Abstract
Background
The COVID-19 pandemic has prompted hospitals to respond with stringent measures. Accurate estimates of costs and resources used in outbreaks can guide evaluations of responses. We report on the financial expenditure associated with COVID-19, the bed-days used for COVID-19 patients and hospital services displaced due to COVID-19 in a Singapore tertiary hospital.
Methods
We conducted a retrospective cost analysis from January to December 2020 in the largest public hospital in Singapore. Costs were estimated from the hospital perspective. We examined financial expenditures made in direct response to COVID-19; hospital admissions data related to COVID-19 inpatients; and the number of outpatient and emergency department visits, non-emergency surgeries, inpatient days in 2020, compared with preceding years of 2018 and 2019. Bayesian time-series was used to estimate the magnitude of displaced services.
Results
USD $41.96 million was incurred in the hospital for COVID-19-related expenses. Facilities set-up and capital assets accounted for 51.6% of the expenditure; patient-care supplies comprised 35.1%. Of the 19,611 inpatients tested for COVID-19 in 2020, 727 (3.7%) had COVID-19. The total inpatient- and intensive care unit (ICU)-days for COVID-19 patients in 2020 were 8009 and 8 days, respectively. A decline in all hospital services was observed from February following a raised disease outbreak alert level; most services quickly resumed when the lockdown was lifted in June.
Conclusion
COVID-19 led to an increase in healthcare expenses and a displacement in hospital services. Our findings are useful for informing economic evaluations of COVID-19 response and provide some information about the expected costs of future outbreaks.
Keywords: COVID-19, Hospital costs, Disease outbreak
Introduction
Coronavirus disease 2019 (COVID-19) was first reported to the World Health Organization (WHO) from Wuhan, China, in December 2019 [1]. Caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), the infection spread worldwide within a few months and resulted in a global pandemic [2]. The first documented case of COVID-19 was identified in Singapore on 23rd January 2020 in a traveller from Wuhan, China [3]. On 7th February 2020 the Ministry of Health Singapore (MOH) raised the Disease Outbreak Response Condition (DORSCON) alert level from yellow to orange (Supplementary data), indicating the severe nature of COVID-19 and the increased risk of community spread [4]. On 7th April 2020, the Singapore Government further announced a circuit breaker, which was essentially a lockdown period aimed at minimizing movements and interactions to limit the spread of community and dormitory COVID-19 cases that had been increasing since March 2020 [4]. As a result of the circuit breaker, all schools and non-essential businesses were closed, social gatherings were prohibited, and residents were requested to stay home. The circuit breaker was progressively lifted from 1st June 2020, and non-essential services were resumed in phases.
The spread of COVID-19 has placed healthcare systems under immense pressure and imposed a considerable financial healthcare burden globally and in Singapore [5,6]. In addition to the direct costs associated with the healthcare resource utilization in COVID-19 patients, hospitals need to respond with enhanced infection control measures such as screening, testing and personal protective equipment (PPE), incur a reduction in ward capacity, and add resources to emergency department, patient isolation facilities and intensive care units (ICUs) [4,6,7]. Moreover, hospitals also defer or cancel elective procedures and other ‘non-essential’ services, resulting in potential reductions in hospital revenue and impact on patient outcomes [6,8,9].
For decision makers to effectively plan for funds and resource allocation in future outbreaks, it is useful to understand the costs and resources used in managing contemporary outbreaks [10]. This is because the management of outbreaks takes up scarce healthcare resources which are inevitably diverted from other health programmes. There is limited local data available describing the costs and resource utilization for COVID-19. The aim of this study was to describe the direct expenditures incurred in the prevention or management of COVID-19, number of bed-days used in COVID-19 patients, and changes in hospital services due to COVID-19 in a large tertiary hospital in Singapore.
Materials and methods
Study design and setting
We conducted a retrospective cost analysis from the hospital's perspective in Singapore General Hospital, which is the largest public hospital in Singapore. The 1900-bed tertiary acute-care hospital, which provides a comprehensive range of medical services including oncological and haematological services, solid organ transplant, and tertiary burns management, accounted for approximately 15% of all acute-care hospital beds in Singapore in 2019. The hospital has an isolation ward consisting of 35 single rooms and 16 beds in cohort-rooms, with negative-pressure infection isolation capabilities. In 2018 and 2019, the hospital had an inpatient occupancy rate of 84.4% and 82.7%, respectively. Most of the annual budget is provided by the government through block-based and/or activity-based funding; less than 13% is derived from the admission of private patients [11]. Our study was reviewed by the institutional ethics review board (CIRB ref. 2020/2089). Given the use of de-identified data exclusively, informed consent was waived.
Measures adopted by the hospital because of the COVID-19 pandemic
-
a.
Overview of government response
On 7th February 2020, the Singapore government raised the DORSCON level from yellow to orange after the first COVID-19 community transmission cases were confirmed (Supplementary data). This was quickly followed a circuit breaker on 7th April 2020, where schools and all non-essential services were halted [12].
-
b.
Healthcare workers
In response to the DORSCON orange status, several protective measures, which were escalated/de-escalated in response to the rapidly evolving epidemiology of the pandemic, were implemented across the hospital. Mask wearing and twice daily temperature checks were mandated for staff. Staff who developed fever or respiratory symptoms had to visit the staff clinic, where a COVID-19 swab test was performed and a five-day medical leave was mandated. Local conferences and official overseas trips were cancelled. Staff returning from high-risk countries were placed on a mandatory 14-day quarantine. Vacation leave was cancelled for all staff to allow for rapid deployment for COVID-19-related processes. Inter-hospital movement of patients and healthcare workers was restricted.
-
c.
Outpatient and emergency department
The number of hospital visitors was restricted. Temperature screening stations and questionnaires were set-up at all hospital entrances to determine the visitors’ travel history, contact history and presence of acute respiratory symptoms (ARI). Dedicated ‘fever areas’ were set up at the emergency department, so that high-risk patients presenting with fever, respiratory symptoms, or epidemiologic risk factors were separated from the common waiting areas and tested for COVID-19 using oropharyngeal swabs for SARS-CoV-2 PCR [13]. Strict limitations were placed on outpatient and elective surgery services [14]. For patients requiring repeat medications, the hospital's pharmacy instituted electronic filling of prescriptions with home delivery [15]. Gradual resumption of outpatient and elective surgeries were allowed when the circuit breaker was lifted – from 1st June 2020, specialist outpatient visits and medical procedures were first resumed with teleconsultation being the preferred mode of service provision; from 19th June 2020, screening services and pre-employment check-up were also resumed.
-
d.
Inpatient
The measures taken in the inpatient setting were described by Wee et al. [7]. Briefly, patients presenting with ARI and high COVID-19 risk were admitted to isolation wards, while those with ARI and low COVID-19 risk were placed in ARI wards converted from general wards [7]. Oropharyngeal COVID-19 swabs for SARS-CoV-2 PCR were regularly performed for all patients in ARI wards and isolation wards [7]. An infection control bundle, comprising infrastructural enhancements, improved PPE, environmental surveillance, patient surveillance and social distancing was implemented in ARI wards. As part of the pandemic preparedness response, the hospital additionally set up a new isolation facility with 50 isolation single rooms to ensure that the hospital had reserve capacity to respond to a full-blown community outbreak.
-
e.
External facilities
COVID-19 testing services and medical services were extended by the hospital to external facilities [16]. This included eight dormitories where the COVID-19 outbreak were predominantly occurring, two swab isolation facilities, and one community care facility (CCF) housing low-risk COVID-19 patients. In the CCF, healthcare staff provided round-the-clock essential primary care and medical consultation. Pharmacists stocked key essential medications, packaged and dispensed them remotely [16].
Data sources
Direct expenditure associated with the management or prevention of COVID-19 from January 2020 to December 2020, including costs expended for the support of community COVID-19 operations, was obtained from the hospital's finance department. These costs were classified as: capital assets and facilities set-up for the prevention or management of COVID-19, labour-related costs, patient-care-related materials and supplies, and non-patient-care materials, related to the prevention or management of COVID-19, and costs associated with services for external facilities. All costs were presented in 2020 US dollars (USD) (1 Singapore dollar = 1.354 USD). Time losses in existing healthcare staff or time spent by existing healthcare staff redeployed for COVID-19 related processes and overhead costs were not considered as these were deemed to be sunk costs. Lost revenue due to deferment of services was also not included as it was not deemed to be direct expenditure. Data on patients hospitalized with COVID-19 from January to December 2020 were identified from the hospital's electronic database. Data collected were length of inpatient stay and length of stay in the ICU, number of COVID-19 tests done, and discharge status. To describe changes in hospital services due to COVID-19, weekly data pertaining to number of outpatient visits, non-emergency surgeries, inpatient days, and emergency department visits for 2020 and the preceding years of 2018 and 2019 were extracted from the hospital's database.
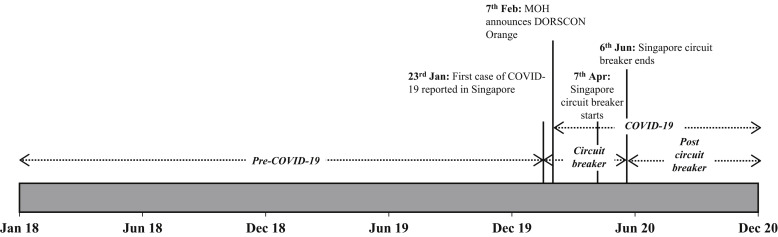
Statistical analysis
All statistical analyses were performed in R software (R Core Team (2020). R: A language and environment for statistical computing; R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/). We employed descriptive statistics to summarize the hospitalization characteristics and costs. Frequency and percentages were reported for categorical variables. Mean (95% confidence intervals (CIs)) or median (first quartile – third quartile) were reported for continuous variables. Changes in hospital services associated with COVID-19 were explored by reporting the average weekly numbers along with 95% CIs in a Bayesian time series model [17]. Four time-periods were considered in the time series, as shown in Figure 1 : before the DORSCON Orange status was termed pre-COVID-19 period, announcement of the DORSCON Orange and the subsequent circuit breaker was termed circuit breaker period, the lifting of the circuit breaker to the end of 2020 was termed post-circuit-breaker period, and the entire period from announcement of DORSCON Orange to the end of 2020 was termed COVID-19 period. To determine the relative effect of COVID-19 pandemic on the reduction in hospital services in each time period compared with the pre-COVID-19 period, analyses were conducted using the ‘bsts’ and ‘CausalImpact’ packages [17]. The ‘CausalImpact’ package provides an estimate of the absolute and relative effect of an intervention in a targeted time series by analysing the difference between a forecasted counterfactual model and the actual model [17]. A two-sided P-value of ≤0.05 was significant.
Figure 1.
Timeline of COVID-19 in Singapore in 2020. Based on the timeline, a total of three time periods were modelled in the time-series analysis: (1) pre-COVID-19 phase; (2) circuit breaker phase (encompasses the start of Disease Outbreak Response Condition (DORSCON) Orange and circuit breaker); and (3) post circuit breaker COVID-19 phase. The entire period from the start of DORSCON Orange to the end of 2020 was modelled as ‘COVID-19’ period in the time-series analysis. MOH, Ministry of Health, Singapore.
Results
Actual expenditure associated with COVID-19
The response to the pandemic incurred USD $45.39 million cash expenditures with USD $3.43 million (7.6%) for services rendered to support community COVID-19 operations and USD $41.96 million (92.4%) for hospital-based services. Table I is an itemized listing of COVID-19 related expenditures in 2020. Facilities set-up and purchase of capital assets in response to the pandemic was USD $21.67 million and accounted for 51.6% of the in-hospital expenditure. Patient-care-related supplies and services were USD $14.72 million and accounted for 35.1% of the in-hospital expenditure. The largest single item category of expenditure incurred was medical supplies at USD $14.08 million, which accounted for 33.6% of all in-hospital expenditure. Expenditure for labour costs comprised mainly of wages of newly hired staff in response to the pandemic and overtime wages and this was 62.2% of all in-hospital labour-related costs.
Table I.
Summary of COVID-19-related costs incurred by the hospital in 2020
| Item | Cost in millions (2020 SGD) | Cost in millions (2020 USD) | Percentage (%) |
|---|---|---|---|
| Costs incurred in the hospital | |||
| Facilities set-up and capital assets | 29.34 | 21.67 | 51.6 |
| Facilities set-up | 13.9 | 10.27 | 24.5 |
| Large capital assets | 15.02 | 11.09 | 26.4 |
| Minor capital assets | 0.42 | 0.31 | 0.7 |
| Labour-related costs | 4.33 | 3.20 | 7.6 |
| New hires and overtime salary | 2.7 | 1.99 | 4.8 |
| Staff support | 1.5 | 1.11 | 2.6 |
| Other miscellaneous labour-related costs | 0.13 | 0.10 | 0.2 |
| Patient-care supplies and services | 19.92 | 14.71 | 35.1 |
| Medical supplies | 19.07 | 14.08 | 33.6 |
| Pharmaceuticals | 0.11 | 0.08 | 0.2 |
| Housekeeping | 0.7 | 0.52 | 1.2 |
| Other patient-care related supplies/services | 0.04 | 0.03 | 0.1 |
| Non-patient-care supplies and services | 3.23 | 2.39 | 5.7 |
| Security | 0.65 | 0.48 | 1.1 |
| Transport services | 0.62 | 0.46 | 1.1 |
| IT and communications | 0.21 | 0.16 | 0.4 |
| Other non-patient-care related supplies and services | 1.75 | 1.29 | 3.1 |
| Total |
56.82 |
41.96 |
100 |
| Costs incurred due to services rendered to external locations | |||
| Labour-related costs | 3.05 | 2.25 | 65.6 |
| Patient-care supplies and services | 1.11 | 0.82 | 23.9 |
| Non-patient-care supplies and services | 0.49 | 0.36 | 10.5 |
| Total | 4.65 | 3.43 | 100 |
Patients hospitalized with COVID-19
From January to December 2020, 35,205 COVID-19 test swabs was performed on 19,611 patients admitted to the hospital. Of the 19,611 patients tested for COVID-19, 727 (3.7%) were positive for COVID-19. The median length of hospital stay of COVID-19 patients was eight days (6–13 days). Of the 727 COVID-19 patients, only three (0.4%) were admitted to the ICU for a median of two days (1–5 days). The total number of inpatient and ICU days for COVID-19 patients in 2020 was 8009 days and eight days, respectively. This accounted for 0.7% and 0.02% of the hospital's total inpatient and ICU bed-days in 2020, respectively.
Changes in hospital services associated with COVID-19
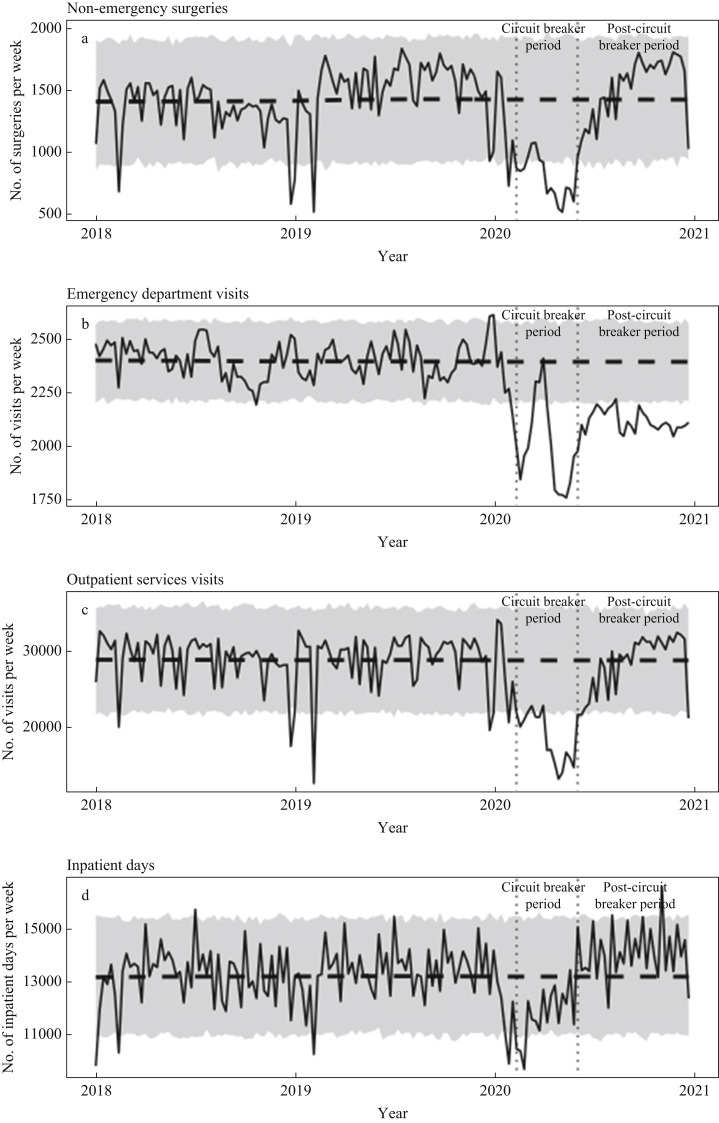
In response to the DORSCON orange status and the subsequent implementation of circuit breaker, we observed reductions in the frequency of hospital-based services for the circuit breaker period compared with the pre-COVID-19 period in 2018 and 2019. The weekly trends for the services are shown in Figure 2 , and a summary of the relative effects shown in Table II . In the circuit breaker period, the greatest reduction was observed for non-emergency surgeries (45%, P<0.001) and outpatient visits (36%, P<0.001); inpatient days were reduced by 11% (P<0.001). Most services resumed in the post-circuit breaker period, except for emergency department visits, which remained significantly lower (13%, P<0.001) compared with the pre-COVID-19 period. When the entire COVID-19 period was collectively compared with the pre-COVID-19 period, no significant reduction was observed in inpatient days (1%, P=0.206). Non-emergency surgeries (P<0.001) and outpatient visits (P<0.001) services were both reduced by 13% when the entire COVID-19 period was compared with the pre-COVID-19 period.
Figure 2.
Actual weekly data (solid line) versus predicted (dashed line) with 95% confidence interval for (a) non-emergency surgeries; (b) Emergency Department visits; (c) outpatient visits; and (d) inpatient bed-days. Significant drops were observed for all services during the circuit breaker phase, following the Disease Outbreak Response Condition (DORSCON) Orange alert.
Table II.
Summary of lost opportunities associated with COVID-19
| Type of service | Pre-COVID-19 |
Circuit breaker |
Post circuit-breaker |
COVID-19 |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Average weekly no. (95% CI) | Average weekly no. (95% CI) | Effect size compared to pre-COVID-19 |
Average weekly no. (95% CI) | Effect size compared to pre-COVID-19 |
Average weekly no. (95% CI) | Effect size compared to pre-COVID-19 |
||||
| Relative effect (95% CI) | P | Relative effect (95% CI) | P | Relative effect (95% CI) | P | |||||
| Non-emergency surgeries | 1426 (1377–1473) | 803 (708–899) | -45% (-54%, -35%) | <0.001 | 1509 (1406–1612) | 6% (-1%, 13%) | 0.063 | 1264 (1139–1388) | -11% (-18%, -4%) | <0.001 |
| Emergency department visits | 2397 (2379–2415) | 2000 (1888–2111) | -16% (-19%, -14%) | <0.001 | 2089 (2024–2154) | -13% (-14%, -11%) | <0.001 | 2058 (2002–2114) | -13% (-15%, -12%) | <0.001 |
| Outpatient visits | 28,906 (28,243–29,569) | 18,580 (16,779–20,382) | -36% (-43%, -29%) | <0.001 | 28,307 (26,833–29,782) | -2% (-7%, 4%) | 0.260 | 24,924 (23,147–26,701) | -13% (-18%, -9%) | <0.001 |
| Inpatient bed days | 13,258 (13,048–13,468) | 12,036 (11,368–12,704) | -11% (-15%, -6%) | <0.001 | 13,940 (13,408–14,472) | 6% (2%, 10%) | 0.003 | 13,278 (12,793–13,763) | 1% (-2%, 5%) | 0.206 |
CI, confidence interval.
Discussion
Cost studies in healthcare are useful to inform decisions for efficient allocation of healthcare resources. In this study, we reported the cash expenditures, bed-days used for COVID-19 patients and changes in healthcare services due to the COVID-19 pandemic in a tertiary hospital in Singapore. We found that a small number of COVID-19 patients were admitted to the hospital in 2020, accounting for only 0.7% of all inpatient bed-days. However, the actual expenditure incurred by the hospital was substantial, mainly due to costs in facilities set-up, capital assets and medical supplies for prevention or management of COVID-19. While we did not tabulate the actual costs associated with lost opportunities due to missed revenue, we observed significant reduction in volumes in all hospital services during the circuit breaker period compared with the pre-COVID-19 period.
In 2003, Singapore was one of the countries most affected by the severe acute respiratory syndrome (SARS) outbreak [18]. The experience has led local hospitals to adopt a prudent approach in dealing with the COVID-19 pandemic in 2020 [19]. However, the stringent infection prevention measures translated to high expenditures incurred by the hospital. Notably, facilities set-up for infection prevention and purchase of capital assets in response to the pandemic accounted for more than half of the COVID-19-related expenditure. Interestingly, labour-related costs incurred by the hospital were modest. This is likely attributed to the fact that opportunity costs associated with lost clinical time due to redeployment of staff for COVID-19-related processes were not included in our tabulation of direct hospital expenditure. In the two months before circuit breaker was announced, clinical and non-clinical hospital staff were trained to manage fever screening areas and had conducted full-scale simulations as part of the hospital's Preparedness and Response plan, Upon circuit breaker announcement, existing hospital staff were quickly redeployed to manage COVID-19-related processes, and were also separated into multiple teams to allow for longer shift hours and to ensure business continuity should any staff be quarantined due to COVID-19 [13,20,21].
Despite being the largest Singapore tertiary acute care hospital with 15% of all Singapore inpatient beds in 2019, only 727 (1.2%) of 58,599 COVID-19 patients in Singapore in 2020 were admitted to our study hospital. There are two reasons for small number of COVID-19 patients in our hospital: firstly, large-scale dedicated isolation units termed CCFs have been set up to house low-risk COVID-19 patients to prevent the nation's healthcare infrastructure from becoming overwhelmed [16]. Secondly, patients who presented at primary care clinics fulfilling criteria for COVID-19 and requiring hospitalization were predominantly sent to the National Centre for Infectious Diseases, which is a 330-bedded high-level isolation hospital purpose built for infectious diseases and outbreak management. Of the 727 patients that were admitted, only three were admitted to the ICU during their stay. This is likely because almost 95% of the infected patients in Singapore in 2020 comprised migrant workers in their 20s or 30s with little or no comorbidities, in which the likelihood of severe disease is markedly lower compared with elderly individuals or those with comorbidities [22]. Previous studies have estimated that the direct medical cost of a COVID-19 patient to range from USD $3,000 to USD $12,000 per patient in USA [5,23]. While we did not estimate the average direct medical costs of each COVID-19 patient, we observed that the expenditure for medical supplies and pharmaceutical products in COVID-19 prevention or management was almost USD $15 million despite the small number of COVID-19 patients. We found that this was because all patients presenting with acute respiratory disease, including those without travel history or prior known contact with COVID-19 patients, were considered to be at risk of having COVID-19. Hence, dedicated wards, termed ARI wards, were set up to segregate these patients from the rest of the hospital. In these ARI wards, extensive infection control measures, including infrastructural enhancement and social distancing, risk stratified PPE use, enhanced cleaning and sanitation, and regular testing for COVID-19 infection was instituted, which contributed to the COVID-19-related medical supplies expenditure incurred by the hospital [7].We consider our costs estimates to be conservative as we did not include costs that were not a direct part of the infection control measures. For instance, costs associated with the implementation of services to provide alternative methods of care, such as remote counselling and teleconsultation clinics during the circuit breaker phase were excluded from our cost estimates.
Previous studies have suggested that the monetary losses of clinical and surgical revenues due to reduction in hospital services are likely to eclipse the direct financial expenditures in an outbreak [6,10,24]. Mulholland et al. described overall sharp drops in emergency department, inpatient admissions, and surgical admissions in Scotland hospitals following the WHO COVID-19 pandemic announcement and the consequent UK lockdown [8]. In our study, we similarly observed reductions in all hospital services following the declaration of the DORSCON orange status and subsequent circuit breaker. Notably, approximately one-third of all outpatient services and almost half of non-emergency surgeries were cancelled during the circuit breaker period, which may result in lost clinical revenue. However, this loss is likely to be low considering that most of hospital's revenue is derived from annual block funding from the government, which is not directly affected by patient volume [11]. Most services rallied after the circuit breaker was lifted likely due to pent-up demand; hence, the onset of COVID-19 in 2020 resulted in approximately only 10% reduction in services compared with the pre-COVID-19 period. Despite this, it should be noted that to allow business continuity during the COVID-19 pandemic, hospitals can incur higher costs in service provision due to the need for additional infection prevention measures such as increased COVID-19 testing, more stringent use of PPEs, and reduced visits for social distancing [14].
Our study has limitations. We did not quantify the costs associated with lost revenue due to the lack of data informing the clinical revenue associated with each service. However, we postulated that this loss in revenue is likely to be modest considering the minimal reduction in overall service provision by the hospital in 2020 and the funding mechanism of the hospital. Another limitation is that our findings may be less generalizable for other healthcare systems in other countries with different policy responses against COVID-19, or for healthcare systems with different payment structures. Nevertheless, we believe that our findings are valuable in informing local healthcare administrators and decision makers in subsequent responses in future pandemics. Our study also did not consider the wider socio-economic impact of COVID-19, including its impact on healthcare workers' well-being and productivity. In a survey by Tan et al., it was reported that burnout and disengagement was observed in three-quarters of surveyed healthcare workers during the COVID-19 pandemic [25]. The efficacy and cost-effectiveness of methods to support the mental well-being of healthcare workers, such as mobile health apps, may be of interest in future studies [26]. Finally, continued analysis of the hospital costs will be warranted, as cost structures will change when hospitals evolve from the traditional face-to-face patient–physician care model to novel models of remote consultations, such as the use of artificial intelligence or machine learning for automated clinical diagnosis and home-based monitoring [27].
In conclusion, in our study, we found that the prevention and management of the COVID-19 pandemic is associated with high financial expenditure to Singapore hospitals. While healthcare services were disrupted during lockdown, these services quickly rallied after the lockdown was lifted. Given that we are still in the midst of the COVID-19 pandemic, it is uncertain how subsequent waves of infection or changes in vaccination rates may impact hospital responses and costs. Understanding the key costs in the response to the COVID-19 pandemic can enable us to make better-informed decisions as we prepare to respond to future epidemics.
Acknowledgements
The authors thank the Singapore General Hospital Finance Department for the assistance in data extraction. We also thank Professor Kenneth Kwek, Chief Executive Officer of Singapore General Hospital, as well as the SingHealth Duke-NUS AMII Impact Assessment Unit for their support in this study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jhin.2021.12.007.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Funding sources
This study was funded by the National Medical Research Council COVID-19 Research Grant (MOH-000410) and the Pfizer Investigator Sponsored Research Grant (62978547). The funders had no role in the design of this study and or in its execution, analyses, interpretation of the data, or decision to submit results.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.World Health Organization . 2020. Timeline: WHO's COVID-19 response.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline#!; 2020 Available at: [last accessed September 2021] [Google Scholar]
- 2.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wong J.E.L., Leo Y.S., Tan C.C. COVID-19 in Singapore – current experience: critical global issues that require attention and action. JAMA. 2020;323(13):1243–1244. doi: 10.1001/jama.2020.2467. [DOI] [PubMed] [Google Scholar]
- 4.Tan T.H.Y., Toh M., Vasoo S., Lye D.C.B., Ang B.S.P., Leo Y.S., et al. Coronavirus disease 2019 (COVID-19): the Singapore experience. A review of the first eight months. Ann Acad Med Singap. 2020;49(10):764–778. [PubMed] [Google Scholar]
- 5.Bartsch S.M., Ferguson M.C., McKinnell J.A., O'Shea K.J., Wedlock P.T., Siegmund S.S., et al. The potential health care costs and resource use associated with COVID-19 in the United States. Health Aff (Millwood) 2020;39(6):927–935. doi: 10.1377/hlthaff.2020.00426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaye A.D., Okeagu C.N., Pham A.D., Silva R.A., Hurley J.J., Arron B.L., et al. Economic impact of COVID-19 pandemic on healthcare facilities and systems: International perspectives. Best Pract Res Clin Anaesthesiol. 2021;35:293–306. doi: 10.1016/j.bpa.2020.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wee L.E.I., Sim X.Y.J., Conceicao E.P., Aung M.K., Tan K.Y., Ko K.K.K., et al. Containing COVID-19 outside the isolation ward: the impact of an infection control bundle on environmental contamination and transmission in a cohorted general ward. Am J Infect Control. 2020;48(9):1056–1061. doi: 10.1016/j.ajic.2020.06.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mulholland R.H., Wood R., Stagg H.R., Fischbacher C., Villacampa J., Simpson C.R., et al. Impact of COVID-19 on accident and emergency attendances and emergency and planned hospital admissions in Scotland: an interrupted time-series analysis. J R Soc Med. 2020;113(11):444–453. doi: 10.1177/0141076820962447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shin J.H., Takada D., Morishita T., Lin H., Bun S., Teraoka E., et al. Economic impact of the first wave of the COVID-19 pandemic on acute care hospitals in Japan. PLoS One. 2020;15(12) doi: 10.1371/journal.pone.0244852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Achonu C., Laporte A., Gardam M.A. The financial impact of controlling a respiratory virus outbreak in a teaching hospital: lessons learned from SARS. Can J Public Health. 2005;96(1):52–54. doi: 10.1007/BF03404018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haseltine W.A. Brookings Institution Press; 2013. Affordable excellence: the Singapore health system. [Google Scholar]
- 12.Moh S. 2020. Circuit breaker to minimise futher spread of COVID-19.https://www.moh.gov.sg/news-highlights/details/circuit-breaker-to-minimise-further-spread-of-covid-19 Available at: [last accessed September 2021] [Google Scholar]
- 13.Quah L.J.J., Tan B.K.K., Fua T.P., Wee C.P.J., Lim C.S., Nadarajan G., et al. Reorganising the emergency department to manage the COVID-19 outbreak. Int J Emerg Med. 2020;13(1):32. doi: 10.1186/s12245-020-00294-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wong J., Goh Q.Y., Tan Z., Lie S.A., Tay Y.C., Ng S.Y., et al. Preparing for a COVID-19 pandemic: a review of operating room outbreak response measures in a large tertiary hospital in Singapore. Can J Anaesth. 2020;67(6):732–745. doi: 10.1007/s12630-020-01620-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kee T., Hl V.G., Shimin J.C., Sing T.P., Moi L.Y., Peng C.L., et al. Managing a renal transplant programme during the COVID-19 pandemic: practical experience from a Singapore transplant centre. Ann Acad Med Singap. 2020;49(9):652–660. [PubMed] [Google Scholar]
- 16.Chia M.L., Him Chau D.H., Lim K.S., Yang Liu C.W., Tan H.K., Tan Y.R. Managing COVID-19 in a novel, rapidly deployable community isolation quarantine facility. Ann Intern Med. 2021;174(2):247–251. doi: 10.7326/M20-4746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brodersen K.H., Gallusser F., Koehler J., Remy N., Scott S.L. Inferring causal impact using Bayesian structural time-series models. Ann Appl Stat. 2015;9(1):247–274. [Google Scholar]
- 18.Oh V.M., Lim T.K. Singapore's experience of SARS. Clin Med (Lond) 2003;3(5):448–451. doi: 10.7861/clinmedicine.3-5-448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lin R.J., Lee T.H., Lye D.C. From SARS to COVID-19: the Singapore journey. Med J Aust. 2020;212(11):497–502 e1. doi: 10.5694/mja2.50623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Monica F.P.E., Aloweni F., Yuh A.S., Ayob E.B.M., Ahmad N.B., Lan C.J., et al. Preparation and response to COVID-19 outbreak in Singapore: a case report. Infect Dis Health. 2020;25(3):216–218. doi: 10.1016/j.idh.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thangayah J.R., Tan K.B.K., Lim C.S., Fua T.P. Disease outbreak surge response: how a Singapore tertiary hospital converted a multi-story carpark into a flu screening area to respond to the COVID-19 pandemic. Disaster Med Public Health Prep. 2021;15(3):e37–42. doi: 10.1017/dmp.2020.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li X., Xu S., Yu M., Wang K., Tao Y., Zhou Y., et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol. 2020;146(1):110–118. doi: 10.1016/j.jaci.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Di Fusco M., Shea K.M., Lin J., Nguyen J.L., Angulo F.J., Benigno M., et al. Health outcomes and economic burden of hospitalized COVID-19 patients in the United States. J Med Econ. 2021;24(1):308–317. doi: 10.1080/13696998.2021.1886109. [DOI] [PubMed] [Google Scholar]
- 24.Otter J.A., Burgess P., Davies F., Mookerjee S., Singleton J., Gilchrist M., et al. Counting the cost of an outbreak of carbapenemase-producing Enterobacteriaceae: an economic evaluation from a hospital perspective. Clin Microbiol Infect. 2017;23(3):188–196. doi: 10.1016/j.cmi.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 25.Tan B.Y.Q., Kanneganti A., Lim L.J.H., Tan M., Chua Y.X., Tan L., et al. Burnout and associated factors among health care workers in Singapore During the COVID-19 pandemic. J Am Med Dir Assoc. 2020;21(12):1751–1758.e5. doi: 10.1016/j.jamda.2020.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yoon S., Goh H., Nadarajan G.D., Sung S., Teo I., Lee J., et al. Perceptions of mobile health apps and features to support psychosocial well-being among frontline health care workers involved in the COVID-19 pandemic response: qualitative study. J Med Internet Res. 2021;23(5) doi: 10.2196/26282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gunasekeran D.V., Tham Y.C., Ting D.S.W., Tan G.S.W., Wong T.Y. Digital health during COVID-19: lessons from operationalising new models of care in ophthalmology. Lancet Digit Health. 2021;3(2):e124–e134. doi: 10.1016/S2589-7500(20)30287-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.