Highlights
-
•
Peer support specialists effectively screen patients for substance use disorder.
-
•
Utilizing peer support specialists enhanced feasibility medication initiation.
-
•
Emergency room-initiated medication connects patients to treatment.
Keywords: Peer support specialists, Buprenorphine, Emergency department, Medication for opioid use disorder
Abstract
Introduction
Evidence suggests emergency department (ED)-initiated buprenorphine as efficacious in connecting ED patients to Medications for Opioid Use Disorder (MOUD) utilizing peer support specialists (PSS). However, there are no reports of implementation of ED-initiated buprenorphine in practice. Such information is crucial to support the adoption of ED-initiated buprenorphine.
Methods
In this quality improvement pilot study, a PSS screened ED patients over age 18 with the Tobacco, Alcohol, Prescription medication, and other Substance use – 1 (TAPS-1). The PSS considered the patient a positive screen if the patient met the following criteria: risky weekly alcohol use, illicit drugs, or prescription drugs. For patients who screened positive, the PSS delivered a brief intervention and assessed interest in treatment. An ED clinician assessed patients who screened positive for heroin/opioid use and were interested in treatment for buprenorphine induction.
Results
From January through June 2019, 1037 patients were screened for risky substance use, and, of these, 238 (23%) screened positive. The distribution of primary substance used was: 51% alcohol, 26% cannabis, 7.5% cocaine, 7.5% heroin, and 3.3% prescription opioids. Of the 23 patients who screened positive for heroin/opioid use and requested treatment, seven were admitted to the hospital. Of the remaining 16 patients, 14 patients wanted buprenorphine treatment, seven were provided buprenorphine in the ED, and four of these attended their intake appointments for community-based MOUD treatment.
Conclusion
ED-initiated buprenorphine facilitated by a PSS is feasible and requires coordination and planning. Approaches to ED-initiated buprenorphine that screen only for opioid use will miss many patients interested in substance use treatment.1
1. Introduction
The emergency department (ED) is an important site for detecting and treating opioid use disorder (OUD) (Martin, Mitchell, Wakeman, White, & Raja, 2018). A randomized controlled trial found that ED patients with OUD who received buprenorphine had a higher engagement in addiction treatment post-discharge (Martin et al., 2018). This study also observed lower self-reported illicit opioid use 30 days after discharge compared to patients who only received a brief intervention and referral to treatment (D’Onofrio et al., 2015). Despite these promising findings, clinical practice lags. A Massachusetts cohort study found that less than 1/3 of individuals with hospital encounters for nonfatal opioid overdose received Medication for OUD (MOUD) in the 12 months after discharge (Larochelle et al., 2018). This low rate of MOUD after opioid overdose suggests ED-initiated buprenorphine is far from widespread. MOUD stands as a life-saving measure for treating OUD, of which engagement in treatment may prevent patients from requiring ED services in the future. Further, MOUD is known to reduce opioid overdoses, making it an ideal choice to be initiated in the ED setting (Morgan, Schackman, Weinstein, Walley, & Linas, 2019). Information about implementation is crucial for ED administrators and providers to assess the feasibility of ED-initiated buprenorphine.
Having a peer support specialist (PSS) as a medical team member presents a promising access point to increase ED-initiated buprenorphine (McGuire et al., 2020). The PSS has lived experience with substance use and recovery and engages the patient as a peer. Recent literature names the PSS as a promising team member who can identify persons living with OUD and provide psychosocial support. Further, PSS have shown to be a promising practice in identifying patients with OUD who present in the ED (Monico et al., 2020).
We report on a quality improvement initiative to provide ED-initiated buprenorphine utilizing a universal screening approach combined with a brief intervention delivered by a PSS in a large ED. The project focus includes universal screening for substance misuse in an ED setting, a patient's interest in treatment, ED-initiated buprenorphine induction, and linkage to OUD treatment.
2. Materials and methods
2.1. Design
This quality improvement project implemented a screening, brief intervention, referral to treatment, and ED-initiated buprenorphine in the University of North Carolina (UNC) ED located in Chapel Hill, North Carolina (NC). An interdisciplinary team was convened, including system administrators, nurses, clinicians, PSSs, pharmacists, and addiction specialists. The team chose a screening modality, developed a brief assessment intervention, identified community partners for treatment referral, developed an ED-initiated buprenorphine prescription algorithm, and created a project workflow.
We excluded the psychiatric emergency department to increase the generalizability of this quality improvement project's results. The team conducted trainings for nursing staff and offered DATA 2000 DEA waiver training for ED clinicians. Due to the quality improvement nature of this project, we applied for and received exempt status from the UNC Institutional Review Board for Human Subject Research.
2.2. Setting and population
The UNC ED is a level I trauma center, seeing approximately 175 patients daily. From 2016 to 2017, the opioid overdose death rate in NC increased by 29%, faster than in any other state (Scholl, Seth, Kariisa, Wilson, & Baldwin, 2019). While preliminary data suggest the NC opioid overdose death rate decreased slightly in 2018 and 2019 (Ahmad, Rossen, & Sutton, 2021), the state experienced a 24% increase in ED visits for opioid overdoses in 2020. The majority of these patients are between the ages of 25 and 34 and are uninsured. NC is one of 14 states that has not adopted Medicaid expansion (North Carolina Emergency Department (ED) Visits For Opioid Overdose: October 2020, 2020; Status of State Action on the Medicaid Expansion Decision, 2020).
2.3. Project protocol
The PSS worked 20 h per week during daytime hours. After ED triage, the PSS screened patients over age 18 with the Tobacco, Alcohol, Prescription medication, and other Substance use – 1 (TAPS-1) tool. The PSS moved sequentially room to room through the ED, offering to screen all patients cognitively able to respond. The project held no criteria to prioritize patients for screening.
When patients screened positive, the PSS delivered a brief intervention, including assessment of patient's drug of choice, stage of change, and interest in treatment. If the PSS assessed the drug of choice as opioids or heroin, the PSS notified the ED case manager and pharmacist. The case manager coordinated a referral to treatment while the pharmacist ensured the patient received a naloxone prescription and patient education regarding MOUD. The ED clinician was notified for assessment of whether to initiate buprenorphine. For those who screened positive for alcohol or other non-opioid substances, the PSS assessed their readiness for change and connected interested patients with resources for treatment.
2.4. Data collection and analyses
The PSS documented the outcome of the screening and brief intervention. The project team followed patients who received ED-initiated buprenorphine and referral for MOUD treatment to ensure connection to outpatient treatment. Results were summarized using descriptive statistics.
3. Results
The PSS provided screening and brief intervention for approximately 20 patients over an 8-hour period. From January through June 2019, the PSS screened 1037 patients. Table 1 describes the frequency of reported substance use by category from the TAPS-1 screen.
Table 1.
Frequency of Substance Use from TAPS-1 Screening.
| Substance misuse screening (N = 1037) |
||||
|---|---|---|---|---|
| Tobacco | Alcohol | Illicit drug | Prescription drug | |
| Daily or almost daily | 20% (308) | 5.5% (57) | 7.1% (74) | 1.7% (18) |
| Weekly | 3.0% (31) | 7.8% (81) | 6.4% (66) | 1.5% (15) |
| Monthly | 1.9% (20) | 4.9% (51) | 2.7% (28) | 1.0% (10) |
| Less than monthly | 5.7% (59) | 15% (156) | 7.3% (76) | 2.5% (26) |
| Never | 58% (605) | 63% (650) | 72% (749) | 91% (942) |
| Did not respond | 1.4% (14) | 4.1% (42) | 4.2% (44) | 2.5% (26) |
Description: The TAPS-1 screening tool asks respondents about frequency of use in the past year of any tobacco or nicotine delivery product, use of 5 or more alcoholic drinks for men in a day and 4 or more alcohol drinks for women in a day, use of prescription medications for nonmedical purposes, and use of drugs such as marijuana, cocaine or crack, heroin, methamphetamine (crystal meth), hallucinogens, and ectasy/MDMA.
Of all patients screened, 260 indicated at least weekly risky alcohol use, illicit drugs, or prescription drugs. Fifty-six percent (1 3 3) of patients presented to the ED with a physical chief complaint rather than a psychiatric or substance-related complaint. Forty- two percent of patients who screened positive had no insurance (100 patients). Alcohol was the primary substance used for 51% (122 patients) and heroin or opioid misuse was the primary substance for 11% (23 patients). All patients who screened positive for heroin or opioid misuse were prioritized, regardless if heroin/opioids was listed as their primary or secondary substance.
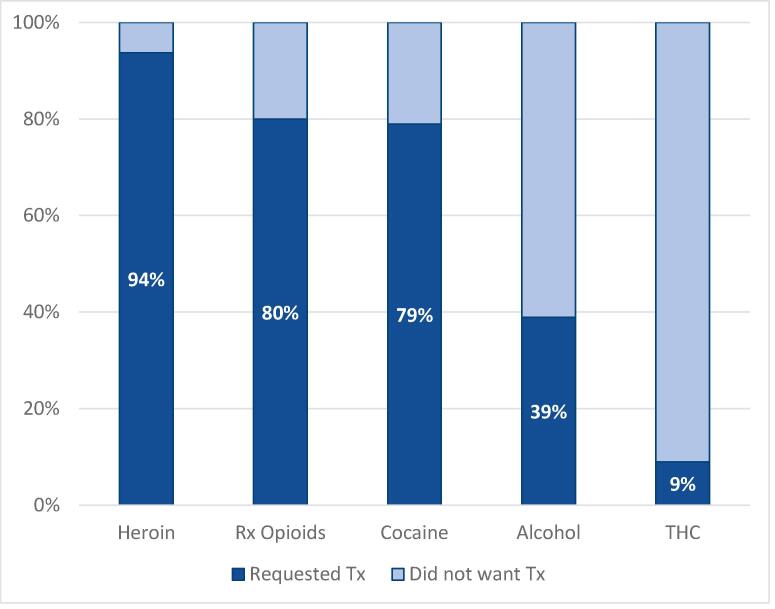
Patients whose primary substance was heroin were the most likely to request OUD treatment (Fig. 1). Twenty-three patients screened positive for heroin/opioid use and requested treatment. Seven were admitted to the hospital. Of the remaining 16 patients, 14 requested MOUD. Of those who requested MOUD, seven were provided buprenorphine in the ED, and four of these attended their intake appointment for MOUD treatment.
Fig. 1.
Request for treatment per substance used. Description: Those who screened positive for opioids and heroin were more likely to request treatment than those who screened positive for other substances.
4. Discussion
ED-initiated buprenorphine was feasible in practice, requiring substantial resources, planning, and coordination. An essential aspect of this feasibility was the PSS presence in the ED. Coordinating with a pharmacist, a case manager, and an ED clinician, the PSS screened approximately 148 patients for every one patient who received ED-initiated buprenorphine. Through this screening, we were able to identify those with present substance use that may have otherwise gone unnoticed, initiated buprenorphine, and connect patients to treatment.
We chose the TAPS-1 screen because of its brevity, the breadth of substances covered, and its validation in a primary care population (Gryczynski et al., 2017), although no studies exist that state the ideal TAPS-1 cutoffs for ED settings. Patients self-administered the TAPS-1 screen due to evidence of higher disclosure rates with self-administered versus interview-administered screening (Gryczynski et al., 2017). Because research shows ED patients have a high prevalence of SUDs (Macias Konstantopoulos et al., 2014, Rockett et al., 2003), we used higher cutoffs for a positive screen than primary care to target the highest need patient and to avoid overwhelming ED resources. At least weekly risky alcohol use, illicit drugs, or prescription drugs was considered a positive screen.
Consistent with previous research, the PSS is uniquely positioned to connect with patients on a personal level (Monico et al., 2020). The PSS's ability to have prolonged engagement with patients allowed for better screening. We hypothesize that the PSS positively impacted the patient's engagement with continued treatment. Future research should explore the impact of ED-based PSS in patient engagement with OUD treatment.
Some important limitations should be noted. Many patients who screened positive were interested in treatment, even though their presenting ED complaints were not SUD-related, indicating the importance of general screening for all ED patients. Of those who requested MOUD, only 50% were initiated on buprenorphine. We hypothesize this reduced initiation as a result of two factors. First, a DEA waivered provider may not have been present during that ED shift. Second, providers may not have initiated buprenorphine if they could not acquire a follow-up appointment for the patient within seven days of the ED visit. Further, ED screening approaches focused only on OUD will miss many patients interested in substance use treatment. Future research should assess these limitations.
Consistent with previous research, our results suggest a high burden of undiagnosed and untreated SUDs exists among ED patients (Hawk & D’Onofrio, 2018). Our screening underestimates the prevalence of SUDs in the ED setting, given the high cutoffs utilized. Lowering cutoffs would require a more significant investment of ED resources to assess patients who screen positive. Research is needed to develop implementation strategies for ED-initiated buprenorphine to better support the widespread adoption of this promising approach. Research on improving patients' openness to MOUD and improving the connection from ED to community MOUD are also needed.
CRediT authorship contribution statement
Alex K. Gertner: Methodology, Writing – original draft. Kate E. Roberts: Writing – review & editing. Grayson Bowen: Data curation. Brenda L. Pearson: Conceptualization, Investigation, Data curation, Methodology, Project administration. Robyn Jordan: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Supervision, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
This work was supported by North Carolina Department of Human Health Services, Division of Public Health, Injury and Violence Prevention Branch.
This work was supported by North Carolina Department of Human Health Services, Division of Public Health, Injury and Violence Prevention Branch.
Contributor Information
Alex K. Gertner, Email: alex_gertner@med.unc.edu.
Kate E. Roberts, Email: kate_roberts@med.unc.edu.
Grayson Bowen, Email: grayson_bowen@med.unc.edu.
Brenda L. Pearson, Email: brenda_pearson@med.unc.edu.
Robyn Jordan, Email: robyn_jordan@med.unc.edu.
References
- Ahmad, F. B., Rossen, L. M., & Sutton, P. (2021). Provisional drug overdose death counts. National Center for Health Statistics. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm.
- D’Onofrio G., O’Connor P.G., Pantalon M.V., Chawarski M.C., Busch S.H., Owens P.H.…Fiellin D.A. Emergency department-initiated buprenorphine/naloxone treatment for opioid dependence: A randomized clinical trial. JAMA. 2015;313(16):1636. doi: 10.1001/jama.2015.3474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gryczynski J., McNeely J., Wu L.-T., Subramaniam G.A., Svikis D.S., Cathers L.A.…Schwartz R.P. Validation of the TAPS-1: A four-item screening tool to identify unhealthy substance use in primary care. Journal of General Internal Medicine. 2017;32(9):990–996. doi: 10.1007/s11606-017-4079-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawk K., D’Onofrio G. Emergency department screening and interventions for substance use disorders. Addiction Science & Clinical Practice. 2018;13(1):18. doi: 10.1186/s13722-018-0117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larochelle M.R., Bernson D., Land T., Stopka T.J., Wang N.a., Xuan Z.…Walley A.Y. Medication for opioid use disorder after nonfatal opioid overdose and association with mortality: A cohort study. Annals of Internal Medicine. 2018;169(3):137. doi: 10.7326/M17-3107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macias Konstantopoulos W.L., Dreifuss J.A., McDermott K.A., Parry B.A., Howell M.L., Mandler R.N.…Weiss R.D. Identifying patients with problematic drug use in the emergency department: Results of a multisite study. Annals of Emergency Medicine. 2014;64(5):516–525. doi: 10.1016/j.annemergmed.2014.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin A., Mitchell A., Wakeman S., White B., Raja A. Emergency department treatment of opioid addiction: An opportunity to lead. Academic Emergency Medicine: Official Journal of the Society for Academic Emergency Medicine. 2018;25(5):601–604. doi: 10.1111/acem.2018.25.issue-510.1111/acem.13367. [DOI] [PubMed] [Google Scholar]
- McGuire A.B., Powell K.G., Treitler P.C., Wagner K.D., Smith K.P., Cooperman N.…Watson D.P. Emergency department-based peer support for opioid use disorder: Emergent functions and forms. Journal of Substance Abuse Treatment. 2020;108:82–87. doi: 10.1016/j.jsat.2019.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monico L.B., Oros M., Smith S., Mitchell S.G., Gryczynski J., Schwartz R. One million screened: Scaling up SBIRT and buprenorphine treatment in hospital emergency departments across Maryland. The American Journal of Emergency Medicine. 2020;38(7):1466–1469. doi: 10.1016/j.ajem.2020.03.005. [DOI] [PubMed] [Google Scholar]
- Morgan J.R., Schackman B.R., Weinstein Z.M., Walley A.Y., Linas B.P. Overdose following initiation of naltrexone and buprenorphine medication treatment for opioid use disorder in a United States commercially insured cohort. Drug and Alcohol Dependence. 2019;200:34–39. doi: 10.1016/j.drugalcdep.2019.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rockett I.R.H., Putnam S.L., Jia H., Smith G.S. Assessing substance abuse treatment need: A statewide hospital emergency department study. Annals of Emergency Medicine. 2003;41(6):802–813. doi: 10.1067/mem.2003.189. [DOI] [PubMed] [Google Scholar]
- Scholl, L., Seth, P., Kariisa, M., Wilson, N., & Baldwin, G. (2019). Drug and opioid-involved overdose deaths—United States, 2013–2017 (Vol. 67, pp. 9). [DOI] [PMC free article] [PubMed]