Abstract
Background
Early in 2020, mental health services had to rapidly shift from face-to-face models of care to delivering the majority of treatments remotely (by video or phone call or occasionally messaging) due to the COVID-19 pandemic. This resulted in several challenges for staff and patients, but also in benefits such as convenience or increased access for people with impaired mobility or in rural areas. There is a need to understand the extent and impacts of telemental health implementation, and barriers and facilitators to its effective and acceptable use. This is relevant both to future emergency adoption of telemental health and to debates on its future use in routine mental health care.
Objective
To investigate the adoption and impacts of telemental health approaches during the COVID-19 pandemic, and facilitators and barriers to optimal implementation.
Methods
Four databases (PubMed, PsycINFO, CINAHL, and Web of Science) were searched for primary research relating to remote working, mental health care, and the COVID-19 pandemic. Preprint servers were also searched. Results of studies were synthesized using framework synthesis.
Results
A total of 77 papers met our inclusion criteria. In most studies, the majority of contacts could be transferred to a remote form during the pandemic, and good acceptability to service users and clinicians tended to be reported, at least where the alternative to remote contacts was interrupting care. However, a range of impediments to dealing optimal care by this means were also identified.
Conclusions
Implementation of telemental health allowed some continuing support to the majority of service users during the COVID-19 pandemic and has value in an emergency situation. However, not all service users can be reached by this means, and better evidence is now needed on long-term impacts on therapeutic relationships and quality of care, and on impacts on groups at risk of digital exclusion and how to mitigate these.
Trial Registration
PROSPERO International prospective register of systematic reviews CRD42021211025; https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021211025
Keywords: telemental health; COVID-19; remote care; telemedicine; mental health; systematic review, implementation science
Introduction
Since the onset of the COVID-19 pandemic in the first few months of 2020, most countries have experienced a severe disruption of mental health service delivery in its usual forms [1]. Community-based outpatient, day and home treatment programs, prevention and mental health promotion programs, and services for specific age groups, such as older adults, children, and adolescents and people with substance misuse problems, have been among those severely affected at a time of potentially increased demand due to the adverse mental health consequences of the pandemic [2,3].
Mental health care providers around the world responded to the disruption of services in many ways, including the significant and widely documented shift to remote delivery of mental health services to replace in-person consultations [1,4,5]. Telemental health, defined as “the provision of behavioral and/or mental health care services using technological modalities in lieu of, or in addition to, traditional face-to-face methods” [6], including video conferencing, telephone, email or text messaging, has been central to continuing assessment and support in the community. Additionally, technological innovations are helping to address isolation and service disruption in hospital and residential settings [4,7].
Multiple research studies conducted both before and during the pandemic have reported evidence of the effectiveness of telemental health in reducing treatment gaps and improving access to care for a range of service users [8-10]. Findings from studies, often of telemental health programs established for purposes of research, have suggested that, overall, synchronous modalities such as video conferencing are comparable to face-to-face delivery in terms of quality of care, reliability of clinical assessments, and treatment outcomes and adherence [11-15]. Good levels of service user acceptance and satisfaction with telemental health services have also been reported [10]. Successful adoption of telemental health has been described across a wide range of populations (adult, child and adolescent, older people, ethnic minorities), settings (hospital, primary care, community), and conditions [11,13,16]. For certain populations, including some with autism and severe anxiety disorders, and those with physical disabilities or geographical barriers to accessing services, telemental health can be preferable for some service users [6,17], although individuals experiencing significant social disadvantage or severe mental health problems, such as psychosis, have been found to benefit less [18]. Research suggests that telemental health can also work for group interventions [19]. The attitudes of clinicians who have delivered care via synchronous telemental health appear to be largely positive, with professionals finding it both effective and acceptable [20] and recognizing its potential to enhance communication within and between mental health teams [4,7]. There is also some positive health economic evidence, with several studies suggesting telemental health is no more expensive than face-to-face delivery and tends to be more cost-effective [12]. This approach also appears to be a viable and inexpensive treatment option where access to emergency services is limited, and associations have been found with reduced psychiatric admissions [10].
However, despite this evidence base, integration of telemental health approaches into routine mental health care or the widespread adoption of remote working across whole systems has rarely been reported. Even during the pandemic, adoption of such technologies has been piecemeal, with utilization varying substantially both between and within countries [1,7]. Technological barriers to the wider adoption of telemental health include (1) the risk of digital exclusion of some service users, such as those facing significant social disadvantage or with limited technological access and expertise, and (2) the lack of technological infrastructure and clear protocols within services, impeding the integration of telemental health with face-to-face care [4,21,22]. Other barriers include difficulty in establishing and maintaining therapeutic relationships and in conducting high-quality assessments; service users who lack private space or find participating in sometimes intimate and distressing discussions from home intrusive [4,11,12,18,21-23]. A range of other ethical, regulatory, technological, cultural, and organizational barriers have also been identified, both before and during the pandemic [12,24-27].
The widespread emergency adoption of telemental health since the onset of the pandemic has generated a substantial literature. Numerous commentaries, service evaluations and reports of telemental health innovations, and service user, carer and staff experiences, in addition to a growing number of research studies addressing effectiveness and implementation issues [28-31] have been published internationally. Clinical guidelines have been rapidly produced in a number of countries [32].
A synthesis of the relevant empirical evidence gathered during the pandemic is therefore timely and informative for planning by generating evidence of effects of adopting telemental health across whole populations and service systems rather than in the context of relatively small-scale research studies involving volunteer participants. Capturing the learning and experiences gained through the rapid shift to telemental health will help optimize remote health care in a population that presents unique relational challenges associated with mental distress. It will also help to understand and overcome implementation barriers and inform strategies for improving the flexibility, effectiveness, and efficiency of mental health services through the sustained integration into routine care of telemental health approaches, to ensure that it brings the greatest benefits for patients, carers, and staff.
The aim of this review is to synthesize the international literature specific to remote working in mental health services (as a replacement for or in conjunction with face-to-face service delivery) in the context of early stages of the COVID-19 pandemic. The paper complements our previous umbrella review (systematic review of reviews) of literature on telemental health prior to the COVID-19 pandemic [15]: focusing on the literature from the pandemic period allows us to identify specified learning from the very wide implementation that occurred during this period. Our research questions are as follows:
What evidence has been obtained during the COVID-19 pandemic regarding the effectiveness and cost-effectiveness of telemental health and regarding its safety (including adverse events due to breaches of privacy and safety)?
What coverage has been achieved through telemental health adoption in the pandemic (including extent of adoption by services and reach among clinical populations in which it is adopted); in which groups and for which service settings is telemental health more or less likely to be implemented successfully; what are potential risks associated with digital exclusion for those not reached; and what barriers and facilitators influence success in implementation?
How acceptable are telemental health approaches to service users, carers, and staff as applied during the pandemic, including perceived impacts on therapeutic relationships, communication, and privacy?
What innovations and improvements have been introduced to make clinical care via telemental health more effective and acceptable, achieve greater coverage, and address barriers to delivering care in this way? (This includes descriptions and evaluations of specific strategies designed to make telemental health work better than usual delivery, and of adaptations of telemental health to specific settings, such as inpatient wards and crisis services).
Methods
A systematic review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [33]. The protocol for this review was registered with PROSPERO (CRD42021211025).
Search Strategy
Four electronic databases (PubMed, PsycINFO, CINAHL, and Web of Science), preprint servers medRxiv, PsyArXiv, Wellcome Open Research, and JMIR were searched for research relating to COVID-19, mental illness, and remote working from January 1 to December 9, 2020. An example search strategy can be found in Multimedia Appendix 1.
This search was supplemented by searching the references listed in included studies for any additional studies that met our inclusion criteria.
Screening
The resulting list of articles was deduplicated using Endnote [34] and all references were imported into Rayyan [35] for title and abstract screening. Full texts were sourced for articles deemed relevant for inclusion, and these were screened against the full review eligibility criteria. To establish consistency in study selection, title and abstract screening was conducted by 4 reviewers (MS, ZH, JH-S, and LSR), with 100% of included and 25% of excluded references checked by another reviewer (RA). Full texts were screened by 3 reviewers (RA, MB, and MS), with 100% of included and 25% of excluded papers checked by another reviewer (task divided between LG, HJ, JW, PB, and LSR). Any disagreements were resolved through team discussion.
Inclusion Criteria
Participants
Staff working within the field of mental health, people receiving organized mental health care for any condition (including addictions, dementia, and intellectual disability), family members or carers of people receiving mental health care (regarding their views on the impact of remote working on the service user, and interventions aimed at reducing carer distress). There are no age restrictions on participants in this review.
Interventions
Any form of spoken or written communication carried out between mental health professionals or between mental health professionals and service users/family members/unpaid carers or peer support communications using the internet, the telephone, text messaging platforms, or hybrid approaches combining different platforms.
Comparator(s)/Control
Any mental health communication delivered face-to-face, digitally or remotely, waitlist control, or placebo. Studies comparing different modes of delivery during the pandemic, and those comparing care delivery and outcomes during the pandemic with those before the pandemic were included. Relevant studies with no comparator were also included.
Outcomes
Qualitative and quantitative outcomes describing implementation effectiveness (including process evaluations) and barriers and facilitators to digital engagement, clinical effectiveness, cost-effectiveness, acceptability (including service user, carer, and staff satisfaction), impacts on communication and therapeutic relationships, coverage and impacts of digital exclusion, interventions to improve quality or coverage, improvements in quality of life, and economic impacts.
Design
Any papers that present qualitative or quantitative data from study designs of any type (including relevant service evaluations and case series). If the focus of the study was not solely remote working but the results section contained substantial data relevant to our research questions, these were also included. Any relevant reviews identified in the searches were checked for included research which met our inclusion criteria.
Exclusion Criteria
We excluded studies that were (1) not specific to the pandemic response; (2) reporting on interventions with patients with primary sleep disorders; (3) reporting on those with subclinical symptoms (unless combined with another included mental health problem); (4) focused on digital interventions such as apps, websites, and virtual reality tools, except where the sole purpose of the digital intervention was to facilitate direct spoken or written communication; (5) focused on interventions aimed at improving the mental health or well-being of health care professionals; and (6) editorials, opinion pieces, guidance documents, protocols, conference abstracts, and letters, with the exception of editorials or letters which contained primary research findings.
No language or location restrictions were applied in this review.
Data Extraction
Data extraction was supported by well-established implementation science frameworks. A data extraction form was developed based on a brief version of the Consolidated Framework for Implementation Research (CFIR) [36] and the taxonomy of implementation outcomes [37]. We used the higher-level CFIR constructs (see Table 2 in section Barriers and Facilitators to Telemental Health for a brief definition of each one of the implementation facets that CFIR constructs capture) to extract data on factors influencing implementation success [38], and the taxonomy of implementation outcomes including acceptability, adoption, and feasibility. We also extracted information deemed relevant based on previous studies conducted by the research team, including an umbrella review of pre-COVID-19 systematic reviews on telemental health and a qualitative study [15,21]. Data extracted consisted of study details, including design and focus of study; gender, ethnicity, age; diagnosis of participants; details of staff occupation; setting and context of study; intervention details, implementation outcomes (including acceptability, adoption, appropriateness, feasibility, fidelity, cost effectiveness, penetration, and sustainability); barriers and facilitators to implementation; and clinical and safety outcomes. The full data extraction form can be viewed in Multimedia Appendix 1.
Table 2.
Implementation barriers and drivers for telemental health grouped according to condensed CFIRa domains.
| CFIR domain | Findings | Example references |
| Intervention characteristics: Whether the intervention was internally/externally developed, evidence supporting the intervention, advantages compared with other methods of delivery, adaptability, trialability, and complexity |
|
[43,51,56,86,108,109] |
| Outer setting: Information on whether the organization is networked with others, peer pressure to implement intervention, and external policies and incentives |
|
[29,56,57,75] |
| Inner setting: Information on the structural characteristics, networks and culture of an organization, as well as the implementation climate (eg, capacity for change) |
|
[76,100,102,105] |
| Staff characteristics: Information on the following psychological attributes and also on any effects of staff demographic and professional backgrounds |
|
[43,52,111] |
| Process: Training provided and any processes put in place to support telemental health intervention, planning, and feedback on progress of implementation |
|
[7,28,44,45,50,59,61,62, 74,105,112,115] |
| Service user needs/resources: Statements demonstrating awareness of the needs and resources of those served by the organization (eg, barriers and facilitators and feedback) |
|
[50,62,77,86,98,116] |
aCFIR: Consolidated Framework for Implementation Research.
Data extraction was completed by 9 reviewers (AP, JW, MS, ER, RA, MT, JM, SS, HJ, approximately 8 studies each) using EPPI-Reviewer 4 [39]. All reviewers were trained on how to extract data to ensure consistency, and extracted data were checked by a second reviewer (RA & NVSJ). The extraction form was first piloted on 9/77 (12%) of included studies to assess usability and content, with amendments made before completing extraction for the whole data set.
Quality Appraisal
Given the diversity of the included article types and methods, 2 quality appraisal tools were used. Primary research studies were assessed with the Mixed Methods Appraisal Tool (MMAT) [40]. Commentaries and service evaluations were assessed using AACODS (authority, accuracy, coverage, objectivity, date, significance) tool, which appraises the veracity, clarity, acknowledgement of bias, and relevance of the contribution to the field [41]. Study quality was assessed by RA and verified by NVSJ. Disagreements were resolved through discussion.
Evidence Synthesis
We conducted a framework synthesis of study characteristics and outputs. Study outcomes were tabulated by applying existing implementation science frameworks, that is, the CFIR framework [36], Proctor et al’s [37] taxonomy of implementation outcomes; and also by relevant topics/themes that emerged during data extraction. This table-based synthesis of the study outcomes combined a deductive and inductive approach to data analysis by using existing frameworks, while identifying emerging themes. Results reported in this paper include a narrative synthesis of the study characteristics and quantitative study outputs [42] and the tabulated results.
Results
Study Selection
A total of 3956 references were identified through searching databases of published papers. medRxiv was the only preprint database where included papers were found (n=10); 1 more relevant paper was identified by a member of the research team and a further paper was found through reference searching of included studies.
A PRISMA flow diagram [33] of the screening and selection process is presented in Figure 1.
Figure 1.
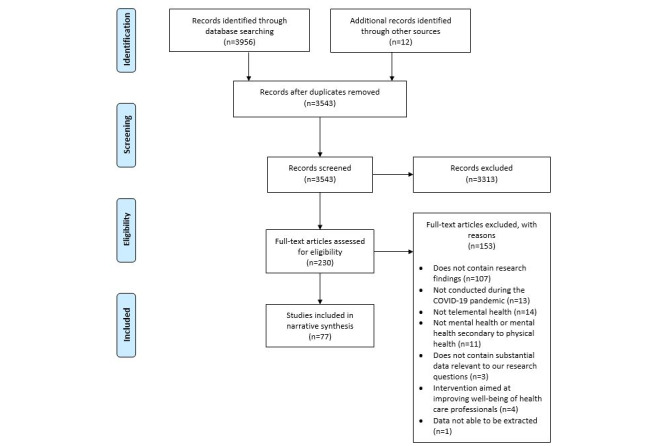
PRISMA diagram showing screening and included studies.
Quality of Included Studies
The quality of included primary research studies was moderate to high: 23 out of 48 studies appraised using the MMAT met above 80% of quality criteria, whereas 21 out of 48 met between 50% and 79%. The quality of included service evaluations or audits was generally high: 27 out of 29 studies appraised using the AACODS met at least 4 out of the 6 quality criteria assessed. These include being written by recognized experts; including reference lists; having a clear aim; stating details such as date, location, and limitations; and making a meaningful contribution to the research literature.
Study Characteristics
Of the 77 studies which were eligible for inclusion in the review (Table 1), 45 were primary research studies, 24 were service evaluations or audits, and 8 were editorials or letters that included data. Thirty-three were conducted in the United States, 9 in the United Kingdom, and 5 each in Australia, Canada, and Spain. Five were conducted across more than 1 country.
Table 1.
Study characteristics.
| Study | Aim of study | Modality used | Mental health problem/diagnosis | Participants (sample size) |
| Aafjes-van Doorn et al [43] | Survey of therapists’ experiences of video therapy during the pandemic | Va | Not stated | Staff (n=144) |
| Anton et al [44] | Description of transition to telemedicine | V, Pb, TMc, Ed, Me | Depression, posttraumatic stress disorder | Staff |
| Barney et al [45] | Description of transition to telemedicine | V | Mixed | Staff |
| Békés et al [46] | Survey of psychotherapists’ attitudes toward online psychotherapy | V | Mixed | Staff (n=145) |
| Békés et al [47] | Survey of psychoanalytical therapists’ experiences of videoconference therapy during the pandemic | V, P | Mixed | Staff (n=190) |
| Benaque et al [48] | Description of service changes due to the pandemic | V, P, TM | Dementia | Staff |
| Berdullas Saunders et al [49] | Description of the use of a psychological helpline | P | Mixed | General population (15,170 calls) |
| Bhome et al [50] | Survey of staff perspectives on delivery of services to older adults during the pandemic | NAf | Dementia | Staff (n=158) |
| Bierbooms et al [51] | Interviews with health professionals on the sustainability of online treatment after the pandemic | V, TM, Og | Mixed | Staff (n=11) |
| Boldrini et al [52] | Survey of psychotherapists’ experience with telepsychotherapy during the pandemic | V, P, M | Mixed | Staff (n=308) |
| Burton et al [53] | Interviews with people with mental health conditions on their experience during the pandemic | NA | Mixed | Service users (n=22) |
| Carpiniello et al [54] | Survey to explore the impact of the pandemic on the functioning of mental health services | NA | Mixed | Staff (n=71) |
| Cheli et al [55] | Evaluation of a crisis intervention for patients diagnosed with psychosis | V | Psychosis and bipolar | Service users (n=6) |
| Chen et al [56] | Description of changes made to mental health services due to the pandemic | V, P | Mixed | NA (description of service change) |
| Childs et al [57] | Description of changes made in an outpatient psychiatric service due to the pandemic | V, P | Mixed | Service users |
| Colle et al [58] | Evaluation of teleconsultation during the pandemic | V, P | Mixed | Service users |
| Connolly et al [29] | Description of changes to services during the pandemic | V, P | Mixed | NA (description of service change) |
| Datta et al [59] | Description of transition to telehealth during the pandemic | V | Eating disorders | NA (description of service change) |
| Dores et al [60] | Exploration of mental health professionals’ attitudes regarding information and communications technology use | V, P, O, E | Mixed | Staff (n=108) |
| Erekson et al [61] | Exploration of use of telehealth in a student counseling service during the pandemic | V | Mixed | Staff |
| Feijt et al [62] | Exploration of staff experiences of online treatment during the pandemic | V, P, O, E | Mixed | Staff (n=51) |
| Fernandez et al [63] | Survey on the impact of the pandemic for people diagnosed with an eating disorder | NA | Eating disorders | Service users (n=121) |
| Foye et al [64] | Exploration of the impact of the pandemic on mental health nurses | V, P | Mixed | Staff |
| Gaddy et al [65] | Exploration of the impact of the pandemic on music therapy professionals | V, P | NA | Staff (n=1196) |
| Gillard et al [66] | Exploration of the experiences of people with mental health problems during the COVID-19 pandemic | V, P, TM | Mixed | Service users |
| Gomet et al [67] | Description and review of the implementation of remote working in an addiction outpatient service | P | Substance abuse | Service users |
| Graell et al [68] | Exploration of the impact of the pandemic on a child and adolescent eating disorders service | V, P, M | Child and adolescent eating disorders | Service users (n=365) |
| Grover et al [69] | Evaluation of the monitoring of patients with schizophrenia on clozapine during the pandemic | P, TM | Psychosis and bipolar | Service users |
| Grover et al [70] | Evaluation of the impact of the pandemic on mental health services in India | V, P | Mixed | Staff (n=396) |
| Grover et al [71] | Evaluation the impact of the pandemic on mental health services in India | V, P | Mixed | Staff (n=109) |
| Haxhihamza et al [72] | Evaluation of the satisfaction of patients with telepsychiatry due to the pandemic | M | Mixed | Service users (n=28) |
| He et al [73] | Evaluation of a psychological intervention program | V, P, M, O | General population | NA |
| Hom et al [74] | Description of the development of a virtual program for an acute psychiatric population | V | Mixed | Staff and service users |
| Humer et al [75] | Survey of psychotherapists’ views on working during the pandemic | V, P, E, M | NA | Staff (n=338) |
| Humer et al [76] | Survey of psychotherapists view on the use of the internet during the pandemic | V | NA | Staff (n=1547) |
| Izakova et al [77] | Survey of the impact of the pandemic on mental health experts | V, P | NA | Staff (n=157) |
| Johnson et al [7] | Survey of the experiences of mental health staff during the pandemic | V, P, M | Mixed | Staff (n=2180) |
| Jurcik et al [78] | Exploration of how the pandemic affected mental health services | V, P, M | Mixed | Staff (n=8) |
| Khanna et al [79] | Description of services changes in a trauma service during the pandemic | V, P, M | Posttraumatic stress disorder | Staff (n=21) |
| Kopec et al [80] | Description of the transition to telehealth in a community mental health service | V, P | Mixed | NA (description of service change) |
| Lai et al [81] | Evaluation of the benefits of telehealth to people with dementia and their carers | V, P | Dementia | Service users (n=60) |
| Lakeman and Crighton [82] | Exploration of providing dialectical behavior therapy using telehealth technology | V, P, M | Personality disorder | Staff (n=28) |
| Lin et al [83] | Evaluation of psychological hotline services set up during the pandemic | P, TM | General population | NA (evaluation of a new service) |
| Looi et al [84] | Evaluation of the use of psychiatry telehealth in smaller states | V, P, M | Mixed | Staff |
| Looi et al [85] | Evaluation of the use of psychiatry telehealth in larger states | V, P, M | Mixed | Staff |
| Lynch et al [86] | Description of change to telehealth in a service for people with psychosis | V | Psychosis and bipolar | Service users (n=64) |
| McBeath et al [87] | Exploration of the experiences of psychotherapists working remotely during the pandemic | V, P, TM, E | Mixed | Staff (n=335) |
| Medalia et al [88] | Description of the change to telehealth in a service for people with serious mental illness | V | Mixed | NA (description of service change) |
| Miu et al [89] | Evaluation of the engagement with telehealth of people with severe mental illness during the pandemic | V, P | Mixed | Staff (n=24) |
| Olwill et al [90] | Survey of psychiatrists’ experience of remote consultations | P | Mixed | Staff (n=26) |
| Patel et al [91] | Analysis of health record data on the impact of remote consultation during the pandemic | NA | Mixed | NA (description of whole service) |
| Peralta et al [92] | Evaluation of the effectiveness of teleconsultation use during the pandemic | V, P, TM | General population | NA (6800 interventions) |
| Pierce et al [93] | Survey of the impact of telepsychology use by psychologists before and during the pandemic | V, P | Mixed | Staff (n=2619) |
| Probst et al [94] | Investigation of changes to psychotherapy compared with the months before the pandemic | P | Mixed | Staff (n=1547) |
| Reilly et al [95] | Survey to understand change in practice by health care staff during the pandemic | NA | Mixed | Staff (n=903) |
| Roach et al [96] | Interviews to understand the experience of people with dementia during the pandemic | NA | Dementia | Service users (n=21) |
| Roncero et al [97] | Description of the response of a mental health network to the pandemic | V, P, M | Mixed | NA (description of service change) |
| Rosen et al [98] | Description of transition to telemental health services | V, P | Mixed | NA (description of service change) |
| Sasangohar et al [99] | Description of implementation of telepsychiatry in a psychiatric practice | V, P, E | Mixed | NA (description of service change) |
| Scharff et al [100] | Description of changes made by a psychological service during the pandemic | V | Mixed | NA |
| Schlegl et al [101] | Survey to investigate the impact of the pandemic on patients with bulimia nervosa | NA | Eating disorders | Service users (n=55) |
| Sciarrino et al [102] | Description of providing trauma-focused treatment using telehealth during the pandemic | V, O | Posttraumatic stress disorder | NA |
| Sequeira et al [103] | Description of change to services for people with obsessive compulsive disorder during the pandemic | V | OCD | Service users (n=5) |
| Severe et al [104] | Survey of patients using a mental health service to explore decisions to accept or decline telepsychiatry | V, P | Mixed | Service users (n=244) |
| Sharma et al [28] | Description of the implementation of a home-based telemental health service during the pandemic | V, P | Child and adolescent services | Staff (n=105) |
| Sheehan et al [105] | Survey of the experiences of staff working with people with intellectual and other developmental disabilities | NA | Intellectual disabilities | Staff (n=648) |
| Sklar et al [106] | Exploring the impact of the pandemic on mental health services in Indiana | NA | NA | Staff |
| Termorshuizen et al [107] | Survey to evaluate the impact of the pandemic on people with eating disorders | NA | Eating disorders | Service users (n=1021) |
| Uscher-Pines et al [108] | Interviews with psychiatrists to understand how change in delivery has affected mental health care | V, P | Mixed | Staff (n=20) |
| Uscher-Pines et al [109] | Interviews with clinicians to understand the experience of using telemedicine for opiate use disorder | V, P | Opiate use disorder | Staff (n=18) |
| van Dijk et al [110] | Description of transforming a day-treatment program for older people into an online program | V | Mixed | Staff |
| Wang et al [111] | Survey to compare Chinese and US practitioners’ attitudes toward teletherapy during the pandemic | V, P | Mixed | Staff (n=329) |
| Wilson et al [112] | Survey to explore staff perceptions of the impact of the pandemic on perinatal services | V, P, M | Perinatal services | Staff (n=363) |
| Wood et al [113] | Description of the implementation of group teletherapy for people with first-episode psychosis | V | Psychosis and bipolar | Service users (n=7) |
| Wyler et al [114] | Exploration of the experience of therapy sessions for people with attention deficit hyperactivity disorder and their therapists during the pandemic | V, P | Attention deficit hyperactivity disorder | Staff and service users (n=60 therapist/service user dyads) |
| Yellowlees et al [115] | Description of the rapid conversion of an outpatient psychiatric clinic to a telepsychiatry clinic | V, P | Mixed | NA (description of service change) |
| Zulfic et al [116] | Audit to understand the move to telephone support for people using a community mental health team | P | Mixed | Service users (n=314) |
aV: video.
bP: phone.
cTM: text message.
dE: email.
eM: mobile.
fNA: not applicable/not stated.
gO: other.
Of the 45 primary research studies, 32 involved staff and 9 involved service users. The remaining 4 analyzed service use data (3 evaluated contacts with hotlines and 1 evaluated service use in 1 UK National Health Service [NHS] service provider).
Most studies were conducted in services that worked with people with mixed psychiatric diagnoses (n=30), although we also found studies conducted with groups with a single diagnosis (eg, dementia or eating disorders). Studies could include more than 1 service type, the most commonly studied being community mental health teams (CMHTs) or outpatient settings (n=39), followed by psychology or psychotherapy services (n=17). Inpatient or residential services were included in 15 studies, while 12 included general hospitals. Eight studies included private hospitals or clinics, while 4 explored telemental health use in helplines, voluntary sector services, crisis teams, or veterans’ health services, respectively. Five studies did not report any specific setting.
The aims of most studies were either a description of changes made due to the pandemic, new services set up because of the pandemic, or an evaluation of the impact of the pandemic on either staff or service users. The descriptions of changes either focused specifically on the move to telemental health or were wider descriptions of changes to services including the use of telemental health. The characteristics of each of the included studies are shown in Table 1, with a more detailed summary in Multimedia Appendix 2.
Data Synthesis
Barriers and Facilitators to Telemental Health
Implementation barriers and facilitators were categorized using a condensed version of the CFIR framework (see Table 2, where definitions of the CFIR constructs are also provided). The key findings are summarized below.
Intervention Characteristics
Video and phone calls were the most common modalities used for remote care; studies also reported the use of emails, instant messaging services, apps, prerecorded videos and forums (further details about the modality used in each study can be found in Table 1).
When comparing remote care with traditional face-to-face settings, studies identified advantages for both methods. Benefits for remote care included being more convenient (for both staff and service users), making care more accessible to groups who may previously have been excluded, reducing travel (resulting in both time and cost savings), and helping clinicians understand more about the service user, as they had more insight into their home lives. A further benefit is that more family members were readily able to attend family therapy or family education sessions since care was moved online (eg, [43]). However, clinicians reported difficulties in picking up on nonverbal cues in remote compared with face-to-face care, and that remote care could sometimes require more concentration.
Outer Setting
Services commonly implemented remote methods of working due to “stay at home” orders or national lockdowns, or due to a high level of cases in their local area. Overall, all settings described in papers had sufficient capacity to make a rapid shift to remote forms of care. Several studies in the United States in particular mentioned the impact of health insurance regarding uptake of telemental health (eg, [56]), as not all insurance providers covered remote care. However, this did change during the course of the pandemic as telemental health delivery was eased by the relaxation of policy and billing reimbursements [56,75]. The change from face-to-face to remote delivery of care was also facilitated by professional societies who posted guidelines on their websites to assist clinicians.
Staff Characteristics
Enablers for clinician uptake included supporting clinicians by ensuring supervision, supportive leadership, clear communication, keeping track of clinicians’ needs, optimizing physical space for comfort and privacy (eg, using headphones or ergonomic seating), and arranging times away from the computer.
However, staff in several studies reported a lack of initial training for telemental health, and therefore identified training needs regarding the use of online platforms and meeting privacy regulations in particular. In some studies, having no previous experience with telemental health was also found to be associated with higher anxiety [43] and lower uptake [52] of remote care. However, others found that previous experience did not impact clinicians’ views of telemental health during the pandemic [47].
Process
As telemental health was not commonly used in most services before COVID-19, staff had to rapidly adjust to a new way of working. Several studies discussed the training which was put in place for staff, which included training courses, shadowing, or observing senior colleagues; discussion within clinical teams’ facility-level telehealth coordinators and clinical champions providing training; webinars; and checking official guidelines. New workflows also had to be developed to allow staff to access patient records remotely, and service users had to be informed about the transition to telemental health.
Service User Needs/Resources
In addition to the needs of staff, service users also identified certain needs and resources to enable them to effectively transition to telemental health care. A commonly reported issue was access to technology, particularly among service users with diagnoses such as schizophrenia (eg, [116]), older adults (eg, [50]), and service users from lower socioeconomic backgrounds (eg, [78]). Service users also reported problems having a stable internet connection to allow for uninterrupted communication, which could negatively impact the therapeutic relationship. Concerns were also raised by both clinicians and service users regarding privacy and confidentiality, and in some cases service users had difficulties concentrating on remote care. Several studies (eg, [86,98]) mentioned the need for an agreed “Zoom etiquette” for service users, including attire, audio/visual set up, and background distractions.
Implementation Outcomes
Outcomes of the implementation of telemental health have been summarized below using Proctor et al’s [37] taxonomy of implementation outcomes. Further information can be found in Table 3.
Table 3.
Implementation outcomes summary findings for telemental health.
| Implementation outcome | Findings | Example studies |
| Acceptability |
|
[7,45,60,64,70,74,76,78,87,91,94,96,97,100,104] |
| Adoption |
|
[7,50,52,54,56,58,61,75,79,81,82,113,114] |
| Appropriateness |
|
[56,60,78,82,99,100,112] |
| Feasibility |
|
[7,56,58,62,64,73,74,78,82,94,96,104] |
| Fidelity |
|
|
| Implementation cost |
|
[59,70,87,103] |
| Penetration |
|
[7,54,105] |
| Sustainability |
|
[43,64,85,93,95,104] |
Acceptability
Remote care was seen as satisfactory by the majority of clinicians and service users in most studies in the context of the pandemic. A number of studies also reported that telemental health enabled some groups to access care who found it difficult to engage with face-to-face support (eg, [7]). Some clinicians reported that they would also be willing to continue with some aspects of remote care in the future (eg, [43,77]). However, it is important to note that while acceptability was high overall, this was not the case for all groups; for example, Grover et al [71] reported acceptability rates of around 45% for both clinicians and service users using services in a range of settings in India. Further details of satisfaction and acceptability outcomes are presented in Table 4.
Table 4.
Levels of acceptability of telemental health during the COVID-19 pandemic.
| Author | Type of service | Service location | Acceptability data |
| Aafjes-van Doorn et al [43] | Psychology/psychotherapy/counseling service | United States, Canada, Europe (Hungary, Italy, United Kingdom, Germany, Norway, Sweden, Switzerland, Latvia, Ireland) |
|
| Békés et al [46] | Psychology/psychotherapy/counseling service; private hospital/clinic; CMHTa and outpatient services | Canada, United States, Europe (countries not stated) |
|
| Békés et al [47] | CMHT and outpatient services; psychology/psychotherapy/counseling service; private hospital/clinic | Canada, United States, Europe (countries not stated) |
|
| Benaque et al [48] | Voluntary sector/nonprofit | Spain |
|
| Colle et al [58] | CMHT and outpatient services | France |
|
| Dores et al [60] | Psychology/psychotherapy/counseling service | Portugal |
|
| Grover et al [69] | CMHT and outpatient services | India |
|
| Grover et al [70] | CMHT and outpatient services; inpatient mental health service; private hospital/clinic | India |
|
| Grover et al [71] | Medical colleges, government-funded institutes, general hospital psychiatry units | India |
|
| Haxhihamza et al [72] | Day hospital | Macedonia |
|
| He et al [73] | Helplines; online media programs | China |
|
| Hom et al [74] | Private hospital/clinic | United States |
|
| Izakova et al [77] | CMHT and outpatient services; inpatient mental health service | Slovakia |
|
| Johnson et al [7] | All service settings, including inpatient, CMHTs, voluntary sector | United Kingdom |
|
| Lakeman and Crighton [82] | Psychology/psychotherapy/counseling service | Australia |
|
| Lynch et al [86] | CMHT and outpatient services | United States |
|
| Olwill et al [90] | CMHT and outpatient services | Ireland |
|
| Sheehan et al [105] | CMHT and outpatient services | United Kingdom |
|
| Wang et al [111] | Not stated/unclear | United States and China |
|
| Wilson et al [112] | CMHT and outpatient services; crisis and emergency mental health services; inpatient mental health service | United Kingdom |
|
aCMHT: community mental health team.
bHCW: health care worker.
cDBT: dialectical behavior therapy
dCP: complex psychosis
eCAPA: China American Psychoanalytic Alliance.
Telemental health services were acceptable to people during the pandemic as a way of continuing their treatment; however, findings from several studies also indicated that participants wanted at least some appointments to be face-to-face once restrictions on in-person contact had loosened.
Adoption
Adoption rates were relatively high across studies, with most services or clinicians moving their appointments to remote methods. Rates of adoption of telemental health for service users who were already receiving care at the start of the pandemic ranged from 48% [89] to 100% [44,67,110]. Some studies reported face-to-face appointments still took place if necessary, for example, for initial assessments or for medication reviews (eg, [116]). Most studies that examined impact on attendance reported no adverse effects on attendance rates after introducing telemental health: there was either no difference in missed appointments when comparing remote with face-to-face care [45,86], or nonattendance after adoption of telemental health decreased [79,91,103]. Further details about adoption of telemental health across studies can be found in Table 5.
Table 5.
Levels of adoption and coverage of telemental health during the COVID-19 pandemic.
| Author | Type of service | Service location | Adoption/coverage data |
| Anton et al [44] | General hospital/physical health service | United States | 77% (n=20) of those approached via telephone enrolled in the program, higher than the observed in-person rates of 61%. 80% of patients who were contacted by phone in the hospital agreed to be enrolled, lower than the 98% success rate when staff approaches patients in person at the bedside. 100% of patients who received in person care and 100% on the waitlist (n=5) transitioned to telepsychotherapy. |
| Barney et al [45] | CMHTa and outpatient services | United States | The percentage of provider telemedicine visits increased from 0% to 97%. The number of overall clinic visits did not decline when compared with that a year before (337 visits in March 2019 vs. 332 visits in March 2020), No-show rates were comparable between remote and face-to-face care. |
| Békés et al [47] | CMHT and outpatient services; psychology/psychotherapy/counseling service; private hospital/clinic | Canada, United States, Europe (countries not stated) | Before COVID-19 an average of 23 sessions (SD 10.58) per week were conducted in person, 3 sessions (SD 2.28) by phone, and 1 session (SD 2.84) online via videoconferencing. During COVID-19 an average of 7 (SD 7.91) of the in-person sessions changed to sessions by phone, and 15 (SD 10.33) to online sessions. |
| Benaque et al [48] | Voluntary sector/nonprofit organization | Spain | Initially, average weekly visits dropped from 657 to 254 in the first week after the state of alarm was declared. This drop was of 44% for follow-up visits and 40% for on-demand consultations. By week 16 the total number of visits (n=514; 78%) was almost up to prepandemic levels. |
| Boldrini et al [52] | CMHT and outpatient services; psychology/psychotherapy/counseling service; private hospital/clinic | Italy | 42.1% (SD 28.9) of their psychotherapy treatments were interrupted during the lockdown. The remainder of their treatments was primarily delivered via online video (63.7% [SD 38.3]) or telephone (29.1% [SD 25.3]). 7.2% (SD 15.1) of their treatments were delivered face-to-face. |
| Carpiniello et al [54] | CMHT and outpatient services; inpatient mental health service | Italy | 75% of appointments were switched to remote. Telehealth modalities used were mainly phone calls (100% of the Italian Departments of Mental Health), videocalls (67%), or emails (19%), with 41% of units adopting all these means of contact. |
| Chen et al [56] | General hospital/physical health service | United States | The outpatient psychiatry division switched from under 5% virtual visits in March 2019 to over 97% in March 2020. Productivity was maintained at about 95% of previous levels, with 9206 virtual visits in March 2020. Between March 30 and April 24, 2020, 30% of the virtual visits were conducted via phone. |
| Childs et al [57] | CMHT and outpatient services | United States | Before COVID-19, 100% of care was delivered in person. In the first week after shutdown, telehealth comprised 65.45% of visits (100% over the telephone). In the second week, 91.6% of visits were conducted using telehealth (83.49% over the telephone and 15.6% video). By the third week 99% of appointments used telehealth (30% using video). The percentage of appointments using video increased weekly, peaking at 69.9% |
| Colle et al [58] | CMHT and outpatient services | France | After 2 weeks of teleconsultations, 376 (91.0%) out of the 413 previously planned appointments were performed. |
| Connolly et al [29] | CMHT and outpatient services; Veterans Affairs service | United States | Daily TMH-Vb encounters rose from 1739 on March 11 to 11,406 on April 22 (556% growth, 222,349 total encounters). Between March 11 and April 22, 114,714 patients were seen via TMH-V. A total of 88,908 (77.5%) were first-time TMH-V users. A total of 12,342 mental health providers completed a TMH-V appointment between March 11 and April 22; 4281 (34.7%) were first-time TMH-V users. Daily telephone encounters rose from 6348 on March 11 to 34,396 on April 22 (442% growth). Daily in-person encounters fell from 57,296 on March 11 to 10,931 on April 22 (81% decrease). |
| Dores et al [60] | Psychology/psychotherapy/counseling service | Portugal | During the lockdown period, 17 (15.7%) of the 108 psychologists discontinued therapy and counseling; 53 (58.2%) continued to provide services to most or all of their clients; 23 psychologists (25.3%) decreased the number of clients they saw to a range of between 0% and 25%, and for another 15 psychologists (16.5%) that number diminished to a range of between 26% and 50%. |
| Erekson et al [61] | Psychology/psychotherapy/counseling service | United States | Attendance rates for individual therapy temporarily dropped by about 35% but climbed to previous levels within 2 weeks. Group therapy attendance dropped by about 30% but did not fully recover, remaining about 15% lower after 2 weeks. The number of clients receiving individual therapy in 2020 dropped by 43%. Between March 22 and April 4, 2020, the service had fewer than half the intakes of any other recent year. |
| Gaddy et al [65] | Music therapy service | United States | Of the 869 respondents indicating current contact hours, 70.54% reported that they were providing alternative services, including telehealth services (54.81%), virtual music lessons (17.01%), prerecorded songs/playlists (16.98%), and prerecorded video sessions (16.00%). Individual services increased (mean 61.58% [SD 41.26], whereas group services decreased (mean 24.97% [SD 37.56]). |
| Gomet et al [67] | General hospital: addiction service | France | 100% of service users took part in remote care |
| Graell et al [68] | CMHT and outpatient services; inpatient mental health service | Spain | During the study period, a total of 1818 outpatient consultations were carried out: 1329 (73.10%) by telephone or videoconferencing and 489 (26.9%) face-to-face. |
| Grover et al [69] | CMHT and outpatient services | India | The majority of the patients reported that they were in touch with their treating doctor (81.5%), with contact initiated by the treating team in 79% of patients. |
| Grover et al [70] | CMHT and outpatient services; inpatient mental health service; private hospital/clinic | India | Use of teleservices almost doubled during the lockdown period: 206 (52%) participants provided telecommunication services during the lockdown period, 186 (47%) provided free tele-consultation to the general public, and 269 (67.9%) provided free tele-consultation to their patients; 132 (33.3%) were using both voice and video calls (combination of free and paid services), 31 (7.8%) were using only voice calls (combination of free and paid services), and 31 (7.8%) were using only voice calls (combination of free and paid services). |
| Grover et al [71] | Medical colleges, government-funded institutes mental hospital setting, general hospital psychiatry units | India | Around 25% of institutes began offering telemental health services; 45.9% of institutes reported that telecommunication services continued during lockdown. Mental health services were being provided to people in quarantine (66.1%) and those with COVID-19 infection (59.6%), family members of patients with COVID-19, and those in quarantine (40.4%). |
| Humer et al [75] | Psychology/psychotherapy/counseling service | Czech Republic, Germany, Slovakia | Among all countries, the combined (personal contact + telephone + internet) number of patients treated on average per week during COVID-19 (mean 18.32 [SD 12.86]) did not differ from the combined (personal contact + telephone + internet) number of patients treated on average per week in the months before the COVID-19 situation (mean 19.35 [SD 13.73]), t337=−1.506; P=.133. |
| Humer et al [75] | Psychology/psychotherapy/counseling service | Austria | During the COVID-19 pandemic, face-to-face psychotherapy remained the most abundant treatment modality. |
| Khanna et al [79] | CMHT and outpatient services | Australia | There was a 3% increase in appointment bookings compared with the same period in 2019. Cancellation/nonattendance rate dropped from an average of 19% last year to 12% for 2020 |
| Kopec et al [80] | CMHT and outpatient services | United States | Prior to COVID-19, Network180 served an average of 2390 patients/month, which decreased to an average of 1921 patients/month during the pandemic. This decrease was noted most significantly in crisis services (averaging 822 patients/month before COVID-19 and 640 patients/month during COVID-19). Telehealth increased from 5% of all services prior to COVID-19 to 84% of all services during COVID-19. The majority of services provided via telehealth were audio only (versus audiovisual), with a ratio of 1.9:1 for crisis services and 4:1 for noncrisis services. |
| Looi et al [84] | Psychiatrist telehealth service | Australia | Percentage of consultations conducted using telemental health—ACT: 62% (April), 58% (May); NT: 53% (April), 51% (May); SA: 69% (April), 58% (May); Tasmania: 38% (April), 40% (May) |
| Looi et al [85] | Psychiatrist telehealth service | Australia | The majority of private practice was conducted by telehealth in April but was lower in May as new COVID-19 case rates fell. Percentage of consultations conducted using telemental health—NSW: 56% (April), 52% (May); QLD: 63% (April), 53% (May); VIC: 61% (April), 59% (May); WA: 51% (April), 36% (May) |
| Lynch et al [86] | CMHT and outpatient services | United States | The service continued providing all services except community-based coaching via telehealth. 90% of patients with complex psychosis accepted telehealth sessions and maintained their specific treatment plans. 2 opted out of telemental health. Mean comparisons between session attendance and cancellations/no-shows during the 6-week period before and after telehealth conversion showed no significant differences in service utilization. |
| Medalia et al [88] | CMHT and outpatient services | United States | Tracking the number of RS enrollees with active participation indicated that in the week before telehealth conversion, when shelter-in-place recommendations commenced, participation dropped from 94% to 52%; after telehealth conversion, participation rose from 67% in the first 4 days to 79% after 1 week and to 84% after 2 weeks. |
| Miu et al [89] | CMHT and outpatient services | United States | A total of 816 participants comprised the analytic sample. A total of 400 converted to telehealth and of those 64 were SMIc. The conversion rates from in-person psychotherapy to teletherapy were similar for SMI (n=64, 51.6%) and non-SMI (n=334, 48.3%) groups. The rate at which the SMI group converted from in-person therapy to teletherapy (52%) was not statistically different from that of the non-SMI group (48%) during COVID-19. |
| Patel et al [91] | All National Health Service Trust services | United Kingdom | From March 2020, in‐person contacts reduced substantially from around 9000 per week to 3000 per week in early April 2020. Over the same period there was an increase in remote contacts from around 2500 per week in early March 2020 to around 8000 per week by the end of April 2020. Total clinical contacts per week dropped from around 12,500 in mid‐March to around 10,000 in mid‐April 2020. The number of unattended appointments was temporarily reduced in April, May, June, and September 2020. |
| Pierce et al [93] | Variety of MH service settings | United States | Psychologists estimated that telepsychology comprised 85.53% of their clinical work during the pandemic, compared with the prepandemic context when only 7.07% of their clinical work was conducted remotely. |
| Probst et al [94] | Psychology/psychotherapy/counseling service | Austria | Face-to-face psychotherapies in personal contact were reduced and remote psychotherapies (via telephone or internet) were increased in the early weeks of the COVID-19 lockdown as compared with the months before. Although average increases in psychotherapies via telephone (979%) or via internet (1561%) were dramatic, there was an undersupply of psychotherapy in Austria in the early weeks of the COVID-19 lockdown as the total number of patients treated on average per week was lower in COVID-19 lockdown than in the months before. |
| Reilly et al [95] | Various service types | United States | There was uptake of telemental health by approximately 80% of respondents by late March or early April 2020. All but 2.11% (19/903) of providers in this study made practice adjustments (transition to telemental health). |
| Rosen et al [98] | VHAd mental health services | United States | VHA provided nearly 1.2 million telephone and video encounters to veterans in April 2020 and reduced in-person visits by approximately 80% when compared with the October 2019 to February 2020 period before the pandemic. By June 2020, VHA had an 11-fold increase in encounters using direct-to-home video and a fivefold increase in telephone contacts relative to before the pandemic. VHA reduced in-person visits by approximately 80% when compared with the October 2019 to February 2020 period before the pandemic. |
| Scharff et al [100] | Community-based training clinic providing therapy | United States | The Psychological Services Centre saw an initial retention rate of 82% in the first week of teletherapy, with more clients resuming services in the weeks that followed. |
| Schlegl et al [101] | Inpatient mental health service | Germany | More than 80% of patients with bulimia nervosa received face-to-face therapy before the COVID-19 pandemic (81.8%) compared with 36.4% during the pandemic (ie, a decrease by 55.5%). Use of videoconference-based therapy increased from 3.6% to 21.8% and use of telephone contacts from 18.2% to 38.2%, whereas the use of additional online interventions decreased from 3.6% to 0%. Face-to-face psychotherapy decreased by 56% but videoconferencing therapy was only used by 22% of patients. |
| Sciarrino et al [102] | Veterans Healthcare Administration | United States | Approximately 76% of veterans engaged in posttraumatic stress disorder treatment chose to continue despite the COVID-19 pandemic via telehealth. |
| Sequeira et al [103] | Residential services | United States | After transition to teletherapy, the average daily virtual program census from March 19, 2020, to April 18, 2020, was 3.3 intensive outpatient program patients and 22.4 outpatients. These numbers indicate a slight decrease in intensive outpatient program patients (−0.3/per day) and an increase in outpatients seen per day (+2.7/per day). There was an increase in the outpatient sessions retained and a decrease in the appointments cancelled. |
| Severe et al [104] | CMHT and outpatient services | United States | Take up for remote care was over 95%; 82.8% (n=202) initially chose to receive psychiatric care through video visits, whereas 13.5% (n=33) chose telephone visits; 1.2% (n=3) decided to postpone care until in-person visit availability. |
| Sharma et al [28] | General hospital/physical health service | United States | By March 20, 2020, 67% of all outpatient appointments were conducted at home. Most of these appointments were conducted by phone with some TMH sessions. By March 27, 2020, 90% of all outpatient appointments were done at home, predominantly by phone (59%) but increasingly by HB-TMHe (31%). One week later (April 3, 2020), these rates were 48% versus 45%, respectively. By March 31, 2020, 98% of faculty completed expedited training and obtained departmental approval for HB-TMH services during the COVID-19 crisis. By April 10, 2020, HB-TMH was offered to all established outpatients for individual visits. Only the crisis clinic continued a regular in-clinic presence. |
| Sheehan et al [105] | CMHT and outpatient services | United Kingdom | 64% were spending at least some time working from their workplace (either solely or in combination with home working); 33.9% were working from home only. Just over a third were at the workplace (n=178, 35.1%) and the remainder (n=147, 28.9%) worked from both home and at the workplace. |
| Termorshuizen et al [107] | CMHT and outpatient services | The Netherlands and United States | Most transitioned to telehealth care (United States 45%; Netherlands 42%), with fewer still receiving face‐to‐face care (United States 3%; Netherlands 6%), or not having been able to engage with their provider at all (United States 6%; Netherlands 5%). |
| Uscher-Pines et al [108] | CMHT and outpatient services and private hospital/clinic | United States | Most of the psychiatrists had transitioned to fully virtual practices. Only a quarter of the participants were seeing any patients in person. |
| Uscher-Pines et al [109] | CMHT and outpatient services; private hospital/clinic; general hospital/physical health service | United States | Telemedicine use: None (in-person only), 1 (5.6%); phone only, 2 (16.7%); video only, 0 (0.0%); combination of video and phone, 15 (83.3%). |
| van Dijk et al [110] | CMHT and outpatient services; psychology/psychotherapy/counseling service | The Netherlands | Treatment adherence was 100%. |
| Yellowlees et al [115] | General hospital/physical health service | United States | By the second day after shutdown, only 8% (n=52) of our appointments were in-person clinic visits, compared with our baseline average of 98%. By the third business day, 100% (n=73) of appointments were conducted virtually, with 92% (n=67) via videoconference and 8% (n=6) by phone. |
| Zulfic et al [116] | CMHT and outpatient services | Australia | Some patients still required regular face-to-face reviews, including the 91 patients (29%) who are treated with depot medications and 71 (23%) taking clozapine. |
aCMHT: community mental health team.
bTMH-V: telemental health: video.
cSMI: serious mental illness.
dVHA: Veterans Health Administration.
eHB-TMH: home-based telemental health.
While most studies reported high adoption rates, a few studies reported a decrease in attendance: for example, Erekson et al [61] (though possibly because of the university setting) and Dores et al [60] identified challenges in retention due to low client adherence, lack of privacy, interruptions at home, lack of appropriate technology, or simply preference for face-to-face contact.
There was also evidence to indicate that adoption rates of telemental health fell as COVID-19 cases decreased (eg, [84,85]).
Appropriateness
There were some concerns raised over the appropriateness of remote care, for example, studies reported difficulties managing medication (eg, [45,108,109]) and concerns around engaging and assessing new patients (eg, [78]). Clinicians also found it harder to assess some physical indicators of mental health status (eg, hygiene, eye contact, physical symptoms of opioid withdrawal) without being able to see the service user in person. However, by contrast, remote methods of working felt safer for clinicians who worked with service users at risk for violence and behavioral dysregulation (eg, [56]). Online care was also not necessarily appropriate for patients with auditory or visual impairments, or with conditions such as migraines.
Staff reported concerns around the management of risk and safeguarding of service users when using remote methods of care (eg, [79,93]). Some helpful features of platforms which were thought to improve safety were using the waiting room function, being able to remove call participants, renaming participants (to protect anonymity), and using the private chat function.
Feasibility
In general, all studies reported good feasibility, at least for the short-term emergency response during the pandemic. However, some studies reported that telemental health is not suitable for all types of therapy, for example, those that require a physical presence (exposure therapy, role play, collaborative models; eg, [106]). Telemental health may also be less suitable for treating trauma [62,102]; clients with severe anxiety [62], learning difficulties or autism [105]; children [62]; and clients with cognitive impairment [62,90].
Cost-Effectiveness
There was limited information about costs of implementation of remote care in the included studies and no actual costs of telemental health were reported in the papers. However, initial evidence suggests remote care is not a costly intervention, with 1 paper stating that telemental health is “cost-effective” [69], while another mentions the use of “low-cost technologies” by clinicians [72].
Penetration
There was widespread penetration (the extent to which telemental health was integrated into mental health services) of remote methods of care delivery due to the COVID-19 pandemic, despite few services utilizing telemental health previously. Services were able to rapidly adapt to this new way of working, with the majority of appointments conducted remotely after the first few weeks of “stay at home” orders.
Sustainability
The sustainability of telemental health cannot be completely determined from the included studies, as they present data mostly from the early stages of the COVID-19 pandemic. However, there was some indication that although remote working was widely accepted as a necessity, once restrictions loosened, rates of telemental health use declined (corresponding with the drop in cases in Europe in summer 2020). This correlates with findings that not all staff and service users would want to continue using remote methods of care after the pandemic ends. However, there are some aspects of remote working that both clinicians and service users would like to keep in the future in combination with face-to-face care (eg, [93,104]), as this approach has benefits such as being more efficient, flexible, and enabling access for certain groups (eg, [7,60,62]).
Clinical Outcomes
Comparing the clinical outcomes of face-to-face and remote care using quantitative measures indicated that telemental health approaches could be as effective as face-to-face care (eg, [55,103]), although it should be noted that most studies were on a small scale. Several studies also reported no psychiatric decompensations after switching to remote care (eg, [86,88]). However, it is important to note that clinical outcomes for telemental health were not comparable for all service users; for example, Dores et al [60] found that a quarter of psychiatrists reported poorer clinical outcomes after switching to remote care. Another study also indicated that only one-third of clinicians felt as though telemental health consultations were comparable to prepandemic sessions [114]. A full presentation of the clinical outcomes reported in included studies is shown in Table 6.
Table 6.
Studies which reported clinical outcomes of telemental health.
| Item | Type of service | Country | Clinical outcomes |
| Cheli et al [55] | Psychology/psychotherapy/counseling service | Italy |
|
| Dores et al [60] | Psychology/psychotherapy/counseling service | Portugal |
|
| Erekson et al [61] | Psychology/psychotherapy/counseling service | United States |
|
| Gomet et al [67] | General hospital/physical health service (addictions service) | France |
|
| Lai et al [81] | Day center (dementia service) | Hong Kong |
Patient outcomes
|
| Lynch et al [86] | CMHTb and outpatient services | United States |
|
| Medalia et al [88] | CMHT and outpatient services | United States |
|
| Sequeira et al [103] | Residential services (obsessive compulsive disorder) | United States |
|
| Wyler et al [114] | Mental health team and outpatient services | Switzerland |
|
aMoCA: Montreal Cognitive Assessment.
bCMHT: community mental health team.
Although the quality of therapeutic relationships reported by studies was generally good, clinicians reported problems reading patients’ emotions (eg, [43]) or feeling less connected to the service user compared with face-to-face sessions (eg, [56]). Clinicians also reported difficulties regarding feeling and expressing empathy remotely. Other challenges to therapeutic relationships when using remote care included a lack of client engagement, possible misunderstandings due to lack of nonverbal signals, common context, or not having a clear idea of patients’ physical state (alongside reduced privacy).
Social Outcomes
One study [81] compared social outcomes in a trial comparing telephone-only care with caregivers of older adults with neurocognitive disorder, with supplementary video care to both carers and service users. Findings indicated that those who received both telephone and video support had greater resilience, better cognitive functioning, and a higher quality of life.
Organizational and Care Delivery Outcomes
Improved communication was noted between staff when using telemental health when compared with traditional face-to-face care, as the use of online file sharing or discussion platforms facilitated communication between staff (eg, [74,105]). The use of online methods also facilitated staff training and some staff reported that remote working resulted in a better work–life balance (eg, [59]).
Discussion
Summary of Findings
This review collated evidence regarding the implementation and outcomes of remote working in mental health services in the context of the COVID-19 pandemic. Most studies indicate a relatively high level of activity, suggesting that at least in the services studied in higher-income countries, much mental health care can be shifted to telemental health in a crisis. Services mainly reported using a mixture of phone and video calls, with both service users and clinicians varying in their preference for these modalities. There were some indicators of reduced numbers of missed appointments, potentially due to the greater convenience of remote care, which may make access to services easier for some service users.
There was reasonable acceptability across the studies, at least in conditions where the alternative may have been no contact with services at all. However, there were situations where telemental health may be less acceptable, including for new patients, physical health aspects of care, and for service users without a private space at home to use for therapy. Telemental health also may not be as feasible for certain types of support, including support which needs a physical presence such as exposure therapy or role play. This finding reflects those in a systematic review by Turgoose et al [117], which found that service users had concerns around managing emotions during exposure tasks without the physical presence of a clinician. There was also evidence that telemental health may not be feasible for some clinical presentations, including some service users with psychosis, learning difficulties, or autism. Clinicians also reported a decrease in their ability to develop and maintain a strong therapeutic relationship with service users, due to being unable to pick up on nonverbal cues and a lack of connectedness, something which was also identified in a review conducted prior to the pandemic [118]. The acceptability levels found in this study are not dissimilar to previous studies (eg, [15]), even though the participants in the current studies are less likely to be volunteering to pilot a new type of care and more likely to be using telemental health because they have no alternative.
Few formal investigations of how to improve implementation were identified in this review, which may reflect the rapid nature of research conducted during the pandemic. However, some strategies for improving adoption/penetration/acceptability may include staff training, the use of telemental health champions, strategies for introducing service users to technology, and providing some simple guidance on how to use it best, identifying situations or populations when telemental health is not a good idea and those where it might be better. There was also a lack of fidelity assessments when therapies had to be adapted to fit telemental health delivery formats; therefore, little is known about the consequences of these adaptations.
Our interpretation of this pattern of findings is that the successful delivery in a pandemic of telemental health should not necessarily be seen as confirmation that people are happy with this mode of delivery long-term, as some of the identified problems may become more serious over time, and reports of being satisfied may have reflected awareness that at the time of the study, it was difficult to offer care by any other means. The longevity of these changes will ultimately turn not only on information technology, safety, and quality, but also on whether policy changes will support the reimbursements and regulatory adjustments implemented during the current crisis [29,57].
Implications for Future Research
There was a lack of reporting in included studies of trying to identify and reach those patients who are at increased risk of digital exclusion (Textbox 1). The needs of those at risk of digital exclusion are still largely underreported in both pre-COVID-19 [15] and COVID-19–specific literature and should be made a priority for future research. Studies also included little information regarding the cost-effectiveness of telemental health implementation. Further research is needed to explore the differences in cost (both to the service and to the service user) between face-to-face and telemental health care. Further research can also formally compare (rather than simply observe) different delivery support strategies that can improve the implementation and potentially also the clinical effectiveness of telemental health, including for specific conditions and service user groups.
Lived experience perspective commentary.
Lived experience commentary by Karen Machin and Raza Griffiths, members of the NIHR Mental Health Policy Unit's Lived Experience Working Group.
Systematic reviews aim to give an overview of research findings around a particular topic, although, as in this review, they may find that many of the primary studies are of moderate to low quality. At times of intense pressure, such as those presented by the COVID pandemic, overviews may be welcomed, and researchers may feel a need to respond promptly. This urgency creates a potential for gaps to be overlooked.
The main concern for us is around service user involvement, which has been acknowledged as key to good quality research, but has still not become the default for research teams. Participatory approaches are largely absent from the reviewed studies, with service user and carer views “reported by clinicians” ignoring the likelihood of misunderstandings and service user views being skewed by unequal power dynamics. There is no statement about the involvement of lived experience researchers in the review itself either. While some researchers may not wish to expose their personal experiences, it is important to be clear about the level of involvement within all studies.
Service users can shine a spotlight on aspects of mental health support of importance to people who rely on services which may otherwise be missed. Their lack of involvement in this review may be one reason why only one out of 41 primary research studies reviewed looks at the voluntary sector, and none at peer support or social care. It is unclear if this is a result of the review process itself or a lack of evidence. Had service users been involved, this fundamental gap might have been explored at an earlier stage.
The review does identify some factors that can help determine how useful or accessible telemental health is for different groups of people. However, an analysis linking these factors to broader underlying factors such as poverty would be more helpful.
Further research is needed to ensure future service planning can more accurately assess which elements of telemental health work well, why, and for whom, and to have service user involvement integral to the whole process from beginning to end.
Finally, there is scope to conduct big data studies to identify who is not accessing remote care or those at risk of disengaging, and potential comparisons for matched groups to try to compare effectiveness across a range of settings, as this could be done more quickly than in clinical trials while respecting patient preference.
Strengths and Limitations
The studies included in this review identified outcomes across different settings and health care systems, which may help findings generalize to different settings. This review also captured recent findings on the use of telemental health during the COVID-19 pandemic, allowing findings to be used to improve both existing and future models of remote mental health care.
However, it is also important to take some limitations into account when interpreting the findings from this review. First, the results from quality assessment indicated that while around half of primary research studies and the majority of the service evaluations were high quality, around half of primary research studies were scored as moderate to low. This reflects the short nature of studies and often quick turnaround from data collection to publication. Some studies were also published in preprint form and therefore had not undergone peer review. The majority of studies used cross-sectional data, rather than more rigorous methods. Second, there was a lack of high-quality quantitative evidence for the clinical effectiveness of telemental health care. Clinical effectiveness outcomes were only reported in 9/77 included studies, with some of these findings only based on qualitative evidence or a small number of service users. It is also important to note that the voices of those who dropped out of care may not be included.
The short time scale for data collection and assessment of changes in practice in included studies could also be viewed as a limitation of this research, as it is not clear if changes will be sustained over time or in other contexts (eg, lower-income countries). We also recognize that the search dates do not cover the whole of the pandemic to date; however, as plans for the medium- to long-term adoption of telemental health are currently being made in several countries, we think it best to make the findings from this research available promptly. Research was also not inclusive of those not accessing or using remote technologies, meaning there is a risk of those at risk of digital exclusion being forgotten when taking the findings of this review into consideration.
We also designed this review to be conducted rapidly to ensure results would be relevant and quickly available, therefore we chose to search 4 databases and not all studies were independently double screened by blinded researchers. Although quality assessment was conducted by 2 reviewers independently, they were also not blinded to the previous decision. However, we are confident that the rigor of our searches and inclusion of preprint servers meant that the papers included are representative of the literature on this topic.
Conclusion
Telemental health was a largely effective method to enable continuation of mental health support during the COVID-19 pandemic. While most reported outcomes were positive, telemental health was not feasible for all types of support and may not be acceptable to all service user groups. A blended approach combining face-to-face and telemental health care may be the most desirable service model for future care. The need remains for higher-quality evidence regarding the clinical effectiveness of telemental health and how uptake can be improved for groups at risk of digital exclusion.
Acknowledgments
Policy Research Unit
This paper presents independent research commissioned and funded by the National Institute for Health Research (NIHR) Policy Research Programme, conducted by the NIHR Policy Research Unit (PRU) in Mental Health. The views expressed are those of the authors and not necessarily those of the NIHR, the Department of Health and Social Care or its arm’s length bodies, or other government departments.
Applied Research Collaboration South London and King’s Improvement Science
This study is supported by the National Institute for Health Research (NIHR) Applied Research Collaboration South London (NIHR ARC South London) at King’s College Hospital NHS Foundation Trust. NS and LG are members of King’s Improvement Science, which offers co-funding to the NIHR ARC South London and is funded by King’s Health Partners (Guy’s and St Thomas’ NHS Foundation Trust, King’s College Hospital NHS Foundation Trust, King’s College London and South London and Maudsley NHS Foundation Trust), and Guy’s and St Thomas’ Foundation. The views expressed are those of the author(s) and not necessarily those of the NIHR, the NHS, the charities, or the Department of Health and Social Care.
LG is funded by King’s Improvement Science, which is part of the NIHR ARC South London and comprises a specialist team of improvement scientists and senior researchers based at King’s College London. King’s Improvement Science is funded by King’s Health Partners (Guy’s and St Thomas’ NHS Foundation Trust, King’s College Hospital NHS Foundation Trust, King’s College London and South London and Maudsley NHS Foundation Trust), and the Guy’s and St Thomas’ Foundation.
Abbreviations
- AACODS
authority, accuracy, coverage, objectivity, date, significance (tool)
- CFIR
Consolidated Framework for Implementation Research
- CMHT
community mental health team
- MMAT
Mixed Methods Appraisal Tool
- NHS
National Health Service
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Supplementary Table 1 - PubMed search strategy.
Supplementary Table 2 - Details of study characteristics.
Footnotes
Conflicts of Interest: NS is the director of the London Safety and Training Solutions Ltd, which offers training in patient safety, implementation solutions and human factors to healthcare organizations and the pharmaceutical industry. The other authors have no conflicts of interest to declare.
References
- 1.World Health Organization The Impact of COVID-19 on Mental, Neurological and Substance Use Services: Results of a Rapid Assessment. 2020. [2021-11-29]. https://www.who.int/publications/i/item/978924012455 .
- 2.Pfefferbaum B, North CS. Mental Health and the Covid-19 Pandemic. N Engl J Med. 2020 Aug 06;383(6):510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- 3.Rajkumar RP. COVID-19 and mental health: A review of the existing literature. Asian J Psychiatr. 2020 Aug;52:102066. doi: 10.1016/j.ajp.2020.102066. http://europepmc.org/abstract/MED/32302935 .S1876-2018(20)30177-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sheridan Rains Luke, Johnson S, Barnett P, Steare T, Needle J, Carr S, Lever Taylor Billie, Bentivegna Francesca, Edbrooke-Childs Julian, Scott Hannah Rachel, Rees Jessica, Shah Prisha, Lomani Jo, Chipp Beverley, Barber Nick, Dedat Zainab, Oram Sian, Morant Nicola, Simpson Alan, COVID-19 Mental Health Policy Research Unit Group Early impacts of the COVID-19 pandemic on mental health care and on people with mental health conditions: framework synthesis of international experiences and responses. Soc Psychiatry Psychiatr Epidemiol. 2021 Jan;56(1):13–24. doi: 10.1007/s00127-020-01924-7. http://europepmc.org/abstract/MED/32804258 .10.1007/s00127-020-01924-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moreno C, Wykes T, Galderisi S, Nordentoft M, Crossley N, Jones N, Cannon M, Correll CU, Byrne L, Carr S, Chen EYH, Gorwood P, Johnson S, Kärkkäinen Hilkka, Krystal JH, Lee J, Lieberman J, López-Jaramillo Carlos, Männikkö Miia, Phillips MR, Uchida H, Vieta E, Vita A, Arango C. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. 2020 Sep;7(9):813–824. doi: 10.1016/S2215-0366(20)30307-2. http://europepmc.org/abstract/MED/32682460 .S2215-0366(20)30307-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Psychological Association What Are Telehealth and Telepsychology. 2017. [2021-11-25]. https://www.apa.org/pi/disability/resources/publications/telepsychology .
- 7.Johnson S, Dalton-Locke C, Vera San Juan Norha, Foye U, Oram S, Papamichail A, Landau Sabine, Rowan Olive Rachel, Jeynes Tamar, Shah Prisha, Sheridan Rains Luke, Lloyd-Evans Brynmor, Carr Sarah, Killaspy Helen, Gillard Steve, Simpson Alan, COVID-19 Mental Health Policy Research Unit Group Impact on mental health care and on mental health service users of the COVID-19 pandemic: a mixed methods survey of UK mental health care staff. Soc Psychiatry Psychiatr Epidemiol. 2021 Jan;56(1):25–37. doi: 10.1007/s00127-020-01927-4. http://europepmc.org/abstract/MED/32857218 .10.1007/s00127-020-01927-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Telehealth bibliography. Telebehavioural Health Institute. [2021-12-01]. https://telehealth.org/bibliography/
- 9.Bashshur RL, Shannon GW, Bashshur N, Yellowlees PM. The Empirical Evidence for Telemedicine Interventions in Mental Disorders. Telemed J E Health. 2016 Mar;22(2):87–113. doi: 10.1089/tmj.2015.0206. http://europepmc.org/abstract/MED/26624248 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Salmoiraghi A, Hussain S. A Systematic Review of the Use of Telepsychiatry in Acute Settings. J Psychiatr Pract. 2015 Sep;21(5):389–93. doi: 10.1097/PRA.0000000000000103.00131746-201509000-00009 [DOI] [PubMed] [Google Scholar]
- 11.Hilty DM, Ferrer DC, Parish MB, Johnston B, Callahan EJ, Yellowlees PM. The effectiveness of telemental health: a 2013 review. Telemed J E Health. 2013 Jun;19(6):444–54. doi: 10.1089/tmj.2013.0075. http://europepmc.org/abstract/MED/23697504 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hubley S, Lynch SB, Schneck C, Thomas M, Shore J. Review of key telepsychiatry outcomes. World J Psychiatry. 2016 Jun 22;6(2):269–82. doi: 10.5498/wjp.v6.i2.269. https://www.wjgnet.com/2220-3206/full/v6/i2/269.htm . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Varker T, Brand RM, Ward J, Terhaag S, Phelps A. Efficacy of synchronous telepsychology interventions for people with anxiety, depression, posttraumatic stress disorder, and adjustment disorder: A rapid evidence assessment. Psychol Serv. 2019 Nov;16(4):621–635. doi: 10.1037/ser0000239.2018-24930-001 [DOI] [PubMed] [Google Scholar]
- 14.Fletcher TL, Hogan JB, Keegan F, Davis ML, Wassef M, Day S, Lindsay JA. Recent Advances in Delivering Mental Health Treatment via Video to Home. Curr Psychiatry Rep. 2018 Jul 21;20(8):56. doi: 10.1007/s11920-018-0922-y.10.1007/s11920-018-0922-y [DOI] [PubMed] [Google Scholar]
- 15.Barnett P, Goulding L, Casetta C, Jordan H, Sheridan-Rains Luke, Steare T, Williams Julie, Wood Lisa, Gaughran Fiona, Johnson Sonia. Implementation of Telemental Health Services Before COVID-19: Rapid Umbrella Review of Systematic Reviews. J Med Internet Res. 2021 Jul 20;23(7):e26492. doi: 10.2196/26492. https://www.jmir.org/2021/7/e26492/ v23i7e26492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gloff NE, LeNoue SR, Novins DK, Myers K. Telemental health for children and adolescents. Int Rev Psychiatry. 2015 Nov 05;27(6):513–24. doi: 10.3109/09540261.2015.1086322. [DOI] [PubMed] [Google Scholar]
- 17.Seritan AL, Heiry M, Iosif A, Dodge M, Ostrem JL. Telepsychiatry for patients with movement disorders: a feasibility and patient satisfaction study. J Clin Mov Disord. 2019;6:1. doi: 10.1186/s40734-019-0077-y. https://clinicalmovementdisorders.biomedcentral.com/articles/10.1186/s40734-019-0077-y .77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Santesteban-Echarri O, Piskulic D, Nyman RK, Addington J. Telehealth interventions for schizophrenia-spectrum disorders and clinical high-risk for psychosis individuals: A scoping review. J Telemed Telecare. 2020;26(1-2):14–20. doi: 10.1177/1357633X18794100. [DOI] [PubMed] [Google Scholar]
- 19.Gentry MT, Lapid MI, Clark MM, Rummans TA. Evidence for telehealth group-based treatment: A systematic review. J Telemed Telecare. 2019 Jul;25(6):327–342. doi: 10.1177/1357633X18775855. [DOI] [PubMed] [Google Scholar]
- 20.Connolly SL, Miller CJ, Lindsay JA, Bauer MS. A systematic review of providers’ attitudes toward telemental health via videoconferencing. Clinical Psychology: Science and Practice. 2020 Jun;27(2):e12311. doi: 10.1111/cpsp.12311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vera San Juan Norha, Shah P, Schlief M, Appleton R, Nyikavaranda P, Birken M, Foye Una, Lloyd-Evans Brynmor, Morant Nicola, Needle Justin J, Simpson Alan, Lyons Natasha, Rains Luke Sheridan, Dedat Zainab, Johnson Sonia. Service user experiences and views regarding telemental health during the COVID-19 pandemic: A co-produced framework analysis. PLoS One. 2021;16(9):e0257270. doi: 10.1371/journal.pone.0257270. https://dx.plos.org/10.1371/journal.pone.0257270 .PONE-D-21-05340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stoll J, Müller Jonas Adrian, Trachsel M. Ethical Issues in Online Psychotherapy: A Narrative Review. Front Psychiatry. 2019 Feb 11;10:993. doi: 10.3389/fpsyt.2019.00993. doi: 10.3389/fpsyt.2019.00993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tullio V, Perrone G, Bilotta C, Lanzarone A, Argo A. Psychological support and psychotherapy via digital devices in Covid-19 emergency time: Some critical issues. Med Leg J. 2020 Jul 03;88(2):73–76. doi: 10.1177/0025817220926942. [DOI] [PubMed] [Google Scholar]
- 24.Europe Economics Regulatory Approaches to Telemedicine. 2018. [2021-11-26]. https://www.gmc-uk.org/about/what-we-do-and-why/data-and-research/research-and-insight-archive/regulatory-approaches-to-telemedicine .
- 25.Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: A systematic review. J Telemed Telecare. 2018 Jan;24(1):4–12. doi: 10.1177/1357633X16674087. https://journals.sagepub.com/doi/10.1177/1357633X16674087?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cowan K, McKean A, Gentry M, Hilty D. Barriers to Use of Telepsychiatry: Clinicians as Gatekeepers. Mayo Clin Proc. 2019 Dec;94(12):2510–2523. doi: 10.1016/j.mayocp.2019.04.018.S0025-6196(19)30400-8 [DOI] [PubMed] [Google Scholar]
- 27.Vis C, Mol M, Kleiboer A, Bührmann Leah, Finch T, Smit J, Riper H. Improving Implementation of eMental Health for Mood Disorders in Routine Practice: Systematic Review of Barriers and Facilitating Factors. JMIR Ment Health. 2018 Mar 16;5(1):e20. doi: 10.2196/mental.9769. https://mental.jmir.org/2018/1/e20/ v5i1e20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sharma A, Sasser T, Schoenfelder Gonzalez E, Vander Stoep A, Myers K. Implementation of Home-Based Telemental Health in a Large Child Psychiatry Department During the COVID-19 Crisis. J Child Adolesc Psychopharmacol. 2020 Sep 01;30(7):404–413. doi: 10.1089/cap.2020.0062. [DOI] [PubMed] [Google Scholar]
- 29.Connolly SL, Stolzmann KL, Heyworth L, Weaver KR, Bauer MS, Miller CJ. Rapid Increase in Telemental Health Within the Department of Veterans Affairs During the COVID-19 Pandemic. Telemed J E Health. 2021 Apr 01;27(4):454–458. doi: 10.1089/tmj.2020.0233. [DOI] [PubMed] [Google Scholar]
- 30.Gentry MT, Puspitasari AJ, McKean AJ, Williams MD, Breitinger S, Geske JR, Clark MM, Moore KM, Frye MA, Hilty DM. Clinician Satisfaction with Rapid Adoption and Implementation of Telehealth Services During the COVID-19 Pandemic. Telemed J E Health. 2021 Mar 19;:e1. doi: 10.1089/tmj.2020.0575. (forthcoming) [DOI] [PubMed] [Google Scholar]
- 31.Nicholas J, Bell IH, Thompson A, Valentine L, Simsir P, Sheppard H, Adams S. Implementation lessons from the transition to telehealth during COVID-19: a survey of clinicians and young people from youth mental health services. Psychiatry Res. 2021 May;299:113848. doi: 10.1016/j.psychres.2021.113848.S0165-1781(21)00145-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Smith K, Ostinelli E, Macdonald O, Cipriani A. COVID-19 and Telepsychiatry: Development of Evidence-Based Guidance for Clinicians. JMIR Ment Health. 2020 Aug 28;7(8):e21108. doi: 10.2196/21108. https://mental.jmir.org/2020/8/e21108/ v7i8e21108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009 Jul 21;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. https://dx.plos.org/10.1371/journal.pmed.1000097 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.The Endnote Team . Endnote X9. Philadelphia, PA: Clarivate; 2013. [Google Scholar]
- 35.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016 Dec 05;5(1):210. doi: 10.1186/s13643-016-0384-4. https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-016-0384-4 .10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009 Aug 07;4(1):50. doi: 10.1186/1748-5908-4-50. https://implementationscience.biomedcentral.com/articles/10.1186/1748-5908-4-50 .1748-5908-4-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, Griffey R, Hensley M. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. 2011 Mar 19;38(2):65–76. doi: 10.1007/s10488-010-0319-7. http://europepmc.org/abstract/MED/20957426 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Safaeinili N, Brown-Johnson Cati, Shaw JG, Mahoney M, Winget M. CFIR simplified: Pragmatic application of and adaptations to the Consolidated Framework for Implementation Research (CFIR) for evaluation of a patient-centered care transformation within a learning health system. Learn Health Syst. 2020 Sep 26;4(1):e10201. doi: 10.1002/lrh2.10201. doi: 10.1002/lrh2.10201.LRH210201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Thomas J, Graziosi S, Brunton J, Ghouze Z, O'Driscoll P, Bond M. EPPI-Reviewer: Advanced Software for Systematic Reviews, Maps and Evidence Synthesis. London, UK: UCL Social Research Institute; 2020. [Google Scholar]
- 40.Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, Gagnon M, Griffiths F, Nicolau B, O’Cathain A, Rousseau M, Vedel I, Pluye P. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. EFI. 2018 Dec 18;34(4):285–291. doi: 10.3233/efi-180221. [DOI] [Google Scholar]
- 41.Tyndall J. AACODS Checklist. 2010. [2021-01-12]. https://dspace.flinders.edu.au/xmlui/bitstream/handle/2328/3326/AACODS_Checklist.pdf .
- 42.Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews. 2006. [2021-11-25]. https://www.lancaster.ac.uk/media/lancaster-university/content-assets/documents/fhm/dhr/chir/NSsynthesisguidanceVersion1-April2006.pdf .
- 43.Aafjes-van Doorn K, Békés V, Prout TA. Grappling with our therapeutic relationship and professional self-doubt during COVID-19: will we use video therapy again? Counselling Psychology Quarterly. 2020 Jun 03;:1–12. doi: 10.1080/09515070.2020.1773404. [DOI] [Google Scholar]
- 44.Anton MT, Ridings LE, Gavrilova Y, Bravoco O, Ruggiero KJ, Davidson TM. Transitioning a technology-assisted stepped-care model for traumatic injury patients to a fully remote model in the age of COVID-19. Counselling Psychology Quarterly. 2020 Jun 26;:1–12. doi: 10.1080/09515070.2020.1785393. [DOI] [Google Scholar]
- 45.Barney A, Buckelew S, Mesheriakova V, Raymond-Flesch M. The COVID-19 Pandemic and Rapid Implementation of Adolescent and Young Adult Telemedicine: Challenges and Opportunities for Innovation. J Adolesc Health. 2020 Aug;67(2):164–171. doi: 10.1016/j.jadohealth.2020.05.006. http://europepmc.org/abstract/MED/32410810 .S1054-139X(20)30225-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Békés V, Aafjes-van Doorn K. Psychotherapists’ attitudes toward online therapy during the COVID-19 pandemic. Journal of Psychotherapy Integration. 2020 Jun;30(2):238–247. doi: 10.1037/int0000214. [DOI] [Google Scholar]
- 47.Békés Vera, Aafjes-van Doorn Katie, Prout TA, Hoffman L. Stretching the Analytic Frame: Analytic Therapists' Experiences with Remote Therapy During COVID-19. J Am Psychoanal Assoc. 2020 Jun 26;68(3):437–446. doi: 10.1177/0003065120939298. [DOI] [PubMed] [Google Scholar]
- 48.Benaque A, Gurruchaga MJ, Abdelnour C, Hernández Isabel, Cañabate Pilar, Alegret M, Rodríguez Isabel, Rosende-Roca M, Tartari JP, Esteban E, López Rogelio, Gil S, Vargas L, Mauleón Ana, Espinosa A, Ortega G, Sanabria A, Pérez Alba, Alarcón Emilio, González-Pérez Antonio, Marquié Marta, Valero S, Tárraga Lluís, Ruiz A, Boada M, Research CenterMemory Clinic‚ Fundació ACE Dementia Care in Times of COVID-19: Experience at Fundació ACE in Barcelona, Spain. J Alzheimers Dis. 2020;76(1):33–40. doi: 10.3233/JAD-200547. http://europepmc.org/abstract/MED/32538856 .JAD200547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Berdullas Saunders Silvia, Gesteira Santos Clara, Morán Rodríguez Noelia, Fernández Hermida José Ramón, Santolaya F, Sanz Fernández Jesús, García-Vera María Paz. [The COVID-19 psychological helpline of the Spanish Ministry of Health and Spanish Psychological Association: characteristics and demand.] Rev Esp Salud Publica. 2020 Oct 14;94:e1. (forthcoming) [PMC free article] [PubMed] [Google Scholar]
- 50.Bhome R, Huntley J, Dalton-Locke C, San Juan NV, Oram S, Foye U, Livingston G. Impact of the COVID-19 pandemic on older adults mental health services: A mixed methods study. Int J Geriatr Psychiatry. 2021 Nov;36(11):1748–1758. doi: 10.1002/gps.5596. http://europepmc.org/abstract/MED/34216045 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bierbooms JJPA, van Haaren M, IJsselsteijn WA, de Kort YAW, Feijt M, Bongers IMB. Integration of Online Treatment Into the "New Normal" in Mental Health Care in Post-COVID-19 Times: Exploratory Qualitative Study. JMIR Form Res. 2020 Oct 08;4(10):e21344. doi: 10.2196/21344. https://formative.jmir.org/2020/10/e21344/ v4i10e21344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Boldrini T, Schiano Lomoriello A, Del Corno F, Lingiardi V, Salcuni S. Psychotherapy During COVID-19: How the Clinical Practice of Italian Psychotherapists Changed During the Pandemic. Front Psychol. 2020 Oct 21;11:591170. doi: 10.3389/fpsyg.2020.591170. doi: 10.3389/fpsyg.2020.591170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Burton A, McKinlay A, Aughterson H, Fancourt D. Impact of the COVID-19 pandemic on the mental health and well-being of adults with mental health conditions in the UK: a qualitative interview study. J Ment Health. 2021 Jul 29;:1–8. doi: 10.1080/09638237.2021.1952953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Carpiniello B, Tusconi M, di Sciascio Guido, Zanalda E, di Giannantonio Massimo, Executive Committee of the Italian Society of Psychiatry Mental health services in Italy during the COVID-19 pandemic. Psychiatry Clin Neurosci. 2020 Aug 30;74(8):442–443. doi: 10.1111/pcn.13082. doi: 10.1111/pcn.13082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cheli S, Cavalletti V, Petrocchi N. An online compassion-focused crisis intervention during COVID-19 lockdown: a cases series on patients at high risk for psychosis. Psychosis. 2020 Jul 20;12(4):359–362. doi: 10.1080/17522439.2020.1786148. [DOI] [Google Scholar]
- 56.Chen JA, Chung W, Young SK, Tuttle MC, Collins MB, Darghouth SL, Longley R, Levy R, Razafsha M, Kerner JC, Wozniak J, Huffman JC. COVID-19 and telepsychiatry: Early outpatient experiences and implications for the future. Gen Hosp Psychiatry. 2020 Sep;66:89–95. doi: 10.1016/j.genhosppsych.2020.07.002. http://europepmc.org/abstract/MED/32750604 .S0163-8343(20)30103-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Childs AW, Unger A, Li L. Rapid design and deployment of intensive outpatient, group-based psychiatric care using telehealth during coronavirus disease 2019 (COVID-19) J Am Med Inform Assoc. 2020 Jul 01;27(9):1420–1424. doi: 10.1093/jamia/ocaa138. http://europepmc.org/abstract/MED/32687151 .5873874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Colle R, Ait Tayeb AEK, de Larminat Delphine, Commery L, Boniface B, Lasica P, Gressier F, Mecifi R, Rotenberg S, Rigal A, Zitoun S, Mezzacappa A, Nicolicea C, Chaneac E, Martin S, Choucha W, Hardy P, Schouman-Claeys Elisabeth, Corruble E. Short-term acceptability by patients and psychiatrists of the turn to psychiatric teleconsultation in the context of the COVID-19 pandemic. Psychiatry Clin Neurosci. 2020 Aug 28;74(8):443–444. doi: 10.1111/pcn.13081. doi: 10.1111/pcn.13081. [DOI] [PubMed] [Google Scholar]
- 59.Datta N, Derenne J, Sanders M, Lock JD. Telehealth transition in a comprehensive care unit for eating disorders: Challenges and long-term benefits. Int J Eat Disord. 2020 Nov 27;53(11):1774–1779. doi: 10.1002/eat.23348. [DOI] [PubMed] [Google Scholar]
- 60.Dores AR, Geraldo A, Carvalho IP, Barbosa F. The Use of New Digital Information and Communication Technologies in Psychological Counseling during the COVID-19 Pandemic. Int J Environ Res Public Health. 2020 Oct 21;17(20):7663. doi: 10.3390/ijerph17207663. https://www.mdpi.com/resolver?pii=ijerph17207663 .ijerph17207663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Erekson DM, Bailey RJ, Cattani K, Fox ST, Goates-Jones MK. Responding to the Covid-19 pandemic at a university counseling center: administrative actions, client retention, and psychotherapy outcome. Counselling Psychology Quarterly. 2020 Aug 17;:1–15. doi: 10.1080/09515070.2020.1807914. [DOI] [Google Scholar]
- 62.Feijt M, de Kort Y, Bongers I, Bierbooms J, Westerink J, IJsselsteijn W. Mental Health Care Goes Online: Practitioners' Experiences of Providing Mental Health Care During the COVID-19 Pandemic. Cyberpsychol Behav Soc Netw. 2020 Dec 01;23(12):860–864. doi: 10.1089/cyber.2020.0370. [DOI] [PubMed] [Google Scholar]
- 63.Fernández-Aranda Fernando, Munguía Lucero, Mestre-Bach Gemma, Steward Trevor, Etxandi Mikel, Baenas Isabel, Granero Roser, Sánchez Isabel, Ortega Emilio, Andreu Alba, Moize Violeta L, Fernández-Real Jose M, Tinahones Francisco J, Diegüez Carlos, Frühbeck Gema, Le Grange Daniel, Tchanturia Kate, Karwautz Andreas, Zeiler Michael, Favaro Angela, Claes Laurence, Luyckx Koen, Shekriladze Ia, Serrano-Troncoso Eduardo, Rangil Teresa, Meler Maria Eulalia Loran, Soriano-Pacheco Jose, Carceller-Sindreu Mar, Bujalance-Arguijo Sara, Lozano Meritxell, Linares Raquel, Gudiol Carlota, Carratala Jordi, Sanchez-Gonzalez Jessica, Machado Paulo Pp, Håkansson Anders, Túry Ferenc, Pászthy Bea, Stein Daniel, Papezová Hana, Bax Brigita, Borisenkov Mikhail F, Popov Sergey V, Kim Youl-Ri, Nakazato Michiko, Godart Nathalie, van Voren Robert, Ilnytska Tetiana, Chen Jue, Rowlands Katie, Treasure Janet, Jiménez-Murcia Susana. COVID Isolation Eating Scale (CIES): Analysis of the impact of confinement in eating disorders and obesity-A collaborative international study. Eur Eat Disord Rev. 2020 Nov;28(6):871–883. doi: 10.1002/erv.2784. http://europepmc.org/abstract/MED/32954595 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Foye U, Dalton-Locke C, Harju-Seppänen Jasmine, Lane R, Beames Lewys, Vera San Juan Norha, Johnson Sonia, Simpson Alan. How has COVID-19 affected mental health nurses and the delivery of mental health nursing care in the UK? Results of a mixed-methods study. J Psychiatr Ment Health Nurs. 2021 Apr;28(2):126–137. doi: 10.1111/jpm.12745. http://europepmc.org/abstract/MED/33608956 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gaddy S, Gallardo R, McCluskey S, Moore L, Peuser A, Rotert R. COVID-19 and Music Therapists' Employment, Service Delivery, Perceived Stress, and Hope: A Descriptive Study. Music Therapy Perspectives. 2020 Sep 08;38(2):157–166. doi: 10.1093/mtp/miaa018. [DOI] [Google Scholar]
- 66.Gillard S, Dare C, Hardy J, Nyikavaranda P, Rowan Olive R, Shah P, Birken M, Foye U, Ocloo J, Pearce E, Stefanidou T, Pitman A, Simpson A, Johnson S, Lloyd-Evans B, NIHR Mental Health Policy Research Unit Covid coproduction research group Experiences of living with mental health problems during the COVID-19 pandemic in the UK: a coproduced, participatory qualitative interview study. Soc Psychiatry Psychiatr Epidemiol. 2021 Aug;56(8):1447–1457. doi: 10.1007/s00127-021-02051-7. http://europepmc.org/abstract/MED/33665680 .10.1007/s00127-021-02051-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gomet R, Souchet C, Mouellic ML, Maafa M, Labey A. Addiction outpatient hospital reinvents itself during the Coronavirus outbreak. Alcoologie et Addictologie. 2020;42(1):54–57. [Google Scholar]
- 68.Graell M, Morón-Nozaleda M Goretti, Camarneiro R, Villaseñor Ángel, Yáñez Silvia, Muñoz Rudiger, Martínez-Núñez Beatriz, Miguélez-Fernández Carolina, Muñoz María, Faya M. Children and adolescents with eating disorders during COVID-19 confinement: Difficulties and future challenges. Eur Eat Disord Rev. 2020 Nov 29;28(6):864–870. doi: 10.1002/erv.2763. [DOI] [PubMed] [Google Scholar]
- 69.Grover S, Mishra E, Chakrabarti S, Mehra A, Sahoo S. Telephonic monitoring of patients on clozapine in the resource-poor setting during the COVID-19 pandemic. Schizophr Res. 2020 Aug;222:489–490. doi: 10.1016/j.schres.2020.05.062. http://europepmc.org/abstract/MED/32563610 .S0920-9964(20)30342-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Grover S, Mehra A, Sahoo S, Avasthi A, Tripathi A, D'Souza A, Saha G, Jagadhisha A, Gowda M, Vaishnav M, Singh O, Dalal P, Kumar P. Impact of COVID-19 pandemic and lockdown on the state of mental health services in the private sector in India. Indian J Psychiatry. 2020;62(5):488. doi: 10.4103/psychiatry.indianjpsychiatry_568_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Grover S, Mehra A, Sahoo S, Avasthi A, Tripathi A, D'Souza A, Saha G, Jagadhisha A, Gowda M, Vaishnav M, Singh O, Dalal P, Kumar P. State of mental health services in various training centers in India during the lockdown and COVID-19 pandemic. Indian J Psychiatry. 2020;62(4):363. doi: 10.4103/psychiatry.indianjpsychiatry_567_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Haxhihamza K, Arsova S, Bajraktarov S, Kalpak G, Stefanovski B, Novotni A, Milutinovic M. Patient Satisfaction with Use of Telemedicine in University Clinic of Psychiatry: Skopje, North Macedonia During COVID-19 Pandemic. Telemed J E Health. 2021 Apr 01;27(4):464–467. doi: 10.1089/tmj.2020.0256. [DOI] [PubMed] [Google Scholar]
- 73.He Z, Chen J, Pan K, Yue Y, Cheung T, Yuan Y, Du N, Zhao Y, Feng Y, Zhou D, Zhou Y, Lu F, Chen Y, He M, Xiang Y. The development of the 'COVID-19 Psychological Resilience Model' and its efficacy during the COVID-19 pandemic in China. Int J Biol Sci. 2020;16(15):2828–2834. doi: 10.7150/ijbs.50127. https://www.ijbs.com/v16p2828.htm .ijbsv16p2828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hom MA, Weiss RB, Millman ZB, Christensen K, Lewis EJ, Cho S, Yoon S, Meyer NA, Kosiba JD, Shavit E, Schrock MD, Levendusky PG, Björgvinsson T. Development of a virtual partial hospital program for an acute psychiatric population: Lessons learned and future directions for telepsychotherapy. Journal of Psychotherapy Integration. 2020 Jun;30(2):366–382. doi: 10.1037/int0000212. [DOI] [Google Scholar]
- 75.Humer E, Pieh C, Kuska M, Barke A, Doering BK, Gossmann K, Trnka R, Meier Z, Kascakova N, Tavel P, Probst T. Provision of Psychotherapy during the COVID-19 Pandemic among Czech, German and Slovak Psychotherapists. Int J Environ Res Public Health. 2020 Jul 04;17(13):4811. doi: 10.3390/ijerph17134811. https://www.mdpi.com/resolver?pii=ijerph17134811 .ijerph17134811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Humer E, Stippl P, Pieh C, Schimböck Wolfgang, Probst T. Psychotherapy via the Internet: What Programs Do Psychotherapists Use, How Well-Informed Do They Feel, and What Are Their Wishes for Continuous Education? Int J Environ Res Public Health. 2020 Nov 05;17(21):8182. doi: 10.3390/ijerph17218182. https://www.mdpi.com/resolver?pii=ijerph17218182 .ijerph17218182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Izakova L, Breznoscakova D, Jandova K, Valkucakova V, Bezakova G, Suvada J. What mental health experts in Slovakia are learning from COVID-19 pandemic? Indian J Psychiatry. 2020;62(9):459. doi: 10.4103/psychiatry.indianjpsychiatry_758_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Jurcik T, Jarvis GE, Zeleskov Doric J, Krasavtseva Y, Yaltonskaya A, Ogiwara K, Sasaki J, Dubois S, Grigoryan K. Adapting mental health services to the COVID-19 pandemic: reflections from professionals in four countries. Counselling Psychology Quarterly. 2020 Jul 16;:1–27. doi: 10.1080/09515070.2020.1785846. [DOI] [Google Scholar]
- 79.Khanna R, Murnane T, Kumar S, Rolfe T, Dimitrieski S, McKeown M, Ejareh Dar Maryam, Gavson L, Gandhi C. Making working from home work: reflections on adapting to change. Australas Psychiatry. 2020 Oct 10;28(5):504–507. doi: 10.1177/1039856220953701. [DOI] [PubMed] [Google Scholar]
- 80.Kopec K, Janney CA, Johnson B, Spykerman K, Ryskamp B, Achtyes ED. Rapid Transition to Telehealth in a Community Mental Health Service Provider During the COVID-19 Pandemic. Prim. Care Companion CNS Disord. 2020 Oct 01;22(5):e1. doi: 10.4088/pcc.20br02787. [DOI] [PubMed] [Google Scholar]
- 81.Lai FH, Yan EW, Yu KK, Tsui W, Chan DT, Yee BK. The Protective Impact of Telemedicine on Persons With Dementia and Their Caregivers During the COVID-19 Pandemic. Am J Geriatr Psychiatry. 2020 Nov;28(11):1175–1184. doi: 10.1016/j.jagp.2020.07.019. http://europepmc.org/abstract/MED/32873496 .S1064-7481(20)30438-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lakeman R, Crighton J. The Impact of Social Distancing on People with Borderline Personality Disorder: The Views of Dialectical Behavioural Therapists. Issues Ment Health Nurs. 2021 May 15;42(5):410–416. doi: 10.1080/01612840.2020.1817208. [DOI] [PubMed] [Google Scholar]
- 83.Lin X, Swift J, Cheng Y, An Q, Liang H, Wang Y. The Psychological Hotline Services Quality Survey during the Pandemic of COVID-19 in Mainland China. International Journal of Mental Health Promotion. 2020;22(3):109–13. [Google Scholar]
- 84.Looi JC, Allison S, Bastiampillai T, Pring W. Private practice metropolitan telepsychiatry in smaller Australian jurisdictions during the COVID-19 pandemic: preliminary analysis of the introduction of new Medicare Benefits Schedule items. Australas Psychiatry. 2020 Dec 05;28(6):639–643. doi: 10.1177/1039856220960381. [DOI] [PubMed] [Google Scholar]
- 85.Looi JC, Allison S, Bastiampillai T, Pring W. Private practice metropolitan telepsychiatry in larger Australian states during the COVID-19 pandemic: an analysis of the first 2 months of new MBS telehealth item psychiatrist services. Australas Psychiatry. 2020 Dec 30;28(6):644–648. doi: 10.1177/1039856220961906. [DOI] [PubMed] [Google Scholar]
- 86.Lynch DA, Medalia A, Saperstein A. The Design, Implementation, and Acceptability of a Telehealth Comprehensive Recovery Service for People With Complex Psychosis Living in NYC During the COVID-19 Crisis. Front Psychiatry. 2020 Sep 8;11:581149. doi: 10.3389/fpsyt.2020.581149. doi: 10.3389/fpsyt.2020.581149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.McBeath AG, du Plock Simon, Bager-Charleson Sofie. The challenges and experiences of psychotherapists working remotely during the coronavirus pandemic. Couns Psychother Res. 2020 Jun 23;20(3):394–405. doi: 10.1002/capr.12326. http://europepmc.org/abstract/MED/32837329 .CAPR12326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Medalia A, Lynch DA, Herlands T. Telehealth Conversion of Serious Mental Illness Recovery Services During the COVID-19 Crisis. Psychiatr Serv. 2020 Aug 01;71(8):872–872. doi: 10.1176/appi.ps.71705. [DOI] [PubMed] [Google Scholar]
- 89.Miu AS, Vo HT, Palka JM, Glowacki CR, Robinson RJ. Teletherapy with serious mental illness populations during COVID-19: telehealth conversion and engagement. Counselling Psychology Quarterly. 2020 Jul 12;:1–18. doi: 10.1080/09515070.2020.1791800. [DOI] [Google Scholar]
- 90.Olwill C, Mc Nally D, Douglas L. Psychiatrist experience of remote consultations by telephone in an outpatient psychiatric department during the COVID-19 pandemic. Ir J Psychol Med. 2021 Jun 22;38(2):132–139. doi: 10.1017/ipm.2020.51. http://europepmc.org/abstract/MED/32438945 .S0790966720000518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Patel R, Irving J, Brinn A, Broadbent M, Shetty H, Pritchard M, Downs J, Stewart R, Harland R, McGuire P. Impact of the COVID-19 pandemic on remote mental healthcare and prescribing in psychiatry: an electronic health record study. BMJ Open. 2021 Mar 30;11(3):e046365. doi: 10.1136/bmjopen-2020-046365. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=33785494 .bmjopen-2020-046365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Peralta E, Taveras M. Effectiveness of teleconsultation use in access to mental health services during the coronavirus disease 2019 pandemic in the Dominican Republic. Indian J Psychiatry. 2020;62(9):492. doi: 10.4103/psychiatry.indianjpsychiatry_1047_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Pierce BS, Perrin PB, Tyler CM, McKee GB, Watson JD. The COVID-19 telepsychology revolution: A national study of pandemic-based changes in U.S. mental health care delivery. Am Psychol. 2021 Jan;76(1):14–25. doi: 10.1037/amp0000722.2020-61592-001 [DOI] [PubMed] [Google Scholar]
- 94.Probst T, Stippl P, Pieh C. Changes in Provision of Psychotherapy in the Early Weeks of the COVID-19 Lockdown in Austria. Int J Environ Res Public Health. 2020 May 27;17(11):3815. doi: 10.3390/ijerph17113815. https://www.mdpi.com/resolver?pii=ijerph17113815 .ijerph17113815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Reilly SE, Zane KL, McCuddy WT, Soulliard ZA, Scarisbrick DM, Miller LE, Mahoney Iii James J. Mental Health Practitioners' Immediate Practical Response During the COVID-19 Pandemic: Observational Questionnaire Study. JMIR Ment Health. 2020 Oct 01;7(9):e21237. doi: 10.2196/21237. https://mental.jmir.org/2020/9/e21237/ v7i9e21237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Roach P, Zwiers A, Cox E, Fischer K, Charlton A, Josephson C, Patten Scott B, Seitz Dallas, Ismail Zahinoor, Smith Eric E. Understanding the impact of the COVID-19 pandemic on well-being and virtual care for people living with dementia and care partners living in the community. Dementia (London) 2021 Aug;20(6):2007–2023. doi: 10.1177/1471301220977639. https://journals.sagepub.com/doi/10.1177/1471301220977639?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Roncero C, García-Ullán Llanyra, de la Iglesia-Larrad JI, Martín Carmen, Andrés Pilar, Ojeda A, González-Parra David, Pérez Javier, Fombellida C, Álvarez-Navares Ana, Benito JA, Dutil V, Lorenzo C, Montejo The response of the mental health network of the Salamanca area to the COVID-19 pandemic: The role of the telemedicine. Psychiatry Res. 2020 Sep;291:113252. doi: 10.1016/j.psychres.2020.113252. http://europepmc.org/abstract/MED/32623263 .S0165-1781(20)31600-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Rosen CS, Morland LA, Glassman LH, Marx BP, Weaver K, Smith CA, Pollack S, Schnurr PP. Virtual mental health care in the Veterans Health Administration's immediate response to coronavirus disease-19. Am Psychol. 2021 Jan;76(1):26–38. doi: 10.1037/amp0000751.2020-81589-001 [DOI] [PubMed] [Google Scholar]
- 99.Sasangohar F, Bradshaw MR, Carlson MM, Flack JN, Fowler JC, Freeland D, Head J, Marder K, Orme W, Weinstein B, Kolman JM, Kash B, Madan A. Adapting an Outpatient Psychiatric Clinic to Telehealth During the COVID-19 Pandemic: A Practice Perspective. J Med Internet Res. 2020 Oct 01;22(10):e22523. doi: 10.2196/22523. https://www.jmir.org/2020/10/e22523/ v22i10e22523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Scharff A, Breiner CE, Ueno LF, Underwood SB, Merritt EC, Welch LM, Fonda C, Weil Malatras J, Lin B, Hormes JM, Pieterse AL, Gordis EB, Halpern LF, Pazienza R, Litchford GB. Shifting a training clinic to teletherapy during the COVID-19 pandemic: a trainee perspective. Counselling Psychology Quarterly. 2020 Jun 28;:1–11. doi: 10.1080/09515070.2020.1786668. [DOI] [Google Scholar]
- 101.Schlegl S, Meule A, Favreau M, Voderholzer U. Bulimia nervosa in times of the COVID-19 pandemic-Results from an online survey of former inpatients. Eur Eat Disord Rev. 2020 Nov 07;28(6):847–854. doi: 10.1002/erv.2773. http://europepmc.org/abstract/MED/32767858 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sciarrino NA, Myers US, Wangelin BC. When chaos is the norm: How some veterans with PTSD are continuing to engage in trauma-focused treatments during the COVID-19 pandemic. Psychol Trauma. 2020 Aug;12(S1):S69–S70. doi: 10.1037/tra0000718.2020-37264-001 [DOI] [PubMed] [Google Scholar]
- 103.Sequeira A, Alozie A, Fasteau M, Lopez AK, Sy J, Turner KA, Werner C, McIngvale E, Björgvinsson T. Transitioning to virtual programming amidst COVID-19 outbreak. Counselling Psychology Quarterly. 2020 Jun 12;:1–16. doi: 10.1080/09515070.2020.1777940. [DOI] [Google Scholar]
- 104.Severe J, Tang R, Horbatch F, Onishchenko R, Naini V, Blazek MC. Factors Influencing Patients' Initial Decisions Regarding Telepsychiatry Participation During the COVID-19 Pandemic: Telephone-Based Survey. JMIR Form Res. 2020 Dec 22;4(12):e25469. doi: 10.2196/25469. https://formative.jmir.org/2020/12/e25469/ v4i12e25469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sheehan R, Dalton-Locke C, Ali A, Vera San Juan Norha, Totsika Vaso, Hassiotis A. Effects of the COVID-19 pandemic on mental healthcare and services: results of a UK survey of front-line staff working with people with intellectual disability and/or autism. BJPsych Bull. 2021 May 12;:1–7. doi: 10.1192/bjb.2021.52. https://www.cambridge.org/core/product/identifier/S2056469421000528/type/journal_article .S2056469421000528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sklar M, Reeder K, Carandang K, Ehrhart M, Aarons G. An Observational Study of the Impact of COVID-19 and the Transition to Telehealth on Community Mental Health Center Providers. Res Sq. 2020 Jul 29; doi: 10.21203/rs.3.rs-48767/v1. doi: 10.21203/rs.3.rs-48767/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Termorshuizen Jet D, Watson Hunna J, Thornton Laura M, Borg Stina, Flatt Rachael E, MacDermod Casey M, Harper Lauren E, van Furth Eric F, Peat Christine M, Bulik Cynthia M. Early impact of COVID-19 on individuals with self-reported eating disorders: A survey of ~1,000 individuals in the United States and the Netherlands. Int J Eat Disord. 2020 Nov;53(11):1780–1790. doi: 10.1002/eat.23353. [DOI] [PubMed] [Google Scholar]
- 108.Uscher-Pines L, Sousa J, Raja P, Mehrotra A, Barnett ML, Huskamp HA. Suddenly Becoming a "Virtual Doctor": Experiences of Psychiatrists Transitioning to Telemedicine During the COVID-19 Pandemic. Psychiatr Serv. 2020 Nov 01;71(11):1143–1150. doi: 10.1176/appi.ps.202000250. http://europepmc.org/abstract/MED/32933411 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Uscher-Pines L, Sousa J, Raja P, Mehrotra A, Barnett M, Huskamp HA. Treatment of opioid use disorder during COVID-19: Experiences of clinicians transitioning to telemedicine. J Subst Abuse Treat. 2020 Nov;118:108124. doi: 10.1016/j.jsat.2020.108124. http://europepmc.org/abstract/MED/32893047 .S0740-5472(20)30380-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.van Dijk SDM, Bouman R, Folmer EH, den Held RC, Warringa JE, Marijnissen RM, Voshaar RCO. (Vi)-rushed Into Online Group Schema Therapy Based Day-Treatment for Older Adults by the COVID-19 Outbreak in the Netherlands. Am J Geriatr Psychiatry. 2020 Sep;28(9):983–988. doi: 10.1016/j.jagp.2020.05.028. https://linkinghub.elsevier.com/retrieve/pii/S1064-7481(20)30367-5 .S1064-7481(20)30367-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Wang X, Gordon RM, Snyder EW. Comparing Chinese and US practitioners' attitudes towards teletherapy during the COVID-19 pandemic. Asia Pac Psychiatry. 2021 Mar 27;13(1):e12440. doi: 10.1111/appy.12440. http://europepmc.org/abstract/MED/33108828 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Wilson C, Dalton-Locke C, Johnson S, Simpson A, Oram S, Howard L. Challenges and opportunities of the COVID-19 pandemic for perinatal mental health care: a mixed-methods study of mental health care staff. Arch Womens Ment Health. 2021 Oct;24(5):749–757. doi: 10.1007/s00737-021-01108-5. http://europepmc.org/abstract/MED/33830374 .10.1007/s00737-021-01108-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Wood HJ, Gannon JM, Chengappa KR, Sarpal DK. Group teletherapy for first-episode psychosis: Piloting its integration with coordinated specialty care during the COVID-19 pandemic. Psychol Psychother. 2021 Jun 20;94(2):382–389. doi: 10.1111/papt.12310. [DOI] [PubMed] [Google Scholar]
- 114.Wyler H, Liebrenz M, Ajdacic-Gross V, Seifritz E, Young S, Burger P, Buadze A. Treatment provision for adults with ADHD during the COVID-19 pandemic: an exploratory study on patient and therapist experience with on-site sessions using face masks vs. telepsychiatric sessions. BMC Psychiatry. 2021 May 05;21(1):237. doi: 10.1186/s12888-021-03236-9. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-021-03236-9 .10.1186/s12888-021-03236-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Yellowlees P, Nakagawa K, Pakyurek M, Hanson A, Elder J, Kales HC. Rapid Conversion of an Outpatient Psychiatric Clinic to a 100% Virtual Telepsychiatry Clinic in Response to COVID-19. Psychiatr Serv. 2020 Jul 01;71(7):749–752. doi: 10.1176/appi.ps.202000230. [DOI] [PubMed] [Google Scholar]
- 116.Zulfic Z, Liu D, Lloyd C, Rowan J, Schubert KO. Is telepsychiatry care a realistic option for community mental health services during the COVID-19 pandemic? Aust N Z J Psychiatry. 2020 Dec 22;54(12):1228–1228. doi: 10.1177/0004867420937788. http://europepmc.org/abstract/MED/32571079 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Turgoose D, Ashwick R, Murphy D. Systematic review of lessons learned from delivering tele-therapy to veterans with post-traumatic stress disorder. J Telemed Telecare. 2018 Oct;24(9):575–585. doi: 10.1177/1357633X17730443. [DOI] [PubMed] [Google Scholar]
- 118.Norwood C, Moghaddam NG, Malins S, Sabin-Farrell Rachel. Working alliance and outcome effectiveness in videoconferencing psychotherapy: A systematic review and noninferiority meta-analysis. Clin Psychol Psychother. 2018 Nov;25(6):797–808. doi: 10.1002/cpp.2315. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1 - PubMed search strategy.
Supplementary Table 2 - Details of study characteristics.


