Highlights
-
•
Contact with stigmatized groups is a promising mechanism for reducing bias.
-
•
The nature of contact with patients who misuse opioids matters significantly.
-
•
Contact with patients who misuse opioids can have negative consequences for physicians.
-
•
Consequences occur in physicians who are experiencing stress, burnout, and bias.
-
•
Interventions need to consider factors that may reduce the effectiveness of contact.
Keywords: Bias, Stigma, Opioid use disorder, Contact, Intervention
Abstract
Introduction
Prior research suggests that some physicians hold negative attitudes toward patients who misuse opioids and that this serves as a barrier which limits the availability and effectiveness of health care services. Interventions which improve physicians’ attitudes have thus garnered attention, many of which have focused on increasing contact between physicians and patients who misuse opioids. However, drawing on recent literature on intergroup contact, the current paper argues that contact may not have uniformly positive effects on prejudice.
Methods
We surveyed 408 board-certified physicians in the state of Ohio where many opioid overdose deaths have been concentrated. We used regression to test for interactions between contact and three focal variables, bias, burnout, and stress, on physician willingness to work with patients who misuse opioids.
Results
The negative relationships between bias, physician burnout, and stress induced by working with patients who misuse opioids and physicians’ willingness to work with this patient population are each exacerbated when contact with patients who misuse opioids is high.
Conclusions
Although intervention studies have shown promise for the role that increased contact may have in reducing stigma toward patients who misuse opioids, these interventions may not be appropriate for physicians who are experiencing strain or who hold preexisting negative attitudes toward this patient population. Future interventions may need to target bias, burnout, and stress, in addition to facilitating contact, to increase physician willingness to work with these patients.
The opioid crisis in the United States has claimed over 700,000 lives in the last decade (Centers for Disease Control and Prevention, 2020) and has significantly strained the health care system as substantial personnel and material resources are needed to treat opioid misuse, defined as opioid use that occurs outside of the parameters of a prescription (Substance Abuse and Mental Health Services Administration, 2017), and its secondary health consequences (Hagemeier, 2018). Although we have begun to see a levelling off of opioid overdose deaths in many communities (Hedegaard, Minino, & Warner, 2020), evidence suggests important barriers still exist that prevent patients who misuse opioids from receiving substance use services and the general medical care required to combat this epidemic. One key barrier is negative attitudes toward patients who misuse opioids held by health care professionals, which limits the accessibility and quality of health care services available for these patients (van Boekel, Brouwers, van Weeghel, & Garretsen, 2013).
Highlighting the importance of this barrier, research has documented pervasive negative attitudes toward people and patients who use drugs more generally and has shown that these negative attitudes surpass those felt for other stigmatized patient populations (Broady et al., 2020, Gilchrist et al., 2011, Lloyd, 2013). Additionally, stigmatization might be particularly pronounced for some groups of patients who use opioids such as those who inject opioids (Kennedy-Hendricks et al., 2017, McCradden et al., 2019). Physicians also report finding interactions with patients who misuse substances to be more challenging, less motivating, and less satisfying, thus leading physicians to avoid treating such patients (van Boekel et al., 2013). Most importantly, emerging evidence suggests these negative attitudes can impede effective health care for patients with substance use disorders such as opioid use disorder (Brener, Hippel, Kippax, & Preacher, 2010). That is, when such patients perceive biased treatment from their health care providers, their likelihood of adhering to or completing recommended treatment programs diminishes (Brener et al., 2010). Research has also suggested that negative attitudes toward patients who use drugs can adversely affect health care providers through reducing their job satisfaction and increasing their desire to leave the health care profession (von Hippel, Brener, & von Hippel, 2008).
The role of physician attitudes in determining health care outcomes among patients who misuse opioids and other substances underscores the need to identify potential interventions to mitigate bias and improve physicians’ willingness to work with these patients. Among extant work attempting to design effective interventions, one of the most common approaches is to facilitate contact between physicians and patients who misuse opioids or other substances (Lloyd, 2013). This approach is utilized because contact between majority group members and members of stigmatized social groups has long been proposed as an efficacious way to reduce prejudice and intergroup conflict (Allport, 1954). Contact, it is argued, can alleviate negative attitudes through decreasing anxiety about intergroup interactions and increasing knowledge about and empathy toward members of the stigmatized group (Pettigrew & Tropp, 2008). The theoretical role of contact in reducing prejudice has also been supported by empirical evidence which has found that increased contact is associated with lower prejudice toward a number of minority groups (Pettigrew & Tropp, 2008). These findings have also been replicated for prejudice toward patients who misuse substances such as opioids (Broady et al., 2020, Broady et al., 2021, Livingston et al., 2012, Lloyd, 2013). Indeed, two recent reviews on stigma relating to substance use and interventions to reduce such stigma concluded that increasing contact was one of the most commonly used and supported intervention methods (Livingston et al., 2012, van Boekel et al., 2013).
Despite the seemingly consistent evidence that contact can improve attitudes toward patients who misuse substances, research in other areas has started to challenge the conclusion that intergroup contact uniformly reduces bias. That is, recent research has begun to recognize that other situational and personal factors can influence the effects contact has on prejudice, and has demonstrated that contact with outgroup members that is appraised as negative can more strongly influence prejudice than contact which is appraised as positive (Aberson, 2015, Barlow et al., 2012). We argue that these findings are of relevance to our understanding of the role of contact in determining physicians’ bias toward patients who misuse opioids. As noted above, some physicians describe their interactions with patients who misuse opioids as difficult, taxing, and unsatisfying (van Boekel et al., 2013). Thus, the types of routine, on-the-job contact physicians have with patients who misuse opioids may, in some cases, more closely mirror negative rather than positive contact. Importantly, this may limit the generalizability of the conclusions drawn from experiments which facilitate contact between physicians and patients who misuse opioids in highly controlled environments because the strenuous nature of physician-patient interactions may not engender the same benefits. Indeed, some findings have begun to challenge the positive relationship between contact and prejudice toward patients who misuse substances, demonstrating that contact may not be effective at erasing strongly held negative attitudes and can actually increase implicit biases (Brener et al., 2007, Crapanzano et al., 2014).
The goal of this paper is to strengthen our understanding of the role of intergroup contact by proposing that increased on-the-job contact with substance users may actually amplify the effects of negative beliefs and appraisals about patients who misuse opioids when the contact occurs under strained conditions. More specifically, we posit that contact may increase the negative impact of bias, burnout, and stress induced by working with patients who misuse opioids on physician’s willingness to work with this patient population. We chose to focus on bias, burnout, and stress induced by working with patients who misuse opioids because these constructs impact the likelihood that physicians’ will negatively appraise their interactions with this patient population. Further, physicians who already have negative appraisals of working with patients who misuse opioids may experience even more strain when they have higher contact with this patient population and may resultingly want to avoid difficult patient interactions. The result, we hypothesize, is that physicians who experience contact with patients who misuse opioids under negative conditions will report lower willingness to engage with this patient population.
We also contend that stress and burnout are important to consider given the evidence suggesting that health care providers, particularly those who specialize in alcohol and drug services, report high levels of stress and burnout (Duraisingam, Pidd, & Roche, 2009; Elman and Dowd, 1997, Knudsen et al., 2006, Vilardaga et al., 2011). As Oser, Biebel, Pullen, and Harp (2013) summarize, stress and burnout may originate from general job conditions as well as from working with patients who experience relapse, have comorbid physical (e.g., HIV or HCV) or mental health conditions, or may have difficulty identifying and overcoming their drug use. Each of these factors can also contribute to health care providers having strenuous interactions with patients who use substances, which may explain why providers often find interactions with patients who use drugs to be challenging and unsatisfying (van Boekel et al., 2013). Together, this suggests the need to consider stress and burnout given that they are commonplace among providers and emphasizes the unique forms of contact providers may have with this patient population.
Addressing this question contributes to the literature in two primary ways. First, researchers have underscored the need to examine the variables that may affect the relationship between intergroup contact and prejudice, stating that “factors that curb contact’s ability to reduce prejudice are now the most problematic theoretically, yet the least understood. These negative factors… deserve to become a major focus of future contact research” (Pettigrew & Tropp, 2006). Our study advances this goal by examining bias, burnout, and stress as potential situational and personal characteristics which may hamper the positive benefits assumed to be associated with intergroup contact. Additionally, our study can inform the development of future interventions aimed at increasing physicians’ willingness to work with patients who misuse opioids by examining the potential boundary conditions surrounding the effectiveness of intergroup contact as an intervention. By identifying the conditions under which contact may not have the intended benefits, interventionists can design more targeted interventions which address important barriers that may alter physician responses to contact.
1. Method
1.1. Participants
Data were collected from 408 board-certified physicians licensed to practice in Ohio. Physicians were recruited to participate in a survey regarding their experiences and perceptions surrounding the opioid crisis in the United States. Email invitations to participate in the survey were sent to board-certified physicians who listed an Ohio residence in October 2019 and the survey remained open through November 2019. Participants were entered into a drawing to win one of three $200 Amazon gift cards in exchange for their participation.
Of the 408 physicians who participated in the survey, 58.8% identified as male, the average age was 51.22, the average number of hours worked per week was 46.01, and physicians had worked in their current position for an average of 12.89 years. An examination of the medical credentials held by our sample revealed that 75.50% of our sample had a Doctor of Medicine (M.D.) degree whereas 24.50% reported holding a Doctor of Osteopathic Medicine (D.O.) and participants were nearly evenly split between primary care (56.04%) and specialty practice (43.96%). This study was approved by the [name redacted] internal review board and electronic informed consent was obtained from all participants.
1.2. Measures
We measured bias toward and contact with patients who misuse opioids, burnout, and stress induced by working with patients who misuse opioids as our predictor variables. Bias was measured using a 10-item scale originally designed to capture negative attitudes toward patients who injected drug (Brener & von Hippel, 2008). Items were adapted to assess bias toward patient who misuse opioids by replacing references to “injecting drug use/users” with “opioid misuse/misusers”. A sample item is: “I avoid opioid misusers whenever possible.” Burnout was measured using the work-related (7 items) and client-related (6 items) subscales of the Copenhagen Burnout Inventory (Kristensen, Borritz, Villadsen, & Christensen, 2005). Work-related burnout assessed how exhausting or draining respondents find their work in general and client-related burnout assessed feelings of exhaustion specific to working with clients. Stress induced by working with opioid misusers was measured using two items taken from von Hippel, Brener, and Von Hippel (Brener & von Hippel, 2008). Those items were, “Working with opioid misusers is really a strain for me,” and “Working with opioid misusers directly puts too much stress on me.” Finally, and consistent with prior work on bias, we measured contact using a single item that asked respondents to report the percentage of their time on the job that is spent working with patients who misuse opioids (Brener et al., 2007). These measures were selected because they have been validated for use among health care professionals and have demonstrated adequate reliability in previous studies.
Our dependent variable was willingness to work with patients who misuse opioids, which was assessed using 5 items that asked physicians to report their desire to continue working with patients who misuse opioids. Given that a validated scale was unavailable in the extant literature, we created these items by drawing on measures of therapeutic attitudes toward other patient populations. An example item is: “In the future, I would accept more patients that are opioid misusers.” All measures demonstrated adequate reliabilities (α > 0.81) and are reported in Table 1.
Table 1.
Bivariate correlations among study variables.
| Variable | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gender | 1.41 | 0.49 | |||||||||||
| Age | 51.22 | 12.00 | −0.26* | ||||||||||
| Work hours | 46.01 | 17.30 | −0.09 | −0.31* | |||||||||
| Tenure | 12.88 | 10.27 | −0.22* | 0.59* | −0.09 | ||||||||
| Current prescribing | 1.21 | 0.41 | 0.00 | 0.08 | −0.15* | −0.09 | |||||||
| Past prescribing | 1.05 | 0.22 | −0.01 | −0.05 | 0.06 | 0.02 | 0.38* | ||||||
| Burnout | 2.25 | 0.77 | 0.02 | −0.13* | 0.15* | −0.02 | −0.11* | 0.00 | (0.91) | ||||
| Stress | 3.74 | 1.19 | 0.01 | −0.06 | 0.08 | 0.06 | −0.14* | 0.00 | 0.41* | (0.89) | |||
| Contact | 18.69 | 20.44 | 0.01 | 0.05 | −0.13* | −0.22* | 0.04 | −0.01 | 0.10 | 0.00 | |||
| Bias toward opioid misusers | 2.97 | 0.74 | −0.08 | 0.00 | 0.13* | 0.14* | 0.02 | 0.00 | 0.19* | 0.30* | −0.17* | (0.81) | |
| Willingness to work with opioid misusers | 2.76 | 1.04 | 0.14* | −0.06 | −0.06 | −0.20* | 0.01 | 0.01 | −0.29* | −0.41* | 0.32* | −0.60* | (0.87) |
Note: N = 339–408, alphas appear on the diagonal; gender is coded 1 = male and 2 = female; * p < .05.
1.3. Analyses
We assessed the relationships among our study variables by computing bivariate correlations as well as testing the interactions between contact and bias, burnout, and stress. All analyses were conducted using SPSS (IBP Corp, 2020). Interactions between our three focal variables (i.e., bias, stress, and burnout induced by working with patients who misuse opioids) and contact were tested using three regression models. For each model, demographic variables (i.e., gender, age, work hours, tenure, and current and past prescribing behaviors) were entered in the first step. The second step then added contact and bias (Model 1), stress (Model 2), or burnout (Model 3). The final step then included the product term calculated between contact and bias, stress, or burnout, respectively. Following best practice recommendations (Hayes, 2018), we interpreted the interaction by estimating the conditional relationship between each predictor and willingness to work with patients who misuse opioids at various levels of the moderating variable (i.e., contact). Specifically, we estimated the conditional effects at one standard deviation below the mean, the mean, and one standard deviation above the mean for contact. This allows us to estimate whether and how the relationship between the predictor variable and willingness to work with patients who misuse opioids changes as a function of contact with these patients. The conditional effects were computed using the PROCESS Macro in SPSS, which was designed to examine relationships between predictor and outcome variables as conditioned by moderating variables (Hayes, 2018). The macro uses ordinary least squares regression to compute the conditional effects at the levels of the moderator previously stated.
2. Results
Table 1 displays the means, standard deviations, and bivariate correlations among study variables. An examination of the correlations demonstrated that gender (r = 0.14, p = .005) and tenure (r = −0.20, p < .001) were both significantly related to willingness to work with patients who misuse opioids such that women and physicians with less tenure reported greater willingness. Further, bias (r = −0.60, p < .001), burnout (r = −0.29, p < .001), stress induced by working with patients who misuse opioids (r = −0.41, p < .001), and contact (r = 0.32, p < .001) were significantly correlated with willingness to work with patients who misuse opioids. These findings suggest that physicians report lower willingness to work with this patient population when they are more biased and experience more burnout and stress when working with these patients. Of interest, the bivariate relationship between contact and willingness to work with patients who misuse opioids was significant and positive, suggesting the direct relationship indicates higher levels of contact is associated with greater willingness to work with patients who misuse opioids.
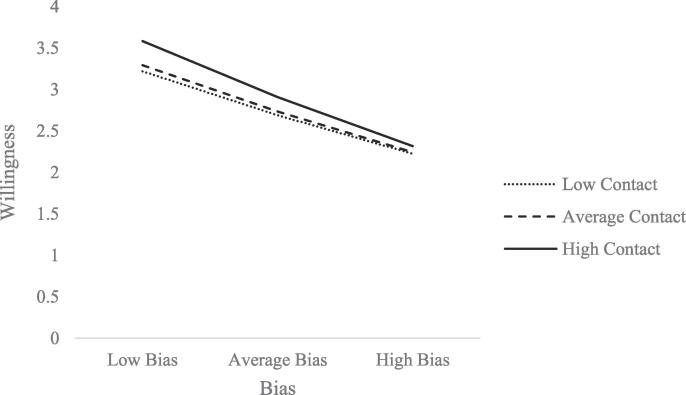
Table 2, Table 3, Table 4 display the results for our three regression models. Each model tested the relationship between bias, stress, or burnout and treatment willingness; the relationship between contact and treatment willingness; and the interaction between the predictor variable and contact. Results for Model 1, which examined the interaction between bias and contact, revealed a significant relationship between treatment willingness and tenure (b = −0.03, p < .001) in Step 1 and a significant relationship for bias (b = −0.76, p < .001) and contact (b = 0.01, p = .001) in Step 2. These findings suggest that bias decreases and contact increases willingness to work with patients who misuse opioids. We further found a significant interaction between bias and contact in Step 3 (b = −0.01, p = .033). To examine the nature of the interaction, we estimated the relationship between bias and treatment willingness at one standard deviation below the mean, the mean, and one standard deviation above the mean for contact. The interaction is depicted in Fig. 1. The conditional effects indicate the negative relationship between bias and willingness is strengthened as the amount of contact increased. The relationship between bias and willingness was b = −0.66 at one SD below the mean for contact, b = −0.70 at the mean of contact, and b = −0.84 at one SD above the mean for contact. The interaction demonstrates that the negative impact of bias on willingness to work with patients who misuse opioids is exacerbated by increased contact with these patients.
Table 2.
Regression analyses examining the interaction between bias and contact.
| Step 1 |
Step 2 |
Step 3 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | B | SE | 95% CI | B | SE | 95% CI | B | SE | 95% CI |
| Gender | 0.182 | 0.121 | −0.055, 0.420 | 0.126 | 0.096 | −0.063, 0.315 | 0.137 | 0.096 | −0.052, 0.325 |
| Age | 0.010 | 0.006 | −0.002, 0.023 | 0.001 | 0.005 | −0.009, 0.011 | −0.002 | 0.005 | −0.012, 0.009 |
| Work hours | −0.006 | 0.004 | −0.014, 0.001 | 0.001 | 0.003 | −0.005, 0.007 | 0.001 | 0.003 | −0.004, 0.007 |
| Tenure | −0.027*** | 0.007 | −0.040, −0.013 | −0.008 | 0.006 | −0.019, 0.003 | −0.006 | 0.006 | −0.018, 0.005 |
| Current Prescribing | −0.181 | 0.160 | −0.496, 0.133 | −0.050 | 0.128 | −0.301, 0.201 | −0.082 | 0.128 | −0.334, 0.169 |
| Past Prescribing | 0.252 | 0.300 | −0.338, 0.842 | 0.045 | 0.239 | −0.425, 0.516 | 0.090 | 0.239 | −0.379, 0.560 |
| R2 = 0.075 | |||||||||
| Bias | −0.761*** | 0.065 | −0.888, −0.634 | −0.627*** | 0.090 | −0.803, −0.450 | |||
| Contact | 0.012*** | 0.002 | 0.007, 0.016 | 0.030** | 0.009 | 0.012, 0.047 | |||
| R2 (ΔR2) = 0.418 (0.344) | |||||||||
| Bias * Contact | −0.007* | 0.003 | −0.014, −0.001 | ||||||
| R2 (ΔR2) = 0.427 (0.009) | |||||||||
Note: N = 316; * p < .05, ** p < .01, *** p < .001.
Table 3.
Regression analyses examining the interaction between stress and contact.
| Step 1 |
Step 2 |
Step 3 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | B | SE | 95% CI | B | SE | 95% CI | B | SE | 95% CI |
| Gender | 0.178 | 0.120 | −0.058, 0.414 | 0.178 | 0.100 | −0.018, 0.374 | 0.202 | 0.099 | 0.007, 0.397 |
| Age | 0.009 | 0.006 | −0.004, 0.021 | −0.002 | 0.005 | −0.013, 0.008 | −0.003 | 0.005 | −0.014, 0.007 |
| Work hours | −0.007 | 0.004 | −0.014, 0.000 | −0.002 | 0.003 | −0.008, 0.004 | −0.002 | 0.003 | −0.008, 0.004 |
| Tenure | −0.025*** | 0.007 | −0.038, −0.012 | −0.008 | 0.006 | −0.020, 0.003 | −0.009 | 0.006 | −0.020, 0.003 |
| Current Prescribing | −0.179 | 0.160 | −0.493, 0.136 | −0.319* | 0.134 | −0.582, −0.056 | −0.343 | 0.133 | −0.604, −0.081 |
| Past Prescribing | 0.240 | 0.300 | −0.350, 0.831 | 0.288 | 0.249 | −0.202, 0.778 | 0.319 | 0.247 | −0.166, 0.805 |
| R2 = 0.071 | |||||||||
| Stress | −0.417*** | 0.041 | −0.498, −0.336 | −0.307*** | 0.058 | −0.421, −0.194 | |||
| Contact | 0.017*** | 0.003 | 0.012, 0.002 | 0.033*** | 0.006 | 0.020, 0.045 | |||
| R2 (ΔR2) = 0.365 (0.293) | |||||||||
| −0.005** | 0.002 | −0.009, −0.001 | |||||||
| Stress * Contact | |||||||||
| R2 (ΔR2) = 0.379 (0.014) | |||||||||
Note: N = 321; * p < .05, ** p < .01, *** p < .001.
Table 4.
Regression analyses examining the interaction between burnout and contact.
| Step 1 |
Step 2 |
Step 3 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | B | SE | 95% CI | B | SE | 95% CI | B | SE | 95% CI |
| Gender | 0.190 | 0.121 | −0.049, 0.429 | 0.190 | 0.053 | −0.025, 0.404 | 0.201 | 0.109 | −0.013, 0.414 |
| Age | 0.007 | 0.006 | −0.005, 0.019 | −0.004 | 0.268 | −0.015, 0.008 | −0.005 | 0.006 | −0.016, 0.007 |
| Work hours | −0.007* | 0.004 | −0.015, 0.000 | −0.002 | 0.002 | −0.009, 0.005 | −0.003 | 0.003 | −0.010, 0.004 |
| Tenure | −0.023** | 0.007 | −0.037, −0.010 | −0.010 | 0.017 | −0.023, 0.003 | −0.010 | 0.006 | −0.023, 0.003 |
| Current Prescribing | −0.119 | 0.163 | −0.440, 0.202 | −0.186 | 0.080 | −0.476, 0.103 | −0.172 | 0.146 | −0.460, 0.117 |
| Past Prescribing | 0.205 | 0.301 | −0.388, 0.797 | 0.197 | 0.063 | −0.335, 0.729 | 0.214 | 0.269 | −0.315, 0.743 |
| R2 = 0.071 | |||||||||
| Burnout | −0.433*** | 0.067 | −0.565, −0.301 | −0.282** | 0.097 | −0.473, −0.091 | |||
| Contact | 0.018*** | 0.003 | 0.013, 0.024 | 0.033*** | 0.007 | 0.019, 0.047 | |||
| R2 (ΔR2) = 0.256 (0.185) | – | ||||||||
| Burnout * Contact | −0.007* | 0.003 | −0.013, −0.001 | ||||||
| R2 (ΔR2) = 0.267 (0.011) | |||||||||
Note: N = 313; * p < .05, ** p < .01, *** p < .001.
Fig. 1.
Interaction of Bias and Contact Predicting Treatment Willingness.
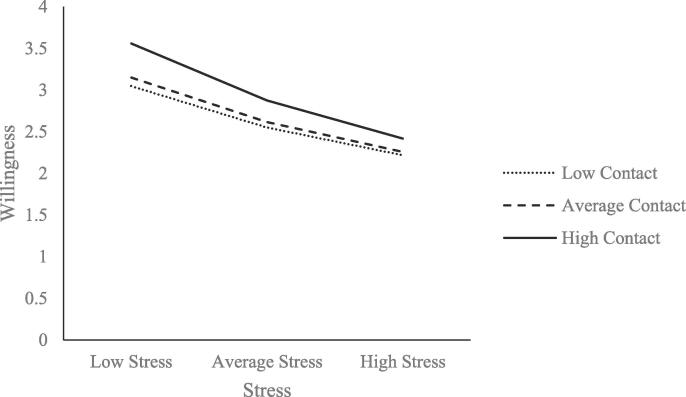
Results for Model 2, which assessed the relationships between stress, contact, and treatment willingness, were similar. There were significant relationships between treatment willingness and stress (b = −0.42, p < .001) and contact (b = 0.02, p < .001) such that stress decreased and contact increased treatment willingness. There was also a significant interaction between stress and contact (b = −0.01, p = .008). The nature of the interaction is depicted in Fig. 2. The conditional effects suggest the relationship between stress and willingness is stronger when contact is higher rather than lower (b = −0.33 at one SD below the mean for contact, b = −0.36 at the mean for contact, and b = −0.46 at one SD above the mean for contact). The interaction again suggests that the negative impact of stress on treatment willingness is the strongest when physicians have higher contact with patients who misuse opioids.
Fig. 2.
Interaction of Stress and Contact Predicting Treatment Willingness.
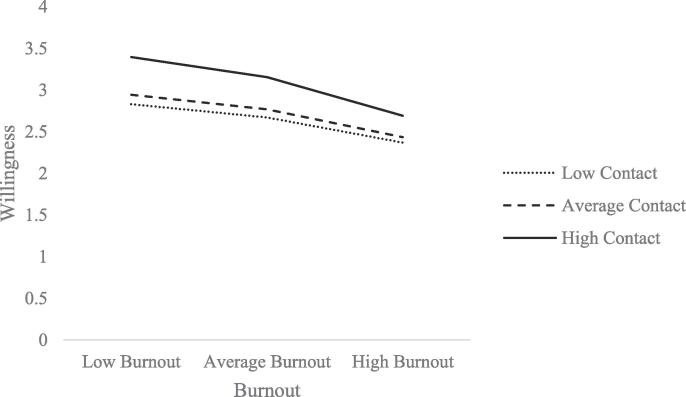
Finally, Model 3 tested the effects of burnout and contact on willingness to work with patients who misuse opioids. Results demonstrated a significant effect for burnout (b = −0.43, p < .001) and for contact (b = 0.02, p < .001) such that burnout decreases and contact increases treatment willingness. The model also demonstrated a significant interaction between burnout and contact (b = −0.01, p = .033). The interaction is shown in Fig. 3. Similar to the previous models, the conditional effects for the relationship between burnout and willingness were strongest when contact was at one SD above the mean (b = −0.48) rather than at the mean (b = −0.35) or at one SD below the mean (b = −0.32). This suggests that, as contact with patients who misuse opioids increases, the negative relationship between burnout and willingness to work with these patients becomes stronger.
Fig. 3.
Interaction of Burnout and Contact Predicting Treatment Willingness.
3. Discussion
The goal of this study was to reexamine the role of intergroup contact in predicting physician attitudes toward patients who misuse opioids and our findings both support and challenge prevailing assumptions about contact. In support of the beneficial role of contact, we find that contact has a positive direct relationship with physician willingness to work with patients who misuse opioids. However, we also find that contact interacts with bias, burnout, and stress induced by working with these patients such that increased contact strengthened the negative relationship between bias, burnout, and stress and physicians’ willingness to work with patients who misuse opioids. Indeed, we found that the conditional negative effects of bias, stress, and burnout on willingness to work with patients who misuse opioids were the strongest when levels of contact were high. This finding thus qualifies prior work on contact by demonstrating that, at least under certain conditions, contact may not improve physicians’ willingness to treat patients who misuse opioids (Brener et al., 2007). Conversely, contact may actually heighten the effects of bias, burnout, and stress, perhaps because these physician-patient interactions may be seen as aversive. In the context of the U.S. opioid epidemic when physicians may see an increase in patients who misuse opioids, increasing contact in the absence of specific interventions to reduce stress, burnout, and bias, may not produce the expected positive impacts on patient outcomes.
4. Implications
Our results have implications for policy and future research. Specifically, our findings suggest the need for policymakers and researchers to carefully consider that interventions which increase contact between physicians and patients who misuse opioids may not produce the positive effects one might expect, at least for physicians experiencing high levels of bias, burnout, or stress. In the same way, interventions may not be successful in the absence of efforts to address underlying stigma toward patients who misuse opioids or resulting physician strain. This suggests a need to improve current intervention and training methods by also focusing on engendering positive appraisals of working with patients who misuse opioids (e.g., reinforcing the positive impact of reducing opioid dependence for the patient and overall public health) or providing support to physicians to mitigate the strain they experience when working with these patients.
Our findings also suggest a need for future research to more critically evaluate the role of contact in determining physician attitudes by discerning the types of contact that may reduce negative attitudes and the types of contact that may be ineffective or even harmful. Future research should also build on these findings to better contextualize the role of contact in relation to other physician experiences and perceptions. In particular, the design of future interventions would benefit from attempts to identify specific aspects of interactions with patients who misuse opioids that heighten the negative effects of bias, burnout, and stress. For example, recent work has found that having a personal relationship with someone who injects drugs (Broady et al., 2020) and exposure to narrative accounts of a person who injects drugs’ lived experiences (Broady et al., 2021) are associated with reduced prejudice, suggesting that these particular forms of contact may be beneficial. Health care organizations may therefore attempt to foster interactions between providers and patients who misuse opioids that replicate these types of contact.
The recommendation to identify more targeted contact-based interventions also aligns with previous calls for research to better identify the factors which alter the effects of intergroup contact and reduce its positive benefits (Pettigrew & Tropp, 2008). Thus, in addition to providing patients who misuse opioids with affirming health care services, identifying the types of contact that most successfully alleviate prejudice can also contribute to our theoretical understanding of intergroup contact. Finally, future research would also benefit from exploring the types of social and organizational support that can help to mitigate stress, burnout, and bias toward patients who misuse opioids. Doing so may bolster the positive impact of contact with patients who misuse opioids and would have more general benefits for health care providers, such as increasing job satisfaction, reducing turnover intentions (Duraisingam et al., 2009; von Hippel et al., 2008), and increasing the quality of clinical care (Oser et al., 2013). Research on alcohol and drug counselors suggest that interventions which focus on increasing organizational support (Leykin, Cucciare, & Weingardt, 2011) and acceptance and commitment training (Hayes et al., 2004) can successfully reduce burnout, and organizations may therefore consider incorporating these approaches into their efforts to improve treatment quality and access for patients who misuse opioids.
5. Limitations and future directions
There are limitations of the current study that should be acknowledged. First, our data were collected in a cross-sectional survey of physician attitudes and thus do not enable us to draw conclusions about directionality or causality. Some research has demonstrated that contact can reduce subsequent prejudicial attitudes, but prejudicial attitudes also reduce subsequent contact.17 Thus, it is important that future studies use time-lagged designs to better estimate the magnitude and directionality of the relationship between contact and attitudes. Further, we collected data from physicians working within Ohio, which has been one of the states most affected by the opioid epidemic. As such, physicians in this context may have had more pronounced negative interactions with patients who misuse opioids which may not reflect the experiences of physicians working in other contexts.
Further, the language used to recruit physicians to the survey (i.e., the mention of the opioid crisis) may have influenced responses by priming physicians to reflect on negative attitudes and/or experiences. Relatedly, the survey items used the terms “opioid misuse/opioid misusers” which may have similarly affected physicians’ responses. We chose this terminology to distinguish between prescription use of opioids and non-prescription use, the latter of which is typically labeled “misuse” (e.g., Brady, McCauley, & Back, 2016). However, it is possible that “misuse” activated thoughts of more severe forms of nonmedical opioid use or was stigmatizing itself since it did not use the preferred person-first language. Research is needed to better understand the impact of such terminology on physicians’ perceptions and survey responses.
Finally, our study examined physicians’ general attitudes toward people who misuse opioids and future research would benefit from differentiating between or among different forms of opioid use. For example, physicians may have different experiences with or hold unique biases toward patients who inject opioids as compared to patients who use other forms of opioids (e.g., prescription opioids) (Kennedy-Hendricks et al., 2017, McCradden et al., 2019). Subsequent studies could examine whether there are differences in treatment willingness, bias, and experienced stress related to different groups of patients who use opioids, whether physicians’ appraisals of their contact with each group varies, and the degree to which experiences with one group of patients who use opioids (or even other substances) influences perceptions about others.
6. Conclusion
In light of research demonstrating the damaging effects of physician bias toward patients who misuse opioids, an increasing number of studies have sought to design interventions to improve physicians’ attitudes toward this patient population. Increased intergroup conflict has been among the most commonly used intervention methods, but recent findings have begun to challenge the effectiveness of this intervention strategy. Our study revisited the role of contact and found that contact can decrease physicians’ willingness to work with patients who misuse opioids when it occurs under strained conditions, such as when physicians have prejudicial attitudes toward patients who misuse opioids or are experiencing burnout or stress. It is critical to understand and address the barriers that limit physician willingness to work with patients who misuse opioids because of the important implications of such attitudes for patients’ access to quality health care services. As such, these findings demonstrate a timely need to differentiate between positive and negative intergroup contact and carefully consider the types of contact that will improve both physician and patient outcomes.
CRediT authorship contribution statement
Lindsay Y. Dhanani: Conceptualization, Methodology, Investigation, Resources, Formal analysis, Data curation, Writing – original draft. Berkeley Franz: Conceptualization, Methodology, Investigation, Writing – review & editing. Taylor K. Hall: Formal analysis, Data curation, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We wish to acknowledge Lee Ann Williams and the Clinical and Translational Research Unit at Ohio University who provided assistance with recruitment for the study.
Contributor Information
Lindsay Y. Dhanani, Email: dhanani@ohio.edu.
Berkeley Franz, Email: franzb@ohio.edu.
Taylor K. Hall, Email: th215116@ohio.edu.
References
- Aberson C.L. Positive intergroup contact, negative intergroup contact, and threat as predictors of cognitive and affective dimensions of prejudice. Group Processes & Intergroup Relations. 2015;18(6):743–760. doi: 10.1177/1368430214556699. [DOI] [Google Scholar]
- Allport G.W. Addison-Wesley; Cambridge, MA: 1954. The nature of prejudice. [Google Scholar]
- Barlow F.K., Paolini S., Pedersen A., Hornsey M.J., Radke H.R.M., Harwood J.…Sibley C.G. The contact caveat: Negative contact predicts increased prejudice more than positive contact predicts reduced prejudice. Personality and Social Psychology Bulletin. 2012;38(12):1629–1643. doi: 10.1177/0146167212457953. [DOI] [PubMed] [Google Scholar]
- Brady K.T., McCauley J.L., Back S.E. Prescription opioid misuse, abuse, and treatment in the United States: An update. American Journal of Psychiatry. 2016;173(1):18–26. doi: 10.1176/appi.ajp.2015.15020262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brener L., Hippel W.V., Kippax S., Preacher K.J. The role of physician and nurse attitudes in the health care of injecting drug users. Substance Use and Misuse. 2010;45(7–8):1007–1018. doi: 10.3109/10826081003659543. [DOI] [PubMed] [Google Scholar]
- Brener L., von Hippel W. Measuring attitudes toward injecting drug users and people with hepatitis C. Substance Use and Misuse. 2008;43(3–4):295–302. doi: 10.1080/10826080701202627. [DOI] [PubMed] [Google Scholar]
- Brener L., von Hippel W., Kippax S. Prejudice among health care workers toward injecting drug users with hepatitis C: Does greater contact lead to less prejudice? International Journal of Drug Policy. 2007;18(5):381–387. doi: 10.1016/j.drugpo.2007.01.006. [DOI] [PubMed] [Google Scholar]
- Broady T.R., Brener L., Cama E., Hopwood M., Treloar C. Stigmatising attitudes towards people who inject drugs, and people living with bloor borne viruses or sexually transmissible infections in a representative sample of the Australian population. Plos ONE. 2020;15 doi: 10.1371/journal.pone.0232218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broady T.R., Brener L., Vuong T., Cama E., Treloar C. Online interventions to reduce stigma towards population groups affected by bloor borne viruses in Australia. International Journal of Drug Policy. 2021;103292 doi: 10.1016/j.drugpo.2021.103292. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2020, March 19). Understanding the Epidemic | Drug Overdose | CDC Injury Center. Retrieved January 21, 2021, from https://www.cdc.gov/drugoverdose/epidemic/index.html.
- Crapanzano K., Vath R.J., Fisher D. Reducing stigma towards substance users through an educational intervention: Harder than it looks. Academic Psychiatry. 2014;38(4):420–425. doi: 10.1007/s40596-014-0067-1. [DOI] [PubMed] [Google Scholar]
- Duraisingam V., Pidd K., Roche A.M. The impact of work stress and job satisfaction on turnover intentions: A study of Australian specialist alcohol and other drug workers. Drugs: Education, Prevention and Policy. 2009;16:217–231. doi: 10.1080/09687630902876171. [DOI] [Google Scholar]
- Elman B.D., Dowd E.T. Correlates of burnout in inpatient substance abuse treatment therapists. Journal of Addictions & Offender Counselling. 1997;17:56–65. [Google Scholar]
- Gilchrist G., Moskalewicz J., Slezakova S., Okruhlica L., Torrens M., Vajd R., Baldacchino A. Staff regard towards working with substance users: a European multi-centre study. Addiction. 2011;106(6):1114–1125. doi: 10.1111/j.1360-0443.2011.03407.x. [DOI] [PubMed] [Google Scholar]
- Hagemeier N.E. Introduction to the opioid epidemic: The economic burden on the healthcare system and impact on quality of life. The American Journal of Managed Care. 2018;24:S200–S206. NLM (Medline) [PubMed] [Google Scholar]
- Hayes, A. F. (2018). Introduction to Mediation, Moderation, and Conditional Process Analysis, Second Edition: A Regression-Based Approach.
- Hayes S.C., Bissett R., Roget N., Padilla M., Kohlenberg B.S., Fisher G.…Niccolls R. The impact of acceptance and commitment training and multicultural training on the stigmatizing attitudes and professional burnout of susbtance abuse counselors. Behavioral Therapy. 2004;35:821–835. [Google Scholar]
- Hedegaard, H., Minino, A. M., & Warner, M. (2020). Drug Overdose Deaths in the United States, 1999–2018. [PubMed]
- Corp I.B.M. IBM Corp; Armonk, NY: 2020. SPSS Statistics for Windows, Version 27. [Google Scholar]
- Kennedy-Hendricks A., Barry C.L., Gollust S.E., Ensminger M.E., Chisolm M.S., McGinty E.E. Social stigma toward persons with prescription opioid use disorder: Associations with public support for punitive and public health-oriented policies. Psychiatric Services. 2017;68(5):462–469. doi: 10.1176/appi.ps.201600056. [DOI] [PubMed] [Google Scholar]
- Knudsen H.K., Ducharme L.J., Roman P.M. Counselor emotional exhaustion and turnover intention in therapeutic communities. Journal of Substance Abuse Treatment. 2006;31(2):173–180. doi: 10.1016/j.jsat.2006.04.003. [DOI] [PubMed] [Google Scholar]
- Kristensen T.S., Borritz M., Villadsen E., Christensen K.B. The Copenhagen Burnout Inventory: A new tool for the assessment of burnout. Work and Stress. 2005;19(3):192–207. doi: 10.1080/02678370500297720. [DOI] [Google Scholar]
- Leykin Y., Cucciare M.A., Weingardt K.R. Differential effects of online training on job-related burnout among substance abuse counsellors. Journal of Substance Use. 2011;16(2):127–135. [Google Scholar]
- Livingston J.D., Milne T., Fang M.L., Amari E. The effectiveness of interventions for reducing stigma related to substance use disorders: A systematic review. Addiction. 2012;107(1):39–50. doi: 10.1111/j.1360-0443.2011.03601.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd C. The stigmatization of problem drug users: A narrative literature review. Drugs: Education, Prevention and Policy. 2013;20(2):85–95. doi: 10.3109/09687637.2012.743506. [DOI] [Google Scholar]
- McCradden M.D., Vasileva D., Orchanian-Cheff A., Buchman D.Z. Ambiguous identities of drugs and people: A scoping review of opioid-related stigma. International Journal of Drug Policy. 2019;74:205–215. doi: 10.1016/j.drugpo.2019.10.005. [DOI] [PubMed] [Google Scholar]
- Oser C.B., Biebel E.P., Pullen E., Harp K.L.H. Causes, consequences, and prevention of burnout among susbtance abuse treatment counselors: A rural versus urban comparison. Journal of Psychopactive Drugs. 2013;45:17–27. doi: 10.1080/02791072.2013.763558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettigrew T.F., Tropp L.R. A meta-analytic test of intergroup contact theory. Journal of Personality and Social Psychology. 2006;90(5):751–783. doi: 10.1037/0022-3514.90.5.751. [DOI] [PubMed] [Google Scholar]
- Pettigrew T.F., Tropp L.R. How does intergroup contact reduce prejudice? Meta-analytic tests of three mediators. European Journal of Social Psychology. 2008;38(6):922–934. doi: 10.1002/ejsp.v38:610.1002/ejsp.504. [DOI] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2017). Key substance use and mental health indicators in the United States: Results from the 2016 National Survey on Drug Use and Health. Available at https://www.samhsa.gov/data/sites/default/files/NSDUH-FFR1-2016/NSDUH-FFR1-2016.pdf.
- van Boekel L.C., Brouwers E.P.M., van Weeghel J., Garretsen H.F.L. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: Systematic review. Drug and Alcohol Dependence. 2013;131(1-2):23–35. doi: 10.1016/j.drugalcdep.2013.02.018. [DOI] [PubMed] [Google Scholar]
- Vilardaga R., Luoma J.B., Hayes S.C., Pistorello J., Levin M.E., Hildebrandt M.J.…Bond F. Burnout among the addition counseling workforce: The differential roles of mindfulness and values-based processes and work-site factors. Journal of Substance Abuse Treatment. 2011;40:323–335. doi: 10.1016/j.jsat.2010.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Hippel W., Brener L., von Hippel C. Implicit prejudice toward injecting drug users predicts intentions to change jobs among drug and alcohol nurses. Psychological Science. 2008;19(1):7–11. doi: 10.1111/j.1467-9280.2008.02037.x. [DOI] [PubMed] [Google Scholar]