Highlights
-
•
Online Adaptive Radiation Therapy (oART) provides a solution to account for daily patient variations, but wide spread implementation is hindered by human resources and training.
-
•
Physicians can mentor Radiation Therapists (RTTs) through traditional tasks such as contouring and plan approval.
-
•
With evidence-based credentialing activities, decision support aids and ‘on-call’ caveats, RTTs can lead the oART workflow and a ‘Clinician-Lite’ approach.
-
•
Compliance with legislative, regulatory and medico-legal governing bodies can be addressed through post-graduate study, advanced practice pathways, exemptions and delegation of task.
Keywords: Online adaptive radiotherapy, Credentialing, RTT-led, Workflow, Advanced practice, Professional roles, Training
Abstract
Online adaptive radiotherapy (oART) is an emerging advanced treatment option for cancer patients worldwide. Current oART practices using magnetic resonance (MR) and cone beam computed tomography (CBCT) based imaging are resource intensive and require physician presence, which is a barrier to widespread implementation. Global evidence demonstrates Radiation Therapists (RTTs) can lead the oART workflow with decision support tools and on ‘on-call’ caveats in a ‘clinician-lite’ approach without significantly compromising on treatment accuracy, speed or patient outcomes. With careful consideration of jurisdictional regulations and guidance from the multi-disciplinary team, RTTs can elevate beyond traditional scopes of practice. By implementing robust and evidence-based credentialing activities, they enable service sustainability and expand the real-world gains of adaptive radiotherapy to a greater number of cancer patients worldwide. This work summarises the evidence for RTT-led oART treatments and proposes a pathway for training and credentialing.
Introduction
Online adaptive radiotherapy (oART) is a novel and emerging treatment option for cancer patients. oART assesses patient anatomy daily, with a treatment plan ‘adapted’ from an original ‘reference’ plan with the patient on the treatment couch. Delivery of oART provides personalised radiotherapy (RT), adapting to the patient for high conformity and accuracy, guided by either Cone Beam Computed Tomography (CBCT) or Magnetic Resonance Imaging (MRI). oART provides a solution to account for inter-fraction variation of tumours and organs at risk (OAR) including weight-loss, tumour regression and organ shape changes [1], [2]. Evidence of patient benefit is provided for bladder [3], [4], rectum [5], prostate [6], [7], head and neck [8] and abdominal tumours [9], [10], [11], [12]. Margin reduction and favourable dosimetric and clinical outcomes have been demonstrated [12], [13], [14], [15], [16].
Early adopters have generally implemented oART with conventional treatment planning and approval processes repeating on each day of treatment. Generally, oART requires specialist staff such as a Radiation Oncologist (RO), dosimetrist and Radiation Oncology Medical Physicist (ROMP) to be present in addition to the RTT treatment team. Human resources and training are clearly barriers to widespread implementation of oART [2], [17], [18], [19], [20], [21]. It is widely acknowledged that global variances exist for role responsibilities during oART. In conventional roles, two RTTs are responsible for image matching and treatment delivery, the prescribing RO finalises contouring and plan approval, with the ROMP completing plan quality assurance (QA). Evidence of RTTs successfully leading the oART workflow with training has been demonstrated [21], with identification of additional skills and knowledge, in particular MRI guided adaptive radiotherapy (MRIgART) [6], [21]. Some traditional RO tasks might be delegated to advanced practice RTT’s who are ‘Advanced Online Adapters’ and under controlled guidance of the physician with ‘on-call’ caveats can lead oART treatments [6], [18], [21], [22]. Alternatively, ROs may still need to attend the treatment console satisfying local codes of practice [22].
The scientific literature suggests conventional roles are unsuitable for oART [21], [24].
A shift towards ensuring RTTs are trained to lead the oART workflow, consistent with conventional treatment delivery resourcing, relies upon clear communication and documentation of planning goals with decision support tools, multidisciplinary team (MDT) on-call [23], real-time, post-fraction and dose accumulation evaluation. Given the base skillset of RTTs differs internationally, variation in the credentialing tasks and level of support required to enact these programs is to be expected. The tools for oART are also maturing; with faster computation [25], better software interfaces, automation and artificial intelligence (AI). The RTT skillset at treatment for conventional and oART is changing. This is similar to the changes in role expectations and responsibilities alongside technological advancements including the introduction of CBCT into the clinic with online image matching moved from two, to three dimensional accuracy [26]. This manuscript seeks to provide evidence-based recommendations to inform education, training and credentialing activities for RTTs to safely lead oART. Under the guidance of ROs (or Technical Physicians) and supported by the MDT, RTTs can elevate to Advanced Online Adapters, facilitating more adaptive treatments for patients using safe, efficient and sustainable workflows.
Current online adaptive workflow responsibilities
The workflows for CBCT guided oART and MRIgART are well established [3], [5], [8], [9], [27], [28], [29]. Despite global differences in the oART team make up, Table 1 outlines a synthesis of evidenced-based practice covering general workflow tasks and responsibilities for CBCT oART and MRIgART [6], [21]. Outlining clear task responsibilities is asserted in the literature [21] and highlights the potential credentialing opportunities for an RTT-led workflow. The oART workflow begins before on-couch adaption, where a reference plan is created following a physician order to meet clinical goals; these clinical goals are carried through oART. At treatment delivery, a pre-treatment image is acquired and usability for contouring and dose calculation verified, usually by the RTTs. The OARs and targets are then propagated, either automatically by AI or manually by human edits. The role-responsibility of the human propagated and edited contours varies between departments and globally. Often, a RTT or dosimetrist with considerable treatment planning and soft tissue knowledge and experience derives and edits the contours with final review by RO [21]. Standardly, for non-oART, current practice is RTTs or dosimetrists creating and evaluating OAR contour accuracy across all body sites, with ultimate responsibility for targets and OARs residing with the RO [30]. Final plan QA in the daily oART workflow is performed by a ROMP, to validate the new treatment plan independently prior to confirming patient position via intra-fraction motion assessment. The intra-fraction assessment is commonly completed by RTTs, prior to and during delivery of the online-adapted plan.
Table 1.
Current General Online Adaptive Workflow, Responsibilities & RTT Credentialing tasks for CBCT and MR Guided.
|
On couch adaptation Workflow |
Multi-Disciplary oART Treatment Team |
Credentialing tasks for RTT led oART | ||
|---|---|---|---|---|
|
Physicist ROMP |
Radiation Therapist RTT Dosimetrist |
Radiation Oncologist Physician Technical Physician |
||
| Set up patient | X | |||
| Acquire Imaging (MR, CBCT) | X | |||
| Review and accept imaging, registrations | X | X | ||
| Review, edit and accept contours | X | X | X | |
| Review, edit and accept target volume | X | X | X | |
| Review, edit and accept OARs | X | X | X | |
| Review clinical aspects of original and daily Adaptive treatment plans | X | X | X | |
| Re-optimisation (MR-Linac) | X | X | ||
| Select treatment plan | X | X | X | |
| Sign off clinical plan report | X | X | ||
| Review technical aspects of plan | X | X | ||
| Review independent QA results | X | |||
| Sign off technical plan report | X | X | X | |
| Acquire additional pre-treatment image, review and apply shift | X | |||
| Deliver treatment | X | |||
| Acquire on treatment images, Review and Apply shift | X | |||
Experiences of early adopters of online adaptive RT
Historically, oART has been implemented as a Plan of the Day (POD), with multiple contours and treatment plans (e.g. empty, mid and full bladder) available for selection at treatment. A POD approach relied upon RO approval of multiple treatment plans prior to on-couch delivery with decision to treat based on target volume fit to patient anatomy of the day. Online contouring or dose assessment is not available in POD adaptive. The RTTs made the IGRT-based decision of which plan to treat each day. Much of the experience with POD arises from thorough multi-center clinical trials, specific to anatomical sites such as bladder (RAIDER [2] and HYBRID [31]) in the United Kingdom (UK), and the BOLART trial in Australia and New Zealand [32]). These studies demonstrated the success of simple RTT-led adaptive treatments supported by comprehensive training and credentialing programs, whereby RTTs were able to complete unassisted almost all tasks in Table 1, except online contouring and dose assessment. The POD credentialing programs were developed through inter-professional collaboration in teaching and assessing decision-making for POD guidance across several hundred trainees [4], [31], [33]. Further, oART is showing increasing justification in hypo-fractionated treatments [25].
Initial publications detail feasibility and safety of MRIgART and CBCT oART and provide insights into local task expectations and training methodologies. Hales et al [6] outline steps taken for UK Radiation Oncology clinics to adjust to a ‘clinician-lite’ workflow. Clinician-lite in oART is when the RO is on-call for the RTTs if issues arise, they are not needed at the console to deliver treatment. The ‘clinician-lite’ workflow is commonly reached following a two-phased approach. Firstly, a needs assessment by the multi-disciplinary-team (MDT) to identify the skills required during real-time adaptation, which informs the creation of the in-house oART staff-training program. Secondly, the RO defines the clinical goals and thresholds for a patient or body-site indicating when they are to be called to the treatment console. In the Hales et al study [6], the treatment team (one RO, two RTTs and ROMPs) developed action thresholds after 40 prostate oART fractions which informed threshold breach interventions for future prostate patients. A ‘clinician-lite’ approach hinges on delegation of task to the RTT and will involve many details whereby the RTT may assume responsibility for contouring, plan evaluation and decision to proceed with oART [34]. The RTT is responsible for ensuring the clinical goals derived by the RO are being delivered during oART. Intven et al [5] describe their experience with RTTs assuming responsibility for contouring in rectal cancer MRIgART, where twelve patients were ‘RO-adapted’, then trained RTTs adapted all contours and contacted the on-call RO if needed. Currently, final plan approval is by ROMP and RO, with future directions for RTTs to execute daily plan approval [5], [27]. Additionally, McNair et al [21] detail the positive effect of weekly MDT meetings or meeting prior to a complex patient’s treatment, to maintain team communications and refine safe work practices in oART.
RTT led online adaptive radiotherapy
As more patients are being treated using oART systems, an RTT-led staffing model seeks to overcome the barrier of physician availability to treat adaptively. In the Netherlands, Daal et al [28] and Willigenburg et al [7] describe implementation practices for RTT-led workflow in prostate oART. A comprehensive RTT training program was developed, incorporating anatomy contouring and planning training using real-time on-couch and emulated environments. A physician and senior RTT planner guided five RTTs with experience in treatment planning optimization and review, to advanced-adapter status, whereby trained RTTs were able to independently treat prostate patients after the four fractions [29]. The RO was present for the first week to oversee potential clinical issues. Between July 2020 and February 2021, 1000 fractions and up to 15 prostate patients per-day have been successfully treated by RTT advanced adapters. Only on 5 occasions needing physician consultation. Willigenburg et al [7] also successfully trained RTT’s to perform daily online Clinical Target Volume (CTV) contour adaptation for MRIgART prostate treatments. Results of the training program indicate that 94% of 150 RTT contours were clinically acceptable. Vendor application training is appraised as an introduction to the basics of the system and software [21].
Advanced practice radiation therapy roles
Globally, governing bodies such as The Australian Society of Medical Imaging and Radiation Therapy (ASMIRT) and The Canadian Association of Medical Radiation Technologists (CAMRT) have established policies and frameworks to support RTT advanced practice in delivering models of care that expand beyond the traditional RTT scope of practice. Advanced practice pathways help to ensure a motivated and flexible workforce, retaining employees with high-level skills who provide high-quality care underpinned by postgraduate study [7], [35], [36]. ESTRO have also supported specialised advanced-practice RTTs, benchmarked with level 7 and 8 descriptors and competencies from the framework of European Higher Education Area (EHEA) [35]. The framework describes level 8 practitioners having “knowledge at the most advanced frontier of a field of work or study and at the interface between fields” with examples provided for competencies in advanced OAR delineation and volume determination, underpinned by a Masters or Doctorate education [36]. In the UK, delegation of task by the prescribing RO allows RTTs the legal requirements for completing tasks confined to the prescribing RO [34]. In the Netherlands, a new academic professional role has been created to facilitate oART [37]. The ‘Technical Physician’ is a medically trained professional who is authorized to assume the role of the RO at oART treatments [37], [38]. Other countries, including Australia and NZ, who are bound by rigid codes of practice with tasks linked to billing, may still require clinicians at the treatment console for oART treatments unless exemptions from governing bodies are sought.
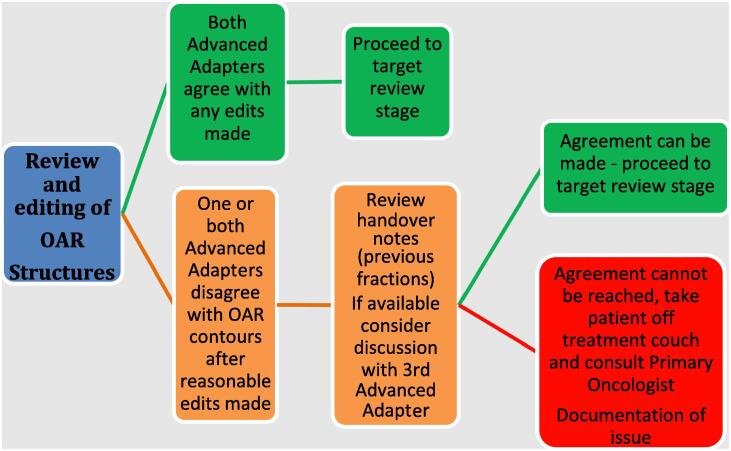
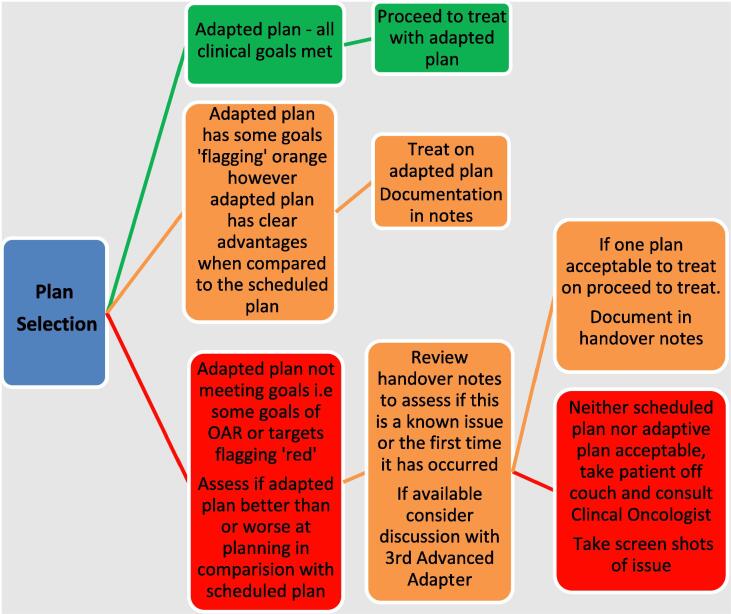
Managing deviations during online adaptive
Support for development of a ‘clinician-lite’ treatment setting in oART is gaining momentum due to the ever-growing workload on the physician and associated shortages of availability to attend treatment. This can be done safely, with a feasible infrastructure to bring the great benefit of oART to patients. The literature recommends establishing decision-aids for notifying the RO should any issues arise during particular RO-oriented tasks [27], [5], [6], [7]. Fig. 1, Fig. 2 detail examples of OAR review and plan selection decision-making guides for oART treatment (pelvis) in a ‘clinician-lite’ setting used at Queens Hospital (BHRUT NHS Trust), Romford, UK. If the treatment team are concerned regarding OAR edits or plan selection, then communication with the primary RO must occur before the next fraction. If goals are consistently exceeded but adaption felt to be optimal for the patient, then a revision of plan goals by the RO is amended to reflect what is achievable. Hales et al [6] details with a protocol-driven ‘clinician-lite’ prostate oART workflow, clinician input was needed in 1.5% of 200 oART occasions. Subsequently, a real-time post-fraction offline review by RO and ROMP may be implemented, with potential requirements being placed on this being performed daily or at some regular interval, in addition to treatment accumulation evaluations.
Fig. 1.
Review of OAR structures for decision-making at the point of care during oART treatment (pelvis).
Fig. 2.
Review of plan selection for decision making at the point of care during oART treatment (pelvis).
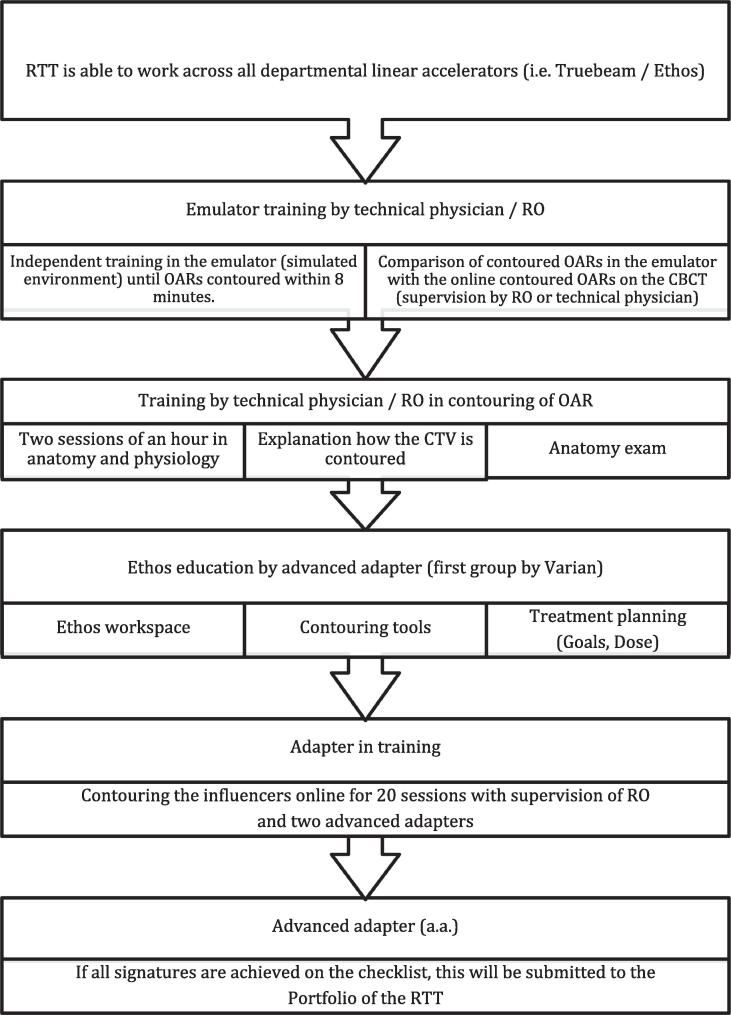
Credentialing of RTTs for advanced practice in oART
The evidence-base for credentialing frameworks that support role extension of RTTs to up-skill and train as advanced adapters is mounting. Requirements include target and OAR contouring, complex planning, planning knowledge and experience, image recognition and registrations, recognizing individual patient requirements and comprehensive general radiotherapy knowledge [21]. Medisch Spectrum Twente (MST) in Enschede, The Netherlands, provide a training outline that has successfully trained RTTs to lead CBCT guided oART treatments since 2020 (Fig. 3).
Fig. 3.
Example RTT credentialing process: Medisch Spectrum Twente (MST): Outline for Advanced Adapters (CBCT guided, prostate alone).
Use of e-learning, online tutorials, face-to-face lectures and workshops have been reported when administering and assessing RTT adaptive education for bladder [4], [27], [39], [31], [33], [32], cervix [40], lung [17] and prostate treatments [6]. There are limited reports on trainee education preferences for oART. Pham et al [33] reports RTTs prefer e-learning over in-person tutorials and Webster et al [4] report high engagement with remote-access education. Contents of oART e-learning modules include disease pathology/aetiology, site-specific anatomy (including CT, MRI), treatment workflows and reading of relevant scientific literature. Willigenburg et al [7] reports on a 4–6 week RTT training program for prostate contour credentialing. The training included workflow, image registration, contouring, treatment planning, dose-wash QA and treatment plan approval tasks. Often, emulation or test environments are made available whereby retrospective patient data sets can be injected for credentialing activities [39], [41]. Leveraging published guidance on credentialing in oART and POD clinical trials such as RAIDER [4] and BOLART [31], [33]. These multi-centre clinical trials demonstrated success in POD guidance and decision-making via coordinated training programs; BOLART, HYBRID and RAIDER training over 185, 70 and 500 RTT’s respectively for CT-guided Bladder POD treatments. The use of phantoms for simulated training exercises to mimic the decision-making process for adaptive radiotherapy was well suited in credentialing ART for bladder [31], [39]. Credentialing, training and support is a MDT effort for successfully activating, implementing and delivering adaptive treatments [33], [40].
Undertaking pre and post education training questionnaires to assess trainee capability and ‘knowledge-based’ experience level helps facilitate efficiencies and record improvements in decision-making and confidence in oART [4], [39]. Additionally, formalised feedback points are necessary during training as education teams can respond and update in real-time. Feedback showed positive effects on treatment accuracy, confidence and perceived support levels [4], [33], [40].
Discussion
RTTs, dosimetrists, medical physicists and physicians all play key roles in the successful delivery of oART in both MR and CBCT-guided oART [21], therefore open communication and mentorship for training and credentialing activities should be a collaborative effort. A strong internal and external (consortium) MDT environment empowers the delivery of oART [21]. This will help to overcome oART implementation challenges of limited staffing. Through a shared approach to training, assessment and competence, clinicians can mentor RTTs through tasks that are traditionally RO assumed such as contouring and plan approval. It is important to invest in RTT training to instill appropriate confidence [21]. RTTs are well poised to take on advanced practice roles crossing the barriers of standard operating procedures. Indeed, AI has facilitated a redistribution of tasks to promote efficiency and release ROs valuable time for other tasks that cannot be automated or delegated [42]. Whereby, AI OAR contouring has replaced RTT contouring, abet some leniency [8] and similarly RO delineation activities have been replaced by RTTs, if not AI segmented [42]. Often clinicians are involved in credentialing and assessment of adaptive training techniques, assessing accuracy in skills and decision-making [7], [28]. Willigenburg et al [7] demonstrated successful RTT prostate CTV contour training for online adaption purposes, supervised by ROs. Using both online (actual patients) and simulated case studies, mentorship by ROs or similar technology that demonstrates a gold standard [7], [31], [32] will help to produce competent RTT advanced adapters.
The literature does recommend that when initially implementing oART for each patient and anatomical site, the treatment team should comprise of members from the MDT including ROs and ROMPs, particularly during the assessment of the adaptive system’s ability to propagate contours, plans and dose distributions on the patient’s anatomy of the day [27]. RTT experiences on conventional C-Arm linacs remain important such soft tissue knowledge, patient positioning and problem solving [21]. Such experiences allow the transfer of skills to the oART workflow. The ‘clinician-lite’ approach to oART requires on-call support during oART workflow and decision tools made available at the point of care.
With adequate training, the MDT must trust the RTTs to enact the patient clinical goals safely. McNair et al [18] highlight the importance of balancing number of trainees to number of patients referred for oART. Initial scoping exercises should consider number of linear accelerators, CT and MR images to sufficiently train enough RTTs to provide oART and maintain competency. Additionally, it is important that the skills are eventually passed to all available professionals and not a select few [21]. The online adaptive team will be required to make decisions on propagated contours and dose-wash review quicker than ever before, with expectation of minimal clinical effect on treatment accuracy. The time versus accuracy paradigm has been addressed in published literature and can inform authentic expectations for the number of contouring instances and time expectations for oART training programs. McNair et al [18] reports on RTT training for oART bladder in a single site with credentialing activities reduced over time, from 40 to 25 instances with an 80% pass mark for competence. Bertelsen et al [22] and others [7], [8], [27], [28] report median contouring time for trainees at 12 min for bladder, prostate and head and neck ‘Adapt to Shape’ MRIgART. When transitioning RO tasks to RTT-led, minor practical implications on time and accuracy are seen [5], [7]. Suggestions to further limit contouring time are proposed in the literature [7], [28].
To ensure compliance with legislative, regulatory and medico-legal governing bodies, published adaptive credentialing pathways require trainees to complete a workbook or evidence log of training to accurately record times, dates and details of training events, additional reading and assessment activities [17]. The advanced adapter RTT workbook will serve to document the trainee's competency profile as well as assist in auditing measures to ensure skill maintenance for continuing to practice for advanced adaptive treatments [28]. With formalised and ongoing feedback between the trainee and mentoring team, improvements are seen in accuracy, confidence and support as feedback sessions are used to clarify knowledge and understanding, as well as provide real time updates to training as required [4], [32], [40].
Credentialing activities need to prepare RTTs to use new techniques safely and accurately, providing guidance and support during implementation. A step-by-step guide for oART-advanced adapter RTT credentialing is presented in the Table 2. This outline draws upon key evidence-based activities for RTT credentialing in oART.
Table 2.
Outline for Credentialing activities for Advanced Online Adapter RTT in oART.
|
Ongoing maintenance of competency (12–20 cases per year, per site)
Conclusion
The benefits seen with the use of oART will likely lead to a progressive increase in its utilisation. Globally, treatment team ‘make-up’ and workflow responsibilities for oART are diverse and driven by local codes of practice and governing bodies. These differences should not be seen as a barrier or divider to designing a shared approach for a robust credentialing program for oART. But rather, serve as a vehicle to enhance global collaboration in transitioning RTTs to advanced adapters in a ‘clinician-lite’ oART workflow. Development of an advanced career pathway for RTTs will promote life-long learning, resulting in a more employable workforce with greater levels of retention within the profession [35], [36]. The application of oART into the clinic as routine, needs to harness the alliance of all radiation oncology professionals with the common goal of providing optimal care and improving patient outcomes.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: All authors are members of the Varian Adaptive Intelligence Consortium.
References
- 1.Sonke J.J., Aznar M., Rasch C. Adaptive radiotherapy for anatomical changes. Semin Radiat Oncol. 2019;29:245–257. doi: 10.1016/j.semradonc.2019.02.007. [DOI] [PubMed] [Google Scholar]
- 2.Bertholet J., Anastasi G., Noble D., Bel A., van Leeuwen R., Roggen T., et al. Patterns of practice for adaptive and real-time radiation therapy (POP-ART RT) part II: Offline and online plan adaption for interfractional changes. Radiother Oncol. 2020;153:88–96. doi: 10.1016/j.radonc.2020.06.017. ISSN 0167-8140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sibolt P., Andersson L.M., Calmels L., Sjöström D., Bjelkengren U., Geertsen P., et al. Clinical implementation of artificial intelligence-driven cone-beam computed tomography-guided online adaptive radiotherapy in the pelvic region. Phys Imaging Radiat Oncol. 2021;17:1–7. doi: 10.1016/j.phro.2020.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Webster A., Hafeez S., Lewis R., Griffins C., Warren-Oseni K., Patel E., et al. The Development of Therapeutic Radiographers in Imaging and Adaptive Radiotherapy Through Clinical Trial Quality Assurance. Clin Oncol (R Coll Radiol). 2021 doi: 10.1016/j.clon.2021.02.009. S0936-6555(21)00052-2. Epub ahead of print. PMID: 33766503. [DOI] [PubMed] [Google Scholar]
- 5.Intven M.P.W., de Mol van Otterloo S.R., Mook S., Doornaert P.A.H., de Groot-van Breugel E.N., Sikkes G.G., et al. Online adaptive MR-guided radiotherapy for rectal cancer; feasibility of the workflow on a 1.5T MR-linac: clinical implementation and initial experience. Radiother Oncol. 2021;154:172–178. doi: 10.1016/j.radonc.2020.09.024. Epub 2020 Sep 22. PMID: 32976875. [DOI] [PubMed] [Google Scholar]
- 6.Hales R.B., Rodgers J., Whiteside L., McDaid L., Berresford J., Budgell G., et al. Therapeutic Radiographers at the Helm: Moving Towards Radiographer-Led MR-Guided Radiotherapy. J Med Imaging Radiat Sci. 2020;51(3):364–372. doi: 10.1016/j.jmir.2020.05.001. [DOI] [PubMed] [Google Scholar]
- 7.Willigenburg T., de Muinck Keizer D.M., Peters M., Claes A., Lagendijk J.J.W., de Boer H.C.J. van der Voort van Zyp JRN. Evaluation of daily online contour adaptation by radiation therapists for prostate cancer treatment on an MRI-guided linear accelerator. Clin Transl Radiat Oncol. 2021;27:50–56. doi: 10.1016/j.ctro.2021.01.002. PMID: 33532630; PMCID: PMC7822780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yoon S.W., Lin H., Alonso-Basanta M., Anderson N., Apinorasethkul O., Cooper K., et al. Initial Evaluation of a Novel Cone-Beam CT-Based Semi-Automated Online Adaptive Radiotherapy System for Head and Neck Cancer Treatment - A Timing and Automation Quality Study. Cureus. 2020;12(8) doi: 10.7759/cureus.9660. PMID: 32923257; PMCID: PMC7482986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Acharya S., Fischer-Valuck B.W., Kashani R., Parikh P., Yang D., Zhao T., et al. Online Magnetic Resonance Image Guided Adaptive Radiation Therapy: First Clinical Applications. Int J Radiat Oncol Biol Phys. 2016;94(2):394–403. doi: 10.1016/j.ijrobp.2015.10.015. Erratum in: Int J Radiat Oncol Biol Phys. 2016 Sep 1;96(1):243. PMID: 26678659. [DOI] [PubMed] [Google Scholar]
- 10.Bohoudi O., Bruynzeel A.M.E., Senan S., Cuijpers J.P., Slotman B.J., Lagerwaard F.J., et al. Fast and robust online adaptive planning in stereotactic MR-guided adaptive radiation therapy (SMART) for pancreatic cancer. Radiother Oncol. 2017;125(3):439–444. doi: 10.1016/j.radonc.2017.07.028. ISSN 0167-8140. [DOI] [PubMed] [Google Scholar]
- 11.Placidi L., Romano A., Chiloiro G., Cusumano D., Boldrini L., Cellini F., et al. On-line adaptive MR guided radiotherapy for locally advanced pancreatic cancer: Clinical and dosimetric considerations, Technical Innovations & Patient Support in Radiation. Oncology. 2020;15:15–21. doi: 10.1016/j.tipsro.2020.06.001. ISSN 2405-6324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Palacios M.A., Bohoudi O., Bruynzeel A.M.E., van Sörsen de Koste J.R., Cobussen P., Slotman B.J., et al. Role of Daily Plan Adaptation in MR-Guided Stereotactic Ablative Radiation Therapy for Adrenal Metastases. Int J Rad Onc Bio Phy. 2018;102(2):426–433. doi: 10.1016/j.ijrobp.2018.06.002. ISSN 0360-3016. [DOI] [PubMed] [Google Scholar]
- 13.Vestergaard A., Muren L.P., Lindberg H., Jakobsen K.L., Petersen J.B.B., Elstrøm U.V., et al. Normal tissue sparing in a phase II trial on daily adaptive plan selection in radiotherapy for urinary bladder cancer. Acta Oncol (Madr) 2014;53(8):997–1004. doi: 10.3109/0284186X.2014.928419. [DOI] [PubMed] [Google Scholar]
- 14.Henke L., Kashani R., Robinson C., Curcuru A., DeWees T., Bradley J., et al. Phase I trial of stereotactic MR-guided online adaptive radiation therapy (SMART) for the treatment of oligometastatic or unresectable primary malignancies of the abdomen. Radiother Oncol. 2018;126:519–526. doi: 10.1016/j.radonc.2017.11.032. [DOI] [PubMed] [Google Scholar]
- 15.Thörnqvist S., Hysing L.B., Tuomikoski L., Vestergaard A., Tanderup K., Muren L.P., et al. Adaptive radiotherapy strategies for pelvic tumors – a systematic review of clinical implementations. Acta Oncol (Madr) 2016;55(8):943–958. doi: 10.3109/0284186X.2016.1156738. [DOI] [PubMed] [Google Scholar]
- 16.Yeh J., Bressel M., Tai K.H., Kron T., Foroudi F. A retrospective review of the long-term outcomes of online adaptive radiation therapy and conventional radiation therapy for muscle invasive bladder cancer. Clin Transl Radiat Oncol. 2021;30:65–70. doi: 10.1016/j.ctro.2021.08.001. Published 2021 Aug 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boejen A., Vestergaard A., Hoffmann L., Ellegaard M.-B., Rasmussen A.-M., Møller D., et al. A learning programme qualifying radiation therapists to manage daily online adaptive radiotherapy. Acta Oncol. 2015;54(9):1697–1701. doi: 10.3109/0284186X.2015.1062914. [DOI] [PubMed] [Google Scholar]
- 18.McNair H.A., Hafeez S., Taylor H., Lalondrelle S., McDonald F., Hansen V.N., et al. Radiographer-led plan selection for bladder cancer radiotherapy: initiating a training programme and maintaining competency. Br J Radiol. 2015;88(1048):20140690. doi: 10.1259/bjr.20140690. [DOI] [PubMed] [Google Scholar]
- 19.Price A., Kim H., Henke L.E., Knutson N.C., Spraker M.B., Michaelski J., et al. Implementing a Novel Remote Physician Treatment Coverage Practice for Adaptive Radiation Therapy During the Coronavirus Pandemic. Adv Radiat Oncol. 2020;5(4):737–742. doi: 10.1016/j.adro.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McNair H.A., Wiseman T., Joyce E., Peet B., Huddart R.A. International survey; current practice in On-line adaptive radiotherapy (ART) delivered using Magnetic Resonance Image (MRI) guidance. Tech Innovat Pat Supp Radiat Oncol. 2020;16:1–9. doi: 10.1016/j.tipsro.2020.08.002. ISSN 2405-6324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McNair H.A., Joyce E., O'Gara G., Jackson M., Peet B., Huddart R.A., et al. Radiographer-led online image guided adaptive radiotherapy: A qualitative investigation of the therapeutic radiographer role. Radiography (Lond). 2021 doi: 10.1016/j.radi.2021.04.012. S1078-8174(21)00051-1. Epub ahead of print. PMID: 34006442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bertelsen A.S., Schytte T., Møller P.K., Mahmood F., Riis H.L., Gottlieb K.L., et al. First clinical experiences with a high field 1.5 T MR linac. Acta Oncol. 2019;58(10):1352–1357. doi: 10.1080/0284186X.2019.1627417. [DOI] [PubMed] [Google Scholar]
- 23.Glide-Hurst C.K., Lee P., Yock A.D., Olsen J.R., Cao M., Siddiqui F., et al. Adaptive Radiation Therapy (ART) Strategies and Technical Considerations: A State of the ART Review From NRG Oncology. Int J Radiat Oncol Biol Phys. 2021;109(4):1054–1075. doi: 10.1016/j.ijrobp.2020.10.021. Epub 2020 Oct 24. PMID: 33470210; PMCID: PMC8290862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Duffton A., Moore K., Williamson A. Diversity in radiation therapist/therapeutic radiographer (RTT) advanced practice (AP) roles delivering on the four domains. Technical Innovations & Patient Support in Radiation Oncology. 2021;17:102–107. doi: 10.1016/j.tipsro.2021.02.003. ISSN 24056324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Winkel D., Bol G.H., Kroon P.S., van Asselen B., Hackett S.S., Werensteijn-Honingh A.M., et al. Adaptive radiotherapy: The Elekta Unity MR-linac concept, Clinical and Translational. Radiation Oncology. 2019;18:54–59. doi: 10.1016/j.ctro.2019.04.001. ISSN 2405-6308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jaffray D.A., Siewerdsen J.H., Wong J.W., Martinez A.A. Flat-panel cone-beam computed tomography for image-guided radiation therapy. Int J Radiat Oncol Biol Phys. 2002;53(5):1337–1349. doi: 10.1016/s0360-3016(02)02884-5. [DOI] [PubMed] [Google Scholar]
- 27.Hunt A., Hanson I., Dunlop A., Barnes H., Bower L., Chick J., et al. Feasibility of magnetic resonance guided radiotherapy for the treatment of bladder cancer, Clinical and Translational. Radiation Oncology. 2020;25:46–51. doi: 10.1016/j.ctro.2020.09.002. ISSN 2405-6308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Daal D.M., Haverkate L.E., ten Asbroek L., Zwart L.G.M., van Dieren E.B., de Wit E. CBCT-guided online adaptive radiotherapy: implementation of an RTT-led workflow. ESTRO Abstract. 2021 [Google Scholar]
- 29.Werensteijn-Honingh A.M., Kroon P.S., Winkel D., Aalbers E.M., van Asselen B., et al. Feasibility of stereotactic radiotherapy using a 1.5 T MR-linac: Multi-fraction treatment of pelvic lymph node oligometastases. Radiother Oncol. 2019;134:50–54. doi: 10.1016/j.radonc.2019.01.024. ISSN 0167-8140. [DOI] [PubMed] [Google Scholar]
- 30.Glide-Hurst C.K., Lee P., Yock A.D., Olsen J.R., Cao M., Siddiqui F., et al. Adaptive Radiation Therapy (ART) Strategies and Technical Considerations: A State of the ART Review From NRG Oncology. Int J Radiat Oncol Biol Phys. 2021;109(4):1054–1075. doi: 10.1016/j.ijrobp.2020.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Patel E., Tsang Y., Baker A., Callender J., Hafeez S., Hall E., et al. Quality assuring “Plan of the day” selection in a multicentre adaptive bladder trial: Implementation of a pre-accrual IGRT guidance and assessment module. Clin Transl Radiat Oncol. 2019;19:27–32. doi: 10.1016/j.ctro.2019.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Foroudi F., Wong J., Kron T., Roxby P., Haworth A., Bailey A., et al. Development and evaluation of a training program for therapeutic radiographers as a basis for online adaptive radiation therapy for bladder carcinoma. Radiography. 2010;16(1):14–20. doi: 10.1016/j.radi.2009.09.00230. ISSN 1078-8174. [DOI] [Google Scholar]
- 33.Pham D., Roxby P., Kron T., Rolfo A., Foroudi F. Introduction of online adaptive radiotherapy for bladder cancer through a multicentre clinical trial (Trans-Tasman Radiation Oncology Group 10.01): Lessons learned. J Med Phys. 2013;38(2):59–66. doi: 10.4103/0971-6203.111308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ionising Radiation (Medical Exposure) Regulations: Implications for clinical practice in radiotherapy – Guidance from the Radiotherapy Board. Royal College of Radiologists; June 2020. Available: https://www.rcr.ac.uk/sites/default/files/guidance-on-irmer-implications-for-clinical-practice-in-radiotherapy.pdf.
- 35.Coffey M., Leech M. The European Society of Radiotherapy and Oncology (ESTRO) European Higher Education Area levels 7 and 8 postgraduate benchmarking document for Radiation TherapisTs (RTTs) Tech Innovat Pat Supp Radiat Oncol. 2018;8:22–40. doi: 10.1016/j.tipsro.2018.09.009. ISSN 2405-6324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Khine N.M., Stewart-Lord A. An examination of Advanced Clinical Practice: Qualitative insights from therapeutic radiography advanced and consultant practitioners based in England, Technical Innovations & Patient Support in Radiation. Oncology. 2021;17:97–101. doi: 10.1016/j.tipsro.2020.12.003. ISSN 2405-6324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Technical Medicine. The Dutch Association for Technical Medicine (NVvTG) [online]. Available: nvvtg.nl/en/technical-medicine (no date) Last accessed 07/07/21.
- 38.Individual Health Care Professionals Act (BIG Act), [online]. Available: https://wetten.overheid.nl/BWBR0006251/2021-07-01#HoofdstukIII Last updated: 01/07/2021.
- 39.Kron T., Pham D., Roxby P., Rolfo A., Foroudi F. Credentialing of radiotherapy centres for a clinical trial of adaptive radiotherapy for bladder cancer (TROG 10.01) Radiother Oncol. 2012;103(3):293–298. doi: 10.1016/j.radonc.2012.03.003. ISSN 0167-8140. [DOI] [PubMed] [Google Scholar]
- 40.Alexander S.E., Hopkins N., Lalondrelle S., Taylor A., Titmarsh K., McNair H.A. RTT-led IGRT for cervix cancer; training, implementation and validation. Tech Innovat Pat Supp Radiat Oncol. 2019;12:41–49. doi: 10.1016/j.tipsro.2019.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mazur L.M., Adams R., Mosaly P.R., Stiegler M.P., Nuamah J., Adapa K., et al. Impact of Simulation-Based Training on Radiation Therapists’ Workload, Situation Awareness, and Performance. Adv Radiat Oncol. 2020;5(6):1106–1114. doi: 10.1016/j.adro.2020.09.008. ISSN 2452-1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Korreman S., Eriksen J.G., Grau C. The changing role of radiation oncology professionals in a world of AI - Just jobs lost - Or a solution to the under-provision of radiotherapy? Clin Transl Radiat Oncol. 2020;26:104–107. doi: 10.1016/j.ctro.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]