Key message
The pathological mechanism of catastrophic APS after severe acute respiratory syndrome coronavirus 2 vaccination implies a clinical resemblance between catastrophic APS and COVID-19 infection.
Dear Editor, Catastrophic APS (CAPS) is a life-threatening condition characterized by multiple thromboembolic events occurring in a short period of time, frequently accompanied by significant systemic inflammation [1]. There have been severe coronavirus disease 2019 (COVID-19) cases that closely resemble CAPS given the concurrence of aPLs, large vessel thrombosis and thrombotic microangiopathy with complement activation [2, 3]. Here, we report a case of CAPS in a patient who developed thrombosis in multiple organs, including brain, heart, kidney, spleen and digits, 1 day after COVID-19 vaccination, and subsequent investigation showed triple-positive aPLs. We discuss potential hypotheses on the mechanism behind this very rare case of CAPS following the COVID-19 vaccination.
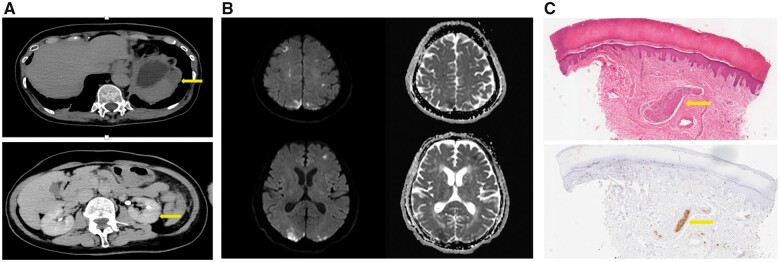
A 71-year-old Japanese female with a past medical history of coronary artery disease presented to emergency room at a local hospital with a sudden onset of weakness of the lower extremities. She received a first dose of COVID-19 vaccine (BNT162b by BioNTech/Pfizer) 1 day before presentation. On her arrival at the emergency room, physical examination was remarkable for a cyanotic change of multiple digits and decreased strength of the lower extremities. ECG showed ST elevation in leads, III and aVf and ST depression in leads V2–V5. Complete blood count showed a white blood cell count of 25 370 cells/µl, including 95.4% neutrophils, haemoglobin of 11.2 g/dl and a platelet count of 759 000/μl (Supplementary Table S1, available at Rheumatology Advances in Practice online). Other investigations were remarkable for a troponin I of 336 ng/ml (normal, <0.04 ng/ml) and CKMB 451 U/l (normal, <9 U/l), D-dimer 12.3 µg/ml (normal, <1.0 µg/ml) and CRP of 0.62 mg/dl (normal, <0.3 mg/dl). Kidney and liver function tests were unremarkable. She was transferred to a cardiovascular centre for probable acute myocardial infarction and started on heparin infusion. Further ECG showed resolution of the ST elevation. Coronary arteriography revealed no new occlusion, including previously known total occlusion of the right coronary artery and 75% occlusion of the left anterior descending artery, indicating spontaneous coronary reperfusion. Abdominal CT scan showed renal and splenic infarction (Fig. 1A). Head MRI revealed acute bi-hemispheric infarctions (Fig. 1B). Given the probable multiple thromboembolic episodes despite being on aspirin and heparin, aspirin was changed to clopidogrel 75 mg daily, and heparin infusion was switched to argatroban infusion. Trans-thoracic and trans-oesophageal echocardiogram was negative for vegetation or right-to-left shunt. US of the lower extremities showed no deep venous thrombosis.
Fig. 1.
Clinical manifestations of CAPS after COVID-19 vaccination
(A) Abdominal CT scan showing renal and splenic infarction (arrows). (B) Head MRI (diffusion weighted and ADC) showing acute bi-hemispheric infarctions. (C) (a) Haematoxylin and Eosin staining of right-hand second digit showing microthrombus (arrow). (b) Immunocytochemical staining of platelet glycoproteins with CD61 (arrow). ADC: Apparent diffusion coefficient.
Four days post-admission at the cardiovascular centre, she developed a new lesion of digital cyanosis (left thumb). Given the ongoing embolic events despite antithrombic treatment, the patient was transferred to our hospital for further evaluation and treatment. The additional work-up demonstrated positive aPLs, including positive lupus anticoagulant, elevated anti-beta2-GP1 IgM antibodies of 49.0 U/ml (normal, <20 U/ml) and IgG antibodies of 583.9 U/ml (normal, <20 U/ml), with cardiolipin IgM antibodies of 66.1 U/ml (normal, <20 U/ml) and IgG antibodies of 74.3 U/ml (normal, <20 U/ml). Complement levels were low, with C3 of 47 (normal, 65–135 mg/dL) and C4 of 3 (normal, 13–35 mg/dL). Skin biopsy of the right-hand second digit at the cardiovascular centre showed microthrombus formation in the superficial dermis (Fig. 1C). The patient met the four criteria for CAPS. Methylprednisolone 500 mg per day i.v. was started, followed by oral prednisolone 1 mg/kg (40 mg) per day. Plasmapheresis was also initiated.
After initiation of treatment, the patient’s symptoms subsided, with improvements of digital ischaemia. She was placed on long-term oral anticoagulation with warfarin and discharged with steroid taper. Of note, the patient had thrombocytosis. Bone marrow biopsy showed proliferation mainly of the megakaryocyte lineage. Further evaluation showed the JAK2V617F variant by allele-specific polymerase chain reaction [45.741% (normal, <1.000%)], consistent with essential thrombocythaemia. She was also treated with hydroxyl carbamide.
Although the mechanisms by which BNT162b vaccination can trigger APS or CAPS remain unclear, the similarity seen in the pathophysiology of thrombosis between severe COVID-19 infection and CAPS is interesting. Given that CAPS occurred on the day after vaccination, immunization induction of aPL by the vaccine is unlikely. We postulate that the patient had a serological background of aPL, and subsequently developed CAPS after the vaccination (second hit) by the following mechanism. BNT162b mRNA vaccines promote innate immune responses along with production of spike proteins [4]. Intracellular RNA sensors, such as Toll-like receptor 7 and MDA5, recognize the mRNA vaccines [4], resulting in local and systemic inflammation. But this patient had little or no inflammation at the injection site or systemically, suggesting that other factors should be taken into consideration. One possible mechanism is that the S1 and S2 subunits of spike proteins that are created in response to the vaccine might form a phospholipid-like epitope that induces the generation of aPLs [5]. It is reasonable to think that coexistence of essential thrombocythaemia was also involved. Given that the patient did not have preceding symptoms, such as fever, before developing CAPS, other precipitating factors, such as viral infections, are unlikely. From our case, the rationale for withholding BNT162b vaccination in patients with aPL or APS is weak, but rather useful in understanding the pathophysiology of COVID-19 and APS.
Supplementary Material
Acknowledgements
The authors would like to thank Rei Yoshimine for editing and reviewing this manuscript for English language.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Disclosure statement: The authors have declared no conflicts of interest.
Patient consent for publication: Informed consent was obtained for the publication of this manuscript.
Data availability statement
All data are incorporated into the article and its online supplementary material.
Supplementary data
Supplementary data are available at Rheumatology Advances in Practice online.
References
- 1. Rodriguez-Pintó I, Espinosa G, Cervera R.. Catastrophic antiphospholipid syndrome: the current management approach. Best Pract Res Clin Rheumatol 2016;30:239–49. [DOI] [PubMed] [Google Scholar]
- 2. Helms J, Tacquard C, Severac F. et al. ; CRICS TRIGGERSEP Group (Clinical Research in Intensive Care and Sepsis Trial Group for Global Evaluation and Research in Sepsis). High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med 2020;46:1089–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Magro C, Mulvey JJ, Berlin D. et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res 2020;220:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Teijaro JR, Farber DL.. COVID-19 vaccines: modes of immune activation and future challenges. Nat Rev Immunol 2021;21:195–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tung ML, Tan B, Cherian R, Chandra B.. Anti-phospholipid syndrome and COVID-19 thrombosis: connecting the dots. Rheumatol Adv Pract 2021;5:rkaa081. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data are incorporated into the article and its online supplementary material.