Abstract
Public outrage regarding physician shortages during the past two decades have led to policies aimed at significantly increasing physician supply, yet access remains elusive. In this paper, we examine this puzzling trend and the causes underlying it by analyzing physician supply, compensation and productivity and the reasons behind productivity decline. We hypothesize that excess physician compensation beyond a target income induces productivity decline. In contrast to a wage–productivity gap for the average Canadian worker (where productivity has increased but compensation has not kept pace), physicians are experiencing a “reverse wage–productivity gap” whereby compensation is increasing but productivity is decreasing, resulting in more physicians, higher compensation and fewer services. We conclude by discussing potential policy options to address how best to provide timely access to medical care for Canadians while keeping physician healthcare expenditures at sustainable levels.
Abstract
L'indignation de la population concernant les pénuries de médecins au cours des vingt dernières années a mené à des politiques qui visent à augmenter considérablement l'offre de médecins, mais l'accès reste difficile à atteindre. Dans cet article, nous examinons cette tendance déroutante et les causes qui la sous-tendent en analysant l'offre, la rémunération et la productivité des médecins ainsi que les raisons de la baisse de la productivité. Nous émettons l'hypothèse qu'une rémunération excessive des médecins au-delà d'un revenu cible induit une baisse de la productivité. Contrairement à un écart salaire–productivité pour le travailleur canadien moyen (où la productivité a augmenté mais la rémunération n'a pas suivi le rythme), les médecins connaissent un « écart salaire–productivité inversé » où la rémunération augmente mais la productivité diminue, ce qui entraîne un plus grand nombre de médecins, une rémunération plus élevée et moins de services. Nous concluons en discutant des options politiques permettant de déterminer la meilleure façon de fournir un accès rapide aux soins médicaux pour les Canadiens tout en maintenant les dépenses de santé des médecins à des niveaux durables.
Introduction
Physicians play an integral role in the Canadian healthcare system; however, consensus about the optimum ratio of physicians to population continues to be debated. During the past two decades, the public has expressed concerns about the availability of physicians, and physician supply has been significantly increased in response (Chan 2002b; CIHI 2020a). Notwithstanding these efforts, access remains a problem for many patients (Brend 2017; Martin et al. 2018). Previous authors have reported reduced physician productivity over short time frames (Ariste 2015), with older data (Chan 2002a) or by examining specific factors impacting productivity, such as sex (Weizblit et al. 2009) or intergenerational differences (Watson et al. 2006). Our objective was to examine recent trends of physician supply, compensation and productivity in Canada, the reasons for these trends and how their relationships may affect physician availability and policies for managing physician supply and demand. We hypothesize that excess physician compensation beyond a target income induces productivity decline (induced productivity decline hypothesis).
Physician supply in Canada
Physician supply in Canada has fluctuated over time. In the 1980s and early 1990s, there was a perceived surplus of physicians (Barer et al. 1991; Chan 2002b), leading to policies to restrict physician supply in the 1990s (Barer et al. 1991; Malko and Huckfeldt 2017). Within a decade, public outcries regarding poor access to physicians and long wait times led provincial governments to reverse course and significantly boost physician supply through increased medical school enrollment and recruitment and retention strategies for foreign medical graduates (Malko and Huckfeldt 2017), especially in underserved areas. The increase in supply has led to the highest ratio of physicians per capita ever recorded in Canada (2.41 physicians/1,000 population in 2019 [CIHI 2020a]), with a growth rate more than double that of the Canadian population over the last five years (see Figure 1), and especially high in urban settings (CIHI 2020b). Yet Canadians continue to express concerns about obtaining timely medical care, particularly from family physicians (FPs) (Brend 2017; The Canadian Press 2019). In international rankings, Canada and Norway rank the lowest for same- or next-day appointments with a doctor or nurse (Schneider et al. 2017). To address these concerns, it is critical to understand why the increase in physician supply has failed to meet the public's medical care needs.
Figure 1.
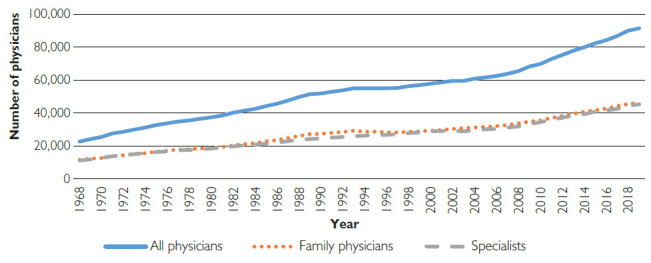
Physician supply (1968–2019)
International comparisons of physician supply
The ideal physician-to-population ratio in developed countries has been difficult to define. For example, physician-to-population ratios in Canada remain low compared with other developed nations. According to Organisation for Economic Co-operation and Development (OECD) data in 2016, Canada ranked 24th of 31 countries (2.6/1,000 population vs. an average of 3.4/1,000) in physician-to-population ratio, including medical interns and residents. Interestingly, however, the FP-to-population ratio in Canada is higher than the OECD average (1.3/1,000 vs. an average of 1.0/1,000, ranking Canada eighth), whereas the specialist ratios are lower (1.4/1,000 vs. an average of 2.2/1,000, ranking Canada 28th) (OECD 2020a). This may derive, at least in part, from Canada's deliberate policy to have FPs act as “gatekeepers” to the healthcare system and to use specialists mainly as consultants rather than primary care providers. Regardless of whether this is an appropriate policy, the physician-to-population ratio in Canada has never been higher, and the number of FPs per capita is higher than in most OECD nations. Although many health systems in developed countries are similar to Canada's, they may differ in the way they are funded, which may impact health system outcomes differently.
Physician productivity
Productivity is key to the labour market, and physicians are no exception. For the purposes of this paper, physician productivity is defined as the number of patient services provided per physician per annum. In Canada, different fee for service (FFS) models, alternate payment plans (APPs) and salary and blended arrangements exist within and among provinces. Ariste (2015) reported that in the FFS model, the volume of services per physician decreased at an average annual rate of 0.6% from 2004 to 2010, indicating that physician productivity had fallen.
Data and Methods
We used data from the Canadian Institute for Health Information's (CIHI) National Physician Database from 1996 to 2019, which include data sets with both FFS and APP payments. However, the data sets include FFS-based services (defined as billable services under the FFS fee code) but not APP services, which have accounted for 20% to 28% of physician payments since 2004 (CIHI 2020a). Physicians were separated into two groups: FPs and specialists (including surgical and non-surgical). To estimate the average and total number of services per 100,000 population and per physician by year, we used Ariste's (2015) method of “same-fee assumption” to estimate the service volume for physicians receiving APP; this is achieved by deflating APP compensation by average FFS fees for physicians in the same specialty. To examine potential reasons for changing productivity, we examined data from the Canadian Medical Association's (CMA) National Physician Health Survey, which published the weekly working hours of physicians from 1998 to 2019 – grouped by sex, age group and specialty – and categorized the work according to direct and indirect (e.g., health committees, managing practice, indirect patient care, research, administration, teaching, continuing medical education and others) patient care activities. We compared the trends of physician payments (total and average per physician) with inflation and the gross domestic product (GDP) in Canada over time and with the median real hourly earnings growth for the average Canadian worker, as well as international physician expenditures.
Results
Reduced productivity
Physician Services Provided Per Capita
Our results show that the number of physician services provided per capita (FFS and APP) has fallen by 5% despite a 7% growth in the number of physicians per capita during the past five years, from 2014 to 2019 (Figure 2) (CIHI 2020c). The decline in total number of services provided was the greatest among FPs at 9% compared to an increase of 1% for specialists during the same five years. The pattern was similar over a 10-year period from 2008 to 2018, with the number of physician services per capita falling by 4%, while the number of physicians grew by 37%.
Figure 2.
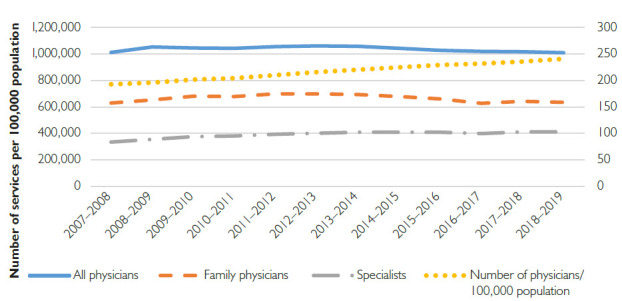
Number of services versus number of physicians per 100,000 population
Physician Services Provided Per Physician
Between 2013 and 2018, the number of services provided per physician (FFS and APP) decreased by 13%, with the decrease being greater among FPs (–16%) compared to specialists (–8%). Similarly, over the 10-year period between 2008 and 2018, the number of services provided per physician decreased by 23%, with the decrease greater among FPs (–21%) than among specialists (–4%) (Appendix 1: Figure A1, available online here).
Reasons for reduced productivity
Working Hours
Survey data from CMA's National Physician Health Survey from 1998 to 2019 (Figure 3) show that the total weekly working hours for physicians have declined by an average of 9% over the past 21 years (from 51.3 to 46.8 hours/week) (CMA n.d.).
Figure 3.
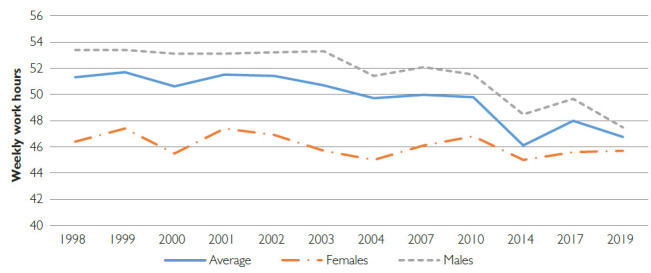
Weekly work hours
Sex-Based Comparisons
Male physicians report working longer hours than female physicians. Since 1998, there has been an overall decline in the number of weekly hours worked by both male and female physicians; however, the decline has been greater for men (11% vs. 2%) than women (Figure 3).
Age
In 1998, the average number of hours worked by physicians increased with age until 65 years, after which it decreased. This pattern has since changed. Physicians of all age groups report reduced working hours (Appendix 1: Figure A2, available online here); however, the decline has been greater as age increased until the age of 65 years (in comparison to 1998, the age groups in 2019 reported a decline in working hours of 1% for <35 years, 8% for 35–54 years, 12% for 55–64 years and 5% for 65+ years).
Category of work activity
Table 1 shows categories of physician activity as published by CMA's National Physician Health Survey. Between 1998 and 2019, all categories of physician activity, except indirect patient care, decreased between 10% and 51%. Most significantly, direct patient care hours decreased by 12%, or 4.5 hours per physician per week, while indirect patient care hours increased by 61%, or 2.8 hours per physician per week.
Table 1.
Growth rate of weekly work hours by category (from 1998 to 2019)
| Work activity | Growth rate (%) |
|---|---|
| Direct patient care | −12 |
| Direct patient care without a teaching component* | −12 |
| Direct patient care with a teaching component* | 21 |
| Health committees | −27 |
| Managing your practice | −28 |
| Indirect patient care | 61 |
| Research | −21 |
| Administration | −42 |
| Teaching | −10 |
| Continuing medical education | −18 |
| Other | −51 |
Data for direct patient care with or without a teaching component are only available from 2004 to 2019.
FPs versus Specialists
Specialists consistently work more hours than FPs; however, both groups have reduced their working hours since 1998 by approximately 8% and 9%, respectively. In 2019, FPs reported working 46 hours/week compared to specialists who reported working 49 hours/week.
Physician compensation: International comparison
In a recent study of healthcare spending in 10 high-income countries, Papanicolas et al. (2018) reported that Canadian physicians are well compensated compared to other countries. Not including the US, FPs in Canada earn more than FPs in any other country except for Germany, while specialists rank only behind those in Australia and the Netherlands (Appendix 1: Figure A3, available online here). In addition, among the 31 OECD countries, Canada has some of the highest ratios of physician-to-average–worker income at a ratio of 3.1 for FPs – second only to Germany and on par with the UK – and 4.9 for specialists, on par with France and higher than all other countries apart from Belgium, Chile, Luxembourg and Germany (OECD 2019). The US was not included in the OECD analysis as physician compensation data were unavailable.
Physician compensation growth in Canada
CIHI data from 2019 show that the three largest health expenditure categories since 1975 have been hospitals (27%), physician payments (15%) and drugs (15%) (CIHI 2019). Physician expenditure growth rates have consistently exceeded both inflation (adjusted for population growth) and GDP growth rates, except for a short period in the early 1990s (Figure 4). Between 1999 and 2018, the average gross FFS-based physician income for those earning above $60,000 increased from $210,812 to $332,233 at an average annual rate of 3.0% compared to the average annual inflation rate of 1.7% (CIHI 2019). Physician expenditure per capita increased by an average of 8% per annum from $408 in 1999 to $1,064 in 2019 (CIHI 2019).
Figure 4.
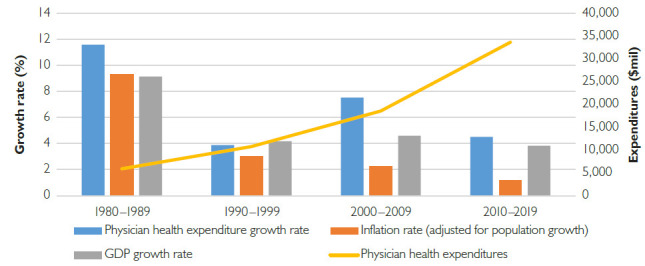
Physician health expenditure versus inflation and GDP growth rates
Discussion
Our results show that after a brief slowdown in the early 1990s, physician supply has increased significantly, growing by 63% between 1998 and 2019, and more recently by 37% between 2008 and 2018, resulting in the highest physician–population ratio in Canadian history with 241 physicians/100,000 population by 2019. However, the expected increase in physician service provision has been offset by a dramatic decrease in physician productivity (or services provided) by 23% per physician between 2008 and 2018. The result has been a net increase in total physician services of only 0.2% per annum from 2013 to 2018. With Canada's population growing at just over 1% per annum, this translates into a net decrease of 5% in services per capita between 2013 and 2018. Our results support the “induced productivity decline hypothesis,” whereby excess physician compensation beyond a target income induces productivity decline. It is a small wonder that public complaints about long wait times and difficulties with access to physicians have not abated (Brend 2017; Martin et al. 2018).
From the physician survey, we were able to discern the following, albeit an incomplete, picture. The reduction in physician services provided appears to be due to both decreased average physician work hours and changes in the types of work performed. Average physician work hours decreased by 9% or over 4.6 hours/week/physician between 1998 and 2019. The impact on service provision is further compounded by a decrease in direct patient care activities of 12% (or 4.5 hours/week/physician) between 1998 and 2019. In contrast, indirect patient care activities increased by 61% (from 4.5 to 7.3 hours/week/physician). The CMA defines indirect patient care activities as “reports, charting, patient or family phone calls” (CMA 2019b). Several advances in medical practice, such as electronic medical records, may improve documentation; however, they almost universally decrease productivity (Howley et al. 2015). Moreover, as the population ages and comorbidities increase, the patients' needs become more complex and require more time (CIHI 2011a; Pereles and Russell 1996).
The significant increase in indirect patient care activities merits further research to better understand why physician activities are changing, what value they provide to patients and how they are being compensated. Crossley et al. (2009) reported that increasing hours of direct patient care by 5% among currently practising physicians would have a greater impact on effective physician supply than large increases in Canadian medical school enrolments. We also observed that between 2008 and 2018, the number of services provided per physician decreased by 21% for FPs and 4% for specialists. It is unclear why the decrease has been especially marked for FPs. It is possible that this may reflect the changing roles and scope of practice of FPs and specialists as medical technologies advance. Chan (2002a) and a CIHI study reported that FP service provision has become less comprehensive (Tepper 2004); that is, FPs are referring more to specialists for services that they would have performed themselves in the past. Sarma et al. (2018) reported that capitation models (APP) among FPs lead to more specialist referrals. The shift to virtual care in primary care practice during the COVID-19 pandemic on productivity will also need to be monitored once the pandemic is controlled (Glazier et al. 2021).
The reasons for decreased physician productivity are multifactorial and require further research. A major factor underlying decreased work hours may be a shift in attitudes of physicians toward a better work–life balance with reduced working hours and an increased focus on earlier retirement (Malko and Huckfeldt 2017; Weizblit et al. 2009). This is particularly relevant among female physicians, who work fewer hours and take more personal leaves (Weizblit et al. 2009). It is also pertinent in the context of the increasing female enrollment in medical schools, where the male–female ratio has shifted dramatically from 60:40 in the 1980s (Burton and Wong 2004) to 44:56 in 2018 (CMA 2019a). However, male physicians have recently also reduced their working hours to approximate their female colleagues more closely, narrowing the gap from seven hours in 1998 to two hours in 2019. Another important change is the reduction in working hours of older physicians, who traditionally worked more hours than younger physicians. This has since reversed and may be attributable at least in part to the attitudes of a younger generation as they age in the workforce. A greater supply of alternative providers, the development of group practices and the evolution of practice networks have also likely decreased the need for many physicians to work longer hours.
Our finding of rising physician compensation even while physician hours and productivity have decreased is paradoxical. In a comprehensive study of physician compensation, Grant and Hurley (2013) reported that between 2001 and 2010, the average gross income of physicians increased at their fastest rate since the introduction of medicare – rising by 33% from $187,134 to $248,113 (Grant and Hurley 2013). Data from CIHI show that this has since increased to $332,233 in 2018, indicating that gross FFS-based physician income has grown at a faster rate than inflation over the past 19 years (average of 3.0% vs 1.7% per annum) (CIHI 2020c), which is unsustainable when healthcare costs consume an ever-increasing proportion of the GDP. Buys et al. (2019) reported that younger cohorts of physicians received higher annual gross incomes compared to older cohorts at the same age, despite seeing similar or fewer numbers of patients. A study by CIHI (2011b) also reported that growth in physician fees is a major driver that accounts for over half (53%) of physician expenditure increases. At the same time, Ariste (2015) reported that services per physician in Canada decreased by 0.6% annually between 2004 and 2010, and we found that the number of services provided per physician on FFS decreased by 23% between 2008 and 2018, with a greater decrease occurring among FPs (–21%).
Some provinces have tried to reform primary care by trialling variants of the APP model using salaried, capitated or blended capitation variants, in part, to see whether these interventions improved care and cost efficiency compared to the FFS model. In Alberta, primary care networks (PCNs) were established in 2005, with physicians receiving either FFS-based or capitated payments (Peckham et al. 2018), and have been shown to lead to decreased emergency department visits and hospital stays (McAlister et al. 2018), as well as better management of chronic diseases (Manns et al. 2011). However, several reviews of PCNs found an inconsistency in financial management and accountability (Peckham et al. 2018), and it is unclear whether there is a relationship between outcomes and FFS-based or capitation funding models. In Ontario, FFS-based physicians had higher productivity than APP-based physicians (Sarma et al. 2010), but through longer working hours and more time spent on direct patient care (Laberge et al. 2016), that is, financial incentives increased productivity. Marchildon and Hutchison (2016) reported that team-based capitation models provided better preventive care and chronic care management, although patient-reported outcomes were unchanged. Laberge et al. (2017) reported that enhanced FFS models using physician-based teams had the lowest primary care and total healthcare costs, whereas blended capitation models using multidisciplinary or physician-based teams were associated with higher primary care costs but lower total healthcare costs than FFS models. However, the annual report of the Office of the Auditor General of Ontario (2016) found that the patient enrolment model is more expensive than the FFS model, and the Ontario Ministry of Health and Long-Term Care could not demonstrate whether the new models improved patient access, quality of care or cost-effectiveness. Thus, primary care costs have increased with the reforms, although this may be offset by lower total healthcare costs per patient (Laberge et al. 2017). To date, various attempts to reform primary care have not led to significant changes in total physician expenditures.
In a recent study, Uguccioni (2016) described a “wage–productivity gap” in which median real hourly earnings grew by only 0.09% per annum for the average Canadian worker between 1976 and 2014, while productivity grew by 1.12%. The situation is reversed for physicians in Canada, where average gross FFS-based income increased by 20%, while productivity decreased by 23% between 2008 and 2018; that is, the price per service has increased significantly. This “reverse wage–productivity gap” lies at the heart of the failure to increase physician services through increasing physician supply and compensation. It is possible that the “induced productivity decline hypothesis” is at play, with physicians reducing services when compensation exceeds their income targets. It is also possible that governments are politically ill-equipped to deal with the monopoly power of physicians to set fee increases, and alternate strategies are needed to control physician expenditures. Physicians have a right to work less, but compensation should be based on a combination of productivity, quality of care and outcomes. Rising physician compensation also contributes to the increasing income inequality between the top 1% of earners and the average Canadian worker (Marchildon and Di Matteo 2014) and must be addressed by policy makers to ensure sustainability of the public healthcare system.
Finally, Canadian physicians are well compensated compared to physicians from other developed countries. Canadian physicians are among the best compensated in the OECD countries with reported data, with an average gross FP income of $163,000 (US$, Purchasing Power Parity [PPP]) (versus an OECD average of $127,000) and an average gross specialist income of $257,000 (US$, PPP) (versus an OECD average of $231,000) for self-employed physicians in 2016 (OECD 2020b). Canadian physicians also have one of the highest ratios of physician-to-average–worker incomes at 3.1 for FPs and 4.9 for specialists, ranking Canada second and fifth highest, respectively, among 31 OECD countries (OECD 2019). In addition, physician expenditure growth rates have consistently exceeded inflation and GDP growth rates, which is financially unsustainable for the publicly funded healthcare system. To improve availability of physician services, it is imperative that governments understand the implications of the “induced productivity decline hypothesis” and address the physician “reverse wage–productivity gap” rather than rely on the current strategy of increasing both physician supply and compensation because it is not yielding the intended benefits and is financially unsustainable.
Policy Options
Having examined physician supply, productivity and physician availability, we now discuss policies for managing physician supply and demand. Our analysis highlights the importance of simultaneously addressing the twin problems of physician compensation increase and productivity decline. As previous research has demonstrated that systems with higher rates of private financing are negatively associated with universality, equity, accessibility and quality of care (Lee et al. 2021), private financing of healthcare is not a solution. Physician expenditure increases should be constrained by principle-based criteria (e.g., no more than either the rate of inflation or GDP growth). Physician compensation should be linked to productivity and important patient-centred outcomes such as evidence-based care and health outcomes. Healthcare processes such as documentation and referrals should be automated and streamlined to improve productivity, and reimbursement for indirect patient care services should be based on value to patients. Physician productivity may be increased by greater use of extenders such as physician assistants. In the case of primary care, alternate care providers, such as nurse practitioners and pharmacists, should be licensed and funded to practise independently. Primary care teams may improve care and reduce total health costs but their relationship with funding models is unclear and should be monitored and adjusted. Primary care fund-holding organizations based on geography could be employed to improve efficiency and distribution of physicians (Price et al. 2015).
Limitations
There are a number of limitations to our study. As APPs comprise 20% to 28% of physician expenditures, using “same fee assumptions” based on FFS service levels may be inaccurate. The data analyzed from the CIHI National Physician Database do not include anaesthesia, laboratory and imaging specialists, and services/capita calculations do not include data from Alberta or the Territories, which may bias the results. Overhead costs of physicians were not available. Physician productivity measures are impacted by the value and mix of services provided, which change over time. Because the dollar value assigned to each service is determined through a bargaining process between the government funders and the medical associations at the provincial level, it may not reflect the true value that patients place on the services. Patient complexity is not measured in any of these databases, which varies widely by practice and location. Response rates for the CMA National Physician Health Surveys averaged 40% of a random sampling of 8,000 physicians across the country from 1998 to 2004 and 20% of all physicians between 2004 and 2019 and may not be generalizable to all physicians.
Conclusion
Although physician supply in Canada has increased significantly in recent decades, physician productivity has decreased, resulting in a net reduction of physician services per capita. At the same time, physician compensation has increased, resulting in a “reverse wage–productivity gap” of more physicians, higher compensation and fewer services, which supports the “induced productivity decline hypothesis.” The current physician supply and compensation strategies do not improve physician availability, are not patient-focused, are not financially sustainable and need to be addressed comprehensively at a policy level.
Contributor Information
Shoo K. Lee, Professor of Paediatrics, Obstetrics & Gynecology, and Public Health, University of Toronto; Director, Maternal-Infant Care Research Centre, Mount Sinai Hospital, Toronto, ON.
Sukhy K. Mahl, Assistant Director, Maternal-Infant Care Research Centre, Mount Sinai Hospital, Toronto, ON.
Brian H. Rowe, Professor, Department of Emergency Medicine and School of Public Health, University of Alberta, Edmonton, AB.
Funding Statement
Although no specific funding has been received for this study, organizational support was provided by the Maternal-Infant Care Research Centre (MiCare) at Mount Sinai Hospital in Toronto, ON. MiCare is supported by a Canadian Institutes of Health Research (CIHR) Team Grant (CTP 87518) and the Ontario Ministry of Health. Brian Rowe's research is supported by a Scientific Directors Operating Grant (SOP 168483) from CIHR. The funding agencies had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; and decision to submit the manuscript for publication.
References
- Ariste R. 2015. Fee-Schedule Increases in Canada: Implication for Service Volumes among Family and Specialist Physicians. Journal of Health and Human Services Administration 38(3): 381–407. [PubMed] [Google Scholar]
- Barer M.L., Stoddart G.L.; Centre for Health Economics Policy Analysis; Conference of Deputy Ministers of Health (Canada). 1991. Toward Integrated Medical Resource Policies for Canada. CHEPA Working Paper Series No. 91–7, 91–8. Centre for Health Economics and Policy Analysis. Retrieved April 20, 2020. <http://hdl.handle.net/11375/17057>. [Google Scholar]
- Brend Y. 2017, May 4. We're Graduating More Doctors than Ever, so Why Is It So Hard to Find a GP? CBC News. Retrieved July 5, 2020. <https://www.cbc.ca/news/canada/british-columbia/bc-doctor-shortage-medical-fees-1.4100251>.
- Burton K.R., Wong I.K. 2004. A Force to Contend with: The Gender Gap Closes in Canadian Medical Schools. CMAJ 170(9): 1385–86. doi:10.1503/cmaj.1040354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buys Y.M., Canizares M., Felfeli T., Jin Y.. 2019. Influence of Age, Sex, and Generation on Physician Payments and Clinical Activity in Ontario, Canada: An Age-Period-Cohort Analysis. American Journal of Ophthalmology 197: 23–35. doi:10.1016/j.ajo.2018.09.003. [DOI] [PubMed] [Google Scholar]
- Canadian Institute for Health Information (CIHI). 2011a, January. Seniors and the Health Care System: What Is the Impact of Multiple Chronic Conditions? Retrieved January 19, 2021. <https://secure.cihi.ca/free_products/air-chronic_disease_aib_en.pdf>.
- Canadian Institute for Health Information (CIHI). 2011b, October. Health Care Cost Drivers: The Facts. Retrieved June 29, 2020. <https://secure.cihi.ca/free_products/health_care_cost_drivers_the_facts_en.pdf>.
- Canadian Institute for Health Information (CIHI). 2019. National Health Expenditure Trends, 1975 to 2019. Retrieved April 20, 2020. <https://www.cihi.ca/sites/default/files/document/nhex-trends-narrative-report-2019-en-web.pdf>.
- Canadian Institute of Health Information (CIHI). 2020a. Physicians in Canada, 2019. Retrieved December 3, 2020. <https://www.cihi.ca/sites/default/files/document/physicians-in-canada-report-en.pdf>.
- Canadian Institute for Health Information (CIHI). 2020b. Scott's Medical Database Metadata: SMDB data table release (ZIP). Retrieved February 10, 2021. <https://www.cihi.ca/en/scotts-medical-database-metadata>.
- Canadian Institute for Health Information (CIHI). 2020c. National Physician Database Historical Payments – Data Tables: Annual Report and NPDB Data Table Release. Retrieved December 2, 2020. <https://www.cihi.ca/en/national-physician-database-metadata>.
- Canadian Medical Association (CMA). n.d. Physician Perspectives: Workforce Surveys. Retrieved August 11, 2020. <https://www.cma.ca/physician-perspectives-workforce-surveys>.
- Canadian Medical Association (CMA). 2019a. Quick Facts on Canada's Physicians. Retrieved August 7, 2020. <https://www.cma.ca/quick-facts-canadas-physicians>.
- Canadian Medical Association (CMA). 2019b. CMA Physician Workforce Survey. Retrieved October 14, 2021. <https://www.cma.ca/sites/default/files/pdf/Survey/Questionnaire-2019%20CMA_Physician_Workforce_Survey-e.pdf>.
- The Canadian Press. 2019, September 26. Number of Doctors per Capita in Canada Reaches Record High. CBC News. Retrieved July 20, 2020. <https://www.cbc.ca/news/health/doctor-supply-cihi-1.5298005>.
- Chan B.T.B. 2002a. The Declining Comprehensiveness of Primary Care. CMAJ 166(4): 429–34. [PMC free article] [PubMed] [Google Scholar]
- Chan B.T.B. 2002b, June. From Perceived Surplus to Perceived Shortage: What Happened to Canada's Physician Workforce in the 1990s? Canadian Institute for Health Information. Retrieved April 18, 2020. <https://secure.cihi.ca/free_products/chanjun02.pdf>. [Google Scholar]
- Crossley T.F., Hurley J., Jeon S.-H.. 2009. Physician Labour Supply in Canada: A Cohort Analysis. Health Economics 18(4): 437–56. doi:10.1002/hec.1378. [DOI] [PubMed] [Google Scholar]
- Glazier R.H., Green M.E., Wu F.C., Frymire E., Kopp A., Kiran T.. 2021. Shifts in Office and Virtual Primary Care during the Early COVID-19 Pandemic in Ontario, Canada. CMAJ 193(6): E200–E210. doi:10.1503/cmaj.202303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant H.M., Hurley J.. 2013. Unhealthy Pressure: How Physician Pay Demands Put the Squeeze on Provincial Health-Care Budgets. SPP Research Papers 6(22). University of Calgary. Retrieved November 3, 2019. <https://www.policyschool.ca/wp-content/uploads/2016/03/grant-physician-income.pdf>. [Google Scholar]
- Howley M.J., Chou E.Y., Hansen N., Dalrymple P.W.. 2015. The Long-Term Financial Impact of Electronic Health Record Implementation. Journal of the American Medical Informatics Association 22(2): 443–52. doi:10.1136/amiajnl-2014-002686. [DOI] [PubMed] [Google Scholar]
- Laberge M., Wodchis W.P., Barnsley J., Laporte A.. 2016. Efficiency of Ontario Primary Care Physicians across Payment Models: A Stochastic Frontier Analysis. Health Economics Review 6(1): 22. doi:10.1186/s13561-016-0101-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laberge M., Wodchis W.P., Barnsley J., Laporte A.. 2017. Costs of Health Care across Primary Care Models in Ontario. BMC Health Services Research 17: 511. doi:10.1186/s12913-017-2455-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.K., Rowe B.H., Mahl S.K.. 2021. Increased Private Healthcare for Canada: Is That the Right Solution? Healthcare Policy 16(3): 30–42. doi:10.12927/hcpol.2021.26435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malko A.V., Huckfeldt V.. 2017. Physician Shortage in Canada: A Review of Contributing Factors. Global Journal of Health Science 9(9): 68. doi:10.5539/gjhs.v9n9p68. [Google Scholar]
- Manns B.J., Tonelli M., Zhang J., Campbell D.J.T., Sargious P., Ayyalasomayajula B. et al. 2011. Enrolment in Primary Care Networks: Impact on Outcomes and Processes of Care for Patients with Diabetes. CMAJ 184(2): E144–E152. doi:10.1503/cmaj.110755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchildon G.P., Di Matteo L. (Eds). 2014. Bending the Cost Curve in Health Care: Canada's Provinces in International Perspective. University of Toronto Press. [Google Scholar]
- Marchildon G.P., Hutchison B.. 2016. Primary Care in Ontario, Canada: New Proposals after 15 Years of Reform. Health Policy 120(7): 732–38. doi:10.1016/j.healthpol.2016.04.010. [DOI] [PubMed] [Google Scholar]
- Martin D., Miller A.P., Quesnel-Vallée A., Caron N.R., Vissandjée B., Marchildon G.P.. 2018. Canada's Universal Health-Care System: Achieving Its Potential. The Lancet 391(10131): 1718–35. doi:10.1016/s0140-6736(18)30181-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAlister F.A., Bakal J.A., Green L., Bahler B., Lewanczuk R.. 2018. The Effect of Provider Affiliation with a Primary Care Network on Emergency Department Visits and Hospital Admissions. CMAJ 190(10): E276–84. doi:10.1503/cmaj.170385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of the Auditor General of Ontario. 2016. Annual Report, 2016. Retrieved February 15, 2021. <https://www.auditor.on.ca/en/content/annualreports/arreports/en16/2016AR_v1_en_web.pdf>.
- Organisation for Economic Co-operation and Development (OECD). 2019. Health at a Glance 2019: OECD Indicators. OECD Publishing. doi:10.1787/4dd50c09-en. [Google Scholar]
- Organisation for Economic Co-operation and Development (OECD). 2020a. Health Care Resources. OECD.Stat. Retrieved April 2, 2020. <https://stats.oecd.org/Index.aspx?DataSetCode=HEALTH_REAC>.
- Organisation for Economic Co-operation and Development (OECD). 2020b. Health Care Resources: Remuneration of Health Professionals. OECD.Stat. Retrieved January 6, 2021. <https://stats.oecd.org/index.aspx?queryid=30025>. [Google Scholar]
- Papanicolas I., Woskie L.R, Jha A.K.. 2018. Health Care Spending in the United States and Other High-Income Countries. JAMA 319(10): 1024–39. doi:10.1001/jama.2018.1150. [DOI] [PubMed] [Google Scholar]
- Peckham A., Kreindler S., Church J., Chatwood S., Marchildon G.. 2018, April 25. Rapid Review 2: Primary Care Reforms in Ontario, Manitoba, Alberta, and the Northwest Territories. A Rapid Review Prepared for the Canadian Foundation for Healthcare Improvement. North American Observatory on Health Systems and Policies. Retrieved on February 14, 2021. <https://ihpme.utoronto.ca/wp-content/uploads/2018/09/NAO-Rapid-Review-2-_EN.pdf>.
- Pereles I., Russell M.L.. 1996. Needs for CME in Geriatrics. Part 2: Physician Priorities and Perceptions of Community Representatives. Canadian Family Physician Médecin de famille canadien 42: 632–40. [PMC free article] [PubMed] [Google Scholar]
- Price D., Baker E., Golden B., Hannam R.. 2015, May. Patient Care Groups: A New Model of Population Based Primary Health Care for Ontario: A Report on Behalf of the Primary Health Care Expert Advisory Committee. Retrieved January 16, 2021. <http://health.gov.on.ca/en/common/ministry/publications/reports/primary_care/primary_care_price_report.pdf>.
- Sarma S., Devlin R.A., Hogg W.. 2010. Physician's Production of Primary Care in Ontario, Canada. Health Economics 19(1): 14–30. doi:10.1002/hec.1447. [DOI] [PubMed] [Google Scholar]
- Sarma S., Mehta N., Devlin R.A, Kpelitse K.A, Li L.. 2018. Family Physician Remuneration Schemes and Specialist Referrals: Quasi-Experimental Evidence from Ontario, Canada. Health Economics 27(10): 1533–49. doi:10.1002/hec.3783. [DOI] [PubMed] [Google Scholar]
- Schneider E.C., Sarnak D.O., Squires D., Shah A., Doty M.M.. 2017, July. Mirror, Mirror 2017: International Comparison Reflects Flaws and Opportunities for Better U.S. Health Care. The Commonwealth Fund. Retrieved January 23, 2021. <https://collections.nlm.nih.gov/master/borndig/101712671/Schneider_mirror_mirror_2017.pdf>.
- Tepper J. 2004. The Evolving Role of Canada's Family Physicians, 1992–2001. Canadian Institute for Health Information. Retrieved January 6, 2021. <https://secure.cihi.ca/free_products/PhysiciansREPORT_eng.pdf>.
- Uguccioni J. 2016. Explaining the Gap between Productivity and Median Wage Growth in Canada, 1976–2014. International Productivity Monitor, Centre for the Study of Living Standards 31: 37–56. [Google Scholar]
- Watson E.D., Slade S., Buske L., Tepper J.. 2006. Intergenerational Differences in Workloads among Primary Care Physicians: A Ten-Year, Population-Based Study. Health Affairs 25(6): 1620–28. doi: 10.1377/hlthaff.25.6.1620. [DOI] [PubMed] [Google Scholar]
- Weizblit N., Noble J., Baerlocher M.O. 2009. The Feminisation of Canadian Medicine and Its Impact upon Doctor Productivity. Medical Education 43(5): 442–48. doi:10.1111/j.1365-2923.2009.03309.x. [DOI] [PubMed] [Google Scholar]


