociodemographic factors, health behaviors, perceived health status, and self-reported chronic conditions for more than 400,000 adults per year.21 Beginning in 2014, BRFSS piloted an optional sexual orientation and gender identity (SOGI) module that allowed survey respondents to self-identify as transgender. By 2018, 37 states had administered the SOGI module at least once. This study uses de-identified, publicly available data and therefore did not require submission to the institutional review board for review or exemption.
Measures
Race/ethnicity
BRFSS ascertains race and Hispanic ethnicity separately. Individuals are allowed to self-report multiple racial identities and are asked to respond to the question, “Are you Hispanic, Latino/a, or of Spanish Origin?” to determine ethnicity.22–26 For this study, we include White respondents who did not identity as Hispanic, and Hispanic respondents of all racial identities.
Gender
The optional SOGI module in the BRFSS included the question, “Do you consider yourself to be transgender?,” and if yes, interviewers also asked, “Do you consider yourself to be (1) male-to-female, (2) female-to-male, or (3) gender nonconforming?” In this study, we adopt the preferred terminology of trans feminine, trans masculine, and other gender minority respondents, respectively, to reflect the most up-to-date and inclusive terminology when referring to subgroups. In this study, all individuals who responded affirmatively to the first question are included among transgender respondents.
Outcomes
The outcomes compared in this study fall into four categories: health care access, chronic conditions, risk factors, and perceived health status. All outcomes are self-reported in the BRFSS survey data. For health care access, we compare binary variables for (1) any form of health insurance, (2) access to at least one regular health care provider or personal doctor, and (3) experiencing a cost barrier to receiving care in the previous year. Cost barrier was based on response to “Was there a time in the past 12 months when you needed to see a doctor but could not because of cost?” For chronic conditions, we compare history of cardiovascular disease (stroke, myocardial infarction, or coronary heart disease), diabetes, pulmonary disease (asthma or chronic obstructive pulmonary disease), arthritis, and depression.
Risk factors used in our analysis include alcohol consumption, smoking status, and factors related to HIV infection. For alcohol consumption, we evaluate self-reported ≥1 episodes of binge drinking (≥4 drinks at one time) in the past 30 days to be consistent with previous studies.5,18 For HIV risk, BRFSS included a single item that assessed multiple factors and risk behaviors in aggregate, beginning in 2016. In 2016 and 2017, the item asked respondents to identify if, in the past year, they had (1) used intravenous drugs, (2) been treated for a sexually transmitted or venereal disease, (3) given or received money or drugs in exchange for sex, (4) had anal sex without a condom, or (5) had four or more sex partners. In 2018, the number of sex partners was removed as a criterion.24–26
Perceived health status is measured using four health-related quality-of-life items (HRQOL-4) included in the BRFSS.27 The HRQOL-4 is a validated instrument that captures respondent perception of their physical and mental health and serves as a proxy for acute and chronic disease burden. The HRQOL-4 asks self-rated health (excellent, good, fair, or poor). For our analysis, we follow the CDC recommendation and include outcomes for fair or poor health, severe mental distress (≥14 days of poor mental health), number of days in poor mental or physical health in the past 30 days, and number of activity limited days due to poor physical or mental health.27
Statistical analysis
The BRFSS includes survey weights that, in principle, can be used for design-based analyses to approximate the entire U.S. population. However, the BRFSS weights are based on sex, which is identified by the interviewer based on their perception of the vocal timbre of the respondent, and questions that do not distinguish between natal sex and gender identity.28,29 This method has been shown to misclassify natal sex for transgender individuals by nearly 30%, which introduces differential error that might bias analyses on health outcomes in transgender populations.28 Therefore, we use a modified case–control study structure, matching Hispanic transgender respondents to control individuals. We build three types of matched sets, one matching TH respondents to CW respondents, another matching TH respondents to CH respondents, and a last set matching TH respondents to TW respondents for each outcome. This approach is consistent with the recommendation of a study of bias introduced by the BRFSS survey weights30 and the methods used in our previous study.18 Consistent with previous multiyear studies using BRFSS data to study sexual and gender minority populations, we pool data across years in our analyses.5,31
We use optimal matching based on propensity scores to generate 1:3 matched sets of TH respondents per comparison group per outcome.32 The matching algorithm uses an ensemble of methods that included generalized gradient boosted regression, random forests, and logistic regression, this allows for robust propensity score estimation and relaxes the assumptions of traditional parametric procedures.33,34 In our analyses, we match on age, income, census region, and marital status. These covariates are selected to be consistent with previous studies of risk factors and self-reported health status for gender minority studies.5,18 We evaluate covariate balance based on absolute standardized mean difference (ASMD) with a strict threshold of adequate balance (ASMD ≤0.1).35 Any covariates not adequately balanced are adjusted for in regression analyses. For binary outcomes, we use conditional logistic regression to estimate the odds ratio (OR) and confidence intervals (CIs), and for count outcomes, number of days in the past 30 days, we use negative binomial regression treating matched sets as fixed effects and estimating rate ratios (RRs) and CIs.
To adjust for multiple testing across the 16 outcomes included in this study, we use the Bonferroni correction with a per test type I error rate of (α=0.05/16=0.0031) and calculate 100(1 − α)=99.69% CIs to ensure an overall type I error rate of 0.05 for each set of comparison.36
Results
The data included 733,492 CW, non-Hispanic respondents, 61,129 CH respondents, 2729 TW, non-Hispanic respondents, and 414 TH respondents. Table 1 shows the breakdown of TH and TW individuals by gender identity, with the majority in both groups being trans feminine (43.0% and 46.2%, respectively), followed by trans masculine (32.6% and 33.1%, respectively) and other gender minorities (24.4% and 20.7%, respectively). Table 2 shows that a plurality of TH respondents was White (n=204, 49.3%), with the next largest category being grouped as “Other” (n=57, 13.8%), followed by Black Hispanics (n=33, 8.0%). Table 3 shows the distribution of covariates used in the matching algorithms, which include demographic characteristics (age, census division, education, household income, and marital status) and the number of chronic conditions (0, 1, or ≥2) across all four groups. The CW population tended to be older than the CH and both transgender groups.
Table 1.
Gender Identity Among White, Non-Hispanic, and Hispanic Transgender Respondents to Behavioral Risk Factor Surveillance System 2014–2018
| Hispanic (n=414) | White, non-Hispanic (n=2729) | |
|---|---|---|
| Trans feminine, n (%) | 178 (43.0) | 1260 (46.2) |
| Trans masculine, n (%) | 135 (32.6) | 903 (33.1) |
| Other gender minority, n (%) | 101 (24.4) | 566 (20.7) |
Table 2.
Racial Identity Among Transgender Hispanic Respondents to Behavioral Risk Factor Surveillance System 2014–2018
| Race | Count (%) |
|---|---|
| Asian | 11 (2.7) |
| Black | 33 (8.0) |
| Native American | 13 (3.1) |
| Native Hawaiian or Other Pacific Islander | 19 (4.6) |
| White | 204 (49.3) |
| Multiracial | 24 (5.8) |
| Other | 57 (13.8) |
| Not sure | 31 (7.5) |
| Refused | 22 (5.3) |
Table 3.
Demographics of Cisgender and Transgender White and Hispanic Respondents to Behavioral Risk Factor Surveillance System 2014–2018
| Cisgender White (N=733,492) | Cisgender Hispanic (N=61,129) | Transgender White (N=2729) | Transgender Hispanic (N=414) | |
|---|---|---|---|---|
| Age, years, n (%) | ||||
| 18–24 | 29,698 (4.0) | 7223 (11.8) | 271 (9.9) | 82 (19.8) |
| 25–34 | 55,827 (7.6) | 12,301 (20.1) | 260 (9.5) | 100 (24.2) |
| 35–44 | 72,618 (9.9) | 12,996 (21.3) | 235 (8.6) | 81 (19.6) |
| 45–54 | 115,592 (15.8) | 11,296 (18.5) | 427 (15.6) | 66 (15.9) |
| 55–64 | 171,827 (23.4) | 8964 (14.7) | 625 (22.9) | 44 (10.6) |
| 65+ | 287,930 (39.3) | 8349 (13.7) | 911 (33.4) | 41 (9.9) |
| Census division, n (%) | ||||
| East North Central | 112,316 (15.3) | 4409 (7.2) | 443 (16.2) | 33 (8.0) |
| East South Central | 28,767 (3.9) | 389 (0.6) | 120 (4.4) | 5 (1.2) |
| Middle Atlantic | 94,050 (12.8) | 8412 (13.8) | 351 (12.9) | 65 (15.7) |
| Mountain | 57,243 (7.8) | 5660 (9.3) | 165 (6.0) | 20 (4.8) |
| New England | 81,441 (11.1) | 5978 (9.8) | 231 (8.5) | 43 (10.4) |
| Pacific | 49,304 (6.7) | 10,879 (17.8) | 162 (5.9) | 63 (15.2) |
| South Atlantic | 127,796 (17.4) | 9392 (15.4) | 568 (20.8) | 78 (18.8) |
| West North Central | 136,988 (18.7) | 5360 (8.8) | 541 (19.8) | 37 (8.9) |
| West South Central | 44,975 (6.1) | 10,094 (16.5) | 144 (5.3) | 67 (16.2) |
| Missing | 612 (0.1) | 556 (0.9) | 4 (0.1) | 3 (0.7) |
| Education, n (%) | ||||
| Less than high school | 36,247 (4.9) | 16,968 (27.8) | 269 (9.9) | 162 (39.1) |
| High school graduate | 201,061 (27.4) | 17,116 (28.0) | 998 (36.6) | 120 (29.0) |
| Some college | 202,254 (27.6) | 13,839 (22.6) | 751 (27.5) | 80 (19.3) |
| College graduate | 292,585 (39.9) | 12,939 (21.2) | 702 (25.7) | 50 (12.1) |
| Missing | 1345 (0.2) | 267 (0.4) | 9 (0.3) | 2 (0.5) |
| Household income, n (%) | ||||
| $0–$14,999 | 47,129 (6.4) | 9458 (15.5) | 323 (11.8) | 93 (22.5) |
| $15,000–$24,999 | 89,579 (12.2) | 13,897 (22.7) | 489 (17.9) | 108 (26.1) |
| $25,000–$34,999 | 64,826 (8.8) | 6861 (11.2) | 302 (11.1) | 51 (12.3) |
| $35,000–$49,999 | 90,910 (12.4) | 6516 (10.7) | 318 (11.7) | 31 (7.5) |
| $50,000–$74,999 | 108,389 (14.8) | 5428 (8.9) | 335 (12.3) | 24 (5.8) |
| ≥$75,000 | 227,533 (31.0) | 9290 (15.2) | 561 (20.6) | 45 (10.9) |
| Missing | 105,126 (14.3) | 9679 (15.8) | 401 (14.7) | 62 (15.0) |
| Marital status, n (%) | ||||
| Never married | 93,526 (12.8) | 14,595 (23.9) | 606 (22.2) | 144 (34.8) |
| Divorced, widowed, or separated | 213,214 (29.1) | 13,643 (22.3) | 796 (29.2) | 88 (21.3) |
| Married or coupled | 423,909 (57.8) | 32,559 (53.3) | 1314 (48.1) | 180 (43.5) |
| Missing | 2843 (0.4) | 332 (0.5) | 13 (0.5) | 2 (0.5) |
| No. of chronic conditions, n (%) | ||||
| None | 256,298 (34.9) | 33,125 (54.2) | 777 (28.5) | 216 (52.2) |
| 1 | 216,101 (29.5) | 15,081 (24.7) | 861 (31.6) | 80 (19.3) |
| ≥2 | 261,093 (35.6) | 12,923 (21.1) | 1091 (40.0) | 118 (28.5) |
Regionally, CH and TH respondents were more heavily concentrated in the Western (West North Central, West South Central) and Pacific census divisions compared with CW and TW respondents. Hispanic respondents (cisgender and transgender) on average completed less education and reported lower household incomes than White respondents. Marital status varied across groups, with CH, and TW and Hispanic respondents more likely to have never been married than CW respondents, Hispanic respondents less likely than White respondents to be divorced, widowed, or separated, and TH respondents were least likely to be married or coupled. For census division, education, household income, and marital status, missingness ranged from 0.1% to 0.9% across groups.
Table 4 shows the distribution of outcomes across group. The p-value for comparing the outcome distribution across all four groups was <0.001 for all outcomes based on one-way analysis of variance for continuous variables (days of poor physical or mental health, and activity limited days due to poor health) and the χ2 test for independence for binary variables (all other outcomes), indicating that health care access, risk factors, chronic conditions, and perceived health status varied across transgender and cisgender groups of White and Hispanic respondents.
Table 4.
Distribution of Health Care Access, Risk Factors, Chronic Conditions, and Perceived Health Status for Cisgender and Transgender White and Hispanic Respondents to Behavioral Risk Factor Surveillance System 2014–2018
| Cisgender White (N=733,492) | Cisgender Hispanic (N=61,129) | Transgender White (N=2729) | Transgender Hispanic (N=414) | |
|---|---|---|---|---|
| Health care access, n (%) | ||||
| Health insurance | 694,195 (94.6) | 45,108 (73.8) | 2482 (90.9) | 268 (64.7) |
| Regular provider | 641,429 (87.4) | 41,297 (67.6) | 2308 (84.6) | 248 (59.9) |
| Cost barriers | 59,438 (8.1) | 12,351 (20.2) | 335 (12.3) | 122 (29.5) |
| Risk factors, n (%) | ||||
| HIV risk factors | 15,157 (2.1) | 2850 (4.7) | 138 (5.1) | 69 (16.7) |
| HIV test in past year | 190,993 (26.0) | 26,522 (43.4) | 799 (29.3) | 186 (44.9) |
| Current smoker | 105,030 (14.3) | 7883 (12.9) | 505 (18.5) | 76 (18.4) |
| ≥1 Episode of binge drinking in past 30 days (≥4 drinks at one time) | 105,172 (14.3) | 9679 (15.8) | 431 (15.8) | 83 (20.0) |
| Chronic conditions, n (%) | ||||
| Cardiovascular disease | 89,991 (12.3) | 4241 (6.9) | 434 (15.9) | 50 (12.1) |
| Diabetes | 94,397 (12.9) | 8098 (13.2) | 442 (16.2) | 65 (15.7) |
| Pulmonary disease | 136,676 (18.6) | 9782 (16.0) | 599 (21.9) | 88 (21.3) |
| Arthritis | 269,758 (36.8) | 11,503 (18.8) | 996 (36.5) | 70 (16.9) |
| Depressive disorders | 143,716 (19.6) | 10,271 (16.8) | 821 (30.1) | 117 (28.3) |
| Perceived health status | ||||
| Fair or poor health, n (%) | 125,279 (17.1) | 15,816 (25.9) | 682 (25.0) | 109 (26.3) |
| Severe mental disturbance, n (%) | 73,774 (10.1) | 7214 (11.8) | 504 (18.5) | 91 (22.0) |
| Days of poor physical or mental health, mean (SD) | 6.49 (10.33) | 6.77 (10.37) | 9.15 (11.82) | 9.69 (12.08) |
| Activity limited days due to poor health, mean (SD) | 2.67 (7.17) | 2.58 (6.87) | 3.96 (8.29) | 5.05 (9.59) |
Test of difference across groups (Chi-squared test for counts, one-way analysis of variance for continuous days) was statistically significant (p<0.001) for all outcomes.
SD, standard deviation.
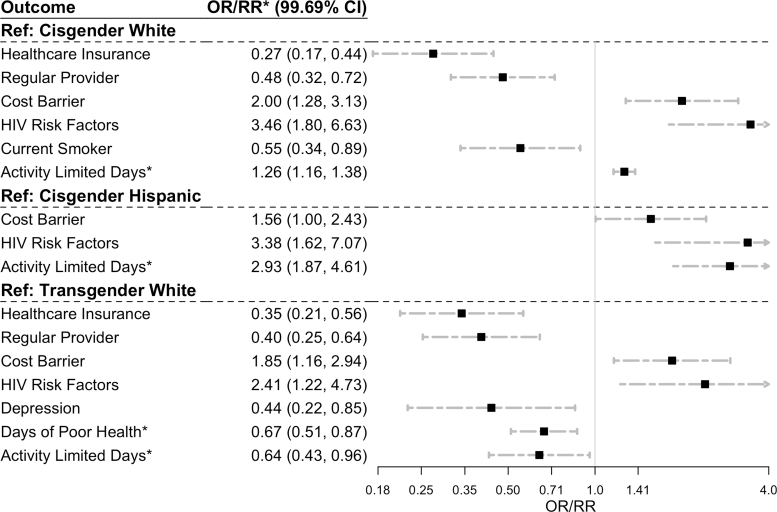
Figure 1 is a forest plot of the statistically significant estimated ORs and RRs with corresponding 99.69% CIs relating the outcomes to race/ethnicity and gender after matching on age, income, census region, and marital status. For all results, including those not statistically significant at the Bonferroni-corrected type I error rate (α=0.0031), see Table 5. Relative to CW respondents, TH respondents were less likely to report having health insurance (OR=0.27, 99.69% CI: 0.17–0.44), a regular provider (OR=0.48, 99.69% CI: 0.32–0.72), or be a current smoker (OR=0.55, 99.69% CI: 0.34–0.89), and were more likely to report experiencing cost barriers (OR=2.00, 99.69% CI: 1.28–3.13), report an HIV risk factor as defined by BRFSS (OR=3.46, 99.69% CI: 1.80–6.63), and reported more activity limited days due to poor health over the past 30 days (RR=1.26, 99.69% CI: 1.16–1.38).
FIG. 1.
Propensity score matched comparisons by outcome for transgender Hispanic respondents relative to cisgender White, cisgender Hispanic, and transgender White respondents. OR based on conditional logistic regression, *RR of number of days of past 30 days based on negative binomial regression with fixed effects for matched sets. OR, odds ratio; RR, rate ratio.
Table 5.
Measures of Association Comparing Transgender Hispanic with Cisgender White, Cisgender Hispanic, and Transgender White Respondents to Behavioral Risk Factor Surveillance System 2014–2018 in 1:3 Matched Sets per Comparison Group, per Outcome
| Sets (n) | Relative to cisgender White |
Relative to cisgender Hispanic |
Relative to transgender White |
||||
|---|---|---|---|---|---|---|---|
| OR (99.69% CI) | p | OR (99.69% CI) | p | OR (99.69% CI) | p | ||
| Health care access | |||||||
| Health care insurance | 347 | 0.27 (0.17–0.44) | <0.001 | 0.76 (0.49–1.18) | 0.0658 | 0.35 (0.21–0.56) | <0.001 |
| Regular provider | 343 | 0.48 (0.32–0.72) | <0.001 | 0.77 (0.50–1.17) | 0.0644 | 0.40 (0.25–0.64) | <0.001 |
| Cost barriers | 345 | 2.00 (1.28–3.13) | <0.001 | 1.56 (1.00–2.43) | 0.0028 | 1.85 (1.16–2.94) | <0.001 |
| Risk factors | |||||||
| HIV risk factors | 237 | 3.46 (1.8–6.63) | <0.001 | 3.38 (1.62–7.07) | <0.001 | 2.41 (1.22–4.73) | <0.001 |
| HIV test | 339 | 1.09 (0.74–1.61) | 0.4911 | 0.96 (0.64–1.43) | 0.7467 | 1.29 (0.86–1.95) | 0.0801 |
| Current smoker | 342 | 0.55 (0.34–0.89) | <0.001 | 1 (0.59–1.67) | 0.9796 | 0.69 (0.42–1.14) | 0.0209 |
| Binge drinking | 330 | 1.10 (0.68–1.77) | 0.5576 | 1.28 (0.81–2.04) | 0.1147 | 1.01 (0.62–1.66) | 0.7825 |
| Chronic conditions | |||||||
| Cardiovascular disease | 347 | 1.55 (0.77–3.11) | 0.0628 | 1.30 (0.45–3.74) | 0.4594 | 1.48 (0.44–4.97) | 0.3396 |
| Diabetes | 346 | 1.69 (0.92–3.1) | 0.0107 | 0.95 (0.44–2.07) | 0.8489 | 2.37 (0.88–6.37) | 0.0098 |
| Pulmonary disease | 347 | 0.80 (0.50–1.29) | 0.1649 | 0.78 (0.36–1.68) | 0.3412 | 1.23 (0.58–2.63) | 0.4125 |
| Arthritis | 342 | 0.60 (0.35–1.02) | 0.0046 | 0.48 (0.20–1.14) | 0.012 | 0.53 (0.25–1.11) | 0.0110 |
| Depression | 342 | 0.81 (0.53–1.25) | 0.1488 | 1.08 (0.56–2.08) | 0.7203 | 0.44 (0.22–0.85) | <0.001 |
| Perceived health status | |||||||
| Fair or poor health | 345 | 1.36 (0.87–2.13) | 0.0412 | 0.72 (0.41–1.24) | 0.0734 | 1.01 (0.61–1.67) | 0.9631 |
| Mental distress | 339 | 1.30 (0.8–2.13) | 0.1125 | 1.38 (0.81–2.34) | 0.0748 | 0.68 (0.41–1.13) | 0.0239 |
| RR (99.69% CI) | RR (99.69% CI) | RR (99.69% CI) | |||||
| Days of poor health | 342 | 0.93 (0.7–1.22) | 0.4189 | 1.22 (0.92–1.61) | 0.0396 | 0.67 (0.51–0.87) | <0.001 |
| Activity limited days | 340 | 1.26 (1.16–1.38) | <0.001 | 2.93 (1.87–4.61) | <0.001 | 0.64 (0.43–0.96) | 0.0011 |
OR based on conditional logistic regression, RR for number of days of past 30 days based on negative binomial regression with fixed effects for matched sets. Bold indicates statistically significant at the Bonferroni-corrected α < 0.0031 significance level.
CI, confidence interval; OR, odds ratio; RR, rate ratio.
Relative to CH respondents, TH respondents were more likely to report experiencing cost barriers (OR=1.56, 99.69% CI: 1.00–2.43), an HIV risk factor (OR=3.38, 99.69% CI: 1.62–7.07), and reported more activity limited days (RR=2.93, 99.69% CI: 1.87–4.61). Relative to TW respondents, TH respondents were less likely to report having health insurance (OR=0.35, 99.69% CI: 0.21–0.56), having a regular provider (OR=0.40, 99.69% CI: 0.25–0.64), depression (OR=0.44, 99.69% CI: 0.22–0.85), and reported fewer days of poor health (RR: 0.67, 99.69% CI: 0.51–0.87) and activity limited days (RR=0.64, 99.69% CI: 0.43–0.96). Relative to TW respondents, TH respondents were more likely to experience cost barriers to care (OR: 1.85, 99.69% CI: 1.16–2.94) and report an HIV risk factor (OR=2.41, 99.69% CI: 1.22–4.73).
Discussion
Our findings fill a critical knowledge gap and characterize the unique health inequities faced by the transgender Hispanic population in the United States. Our results demonstrate that health care access for the TH individuals may be more limited than for TW and CH individuals. Our results also show that self-reported HIV risk factors were two to four times higher among TH respondents than CW and CH respondents, and TW respondents. Despite reduced health care access, TH respondents were less likely than TW respondents to self-report a history of depression and reported 30% fewer days of poor health and days of activity limitations due to poor physical or mental health. Additionally, we found that TH respondents were less likely to endorse smoking status than CW respondents, which is consistent with prior studies of the U.S. Hispanic population across all gender identities that demonstrate lower prevalence of cardiovascular disease and risk factors (smoking and hypertension), among Hispanics compared with non-Hispanic Whites.
Our finding that TH respondents were less likely to report activity limited days than TW respondents warrants additional explanation. In our analyses, TH respondents were also less likely to endorse a history of depression, which may explain the lower amount of activity limited days due to poor mental or physical health. It is also possible that interpretation of activity limitation may vary across cultures, as well as willingness to report high levels of limitation or mental illness.
Framing this work in the appropriate social theory is necessary to achieve accurate interpretation and design appropriate interventions. Our study correlates health inequities with social identities. However, our findings are not evidence of intrinsic characteristics of individuals with these identities but rather point to structural factors that drive the inequitable distribution of health and resources. Specifically, we argue that the observed health inequities are the downstream effects of structural racism, “a system of hierarchy and inequity … that routinely advantages whites while producing cumulative and chronic adverse outcomes for people of color.”1 Intersectionality informs our work and explicates how analogues of structural racism, such as transphobia37,38 and other structural, institutional, and interpersonal forms of discrimination also contribute to inequities experienced by this multiply marginalized group, specifically demonstrated in the context of health care access in this study.
This study has a few limitations. While providing an important contribution to the literature on health inequities for the TH population in the United States, it does not elucidate a causal mechanism. Future studies are necessary in the intersectionality literature that identify causal mediators of inequities.7 These studies are constrained by both the quality of available data and methodological challenges. Data required for describing causal mechanism driving health inequities must include observations from majority and minority groups. Sources such as BRFSS fulfill that requirement but may ascertain minority status with suboptimal strategies that may bias results such as the one-question format previously discussed.
Additionally, sources such as BRFSS do not include information on health outcomes with the appropriate granularity for relevant minority populations. For example, the HIV risk factor question in the 2017 BRFSS survey ascertained intravenous drug use, recent sexually transmitted infections, unprotected anal sex, number of sex partners, and financial compensation for sex in aggregate per individual. Levels of risk and appropriate mitigating strategies for these different forms of potential exposure to HIV vary. Furthermore, a respondent with multiple risk factors may be at increased risk compared with a respondent with just one. And while the survey did specify barrier methods of protection when assessing sexually transmitted HIV risk, it did not assess pre-exposure prophylaxis usage or harm reduction behaviors as potentially modifying levels of HIV risk.39,40
In contrast, the U.S. Transgender Survey, which is explicitly designed for gender minorities, has survey items tailored to the transgender community but does not incorporate information from gender majority respondents so cannot be used to identify drivers of inequity across groups. Finally, traditional mediation analysis techniques do not account for complex mechanisms where there are multiple mediators and multiple comparison groups as is the case when studying multiply marginalized groups, but more contemporary methods are being developed.17,41
With respect to ethnicity, BRFSS collects data on Hispanic individuals without collecting information on demonstrably influential factors such as country-of-origin, immigration status, or immigrant generation.42–44 The U.S. Hispanic population shows significant heterogeneity as it encompasses nearly 20 distinct countries of origin as well as each country's own range of racial, ethnic, and linguistic diversity.45 As a result, major regional differences exist in the social and economic conditions of U.S. Hispanic populations depending on their composition.42,44,46 Future research on Hispanic or Latinx health, especially that which takes an intersectional approach, may stand to benefit from including more detailed questions so as not to treat U.S. Hispanics, a highly diverse group, as a homogeneous category. Finally, our sample size does not allow us to identify the health inequities unique to the Black Hispanic population as a group, an understudied group in public health research,47 and our study design does not disaggregate by gender identity, thereby obscuring differences between trans masculine and trans feminine groups.
Conclusion
Intersectionality is a useful framework that allows us to identify how structural inequalities can oppress multiply marginalized groups. Our study showed how individuals at the intersection of Hispanic and transgender identities face more severe health care access limitations than any intersecting group studied, as well as have significantly increased HIV risk based on metrics included in BRFSS. It is vital that additional research further elucidate the challenges of this vulnerable population and future health care solutions should be responsive to the unique challenges of the TH population in the United States at the individual and institutional level. Future interventions need to support resilience in this multiply marginalized population and capitalize on their strength while we work to dismantle systems of oppression that cause negative health outcomes among vulnerable populations.
Acknowledgments
The authors would like to thank the collaborators of the Trans Health Equity for Youth/Trans Health Equity Matters and the Black Health Scholars Network (BHSN) for their support of this work. E.L. would like to thank the Penn Medicine Office of Inclusion and Diversity, Center for Health Equity Advancement, and Program for Lesbian, Gay, Bisexual and Transgender Health. E.N.A. would like to thank the Robert Wood Johnson Foundation for their support. The authors would also like to thank Kellan E. Baker for curating the BRFSS data.
Abbreviations Used
- ASMD
absolute standardized mean difference
- BRFSS
Behavioral Risk Factor Surveillance System
- CDC
Centers for Disease Control and Prevention
- CH
cisgender Hispanic
- CI
confidence interval
- CW
cisgender White
- HRQOL-4
four health-related quality-of-life items
- OR
odds ratio
- RR
rate ratio
- SD
standard deviation
- SOGI
sexual orientation and gender identity
- TH
transgender Hispanic
- TW
transgender White
Authors' Contributions
E.L. conceptualized the study, conducted the statistical analyses, interpreted the results, and wrote the initial draft of the article. E.N.A. and S.B. co-wrote the initial draft of the article, helped interpret the results, and critically revised the article. N.D. helped conceptualize the study and critically revised the article.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
N.D. is supported by the National Institutes of Health (grant K23MH102128, principal investigator). E.N.A. is supported by the Robert Wood Johnson Foundation Health Policy Research Scholarship.
Cite this article as: Lett E, Asabor EN, Beltrán S, Dowshen N (2021) Characterizing health inequities for the U.S. transgender Hispanic population using the behavioral risk factor surveillance system, Transgender Health 6:5, 275–283, DOI: 10.1089/trgh.2020.0095.
References
- 1. Lawrence K, Keleher T. Structural racism. In: Race and Public Policy Conference, Berkeley, 2004. [Google Scholar]
- 2. Arayasirikul S, Wilson EC, Raymond HF. Examining the effects of transphobic discrimination and race on HIV Risk among transwomen in San Francisco. AIDS Behav. 2017;21:2628–2633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Reisner SL, Vetters R, Leclerc M, et al. Mental health of transgender youth in care at an adolescent urban community health center: a matched retrospective cohort study. J Adolesc Health. 2015;56:274–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. James SE, Herman JL, Rankin S, et al. The report of the 2015 US transgender survey. National Center for Transgender Equality. 2015, p. 302. www.transequality.org/sites/default/files/docs/USTS-Full-Report-FINAL.PDF (accessed July 1, 2020).
- 5. Baker KE. Findings from the Behavioral Risk Factor Surveillance System on health-related quality of life among US transgender adults, 2014–2017. JAMA Intern Med. 2019;179:1141–1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Becasen JS, Denard CL, Mullins MM, et al. Estimating the prevalence of HIV and sexual behaviors among the US transgender population: a systematic review and meta-analysis, 2006–2017. Am J Public Health. 2019;109:E1–E8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Canino G, McQuaid EL, Rand CS. Addressing asthma health disparities: a multilevel challenge. J Allergy Clin Immunol. 2009;123:1209–1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Safford MM, Brown TM, Muntner PM, et al. Association of race and sex with risk of incident acute coronary heart disease events. JAMA. 2012;308:1768–1774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Saydah S, Imperatore G, Cheng Y, et al. Disparities in diabetes deaths among children and adolescents—United States, 2000–2014. MMWR Morb Mortal Wkly Rep. 2017;66:502–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rosser FJ, Forno E, Cooper PJ, Celedón JC. Asthma in Hispanics: an 8-year update. Am J Respir Crit Care Med. 2014;189:1316–1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Schneiderman N, Llabre M, Cowie CC, et al. Prevalence of diabetes among Hispanics/Latinos from diverse backgrounds: the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Diabetes Care. 2014;37:2233–2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. US Department of Health and Human Services Office of Minority Health. Stroke and Hispanic Americans—the Office of Minority Health. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=73 (accessed September 18, 2020).
- 13. US Department of Health and Human Services Office of Minority Health. Heart disease and Hispanic Americans—the Office of Minority Health. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=64 (accessed September 18, 2020).
- 14. Bowleg L. The problem with the phrase women and minorities: intersectionality-an important theoretical framework for public health. Am J Public Health. 2012;102:1267–1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bauer GR. Incorporating intersectionality theory into population health research methodology: challenges and the potential to advance health equity. Soc Sci Med. 2014;110:10–17. [DOI] [PubMed] [Google Scholar]
- 16. Agénor M. Future directions for incorporating intersectionality into quantitative population health research. Am J Public Health. 2020;110:803–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bauer GR, Scheim AI. Methods for analytic intercategorical intersectionality in quantitative research: discrimination as a mediator of health inequalities. Soc Sci Med. 2019;226:236–245. [DOI] [PubMed] [Google Scholar]
- 18. Lett LA, Dowshen N, Baker KE. Intersectionality and health inequities for gender minority Blacks in the United States. Am J Prev Med. 2020;59:639–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nuttbrock L, Bockting W, Rosenblum A, et al. Gender abuse, depressive symptoms, and HIV and other sexually transmitted infections among male-to-female transgender persons: a three-year prospective study. Am J Public Health. 2013;103:300–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Clark H, Babu AS, Wiewel EW, et al. Diagnosed HIV infection in transgender adults and adolescents: results from the National HIV Surveillance System, 2009–2014. AIDS Behav. 2017;21:2774–2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Centers for Disease Control and Prevention. About the Behavioral Risk Factor Surveillance System (BRFSS). https://www.cdc.gov/brfss/about/index.htm (accessed November 25, 2019).
- 22. Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance. 2014 Codebook Report. 2015. https://www.cdc.gov/brfss/annual_data/2014/pdf/codebook14_llcp.pdf (accessed July 1, 2020).
- 23. Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance. 2015 Codebook Report. 2016. www.cdc.gov/brfss/annual_data/2015/pdf/codebook15_llcp.pdf (accessed July 1, 2020).
- 24. Centers for Disease Control and Prevention. System, Behavioral Risk Factor Surveillance. 2016 Codebook Report. 2017. https://www.cdc.gov/brfss/annual_data/annual_2017.html (accessed July 1, 2020).
- 25. Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance. 2017 Codebook Report. 2018. https://www.cdc.gov/brfss/annual_data/2017/pdf/codebook17_llcp-v2-508.pdf (accessed July 1, 2020).
- 26. Centers for Disease Control and Prevention. System BRFS. 2018 Codebook Report. 2019. https://www.cdc.gov/brfss/annual_data/2018/pdf/codebook18_llcp-v2–v508.pdf (accessed July 1, 2020).
- 27. Centers for Disease Control and Prevention. Measuring healthy days: population assessment of health-related quality of life. Vol. 53, 2000. https://www.cdc.gov/hrqol/pdfs/mhd.pdf (accessed July 1, 2020).
- 28. Tordoff D, Andrasik M, Hajat A. Misclassification of sex assigned at birth in the Behavioral Risk Factor Surveillance System and transgender reproductive health: a quantitative bias analysis. Epidemiology. 2019;30:669–678. [DOI] [PubMed] [Google Scholar]
- 29. Riley NC, Blosnich JR, Bear TM, Reisner SL. Vocal timbre and the classification of respondent sex in US phone-based surveys. Am J Public Health. 2017;107:1290–1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cicero EC, Reisner SL, Merwin EI, et al. Application of Behavioral Risk Factor Surveillance System sampling weights to transgender health measurement. Nurs Res. 2020;69:307–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Streed Jr CG, McCarthy EP, Haas JS. Self-reported physical and mental health of gender nonconforming transgender adults in the United States. LGBT Health. 2018;5:443–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hansen BB. Optmatch: flexible, optimal matching for observational studies. R News. 2007;7:18–24. [Google Scholar]
- 33. Pirracchio R, Petersen ML, Van Der Laan M. Improving propensity score estimators' robustness to model misspecification using Super Learner. Am J Epidemiol. 2015;181:108–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lee BK, Lessler J, Stuart EA. Improving propensity score weighting using machine learning. Stat Med. 2010;29:337–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Stuart EA, Lee BK, Leacy FP. Prognostic score-based balance measures can be a useful diagnostic for propensity score methods in comparative effectiveness research. J Clin Epidemiol. 2013;66:S84..e1–S90.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Abdi H. Bonferroni and Šidák corrections for multiple comparisons. Encycl Meas Stat. 2007;3:103–107. [Google Scholar]
- 37. Bowleg L, Huang J, Brooks K, et al. Triple jeopardy and beyond: multiple minority stress and resilience among Black lesbians. J Lesbian Stud. 2003;7:87–108. [DOI] [PubMed] [Google Scholar]
- 38. White Hughto JM, Reisner SL, Pachankis JE. Transgender stigma and health: a critical review of stigma determinants, mechanisms, and interventions. Soc Sci Med. 2015;147:222–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Riddell J, Amico KR, Mayer KH. HIV preexposure prophylaxis: a review. JAMA. 2018;319:1261–1268. [DOI] [PubMed] [Google Scholar]
- 40. Bayani A, Ghiasvand H, Rezaei O, et al. Factors associated with HIV testing among people who inject drugs: a meta-analysis. J Addict Dis. 2020;38:1–14. [DOI] [PubMed] [Google Scholar]
- 41. Bauer GR, Scheim AI. Advancing quantitative intersectionality research methods: intracategorical and intercategorical approaches to shared and differential constructs. Soc Sci Med. 2019;226:260–262. [DOI] [PubMed] [Google Scholar]
- 42. Bustamante AV, Fang H, Rizzo JA, Ortega AN. Understanding observed and unobserved health care access and utilization disparities among U.S. Latino adults. Med Care Res Rev. 2009;66:561–577. [DOI] [PubMed] [Google Scholar]
- 43. Madden EF, Qeadan F. Dialysis hospitalization inequities by Hispanic ethnicity and immigration status. J Health Care Poor Underserved. 2020;28:1509–1521. [DOI] [PubMed] [Google Scholar]
- 44. Hernández-Nieto R, Gutiérrez MC, Moreno-Fernández F. Hispanic Map of the United States 2017. 2017. http://cervantesobservatorio.fas.harvard.edu/sites/default/files/hispanic_map_2017en.pdf (accessed September 1, 2020).
- 45. Lopez MH, Dockterman D. U.S. Hispanic Country-of-Origin Counts for Nation, Top 30 Metropolitan Areas. 2011. https://www.pewresearch.org/hispanic/2011/05/26/us-hispanic-country-of-origin-counts-for-nation-top-30-metropolitan-areas/ (accessed September 1, 2020).
- 46. López-Cevallos DF, Gonzalez P, Bethel JW, et al. Is there a link between wealth and cardiovascular disease risk factors among Hispanic/Latinos? Results from the HCHS/SOL sociocultural ancillary study. Ethn Health. 2018;23:902–913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Cuevas AG, Dawson BA, Williams DR. Race and skin color in Latino health: an analytic review. Am J Public Health. 2016;106:2131–2136. [DOI] [PMC free article] [PubMed] [Google Scholar]