Abstract
Purpose
The purpose of the study was to analyze the dimensions of socket morphology, interradicular bone dimensions, root length and morphology, buccal cortical bone thickness and gap defect between the implant bone in mandibular molars with cone beam computed tomography (CBCT) for immediate molar implant (IMI) placement.
Materials and methods
Sample sizes of 300 mandibular 1st and 2nd molars were each selected from the CBCT scans by inclusion and exclusion criteria. CBCT measurements were performed for socket size morphology, mesiodistal width, and buccolingual cancellous bone width at the crest at the apex. Width of the buccal cortical plate at the crest and interradicular bone (IRB) at the apex, 3 mm cervical to the apex and 6 mm cervical to the apex. Vertical parameters from the crest to furcation (L1), length from furcation to the apex (L2) and mesiodistal root morphology were measured to analyze the root configuration.
Results
All the parameters were analyzed for descriptive statistics for the mean and standard deviation. The majority were of Type B and C socket morphology with peri-implant bone defects of 2–2.5 mm, and the interradicular bone septum (IRB) was moderate for both first molar (1 M) and second molar (2 M) sites, but 2 M was shown to have less IRB than 1 M. Adequate buccal cortical bone thickness of 1.1 mm to 1.4 mm and buccolingual cancellous bone width were measured for both the 1 M and 2 M sites.
Conclusion
The morphology of the molar extraction socket determines the adequate stability for IMI. In mandibular molar teeth, where interradicular bone is incompetent in providing good primary stability, in addition to interradicular bone, clinicians should look for support from the apical bone and interdental septal bone for attaining primary stability of IMI.
Keywords: Immediate molar implants, Interradicular bone, Primary stability, CBCT analysis, Socket morphology
1. Introduction
Immediate molar implants are gaining acceptance in the restoration of missing teeth with a high rate of clinical success. Accurate imaging modalities (CBCT) (Ganguly et al., 2011, Shaikh and Shaikh, 2018), innovative implant treatment planning software, and advanced surgical and prosthetic techniques have made it possible for the success of implants (Alaqeely et al., 2020, Kämmerer et al., 2014). There is growing recognition of IMI by patients and clinicians since the waiting period after extraction is less and is anticipated to maintain bone volume and to improve aesthetic sequelae.
Concurrently, the timing of implant placement after extraction has become a debatable issue with respect to primary stability and osseointegration. Studies have shown a favorable survival rate in IMI if the extraction technique is atraumatic and a minimum gap is maintained between the bone and implant surface since the main difference occurs during the initial stage of osseointegration for the success of the implant (Ebenezer and Balakrishnan, 2015, Schwartz-Arad et al., 2000, Suarez et al., 2013). In contrast, delayed implant placement minimizes failure and complications, which are due to ample alveolar bone remodeling (Antetomaso and Kumar, 2018, Esposito et al., 2010). Primary stability of IMI depends upon the area of implants to be placed. Implants placed immediately into the extraction sites, especially in the anterior or premolar region, offer 100% primary stability because of the smaller socket size and lesser amount of load taken by these implants (Atieh et al., 2013). In the molar region, this perception is controversial; compared to the available implant diameter, the socket size is large. (Smith et al., 2019). Three types of extraction sockets (A, B and C) are proposed based on the amount of bone available within the socket for stability of IMI: “Type A - the implant is completely within the septal bone, without gaps between the implant and the socket walls; Type B - the implant has enough but incomplete septal bone, leaving gaps; and Type C - insufficient septal bone, thus the implant engages the periphery of the socket” (Smith and Tarnow, 2013). As compared to healed sites, there is a higher implant failure rate for implants placed in fresh extraction sockets (Khouly and Keenan, 2015). However, a systematic and meta-analysis review reported no significant difference between immediate or delayed implant insertion and no differences for site specificity in implant failure. (Chrcanovic et al., 2015).
In IMI, primary stability is achieved from interradicular bone and apical threads. The failure of IMI will be higher if the factors as the socket morphology, root length and configuration, buccal cortical bone thickness, and gap defect between implant-bone and interradicular septa are not considered. Other parameters, such as the quality and quantity of bone, atraumatic surgical technique and traumatic occlusal forces, play a role in implant success. (McAllister and Haghighat, 2007, Padhye and Shirsekar, 2019, Rominger and Triplett, 1994). Because there is scant available literature, the aim of the present study was to measure the alveolar bone dimensions responsible for primary stability in mandibular molars for IMI success. The hypothesis tested is for the inadequacy of interradicular bone dimensions of mandibular molars after extraction for IMI.
The objective of the present study was to analyze the socket morphology, interradicular bone dimensions, root length and morphology, buccal cortical bone thickness and gap defects between the implant bone in mandibular molars.
2. Materials and methods
2.1. Subjects
This cross-sectional, retrospective study design underwent formal review and received ethical approval (DRC/008FA/20) from the institutional review board of College of Dentistry in Alrass, Saudi Arabia. The CBCT images were obtained from the archives of the Dento-maxillofacial radiology department. The inclusion criteria were CBCT images of the complete mandible of permanent dentition with healthy mandibular 1st and 2nd molars along with healthy periodontium. Any partial or incomplete images, patients with any pathology in the mandible, such as caries, periapical pathology, cysts, tumors, bony sclerosis, and impacted teeth, 3rd molars, were excluded from the study. All scans were assessed for eligibility against the selection criterion.
2.2. CBCT imaging and analysis
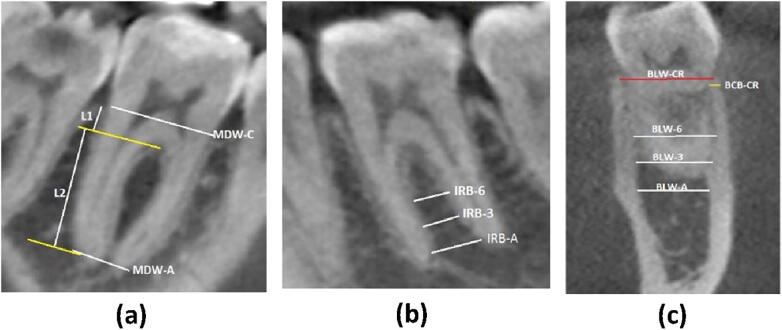
A total of 272 CBCT scans were selected initially, and after the inclusion and exclusion criteria, 201 scans were selected for the study. From these, a sample size of 300 each for the 1st and 2nd molars was selected. All scans were standardized (Galileo’s comfort Sirona Dental Systems GmbH, Blenheim, Germany) with scan parameters of 85 KvP, 21 mAs and 14 sec scan time with FOV of 15 × 15 × 15 cm3 and voxel size 0.3 mm3. All scans were taken in high-definition mode and with Metal Artifact Reduction Software. The data were reconstructed in slices of 1 mm intervals and analyzed using proprietary software (Sidexis 4). A complete image of the molar was opened and aligned in all three sections. Table 1 shows the alveolar bone parameters to be measured. These measurements were performed in sagittal and cross-sections as shown in Fig. 1b, 1b & 1c.
Table 1.
Measured Parameters for 1 M and 2 M sites.
| Parameters Measured | Acronyms |
|---|---|
| Socket Size Morphology | |
| Mesio-distal Width at the Crest | MDW-C |
| Bucco-lingual Width at the Crest | BLW-CR |
| Mesio-distal Width at the Apex (Root tip Morphology – Convergence/Divergence) | MDW-A |
| Vertical Root Length Parameters: | |
| Length from the Crest of Interdental Bone to the Tangent from Furcation | L1 |
| Length from the Tangent of Furcation to the Tangent at Root Apex (Interradicular Septum Bone Length | L2 |
| Total root Length (L1 + L2) | L3 |
| Buccal Cortical Bone Thickness | |
| Buccal Cortical Bone Thickness at the Crest | BCB-CR |
| Interradicular Septal Bone Morphology | |
| Mesio-distal Width at Apex | IRB-A |
| Mesio-distal Width Cervically 3 mm from the Apex | IRB-3 |
| Mesio-distal Width Cervically 6 mm from the Apex | IRB-6 |
| Radicular Bucco-Lingual Width (BLW) of Cancellous Bone Measurements | |
| Bucco-lingual Width (BLW) of Cancellous Bone at the Apex | BLW-A |
| Bucco-lingual Width (BLW) of Cancellous Bone Cervically 3 mm from the Apex | BLW-3 |
| Bucco-lingual Width (BLW) of Cancellous Bone Cervically 6 mm from the Apex | BLW-6 |
Fig. 1.
Measured Parameters of 1 M and 2 M. a: CBCT image of first molar showing measurements L1 (length from crest to furcation) L2 (length from furcation to root apex. In addition, mesio-distal socket width at crest. (MDW-C). b: Mesio-distal interradicular septal bone measurements, (IRB -A, at apex), (IRB −3 3 mm cervical to apex) & (IRB-6) 6 mm cervical to apex).. c: CBCT image of first molar showing BCB-CR, Bucco-lingual socket width at crest (BLW-CR) and BLW of ridge at root apex, 3 mm cervical to root apex & 6 mm cervical to root apex).
All measurements were performed by two qualified observers. Both observers were blinded regarding the aim of the study and received a calibration session prior to the initiation of image evaluation and a training session to understand the various functions of the software. In the event of disagreement between the two observers, cases were discussed until consensus was reached. To analyze interobserver agreement, two measurements were repeated at two different time points for each scanned volume.
2.3. Statistical analysis
All the parameter data were entered into SPSS v.11.5 Software (SPSS Inc., Chicago, IL, USA) for the analysis of descriptive statistics for the mean and standard deviation.
The Kappa value for interexaminer reliability was 0.9.
3. Results
The following mean with standard deviation was obtained for the mandibular 1st molar and 2nd molar as mentioned in Table 2:
Table 2.
Alveolar bone Measurement Readings.
| Mandibular 1st molar (1 M) with n = 300 |
Mandibular 2nd molar (2 M) with n = 300. |
|||||||
|---|---|---|---|---|---|---|---|---|
| Acronym | Min | Max | Mean | Std. Deviation | Min | Max | Mean | Std. Deviation |
| MDW-C | 7.01 | 11.09 | 9.3230 | 0.74785 | 0.26 | 11.09 | 9.1484 | 0.92448 |
| BLW-CR | 7.23 | 10.98 | 8.8969 | 0.78684 | 7.27 | 10.65 | 8.8775 | 0.75076 |
| MDW-A | 4.09 | 10.46 | 7.0442 | 1.49895 | 2.55 | 8.62 | 5.6906 | 1.70465 |
| L1 | 1.70 | 4.75 | 2.9901 | 0.49734 | 1.20 | 6.86 | 2.9775 | 0.65525 |
| L2 | 7.21 | 13.81 | 10.0748 | 1.21509 | 4.10 | 14.05 | 9.2724 | 1.40289 |
| L3 | 10.21 | 16.79 | 13.0649 | 1.30230 | 8.05 | 18.11 | 12.2499 | 1.40571 |
| BCB-CR | 0.75 | 2.12 | 1.1556 | 0.25507 | 0.86 | 2.90 | 1.3382 | 0.38281 |
| IRB-A | 0.65 | 7.13 | 3.7303 | 1.31711 | 0.00 | 6.56 | 2.3480 | 1.37495 |
| IRB-3 | 1.21 | 6.18 | 3.3947 | 1.01280 | 0.00 | 5.08 | 2.2400 | 1.06730 |
| IRB-6 | 1.20 | 5.96 | 3.1962 | 0.76896 | 0.00 | 5.08 | 2.1163 | 0.88789 |
| BLW-A | 3.63 | 12.17 | 7.8688 | 1.60742 | 3.56 | 13.04 | 8.4193 | 1.73886 |
| BLW-3 | 3.39 | 12.82 | 8.2560 | 1.41010 | 3.65 | 13.86 | 9.0423 | 1.61325 |
| BLW-6 | 5.44 | 12.82 | 8.4150 | 1.24321 | 4.20 | 16.19 | 9.3207 | 1.62880 |
3.1. Socket size morphology
1M: - The mean mesio-distal width at the crest (MDW-C) was 9.32 ± 0.74 mm, and the mean bucco-lingual width at the crest (BLW-CR) was 8.8 ± 0.78 mm. The mean mesio-distal width of roots at the apex (MDW-A) was 7.0 ± 1.4 mm.
2M: - The mean MDW-C was 9.1 ± 0.92 mm, mean BLW-CR was 8.8 ± 0.75 mm and mean MDW-A was 5.6 ± 1.7 mm.
3.2. Trunk length
1M: - The mean length from the crest of the bone to the tangent from furcation (L1) was 2.99 ± 0.49 mm, and the mean length from the tangent of furcation to the root apex (L2) was 10.07 ± 1.2 mm. L3, the total mean length of the bone root (L1 + L2) was 13.06 ± 1.3 mm.
2M: - The mean trunk length (L1) was 2.97 ± 0.65 mm and (L2) was 9.2 ± 1.4 mm. L3, the mean total length of the bone root (L1 + L2) was 12.24 ± 1.4 mm.
3.3. Buccal cortical bone thickness at crest
1M: - The mean BCB-CR was 1.15 ± 0.25 mm.
2M: - The mean BCB-CR was 1.33 ± 0.38 mm.
3.4. Intraradicular septal bone measurements
1M: - The mean mesio-distal width of the septum at the apex (IRB-A) was 3.73 ± 1.31 mm and mesio-distal width cervically was 3 mm from the apex (IRB-3) and was mean 3.394 ± 1.01 mm. The cervical mesio-distal width was 6 mm from the apex (IRB-6) and was mean 3.19 ± 0.76 mm.
2M: - The mean IRB-A was 2.34 ± 1.37 mm, mean IRB-3 was 2.24 ± 1.06 mm and mean IRB-6 was 2.11 ± 0.88 mm.
3.5. Radicular bucco-lingual width of cancellous bone
1M: - At the apex, mean (BLW-A) bone was 7.8 ± 1.6 mm, cancellous bone cervically (towards the trunk) was 3 mm from the apex (BLW-3) and was mean 8.2 ± 1.01 mm, and the bucco-lingual width of cancellous bone cervically was 6 mm from the apex (BLW-6) and was mean 8.4 ± 1.24 mm.
2M: - At the apex, mean (BLW-A) bone was 8.4 ± 1.73 mm, mean cancellous bone BLW-3 was 9.04 ± 1.61 mm and mean BLW-6 was 9.6 ± 1.61 mm.
4. Discussion
The present CBCT analysis was carried out to measure the bone support from the extraction socket and interradicular septa in providing primary stability of IMI. Reports of previous studies have shown that the interdental, buccal & lingual cortical bone and interradicular septal bone are primary factors for implant stability and success rate, provided that co-factors, such as tooth morphology, atraumatic extraction with IRB preservation techniques, length, diameter and angulation of implants and presurgical CBCT analysis are taken into consideration (Braut et al., 2012, Chrcanovic et al., 2015, Agostinelli et al., 2018, Lin et al., 2014).
4.1. The molar extraction socket morphology
The socket framework is vital to successful IMI outcomes. The type and size of the socket and trunk, lateral bone (bucco-lingual and mesio-distal) and apical bone (from the interdental crest to interradicular crest) play critical roles in IMI placement and stability.
The results in the present study showed that the coronal socket size was Type B with moderate mesio-distal size and buccolingually suggestive of peripheral defects of approximately 2–2.5 mm. These findings are similar to those reported in the literature, where if the gap defect is less than 2 mm, natural bone healing can be predicted without the need for grafting (Chen et al., 2009, Fugazzotto, 1998, McAllister and Haghighat, 2007). However, if the gap is greater, then guided bone regeneration and soft tissue augmentation are indicated (Rominger and Triplett, 1994, Schliephake et al., 2000, Simion et al., 1994).
The trunk length (the crest to furcation length) is normally unsupported in IMI. This will be further complicated if there is thin and resorbed crestal bone or lateral bone, making implant placement and its success difficult (Matarasso et al., 2009). Our study findings showed moderate mean LI measurements of 2.99 ± 0.49 mm for M1 and 2.98 ± 0.65 for M2, and the calculated peripheral defect was 2–2.5 mm along the trunk area of the implant. “Lesser the gap defect around the implant and more the lateral and apical bone support, higher the stability of implants and hence higher success rate”. If the lateral and apical bone support is compromised, then a delayed implant placement protocol should be opted (Smith and Tarnow, 2013). In contrast, others reported larger gap defects between the implant and bone after extraction and proposed greater amounts of new bone formed or no difference with narrow gaps (Botticelli et al., 2004, Ferrus et al., 2010).
4.2. The root length and the interradicular bone length
It is a general concept that the longer the length is, the better the stability of implants is, and the same applies for IMI. The average length of the lower molar roots is 14–16 mm (Akhlaghi et al., 2017, Dunlap and Gher, 1985, Shakil et al., 2014). IMI uses an interradicular septum for initial stability. In the present study, the mean L3 values were 13.06 ± 1.31 mm for 1 M and 12.25 ± 1.41 mm for 2 M. If the implant length is decreased by 40%, the implant anchorage is reduced by 50% (Ueno et al., 2010), and the implant should be placed into a minimum of 3 mm of bone apical to the extraction site (Esposito et al., 2007, Schwartz-Arad and Chaushu, 1997, Werbitt and Goldberg, 1992).
4.3. Buccal cortical bone thickness at the crest
In the present study, the mean BCB-CR thickness for 1 M was 1.156 ± 0.26 mm and that for 2 M was 1.338 ± 0.382 mm. If the BCB-CR thickness is less than 1.8 mm and the BLW of the ridge is compromised, wider or ultra-wide implants should be avoided to prevent marginal bone loss. In cases of deficient thickness, it is preferable to place an implant submerged or to plan for lingual angulation (Tomasi et al., 2010) or to delay placement of the implant. Submerging the implant may also enhance osteointegration (Huang et al., 2015). In the present study, the mean BCB-CR thickness of the 2nd molar was higher than that of the 1st molar sites, suggesting a favorable result for 2 M for IMI. Similar study results were reported for maximum thickness in the 2nd molar area, and the mean alveolar bone height was less in the molar (14.5 mm) area (Soman et al., 2019).
4.4. Interradicular septum morphology
Mesio-distal IRB width in this study was moderately sufficient at the apex and towards furcation up to 6 mm cervical for 1 M and insufficient for 2 M sites (Table 2). These results suggest that the majority of extraction sockets were Type B in 1 M and Type C in 2 M. In these types of sockets, IRB, which influences primary stability, will be inadequate if a standard or wider implant is placed in the interradicular bone. In such cases, the primary stability will be provided by buccal, lingual and apical trabecular bone. These results suggest that IRB might affect the insertion torque value and the need to add augmentive procedures for IMI placement.
The present study results also suggest that if wider implants are placed, the gap defect will be minimal, and there is probability of higher quality bone formation during the healing period. Additionally, the BLW was higher in 2 M than in 1 M. In the literature, higher failure rates have been reported with 6–9 mm diameter implants for IMI. They suggested a minimum of 1.8 mm buccal bone thickness remaining after osteotomy, healthier for higher success (Mordenfeld et al., 2004, Ormianer et al., 2012) If IRB is intact and sufficient after extraction with <2 mm of labial peri-implant socket gap, then primary stability will be good; hence, the healing period should be 3 months, and peri-implant grafting is not indicated (Zamad et al., 2015).
4.5. Bucco-lingual ridge width
In this study, the mean thickness of the BLW at the apex and at the crest was greater at 2 M than at 1 M, which is consistent with the results of previous CBCT studies (Braut et al., 2012, Agostinelli et al., 2018). The type of mandibular ridge appeared to be shared equally by Convergent type and Parallel type in both the 1 M and 2 M sites. Other previous studies observed that the most prevalent mandibular ridge was the Undercut- shaped ridge (Chrcanovic et al., 2015, Lin et al., 2014). According to Tian-You Wang (2013), in their simulated results, bone plate perforation was more prevalent in U-shaped ridges and was higher for 2nd molars (Wang et al., 2019). In contrast, the present study found that the 2nd molar shows a better bucco-lingual width than the 1st molar. Hence, it is essential to consider ridge width at the crest and at the tooth apex during treatment planning.
4.6. The root morphology
In the present study, both 1 M and 2 M had moderately wide interdental septa at the apex, compared to crestal socket width, with moderate mesio-distal convergence of roots at the apex. Mandibular 1 M had parallel or slightly convergent root morphology, and mandibular 2 M were more convergent, suggesting that the 2nd molars favored interdental bone support in addition to IRB for IMI. Similar results were reported by previous studies, where 1 M had a thick interdental septum and the roots were either parallel or divergent compared to 2 M (Braut et al., 2012, Agostinelli et al., 2018).
5. Conclusion
The molar extraction socket morphology determines the adequate stability for IMI placement. The interradicular septal bone and molar socket periphery are the primary areas of bone available for IMI placement. In mandibular molar teeth, where interradicular bone is insufficient in providing good primary stability, in addition to interradicular bone, clinicians should look for support from the apical bone and interdental septal bone for attaining primary stability of IMI. There is definite need for a good selection of cases, atraumatic extraction with preservation of IRB and associated regenerative procedures for higher success of immediate molar implants. However further clinical studies with methods to measure primary stability of IMI are needed to validate our conclusions.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Peer review under responsibility of King Saud University.
Contributor Information
Arshad Jamal Sayed, Email: a.sayed@qu.edu.sa, dr.arshad.sayed@qudent.org.
Safia Shoeb Shaikh, Email: dr.safia.shaikh@qudent.org.
Shoeb Yakub Shaikh, Email: dr.shoeb.shaikh@qudent.org.
References
- Akhlaghi N.M., Khalilak Z., Vatanpour M., Mohammadi S., Pirmoradi S., Fazlyab M., Safavi K. Root canal anatomy and morphology of mandibular first molars in a selected Iranian population: an in vitro study. Iran. Endod. J. 2017;12:87–91. doi: 10.22037/iej.2017.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alaqeely R., Babay N., AlQutub M. Dental implant primary stability in different regions of the Jawbone: CBCT-based 3D finite element analysis. Saudi Dent. J. 2020;32:101–107. doi: 10.1016/j.sdentj.2019.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antetomaso J., Kumar S. Survival rate of delayed implants placed in healed extraction sockets is significantly higher than that of immediate implants placed in fresh extraction sockets. J. Evid. Based Dent. Pract. 2018;18:76–78. doi: 10.1016/j.jebdp.2017.12.003. [DOI] [PubMed] [Google Scholar]
- Atieh M.A., Alsabeeha N.H.M., Duncan W.J., de Silva R.K., Cullinan M.P., Schwass D., Payne A.G.T. Immediate single implant restorations in mandibular molar extraction sockets: a controlled clinical trial. Clin. Oral Implants Res. 2013;24:484–496. doi: 10.1111/j.1600-0501.2011.02415.x. [DOI] [PubMed] [Google Scholar]
- Botticelli D., Berglundh T., Lindhe J. Hard-tissue alterations following immediate implant placement in extraction sites. J. Clin. Periodontol. 2004;31:820–828. doi: 10.1111/j.1600-051X.2004.00565.x. [DOI] [PubMed] [Google Scholar]
- Braut V., Bornstein M.M., Lauber R., Buser D. Bone dimensions in the posterior mandible: a retrospective radiographic study using cone beam computed tomography. Part 1–analysis of dentate sites. Int. J. Periodontics Restorative Dent. 2012;32:175–184. [PubMed] [Google Scholar]
- Chen S.T., Darby I.B., Reynolds E.C., Clement J.G. Immediate implant placement postextraction without flap elevation. J. Periodontol. 2009;80:163–172. doi: 10.1902/jop.2009.080243. [DOI] [PubMed] [Google Scholar]
- Chrcanovic B.R., Albrektsson T., Wennerberg A. Dental implants inserted in fresh extraction sockets versus healed sites: a systematic review and meta-analysis. J. Dent. 2015;43:16–41. doi: 10.1016/j.jdent.2014.11.007. [DOI] [PubMed] [Google Scholar]
- Agostinelli Claudio, Agostinelli Agnese, Berardini Marco, Trisi Paolo. Radiological Evaluation of the Dimensions of Lower Molar Alveoli. Implant Dent. 2018;27:271–275. doi: 10.1097/ID.0000000000000757. [DOI] [PubMed] [Google Scholar]
- Dunlap R.M., Gher M.E. Root surface measurements of the mandibular first molar. J. Periodontol. 1985;56:234–238. doi: 10.1902/jop.1985.56.4.234. [DOI] [PubMed] [Google Scholar]
- Ebenezer V., Balakrishnan R. Immediate Vs Delayed Implants: comparative study of 100 cases. Biomed. Pharmacol. J. 2015;8:375–378. [Google Scholar]
- Esposito M., Grusovin M.G., Polyzos I.P., Felice P., Worthington H.V. Cochrane Database Syst; Rev: 2010. Interventions for replacing missing teeth: dental implants in fresh extraction sockets (immediate, immediate-delayed and delayed implants) [DOI] [PubMed] [Google Scholar]
- Esposito M., Grusovin M.G., Willings M., Coulthard P., Worthington H.V. The effectiveness of immediate, early, and conventional loading of dental implants: a Cochrane systematic review of randomized controlled clinical trials. Int. J. Oral Maxillofac. Implants. 2007;22:893–904. [PubMed] [Google Scholar]
- Ferrus J., Cecchinato D., Pjetursson E.B., Lang N.P., Sanz M., Lindhe J. Factors influencing ridge alterations following immediate implant placement into extraction sockets. Clin. Oral Implants Res. 2010;21:22–29. doi: 10.1111/j.1600-0501.2009.01825.x. [DOI] [PubMed] [Google Scholar]
- Fugazzotto P.A. Report of 302 consecutive ridge augmentation procedures: technical considerations and clinical results. Int. J. Oral Maxillofac. Implants. 1998;13:358–368. [PubMed] [Google Scholar]
- Ganguly R., Ruprecht A., Vincent S., Hellstein J., Timmons S., Qian F. Accuracy of linear measurement in the Galileos cone beam computed tomography under simulated clinical conditions. Dento Maxillo Facial Radiol. 2011;40:299–305. doi: 10.1259/dmfr/72117593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang B., Meng H., Zhu W., Witek L., Tovar N., Coelho P.G. Influence of placement depth on bone remodeling around tapered internal connection implants: a histologic study in dogs. Clin. Oral Implants Res. 2015;26:942–949. doi: 10.1111/clr.12384. [DOI] [PubMed] [Google Scholar]
- Kämmerer P.W., Palarie V., Schiegnitz E., Hagmann S., Alshihri A., Al-Nawas B. Vertical osteoconductivity and early bone formation of titanium–zirconium and titanium implants in a subperiosteal rabbit animal model. Clin. Oral Implants Res. 2014;25:774–780. doi: 10.1111/clr.12175. [DOI] [PubMed] [Google Scholar]
- Khouly I., Keenan A.V. Review suggests higher failure rates for dental implants placed in fresh extraction sites. Evid. Based Dent. 2015;16:54–55. doi: 10.1038/sj.ebd.6401098. [DOI] [PubMed] [Google Scholar]
- Lin M.-H., Mau L.-P., Cochran D.L., Shieh Y.-S., Huang P.-H., Huang R.-Y. Risk assessment of inferior alveolar nerve injury for immediate implant placement in the posterior mandible: a virtual implant placement study. J. Dent. 2014;42:263–270. doi: 10.1016/j.jdent.2013.12.014. [DOI] [PubMed] [Google Scholar]
- Matarasso S., Salvi G.E., Iorio Siciliano V., Cafiero C., Blasi A., Lang N.P. Dimensional ridge alterations following immediate implant placement in molar extraction sites: a six-month prospective cohort study with surgical re-entry. Clin. Oral Implants Res. 2009;20:1092–1098. doi: 10.1111/j.1600-0501.2009.01803.x. [DOI] [PubMed] [Google Scholar]
- McAllister B.S., Haghighat K. Bone augmentation techniques. J. Periodontol. 2007;78:377–396. doi: 10.1902/jop.2007.060048. [DOI] [PubMed] [Google Scholar]
- Zamad Mohit, Zamad Aakanksha, Daga Akshay, Akhare Pankaj. Immediate Placement of Mandibular Molar Dental Implants: Case Reports., Feb 2015, Volume 7, No. 2. J. Implant Adv. Clin. Dent. 2015;7:11–19. [Google Scholar]
- Mordenfeld M.H., Johansson A., Hedin M., Billström C., Fyrberg K.A. A retrospective clinical study of wide-diameter implants used in posterior edentulous areas. Int. J. Oral Maxillofac. Implants. 2004;19:387–392. [PubMed] [Google Scholar]
- Ormianer Z., Palti A., Demiralp B., Heller G., Lewinstein I., Khayat P.G. Implant-supported first molar restorations: correlation of finite element analysis with clinical outcomes. Int. J. Oral Maxillofac. Implants. 2012;27:e1–e12. [PubMed] [Google Scholar]
- Padhye, N., Shirsekar, V., 2019. Tomographic evaluation of mandibular molar alveolar bone for immediate implant placement – A retrospective cross-sectional study. Clin. Oral Implants Res. 30, 265–265. https://doi.org/10.1111/clr.221_13509.
- Rominger J.W., Triplett R.G. The use of guided tissue regeneration to improve implant osseointegration. J. Oral Maxillofac. Surg. 1994;52:106–112. doi: 10.1016/0278-2391(94)90388-3. [DOI] [PubMed] [Google Scholar]
- Schliephake H., Dard M., Planck H., Hierlemann H., Jakob A. Guided bone regeneration around endosseous implants using a resorbable membrane vs a PTFE membrane. Clin. Oral Implants Res. 2000;11:230–241. doi: 10.1034/j.1600-0501.2000.011003230.x. [DOI] [PubMed] [Google Scholar]
- Schwartz-Arad D., Chaushu G. The ways and wherefores of immediate placement of implants into fresh extraction sites: a literature review. J. Periodontol. 1997;68:915–923. doi: 10.1902/jop.1997.68.10.915. [DOI] [PubMed] [Google Scholar]
- Schwartz-Arad D., Grossman Y., Chaushu G. The clinical effectiveness of implants placed immediately into fresh extraction sites of molar teeth. J. Periodontol. 2000;71:839–844. doi: 10.1902/jop.2000.71.5.839. [DOI] [PubMed] [Google Scholar]
- Shaikh S.Y., Shaikh S.S. Direct linear measurement of root dentin thickness and dentin volume changes with post space preparation: A cone-beam computed tomography study. Contemp Clin. Dent. 2018;9:77–82. doi: 10.4103/ccd.ccd_785_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shakil M, Fida M, Jose M., 2014. Golden ratio and length of the teeth: Establishing the Shakil’s concept. 2014; 02, 04, 95–97. UJMDS 2, 95–97.
- Simion M., Trisi P., Piattelli A. Vertical ridge augmentation using a membrane technique associated with osseointegrated implants. Int. J. Periodontics Restorative Dent. 1994;14:496–511. [PubMed] [Google Scholar]
- Smith R.B., Tarnow D.P. Classification of molar extraction sites for immediate dental implant placement: technical note. Int. J. Oral Maxillofac. Implants. 2013;28:911–916. doi: 10.11607/jomi.2627. [DOI] [PubMed] [Google Scholar]
- Smith R.B., Tarnow D.P., Sarnachiaro G. Immediate Placement of Dental Implants in Molar Extraction Sockets: An 11-Year Retrospective Analysis. Compend. Contin. Educ. Dent. Jamesburg NJ. 2019;1995(40):166–170. [PubMed] [Google Scholar]
- Soman D.C., Almuhrij A., Alghusen N., Alsubaie F.A., Aljamal M., Alrasheed R. CBCT Analysis of Alveolar Bone Dimensions in Mandibular Posterior Teeth: A Preliminary Study. Indian J. Appl. Res. 2019;9(10):7–9. [Google Scholar]
- Suarez F., Chan H.-L., Monje A., Galindo-Moreno P., Wang H.-L. Effect of the timing of restoration on implant marginal bone loss: a systematic review. J. Periodontol. 2013;84:159–169. doi: 10.1902/jop.2012.120099. [DOI] [PubMed] [Google Scholar]
- Tomasi C., Sanz M., Cecchinato D., Pjetursson B., Ferrus J., Lang N.P., Lindhe J. Bone dimensional variations at implants placed in fresh extraction sockets: a multilevel multivariate analysis. Clin. Oral Implants Res. 2010;21:30–36. doi: 10.1111/j.1600-0501.2009.01848.x. [DOI] [PubMed] [Google Scholar]
- Ueno T., Yamada M., Hori N., Suzuki T., Ogawa T. Effect of ultraviolet photoactivation of titanium on osseointegration in a rat model. Int. J. Oral Maxillofac. Implants. 2010;25:287–294. [PubMed] [Google Scholar]
- Wang T.-Y., Kuo P.-J., Fu E., Kuo H.-Y., Nie-Shiuh Chang N., Fu M.-W., Shen E.-C., Chiu H.-C. Risks of angled implant placement on posterior mandible buccal/lingual plated perforation: A virtual immediate implant placement study using CBCT. J. Dent. Sci. 2019;14:234–240. doi: 10.1016/j.jds.2019.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werbitt M.J., Goldberg P.V. The Immediate Implant Bone Preservation and Bone Regeneration. Int. J. Periodontics Restorative Dent. 1992;12:207–217. [PubMed] [Google Scholar]