Abstract
Sleep disruption among adolescents represents a major public health concern, and social media use may play an important role in affecting sleep and subsequent mental health. While prior studies of youth sleep and mental health have often focused on social media use frequency and duration, adolescents’ emotional experiences related to social media have been underexplored, particularly among clinically acute populations. This study offers a preliminary investigation of associations among negative emotional experiences using social media, sleep disturbance, and clinical symptom severity in a sample of psychiatrically hospitalized youth. A sample of 243 adolescents (Mage = 15.34) completed self-report measures at a single time point. Measures assessed social media use, including frequency and duration, subjective experiences of use, and emotional responses to use, as well as sleep disturbance and clinical symptom severity, including suicidal ideation, internalizing symptoms, and attention problems. Results revealed that more frequent negative emotional responses to social media use were linked to greater sleep disturbance and higher clinical symptom severity. Furthermore, sleep disturbance mediated the relation between negative emotional responses to social media and clinical symptom severity. While gender differences were revealed in characteristics of social media use, sleep disturbance, and clinical outcomes, the associations among these constructs did not vary across gender groups. Overall, these findings highlight sleep disturbance as a potential mechanism through which negative emotional experiences on social media may impact clinical symptoms in psychiatrically vulnerable youth.
Keywords: adolescents, sleep, social media, suicidal ideation, internalizing symptoms, attention problems
Sleep plays a critical role in adolescent mental health, and sleep disruption in youth represents a major public health concern (Owens, 2014). Indeed, insufficient sleep has been linked to a wide range of adverse medical and psychiatric outcomes in adolescents, including increased depressive symptoms and suicide risk (Littlewood et al., 2019; Owens, 2014; Short & Weber, 2018). In recent years, adolescents’ use of digital devices and social media has increased exponentially (Anderson & Jiang, 2018), leading to questions regarding how these technologies may impact youths’ sleep patterns and subsequent mental health (Carter et al., 2016). These questions may be particularly pressing among youth with acute mental health concerns, such as those who are psychiatrically hospitalized, who are at high risk for both sleep disturbances and problematic patterns of social media use (Boafo et al., 2019; Nesi et al., 2019). However, very little is known about the intersection of social media use, sleep, and mental health among clinically acute adolescents.
The Role of Social Media in Adolescents’ Sleep and Mental Health
Over 95% of adolescents in the U.S. report using social media, with a large proportion of youth (45%) reporting being online almost constantly (Anderson & Jiang, 2018). Recent meta-analyses have shown significant associations between adolescents’ social media use and depressive symptoms (Ivie et al., 2020), suicide attempts (Nesi et al., 2021a; Sedgwick et al., 2019), and risky behaviors (Vannucci et al., 2020). However, high heterogeneity, small overall effect sizes, and mixed findings across studies suggest the need to examine more specific aspects of adolescents’ social media experiences beyond frequency of use, and to examine potential mechanisms underlying associations with mental health outcomes (Beyens et al., 2020; Orben, 2020; Odgers & Jensen, 2020; Twenge, 2020).
One such mechanism by which social media use may impact mental health is sleep disturbance, or disruptions in the amount, restfulness, or quality of sleep (Forrest et al., 2018). A meta-analysis suggests that youths’ nighttime use of digital devices, on which social media is often accessed, is associated with poorer quality sleep, reduced sleep quantity, and daytime sleepiness (Carter et al., 2016). Empirical work also finds that greater use of digital devices at bedtime and during the day, particularly for social media use and Internet browsing, is associated with longer sleep onset latency, shorter sleep duration, and increased sleep deficiency in adolescents (Hisler et al., 2020; Hysing et al., 2015; Johansson et al., 2016; Woods & Scott, 2016). Furthermore, a robust body of evidence suggests a relation between problematic or excessive use of social media and adolescent sleep and mental health (Yang et. al., 2018; Li et. al., 2018; Raudsepp, 2019), and some prior work finds associations between higher frequencies of digital media use and symptoms of inattention (Beyens et al., 2018; Ra et al., 2018).
However, recent work suggests that in addition to the timing, duration, and frequency of social media use, how it is used may also impact sleep (see Scott & Woods, 2019 for review). For example, youth who are more emotionally invested in their online activities and report greater fear of missing out (FoMO) associated with social media use may have greater difficulty disengaging from these platforms, thereby impacting sleep (Scott & Woods, 2018; Woods & Scott, 2016). Furthermore, sleep disruption has been found to mediate the longitudinal effects of problematic social media use (including greater emotional investment in use) on depressed mood in adolescents (Vernon et al., 2017).
Despite this important preliminary work, few studies have analyzed adolescents’ emotional responses to the experiences they have on social media. This is important because one mechanism through which social media use may negatively impact sleep is by increasing cognitive and emotional arousal that interferes with the ability to fall asleep and stay asleep (Scott & Woods, 2018; Scott & Woods, 2019). Adolescents who experience stronger or more frequent negative emotions in response to social media experiences (e.g., feeling left out or excluded by peers online, getting too few “likes” on photos; Nesi et al., 2021b) may thus be at risk for sleep disruption. Disrupted sleep may, in turn, interfere with the proactive use of cognitive-affective coping resources during the day (Krause et al., 2017; Alhola & Polo-Kantola, 2007). These processes may be especially relevant for psychiatrically vulnerable youth, who may experience stronger emotional responses to social media (Nesi et al., 2021b) and for whom disrupted sleep may contribute to clinical symptom severity.
Gender Differences
Gender differences in adolescent sleep (Galland et al., 2017), internalizing symptoms (Nolen-Hoeksema, 2001), suicidal ideation (Miranda-Mendizabal, 2019), and attention difficulties (Rucklidge, 2010) have been well documented for boys and girls, and emerging evidence suggests that gender minority youth are at greater risk for psychopathology and suicide compared to cisgender youth (Bettis et al., 2020; Spivey & Prinstein, 2019). A small but rapidly growing body of evidence also suggests gender differences in screen time and device use, with girls using social media more frequently (Anderson & Jiang, 2018), and girls and gender minority youth more likely to show greater emotional investment in their social media use (Nesi et al., 2021b).
Preliminary evidence also suggests gender differences in relations among adolescents’ social media use, sleep and health. In one study, greater social media use was linked to higher body mass index (BMI) in girls, but not boys, and shorter sleep duration mediated the link between social media use and BMI for boys, but not girls (Sampasa-Kanyinga et al., 2020). A recent longitudinal study also suggests that greater social media stress (i.e., emotional responses to and greater dependency on social media use), was associated with greater sleep latency and daytime sleepiness, among girls but not boys (van der Schuur et al., 2019). However, further work is needed to examine possible gender differences in specific characteristics of social media use and how these may be linked to adolescents’ sleep and mental health.
The Current Study
To the best of our knowledge, no study has examined the relation between social media use, sleep disturbance, and mental health in psychiatrically hospitalized adolescents. Thus, this study aimed to: (1) examine adolescents’ patterns of social media use, including both frequency and duration of use and subjective experiences of use (i.e., emotional responses to use, perceived overuse, importance of use), and their associations with sleep disturbance; (2) examine gender differences in social media use patterns, sleep disturbance, and clinical outcome; and (3) test whether sleep disturbance mediates associations between social media use and clinical outcomes that may be especially relevant in relation to sleep and social media use (i.e., suicidal ideation, internalizing symptoms, and attention problems).
Method
Participants
Participants were 243 adolescents admitted to an adolescent psychiatric inpatient unit between February 2020 and January 2021, who completed study measures and met the inclusion criteria of having access to a smartphone (when outside of the hospital). Participants were 11–18 years old and participant demographics can be found in Table 1. Due to small group sizes, participants who did not identify as male or female were collapsed into a single group (gender minority individuals) for analyses.
Table 1.
Study sample descriptive statistics
| n (%) except where noted | |
|---|---|
| Age, M (SD) | 15.34 (1.66) |
| Gender | |
| Female | 110 (45.3) |
| Male | 86 (35.4) |
| Transgender | 18 (7.9) |
| Gender-queer/gender non-conforming/gender fluid; | 20 (8.2) |
| Other | 5 (2.1) |
| Prefer not to answer | 4 (1.6) |
| Race/Ethnicity | |
| White | 169 (69.5) |
| Black | 30 (12.3) |
| Asian | 3 (1.2) |
| American Indian or Alaska | |
| Native | 1 (0.4) |
| Native Hawaiian or other pacific islander | 2 (0.8) |
| Other | 38 (15.6) |
| Hispanic | 80 (32.9) |
Note. N = 243
Procedures
As part of the inpatient unit’s clinical intake process, adolescents completed a battery of self-report measures. These measures are used to aid assessment, guide intervention, and to improve the quality of clinical care on the unit. The present study was classified as a chart review and the hospital’s Institutional Review Board granted a waiver of consent for participation.
Measures
Sleep Disturbance
Sleep disturbance was measured using an 8-item self-report short-form questionnaire (PROMIS Sleep Disturbance; Forrest et al., 2018), assessing sleep quality and satisfaction, sleep restoration, and difficulty falling asleep and staying asleep within the past 7 days. This measure uses a 5-point Likert scale from 1 (Never) to 5 (Always), with higher scores representing greater sleep disturbance (α = .92). Prior research indicates that this brief measure is not only highly correlated with the well-established Pittsburgh Sleep Quality Index (r = .83), but also may offer superior measurement precision (Yu et al., 2012). Furthermore, evidence indicates that it is moderately correlated with total sleep time as measured by actigraphy among youth (Hanish et al., 2017).
Social media use measures.
Social media use duration.
A single item assessed participants’ daily amount of social media use: “On average, how many hours per day do you typically spend on social media?” Response options ranged from 0 (Less than 1 hour) to 24 (24 hours). Due to the detection of univariate outliers, this variable was winsorized to set the maximum value at 12 hours.
Frequency of checking social media.
A single item assessed the frequency with which youth check social media: “How often do you check social media (for example, Instagram, Snapchat, or Facebook)?” Response options ranged from 0 (Never) to 7 (Almost Constantly) (Rideout & Robb, 2018).
Perceived overuse of social media.
A single item assessed the perception of spending too much time and energy on social media. Participants were asked, “Which of the following statements comes closest to the truth for you?” and were presented with three response options: “I spend too much time and energy on social media”, “I am comfortable with the amount of time and energy I spend on social media”, and “I don’t spend enough time and energy on social media” (Rideout & Robb, 2018). This item was coded dichotomously for analyses, with “I spend too much time and energy on social media” coded as 1 and the other two categories coded as 0.
Importance of social media.
A single item assessed the importance of social media in adolescents’ lives: “How important is social media in your life?“ and response options ranged from 0 (Not at all important) to 4 (Extremely important) (Rideout & Robb, 2018).
Emotional Responses to Social Media Experiences.
The frequency of positive and negative emotional responses to social media experiences were assessed using a 13-item self-report questionnaire (Nesi et al, 2021b). Examples of negative emotional response items include, “When you use social media, how often do you feel worried that you are missing out on things?”, “When you use social media, how often do you feel left out or excluded?”, and “When you use social media, how often do you feel hurt by a negative comment from someone?” Examples of positive emotional response items include, “When you are use social media, how often do you feel more connected to your friends?”, “When you use social media, how often do you feel supported and encouraged by your friends”, and “When you use social media, how often do you feel happy because of a positive comment from someone?” Items were rated on a 5-point Likert scale from 1 (Never) to 5 (Always), with items averaged to create the Positive and Negative subscales (Positive α = .86; Negative α = .86).
Clinical Outcomes
Suicidal ideation.
The Suicidal Ideation Questionnaire-Junior (SIQ-JR; Reynolds & Mazza, 1999) assessed past month suicidal ideation severity. The SIQ-JR has a total of 15 items rated on a 7-point Likert scale from 0 (I’ve never had this thought) to 6 (Almost every day). Items were averaged to create a total score, with higher scores reflecting more severe suicidal ideation (α = .96). The SIQ-JR has been used broadly and has evidenced strong psychometric properties among youth (Reynolds & Mazza, 1999).
Internalizing symptoms.
The Internalizing subscale of the 17-item version of the Youth-Pediatric Symptom Checklist (PSC-17; Gardner et al., 1999) assessed internalizing symptoms. This subscale assesses experiences of depressive and anxious symptomatology (e.g., sadness, worrying, hopelessness). Adolescents rated the extent to which they experience these symptoms on a 3-point Likert scale from 0 (Never) to 2 (Often), and items were summed, with higher total scores reflecting greater internalizing symptomatology (α = .87).
Attention problems.
The Attention subscale of the 17-item version of the Youth-Pediatric Symptom Checklist (PSC-17; Gardner et al., 1999) was used to assess attention problems, including feelings of being easily distracted, having trouble concentrating, and being unable to sit still. Adolescents rated the extent to which they experience these symptoms on a 3-point Likert scale from 0 (Never) to 2 (Often), and items were summed, with higher scores reflecting greater attention problems (α = .73).
Results
Associations between social media use and sleep disturbance
Bivariate correlations were conducted between all study variables (Table 1). No significant associations were revealed between sleep disturbance and the majority of social media variables, i.e., average duration of use, frequency of checking, perceived importance, perceived overuse, and positive emotional responses to social media use. However, there was a significant, small-to-medium association between sleep disturbance and frequency of negative emotional responses to social media experiences. Negative emotional responses to social media use and sleep disturbance were also associated with each clinical outcome: suicidal ideation, internalizing symptoms, and attention problems.
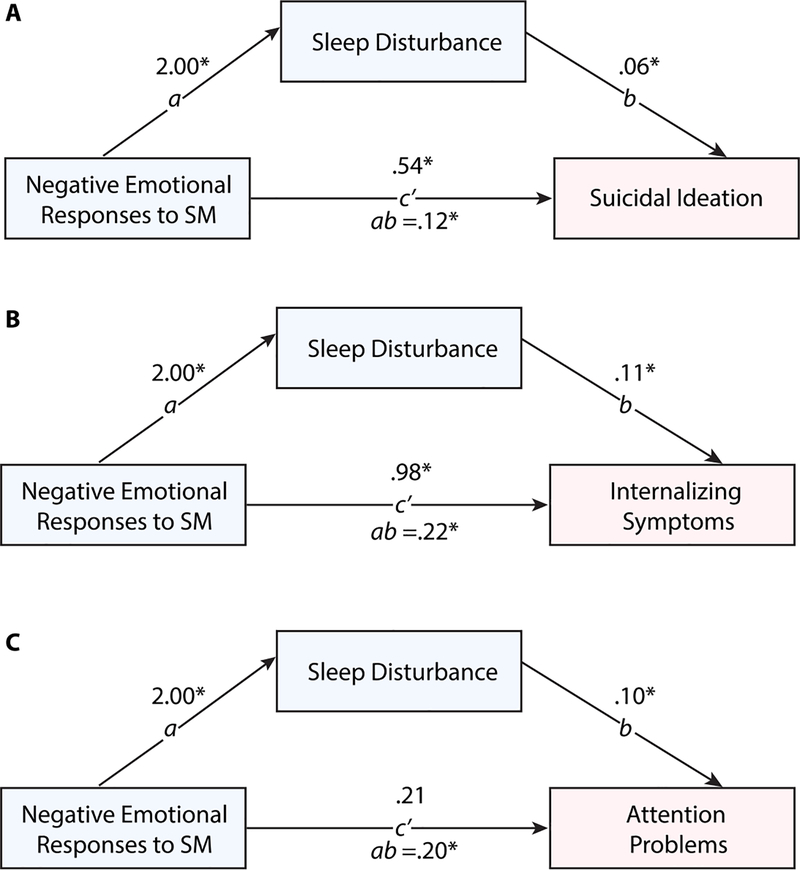
Mediation models for indirect effect of negative emotional response to social media on clinical outcomes, via sleep disturbance
To examine the indirect effect of negative emotional responses to social media on each clinical outcome via sleep disturbance (Figure 1), three mediation models were tested using the PROCESS v3.3 macro (Model 4; Hayes, 2013) in SPSS 25.0. Each model also included the following covariates: gender (male, female, other); race (Black, White, other race); ethnicity (Hispanic vs. non-Hispanic); age; and average duration of social media use. The significance of the indirect effect was testing using bootstrapping procedures with 5,000 bootstrapped samples, and 95% confidence intervals were constructed.
Figure 1.
Models tests mediation of associations between negative emotional responses to social media and clinical symptoms (suicidal ideation, internalizing symptoms, and attention problems) by sleep disturbance. All models also include control variables (social media hours, gender, race, ethnicity, and age) regressed on outcomes and mediator. *p<.05; **p<.01; ***p<.001
All three meditation models (Table 3) indicated a significant effect of negative emotional responses to social media on sleep disturbance (a path), after controlling for all covariates. The direct effect of negative emotional responses to social media, after controlling for all covariates and the effects of sleep disturbance (c’ path), was significant for suicidal ideation and internalizing symptoms, but not for attention problems. The indirect effects (ab path) on each outcome via sleep disturbance were also significant, indicated by bootstrapped 95% Confidence Intervals that did not contain zero.
Table 3.
Mediation model statistics for effects of negative emotional responses to social media on clinical outcomes, via sleep disturbance
| Outcome Variable: Sleep Disturbance (a-path) | b | SE | p | 95% CI |
|---|---|---|---|---|
|
| ||||
| Intercept | 23.32 | 5.13 | <.001 | [13.22, 33.43] |
| Negative Emotional Responses to SM | 2.00 | 0.55 | <.001 | [0.93, 3.08] |
| SM Hours | −0.26 | 0.15 | .086 | [−0.57, 0.37] |
| Gender: Male | −3.42 | 1.13 | .003 | [−5.64, −1.21] |
| Gender: Other | 2.71 | 1.35 | .046 | [0.04, 5.37] |
| Race: Black | 1.86 | 1.57 | .238 | [−1.24, 4.96] |
| Race: Other | 0.29 | 1.35 | .832 | [−2.38, 2.95] |
| Ethnicity: Hispanic | −2.05 | 1.10 | .063 | [−4.22, 0.11] |
| Age | 0.16 | 0.31 | .616 | [−0.45, 0.77] |
|
| ||||
| Outcome Variables: Clinical Outcomes (b-paths) | ||||
|
| ||||
| Outcome: Suicidal Ideation | ||||
| Intercept | 1.42 | 1.05 | .178 | [−0.65, 3.51] |
| Sleep Disturbance | 0.06 | 0.01 | <.001 | [0.04, 0.09] |
| Negative Emotional Responses to SM | 0.54 | 0.11 | <.001 | [0.33, 0.76] |
| SM Hours | 0.01 | 0.03 | .831 | [−0.05, 0.07] |
| Gender: Male | −0.69 | 0.23 | .002 | [−1.14, −0.25] |
| Gender: Other | 0.51 | 0.27 | .057 | [−0.02, 1.04] |
| Race: Black | −0.64 | 0.31 | .040 | [−1.25, −0.03] |
| Race: Other | −0.15 | 0.27 | .575 | [−0.67, 0.38] |
| Ethnicity: Hispanic | 0.12 | 0.22 | .578 | [−0.31, 0.55] |
| Age | −0.07 | 0.06 | .242 | [−0.19, 0.05] |
| Bootstrapped Indirect Effect (ab-path) | 0.12 | 0.04 | -- | [0.05, 0.22] |
| Outcome: Internalizing Symptoms | ||||
| Intercept | 2.85 | 1.61 | .078 | [−0.32, 6.02] |
| Sleep Disturbance | 0.11 | 0.02 | <.001 | [0.08, 0.15] |
| Negative Emotional Responses to SM | 0.98 | 0.17 | <.001 | [0.65, 1.31] |
| SM Hours | 0.00 | 0.05 | .936 | [−0.09, 0.09] |
| Gender: Male | −1.35 | 0.35 | <.001 | [−2.03, −0.67] |
| Gender: Other | 0.18 | 0.41 | .659 | [−0.63, 0.99] |
| Race: Black | −0.84 | 0.47 | .078 | [−1.77, 0.10] |
| Race: Other | −0.05 | 0.41 | .906 | [−0.85, 0.75] |
| Ethnicity: Hispanic | −0.23 | 0.33 | .486 | [−0.89, 0.42] |
| Age | −0.02 | 0.09 | .846 | [−0.20, 1.66] |
| Bootstrapped Indirect Effect (ab-path) | 0.23 | 0.08 | -- | [0.10, 0.40] |
| Outcome: Attention Problems | ||||
| Intercept | 6.58 | 1.46 | <.001 | [3.70, 9.47] |
| Sleep Disturbance | 0.10 | 0.02 | <.001 | [0.07, 0.20] |
| Negative Emotional Responses to SM | 0.21 | 0.02 | .174 | [−0.09, 0.51] |
| SM Hours | −0.01 | 0.04 | .786 | [−0.07, 0.24] |
| Gender: Male | −0.43 | 0.31 | .171 | [−1.05, 0.19] |
| Gender: Other | 0.57 | 0.37 | .128 | [−0.16, 1.30] |
| Race: Black | −1.08 | 0.43 | .013 | [−1.93, −0.24] |
| Race: Other | −0.13 | 0.37 | .719 | [−0.861, 0.595] |
| Ethnicity: Hispanic | −0.13 | 0.30 | .676 | [−0.72, 0.47] |
| Age | −0.23 | 0.08 | .008 | [−0.39, −0.06] |
| Bootstrapped Indirect Effect (ab-path) | 0.20 | 0.07 | -- | [0.08, 0.35] |
Note. SM = social media. Confidence intervals that do not contain zero are considered significant. Total R2 for models for Suicidal Ideation l = 0.15, p <.001; for Internalizing Symptoms = 0.39, p <.001; for Attention Problems = 0.15, p < .001.
Sensitivity analyses were conducted examining whether duration of social media use (average daily hours) was also associated with each clinical outcome indirectly via sleep disturbance. Daily hours spent on social media was not significantly associated with sleep disturbance (a path; b = −0.19, se = 0.15; p = .229). There was no significant direct (c’ path) or indirect (ab path) association between daily hours on social media and any clinical outcome: for suicidal ideation, direct effect b = 0.03, se = 0.03, p = 0.317; indirect effect b = −0.01, se = 0.01, 95% CI [−0.04, 0.01]; for internalizing symptoms, direct effect b = 0.05, se = 0.05, p = 0.315; indirect effect b = −0.03, se = 0.02, 95% CI [−0.07, 0.02]; for attention problems, direct effect b = 0.00, se = 0.04, p = 0.942; indirect effect b = −0.02, se = 0.02, 95% CI [−0.05, 0.01].
Gender differences
As a preliminary test of gender differences in primary variables of interest, a series of one-way ANOVA tests was conducted to examine mean differences across gender groups (Table 4). Results suggested that compared to boys, girls and gender minority youth reported, on average, higher average daily hours of social media use and frequency of checking social media. Gender minority youth showed more frequent positive emotional responses to social media use compared to boys. No gender differences were revealed in frequency of negative emotional responses to social media, importance of social media, or perceived overuse of social media.
Table 4.
Gender differences in sleep disturbance, social media use patterns, and clinical symptoms
| Full Sample (N = 243) | Male (n = 86) | Female (n = 110) | Gender Minority (n = 47) | ||
|---|---|---|---|---|---|
| n (%) / M (SD) | n (%) / M (SD) | n (%) / M (SD) | n (%) / M (SD) | χ2 / F(df) | |
| 1. Sleep Disturbance | 26.43 (8.06) | 23.76 (8.83)a | 27.16 (7.20)b | 29.62 (7.05)b | 9.50 (242)*** |
| 2. SM Hours | 4.15 (3.34) | 3.42 (3.13)a | 4.47 (3.17)b | 4.72 (3.91)b | 3.33 (242)* |
| 3. SM Importance | 1.77 (1.13) | 1.59 (1.12)a | 1.80 (1.14)a,b | 2.04 (1.10)b | 2.48 (241) |
| 4. Frequency of checking SM | 5.33 (1.71) | 4.90 (1.93)a | 5.57 (1.53)b | 5.53 (1.57)b | 4.31 (242)* |
| 5. Perceived overuse of SM | 35 (14.4) | 11 (12.9) | 14 (12.8) | 10 (21.7) | 2.34 |
| 6. Negative Emotional Responses to SM | 1.45 (0.92) | 1.29 (0.92) | 1.52 (0.87) | 1.60 (1.02) | 2.24 (241) |
| 7. Positive Emotional Responses to SM | 2.53 (0.94) | 2.35 (0.99)a | 2.56 (0.92)a,b | 2.76 (0.86)b | 3.13 (241)* |
| 8. Suicidal Ideation | 2.56 (1.81) | 1.70 (1.81)a | 2.79 (1.59)b | 3.59 (1.63)c | 21.28 (242)*** |
| 9. Internalizing Symptoms | 6.41 (2.87) | 5.00 (3.09)a | 7.01 (2.55)b | 7.57 (2.08)b | 19.12 (242)*** |
| 10. Attention Problems | 5.72 (2.35) | 4.98 (2.38)a | 5.86 (2.28)b | 6.72 (2.02)c | 9.42 (242)*** |
Note. Superscript letters denote column proportions or means differ from each other at the p < .05 level. Due to small group sizes, youth who did not identify as male or female were combined into a single “gender minority” group; SM = social media.
p < .05
p < .01
p < .001
To examine gender differences in the effects of negative emotional responses to social media on sleep disturbance, and indirectly on clinical outcomes via sleep disturbance, three moderated mediation models were tested using the PROCESS v3.3 macro (Model 8; Hayes, 2013) in SPSS 25.0. Gender did not moderate the association between negative emotional responses to social media and sleep disturbance, the direct effect of negative emotional responses to social media on any outcome (suicidal ideation, internalizing symptoms, and attention problems), nor the indirect effect (complete results available upon request).
Discussion
The role of social media use in adolescent sleep is an issue of critical importance for youth mental health. While prior work on sleep and mental health has often focused on social media use frequency and duration, adolescents’ emotional experiences related to social media have been underexplored, particularly among clinically acute populations. The current study examined characteristics of youths’ social media use (i.e., duration and frequency of use, emotional responses to use, perceived overuse, and importance of social media), in relation to sleep disturbance and clinical outcomes (i.e., severity of internalizing symptoms, suicidal ideation, and attention problems) among psychiatrically hospitalized youth. More frequent negative, but not positive, emotional responses to social media use were linked to greater sleep disturbance, as well as higher clinical symptom severity. Furthermore, sleep disturbance mediated the relation between adolescents’ negative emotional responses to social media and clinical symptom severity in cross-sectional mediation models, even after controlling for overall time spent using social media use. Although gender differences were revealed in various characteristics of social media use, sleep disturbance, and clinical outcomes, the associations among these constructs did not vary across gender groups. Overall, findings highlight the importance of examining specific, negative emotional responses to social media use, and the potential role of sleep disturbance as a mechanism through which such experiences influence clinical symptoms in psychiatrically vulnerable youth.
Results suggest that negative emotional responses to social media experiences were associated with higher severity of internalizing symptoms, suicidal ideation, and attention problems, and that this association was mediated by sleep disturbance. Notably, however, all other examined characteristics of social media use, including frequency of use and perception of overuse, were not related to sleep disturbance or clinical severity. These findings are in line with prior work suggesting heightened cognitive and emotional arousal as a potential mechanism by which social media use may impact adolescent sleep (Scott & Woods, 2019). Results are also consistent with past literature showing that sleep disturbance mediates the association between problematic social media use and depressive symptoms in youth (Vernon et. al., 2017), and extend prior literature to a population of psychiatrically hospitalized adolescents. Sleep disruptions may be particularly impactful for clinically vulnerable youth, and as negative emotional experiences on social media may lead to sleep disruption in this population, this may be an important area of clinical intervention to mitigate symptom severity.
Furthermore, these findings highlight the need to examine nuanced characteristics of adolescents’ social media use beyond simple frequency and duration. Many prior studies of sleep disruption have focused on overall device use (i.e., including overall time spent on the Internet, watching TV or videos, or playing games), rather than specifically on social media (Fobian et al., 2016; Hisler et al., 2020; Hysing et al., 2015; Johansson et al., 2016). It may be the case that, when it comes to sleep disruption, “screen time” is a more relevant factor for other screen activities, or for overall screen time across devices and platforms, than for social media in particular. Furthermore, it is possible that the time of day that social media is used is especially important, with social media use at bedtime having stronger associations with sleep disturbance compared to using social media use at other times of day (e.g., morning). Indeed, media use at bedtime has been linked to poorer sleep efficiency in adolescents (Fobian et al., 2016). Thus, overall measures of time spent and frequency of checking social media throughout an average day, as used in the current study, may not capture this nuance. However, it should be noted that adolescents reporting greater duration and frequency of social media use were also more likely to report more frequent negative emotional responses to social media, which were associated with poorer sleep and clinical outcomes. Thus, future work will be needed to investigate temporal associations, particularly related to nighttime social media use, and interactions among these factors. Future work will also be needed to analyze the relationship between emotional responses to social media use and sleep duration in adolescents, as social media use and subsequent emotional arousal may be displacing sleep time. Future studies of this kind would also benefit from assessing the relationship between social media and sleep-related behaviors, like sleeping with a phone within reach or waking in the middle of the night to check social media, and clinical outcomes.
Findings reveal a complex portrait of the role of gender in sleep, social media use, and clinical symptoms. Specifically, girls and gender minority youth on average spent more time using social media daily and checked social media more often than boys. Gender minority youth also showed more frequent positive emotional responses to social media use compared to boys. Consistent with previous literature, girls and gender minority youth, compared to boys, reported greater sleep disturbance, higher levels of suicidal ideation, and higher levels of internalizing and attention problems (Bettis et al., 2020; Nolen-Hoeksema, 2001; Galland et al., 2017). Notably, however, adolescents of all genders were equally likely to report negative emotional responses to social media use, and gender did not moderate associations among negative emotional social media experiences, sleep, and clinical symptoms. These findings are consistent with literature on gender differences in social media use frequency (Anderson & Jiang, 2018; Twenge & Martin, 2020), and add to research showing that gender minority status is a significant vulnerability factor for negative clinical outcomes (Bettis et al., 2020; Spivey & Prinstein, 2019). However, results also suggest that negative emotional responses to social media may be a risk factor for poor sleep and subsequent mental health concerns among youth of all genders. It is important to note that this lack of variability in associations across gender groups could be due to the nature of the study population, which consists of high-risk, psychiatrically hospitalized adolescents.
Limitations
This study is one of the first to examine relations among social media use, sleep, and clinical symptom severity in a sample of psychiatrically hospitalized adolescents. However, there are a number of limitations that should be considered when interpreting the present findings. First, although a validated self-report measure of sleep disturbance was used, this measure assesses a wide range of sleep disturbance indices, inclusive of perceptions of quality, satisfaction, restoration, initial insomnia, and middle insomnia. Therefore, we cannot draw conclusions about the specific indices of sleep disturbance that may be driving associations. It is also important to highlight that self-report measures of sleep are inherently limited and are only moderately correlated with objective measures of sleep, such as actigraphy or polysomnography (Wolfson et al., 2003). Second, clinical symptoms were assessed only with self-report measures; interview measures, and particularly those that permit clinical diagnosis, should be considered for use in future studies in order to examine associations with emotional responses to social media use as well as sleep disturbance. Third, daily duration of social media use was assessed, but timing of use was not; there is evidence that nighttime social media use may be particularly important in the association between social media use and sleep (e.g., Caumo et al., 2020; Garmy et al., 2020; Scott & Woods, 2018). Relatedly, we did not measure timing of negative emotional responses to social media use; it is likely that adolescents experiencing stronger emotional responses to social media at night will experience greater interference with sleep. Fourth, the present study was cross-sectional and thus conclusions regarding the temporal relationship between social media use, sleep, and indices of psychopathology cannot be drawn. Mediation was used to test models; however given the cross-sectional design, these analyses should be considered preliminary, and must be replicated within a longitudinal framework in order to evaluate their validity. There might be other cognitive mediators besides sleep problems in the association between negative social media experiences and internalizing symptoms that were not assessed in this study. As cognitive factors such as a negative cognitive bias or ruminative tendencies are consistently linked to increased internalizing symptoms, including suicidal ideation, their potential role in how negative social media experiences affect clinical symptoms needs to be explored in future research (Beevers et al., 2019; Łosiak et al., 2019; Nolen-Hoeksema et al., 2008; Pinto & Whisman, 1996). Additionally, emotional reactions to social media experiences were assessed in this study, but not the specific type or context of these experiences. As objectively negative or challenging experiences on social media, including being cyberbullied or victimized, may affect the sleep quality and clinical symptoms, future research that accounts for the specific types of social media experiences is warranted (e.g., John et al., 2018; Viner et al., 2019).
The limitations of the present study’s design and the conclusions that may be drawn underscore the importance of pursuing a number of future research directions. Future research should evaluate the present results using a longitudinal design, employing both the subjective measures used in the present study, in addition to objective metrics of sleep (e.g., actigraphy) and social media use (e.g., screen time), and the type of social media interactions. Longitudinal designs that permit the analysis of these associations at a daily level will reduce memory bias and allow for a more granular examination of the within- and between-persons associations between social media use, sleep, and psychopathology (e.g., Hamilton et al., 2020).
Clinical Implications
Findings underscore the clinical importance of assessing sleep disturbance and emotional responses to social media use, particularly among psychiatrically vulnerable youth. Such information may help identify those in need of more intensive monitoring and intervention and allow for individual tailoring of treatments based on emotional responses and sleep difficulties. For example, because emotional arousal may impact adolescent sleep, youth who have more negative emotional reactions to social media may benefit from using various emotion regulation strategies particularly before bedtime. In addition, these youth may benefit from parental monitoring and behavioral interventions aimed at improving their sleep and limiting access to social media at night. Overall, these findings suggest the need to closely assess and intervene on emotional responses to social media use and sleep disturbance to decrease clinical symptom severity in psychiatrically vulnerable youth.
Conclusions
Studies of social media use and sleep disruption have been limited by a focus on frequency or duration of use, and have rarely investigated these processes in psychiatrically acute adolescents. The present study offers a preliminary investigation of the role of adolescents’ emotional experiences using social media in sleep disturbance and clinical symptom severity. Findings suggest that negative emotional responses to social media may be an important factor in contributing to sleep disturbance and subsequent mental health outcomes in psychiatrically vulnerable youth.
Table 2.
Correlations between study variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| 1. Sleep Disturbance | |||||||||
| 2. SM Hours | −.02 | ||||||||
| 3. SM Importance | −.02 | .51** | |||||||
| 4. Frequency of checking SM | −.07 | .56** | .46** | ||||||
| 5. Perception of Too Much SM Time | −.00 | .26** | .17** | .21** | |||||
| 6. Negative Emotional Responses to SM | .24** | .15* | .22** | .20** | .25** | ||||
| 7. Positive Emotional Responses to SM | −.11 | .18** | .40** | .24** | −.02 | −.16* | |||
| 8. Suicidal Ideation | .40** | .09 | .04 | .07 | .07 | .39** | −.16* | ||
| 9. Internalizing Symptoms | .46** | .08 | .12 | .01 | .02 | .43** | −.09 | .76** | |
| 10. Attention Problems | .40** | .03 | .10 | −.04 | −.11 | .19** | .02 | .47** | .50** |
Note:
p < .05.
p < .01; SM = social media
Footnotes
Declaration of Interest
J.H. has received an editorial stipend from John Wiley publishers.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bettis AH, Thompson EC, Burke TA, Nesi J, Kudinova AY, Hunt JI, Liu RT, & Wolff JC (2020). Prevalence and clinical indices of risk for sexual and gender minority youth in an adolescent inpatient sample. Journal of Psychiatric Research, 130, 327–332. 10.1016/j.jpsychires.2020.08.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alhola P, & Polo-Kantola P (2007). Sleep deprivation: Impact on cognitive performance. Neuropsychiatric Disease and Treatment, 3(5), 553–567. [PMC free article] [PubMed] [Google Scholar]
- Anderson M, & Jiang J (n.d.). Teens, Social Media & Technology 2018. 10.
- Beevers CG, & Miller IW (2004). Perfectionism, cognitive bias, and hopelessness as prospective predictors of suicidal ideation. Suicide & Life-Threatening Behavior, 34, 126–137. 10.1521/suli.34.2.126.32791 [DOI] [PubMed] [Google Scholar]
- Beevers CG, Mullarkey MC, Dainer-Best J, Stewart RA, Labrada J, Allen JJB, McGeary JE, & Shumake J (2019). Association between negative cognitive bias and depression: A symptom-level approach. Journal of Abnormal Psychology, 128, 212–227. 10.1037/abn0000405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bettis AH, Thompson EC, Burke TA, Nesi J, Kudinova AY, Hunt JI, … & Wolff JC. (2020). Prevalence and clinical indices of risk for sexual and gender minority youth in an adolescent inpatient sample. Journal of Psychiatric Research, 130, 327–332. 10.1016/j.jpsychires.2020.08.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beyens I, Pouwels JL, van Driel II, Keijsers L, & Valkenburg PM (2020). The effect of social media on well-being differs from adolescent to adolescent. Scientific Reports, 10(1), 10763. 10.1038/s41598-020-67727-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beyens I, Valkenburg PM, & Piotrowski JT (2018). Screen media use and ADHD-related behaviors: Four decades of research. Proceedings of the National Academy of Sciences, 115(40), 9875–9881. 10.1073/pnas.1611611114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boafo A, Armitage R, Greenham S, Tavakoli P, Dale A, Nixon A, Lafrenière A, Ray LB, De Koninck J, & Robillard R (2019a). Sleep architecture in adolescents hospitalized during a suicidal crisis. Sleep Medicine, 56, 41–46. 10.1016/j.sleep.2018.12.018 [DOI] [PubMed] [Google Scholar]
- Boafo A, Armitage R, Greenham S, Tavakoli P, Dale A, Nixon A, Lafrenière A, Ray LB, De Koninck J, & Robillard R (2019b). Sleep architecture in adolescents hospitalized during a suicidal crisis. Sleep Medicine, 56, 41–46. 10.1016/j.sleep.2018.12.018 [DOI] [PubMed] [Google Scholar]
- Carter B, Rees P, Hale L, Bhattacharjee D, & Paradkar MS (2016). Association Between Portable Screen-Based Media Device Access or Use and Sleep Outcomes: A Systematic Review and Meta-analysis. JAMA Pediatrics, 170(12), 1202–1208. 10.1001/jamapediatrics.2016.2341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caumo GH, Spritzer D, Carissimi A, & Tonon AC (2020). Exposure to electronic devices and sleep quality in adolescents: A matter of type, duration, and timing. Sleep Health, 6(2), 172–178. 10.1016/j.sleh.2019.12.004 [DOI] [PubMed] [Google Scholar]
- Fobian AD, Avis K, & Schwebel DC (2016). The Impact of Media Use on Adolescent Sleep Efficiency. Journal of Developmental and Behavioral Pediatrics: JDBP, 37(1), 9–14. 10.1097/DBP.0000000000000239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galland BC, Gray AR, Penno J, Smith C, Lobb C, & Taylor RW (2017). Gender differences in sleep hygiene practices and sleep quality in New Zealand adolescents aged 15 to 17 years. Sleep Health, 3(2), 77–83. 10.1016/j.sleh.2017.02.001 [DOI] [PubMed] [Google Scholar]
- Forrest CB, Meltzer LJ, Marcus CL, de la Motte A, Kratchman A, Buysse DJ, Pilkonis PA, Becker BD, Bevans KB (2018). Development and validation of the PROMIS Pediatric Sleep Disturbance and Sleep-Related Impairment item banks. Sleep, 41(6). 10.1093/sleep/zsy054 [DOI] [PubMed] [Google Scholar]
- Gardner W, Murphy M, Childs G, Kelleher K, Pagano M, Jellinek M, … & Chiappetta L. (1999). The PSC-17: A brief pediatric symptom checklist with psychosocial problem subscales. A report from PROS and ASPN. Ambulatory Child Health, 5, 225–225. [Google Scholar]
- Garmy P, Idecrans T, Hertz M, Sollerhed A-C, & Hagell P (2020). Is sleep duration associated with self-reported overall health, screen time, and nighttime texting among adolescents? The Journal of International Medical Research, 48(3), 300060519892399. 10.1177/0300060519892399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton JL, Chand S, Reinhardt L, Ladouceur CD, Silk JS, Moreno M, Franzen PL, & Bylsma LM (2020). Social media use predicts later sleep timing and greater sleep variability: An ecological momentary assessment study of youth at high and low familial risk for depression. Journal of Adolescence, 83, 122–130. 10.1016/j.adolescence.2020.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanish AE, Lin-Dyken DC, & Han JC (2017). PROMIS Sleep Disturbance and Sleep-Related Impairment in Adolescents: Examining Psychometrics Using Self-Report and Actigraphy. Nursing Research, 66(3), 246–251. 10.1097/NNR.0000000000000217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2013). Introduction to mediation, moderation, and conditional process analysis. A regression-based approach. New York, NY: The Guilford Press. [Google Scholar]
- Hisler G, Twenge JM, & Krizan Z (2020). Associations between screen time and short sleep duration among adolescents varies by media type: Evidence from a cohort study. Sleep Medicine, 66, 92–102. 10.1016/j.sleep.2019.08.007 [DOI] [PubMed] [Google Scholar]
- Hysing M, Pallesen S, Stormark KM, Jakobsen R, Lundervold AJ, & Sivertsen B (2015). Sleep and use of electronic devices in adolescence: Results from a large population-based study. BMJ Open, 5(1), e006748. 10.1136/bmjopen-2014-006748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivie EJ, Pettitt A, Moses LJ, & Allen NB (2020). A meta-analysis of the association between adolescent social media use and depressive symptoms. Journal of Affective Disorders, 275, 165–174. 10.1016/j.jad.2020.06.014 [DOI] [PubMed] [Google Scholar]
- Johansson AEE, Petrisko MA, & Chasens ER (2016). Adolescent Sleep and the Impact of Technology Use Before Sleep on Daytime Function. Journal of Pediatric Nursing, 31(5), 498–504. 10.1016/j.pedn.2016.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- John A, Glendenning AC, Marchant A, Montgomery P, Stewart A, Wood S, Lloyd K, & Hawton K (2018). Self-Harm, Suicidal Behaviours, and Cyberbullying in Children and Young People: Systematic Review. Journal of Medical Internet Research, 20, e129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause AJ, Simon EB, Mander BA, Greer SM, Saletin JM, Goldstein-Piekarski AN, & Walker MP (2017). The sleep-deprived human brain. Nature Reviews. Neuroscience, 18(7), 404–418. 10.1038/nrn.2017.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J-B, Mo PKH, Lau JTF, Su X-F, Zhang X, Wu AMS, Mai J-C, & Chen Y-X (2018). Online social networking addiction and depression: The results from a large-scale prospective cohort study in Chinese adolescents. Journal of Behavioral Addictions, 7(3), 686–696. 10.1556/2006.7.2018.69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littlewood DL, Kyle SD, Carter L-A, Peters S, Pratt D, & Gooding P (2019). Short sleep duration and poor sleep quality predict next-day suicidal ideation: An ecological momentary assessment study. Psychological Medicine, 49(3), 403–411. 10.1017/S0033291718001009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Łosiak W, Blaut A, Kłosowska J, & Łosiak-Pilch J (2019). Stressful Life Events, Cognitive Biases, and Symptoms of Depression in Young Adults. Frontiers in Psychology, 10, 2165. 10.3389/fpsyg.2019.02165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda-Mendizabal A, Castellví P, Parés-Badell O, Alayo I, Almenara J, Alonso I, Blasco MJ, Cebrià A, Gabilondo A, Gili M, Lagares C, Piqueras JA, Rodríguez-Jiménez T, Rodríguez-Marín J, Roca M, Soto-Sanz V, Vilagut G, & Alonso J (2019). Gender differences in suicidal behavior in adolescents and young adults: Systematic review and meta-analysis of longitudinal studies. International Journal of Public Health, 64(2), 265–283. 10.1007/s00038-018-1196-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nesi J, Burke TA, Bettis AH, Kudinova AY, Thompson EC, MacPherson HA, Fox KA, Lawrence HR, Thomas SA, Wolff JC, Altemus MK, Soriano S, & Liu RT (2021a). Social media use and self-injurious thoughts and behavior: A systematic review and meta-analysis. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nesi J, Rothenberg WA, Bettis AH, Massing-Schaffer M, Fox KA, Telzer EH, Lindquist KA, & Prinstein MJ (2021b). Emotional responses to social media experiences among adolescents: Longitudinal associations with depressive symptoms. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nesi J, Wolff JC, & Hunt J (2019). Patterns of Social Media Use Among Adolescents Who Are Psychiatrically Hospitalized. Journal of the American Academy of Child & Adolescent Psychiatry, 58(6), 635–639.e1. 10.1016/j.jaac.2019.03.009 [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S (2001). Gender differences in depression. Current Directions in Psychological Science, 10(5), 173–176. 10.1111/1467-8721.00142 [DOI] [Google Scholar]
- Nolen-Hoeksema S, Wisco BE, & Lyubomirsky S (2008). Rethinking Rumination. Perspectives on Psychological Science, 3, 400–424. 10.1111/j.1745-6924.2008.00088.x [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Wisco BE, & Lyubomirsky S (2008). Rethinking Rumination. Perspectives on Psychological Science, 3, 400–424. 10.1111/j.1745-6924.2008.00088.x [DOI] [PubMed] [Google Scholar]
- Odgers CL, & Jensen MR (2020). Annual Research Review: Adolescent mental health in the digital age: facts, fears, and future directions. Journal of Child Psychology and Psychiatry, 61(3), 336–348. 10.1111/jcpp.13190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orben A (2020). Teenagers, screens and social media: A narrative review of reviews and key studies. Social Psychiatry and Psychiatric Epidemiology, 55(4), 407–414. 10.1007/s00127-019-01825-4 [DOI] [PubMed] [Google Scholar]
- Owens J, Group ASW, & Adolescence CO (2014). Insufficient Sleep in Adolescents and Young Adults: An Update on Causes and Consequences. Pediatrics, 134(3), e921–e932. 10.1542/peds.2014-1696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinto A, & Whisman M (1996). Negative Affect and Cognitive Biases in Suicidal and Nonsuicidal Hospitalized Adolescents. Journal of the American Academy of Child & Adolescent Psychiatry, 35, 158–165. 10.1097/00004583-199602000-00008 [DOI] [PubMed] [Google Scholar]
- Ra CK, Cho J, Stone MD, De La Cerda J, Goldenson NI, Moroney E, Tung I, Lee SS, & Leventhal AM (2018). Association of Digital Media Use With Subsequent Symptoms of Attention-Deficit/Hyperactivity Disorder Among Adolescents. JAMA, 320(3), 255–263. 10.1001/jama.2018.8931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudsepp L (2019). Brief report: Problematic social media use and sleep disturbances are longitudinally associated with depressive symptoms in adolescents. Journal of Adolescence, 76, 197–201. 10.1016/j.adolescence.2019.09.005 [DOI] [PubMed] [Google Scholar]
- Reynolds WM, & Mazza JJ (1999). Assessment of suicidal ideation in inner-city children and young adolescents: Reliability and validity of the Suicidal Ideation Questionnaire-JR. School Psychology Review, 28(1), 17–30. [Google Scholar]
- Rideout V, and Robb MB (2018). Social media, social life: Teens reveal their experiences. San Francisco, CA: Common Sense Media. [Google Scholar]
- Rucklidge JJ (2010). Gender differences in attention-deficit/hyperactivity disorder. The Psychiatric Clinics of North America, 33(2), 357–373. 10.1016/j.psc.2010.01.006 [DOI] [PubMed] [Google Scholar]
- Sampasa-Kanyinga H, Colman I, Goldfield GS, Hamilton HA, & Chaput J-P (2020). Sex differences in the relationship between social media use, short sleep duration, and body mass index among adolescents. Sleep Health, 6(5), 601–608. 10.1016/j.sleh.2020.01.017 [DOI] [PubMed] [Google Scholar]
- Scott H, & Woods HC (2019). Understanding links between social media use, sleep and mental health: recent progress and current challenges. Current Sleep Medicine Reports, 5(3), 141–149. 10.1007/s40675-019-00148-9 [DOI] [Google Scholar]
- Scott H, & Woods HC (2018). Fear of missing out and sleep: Cognitive behavioural factors in adolescents’ nighttime social media use. Journal of Adolescensce, 68, 61–65. 10.1016/j.adolescence.2018.07.009 [DOI] [PubMed] [Google Scholar]
- Sedgwick R, Epstein S, Dutta R, & Ougrin D (2019). Social media, internet use and suicide attempts in adolescents. Current Opinion in Psychiatry, 32(6), 534–541. 10.1097/YCO.0000000000000547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Short MA, & Weber N (2018). Sleep duration and risk-taking in adolescents: A systematic review and meta-analysis. Sleep Medicine Reviews, 41, 185–196. 10.1016/j.smrv.2018.03.006 [DOI] [PubMed] [Google Scholar]
- Spivey LA, & Prinstein MJ (2019). A Preliminary Examination of the Association between Adolescent Gender Nonconformity and Suicidal Thoughts and Behaviors. Journal of Abnormal Child Psychology, 47(4), 707–716. 10.1007/s10802-018-0479-6 [DOI] [PubMed] [Google Scholar]
- Twenge JM (2020). Increases in Depression, Self-Harm, and Suicide Among U.S. Adolescents After 2012 and Links to Technology Use: Possible Mechanisms. Psychiatric Research and Clinical Practice, 2(1), 19–25. 10.1176/appi.prcp.20190015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twenge JM, & Martin GN (2020). Gender differences in associations between digital media use and psychological well-being: Evidence from three large datasets. Journal of Adolescence, 79, 91–102. 10.1016/j.adolescence.2019.12.018 [DOI] [PubMed] [Google Scholar]
- van der Schuur WA, Baumgartner SE, & Sumter SR (2019). Social Media Use, Social Media Stress, and Sleep: Examining Cross-Sectional and Longitudinal Relationships in Adolescents. Health Communication, 34(5), 552–559. 10.1080/10410236.2017.1422101 [DOI] [PubMed] [Google Scholar]
- Vannucci A, Simpson EG, Gagnon S, & Ohannessian CM (2020). Social media use and risky behaviors in adolescents: A meta-analysis. Journal of Adolescence, 79, 258–274. 10.1016/j.adolescence.2020.01.014 [DOI] [PubMed] [Google Scholar]
- Vernon L, Modecki KL, & Barber BL (2017). Tracking Effects of Problematic Social Networking on Adolescent Psychopathology: The Mediating Role of Sleep Disruptions. Journal of Clinical Child & Adolescent Psychology, 46(2), 269–283. 10.1080/15374416.2016.1188702 [DOI] [PubMed] [Google Scholar]
- Vertiz E, & Herrick D (n.d.). Data analysis: Melissa Saphir, Ph.D., Saphir Research. 32. [Google Scholar]
- Viner RM, Gireesh A, Stiglic N, Hudson LD, Goddings A-L, Ward JL, & Nicholls DE (2019). Roles of cyberbullying, sleep, and physical activity in mediating the effects of social media use on mental health and wellbeing among young people in England: a secondary analysis of longitudinal data. The Lancet Child & Adolescent Health, 3, 685–696. 10.1016/S2352-4642(19)30186-5 [DOI] [PubMed] [Google Scholar]
- Wolfson AR, Carskadon MA, Acebo C, Seifer R, Fallone G, Labyak SE, & Martin JL (2003). Evidence for the validity of a sleep habits survey for adolescents. Sleep, 26(2), 213–216. 10.1093/sleep/26.2.213 [DOI] [PubMed] [Google Scholar]
- Woods HC, & Scott H (2016). #Sleepyteens: Social media use in adolescence is associated with poor sleep quality, anxiety, depression and low self-esteem. Journal of Adolescence, 51, 41–49. 10.1016/j.adolescence.2016.05.008 [DOI] [PubMed] [Google Scholar]
- Yang J, Guo Y, Du X, Jiang Y, Wang W, Xiao D, Wang T, Lu C, & Guo L (2018). Association between Problematic Internet Use and Sleep Disturbance among Adolescents: The Role of the Child’s Sex. International Journal of Environmental Research and Public Health, 15(12), 2682. 10.3390/ijerph15122682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu L, Buysse DJ, Germain A, Moul DE, Stover A, Dodds NE, Johnston KL, & Pilkonis PA (2011). Development of short forms from the PROMIS™ sleep disturbance and Sleep-Related Impairment item banks. Behavioral Sleep Medicine, 10(1), 6–24. 10.1080/15402002.2012.636266 [DOI] [PMC free article] [PubMed] [Google Scholar]