Abstract
Introduction:
An ED visit for opioid overdose may be a person’s only contact with the medical and behavioral health care systems and is an important opportunity to reduce risk of subsequent overdose and death. While ED initiatives to engage people with opioid use disorder (OUD) are being increasingly implemented, there are significant gaps in the receipt of services at the time of the ED encounter.
Methods:
This is a retrospective cohort study of an outreach pilot project providing real-time telehealth delivered buprenorphine initiation and referral to community harm reduction and addiction treatment services via a follow up telephone call to patients after an ED visit for an opioid overdose.
Results:
From January 2020 to April 2021 there were 606 patients with an ED visit for an opioid overdose eligible for a callback. Of the 606 eligible patients, 254/645 (42%) patients could be contacted and accepted service and/or treatment referrals. Fifteen patients were connected same-day to a buprenorphine prescriber for a telehealth encounter and, of connected patients, nine received a buprenorphine prescription.
Conclusion:
A post-ED follow up telephone call protocol is an opportunity to improve treatment engagement and access to buprenorphine for patients at high risk for opioid overdose and death.
Keywords: opioid use disorder, overdose, medications for opioid use disorder, telehealth, buprenorphine treatment, healthcare access
1.0. Introduction:
After an emergency department (ED) visit for opioid overdose, patients are at extremely high risk for recurrent overdose and death. North American studies estimate between a 5.3% to 9.4% risk of all-cause mortality within one year after treatment in the ED for an opioid overdose.[1-3] An ED visit for opioid overdose may be a person’s only contact with the medical and behavioral health care systems and is an important opportunity to reduce risk of subsequent overdose and death. While ED initiatives to engage people with opioid use disorder (OUD) are being increasingly implemented across the United States, there are significant gaps in the receipt of services at the time of the ED encounter.
During the COVID-19 pandemic, gaps in treatment access have widened and opioid overdose fatality has increased across the United States.[4] Although the COVID-19 pandemic threatens everyone, it poses extremely grave risk to those with opioid use disorders who are already marginalized and experience significant barriers to addiction treatment.[5] Compounding already limited access, during COVID-19 many treatment facilities decreased treatment hours and services availability and to minimize risk of COVID-19 exposure, many people have been reluctant to attend in-person treatment appointments. In many places, ED visits for opioid overdose increased despite overall reduced ED patient volumes,[6] highlighting the importance of the ED clinical encounter in providing harm reduction services and treatment initiation for people with opioid use disorder. However, not all ED patients treated after an opioid overdose are interested or ready to initiate medication for opioid use disorder. This may reflect the discomfort and trauma of having experienced an overdose, fear of precipitated withdrawal associated with buprenorphine initiation closely following use, lack of readiness to engage in treatment, or negative, stigmatizing, or traumatizing experiences within the healthcare system, which can erode trust.
In light of the additional barriers to accessing clinical care during the COVID-19 pandemic, the Drug Enforcement Administration (DEA) temporarily waived the requirement that buprenorphine be prescribed only after an in-person examination, allowing prescribers who are otherwise permitted to prescribe buprenorphine for OUD to initiate buprenorphine treatment via telehealth (video or audio-only) encounters.[7] Given the limitations in treatment access related to COVID-19 and new regulations allowing for buprenorphine initiation via telephone-only telehealth encounters, we developed a post opioid overdose outreach pilot project to try to improve provision of harm reduction services and addiction treatment to ED patients treated for an opioid overdose. The overall goal of the project was to assess the utility of a follow up telephone call to provide harm reduction services and addiction treatment initiation to patients treated in the ED for an opioid overdose.
2.0. Methods:
This is a retrospective cohort study of an ED-callback pilot project providing real-time telehealth delivered buprenorphine initiation and referral to community harm reduction and addiction treatment services for ED patients treated for an opioid overdose.
2.1. ED-Callbacks Pilot Project
Trained research assistants made outreach calls to individuals treated for an opioid overdose at two Rhode Island Lifespan adult emergency departments from January 2020 to April 2021. Calls were initiated in April 2020 after changes in federal telehealth regulations allowing for audio-only buprenorphine treatment initiation and conducted through June, 2021. Patients were identified using a pre-existing departmental quality improvement database which is maintained by an ED quality nurse and populated through electronic health record chart review. ED opioid overdose cases reviewed for inclusion in the database are identified using a broad search query including visits where naloxone was administered, distributed, or prescribed and visits with chief complaints of altered mental status, drug overdose, overdose, or cardiac arrest and discharge diagnosis of opioid overdose, drug overdose, or cardiac arrest. Quality nurses review each visit identified by the query to determine if it fit the case definition of opioid overdose, which is any overdose resulting in respiratory depression involving prescribed or non-prescribed opioids.
Patients were not called if the overdose was intentional, the patient required an interpreter, no phone number was listed in the electronic health record, the patient was incarcerated at the time of ED visit, or was documented as deceased in the electronic health record at time of planned callback. Research assistants made three call attempts for each patient with a working phone number trying different times of day and day of the week. After three attempts, patients were taken off the call list. At the start of the study, April 2020, a backlog of patients who had been seen in the ED for an opioid overdose since January 2020 who met study inclusion criteria were called. During the study period a weekly query of ED overdose cases was performed and added to the research assistant call list for ongoing call outreach.
For patients who could be contacted, research assistants followed a call script with branching logic based on patient responses. All patients reached via phone were offered naloxone, harm reduction resources (syringe services programs, naloxone distribution and home delivery, fentanyl test strips) peer recovery programs, and treatment referrals with local COVID-19 specific updates about services availability. Patients without health insurance were directed to resources to help them obtain health insurance during a expanded enrollment period during the pandemic. Depending on patient preferences, requested resources were provided over the phone, texted, or sent via traditional mail or email.
All patients were asked if they were interested in speaking with a physician for a real-time telehealth encounter to initiate buprenorphine. Interested patients were connected with an x-waivered physician for a telephone-only telehealth encounter and, if clinically appropriate, provided buprenorphine and naloxone prescriptions, instructions for unobserved initiation, and linkage to an outpatient provider for maintenance treatment.
2.2. Study Outcomes and Analysis
The primary outcome was successful initiation of buprenorphine via real-time telephone encounter. Secondary outcomes were the ability to reach patients via a telephone and receipt of referral to community treatment and harm reduction services.
For patients receiving a buprenorphine prescription, we performed chart review to determine whether they had attended a follow up appointment within our health system and queried the PDMP to determine if participants received a subsequent buprenorphine prescription within 30 days of the end of the prescription provided through the callbacks pilot. Data was analyzed in aggregate as proportions of total participants. This study was approved by the Lifespan and Rhode Island Department of Health Institutional Review Boards.
3.0. Results:
From January 2020 to April 2021 there were 855 patients treated in the ED for unintentional opioid overdose (See Figure 1). Twenty-nine percent (249/855) were excluded due to no incorrect, missing, or not working phone number, need for an interpreter, or being incarcerated, deceased status, or previous call-back. Twenty-seven patients were documented as deceased in the EHR (3%) at the time of call attempt. This left a sample of 606 patients eligible for a call-back. See Table 1 for baseline demographics and characteristics of study call-back eligible patients.
Figure 1.
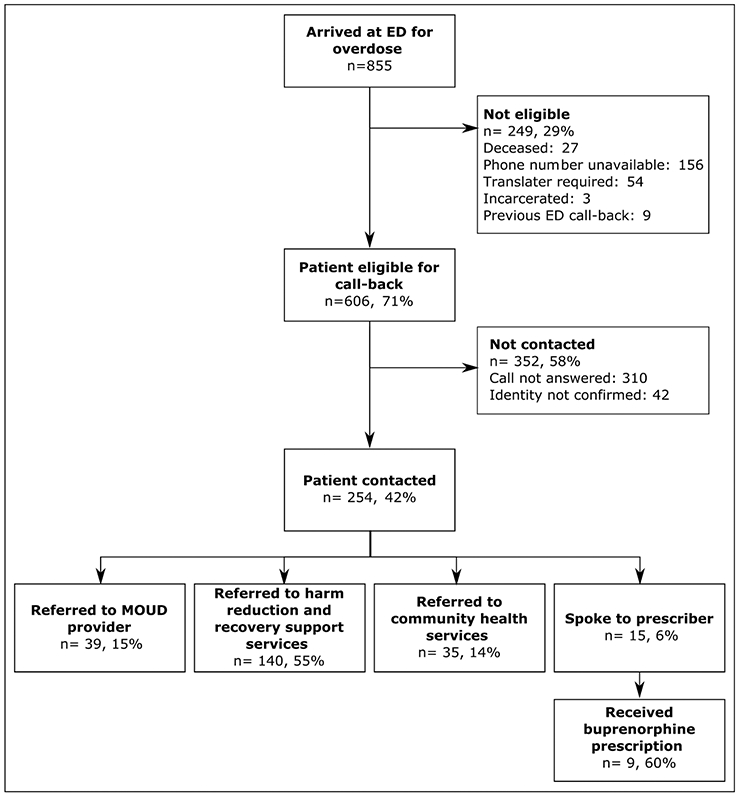
Flow diagram of patients in the ED Call-back Pilot program, January 2020 to April 2021
Table 1:
Baseline characteristics of individuals with attempted or successful call-back following opioid overdose related-Emergency Department visit, Jan 2020 – April 2021
| Total (n=606) | Contact outcome |
||
|---|---|---|---|
| Contacted (n=254) | Not contacted (n=352) | ||
| Age (mean, (SD)) | 36 (29, 47) | 37 (29, 49) | 36 (29, 46) |
| Gender* | |||
| Male | 414 (68) | 163 (64) | 251 (71) |
| Female | 191 (32) | 91 (36) | 100 (28) |
| Race† | |||
| White | 465 (78) | 199 (79) | 266 (76) |
| Black/African America | 65 (11) | 27 (11) | 38 (11) |
| Native American/American Indian | 2 (0) | 0 (0) | 2 (1) |
| Asian | 8 (1) | 2 (1) | 6 (2) |
| Unknow | 5 (1) | 2 (1) | 3 (1) |
| Other | 55 (9) | 22 (9) | 33 (9) |
| Ethnicity‡ | |||
| Non-Hispanic or Latin | 520 (87) | 222 (88) | 298 (87) |
| Hispanic or Latinx | 70 (12) | 29 (12) | 41 (12) |
| Refused | 5 (1) | 1 (0) | 4 (1) |
| Language§ | |||
| English | 541 (99) | 239 (100) | 302 (99) |
| Spanish | 3 (1) | 0 (0) | 3 (1) |
| Other | 1 (0) | 0 (0) | 1 (0) |
| Insurance¶ | |||
| No | 62 (11) | 19 (8) | 43 (13) |
| Yes | 510 (89) | 227 (92) | 283 (87) |
| Hospital# | |||
| RIH | 289 (67) | 127 (69) | 162 (66) |
| TMH | 142 (33) | 57 (31) | 85 (34) |
Missing data:
one participants
six participants
11 participants
61 participants
34 participants
175 participants
More than half (58%, 352/606) could not be contacted. Of the 606 eligible patients, research assistants were able to connect on the phone with 254/606 (42%) patients. The median time from ED visit for overdose to last call for patient successfully contacted was 39 days (IQR: 20, 70), and the median Time to last call for those who could not be contacted was 32.5 days (IQR:21, 65). Overall, the time to last call was 34 days (21, 67.5). Of the 254 patients who were reached over the phone 140 (55%) were referred to harm reduction and recovery support services, 35 (14%) were referred to community health services, and 39 (15%) were referred to a MOUD provider (methadone, buprenorphine, and/or naltrexone treatment options based on participant preference at the time of call). Fifteen patients spoke to a buprenorphine prescriber at the time of the call. Nine were prescribed buprenorphine during the telehealth encounter. Of those prescribed buprenorphine, 89% (8/9) attended a follow up appointment in our health system and 56% (5/9) filled a subsequent buprenorphine prescription within 30 days.
4.0. Discussion:
An ED visit for opioid overdose is a critical opportunity to provide lifesaving harm reduction services and medications for OUD. About 1 in 20 patients treated for a nonfatal opioid overdose in an ED die within 1 year of their visit, many within 2 days.[3] However, an ED visit after an opioid overdose can be extremely stressful and not every individual will be ready or able to engage with ED harm reduction and/or treatment services such as buprenorphine initiation, naloxone distribution, and behavioral counseling. Patients may be suffering trauma from their overdose experience and/or precipitated withdrawal. Our departmental standard of care is to offer all patients that experience an opioid overdose take-home naloxone, consultation with a peer recovery specialist, referral to substance use disorder treatment programs offering MOUD (methadone, buprenorphine, and naltrexone), and harm reduction resources. Additionally, as long as there are no contraindications, patients with opioid overdose are offered buprenorphine in the ED if they are in withdrawal at the time of visit or for patients not yet in withdrawal a prescription for unobserved buprenorphine initiation is offered. Despite these ongoing efforts in the ED our study finding that 3% of all patients presenting to the Emergency Department after an opioid overdose are documented as deceased in the medical record within a few months further emphasizes the urgent need to create alternate avenues for outreach to engage patients after opioid overdose. Increased flexibility around buprenorphine prescribing related to the COVID-19 pandemic created the opportunity to trial a novel approach to provide harm reduction and treatment services to people who recently experienced an overdose outside the acute post-overdose period and traditional healthcare environment.
Overall patients, who could be contacted, expressed appreciation for the follow up call. Of patients who could be reached, over half accepted referral to harm reduction and recovery support services, fourteen and sixteen percent of patients accepted community resources and referral to an MOUD provider respectively. Fifteen patients (6% of all patients who could be contacted) expressed interest and were successfully connected to a provider for a same-day telehealth encounter for evaluation of possible buprenorphine initiation. Most patients connected with a provider for a telehealth encounter voiced that they would not have otherwise entered treatment. Multiple patients were on their way to purchase illicit opioids for use and/or self-treatment of withdrawal symptoms when they received the call from the research assistant. Although patients were not asked why they did not want to speak to a buprenorphine prescriber, possible reasons include lack of time, they had already started treatment, or may not have been ready to start treatment at the time of the call.
Treatment of OUD with buprenorphine decreases mortality in people with OUD by approximately 50%[8] and confers numerous other personal health and social benefits including reduced illicit drug use, maintenance of employment, and improved birth outcomes. Despite its proven efficacy, fewer than 35% of people with OUD receive any form of addiction treatment, and only a fraction of those are treated with medications.[9] Providing a telephone assessment bypasses many barriers to treatment initiation. Patients are able to connect to a treatment provider in real-time and do not have to accommodate clinic hours, prescriber availability, or transportation limitations.
This innovative pilot project helps to address stigma and connect with a difficulty to reach, vulnerable patient population at high risk for death. This callback pilot study highlights a model for additional outreach and treatment engagement for patient after an ED visit for a non-fatal opioid overdose. Future study is warranted to evaluate if a callback affects patient outcomes including treatment engagement, recurrent drug overdose, and mortality. Areas of improvement to be trialed and investigated include differences in services acceptancy by the time between the ED visit and the follow up call and if there are improvement in services uptake if follow up calls are made by a community health worker or peer recovery specialist.
5.0. Limitations:
Many patients were unable to be contacted due to either incorrect contact information listed in the electronic health record or a lack of a working phone number. In future more robust registration efforts and/or having a research assistant or Peer Recovery Specialist stationed in the Emergency Department to establish contact with a patient and document a working phone number or other preferred contact modality could increase contact post-ED visit. Patients were recorded as deceased if the research assistant was informed of such information over the phone when attempting to contact a patient or if deceased status was listed in the EHR at the time of planned callback. As a result, the number of deceased patients identified through patient callbacks is likely an underestimate of true mortality after opioid overdose in this patient population. Unfortunately, over the phone interpreter services were not available in this pilot limiting the population that could be contacted to only individuals speaking English. This is particularly important given increasing rates of opioid-related mortality among Spanish speaking communities in Rhode Island.[10] Future efforts should include telephone interpreter services to improve reach to non-English speaking patients. Finally, continued telehealth delivered buprenorphine may not be possible in the future after the COVID-19 pandemic if federal legislation allowing for use of telehealth for buprenorphine initiation or continuance of the telehealth exceptions put in place during COVID-19 pandemic is not enacted.
6.0. Conclusion:
A post-ED follow up telephone call protocol is an opportunity to improve treatment engagement and access to buprenorphine for patients at high risk for opioid overdose and death.
Funding:
This work was supported by the Rhode Island Department of Health and Department of Behavioral Healthcare, Developmental Disabilities and Hospitals through a SAMHSA Emergency Grant to Address Mental and Substance Use Disorders During COVID-19. Dr. Wightman is partially supported by the National Institute of General Medical Sciences of the NIH under grant number P20GM125507. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Dr. Samuels is partially supported by Institutional Development Award Number U54GM115677 from the National Institute of General Medical Sciences of the National Institutes of Health, which funds Advance Clinical and Translational Research (Advance-CTR).
This work was presented at the Annual Scientific Meeting of the American College of Medical Toxicology, April 14th, 2021. Remote due to COVID-19.
Footnotes
Conflict of interest
All authors declarations of interest: none
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- [1].Boscarino JA, Kirchner HL, Pitcavage JM, Nadipelli VR, Ronquest NA, Fitzpatrick MH, et al. Factors associated with opioid overdose: a 10-year retrospective study of patients in a large integrated health care system. Subst Abuse Rehabil 2016;7:131–41. 10.2147/SAR.S108302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Leece P, Chen C, Manson H, Orkin A, Schwartz E, Juurlink D, et al. One-Year Mortality After Emergency Department Visit for Nonfatal Opioid Poisoning: A Population-Based Analysis. Ann Emerg Med 2020;75. 10.1016/j.annemergmed.2019.07.021. [DOI] [PubMed] [Google Scholar]
- [3].Weiner SG, Baker O, Bernson D, Schuur JD. One-Year Mortality of Patients After Emergency Department Treatment for Nonfatal Opioid Overdose. Ann Emerg Med 2020;75:13–7. 10.1016/j.annemergmed.2019.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Products - Vital Statistics Rapid Release - Provisional Drug Overdose Data 2017. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm (accessed November 28, 2017).
- [5].Alexander GC, Stoller K, Haffajee R, Saloner B. An Epidemic in the Midst of a Pandemic: Opioid Use Disorder and COVID-19. Ann Intern Med 2020;M20–1141. 10.7326/M20-1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Soares WE, Melnick ER, Nath B, D’Onofrio G, Paek H, Skains RM, et al. Emergency Department Visits for Nonfatal Opioid Overdose During the COVID-19 Pandemic Across Six US Health Care Systems. Ann Emerg Med 2021:S0196064421002262. 10.1016/j.annemergmed.2021.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].DEA Policy: Use of Telephone Evaluations to Initiate Buprenorphine Prescribing 2020. https://www.deadiversion.usdoj.gov/GDP/(DEA-DC-022)(DEA068)%20DEA%20SAMHSA%20buprenorphine%20telemedicine%20%20(Final)%20+Esign.pdf (accessed April 23, 2020).
- [8].Sordo L, Barrio G, Bravo MJ, Indave BI, Degenhardt L, Wiessing L, et al. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ 2017;357. 10.1136/bmj.j1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Jones CM, McCance-Katz EF. Co-occurring substance use and mental disorders among adults with opioid use disorder. Drug Alcohol Depend 2019;197:78–82. 10.1016/j.drugalcdep.2018.12.030. [DOI] [PubMed] [Google Scholar]
- [10].Race & Ethnicity – Prevent Overdose Rl n.d. https://preventoverdoseri.org/race-ethnicity-data/ (accessed June 25, 2021). [Google Scholar]


