Abstract
Platelet-rich plasma (PRP) is being used as a treatment modality for skin rejuvenation since the last decade. There has been a lot of ambiguity regarding the ideal protocol to be followed and the specific indications where its use should be promoted. The use of PRP as monotherapy for skin rejuvenation, acne scars, periorbital rejuvenation, lipofilling and in combination with fractional CO2 and other resurfacing modalities is increasing rapidly. In this article, we have reviewed the current scientific evidence available and the IADVL national task force for PRP has come up with standard recommendations for use of PRP in esthetics along with the grade of evidence and strength of recommendation for each indication. The aim of this review is to provide a standard protocol for use of PRP in esthetics, for clinicians and academicians, leading to excellent results with this promising treatment modality.
Keywords: Biofiller, esthetics, lipofilling, periorbital rejuvenation, platelet-rich plasma, recommendations, skin rejuvenation
Introduction
The use of platelet-rich plasma (PRP) as a treatment modality for skin rejuvenation has been increasing rapidly over the past decade. Platelets become the logical choice for replacement and renewal of cells, tissues, or organs due to low invasiveness/high healing, easy availability, and abundance in growth factors. PRP is considered to be a growth factor cocktail, which promotes wound healing, angiogenesis, and tissue remodeling.
Studies have shown that PRP has around 578 different types of proteins like platelet-derived growth factor (PDGF), vascular endothelial growth factor (VEGF), and transforming growth factor beta (TGFβ).[1] These proteins and growth factors can stimulate stem cells and improve cellular proliferation, differentiation, and regeneration, hence, leading to skin rejuvenation and hyaluronic acid production [Table 1].
Table 1.
Role of growth factors
| Growth factor | Role |
|---|---|
| PDGF | Mitogen for fibroblasts and smooth muscle cells, promotes angiogenesis and collagen production |
| TGF-β | Increases collagen content |
| VEGF | Promotes angiogenesis |
| EGF | Promotes cell growth, differentiation, Angiogenesis, and collagen production |
| Pro and antiinflammatory cytokines (IL-4, IL-8, IL-13, IL-17) | Stimulate fibroblasts and collagen synthesis |
PRP can activate fibroblasts and synthesize collagen and other elements of the extracellular matrix and hence becomes an attractive option for skin rejuvenation and scar attenuation.[1,2,3,4] The use of PRP as monotherapy for skin rejuvenation, acne scars, periorbital rejuvenation, lipofilling, and in combination with fractional CO2 and other resurfacing modalities is increasing rapidly.
Scope of recommendations
Though the use of PRP as a modality for skin rejuvenation is increasing over the past decade, there is still no clarity about the licensed skin indications. A vast number of studies for various indications are available but good quality randomized controlled trials with consistent reporting of treatment parameters, use of adequate controls, and objective outcomes are lacking. Some classification systems have been proposed to improve comparison across studies but they have yet to be widely adopted.[5,6,7] In this article, we present a detailed review of literature and recommendations for approved skin indications with level of evidence.
Methodology of preparation of recommendations
A comprehensive literature search was done in the English language on the skin indications for PRP across multiple databases (PubMed, Embase, Medline, Google Scholar, and Cochrane). The search keywords used, alone or in combination, were “PRP” AND “Skin rejuvenation,” “Periorbital pigmentation,” “acne scarring,” “lipofilling,” “Fractional CO2 laser,” and “Dermaroller.” All studies having more than 10 patients were included in the current study. The key studies and their outcomes are mentioned in Tables 2-4.
Table 2.
PRP method of preparation of included studies
| Author | Study design | Sample size | Volume of blood drawn | PRP volume | Activator | Anticoagulant | Method of PRP preparation (any special features) |
|---|---|---|---|---|---|---|---|
| PRP monotherapy for facial rejuvenation | |||||||
| Sevilla et al.[8] | Single blind, split-face prospective, comparative cohort | 80 (1:20) (2:60) |
34 ml | 2.5 ml | nil | Acid citrate dextrose | Double spin 1): 150 g×15 min 2): 2700 rpm×10 min |
| Alam et al.[9] | Double-blind, split-face RCT | 19 | 20 ml | 3 ml | Nil | Acid citrate dextrose | Smart PREP2 APC (Harvest technologies) |
| Zenker[10] | Case series | 418 from Germany, Japan, UK, Israel | 10 ml | 4 ml | Nil | NA | Single centrifugation |
| PRP in combination with laser resurfacing | |||||||
| Hui et al.[11] | Single- blind split-face RCT | 13 | 30 ml | 2.2 ml | CaG | Heparin calcium | Double spin 1) 1200 rpm for 10 min 2) 3500 rpm for 5 min |
| Shin et al.[12] | Randomized controlled study, single-blind | 22 | 12 ml | 3 ml | CaCI2 | CPD- A | Double spin 3000 rpm/5 min |
| PRP in combination with lipofilling | |||||||
| Willemsen et al.[13] | Double-blind, RCT | 25 (1:13) (2:12) |
30 ml | 3 ml | Nil | Acid citrate dextrose | 3000 rpm/15 min |
| PRP in treatment of acne scarring | |||||||
| Chawla[14] | Case series | 30 | 10 ml | NA | Calcium gluconate | Acid citrate dextrose (ACD) | Double spin 1) 1500 rpm for 10 min 2) 3700 rpm for 10 min |
| Nofal et al.[15] | Randomized controlled trial | 45 | 10 ml | 2 ml | CaCI2 | NA | Double spin 1) 175 g for 10 min 2) 1750 g for 15 min |
| Babu et al.[16] | Case series | 20 | 10 ml | NA | NA | Acid citrate dextrose (ACD) | Two stage 1) 1500 rpm for 10 min 2) 3000 rpm for 20 min |
| PRP for infraorbital rejuvenation | |||||||
| Kang et al.[17] | Single blind Split-face RCT |
16 | 12 ml | 1 ml | CaCI2 | Acid citrate dextrose | My cells kit (Estar technology Ltd) |
| Mehryan et al.[18] | Case series | 10 | 10 ml | 1.5 ml | CaCI2 | Acid citrate dextrose | PRP kit (Kimia teb rahavard co) |
Table 4.
Outcome assessment of the included studies
| Author | Duration of follow-up | Assessment method | Results with PRP | Quantitative and Qualitative improvement | Adverse events |
|---|---|---|---|---|---|
| PRP monotheraphy for facial rejuvenation | |||||
| Sevilla et al.[8] | 52 weeks | Patients subjective satisfaction, GAIS assessment by two blinded dermatologists | Better improvement in global esthetic improvement scale in growth factor concentrate group compared to PRP group | Mean PRP vs Growth factor concentrate: GAIS 0.8 vs1.5 | NR |
| Alam et al.[9] | 24 weeks | Patient subjective satisfaction, patient evaluation of texture and wrinkles by 2 blinded dermatologists | Patient reported better improvement in texture and wrinkles with PRP when compared to control at 6 months | Patient assessment showed mean difference between PRP and control: texture: 0.79, wrinkles: 0.73 | Peeling and dryness, redness, edema, itching |
| Zenker[10] | 3,6,9,12, and 24 months following 1st injection | Comparing photographs before and after treatment | Patient’s subjective satisfaction was good with natural looking skin | PRP produced immediate, long lasting and volumetric result | No side effects reported |
| PRP in combination with laser resurfacing | |||||
| Hui et al.[11] | 12 weeks | Patient subjective assessment, photographic evaluation by 2 blinded dermatologists. Wrinkles, texture and pore size by VISIA | Patient subjective assessment showed greater improvement in wrinkles, texture and elasticity by VISIA in PRP + Laser group | Patient’s self-evaluation in PRP + laser group, Mean (SD) Wrinkles 2.3 (0.9) Texture 2.4 (0.8) |
Redness, swelling |
| Shin et al.[12] | One month after completion of treatment | photographs taken by blinded investigators, patients subjective satisfaction, skin biopsies | Good patient satisfaction and increased skin elasticity in the group subjected to PRP gel with fractional laser | erythema index was decreased in group subjected to PRP gel with fractional laser | Pain, redness, edema |
| PRP in combination with lipofilling | |||||
| Willemsen et al.[13] | 52 weeks | Photographic assessment by 2 blinded dermatologist, Elasticity by cutometer | Recovering time was significantly reduced in PRP with lipofilling group | NR | NR |
| PRP in treatment of acne scarring | |||||
| Chawla et al.[14] | 4,8,12,16 weeks | Physician assessment, patient subjective assessment | Good patient satisfaction and improved acne scars | Excellent response was seen in 18.5% of patients who received PRP according to physician assessment | Post inflam matory hyper pig mentation |
| Nofal et al.[15] | 2,4,6, weeks | Patient subjective assessment acne scarring grading system | Acne scars improved and good patient satisfaction in both injection and micro needling groups | Both groups showed significant statistical improvement in degree of acne scars post treatment (P<0.001) | No major adverse events |
| Babu et al.[16] | 4,8 weeks | Digital photographs, qualitative acne scaring grading system | Majority of the patients (70%) showed excellent response on subjective evaluation | Statistically significant difference (P=0.0312) was seen between the baseline and final score among the group who received PRP | No major Adverse events |
| PRP for infraorbital rejuvenation | |||||
| Kang et al.[17] | 12 weeks | Patient subjective assessment. Erythema index and melanin index by spectro photometer | Patient satisfaction was greater in PRP group when compared to PPP and saline control group EI and MI improved | 19% of patients showed good improvement in wrinkles, 25% of patients showed moderate improvement in skin tone with PRP | Pain, swelling, redness |
| Mehryan et al.[18] | 12 weeks | Degree of improvement by blinded dermatologists using photograph. Melanin index by mexameters. Hydration by corneometer | Improvement in infraorbital color homogeneity after treatment when compared to the baseline | Degree of improvement was fair to good in 80% of patients | Swelling, burning sensation. |
Table 3.
Treatment details of the included studies
| Author | Area treated | Type of intervention | Technique of PRP given | Number of PRP sessions |
|---|---|---|---|---|
| PRP monotheraphy for facial rejuvenation | ||||
| Sevilla et al.[8] | Naso labial fold | PRP monotherapy | First group was given growth factor concentrate intradermally on both sides. Second group was given growth factor concentrate intradermally on one side and intradermally PRP on the other side. | One |
| Alam et al.[9] | Cheeks | PRP monotherapy | One side of the face was given intradermal PRP. Other side of the face was given intradermal saline. | One |
| Zenker[10] | Full face and neck | PRP monotherapy | Linear threading fan like placements or cross hatching technique of intradermal PRP | 2 to 4 PRP injections depending on the age of patients |
| PRP in combination with laser resurfacing | ||||
| Hui et al.[11] | Full face | PRP combined with ultra-pulsed fractional CO2 laser therapy for facial rejuvenation | One side of face was given fractional CO2 laser with intradermal PRP. Other side was given fractional CO2 with saline | 3 sessions at 12 weeks interval |
| Shin et al.[12] | Full face | Platelet rich plasma get combined with fractional laser therapy or fractional laser treatment alone | PRP gel | 3 sessions of PRP after fractional laser 4 weeks apart |
| PRP in combination with lipofilling | ||||
| Willemsen et al.[13] | Full face | Intradermal PRP with lipofilling and saline | PRP was injected in lipofilling planes in middle of face and temporal regions | One |
| PRP in treatment of acne scarring | ||||
| Chawla[14] | Atrophic acne scars | Split-face comparative study of micro needling with PRP versus micro needling with vitamin C in treating atrophic post acne scars | In one half of the face, micro needling was followed by topical application of PRP | 4 sessions at 4 weeks interval |
| Nofal et al.[15] | Atrophic acne scars | PRP versus combined skin needling and PRP in the treatment of atrophic acne scars | One group was given intradermal injection of PRP. Other group was given combination of skin needling and PRP | 3 sessions at 2 weeks interval |
| Babu et al.[16] | Post acne scars | PRP verses fractional CO2 laser in the treatment of post acne scars | One group of patients were given intradermal PRP into each scar | 3 sessions at the interval of 1 month. |
| PRP for infraorbital rejuvenation | ||||
| Kang et al.[17] | Infraorbital rejuvenation | Infraorbital rejuvenation using PRP-A prospective study | One group was given intradermal PRP on one side and PPP on the other side of face. Second group was given intradermal PRP on one side and saline on the other side of face | 3 sessions at the interval of 4 weeks |
| Mehryan et al.[18] | Infraorbital and crow’s feet | Assessment of efficacy of PRP on infraorbital dark circles and crow’s feet wrinkles | Intradermal PRP was given (1 ml was injected into infraorbital region and 0.5 ml was injected into crow’s feet | Single session |
The grade of evidence and strength of recommendation were evaluated on the GRADE framework (Grading of Recommendation, Assessment, Development, and Evaluation).[19] The quality of evidence was graded on a four-point scale as follows.[20] This framework was used as this was found to be easy to comprehend.
High quality: Well performed randomized control trials or clear evidence from multiple well conducted observational studies showing very large effect.
Moderate quality: Randomized control trials with essential limitations.
Low quality: Observational studies or controlled trial with severe limitations
Very low quality: Nonsystematic observations, biologic reasoning, or observational studies with severe limitations
Strength of recommendation was determined based on the quality of evidence and other factors and was assigned as follows.[20]
Strong: A strong recommendation was given when benefits distinctly outweighed the risks for nearly all patients. As practitioners, most patients must receive this course of action.
Weak: A weak recommendation was given when risks and benefits were more closely balanced or were uncertain. As practitioners, patients must be explained about all the different options, and an option suitable for patients needs must be chosen.
Facial rejuvenation (I B quality of evidence and 1/2A strength of recommendation)
In today's world, the need for a firm, youthful skin is huge and is increasing by the day. The clinical signs of facial aging include wrinkles, open pores, pigmentation, and sagging. These are caused by changes in all layers of skin, loss of subcutaneous fat, downward migration of the fat pads, increased sebum and melanin production, and change in the bony structure. Skin aging is affected by a number of intrinsic and extrinsic factors. There are striking similarities between the events involved in wound healing and those that could effectively address the effects of intrinsic and extrinsic skin aging. It has been assumed that skin aging is analogous to a wound that is sufficiently extensive to overwhelm the skin's repair mechanisms, which becomes attenuated with age.[21]
PRP being an autologous mixture of growth factors scores highly among the treatment modalities offered to the patients. As skin ages, genetic and environmental factors lead to alterations in dermal extracellular matrix proteins (ECMP), degeneration of connective tissue, and decrease in the hyaluronic acid polymers. At a microscopic level, there is flattening of dermal-epidermal junction, dermal atrophy, and decrease in number of fibroblasts.[22] Activation of dermal fibroblasts and remodeling of the extracellular matrix are essential for rejuvenation of aged skin. Matrix metalloproteinase proteins are involved in the aging process by degradation of collagen and ECM proteins.[23]
Cytologically, PRP can regulate the secretion of biological factors and the proliferation and differentiation of many kinds of cells. PRP promotes collagen regeneration and angiogenesis, reduces pigment secretion, and further promotes facial rejuvenation.[24]
The antiaging effect of PRP has been found in animal studies as well. Cho et al.[25] observed 30 UV radiation exposed, nude mice and concluded that there were significantly fewer wrinkles in the nude mice injected with PRP than in the control groups. Also, significantly higher dermal thickness, fibroblast proliferation, and collagen synthesis were seen in the PRP group.
The utility of leucocytes in PRP for skin rejuvenation is debatable. The antiseptic role of leucocytes has been found to be useful in cases of wound healing. Leukocytes also help in angiogenesis and promote matrix production. The leukocyte population being proinflammatory, less amount of leucocytes in PRP reduces the incidence of inflammatory processes, hence gives better results in facial rejuvenation. Lin et al.[26] found that PRP poor in leukocytes provides objective improvements in skin bio stimulation. Also, RBC contamination is invariable in L-PRP which is not desirable in facial rejuvenation as this leads to the release of ROS and can affect platelet function by altering pH and promoting inflammation. Further studies on the specific cells and growth factors in PRP that contribute to facial rejuvenation would be required to assess the utility of leukocytes. On the basis of the current evidence, authors recommend P-PRP as the preferred type of PRP for facial rejuvenation.
PRP is been increasingly used for skin and neck rejuvenation.[27,28] Most of the studies have shown improvement in skin color and texture and better tissue tension which helps in decreasing wrinkle depth. Activated PRP has been shown to stimulate dermal fibroblast proliferation, and activated PPP has been reported to increase type I collagen. PRP has been reported to increase the dermal elasticity, hyaluronic acid synthesis, and collagen production leading to a smooth and tighter skin. By improving the skin moisturization, hyaluronic acid improves volume and skin turgor. Both, direct intradermal injections and topical PRP under occlusion have been tried. Much evidence for topical PRP under occlusion does not exist in literature.
The application of PRP monotherapy for rejuvenation of aging facial skin was evaluated in 518 patients across three studies.[8,9] Two studies performed single session,[8,9] whereas one study performed two to four sessions depending on the age of the patient.[10] The infraorbital area, nasolabial folds, and crow's feet areas were the most commonly injected; other areas of treatment included the forehead/malar region, the preauricular region, and the jaw region. All studies performed intradermal injections; in addition, Yuksel et al.[23] used a Dermaroller (Cynergy, Carson City, Nev.) and draped each patient's face in gauze soaked in platelet-poor plasma for 30 minutes. Follow-up periods ranged from 1 week to 1 year. Studies within this review confirmed PRP to be beneficial for rejuvenating aging facial skin. Results showed improvements in the volume, texture, and tone of facial skin and decrease both fine and deep wrinkles.
To evaluate the effect of multiple needle punctures during PRP, serial puncture PRP injections were compared to saline injections in 127 patients. PRP injections resulted in significantly greater improvements in skin texture, tone, wrinkles, and dermal collagen compared to saline though plain saline injections also lead to increase in dermal collagen and improvement in skin sallowness to some extent.
Standardized tools for standard recording of results have been developed. The FACE-Q is a validated tool for facial esthetic assessment, assessing patient reported outcomes and patient satisfaction. The five-point photo numeric Allergan Skin Roughness Scale was developed in accordance with U.S. Food and Drug Administration requirements to measure facial skin texture and is similar to the Wrinkle Severity Rating Scale.[29,30]
PRP appears to be safe, with a low-risk profile. The commonly reported side effects include pain during injections, erythema, edema, and bruising. A single case of blindness followed by PRP injection in glabellar region has been reported in literature.[31]
Studies have shown that as the age of the patient increases, the ability for tissue regeneration gradually declines, the expression of growth factor receptors decreases, and the ability of fibroblasts to produce collagen is reduced.[32] Vavken et al.[33] confirmed that young fibroblasts respond well to PRP treatment. Furthermore, as age increases, the tissue regeneration ability is poor and the expression of the cell growth factor receptor is reduced, resulting in poor PRP action.[34] At present, there are few reports of age-related changes in the response to PRP in facial rejuvenation. However, young fibroblasts respond well to PRP treatment, which may imply that the regenerative ability of PRP will decline with age. Hence, PRP might be a better modality in young patients.
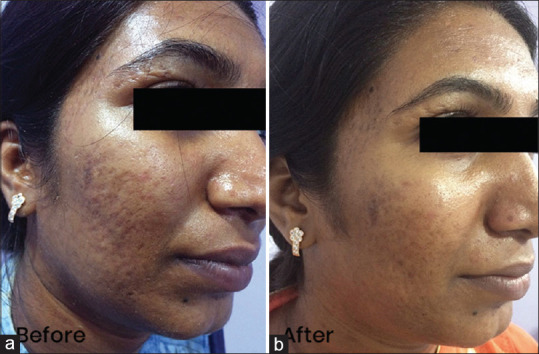
PRP is an excellent treatment modality with high safety profile for improving texture, tone, and early signs of aging in young patients [Figure 1a and b]. The absolute contraindications for PRP include platelet dysfunction syndrome, critical thrombocytopenia, hemodynamic instability, septicemia, and patients with unrealistic expectations. Relative contraindications include heavy smokers, drug or alcohol users, patients with chronic liver pathology, severe metabolic or systemic disorders, patients with cancer especially hematopoietic, patients having low hemoglobin (<10 g/ml) or platelet count (<1 lakh/microL), and patients having a history of recent fever or other illnesses. Also patients on regular use of NSAIDS, omnacortil more than 20 mg per day, and anticoagulant therapy should be avoided. A baseline hemoglobin, platelet count, HIV, HbsAg, and HCV should be done for all cases. In the current Covid era, a rapid antigen test for Covid-19 can be undertaken before the procedure. Patients having a history of herpes simplex can be started on antiviral prophylaxis; acyclovir 400 mg twice a day or valacyclovir 500 mg once a day for 5-7 days started a day before the procedure.
Figure 1.

(a) Open pores, uneven texture, tone. (b) Improvement in 4 weeks after 1 session
The entire procedure should be carried out in a minor OT maintaining strict asepsis. PRP is filled in insulin syringes with 31 G needle (PRP preparation is beyond the purview of this article). The local area can be anesthetized using topical anesthetic creams before, during, and after the procedure or nerve blocks. Intradermal or subdermal injections of PRP are given. Very superficial injections should be avoided as these can lead to cobblestone appearance on the skin. Around 3–4 ml is required for full face injections, 1 ml per cheek, 1 ml for forehead, nose, and chin, and 1 ml for neck. Around 0.01 ml–0.02 ml of PRP is delivered per prick. Slow injections are advocated to decrease the pain. PPP can be used with machines like electroporation which marginally increase the penetration of the fluid. Slight pain and redness are expected post procedure in all cases. Use of NSAIDS 2 weeks post procedure should be avoided. Patients are advised strict sun protection and liberal use of moisturizers for 2 weeks after the procedure. 3–6 sessions at a gap of 4–6 weeks are recommended. Results are usually visible after 4–6 weeks.
The effect of PRP in combination with CO2 laser in skin rejuvenation has been evaluated in a number of studies with beneficial effect. Shin et al.[12] conducted a study on 22 Korean women, of which half of the cases were treated with the laser alone and the rest with laser combined with PRP. The results showed that women treated with PRP and laser were more satisfied with the treatment effect, their skin elasticity was better, and the skin erythema index was lower than that of the women treated with the laser alone. PRP increased the length of the junction between the epidermis and the dermis, the content of collagen, and the number of fibroblasts. Hui et al.[11] found that patient reported better improvement in wrinkles, texture, and elasticity when CO2 laser was combined with PRP compared to PRP alone. Study done by Willemsen et al.[13] concluded that recovery time was significantly reduced in PRP assisted with lipofilling.
The effectiveness of PRP in improving facial skin has a I B quality of evidence and 1/2A strength of recommendation and is recommended by ID PRP for temporary, modest improvement of overall appearance, texture, and wrinkles in aged facial skin. Effectiveness of PRP in improving appearance of perioral skin has a II A quality of evidence, 2B strength of recommendation. PRP basically has a low-quality evidence for modest, temporary improvement of NLF wrinkle severity.[35,36] Effectiveness of PRP in improving appearance of forehead skin has level III quality of evidence and 2 B strength of recommendation. Hence, more good quality randomized trials are needed.
Acne scarring
A number of treatment modalities of proven efficacy including peels, derma rollers, MNRF, fractional CO2 laser, and fillers are being used extensively for treatment of acne scars. The use of PRP for acne scars was first observed by Redaelli et al.,[37] who had also used intradermal injections of PRP for facial skin rejuvenation. Leukocytes have a favorable role in scar healing; hence, L-PRP is the preferred type of PRP for acne scars.
PRP can be used alone or in combination with the conventional treatment modalities like subcision, dermaroller, or laser resurfacing procedures, to increase the efficacy of these treatments.[38] PRP improves and accelerates post-treatment recovery when combined with fractional CO2 laser.[39,40]
PRP monotherapy
PRP reconstitutes an atrophic acne scar through various growth factors which promote connective tissue regeneration by up regulating collagen and protein production. Histologic studies following PRP administration have revealed that there is an increased collagen bundles formation and a thicker epidermal layer compared to control.[41]
A randomized study was conducted by Pooja et al.[42] wherein authors compared the efficacy of fractional CO2 monotherapy, micro needling monotherapy, and PRP intradermal injection monotherapy in post acne scarring. It was concluded that CO2 and micro needling monotherapy was significantly more efficacious than PRP monotherapy. The utility of PRP as a monotherapy for acne scars is still debatable.
PRP in combination with micro needling
Both topical and intradermal PRP have been safely combined with micro needling producing variable results.[43]
1) Topical PRP in combination with micro needling
The beneficial effect of topical PRP in combination with micro needling is still debatable. A decreased healing time has been observed in majority of the studies but statically significant difference in results due to addition of topical PRP has not been consistently seen. A split-face trial of 35 patients compared micro needling with and without topical PRP.[44] Both side of the face showed a significant improvement of acne scars, as rated by Goodman's Qualitative scoring system. Although the PRP-treated side showed greater improvement, this difference was not determined to be statistically significant. The addition of PRP did, however, appear to reduce erythema and edema.[44]
A randomized split-face trial evaluated micro needling alone or in combination with either topical PRP or trichloroacetic acid (TCA) 15% peels.[45] Both combination treatments showed significant cosmetic improvement in acne scars compared to micro needling alone. Assessment was done by blinded dermatologists and independent observers. No significant difference was observed between the combination treatments. On histology, both combination treatments produced a thicker epidermis than micro needling alone. All groups showed more organized and dense collagen bundles following treatment, but this was more pronounced in the topical PRP group.[45]
2) Intradermal PRP in combination micro needling
Micro needling along with PRP has a synergistic action. This combination would intensify the natural wound healing cascade because of high concentration of patients own growth factors induced by skin needling and PRP. This enhanced wound healing response thereby improves the acne scars.
A recent randomized trial for the treatment of scars included 90 patients separated into three treatment groups.[46] One group received micro needling, another group received intradermal PRP, and the third group was treated with alternating micro needling and intradermal PRP treatments. Though improvement was seen in all groups, combination treatment was associated with the greatest mean improvement score, followed by micro needling, then PRP. Patient satisfaction was significantly greater in the combination group. On histology, the combination treatment yielded a thickened epidermis with more developed rete ridges compared to the single treatment modalities.[46]
Chawla[14] and Nofal et al.[15] confirmed the improvement in atrophic acne scars when PRP was applied by means of either micro needling or intradermal injection.
A recent split-face study concluded that the combination of both intradermal injections and micro needling with PRP improved the clinical outcomes when compared to micro needling with distilled water.[47] A 50-patient split-face study evaluated micro needling for acne scars with and without the addition of PRP: Post micro needling, intradermal PRP was injected within acne scars and topical PRP was subsequently spread over the same half and distilled water was used on the other half. Though improvement was seen on both sides, the PRP-treated side scored a higher response using Goodman's Qualitative and Quantitative scoring systems and independent physician assessment scores. Patient satisfaction was also greater, and majority of the patients reported that PRP led to a reduction in the visibility of acne scars and an improvement in skin roughness.[47]
A comparative study was done by Porwal et al.,[48] wherein derma roller alone was used on one side and intradermal injections of PRP with derma roller on other side of the face with acne scars. Authors observed significantly better results on PRP side (58% vs 43%).
The above studies clearly highlight that topical PRP has limited efficacy; hence, intradermal PRP should be the preferred mode of PRP delivery. Interstitial fluid and fibrin fill up the open channels post micro needling or AFR very fast, hence, limiting the uptake of PRP; therefore, topical PRP has very limited efficacy.
PRP in combination with other treatment modalities for acne scars
PRP has been used with a number of routinely done procedures like fractional CO2 laser and autologous fat grafting. Studies have shown encouraging results with decrease in healing time and improved patient satisfaction rate.
PRP combined with Fractional CO2 Laser (PRP in combination with laser resurfacing for minimization of laser associated downtime has a 1B quality of evidence and ½ A strength of recommendation.)
The beneficial effect of combination with PRP with ablative lasers like fractional CO2 has been established in a number of studies. Both topical PRP and intradermal PRP have been studied.
Combination topical PRP with laser has been associated with decreased erythema, swelling, and pain though significant improvement in the final results has not been seen. It is suggested that topical PRP could be used to improve both post-procedural downtime and patient satisfaction when used with ablative fractional laser (AFL).[40]
Intradermal PRP has also been tested with ablative laser procedures in a number of studies. Lee et al.[40] conducted a study on fourteen patients to examine the effects of PRP after treating acne scars with an ablative fractional resurfacing laser (AFR). Split-face trial with two treatments of AFR combined with PRP injections on one side and saline injections on the other was carried out. Compared to saline, PRP treatment was associated with less erythema by Day 4 and decreased duration of erythema. Likewise, after the second treatment, less edema for decreased duration was noted. The authors concluded that PRP hastened recovery of laser-induced injury.
A split-face study by Faghihi et al.[49] evaluated AFR combined with either intradermal PRP or saline in 16 patients found conflicting results. Although atrophic acne scars improved with intradermal PRP compared to control, this difference was not statistically significant at 1 month after the first treatment or 4 months after the second treatment. Unlike other studies, participants experienced more edema and prolonged erythema on the side treated with PRP. The authors concluded that the addition of PRP resulted in worse side effects with longer downtime.[49]
Gawdat et al.[50] conducted a 30-patient split-face study to compare intradermal and topical PRP modalities. One group was subjected to AFR with either intradermal PRP or saline to each side, while the other group received AFR with either intradermal or topical PRP to each side. Combined treatment with AFR and PRP showed better response, shorter downtime, and fewer side effects than laser therapy alone. There were no statistical differences between intradermal and topical PRP with regards to the degree of response and downtime. Topical PRP was associated with lower pain scores compared to intradermal administration. Interestingly, the efficacy of PRP was not compromised by using the less painful topical administration.[50]
In our study on 20 patients, we observed that both PRP and CO2 laser produced statistically significant improvement in the qualitative scoring of acne scars.[16] PRP combined with subcision gives good results [Figure 2a and b]. Both the modalities are effective in treating acne scars with good safety profile. The principle points of interest of PRP are that it prohibits the treatment dismissal. It also avoids transmissible contamination as it is an autologous product and it is a cost-effective treatment.[51,52]
Figure 2.
(a) Acne scars grade 2. (b) Improvement after 1 month of 2 sessions
It is recommended as a adjuvant treatment to fractional laser to decrease duration and intensity of laser associated side effects especially edema and erythema.
2 PRP combined with autologous fat grafting
During fat injection, the period of ischemia is produced, which makes the adipose cells susceptible to necrosis. The proangiogenic activity of PRP may play a critical role in improving the fat graft retention at this stage. The addition of PRP to fat grafting procedures maintained facial volume.[53]
Azzam et al.[54] conducted a comparative study in 28 patients to evaluate the PRP enhanced fat grafting versus fat grafting alone in the treatment of post acne scars. It was concluded that overall improvement in the individual scars was better in PRP enriched fat graft. Autologous fat grafting had advantage of single-session therapy, with minimal downtime and long-lasting results during follow-up period.
Periorbital Rejuvenation (The current quality of evidence is I b and the strength of recommendation is 2 A)
Although periorbital aging is a condition of cosmetic concern, it is usually the first sign of aging and can cause immense psychological distress. All available minimally invasive treatment options have limitations. PRP can be used to treat esthetic problems in the periorbital regions like wrinkles, pigmentation, erythema, xerosis, loss of skin elasticity, and volume. Inspite of the number of treatment options available ranging from topicals to resurfacing lasers, PRP is emerging as a promising treatment for this difficult to treat condition.[55]
Skin fibroblasts in PRP have been found to secrete endogenous hyaluronic acid in high concentration leading to a significant improvement in skin quality and decrease in the signs of skin aging.[54,55] Hyaluronic acid, being hygroscopic leads to improvement in skin turgor and volume. The decrease in production of melanin is attributed to the presence of TGF β. PRP leads to increased collagen production by inducing mild inflammation leading to an improvement in the tear trough deformity. Theoretically PRP has an effect similar to injection of hyaluronic acid fillers with the added effect on pigmentation as well.
A statistically significant reduction in the severity of wrinkles, assessed using Wrinkle severity rating scale, was found in a study conducted in 20 patients. The response was found to be better in patients younger than 40 years of age.[36] Kang et al.[17] reported improvement in both infraorbital wrinkles and skin tone in subjective and objective satisfaction scales in 20 Korean females. Three sessions were done at 1-month interval each. A decrease in the erythema index and melanin index was seen in the PRP-treated side. A significant improvement in dark circles has been reported after the third session of monthly PRP sessions in a trial conducted in Jordan on 50 patients. The improvement lasted through a follow-up of 6 months.[56] After a single injection of PRP statistically significant improvement has been reported in infraorbital color homogeneity, but statistically significant changes in melanin content, stratum corneum hydration, wrinkle volume, and visibility index were not seen.[18] Skin elasticity and skin firmness of lower eyelid showed a statistically significant improvement after three monthly injections of PRP.[57] 2 sessions of PRP at 3 months interval have been found to have improvements in periorbital wrinkles and dyschromia in a case series of 30 patients.[58]
PRP does improve the skin texture, decrease the pigmentation, and reduce the appearance of tear trough after 3 sessions done at monthly intervals [Figure 3a and b]. This area is especially prone to bruising; hence, the patient should be aligned before the procedure for the same. Topical PRP is a modality worth investigating for use in this area. Also, better results are seen in younger patients. The above studies indicate some efficacy of PRP in periorbital rejuvenation, but more data is needed to assess the longevity of the effect. As repeatedly shown, PRP decreases the healing time and enhances the healing overall when combined with other resurfacing modalities. PRP as a monotherapy and in combination with other treatments hold promise for periorbital rejuvenation.
Figure 3.

(a) Loss of volume, tone of periorbital area. (b) Improvement seen, 1 month after 3 monthly sessions
The best response was observed after three monthly injections and that is being recommended. The evidence discussed in this article indicates the increasing importance of minimally invasive modalities in periorbital rejuvenation and a promising role for PRP as solo therapy or in multimodality regimens.
Melasma
The role of intradermal PRP in treatment of melasma is under evaluation currently. Intradermal PRP is being tried as an alternative or adjuvant therapy for melasma. Very few studies have been conducted.
Hofny et al.[59] conducted a split-face study on 23 adult Egyptian melasma patients. PRP was delivered through micro needling with derma pen on one side of face and intradermal microinjections of PRP using mesoneedles on other side of face. A statistically significant decrease in the hemi-MASI score was observed on each side of face following PRP treatment.
A split-face, randomized, single-blinded pilot study was done by Sirithanabadeekul et al.[60] on ten female mixed-type of melasma patients. Intradermal PRP was injected on one side of face and normal saline on other side every 2 weeks for 4 sessions. It was observed that mMASI score and Antera 3 D assessed melanin level showed significant improvement in PRP treated side compared to control side.
Platelet poor plasma biofiller in esthetics
Tissue loss following inflammation and volume loss in the face due to aging are common, yet difficult to treat conditions. Punched out scars like post varicella scars respond poorly to subcision also.[61] Dermal fillers are quite effective in restoring volume loss in these conditions; however, the cost of fillers have always been prohibitive. An innovative new solution to this problem is the use of platelet-poor plasma (PPP) biofiller. PPP, which is normally discarded during the preparation of PRP, is a good source of plasma proteins. These plasma proteins can be coagulated using heat to form a gel-like substance which can be injected in the skin to provide a lift. Dental syringe is used to prepare this biofiller. PPP is filled in glass vial of dental syringe. Glass vial is kept in water bath at 80°C–90°C. Transparent plasma turns opaque. Glass vial is inserted in the dental syringe and 27 G needle is attached[61] [Figure 4a-f].
Figure 4.
(a) Vial for dental syringe is filled with PPP. (b) Vial kept in water bowl at 70°C –80°C. (c) Dental syringe, 27G needles. (d) Biofiller in vials. (e) Vial loaded in the dental syringe. (f) Gel-like consistency
Woo et al.[62] performed an animal study using rats. They injected biofiller in the dorsal surface of the skin of the rats and measured the swelling over 6 months. They found that swelling slowly reduced and disappeared 6 months following the procedure. They also performed a histopathological examination of the biofiller. They did not report any chronic inflammatory infiltrate or foreign body like reaction around the amorphous eosinophilic substance during the period of study duration.
Dashore and Dashore[63] performed biofiller injections in chickenpox scars and found that the biofiller started to disappear and filler volume reduction started to appear by the end of 1 month and the treatment had to be repeated every 3 to 4 months although the filler took nearly 6 months to completely disappear.
Neinaa et al.[64] performed a comparative study between PPP biofiller injection vs PRP injection for infraorbital rejuvenation. This was a split-face study where three injections 2 weeks apart of PRP were given while only single injection of biofiller was performed. Both groups showed significant improvement in tear trough reduction and hyperpigmentation reduction; however, biofiller injection was found to be significantly more effective than PRP on both the parameters. They found the results of biofiller injections to persist up to the end of the study, which was of 3 months duration.
Doghaim et al.[65] performed biofiller injections in various facial wrinkles and tear trough deformities in 52 women in an pre-post study. They found significant improvement in all the facial wrinkles and found the results to be maintained up to 3 months. Main adverse effects seen were transient erythema and edema, which disappeared after few hours. Bruising was also seen predominantly following tear trough injections, which disappeared within a few days. No major long-term adverse effects were seen.
At present, PPP biofiller injection for facial rejuvenation is in its nascent stages and needs further evidence to understand the long-term properties of this product. It is a cost-effective option which can be easily repeated over a few months and is found to be especially effective for superficial volume defects like chicken pox scars [Figure 5a and b].
Figure 5.

(a) Varioliform Scar pretreatment. (b) Scar filled
Limitations
No doubt, PRP is showing promising results in a number of skin conditions but there is an urgent need for large, randomized, controlled trials. Majority studies have small numbers, lack of uniform criteria for preparation protocols and comparison of outcomes, and small follow-up periods. Inspite of the number of studies, the importance of different parameters on the clinical efficacy of PRP in esthetic medicine is not known. Lack of PRP standardization is the main problem with assessing its efficacy between studies. Another major limitation is inadequacy and variability in outcomes assessment. Further studies are needed to determine optimal methods and procedures for collection, treatment, and administration of PRP.
Future research
Future studies are required to determine which aging-specific features (e.g., texture versus color) are most responsive to treatment with PRP and which patient characteristics (e.g., age, gender, ethnicity, history of sun exposure, smoking) best predict a favorable response to treatment. The optimal number of treatments and intervals between them also need to be elucidated. Quantification of fundamental PRP parameters and growth factor concentrations, long-term (≥ 6 months) outcomes, blinded rater assessments, and other specific agreed-upon (i.e., core) standardized outcomes are needed. Uniform outcome reporting across studies would enable pooling of data and more detailed analysis.
IADVL Consensus Statement
P-PRP is the preferred type of PRP for facial rejuvenation while L-PRP is preferred for acne scars.
Moderate level of evidence is available in literature for PRP as a treatment modality for skin rejuvenation, acne scars, periorbital rejuvenation, lipofilling and as a combination therapy with ablative services like Fractional CO2 laser and dermarollers.
Young patients with early signs of aging and those seeking an improvement in texture and tone by a natural, autologous treatment are the ideal patients.
PRP showed an improvement in all types of acne scars in terms of reduction in acne scar size. On visual analogue scale, rolling scars responded better to PRP as compared to boxcar and ice-pick scars.
PRP when combined with needling and subcision can be an effective treatment for even severe atrophic acne scars.
PRP in authors experience is an excellent modality for temporary, modest improvement of periorbital area in terms of texture, pigmentation, and superficial wrinkles.
Addition of PRP to AFR significantly decreases the healing time, hence decreasing the chances of post inflammatory hyperpigmentation and increasing the patient satisfaction.
Bio-filler could prove to be a very cost-effective modality for treating superficial volume defects; further research is needed to establish the longevity and safety of this modality.
Intradermal PRP is the preferred mode to deliver PRP in all cases, as of today.
3–6 sessions at monthly interval are recommended. Results are expected only after 4–6 weeks of treatment.
Topical anesthesia, nerve blocks, icing, and vibrators can be used to make the procedure comfortable for the patient.
The safety of the procedure has been established but the longevity of results is still questionable.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Garcia BA, Smalley DM, Cho H, Shabanowitz J, Ley K, Hunt DF. The platelet microparticle proteome. J Proteome Res. 2005;4:1516–21. doi: 10.1021/pr0500760. [DOI] [PubMed] [Google Scholar]
- 2.Browning SR, Weiser AM, Woolf N, Golish SR, SanGiovanni TP, Scuderi GJ, et al. Platelet-rich plasma increases matrix metalloproteinases in cultures of human synovial fibroblasts. J Bone Joint Surg Am. 2012;94:1721–7. doi: 10.2106/JBJS.K.01501. [DOI] [PubMed] [Google Scholar]
- 3.Cho HS, Song IH, Park S-Y, Sung MC, Ahn M-W, Song KE. Individual variation in growth factor concentrations in platelet-rich plasma and its influence on human mesenchymal stem cells. Korean J Lab Med. 2011;31:212–8. doi: 10.3343/kjlm.2011.31.3.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alsousou J, Thompson M, Hulley P, Noble A, Willett K. The biology of platelet-rich plasma and its application in trauma and orthopaedic surgery: A review of the literature. J Bone Joint Surg Br. 2009;91:987–96. doi: 10.1302/0301-620X.91B8.22546. [DOI] [PubMed] [Google Scholar]
- 5.Mautner K, Malanga GA, Smith J, Shiple B, Ibrahim V, Sampson S, et al. A call for a standard classification system for future biologic research: The rationale for new PRP nomenclature. PM R. 2015;7:S53–9. doi: 10.1016/j.pmrj.2015.02.005. [DOI] [PubMed] [Google Scholar]
- 6.Arshdeep, Kumaran MS. Platelet-rich plasma in dermatology: Boon or a bane? Indian J Dermatol Venereol Leprol. 2014;80:5–14. doi: 10.4103/0378-6323.125467. [DOI] [PubMed] [Google Scholar]
- 7.Magalon J, Chateau AL, Bertrand B, Louis ML, Silvestre A, Giraudo L, et al. DEPA classification: A proposal for standardising PRP use and a retrospective application of available devices. BMJ Open Sport Exerc Med. 2016;2:e000060. doi: 10.1136/bmjsem-2015-000060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sevilla GP, Dhurat RS, Shetty G, Kadam PP, Totey SM. Safety and efficacy of growth factor concentrate in the treatment of nasolabial fold correction: Split face pilot study. Indian J Dermatol. 2015;60:520. doi: 10.4103/0019-5154.159628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alam M, Hughart R, Champlain A, Geisler A, Paghdal K, Whiting D, et al. Effect of platelet-rich plasma injection for rejuvenation of photoaged facial skin: A randomized clinical trial. JAMA Dermatol. 2018;154:1447–52. doi: 10.1001/jamadermatol.2018.3977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zenker S. Platelet rich plasma (PRP) for facial rejuvenation. J Med Esth Chir Derm. 2010;XXXVII:179–83. [Google Scholar]
- 11.Hui Q, Chang P, Guo B, Zhang Y, Tao K. The clinical efficacy of autologous platelet-rich plasma combined with ultra-pulsed fractional CO2 laser therapy for facial rejuvenation. Rejuvenation Res. 2017;20:25–31. doi: 10.1089/rej.2016.1823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shin MK, Lee JH, Lee SJ, Kim NI. Platelet-rich plasma combined with fractional laser therapy for skin rejuvenation. Dermatol Surg. 2012;38:623–30. doi: 10.1111/j.1524-4725.2011.02280.x. [DOI] [PubMed] [Google Scholar]
- 13.Willemsen JC, Van Dongen J, Spiekman M, Vermeulen KM, Harmsen MC, van der Lei B, et al. The addition of platelet-rich plasma to facial lipofilling: A double-blind, placebo-controlled, randomized trial. Plast Reconstr Surg. 2018;141:331–43. doi: 10.1097/PRS.0000000000004081. [DOI] [PubMed] [Google Scholar]
- 14.Chawla S. Split face comparative study of microneedling with PRP versus microneedling with vitamin C in treating atrophic post acne scars. J Cutan Aesthet Surg. 2014;7:209–12. doi: 10.4103/0974-2077.150742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nofal E, Helmy A, Nofal A, Alakad R, Nasr M. Platelet-rich plasma versus CROSS technique with 100% trichloroacetic acid versus combined skin needling and platelet rich plasma in the treatment of atrophic acne scars: A comparative study. Dermatol Surg. 2014;40:864–73. doi: 10.1111/dsu.0000000000000091. [DOI] [PubMed] [Google Scholar]
- 16.Babu AM, Shetty VH, Goel S, Eram H. A comparative study of efficacy and safety of platelet rich plasma versus fractional CO2 laser in the treatment of post acne scars. Int J Res Dermatol. 2019;5:254–8. [Google Scholar]
- 17.Kang BK, Shin MK, Lee JH, Kim NI. Effects of platelet-rich plasma on wrinkles and skin tone in Asian lower eyelid skin: Preliminary results from a prospective, randomised, split-face trial. Eur J Dermatol. 2014;24:100–1. doi: 10.1684/ejd.2014.2267. [DOI] [PubMed] [Google Scholar]
- 18.Mehryan P, Zartab H, Rajani A, Pazhoohi N, Firooz A. Assessment of efficacy of platelet rich plasma (PRP) on infraorbital dark circles and crow's feet wrinkles. J Cosmet Dermatol. 2014;13:72–8. doi: 10.1111/jocd.12072. [DOI] [PubMed] [Google Scholar]
- 19.Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guyatt GH, Oxman AD, Kunz R, Falck-Ytter Y, Vist GE, Liberati A, et al. Going from evidence to recommendations. BMJ. 2008;336:1049–51. doi: 10.1136/bmj.39493.646875.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sundaram H, Mehta RC, Norine JA, Kircik L, Cook-Bolden FE, Atkin DH, et al. Topically applied physiologically balanced growth factors: A new paradigm of skin rejuvenation. J Drugs Dermatol. 2009;8((5 Suppl Skin Rejuenation)):4–13. [PubMed] [Google Scholar]
- 22.Abuaf OK, Yildiz H, Baloglu H, Bilgili ME, Simsek HA, Dogan B. Histologic evidence of new collagen formulation using platelet rich plasma in skin rejuvenation: A prospective controlled clinical study. Ann Dermatol. 2016;28:718–24. doi: 10.5021/ad.2016.28.6.718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yuksel EP, Sahin G, Aydin F, Senturk N, Turanli AY. Evaluation of effects of platelet-rich plasma on human facial skin. J Cosmet Laser Ther Off Publ Eur Soc Laser Dermatol. 2014;16:206–8. doi: 10.3109/14764172.2014.949274. [DOI] [PubMed] [Google Scholar]
- 24.Lei X, Xu P, Cheng B. Problems and solutions for platelet-rich plasma in facial rejuvenation: A systematic review. Aesthetic Plast Surg. 2019;43:457–69. doi: 10.1007/s00266-018-1256-1. [DOI] [PubMed] [Google Scholar]
- 25.Cho JM, Lee YH, Baek R-M, Lee SW. Effect of platelet-rich plasma on ultraviolet b-induced skin wrinkles in nude mice. J Plast Reconstr Aesthetic Surg. 2011;64:31–9. doi: 10.1016/j.bjps.2010.08.014. [DOI] [PubMed] [Google Scholar]
- 26.Lin J, Sclafani AP. Platelet-rich plasma for skin rejuvenation and tissue fill. Facial Plast Surg Clin N Am. 2018;26:439–46. doi: 10.1016/j.fsc.2018.06.005. [DOI] [PubMed] [Google Scholar]
- 27.Elghblawi E. Platelet-rich plasma, the ultimate secret for youthful skin elixir and hair growth triggering. J Cosmet Dermatol. 2018;17:423–30. doi: 10.1111/jocd.12404. [DOI] [PubMed] [Google Scholar]
- 28.Peng GL. Platelet-rich plasma for skin rejuvenation: Facts, fiction, and pearls for practice. Facial Plast Surg Clin N Am. 2019;27:405–11. doi: 10.1016/j.fsc.2019.04.006. [DOI] [PubMed] [Google Scholar]
- 29.Donofrio L, Carruthers A, Hardas B, Murphy DK, Carruthers J, Jones D, et al. Development and validation of a photonumeric scale for evaluation of facial skin texture. Dermatol Surg. 2016;42((Suppl 1)):S219–26. doi: 10.1097/DSS.0000000000000852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Day DJ, Littler CM, Swift RW, Gottlieb S. The wrinkle severity rating scale: A validation study. Am J Clin Dermatol. 2004;5:49–52. doi: 10.2165/00128071-200405010-00007. [DOI] [PubMed] [Google Scholar]
- 31.Kalyam K, Kavoussi SC, Ehrlich M, Teng CC, Chadha N, Khodadadeh S, et al. Irreversible blindness following periocular autologous platelet-rich plasma skin rejuvenation treatment. Ophthal Plast Reconstr Surg. 2017;33((3S Suppl 1)):S12–6. doi: 10.1097/IOP.0000000000000680. [DOI] [PubMed] [Google Scholar]
- 32.Goldstein S, Harley CB. in vitro studies of age-associated diseases. Fed Proc. 1979;38:1862–7. [PubMed] [Google Scholar]
- 33.Vavken P, Saad FA, Murray MM. Age dependence of expression of growth factor receptors in porcine ACL fibroblasts. J Orthop Res. 2010;28:1107–12. doi: 10.1002/jor.21111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mori Y, Hatamochi A, Arakawa M, Ueki H. Reduced expression of mRNA for transforming growth factor beta (TGF beta) and TGF beta receptors I and II and decreased TGF beta binding to the receptors in in vitro-aged fibroblasts. Arch Dermatol Res. 1998;290:158–62. doi: 10.1007/s004030050282. [DOI] [PubMed] [Google Scholar]
- 35.Maisel-Campbell AL, Ismail A, Reynolds KA, Poon E, Serrano L, Grushchak S, et al. A systematic review of the safety and effectiveness of platelet-rich plasma (PRP) for skin aging. Arch Dermatol Res. 2020;312:301–15. doi: 10.1007/s00403-019-01999-6. [DOI] [PubMed] [Google Scholar]
- 36.Elnehrawy NY, Ibrahim ZA, Eltoukhy AM, Nagy HM. Assessment of the efficacy and safety of single platelet-rich plasma injection on different types and grades of facial wrinkles. J Cosmet Dermatol. 2017;16:103–11. doi: 10.1111/jocd.12258. [DOI] [PubMed] [Google Scholar]
- 37.Redaelli A, Romano D, Marciano A. Face and neck revitalization with platelet rich plasma (PRP): Clinical outcome in a series of 23 consecutively treated patients. J Drugs Dermatol. 2010;9:466–72. [PubMed] [Google Scholar]
- 38.Oh IY, Kim BJ, Kim MN. Depressed facial scars successfully treated with autologous platelet-rich plasma and light-emitting diode phototherapy at 830 nm. Ann Dermatol. 2014;26:417–8. doi: 10.5021/ad.2014.26.3.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kar BR, Raj C. Fractional CO2 laser vs fractional CO2 with topical platelet rich plasma in the treatment of acne scars: A split face comparison trial. J Cutan Aesthet Surg. 2017;10:136–44. doi: 10.4103/JCAS.JCAS_99_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee JW, Kim BJ, Kim MN, Mun SK. The efficacy of autologous platelet rich plasma combined with ablative carbon dioxide fractional resurfacing for acne scars: A simultaneous split face trial. Dermatol Surg. 2011;26:931–8. doi: 10.1111/j.1524-4725.2011.01999.x. [DOI] [PubMed] [Google Scholar]
- 41.Na JI, Choi JW, Choi HR, Jeong JB, Park KC, Youn SW, et al. Rapid healing and reduced erythema after ablative fractional carbon dioxide laser resurfacing combined with the application of autologous platelet-rich plasma. Dermatol Surg. 2011;37:463–8. doi: 10.1111/j.1524-4725.2011.01916.x. [DOI] [PubMed] [Google Scholar]
- 42.Pooja T, Gopal KV, Rao TN, Devi BG, Kumar SA. A randomized study to evaluate the efficacy fractional CO2 laser, microneedling and platelet rich plasma in post-acne scarring. Indian Dermatol Online J. 2020;11:349–54. doi: 10.4103/idoj.IDOJ_370_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Badran KW, Nabili V. Lasers, microneedling and platelet rich plasma for skin rejuvenation and repair. Facial PlastSurg Clin North Am. 2018;26:455–68. doi: 10.1016/j.fsc.2018.06.007. [DOI] [PubMed] [Google Scholar]
- 44.Ibrahim MK, Ibrahim SM, Salem AM. Skin microneedling plus platelet rich plasma versus skin microneedling alone in the treatment of atrophic post acne scars: A split face comparative study. J Dermatolog Treat. 2018;29:281–6. doi: 10.1080/09546634.2017.1365111. [DOI] [PubMed] [Google Scholar]
- 45.EL-Domyati M, Abdel-Wahab H, Hossam A. Microneedling combined with platelet rich plasma or trichloroacetic acid peeling for management of acne scarring: A split face clinical and histologic comparison. J Cosmet Dermatol. 2018;17:73–83. doi: 10.1111/jocd.12459. [DOI] [PubMed] [Google Scholar]
- 46.Ibrahim ZA, EL-Ashmawy AA, Shora OA. Therapeutic effect of microneedling and autologous platelet rich plasma in the treatment of acne scars: A randomized study. J Cosmet Dermatol. 2017;16:388–99. doi: 10.1111/jocd.12356. [DOI] [PubMed] [Google Scholar]
- 47.Asif M, Kanodia S, Singh K. Combined autologous platelet rich plasma with microneedling with distilled water in the treatment of atrophic acne scars: A concurrent split face study. J Cosmet Dermatol. 2016;15:434–43. doi: 10.1111/jocd.12207. [DOI] [PubMed] [Google Scholar]
- 48.Porwal S, Chahar YS, Singh PK. A comparative study of combined dermaroller and platelet-rich plasma versus dermaroller alone in acne scars and assessment of quality of life before and after treatment. Indian J Dermatol. 2018;63:403–8. doi: 10.4103/ijd.IJD_118_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Faghihi G, Keyvan S, Asilian A, Nouraei S, Behfar S, Nilforoushzadeh MA. Efficacy of autologous platelet-rich plasma combined with fractional ablative carbon dioxide resurfacing laser in treatment of facial atrophic acne scars: A split-face randomized clinical trial. Indian J Dermatol Venereol Leprol. 2016;82:162–8. doi: 10.4103/0378-6323.174378. [DOI] [PubMed] [Google Scholar]
- 50.Gawdat HI, Hegazy RA, Fawzy MM, Fathy M. Autologous platelet rich plasma: Topical versus intradermal after fractional ablative carbon dioxide laser treatment of atrophic acne scars. Dermatol Surg. 2014;40:152–61. doi: 10.1111/dsu.12392. [DOI] [PubMed] [Google Scholar]
- 51.Rivera AE. Acne scarring: A review and current treatment modalities. J Am Acad Dermatol. 2008;59:659–76. doi: 10.1016/j.jaad.2008.05.029. [DOI] [PubMed] [Google Scholar]
- 52.Langer C, Mahajan V. Platelet rich plasma in dermatology. JK Sci. 2014;16:147–50. [Google Scholar]
- 53.Rophael JA, Craft RO, Palmer JA, Hussey AJ, Thomas GP, Morrison WA, et al. Angiogenic growth factor synergism in a murine tissue engineering model of angiogenesis and adipogenesis. Am J Pathol. 2007;171:2048–57. doi: 10.2353/ajpath.2007.070066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Azzam OA, Atta AT, Sobhi RM, Mostafa PI. Fractional CO(2) laser treatment vs autologous fat transfer in the treatment of acne scars: A comparative study. J Drugs Dermatol. 2013;12:e7–13. [PubMed] [Google Scholar]
- 55.Kassir M, Kroumpouzos G, Puja P, Katsambas A, Galadari H, Lotti T, et al. Update in minimally invasive periorbital rejuvenation with a focus on platelet rich plasma.A narrative review. J Cosmet Dermatol. 2020;19:1057–62. doi: 10.1111/jocd.13376. [DOI] [PubMed] [Google Scholar]
- 56.Al Shami SH. Treatment of periorbital hyperpigmentation using platelet rich plasma injections. Am J Dermatol Venereol. 2014;3:87–94. [Google Scholar]
- 57.Aust M, Pototschnig H, Jamchi S, Busch KH. Platelet rich plasma for skin rejuvenation and treatment of actinic elastosis in the lower eyelid area. Cureus. 2018;10:e2999. doi: 10.7759/cureus.2999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Banihashemi M, Hamidi Alamdaran D, Nakhaeizadeh S. Effects of platelet rich plasma on skin rejuvenation. Int J Pediatr. 2014;2:55. [Google Scholar]
- 59.Hofny ER, Abdel-Motaleb AA, Ghazally A, Ahmed AM, Hussein MRA. Platelet-rich plasma is a useful therapeutic option in melasma. J Dermatolog Treat. 2019;30:396–401. doi: 10.1080/09546634.2018.1524821. [DOI] [PubMed] [Google Scholar]
- 60.Sirithanabadeekul P, Dannarongchai A, Suwanchinda A. Platelet-rich plasma treatment for melasma: A pilot study. J Cosmet Dermatol. 2020;19:1321–7. doi: 10.1111/jocd.13157. [DOI] [PubMed] [Google Scholar]
- 61.Shilpa K, Sacchidanand S, Leelavathy B, Shilpashree P, Divya G, Ranjitha R, et al. Outcome of dermal grafting in the management of atrophic facial scars. J Cutan Aesthetic Surg. 2016;9:244–8. doi: 10.4103/0974-2077.197077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Woo SH, Kim JP, Park JJ, Chung P-S, Lee S-H, Jeong H-S. Autologous platelet-poor plasma gel for injection laryngoplasty. Yonsei Med J. 2013;54:1516–23. doi: 10.3349/ymj.2013.54.6.1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dashore S, Dashore A. Platelet-poor plasma-based biofiller: An innovative alternative to expensive hyaluronic acid–based fillers for treatment of chicken pox scars. J Am Acad Dermatol. 2019;84:e11–3. doi: 10.1016/j.jaad.2019.07.100. [DOI] [PubMed] [Google Scholar]
- 64.Neinaa YME-H, Hodeib AAE-H, Morquos MM, Elgarhy LH. Platelet-poor plasma gel vs platelet-rich plasma for infraorbital rejuvenation: A clinical and dermoscopic comparative study. Dermatol Ther. 2020;30:e14255. doi: 10.1111/dth.14255. [DOI] [PubMed] [Google Scholar]
- 65.Doghaim NN, El-Tatawy RA, Neinaa YM. Assessment of the efficacy and safety of platelet poor plasma gel as autologous dermal filler for facial rejuvenation. J Cosmet Dermatol. 2019;18:1271–9. doi: 10.1111/jocd.12876. [DOI] [PubMed] [Google Scholar]



