Abstract
Background
We aimed to determine the characteristics, risk factors, and outcomes associated with readmission in COVID-19 patients.
Methods
PubMed, Embase, Web of Science, and Scopus databases were searched to retrieve articles on readmitted COVID-19 patients, available up to September 25, 2021. All studies comparing characteristics of readmitted and non-readmitted COVID-19 patients were included. We also included articles reporting the reasons for readmission in COVID-19 patients. Data were pooled and meta-analyzed using random or fixed-effect models, as appropriate. Subgroup analyses were conducted based on the place and duration of readmission.
Results
Our meta-analysis included 4823 readmitted and 63,413 non-readmitted COVID-19 patients. The re-hospitalization rate was calculated at 9.3% with 95% Confidence Interval (CI) [5.5%–15.4%], mostly associated with respiratory or cardiac complications (48% and 14%, respectively). Comorbidities including cerebrovascular disease (Odds Ratio (OR) = 1.812; 95% CI [1.547–2.121]), cardiovascular (2.173 [1.545–3.057]), hypertension (1.608 [1.319–1.960]), ischemic heart disease (1.998 [1.495–2.670]), heart failure (2.556 [1.980–3.300]), diabetes (1.588 [1.443–1.747]), cancer (1.817 [1.526–2.162]), kidney disease (2.083 [1.498–2.897]), chronic pulmonary disease (1.601 [1.438–1.783]), as well as older age (1.525 [1.175–1.978]), male sex (1.155 [1.041–1.282]), and white race (1.263 [1.044–1.528]) were significantly associated with higher readmission rates (P < 0.05 for all instances). The mortality rate was significantly lower in readmitted patients (OR = 0.530 [0.329–0.855], P = 0.009).
Conclusions
Male sex, white race, comorbidities, and older age were associated with a higher risk of readmission among previously admitted COVID-19 patients. These factors can help clinicians and policy-makers predict, and conceivably reduce the risk of readmission in COVID-19 patients.
Keywords: COVID-19, Readmission, Hospital, Emergency department, Risk factor, Systematic review, Meta-analysis
1. Introduction
The new coronavirus pneumonia began to spread in Wuhan, China, in late December 2019. Later, the World Health Organization (WHO) named it coronavirus disease 2019 (COVID-19) and recognized it a public health emergency [1]. WHO has confirmed 226 million COVID-19 cases and 4.6 million deaths worldwide, as of September 21, 2021 [2].
Numerous characteristics and clinical risk factors, including age, gender, race, and comorbidities have been reportedly associated with mortality, morbidity, and admission in COVID-19 patients [3,4]. Readmission, defined as the unplanned return of patients to the hospital wards, is a crucial quality indicator in the health care system [5]. A recent systematic review has divided the post-discharge situation of COVID-19 patients into three categories of mortality, reinfection, and readmission to different hospital wards. The review estimated the readmission rate in COVID-19 patients at around 7.5% [6].
Certain demographic or clinical features can be associated with greater risk of readmission in COVID-19 patients [[7], [8], [9]]. Only a few sparse studies are present on this subject, which have reported contradictory findings, indicating gender [10,11], age [12,13], and comorbidities [14,15], to be influencing the risk of readmission in COVID-19 patients. The limited number of readmitted patients, even in large cohort studies, has made the findings rather inconclusive [8,16]. Therefore, this systematic review and meta-analysis was aimed to elucidate the clinical characteristics, risk factors, and outcomes in readmitted and non-readmitted COVID-19 patients in order to provide new insights that can help clinicians and health policy-makers control the pandemic by altering health policies.
2. Methods
2.1. Search strategy
This is a two-phase systematic review that was performed according to the recommendations of the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA) [17]. PubMed, Embase, Scopus, and Web of Science were searched for articles evaluating readmission of COVID-19 patients up to September 25, 2021. We also searched Google Scholar and the reference lists of the included articles to find other papers that might meet our inclusion criteria. Two main keywords, “COVID-19” and “Readmission”, were used in different combinations to search databases. A complete list of search strategies for all databases is provided in Supplementary Table S1. Articles written in English were included with no limitations in terms of publication date [18]. The present study was approved by the institutional review board of Mashhad University of Medical Sciences (Approval Code: 4001149).
2.2. Selection criteria
Initially, all studies that reported information on readmitted COVID-19 patients were included. Then, in phase 1 of the study, all articles comparing demographic data of readmitted and non-readmitted COVID-19 patients were included. Studies that combined the information of dead patients with live patients were excluded [[19], [20], [21], [22]]. Moreover, we excluded letters if they reported fewer than 10 readmitted patients [23].
In phase 2 of the study, we included studies that reported the readmission causes. We excluded review articles, case-reports, letters, conference abstracts, case-control studies, and gray literature such as unpublished data, reports based on websites, and government regulatory documents [20].
2.3. Eligibility assessment
Four reviewers (A.A., A.F., M.A., and M.R.) were involved in the process of study selection based on the title, abstract, and full text of the articles. In cases where there was no agreement, the decision-making was resolved a fifth reviewer (A.Z.) checked eligibility to determine final inclusion.
2.4. Data extraction
Study characteristics including the first author's surname, publication date, title, study design, site of study (hospital(s), city, province or state, and country), COVID-19 confirmation method, and discharge criteria were extracted from the included articles. Characteristics of COVID-19 patients including date and length of index admission, duration of readmission, place of readmission, demographics, comorbidities, intensive care unit (ICU) admission, and use of different ventilation were also extracted. Data were stored in a Microsoft Excel spreadsheet (Redmond, WA).
2.5. Quality assessment
Two reviewers (A.G. and E.F.) independently screened included articles for quality assessment. The included studies were appraised using the Joanna Briggs Institute (JBI) assessment tools, which provide an appraisal tool for most types of the studies, including observational studies [24]. Any disagreement was resolved by discussion between investigators or a third reviewer.
2.6. Quantitative analysis
The magnitudes of the estimated effects were expressed as odds ratios (OR), with respective 95% confidence intervals (CIs) in brackets. We converted median values to mean using an estimation formula described by Wan et al. [25]. P < 0.05 was considered statistically significant in all calculations. Heterogeneity was quantitatively calculated by the I2 index. If the heterogeneity was high (Cochran's Q < 0.05), we used the random-effects model; otherwise, we used the fixed-effects model. Potential publication bias was investigated using funnel plots, Egger's test, and Begg's test [26,27]. Sensitivity analysis was done by changing the statistical models or removing letter papers. We ran subgroup analyses regarding 30-day readmissions and hospital readmissions. All statistical analyses were done by CMA V.3.
3. Results
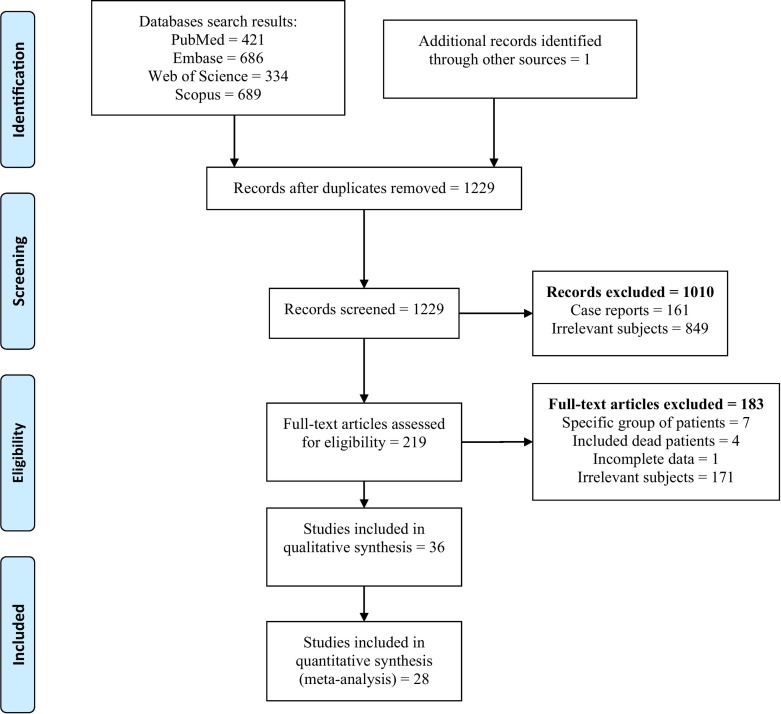
A total of 2130 studies were identified through searching the databases, of which 901 were duplicates (Fig. 1 ). Eventually, 36 studies were included in the present systematic review and 28 were incorporated in the meta-analysis [7,8,9,10,11,[13], [14], [15], [16],19,20,23,[28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52]]. Overall, 28 articles were included in phase 1 to determine risk factors and outcome of readmitted COVID-19 patients, and 19 articles were included in phase 2 to determine the cause of readmissions.
Fig. 1.
PRISMA flow diagram of the study.
Twelve studies were suspected of having the same patients as the Verna et al. study [9]. Out of these 12 studies, five that reported data on fewer than 50 patients were removed from the meta-analysis. We excluded two studies from the meta-analysis due to low quality, heterogeneity, or unclear data [28,53].
3.1. Characteristics of studies
Of the 28 articles included in the meta-analysis, 25 were original articles and three were letters. The majority of the studies (14, 50%) were done in the United States. Overall, 18 studies had assessed readmission in 30 or fewer days (range: 3–30 days), while nine assessed it over longer periods (range: 60–180 days), and one included both periods. Characteristics of the included studies are summarized in Table 1. Quality assessment showed that the included studies were of acceptable quality (Supplementary Table S2). Among the 28 included studies, only two studies did not use a polymerase chain reaction (PCR) test for confirmation of COVID-19 diagnosis [40,54].
Table 1.
Characteristics of the included studies.
| Author | Study design | Hospital(s)/City/Province (State) | Country | Date of primary admission | Readmission period (Days) (Max) | Place of index admission | Place of readmission | Reason for readmission |
|---|---|---|---|---|---|---|---|---|
| Jeon W. | Retrospective cohort | Nationwide Study | Republic of Korea | 2020 | 3 | Hospital | Hospital | Related to COVID-19 |
| Kilaru A‡ | Retrospective cohort | 5 Hospitals/Pennsylvania and New Jersey | United States | 1 March-28 May, 2020 | 3 | ED | Hospital | All-cause readmission |
| Muñoz F. | Retrospective cohort | Infanta Cristina Hospital (ICH)/Madrid | Spain | 17 March-25 April, 2020† | 6 | ED/ Hospital | Hospital | Related to COVID-19 |
| Carroll O.‡ | Prospective cohort | Vincent’s University Hospital/Dublin | Ireland | 2020 | 10 | Hospital | Hospital | All-cause readmission |
| Somani S. | Retrospective cohort | Mount Sinai Health System (MSHS)/New York City Hospitals | United States | 27 February-12 April, 2020 | 14 | ED/Hospital | ED/Hospital | Related to COVID-19 |
| Ye S.⁎ | Retrospective cohort | Tertiary Care Medical Center-Columbia-New York-Presbyterian Hospital | United States | 26 March-8 April, 2020 | 14 | ED/Hospital | ED/Hospital | UC |
| Menditto V. | Retrospective cohort | Ospedali Riuniti and Marche Nord/ Ancona and Pesaro | Italy | 1 March-28 April, 2020 | 15 | ED/Hospital | Hospital | UC |
| Llorens P. | Retrospective cohort | General University Hospital of Alicantet | Spain | 3 March-30 April, 2020 | 19 | ED | ED | Related to COVID-19 |
| Parra L. | Retrospective cohort | University Hospital in Madrid/Madrid | Spain | 26 February-20 April, 2020 | 21 | Hospital | Hospital | Related to COVID-19 |
| Chen S. | Retrospective cohort | Multicentre/Guangdong | China | 12 January-10 March, 2020† | 28 | Hospital | Hospital | Related to COVID-19 |
| Gwin M.⁎ | Retrospective cohort | Washington | United States | 28 February-13 May, 2020† | 30 | Hospital | ED/Hospital | All-cause readmission |
| Yeo I.⁎ | Retrospective cohort | Presbyterian Queens Hospital/New York City | United States | 13 March-9 April, 2020 | 30 | Hospital | ED/Hospital | All-cause readmission |
| Uyaroglu O. | Retrospective cohort | E-Pulse System | Turkey | 20 March-26 April, 2020 | 30 | ED/Hospital | Hospital | UC |
| Ramos-Martínez A. | Retrospective cohort | Nationwide Study | Spain | 1 March-30 April, 2020† | 30 | Hospital | Hospital | All-cause readmission |
| Verna E. | Retrospective cohort | Nationwide Study | United States | 15 February-9 June, 2020 | 30 | Hospital | Hospital | All-cause readmission |
| Ye X. | Retrospective cohort | Wenzhou Central Hospital | China | 17 January-5 March, 2020 | 30 | Hospital | Hospital | UC |
| Lobelo F. | Retrospective cohort | Kaiser Permanente Georgia Affiliated (KPGA) Hospitals/Atlanta/Georgia | United States | 3 March-21 October, 2020 | 30 | ED/Hospital | Hospital | All-cause readmission |
| Lenehan P.§ | Retrospective cohort | Tertiary Medical Centers in Minnesota, Arizona, and Florida | United States | Start of the COVID-19 pandemic-12 December, 2020 | 30 | Hospital | Hospital | All-cause readmission |
| Huang C.‡ | Retrospective cohort | 15 Kaiser Permanente Southern California (KPSC) Medical Centers | United States | 1 April-31 July, 2020 † | 30 | Hospital | Hospital | All-cause readmission |
| Loerinc L.⁎ | Retrospective cohort | Four Emory Healthcare Affiliated Hospitals/Georgia | United States | 26 March-21 April, 2020 † | 30 | ED/Hospital | ED/Hospital | Related to COVID-19 |
| Samuels S. | Retrospective cohort | Memorial Healthcare System (MHS) Facilities/ South Florida | United States | 2 March-31 May, 2020 | 30 | ED/Hospital | Hospital | UC |
| Kirkegaard C. | Retrospective cohort | Valld'Hebron University Hospital/Barcelona | Spain | 1 March-31 May, 2020 | 60 | Hospital | Hospital | All-cause readmission |
| Lobelo F. | Retrospective cohort | KPGA Affiliated Hospitals/Atlanta/Georgia | United States | 3 March-21 October, 2020 | 60 | ED/Hospital | Hospital | All-cause readmission |
| Saab F.⁎ | Case-series | University Of California, Los Angeles (UCLA) Medical Center | United States | 1 March-1 May, 2020 | 86 | Hospital | ED/Hospital | Related to COVID-19 |
| Pawlowskia C.⁎ | Retrospective cohort | Mayo Clinic and Hospitals Affiliated to the Mayo Rochester (Minnesota)/Florida/ Arizona | United States | 15 February-27 October, 2020 | 90 | Hospital | Hospital | All-cause readmission |
| Yang C. | Retrospective cohort | All Hospitals of the Shenzhen | China | 1 February-5 May, 2020 | 113 | Hospital | Hospital | Related to COVID-19 |
| Green H. | Retrospective cohort | Rabin Medical Center/Petah Tiqva | Israel | March-10 October, 2020 | 161 | Hospital | Hospital | All-cause readmission |
| Guarin G.⁎ | Retrospective cohort | Einstein Medical Centre Philadelphia/Philadelphia/Pennsylvania | United States | 1 March-24 April, 2020 | 180 | Hospital | Hospital | UC |
| Günster D. | Retrospective cohort | Nationwide Study | Germany | 1 February-30 April, 2020 | 180 | Hospital | Hospital | All-cause readmission |
| Drewett G. | Retrospective cohort | Austin Health/Melbourne | Australia | 1 March-1 October, 2020 | 180 | Hospital | Hospital | All-cause readmission |
| Lovinsky-Desir S. | Retrospective cohort | New York Presbyterian Hospital Network/New York City | United States | 11 February-7 May, 2020 | - | Hospital | Hospital | UC |
UC: Unclear; ED: emergency department.
Possible data duplication.
Date of first discharge.
Type of article was letter.
The paper mentioned case control study.
3.2. Risk factors and outcomes
Overall, 4823 readmitted and 63,413 none-readmitted patients were included in the meta-analysis. The overall re-hospitalization rate among live discharged patients was about 9.3% [95% CI: 5.5%–15.4%]. As shown in Table 2 and Supplementary Fig. S1, males were more likely to be readmitted and there was no strong association between ethnicity and readmission. The meta-analysis and sensitivity analysis showed different associations between age and readmission (Table 2).
Table 2.
The results of meta-analysis on the risk factors of readmission.
| Variables | Odds ratio [95% confidence intervals] | P-value | I2 (%) | Model | Number of studies | Sample Size (Readmitted/Non-readmitted) | |
|---|---|---|---|---|---|---|---|
| Demographics | |||||||
| Male | ≤30-Days | 1.168 [1.078–1.266] | 0.00 | 23 | F | 16 | 2563/55953 |
| [Hospital/ED] | 1.155 [1.041–1.282] | 0.007 | 36 | R | 21 | 4484/62184 | |
| [Hospital] | 1.190 [1.060–1.336] | 0.003 | 45 | R | 20 | 4407/62156 | |
| >30-Days | 1.076 [0.829–1.396] | 0.584 | 55 | R | 6 | 1996/6956 | |
| Hispanic ethnicity | ≤30-Days | 0.833 [0.632–1.099] | 0.197 | 50 | R†, ⁎ | 10 | 953/15780 |
| [Hospital/ED] | 0.767 [0.647–0.909] | 0.002 | 44 | F†, ⁎ | 11 | 1012/15953 | |
| [Hospital] | 0.966 [0.640–1.457] | 0.868 | 76 | R | 10 | 910/15894 | |
| Asian ethnicity | ≤30-Days | 1.119 [0.806–1.554] | 0.500 | 0 | F | 6 | 830/13744 |
| [Hospital/ED]‡ | 1.038 [0.759–1.419] | 0.815 | 0 | F | 9 | 974/14714 | |
| [Hospital] | 1.095 [0.785–1.528] | 0.593 | 0 | F | 8 | 877/14660 | |
| >30-Days | 0.486 [0.172–1.374] | 0.174 | 0 | F | 3 | 144/970 | |
| Black ethnicity | ≤30-Days | 1.129 [0.766–1.664] | 0.541 | 60 | R | 9 | 607/14776 |
| [Hospital/ED] | 1.072 [0.746–1.540] | 0.377 | 55 | R | 11 | 974/15023 | |
| [Hospital] | 0.945 [0.749–1.193] | 0.635 | 43 | F | 10 | 977/14969 | |
| >30-Days | 0.760 [0.500–1.154] | 0.198 | 0 | F | 3 | 237/1356 | |
| White ethnicity | ≤30-Days | 1.248 [1.019–1.529] | 0.032 | 44 | F†, ⁎ | 8 | 607/7937 |
| [Hospital/ED] | 1.263 [1.044–1.528] | 0.016 | 32 | F†, ⁎ | 10 | 676/8186 | |
| [Hospital] | 1.410 [1.145–1.735] | 0.001 | 0 | F | 9 | 605/8257 | |
| >30-Days | 1.355 [0.935–1.962] | 0.109 | 0 | F | 3 | 144/970 | |
| Age | [Hospital/ED] | 1.214 [0.793–1.858] | 0.372 | 93 | R† | 20 | 1424/18624 |
| [Hospital] | 1.204 [0.761–1.907] | 0.428 | 93 | R† | 18 | 1296/18496 | |
| ≤30-Days | 1.347 [0.869–2.088] | 0.182 | 91 | R† | 14 | 1122/16673 | |
| >30-Days | 0.967 [0.327–2.863] | 0.952 | 95 | R† | 6 | 302/1931 | |
| Comorbidities | |||||||
| No comorbidity | [Hospital/ED] | 0.983 [0.516–1.873] | 0.958 | 87 | R† | 7 | 645/10217 |
| [Hospital] | 0.979 [0.510–1.878] | 0.949 | 87 | R† | 7 | 635/10227 | |
| ≤30 Days | 1.108 [0.498–2.469] | 0.801 | 89 | R† | 6 | 581/9029 | |
| Immunosuppressed | [Hospital/ED] | 1.437 [0.879–2.351] | 0.148 | 30 | F | 6 | 409/8096 |
| [Hospital] | 1.357 [0.798–2.307] | 0.260 | 54 | F | 5 | 353/8101 | |
| <30 Days | 1.156 [0.627–2.133] | 0.642 | 47 | F | 4 | 365/7501 | |
| Cerebrovascular | [Hospital/ED] | 1.812 [1.547–2.121] | 0.00 | 0 | F | 5 | 1935/44267 |
| ≤30 Days | 1.781 [1.517–2.091] | 0.00 | 0 | F | 4 | 1885/43783 | |
| Cardiovascular | [Hospital/ED] | 2.173 [1.545–3.057] | 0.00 | 61 | R | 4 | 1578/36605 |
| [Hospital] | 2.100 [1.494–2.951] | 0.00 | 69 | R | 3 | 1557/36521 | |
| Hypertension | [Hospital/ED] | 1.608 [1.319–1.960] | 0.00 | 61 | R | 14 | 2461/51616 |
| [Hospital] | 1.734 [1.404–2.140] | 0.00 | 65 | R | 13 | 2384/51532 | |
| ≤30 Days | 1.650 [1.328–2.050] | 0.00 | 66 | R | 12 | 2361/50812 | |
| >30 Days | 1.258 [0.855–1.852] | 0.244 | 0 | F | 4 | 159/1061 | |
| Ischemic heart disease | [Hospital/ED] | 1.998 [1.495–2.670] | 0.00 | 13 | F | 8 | 672/12717 |
| [Hospital] | 2.278 [1.685–3.080] | 0.00 | 0 | F | 8 | 606/12783 | |
| ≤30 Days | 1.695 [1.188–2.419] | 0.004 | 8 | F | 6 | 490/12090 | |
| Heart failure | [Hospital/ED] | 2.556 [1.980–3.300] | 0.00 | 16 | F | 10 | 867/15205 |
| [Hospital] | 2.742 [2.107–2.567] | 0.00 | 0 | F | 10 | 801/15271 | |
| ≤30 Days | 2.598 [1.920–3.517] | 0.00 | 42 | F | 6 | 602/13744 | |
| >30 Days | 2.456 [1.527–3.950] | 0.00 | 0 | F | 4 | 199/1461 | |
| Obesity | [Hospital/ED] | 0.963 [0.719–1.289] | 0.798 | 71 | R | 8 | 1739/40956 |
| [Hospital] | 0.932 [0.690–1.260] | 0.647 | 74 | R | 7 | 1718/40872 | |
| ≤30 Days | 1.055 [0.750–1.486] | 0.757 | 77 | R | 6 | 1641/39173 | |
| >30 Days | 0.799 [0.525–1.216] | 0.295 | 27 | F | 3 | 147/1956 | |
| Diabetes | [Hospital/ED] | 1.588 [1.443–1.747] | 0.00 | 33 | F | 14 | 2400/51891 |
| [Hospital] | 1.609 [1.461–1.771] | 0.00 | 21 | F | 13 | 2323/51863 | |
| ≤30 Days | 1.588 [1.414–1.718] | 0.00 | 27 | F | 12 | 2316/50812 | |
| >30 Days | 1.950 [1.316–2.891] | 0.001 | 34 | F | 4 | 143/1336 | |
| Liver disease | [Hospital/ED] | 1.391 [0.681–2.841] | 0.365 | 74 | R† | 7 | 1786/40913 |
| [Hospital] | 1.362 [0.639–2.905] | 0.424 | 74 | R† | 7 | 1730/40969 | |
| ≤30 Days | 1.201 [0.496–2.908] | 0.684 | 82 | R† | 5 | 1782/39834 | |
| Cancer | [Hospital/ED] | 1.817 [1.526–2.162] | 0.00 | 36 | F | 8 | 1767/40866 |
| [Hospital] | 1.868 [1.568–2.225] | 0.00 | 48 | F | 8 | 1711/40922 | |
| ≤30 Days | 1.788 [1.497–2.135] | 0.00 | 41 | F | 7 | 1677/40327 | |
| Kidney disease | [Hospital/ED] | 2.083 [1.498–2.897] | 0.00 | 51 | R | 8 | 1968/42652 |
| [Hospital] | 2.478 [2.195–2.798] | 0.00 | 47 | F | 8 | 1912/42708 | |
| ≤30 Days | 2.519 [1.229–2.848] | 0.00 | 44 | F | 6 | 1868/41758 | |
| >30 Days | 1.574 [0.967–2.563] | 0.068 | 0 | F | 4 | 159/1061 | |
| HIV | [Hospital] | 1.506 [0.959–2.367] | 0.076 | 0 | F | 4 | 1484/36121 |
| Chronic pulmonary disease(COPD/Asthma) | [Hospital/ED] | 1.601 [1.438–1.783] | 0.00 | 34 | F | 14 | 2432/51684 |
| [Hospital] | 1.605 [1.440–1.789] | 0.00 | 38 | F | 13 | 2355/51656 | |
| ≤30 Days | 1.658 [1.324–2.077] | 0.00 | 50 | R | 10 | 2218/49210 | |
| >30 Days | 1.496 [1.047–2.139] | 0.027 | 0 | F | 6 | 273/2733 | |
| COPD | [Hospital/ED] | 2.071 [1.652–2.597] | 0.00 | 40 | F | 7 | 946/18630 |
| [Hospital] | 2.086 [1.657–2.626] | 0.00 | 43 | F | 7 | 875/18701 | |
| ≤30 Days | 2.137 [1.682–2.716] | 0.00 | 57 | F | 5 | 787/17569 | |
| Asthma | [Hospital/ED] | 1.404 [1.100–1.793] | 0.006 | 0 | F | 10 | 998/19689 |
| [Hospital] | 1.428 [1.111–1.834] | 0.005 | 0 | F | 10 | 927/19760 | |
| ≤30 Days | 1.458 [1.096–1.939] | 0.010 | 0 | F | 5 | 775/17440 | |
| >30 Days | 1.266 [0.788–2.032] | 0.329 | 0 | F | 5 | 223/2249 | |
| Inpatient factors | |||||||
| Mechanical ventilation | [Hospital] | 0.517 [0.399–0.668] | 0.000 | 0 | F | 3 | 1248/30732 |
| ICU admission | [Hospital/ED] | 0.907 [0.549–1.498] | 0.703 | 85 | R† | 7 | 1998/47631 |
| [Hospital] | 0.945 [0.570–1.564] | 0.825 | 84 | R | 7 | 1942/47687 | |
| ≤30 Days | 0.813 [0.478–1.382] | 0.444 | 86 | R† | 6 | 1964/47036 | |
| Length of initial hospital stay | [Hospital/ED] | 1.055 [0.693–1.605] | 0.804 | 95 | R† | 10 | 2300/49740 |
| [Hospital] | 1.082 [0.705–1.662] | 0.362 | 95 | R† | 10 | 2244/49796 | |
| ≤30 Days | 0.804 [0.536–1.207] | 0.292 | 94 | R† | 8 | 2173/48759 | |
| >30 Days | 1.703 [0.331–8.771] | 0.524 | 94 | R† | 3 | 137/1065 | |
ED: Emergency department; F: Fixed-effects model; R: Random-effects model; COPD: Chronic Obstructive Pulmonary Disease; HIV: Human immunodeficiency virus; I2: Heterogeneity index.
Sensitivity analysis, removing letter papers, show different results.
Sensitivity analysis, change fixed or random-effects together, show different results.
Presence of publication bias, based on Egger's test.
We conducted a specific subgroup analysis for the age variable after removing two studies that contained only COVID-19 re-positive patients. Subgroup meta-analysis and sensitivity analysis showed that age was another risk factor for readmission (OR = 1.525 [95% CI: 1.175–1.978], P = 0.001). Supplementary Table S3, Supplementary Table S4 present the crude data of all included studies on demographic/inpatient factors and comorbidities, respectively.
As Table 2 implies, patients with kidney disease, heart failure, and chronic obstructive pulmonary disease (COPD) had higher odds of hospital readmission (OR = 2.478 [95% CI: 2.195–2.798], 2.742 [2.107–2.567], 2.086 [1.657–2.626], respectively; P < 0.001). Table 2 also shows effects of inpatient factors on readmission. Moreover, the mortality rate was lower in the second admission compared to the index admission (OR = 0.530 [95% CI: 0.329–0.855], I2 = 78%, P = 0.009).
3.3. Publication bias and sensitivity analysis
The funnel plots for all studied variables are presented in Fig. S1. The Egger's and Begg's tests showed no significant publication bias regarding any of the variables, except for Asian ethnicity [hospital/emergency department (ED)] that showed moderate publication bias in the Eggers test (Table 2). Furthermore, sensitivity analysis showed that the results pertaining to Hispanic and white ethnicities, age, no-comorbidity, liver disease, ICU admission, and length of hospital stay may not be reliable (Table 2).
3.4. Causes of readmission
After discharge, most of the readmission causes were COVID-19-related respiratory complications, cardiac complications, thromboembolism, bacterial infection, trauma, kidney-related complications, and hemorrhages. Supplementary Table S5 presents the most important readmission causes. The respiratory complications of COVID-19 caused 3.5 times more readmissions compared with the cardiac complications; out of a total of 3342 readmitted patients in studies that reported both respiratory and cardiac-related readmissions, 1571 patients were readmitted due to respiratory complications and only 455 were because of cardiac complications.
4. Discussion
Recognizing the risk factors associated with readmission in COVID-19 patients is essential for healthcare professionals and health policymakers to review and change existing rules and standards of practice and provide more effective health management strategies. In this study, we assessed the characteristics, risk factors, and outcomes of readmitted COVID-19 patients. We also assessed the main causes of readmission.
We estimated the pooled rate of readmission among patients previously admitted with COVID-19 to be around 9.3% [95%CI: 5.5%–15.4%]. The discrepancies in the readmission rates reported by different studies can be attributed to the differences in readmission period, readmission setting, discharge criteria, treatment approach, and characteristics of the admitted patients.
We found that male COID-19 patients and those who had comorbidities were more likely to be readmitted to hospital wards. The comorbidities that were associated with higher likelihood of readmission were cerebrovascular disease, hypertension, ischemic heart disease, cardiovascular disease, heart failure, diabetes, cancer, kidney disease, and chronic pulmonary diseases. In terms of ethnicity, white patients were more likely to be readmitted, compared to Hispanics. Moreover, patients who needed invasive mechanical ventilation during their index admission had a lower rate of readmission.
Previous studies have also reported some characteristics to be more common among certain race groups. For example, obesity, hypertension, asthma, and human immunodeficiency virus (HIV) infection are more prevalent among the black race, while diabetes is more common among Asians [36].
The difference between males and females in infectious pandemics has been reportedly linked to differences in various aspects including the immune system, genetics, and body physiology [55]. A previous meta-analysis by Subramaniam et al. has also reported the same results regarding gender [56].
We also found that the rate of mortality was lower in the second admission than in the first admission, because high-risk patients mostly expire during the index admission. According to the results of our meta-analysis, race and ethnicity had no robust effects on COVID-19 patients' readmissions. Pulmonary and cardiac complications were the most prevalent causes of readmission among COVID-19 patients.
The effects of comorbidities on increasing the risk of readmission could be explained by intensified inflammatory responses and organ defects; angiotensin-converting enzyme 2 (ACE2) has been reported to have a key role in this regard [57]. On the other hand, Patients who suffer from comorbidities are usually under treatment with certain medications or do not have proper lifestyle and nutrition status. Hence, they may have a recurrence of the disease or may not recover well and need to be readmitted.
Our results did not exhibit a significant relationship between immunosuppression and patients' readmission. However, Monreal et al. showed the protective role of non-severe immunosuppression against a possible hyper-inflammatory host response seen in COVID-19 patients [58], which alludes that it may help reduce the risk of readmission in these patients.
We found that obesity was not significantly associated with readmission. Suresh et al. found that obese COVID-19 patients are mostly younger and female, both of which are potential protective factors against readmission of COVID-19 patients; however, other comorbidities were more prevalent among obese COVID-19 patients, which may increase the likelihood of readmission in these patients [59]. Liver diseases are also reported as risk factors for hospitalization in COVID-19 patients [60], but we could not find a clear link between this comorbidity and the likelihood of readmission in these patients.
Our results are partially consistent with the recent meta-analysis by Subramaniam et al. [56]. Consistent with our findings, they also found the rate of ICU admission to be similar between the readmitted and non-readmitted patients. In contrast with our results, they found that some comorbidities like congestive heart failure and ischemic heart disease had no significant effects on readmission. They also reported that readmitted patients had a shorter hospital stay in their index admission, while we could not find robust evidence in this regard. These inconsistencies can mainly be attributed to the low number of studies and thus, smaller sample size of their study in comparison to the present meta-analysis.
Our subgroup analysis on the relation between age and readmission illustrated that although all-cause readmission was higher among older patients, readmissions due to COVID-19 reinfection may not be significantly associated with age, and this association should be investigated in further studies. A higher rate of all-cause readmission among older patients can be justified by the frequent existence of various comorbidities among them [61]. These results were in line with a previous systematic review that examined the risk factors of hospitalization, mortality, and severe infection among COVID-19 patients [62]. Similarly, Li et al. showed that being male, suffering from comorbidities, and older age were risk factors for severe COVID-19 disease [63].
4.1. Limitations
This study had some limitations. First, the causes of readmission were heterogeneous between studies. For instance, some studies included only patients who were readmitted because of COVID-19-related complications, while some assessed all-cause readmissions, and some others assessed only re-positive patients who were readmitted. Moreover, since two studies were performed on vast populations, it is probable that they included patients assessed in other studies. We tried to address this issue and reduce the chance of duplication by removing studies with fewer than 50 readmitted patients. Finally, the readmission period of included studies was different. Although we tried to address this limitation by performing subgroup analysis, some disparities still exist in subgroups.
5. Conclusion
Male sex, white race, and comorbidities including cerebrovascular disease, hypertension, cardiovascular disease, diabetes, cancer, kidney disease, and chronic pulmonary diseases are probably associated with a higher risk of readmission. The second admission can be widely associated with pulmonary and cardiac complications of COVID-19. Our findings can help clinicians and policymakers plan better strategies to reduce the rate of readmission in patients previously admitted with COVID-19 during the remaining days of the pandemic.
Funding
None.
Author contributions
E.F. and A.A. designed the study. A.A. and M.A. were involved in searching the databases. A.A., A.F., M.A., and M.R. screened the papers and extracted the relevant data. E.F. and A.G. were involved in the quality assessment of included articles. A.A. and A.Z. analyzed and interpreted the data. A.A., A.F., and M.R. wrote the manuscript, which E.F., A.Z., M.A., and A.G. revised. All authors read and approved the final manuscript.
Data availability statement
The data that support the findings of this study are provided in the supplementary files and are available from the corresponding author on request.
Declaration of Competing Interest
None.
Acknowledgments
We would like to thank from Student Research Committee, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran, for scientific supports.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajem.2021.12.012.
Appendix A. Supplementary data
The following are the supplementary data related to this article.
Forrest and funnel plots of meta-analyzed variables.
Search Strategy.
(A) Quality assessment table for cohort studies based on JBI Critical Appraisal.
Demographic and inpatient characteristics of readmitted and non-readmitted patients.
Distribution of comorbidities among readmitted and non-readmitted patients.
Causes of readmissions among COVID-19 patients.
References
- 1.Organization WH . World Health Organization; 2020. Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected: Interim guidance, 13 March 2020. [Google Scholar]
- 2.Weekly epidemiological update on COVID-19 - 21. 2021. https://covid19.who.int/
- 3.Richardson S., Hirsch J.S., Narasimhan M., Crawford J.M., McGinn T., Davidson K.W., et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. Jama. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Petrilli C.M., Jones S.A., Yang J., Rajagopalan H., O’Donnell L., Chernyak Y., et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020:369. doi: 10.1136/bmj.m1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fischer C., Lingsma H.F., Marang-van de Mheen P.J., Kringos D.S., Klazinga N.S., Steyerberg E.W. Is the readmission rate a valid quality indicator? A review of the evidence. PloS One. 2014;9(11):e112282. doi: 10.1371/journal.pone.0112282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ghorbani S.S., Taherpour N., Bayat S., Ghajari H., Mohseni P., Hashemi Nazari S.S. Epidemiologic characteristics of cases with re-infection, recurrence and hospital readmission due to COVID-19: a systematic review and meta-analysis. J Med Virol. 2021;94(1):44–53. doi: 10.1002/jmv.27281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Günster C., Busse R., Spoden M., Rombey T., Schillinger G., Hoffmann W., et al. 6-month mortality and readmissions of hospitalized COVID-19 patients: a nationwide cohort study of 8,679 patients in Germany. PloS one. 2021;16(8) doi: 10.1371/journal.pone.0255427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ramos-Martínez A., Parra-Ramírez L.M., Morrás I., Carnevali M., Jiménez-Ibañez L., Rubio-Rivas M., et al. Frequency, risk factors, and outcomes of hospital readmissions of COVID-19 patients. Sci Rep. 2021;11(1):1–10. doi: 10.1038/s41598-021-93076-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Verna E.C., Landis C., Brown R.S., Jr., Mospan A.R., Crawford J.M., Hildebrand J.S., et al. Factors associated with readmission in the US following hospitalization with COVID-19. Clinical Infectious Diseases. 2021;5(20):2021. doi: 10.1093/cid/ciab464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lenehan P.J., Ramudu E., Venkatakrishnan A., Berner G., McMurry R., O’Horo J.C., et al. Anemia during SARS-CoV-2 infection is associated with rehospitalization after viral clearance. Iscience. 2021;24(7) doi: 10.1016/j.isci.2021.102780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kirkegaard C., Falcó-Roget A., Sánchez-Montalvá A., Valls Á., Clofent D., Campos-Varela I., et al. Incidence and risk factors for early readmission after hospitalization for SARS-CoV-2 infection: results from a retrospective cohort study. Infection. 2021;1-10 doi: 10.1007/s15010-021-01662-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen S.-L., Xu H., Feng H.-Y., Sun J.-F., Li X., Zhou L., et al. Epidemiological and clinical findings of short-term recurrence of severe acute respiratory syndrome coronavirus 2 ribonucleic acid polymerase chain reaction positivity in 1282 discharged coronavirus disease 2019 cases: a multicenter, retrospective, observational study. Open Forum Infect Dis. 2020;7:ofaa432. doi: 10.1093/ofid/ofaa432. Oxford University Press US. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yeo I., Baek S., Kim J., Elshakh H., Voronina A., Lou M.S., et al. Assessment of thirty-day readmission rate, timing, causes and predictors after hospitalization with COVID-19. J Intern Med. 2021;290(1):157–165. doi: 10.1111/joim.13241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Llorens P., Moreno-Pérez O., Espinosa B., García T., Payá A.B., Sola S., et al. An integrated emergency department/hospital at home model in mild COVID-19 pneumonia: feasibility and outcomes after discharge from the emergency department. Intern Emerg Med. 2021;1-10 doi: 10.1007/s11739-021-02661-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Uyaroglu O.A., Basaran N.Ç., Özisik L., Tellidizman G., Eroglu I., Sahin T.K., et al. 2020. Thirty-day readmission rate of COVID-19 patients discharged from a tertiary care university hospital in Turkey: An observational, single-center study. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jeon W.-H., Seon J.Y., Park S.-Y., Oh I.-H. Analysis of risk factors on readmission cases of COVID-19 in the Republic of Korea: using nationwide health claims data. Int J Environ Res Public Health. 2020;17(16):5844. doi: 10.3390/ijerph17165844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moher D., Shamseer L., Clarke M., Ghersi D., Liberati A., Petticrew M., et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morrison A., Polisena J., Husereau D., Moulton K., Clark M., Fiander M., et al. The effect of English-language restriction on systematic review-based meta-analyses: a systematic review of empirical studies. Int J Technol Assess Health Care. 2012;28(2):138–144. doi: 10.1017/s0266462312000086. [DOI] [PubMed] [Google Scholar]
- 19.Atalla E., Kalligeros M., Giampaolo G., Mylona E.K., Shehadeh F., Mylonakis E. Readmissions among patients with COVID-19. Int J Clin Pract. 2021;75(3) doi: 10.1111/ijcp.13700. [DOI] [PubMed] [Google Scholar]
- 20.Lavery A.M., Preston L.E., Ko J.Y., Chevinsky J.R., DeSisto C.L., Pennington A.F., et al. Characteristics of hospitalized COVID-19 patients discharged and experiencing same-hospital readmission—United States, March–August 2020. Morb Mortal Wkly Rep. 2020;69(45):1695. doi: 10.15585/mmwr.mm6945e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kheir M., Saleem F., Wang C., Mann A., Chua J. Higher albumin levels on admission predict better prognosis in patients with confirmed COVID-19. Plos one. 2021;16(3) doi: 10.1371/journal.pone.0248358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Donnelly J.P., Wang X.Q., Iwashyna T.J., Prescott H.C. Readmission and death after initial hospital discharge among patients with COVID-19 in a large multihospital system. JAMA. 2021;325(3):304–306. doi: 10.1001/jama.2020.21465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.O’Carroll O., MacCann R., O’Reilly A., Dunican E.M., Feeney E.R., Ryan S., et al. Remote monitoring of oxygen saturation in individuals with COVID-19 pneumonia. Eur Respir J. 2020;56(2) doi: 10.1183/13993003.01492-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moola S., Munn Z., Tufanaru C., Aromataris E., Sears K., Sfetcu R., et al. Vol. 5. Joanna Briggs Institute Reviewer’s Manual The Joanna Briggs Institute; 2017. Chapter 7: systematic reviews of etiology and risk. [Google Scholar]
- 25.Wan X., Wang W., Liu J., Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14(1):135. doi: 10.1186/1471-2288-14-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Egger M., Smith G.D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. Bmj. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sterne J., Becker B., Egger M. In: Publication Bias in Meta-analysis: Prevention, assessment and adjustments. Rothstein H.R., Sutton A.J., Borenstein M., editors. Wiley; 2005. The funnel plot; pp. 75–98. [Google Scholar]
- 28.Carrillo-Garcia P., Garmendia-Prieto B., Cristofori G., Montoya I.L., Hidalgo J.J., Feijoo M.Q., et al. Health status in survivors older than 70 years after hospitalization with COVID-19: observational follow-up study at 3 months. European Geriatric Medicine. 2021;1-4 doi: 10.1007/s41999-021-00516-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen S.L., Xu H., Feng H.Y., Sun J.F., Li X., Zhou L., et al. Epidemiological and clinical findings of short-term recurrence of severe acute respiratory syndrome coronavirus 2 ribonucleic acid polymerase chain reaction positivity in 1282 discharged coronavirus disease 2019 cases: a multicenter, retrospective, observational study. Open Forum Infect Dis. 2020;7(10):1–10. doi: 10.1093/ofid/ofaa432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Drewett G.P., Chan R.K., Jones N., Wimaleswaran H., Howard M.E., McDonald C.F., et al. Risk factors for readmission following inpatient management of COVID-19 in a low-prevalence setting. Intern Med J. 2021;51(5):821. doi: 10.1111/imj.15218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Green H., Yahav D., Eliakim-Raz N., Karny-Epstein N., Kushnir S., Shochat T., et al. Risk-factors for re-admission and outcome of patients hospitalized with confirmed COVID-19. Sci Rep. 2021;11(1):1–8. doi: 10.1038/s41598-021-96716-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guarin G., Lo K.B., Bhargav R., Salacup G., Wattoo A., Coignet J.G., et al. Factors associated with hospital readmissions among patients with COVID-19: a single center experience. J Med Virol. 2021;93(9):5582–5587. doi: 10.1002/jmv.27104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gwin M., Saleki M., Lampert H., Meo N., Bann M. Emergency department visits and readmissions after COVID-19 hospitalization: a cross-sectional analysis. Intern Emerg Med. 2021;1-4 doi: 10.1007/s11739-021-02644-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Huang C.W., Desai P.P., Wei K.K., Liu I.L.A., Lee J.S., Nguyen H.Q. Characteristics of patients discharged and readmitted after COVID-19 hospitalisation within a large integrated health system in the United States. Infect Dis. 2021;53(10):800–804. doi: 10.1080/23744235.2021.1924398. [DOI] [PubMed] [Google Scholar]
- 35.Kilaru A.S., Lee K., Snider C.K., Meisel Z.F., Asch D.A., Mitra N., et al. Return hospital admissions among 1419 COVID-19 patients discharged from five US emergency departments. Acad Emerg Med. 2020;27(10):1039–1042. doi: 10.1111/acem.14117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lobelo F., Bienvenida A., Leung S., Mbanya A., Leslie E., Koplan K., et al. Clinical, behavioural and social factors associated with racial disparities in COVID-19 patients from an integrated healthcare system in Georgia: a retrospective cohort study. BMJ Open. 2021;11(5) doi: 10.1136/bmjopen-2020-044052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Loerinc L.B., Scheel A.M., Evans S.T., Shabto J.M., O’Keefe G.A., O’Keefe J.B. Discharge characteristics and care transitions of hospitalized patients with COVID-19. Healthcare. 2021;9(1) doi: 10.1016/j.hjdsi.2020.100512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lovinsky-Desir S., Deshpande D.R., De A., Murray L., Stingone J.A., Chan A., et al. Asthma among hospitalized patients with COVID-19 and related outcomes. J Allergy Clin Immunol. 2020;146(5) doi: 10.1016/j.jaci.2020.07.026. [1027–34. e4] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Menditto V.G., Fulgenzi F., Bonifazi M., Gnudi U., Gennarini S., Mei F., et al. Predictors of readmission requiring hospitalization after discharge from emergency departments in patients with COVID-19. Am J Emerg Med. 2021;46:146–149. doi: 10.1016/j.ajem.2021.04.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Muñoz F.J.T., García-Guijarro E., García-Domingo P., Pérez-Nieto G., Rojas F.R., García-Peña M., et al. A safe protocol to identify low-risk patients with COVID-19 pneumonia for outpatient management. Intern Emerg Med. 2021:1–9. doi: 10.1007/s11739-021-02660-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Parra L.M., Cantero M., Morras I., Vallejo A., Diego I., Jimenez-Tejero E., et al. Hospital readmissions of discharged patients with COVID-19. International Journal of General Medicine. 2020;13:1359–1366. doi: 10.2147/ijgm.s275775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pawlowski C., Venkatakrishnan A., Ramudu E., Kirkup C., Puranik A., Kayal N., et al. Pre-existing conditions are associated with COVID-19 patients’ hospitalization, despite confirmed clearance of SARS-CoV-2 virus. EClinicalMedicine. 2021;34 doi: 10.1016/j.eclinm.2021.100793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Saab F.G., Chiang J.N., Brook R., Adamson P.C., Fulcher J.A., Halperin E., et al. Discharge clinical characteristics and post-discharge events in patients with severe COVID-19: a descriptive case series. J Gen Intern Med. 2021;36(4):1017–1022. doi: 10.1007/s11606-020-06494-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Samuels S., Niu J., Sareli C., Eckardt P. The epidemiology and predictors of outcomes among confirmed COVID-19 cases in a large community healthcare system in South Florida. J Community Health. 2021;1-10 doi: 10.1007/s10900-020-00957-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Somani S.S., Richter F., Fuster V., De Freitas J.K., Naik N., Sigel K., et al. Characterization of patients who return to hospital following discharge from hospitalization for COVID-19. J Gen Intern Med. 2020;35(10):2838–2844. doi: 10.1007/s11606-020-06120-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yang C., Jiang M., Wang X., Tang X., Fang S., Li H., et al. Viral RNA level, serum antibody responses, and transmission risk in recovered COVID-19 patients with recurrent positive SARS-CoV-2 RNA test results: a population-based observational cohort study. Emerging microbes & infections. 2020;9(1):2368–2378. doi: 10.1080/22221751.2020.1837018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ye S.Q., Hiura G., Fleck E., Garcia A., Geleris J., Lee P., et al. Hospital readmissions after implementation of a discharge care program for patients with COVID-19 illness. J Gen Intern Med. 2021;36(3):722–729. doi: 10.1007/s11606-020-06340-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ye X., Yuan Y., Huang R., Cheng A., Yu Z., Huang Z., et al. Clinical characteristics of patients with re-admitted of novel coronavirus 2019 (nCOVID-19) in Wenzhou. China Frontiers in Public Health. 2021;9:476. doi: 10.3389/fpubh.2021.649178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gil M.R., Gonzalez-Lugo J.D., Rahman S., Barouqa M., Szymanski J., Ikemura K., et al. Correlation of coagulation parameters with clinical outcomes during the Coronavirus-19 surge in New York: observational cohort. Front Physiol. 2021;12 doi: 10.3389/fphys.2021.618929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.García-Abellán J., Padilla S., Fernández-González M., García J.A., Agulló V., Andreo M., et al. Antibody response to SARS-CoV-2 is associated with long-term clinical outcome in patients with COVID-19: a longitudinal study. J Clin Immunol. 2021;41(7):1490–1501. doi: 10.1007/s10875-021-01083-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Clark J.R., Batra A., Shlobin N.A., Hoffman S.C., Orban Z.S., Koralnik I.J., et al. Acute-care hospital reencounters in COVID-19 patients. GeroScience. 2021:1–13. doi: 10.1007/s11357-021-00378-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Leijte W.T., Wagemaker N.M., van Kraaij T.D., de Kruif M.D., Mostard G.J., Leers M.P., et al. Mortality and re-admission after hospitalization with COVID-19. Ned Tijdschr Geneeskd. 2020;164 [PubMed] [Google Scholar]
- 53.Drewett G.P., Chan R.K., Jones N., Wimaleswaran H., Howard M.E., McDonald C.F., et al. Risk factors for readmission following inpatient management of COVID-19 in a low-prevalence setting. Intern Med J. 2021;51(5):821–823. doi: 10.1111/imj.15218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Uyaroğlu O.A., BaŞaran N.Ç., Özişik L., Dizman G.T., Eroğlu İ., Şahin T.K., et al. Thirty-day readmission rate of COVID-19 patients discharged from a tertiary care university hospital in Turkey: an observational, single-center study. International J Qual Health Care. 2021;33(1):mzaa144. doi: 10.1093/intqhc/mzaa144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Peckham H., de Gruijter N.M., Raine C., Radziszewska A., Ciurtin C., Wedderburn L.R., et al. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat Commun. 2020;11(1):6317. doi: 10.1038/s41467-020-19741-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Subramaniam A., Lim Z.J., Ponnapa Reddy M., Shekar K. A systematic review and meta-analysis of the characteristics and outcomes of readmitted COVID-19 survivors. Intern Med J. 2021;51(11):1773–1780. doi: 10.1111/imj.15350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gao Yd, Ding M., Dong X., Jj Zhang, Kursat Azkur A., Azkur D., et al. Risk factors for severe and critically ill COVID-19 patients: a review. Allergy. 2021;76(2):428–455. doi: 10.1111/all.14657. [DOI] [PubMed] [Google Scholar]
- 58.Monreal E., Sdl Maza S., Gullón P., Natera-Villalba E., Chico-García J.L., Beltrán-Corbellini Á., et al. Non-severe immunosuppression might be associated with a lower risk of moderate–severe acute respiratory distress syndrome in COVID-19: a pilot study. J Med Virol. 2021;93(4):2243–2251. doi: 10.1002/jmv.26656. [DOI] [PubMed] [Google Scholar]
- 59.Suresh S., Siddiqui M., Abu Ghanimeh M., Jou J., Simmer S., Mendiratta V., et al. Association of obesity with illness severity in hospitalized patients with COVID-19: a retrospective cohort study. Obes Res Clin Pract. 2021;15(2):172–176. doi: 10.1016/j.orcp.2021.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yin T., Li Y., Ying Y., Luo Z. Prevalence of comorbidity in Chinese patients with COVID-19: systematic review and meta-analysis of risk factors. BMC Infect Dis. 2021;21(1):200. doi: 10.1186/s12879-021-05915-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.D’Ascanio M., Innammorato M., Pasquariello L., Pizzirusso D., Guerrieri G., Castelli S., et al. Age is not the only risk factor in COVID-19: the role of comorbidities and of long staying in residential care homes. BMC Geriatr. 2021;21(1):63. doi: 10.1186/s12877-021-02013-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gottlieb M., Sansom S., Frankenberger C., Ward E., Hota B. Clinical course and factors associated with hospitalization and critical illness among COVID-19 patients in Chicago. Illinois Academic Emergency Medicine. 2020;27(10):963–973. doi: 10.1111/acem.14104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Li J., Huang D.Q., Zou B., Yang H., Hui W.Z., Rui F., et al. Epidemiology of COVID-19: a systematic review and meta-analysis of clinical characteristics, risk factors, and outcomes. J Med Virol. 2021;93(3):1449–1458. doi: 10.1002/jmv.26424. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Forrest and funnel plots of meta-analyzed variables.
Search Strategy.
(A) Quality assessment table for cohort studies based on JBI Critical Appraisal.
Demographic and inpatient characteristics of readmitted and non-readmitted patients.
Distribution of comorbidities among readmitted and non-readmitted patients.
Causes of readmissions among COVID-19 patients.
Data Availability Statement
The data that support the findings of this study are provided in the supplementary files and are available from the corresponding author on request.