Abstract
Introduction:
Neuropathic pain is common, but the frequency of misdiagnosis and irrational treatment is high. The aim of this study is to evaluate the rate of neuropathic pain in neurology outpatient clinics by using valid and reliable scales and review the treatments of patients.
Methods:
The study was conducted for 3 months in eleven tertiary health care facilities. All outpatients were asked about neuropathic pain symptoms. Patients with previous neuropathic pain diagnosis or who have neuropathic pain symptoms were included and asked to fill painDETECT and douleur neuropathic en 4 questions (DN4) questionnaire. Patients whose DN4 score is higher than 3 and/or painDETECT score higher than 13 and/or who are on drugs for neuropathic pain were considered patients with neuropathic pain. The frequency of neuropathic pain was calculated and the treatments of patients with neuropathic pain were recorded.
Results:
Neuropathic pain frequency was 2.7% (95% CI: 1.5–4.9). The most common cause was diabetic neuropathy. According to painDETECT, the mean overall pain intensity was 5.7±2.4, being lower among patients receiving treatment. Pharmacological neuropathic pain treatment was used by 72.8% of patients and the most common drug was pregabalin. However, 70% of those receiving gabapentinoids were using ineffective doses. Besides, 4.6% of the patients were on medications which are not listed in neuropathic pain treatment guidelines.
Conclusion:
In our cohort, the neuropathic pain severity was moderate and the frequency was lower than the literature. Although there are many guidelines, high proportion of patients were being treated by ineffective dosages or irrational treatments.
Keywords: Neuropathic pain, gabapentinoid, pregabalin, gabapentin, DN4, painDETECT
INTRODUCTION
Neuropathic pain is caused by a lesion or disease of the somatosensory system, including peripheral fibres (Aβ, Aδ and C fibres) and central neurons (1). Neuropathic pain is a major, generally persistent, epidemiological problem that may require lifelong treatment.
Diabetic polyneuropathy, postherpetic neuralgia, poststroke pain are common causes of neuropathic pain. Moreover, neuropathic pain may be a symptom of some neurological diseases such as Parkinson’s disease (2, 3). To date, several epidemiological studies have been established to estimate the prevalence of neuropathic pain. Cross-sectional studies done by postal or telephone interview survey, general practice research database conducted in general population or representative of general population showed that neuropathic pain prevalence varies between 0.8 and 17.9% (4–6). Considering these data, the prevalence of neuropathic pain has been estimated to be 7–10% in general population (3, 7). But, there is no epidemiological study about neuropathic pain in Turkish population, except one multicenter cross-sectional study which showed that the prevalence of neuropathic pain in Turkish patients with diabetic neuropathy is 14% (8). Thus, epidemiological studies are needed to determine diagnostic and therapeutic requirements. The aim of this study is to evaluate the rate of neuropathic pain in neurology outpatient clinics by using valid and reliable pain scales and to review the treatments of patients with neuropathic pain.
METHODS
The study was conducted between 1st September 2018 and 31st December 2018 in eleven tertiary health care facilities in eight cities from different regions of Turkey. All outpatients were included in 5 centers whereas only outpatients with neuromuscular diseases were included in 5 and only multiple sclerosis (MS) outpatients were included in one center. All participants provided written informed consent to participate in this study and ethical approval was granted by the Hacettepe University Faculty of Medicine Ethical Review Board (GO 18/756). All patients were asked about neuropathic pain symptoms and their previous diagnosis were reviewed. Patients with previous neuropathic pain diagnosis or who have neuropathic pain symptoms were included to the study. Then, these patients were questioned by painDETECT (9) and douleur neuropathic en 4 questions (DN4) (10). Patients whose DN4 score is equal or higher than 4 and/or painDETECT score higher than 13 and/or patients previously diagnosed with neuropathic pain and who are on neuropathic pain treatment were considered patients with neuropathic pain. The neurological examination and the co-morbidities of these patients were recorded.
Statistical analyses were performed by using IBM SPSS (Statistical Package for Social Sciences) 22.0. There was great variability between the centers in terms of both total outpatient numbers and the number of patients with neuropathic pain. Thus, the rate of neuropathic pain in neurology patients was calculated by meta-analysis approach instead of standardized statistical methods. As the heterogeneity was high (I2=98.7%) between the centers, we used random effect model. We also calculated the rate of neuropathic pain by removing the centers with the highest and lowest frequency of neuropathic pain.
RESULTS
In eleven tertiary health care facilities 22847 neurology outpatients were examined during three months. 1007 patients with previous neuropathic pain diagnosis or who suffered from neuropathic pain symptoms were included to the study and asked to fill DN4 and painDETECT questionnaires (Figure 1) . Among them, 668 patients with at least one screening questionnaire supporting neuropathic pain and/or who were on neuropathic pain treatment were diagnosed as having neuropathic pain. (Table 1). The frequency of neuropathic pain was 2.7% (95% CI: 1.5–4.9) in our cohort. The demographical features and clinical findings were fulfilled in 657 patients whose findings were detailed below.
Figure 1.
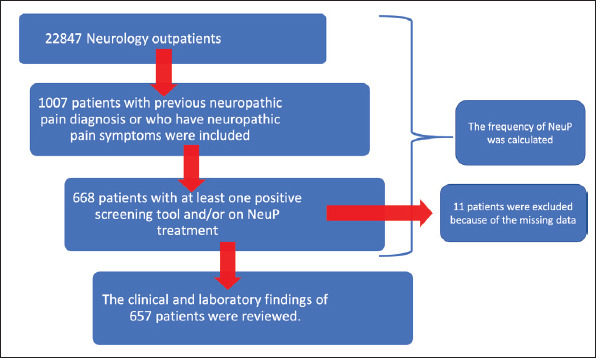
Flowchart of the study.
Table 1.
The number of total neurology outpatients and the number of patients with neuropathic pain in each center
| Centers | Outpatient Clinic Description | Total number of outpatients | Number of patients with NeuP | NeuP frequency |
|---|---|---|---|---|
| Marmara University | Neuromuscular | 429 | 81 | 18.9% |
| Dokuz Eylül University | General Neurology | 3,406 | 82 | 2.4% |
| Pamukkale University | General Neurology | 1,931 | 170 | 8.8% |
| Çukurova University | General Neurology | 2,314 | 111 | 4.8% |
| İnönü University | Neuromuscular | 620 | 29 | 4.7% |
| İstanbul University Cerrahpaşa Medical Faculty | Neuromuscular | 1,150 | 44 | 3.8% |
| Ankara Training Hospital | Neuromuscular | 2,502 | 42 | 1.7% |
| Hacettepe University | General Neurology | 3,682 | 46 | 1.2% |
| Uludağ University | General Neurology | 3,203 | 37 | 1.2% |
| Karadeniz Technical University | Multiple sclerosis | 1,757 | 18 | 1.0% |
| Ege University | Neuromuscular | 1,853 | 8 | 0.4% |
| Total | 22,847 | 668 | 2.7% |
NeuP, neuropathic pain.
The mean age of patients with neuropathic pain was 55.5±14.4 (18–98 years-old) and 57% of these patients were female. The median duration of neuropathic pain was 24 months (mean 44.4±58.9 months; 10 days-480 months) and the diagnosis of neuropathic pain was made during the study in 19% of the patients for the first time. Abnormal neurological examination findings, such as decreased deep tendon reflexes and sensory loss, were observed in 60% of the patients. The most common cause of neuropathic pain was diabetic neuropathy seen in 39.2% (Figure 2), besides, 46% of patients with neuropathic pain had diabetes mellitus. Noteworthy, central neuropathic pain was relatively rare as present in 8% of the patients.
Figure 2.
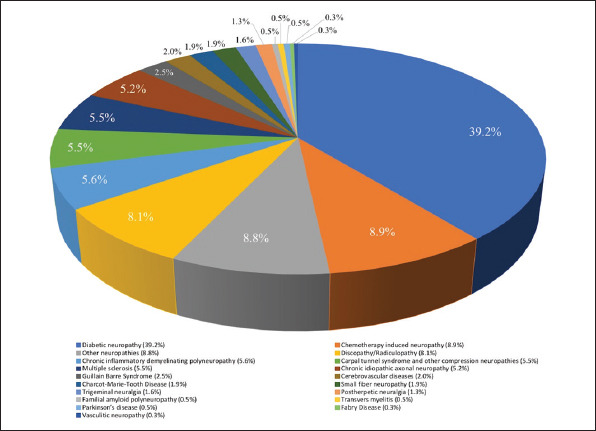
The causes of neuropathic pain.
According to painDETECT, the mean overall pain intensity (during the last 4 weeks) was 5.7±2.4, whereas the mean pain intensity at the examination was 4.7±3.0. Additionally, 35% of the patients claimed that the most severe pain intensity was 10/10 during the last 4 weeks. Most of the patients (31.6%) described their pain as persistent with pain attacks and the pain radiates in 30.2%. The most common positive neuropathic pain symptom was tingling and prickling (87.9%) followed by burning (74.4%), electric shocks (62%), allodynia (46.6%), itching (35.2%) respectively. Furthermore, most of the patients (90.1%) also suffer from numbness in the painful area.
The mean DN4 questionnaire score was 6.1±2.1. While numbness was reported by most of the patients via painDETECT, hypoesthesia to contact was observed in 68.7% and to pricking in 52.8% according to DN4. Although 46.6% of the patients described allodynia in painDETECT, pain provoked by brushing was detected in 28.1% of the patients.
478 patients (72.8%) were receiving pharmacological treatment for neuropathic pain (Table 2). The most common treatment was pregabalin monotherapy (59.2%), followed by gabapentin (15.1%). However, 70% of those receiving gabapentin and 46.7% of those receiving pregabalin were using ineffective doses. Moreover, 30 patients (4.6%) were on medications, such as a-lipoic acid, which are not in the neuropathic pain treatment guidelines.
Table 2.
The neuropathic pain treatments
| Drug | Number of patients (n) | Percentage (%) |
|---|---|---|
| Monotherapy | 402 | 84.1 |
| Pregabalin | 283 | 59.2 |
| Gabapentin | 72 | 15.1 |
| Duloxetine | 35 | 7.3 |
| Carbamazepine | 4 | 0.8 |
| Amitriptyline | 2 | 0.4 |
| Fluoxetine | 2 | 0.4 |
| Escitalopram | 2 | 0.4 |
| Sertraline | 1 | 0.25 |
| Lamotrigine | 1 | 0.25 |
| Combination therapy | 76 | 15.9 |
| Pregabalin + Duloxetine | 48 | 10.0 |
| Gabapentin + Duloxetine | 5 | 1.0 |
| Pregabalin + Carbamazepine | 5 | 1.0 |
| Pregabalin + Amitriptyline | 4 | 0.8 |
| Pregabalin + Gabapentin | 4 | 0.8 |
| Carbamazepine + Amitriptyline | 2 | 0.4 |
| Pregabalin + Gabapentin + Duloxetine | 2 | 0.4 |
| Pregabalin + Amitriptyline + Duloxetine | 1 | 0.25 |
| Pregabalin + Amitriptyline + Carbamazepine | 1 | 0.25 |
| Pregabalin + Fluoxetine | 1 | 0.25 |
| Duloxetine + Fluoxetine | 1 | 0.25 |
| Gabapentin + Sertraline | 1 | 0.25 |
| Gabapentin + Amitriptyline | 1 | 0.25 |
| Total | 478 | 100.0 |
Combination treatment was used in 15.9% of patients and the most common treatment combination was duloxetine with pregabalin. It is noteworthy that 6 patients (1.2%) were treated with pregabalin and gabapentin combination. Although painDETECT and DN4 scores did not differ between patients with and without treatment (p=0.978, p=0.368 respectively), the mean overall pain intensity (during the last 4 weeks) was lower in patients with treatment (p=0.027) according to painDETECT. Additionally, the frequency of highest pain intensity (10/10) was lower in patients with treatment (p=0.012).
DISCUSSION
Neuropathic pain is a well-known persistent pain syndrome with therapeutic challenge. The epidemiology of neuropathic pain has always been a hot topic for researchers. Moreover, adequate diagnostic tools and population data are important to determine therapeutic strategy and health care costs. The overall prevalence of neuropathic pain is estimated to be 7–10% (3, 7). This information comes from medical records, retrospective studies, cross-sectional studies done by postal or telephone-based survey (4–7, 11). As the diagnosis relies on patient-defined subjective assessments, it can be sometimes over or underdiagnosed. Although there are many scales and questionnaires, there is no ‘gold standard’ for determining whether or not an individual has neuropathic pain. DN4 (10), LANSS (12) and painDETECT (9) are the most commonly used screening tools in epidemiological studies. In this study we used two screening tools, DN4 and painDETECT, to increase reliability.
Previous prevalence studies of neuropathic pain in neurology patients consist of survey done among patients with distinct neurological conditions such as ischemic stroke (13) or multiple sclerosis (14). Moreover, our knowledge about the epidemiology of neuropathic pain in Turkey is limited to cross-sectional studies done in small number of patients (less than 1500 patients) with distinct diseases such as diabetes or low back pain (8, 15, 16). As might be expected, the frequency is high in patient with low back pain (43.9%) (15), rheumatic disorders (30%) (16) and diabetes (14%) (8). Interestingly, although we included neurology outpatients, the prevalence of neuropathic pain in our cohort was 2.7% that is lower than estimated neuropathic pain prevalence. This finding may be related to objective diagnostic criteria and the use of two diagnostic questionnaires. Moreover, the neuropathic pain intensity was generally moderate with a mean of 5.7±2.4 according to painDETECT and most of the patients suffer from persistent pain with pain attacks. The most common type of neuropathic pain was tingling and prickling seen in 87.9% followed by burning (74.4%). It is known that negative symptoms can accompany neuropathic pain. Noteworthy, the frequency of hypoesthesia was very high as 90.1% according to painDETECT, and more common than any other positive symptom. Besides hypoesthesia was detected by neurological examination in 70% of neuropathic patients.
In our cohort, not surprisingly, the most common cause of neuropathic pain was diabetic neuropathy and neuropathic pain prevalence was higher among patients with neuromuscular diseases than any other neurological conditions. Noteworthy, central neuropathic pain was relatively rare despite the cohort consisted of patients with all kinds of neurological disorders.
Another remarkable finding was that abnormal neurological findings were present only in 60% of patients with neuropathic pain. This underlines the necessity to use screening and diagnostic tools such as neuropathic pain questionnaires and quantitative sensory tests.
Most of the neuropathic pain treatments have moderate efficacy providing 50% of pain relief (17). In our cohort, the overall pain intensity was lower in patients with treatment but questionnaire scores did not differ between patients receiving and not receiving medical treatment. However, it is noteworthy that most of the patients, more than 70%, were not receiving effective dose of gabapentinoids. This finding could be related to the fear of abuse or side effects and the new limitation in prescription of these drugs in our country. Previous study of our group showed that the cost of irrational treatment on neuropathic pain accounted for 48% of all neuropathic pain treatment in 2007–2009 (18). Optimistically, the frequency of irrational treatment in our cohort was very low as 4.83%.
This study can represent the overall Turkish patients’ characteristics as it was conducted in 11 tertiary health care centers from different regions of Turkey. Besides, the outpatient services varied between the centers as some of them included patients all kinds of neurological diseases whereas some included patients with certain neurological conditions such as MS, neuromuscular diseases. However, the clinical and laboratory findings of the patients are lacking due to high outpatient density in these centers and our findings are limited to neurology patients and to tertiary health care centers. Thus, longitudinal studies with a sample which is representing general population and identifying risk and causal factors are still needed.
Acknowledgement:
The authors thank the doctors who took part in the follow-up of these patients.
Footnotes
Ethics Committee Approval: Ethical approval was granted by the Hacettepe University Faculty of Medicine Ethical Review Board (GO 18/756).
Informed Consent: All participants provided written informed consent to participate in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept- CEBK, ET; Design- CEBK, ET, SEÖ; Supervision- CEBK, ET; Resource- CEBK, ET; Materials- CEBK, Bİ,OB, İŞ, NK, NG, BGÇ, SKG, TKY, DGÖ, FK, ZÜ, ÇE, BU, CB, MT, MAA, ÖK, AÖ, PKK, KU, SEÖ, ET; Data Collection and/or Processing- CEBK, Bİ,OB, İŞ, NK, NG, BGÇ, SKG, TKY, DGÖ, FK, ZÜ, ÇE, BU, CB, MT, MAA, ÖK, AÖ, PKK, KU, SEÖ, ET; Analysis and/or Interpretation- CEBK, Bİ, ET, SEÖ; Literature Search- CEBK, Bİ; Writing- CEBK, Bİ, ET, SEÖ; Critical Reviews- CEBK, Bİ, ET, SEÖ.
Conflict of Interest: None.
Financial Disclosure: Study funded by Abdi Ibrahim Ilac Sanayi ve Tic. A.S. The funder had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
REFERENCES
- 1.Treede RD, Jensen TS, Campbell JN, Cruccu G, Dostrovsky JO, Griffin JW, Hansson P, Hughes R, Nurmikko T, Serra J. Neuropathic pain:redefinition and a grading system for clinical and research purposes. Neurology. 2008;70:1630–1635. doi: 10.1212/01.wnl.0000282763.29778.59. [DOI] [PubMed] [Google Scholar]
- 2.Moreno CB, Hernandez-Beltran N, Munevar D, Gutierrez-Alvarez AM. Central neuropathic pain in Parkinson's disease. Neurologia. 2012;27:500–503. doi: 10.1016/j.nrl.2011.08.001. [DOI] [PubMed] [Google Scholar]
- 3.Colloca L, Ludman T, Bouhassira D, Baron R, Dickenson AH, Yarnitsky D, Freeman R, Truini A, Attal N, Finnerup NB, Eccleston C, Kalso E, Bennett DL, Dworkin RH, Raja SN. Neuropathic pain. Nat Rev Dis Primers. 2017;3:17002. doi: 10.1038/nrdp.2017.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bouhassira D, Lanteri-Minet M, Attal N, Laurent B, Touboul C. Prevalence of chronic pain with neuropathic characteristics in the general population. Pain. 2008;136:380–387. doi: 10.1016/j.pain.2007.08.013. [DOI] [PubMed] [Google Scholar]
- 5.Dieleman JP, Kerklaan J, Huygen FJ, Bouma PA, Sturkenboom MC. Incidence rates and treatment of neuropathic pain conditions in the general population. Pain. 2008;137:681–688. doi: 10.1016/j.pain.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 6.Toth C, Lander J, Wiebe S. The prevalence and impact of chronic pain with neuropathic pain symptoms in the general population. Pain Med. 2009;10:918–929. doi: 10.1111/j.1526-4637.2009.00655.x. [DOI] [PubMed] [Google Scholar]
- 7.Smith BH, Torrance N. Epidemiology of neuropathic pain and its impact on quality of life. Curr Pain Headache Rep. 2012;16:191–198. doi: 10.1007/s11916-012-0256-0. [DOI] [PubMed] [Google Scholar]
- 8.Erbas T, Ertas M, Yucel A, Keskinaslan A, Senocak M TURNEP Study Group. Prevalence of peripheral neuropathy and painful peripheral neuropathy in Turkish diabetic patients. J Clin Neurophysiol. 2011;28:51–55. doi: 10.1097/WNP.0b013e3182051334. [DOI] [PubMed] [Google Scholar]
- 9.Alkan H, Ardic F, Erdogan C, Sahin F, Sarsan A, Findikoglu G. Turkish version of the painDETECT questionnaire in the assessment of neuropathic pain:a validity and reliability study. Pain Med. 2013;14:1933–1943. doi: 10.1111/pme.12222. [DOI] [PubMed] [Google Scholar]
- 10.Unal-Cevik I, Sarioglu-Ay S, Evcik D. A comparison of the DN4 and LANSS questionnaires in the assessment of neuropathic pain:validity and reliability of the Turkish version of DN4. J Pain. 2010;11:1129–1135. doi: 10.1016/j.jpain.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 11.Van Den Kerkhof EG, Mann EG, Torrance N, Smith BH, Johnson A, Gilron I. An Epidemiological Study of Neuropathic Pain Symptoms in Canadian Adults. Pain Res Manag. 2016;2016:9815750. doi: 10.1155/2016/9815750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koc R, Erdemoglu AK. Validity and reliability of the Turkish Self-administered Leeds Assessment of Neuropathic Symptoms and Signs (S-LANSS) questionnaire. Pain Med. 2010;11:1107–1114. doi: 10.1111/j.1526-4637.2010.00837.x. [DOI] [PubMed] [Google Scholar]
- 13.Aprile I, Briani C, Pazzaglia C, Cecchi F, Negrini S, Padua L Don Carlo Gnocchi Pain-Rehab Group. Pain in stroke patients:characteristics and impact on the rehabilitation treatment. A multicenter cross-sectional study. Eur J Phys Rehabil Med. 2015;51:725–736. [PubMed] [Google Scholar]
- 14.Truini A, Barbanti P, Pozzilli C, Cruccu G. A mechanism-based classification of pain in multiple sclerosis. J Neurol. 2013;260:351–367. doi: 10.1007/s00415-012-6579-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Erhan B, Gumussu K, Kara B, Bulut GT, Yalcinkaya EY. The frequency of neuropathic pain in Turkish patients with low back pain:a cross-sectional study. Acta Neurol Belg. 2020 doi: 10.1007/s13760-020-01285-7. [DOI] [PubMed] [Google Scholar]
- 16.Garip Y, Eser F, Kilicarslan A, Bodur H. Prevalence of Neuropathic Pain in Rheumatic Disorders:Association With Disease Activity, Functional Status and Quality of Life. Arch Rheumatol. 2015;30:231–237. [Google Scholar]
- 17.Finnerup NB, Attal N, Haroutounian S, McNicol E, Baron R, Dworkin RH, Gilron I, Haanpaa M, Hansson P, Jensen TS, Kamerman PR, Lund K, Moore A, Raja SN, Rice AS, Rowbotham M, Sena E, Siddall P, Smith BH, Wallace M. Pharmacotherapy for neuropathic pain in adults:a systematic review and meta-analysis. Lancet Neurol. 2015;14:162–173. doi: 10.1016/S1474-4422(14)70251-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tan E, Akıncı A, Ayvaz G, Erbaş T, Erbaş M, Güç O, Hepgüler S, Kiraz S, Oşar S, Öztürk Ş, Özyalçın N, Palaoğlu S, Uyar M, Ünal S, Yalçın Ş. Irrational drug use in neuropathic pain treatment:a two-year data analysis. Int J Med Biomed Res. 2013;2:202–206. [Google Scholar]


