Abstract
The COVID-19 pandemic has tested the resilience of health systems broadly and primary care (PC) specifically. This paper begins by distinguishing the technical and political aspects of resilience and then draws on a documentary analysis and qualitative interviews with health system and PC stakeholders to examine competing resilience-focused responses to the pandemic in Alberta, Canada. We describe the pre-existing linkages between the province's central service delivery agency and its independent PC clinics. Together, these central and independent elements make up Alberta's broader health system, with the focus of this paper being on PC's particular vision of how resilience ought to be achieved. We describe two specific, pandemic-affected areas of activity by showing how competing visions of resilience emerged in the central service delivery agency and independent PC responses as they met at the system's points of linkage. At the first point of linkage, we describe the centralized activation of an incident management system and the replies made by independent PC stakeholders. At the second point of linkage, we describe central efforts to disseminate infection prevention and control guidance to PC clinics and the improvisational efforts of staff at those independent clinics to operationalize the guidance and ensure continuity of operations. We identify gaps between the resilience visions of the central agency and independent PC, drawing broadly applicable policy lessons for improving responses in present and future public health emergencies. Finding ways to include PC in centralized resilience policy planning is a priority.
Abstract
La pandémie de COVID-19 a mis à l'épreuve la résilience des systèmes de santé en général et celle des soins de santé primaires (SSP) en particulier. Cet article commence par distinguer les aspects techniques et politiques de la résilience, puis s'appuie sur une analyse documentaire et des entretiens qualitatifs avec les intervenants du système de santé et des SSP pour examiner les réponses concurrentes axées sur la résilience en Alberta, au Canada. Nous décrivons les liens préexistants entre l'agence centrale de prestation de services de la province et les cliniques de SSP indépendantes. Ensemble, ces éléments centraux et indépendants constituent le vaste système de santé de l'Alberta; le présent document porte sur la vision particulière des SSP en matière d'atteinte de la résilience. Nous décrivons deux domaines d'activité touchés par la pandémie en montrant comment des visions concurrentes de la résilience ont émergé dans les points de liaison entre l'agence centrale de prestation de services et les SSP indépendants. Pour le premier point de liaison, nous décrivons l'activation centralisée d'un système de gestion des incidents et les réponses apportées par les intervenants en SSP indépendants. Pour le deuxième point de liaison, nous décrivons les efforts centraux visant à diffuser des conseils de prévention et de contrôle des infections aux cliniques de SSP ainsi que les efforts d'improvisation du personnel de ces cliniques indépendantes pour opérationnaliser les conseils et assurer la continuité des activités. Nous identifions l'écart entre la vision de l'agence centrale et celle des SSP indépendants, et nous tirons des leçons largement applicables pour améliorer la réponse aux urgences en matière de santé publique actuelles et à venir. Il est prioritaire de trouver des moyens d'inclure les SSP dans la planification centralisée des politiques en matière de résilience.
Introduction
The SARS-CoV-2 virus has been a severe and ongoing test of health system resilience worldwide (El Bcheraoui et al. 2020; Legido-Quigley et al. 2020; Yazdizadeh et al. 2020). As resilience has become a topic of interest in the health policy literature (Haldane et al. 2017; Turenne et al. 2019; Wiig et al. 2020), a range of definitions for the concept have been developed (Castleden et al. 2011). The variation in those definitions has led to it being described as a “boundary term” that exists at the crossroads between technical and political understandings (Blanchet et al. 2017). At the technical level, policy aimed at achieving resilience seeks to adapt or transform health system structures to avoid undesired risk (Leach et al. 2010). At the political level, resilience policy is always subject to debates about which risks are desirable and which ones are not. Although resilience is often described in technical terms as a health system's capacity to sustain its operations and continue delivering care in the face of various external events (Hanefeld et al. 2018), the political is never far away. It reveals itself when stakeholders inside systems or organizations debate the risks and in doing so define the external effect that they are experiencing as a disturbance or as an opportunity (Braithwaite et al. 2015).
Differentiating between disturbances and opportunities here is a fraught political exercise – one health system stakeholder's unwelcome disturbance of the status quo is another's long-sought opportunity for change. In this way, the search for resilience frequently stirs up “resistance” (Forest 2019) as the desirability of risk and change are debated and visions of resilience compete. Achieving resilience in healthcare, then, is not merely a matter of pursuing technical continuity in care delivery. It also involves the interplay of competing visions about how resilience ought to be achieved and contention over which elements of existing care delivery ought to be left undisturbed and which ought to be changed. This paper tracks two such competing visions as a provincial health system responded to COVID-19 and the pandemic tested primary care (PC) resilience. We illustrate how one centralized formal vision of resilience focused on treating PC as one of many services to be managed in response to the pandemic competed with a second vision intent on prioritizing PC operations and voice in broader decision making.
Drawing on documentary analysis and qualitative interviews – evidence gathered in Alberta between March and December 2020 – we first describe policy responses from the province's central health agency that targeted resilience in the face of COVID-19. Next we describe policy workarounds enacted by stakeholders from Alberta's independent PC environment who were similarly seeking to sustain operations and care delivery under pandemic conditions. From the interplay of these two competing visions of resilience, we draw out broadly applicable lessons for jurisdictions seeking to improve action and planning in future public health emergencies. In this sense, and with the resilience of health systems across Canada tested by the pandemic (Lin et al. 2020), we take Alberta's PC experience as an exemplar. Our case study focuses on competing visions of resilience at key points of linkage between the central service delivery system and independent PC.
Independent PC in Alberta's Health System
Alberta has the largest centralized healthcare system in Canada, with over 650 facilities across the province managed by a single health authority – Alberta Health Services (AHS) – delivering care in five geographically based “health zones.” Facilities in these zones deliver public health, acute, long-term and some urgent care, with the province's more than 1,180 PC clinics owned and operated by family doctors operating outside AHS control. While PC is a highly independent element of the province's health system, there are also significant links between it and the central health authority. Indeed, provincial policy specifically seeks greater integration and linkages between the central AHS and independent PC elements of the health system (Government of Alberta 2014). We briefly describe the activity at three key linkage points: finance, administrative and service provision. The analysis in our Findings section then focuses on the latter two, showing how the central service delivery agency and independent PC efforts to achieve resilience intertwined and competed at the administrative and service provision linkage points over the course of the pandemic.
Finance linkages
As in many other provinces, Alberta's Ministry of Health (MoH) finances PC directly, with the vast majority of PC physicians billing the government on a fee-for-service basis. In an MoH budget of $20.8 billion, these PC services account for 7.17% or $1.48 billion annually (Government of Alberta 2020a). Provincial finance of PC, then, is a key element of Alberta's broader health system, as it supports the ongoing operations of independent family doctors. Although AHS is the province's single health authority, PC physicians do not share a governance or accountability relationship with the organization. Rather, PC fee guides are established out of direct negotiations between the MoH and the provincial medical association.
Alberta's approval and adoption of virtual care billing codes (VCBCs) offers a specific example of resilience issues playing out at the finance point of linkage between the central agency and independent PC. The formal, pandemic-induced response by the MoH and medical association was to approve VCBCs that would sustain PC operations. However, the VCBCs they approved were unmodified from the time of their creation during the 2009 H1N1 pandemic, with the consequences that they permitted care exclusively for pandemic disease–related complaints and remunerated physicians at rates that were more than a decade old (Molnar 2020a). As such, the centrally generated codes were seen as unsupportive of resilience by the independent PC community, and a media campaign to have them adjusted emerged (Boothby 2020). Ultimately, and out of these competing central and independent visions of how to achieve resilience, the VCBCs were modified and enjoyed significant uptake with PC operations shifting toward virtual care delivery in Alberta, as elsewhere in Canada (Bhatia et al. 2021; Glazier et al. 2021) and in Europe (Rawaf et al. 2020).
Despite its financial and governance isolation from independent PC, AHS nonetheless undertakes a portfolio of PC-focused work. Along with operating the urgent and family care clinics (https://www.albertahealthservices.ca/), AHS maintains a pair of PC-focused divisions: one operating at an administrative linkage point and the other operating at a service provision linkage point.
Administrative linkages
The health authority's primary health care program (PHCP) relies on a staff of less than 100 to conduct its work while embedded in an organization that employs more than 110,000 workers and is focused on acute and long-term care. Within these constraints, the PHCP works at a provincial level to provide PC clinics with system-wide guidelines and to act as a bridge between personnel in the MoH and community-based PC (https://www.albertahealthservices.ca/).
Service provision linkages
AHS has created zone primary care (ZonePC) groups in each of the five health zones. As their name implies, the ZonePC groups focus on zonal issues, not provincial ones. Inside each health zone, there is a dyad of a zonal lead physician from “inside” the health authority and a counterpart physician from “outside” the health authority who works in community PC. The ZonePC dyads co-plan activities and service provision priorities with local primary care networks (PCNs), which are composed of independent family physician members and formed as joint ventures with AHS. The PCNs have developed into this form and governance structure over the past 18 years (Leslie et al. 2020b). They are financed through capitation payments made as grants by the MoH, which requires accountability from the PCNs on specific performance metrics (Auditor General of Alberta 2017). There are presently 41 PCNs operating in the five zones, each with its own priorities for service delivery and modes of operating within the broader governance structures.
In what follows, we describe moves by the central health system to ensure resilience by activating an incident management system (IMS) and creating infection prevention and control (IPC) guidance for PC. We also describe competing moves by independent PC stakeholders who were motivated by different visions of how best to achieve resilience. PC stakeholders' at both the administrative and service delivery linkage points between the system's elements worked around the IMS and created alternative paths to operationalize IPC guidance. Although both central and independent PC stakeholders shared a technical resilience goal, each brought a different political understanding of how to achieve that goal.
Materials and Methods
The data we present here are part of a larger qualitative study examining the communication and implementation of policy in Alberta's COVID-19 response (CIHR 2020). Our research approach focuses on understanding experiences and perspectives across the provincial health system during the pandemic (Leslie et al. 2020a). Myles Leslie (ML), Raad Fadaak (RF) and Nicole Pinto (NP) conducted semi-structured interviews (n = 85) of health system stakeholders across PC and the PCNs (n = 25) and AHS-PC (n = 12). An interview guide was developed by ML and iterated in the field over the course of the research. All interviews were digitally recorded and transcribed for analysis. Sampling for the analysis of PC resilience was purposive and guided by authorial discussions of relevance based on notes taken during interviews. From these discussions, we selected the subset of interviews (n = 37) focused on PC stakeholders' experiences of the IMS and rollout of IPC guidance.
Supported by the MAXQDA 2020 software (https://www.maxqda.com/), RF and NP used an inductive coding approach to render an interpretive description of PC resilience in the pandemic. ML, RF and NP analyzed the data iteratively – expanding, collapsing and merging themes to arrive at the final analysis. We present passages from the verbatim transcripts to support this analysis, attributing the responses to participant numbers 01 to 82.
An interpretive description approach allows for insights not just into areas of commonality but areas of disagreement among participants, with an eye on providing pragmatic suggestions to improve policies and outcomes (Mejdahl et al. 2018; Thorne et al. 1997, 2016; Yan et al. 2016; Young et al. 2012). We conducted iterative participant checks with stakeholders on the emerging interpretations presented here. This research obtained ethical approval from the Conjoint Health Research Ethics Board at the University of Calgary (REB20-0371). All participants provided written and verbal consent to participate.
Results
Incident management system
After Alberta identified its first COVID-19 case on March 5, 2020, the MoH and AHS responded by initiating a disaster management plan focused on streamlining communications and decision making to ensure the continued, effective operation of the health system. Part of this resilience response included the activation of an IMS that created a nested hierarchy of command and response on top of the existing administrative and service provisional relationships, roles and responsibilities described earlier (AHS 2019). This is to say, the pandemic-induced resilience policy generated at the centre of the health system saw the creation of new structures alongside and on top of the existing administrative and service provisional links between AHS and independent PC (Figure 1).
Figure 1.
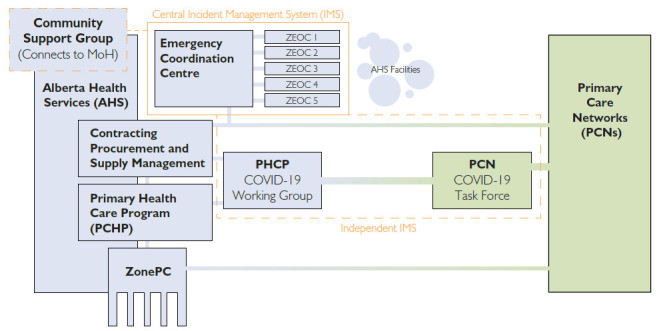
The central IMS response and independent PC replies to the COVID-19 pandemic in Alberta
MoH = Ministry of Health; ZEOC = Zone Emergency Operations Centre.
Inside AHS, an Emergency Coordination Centre (ECC) (AHS n.d.) was created at the provincial level along with Zone Emergency Operations Centres (ZEOCs) (AHS 2019) that implemented high-level pandemic decisions in the five regional health zones. Specifically, the IMS convened ZEOC meetings where personnel from AHS-ZonePC, but not the PCNs, were to be integrated into the pandemic response. After its activation, the IMS’ primary point of contact between the ECC and PC was the ZEOC meetings. These relied on existing working relationships between the ZonePC groups to bridge the central (AHS) and independent (PCNs and PC physicians) components of the broader system. The ZEOC meetings were intended to be information pivot points through which decisions and guidance flowed outward from the ECC and questions and on-the-ground information flowed inward from community PC.
As much as this move to establish a single point of contact between central decision making and independent PC was intended to support health system resilience, it was not received as such by PC personnel. Focused on their own vision for PC resilience, those stakeholders organized three independent bodies outside the IMS. The aim of these bodies was to integrate PC into provincial emergency management efforts generally and, particularly, to improve PC access to IMS’ deliberations and decisions. The three bodies were as follows:
a COVID-19 PCN Incident Response Task Force (Task Force) (PCNs and AHS 2020);
an AHS-PHCP Working Group (Working Group); and
Pandemic Community Care Support Group (Support Group).
The first two bodies – the Task Force and the Working Group – were organized by a range of PHCP, ZonePC and PCN personnel. They continued to meet as of January 2021. The third body – the Support Group – brought together senior MoH staff with PHCP and PCN personnel to identify and support the needs of PC and specialist physicians working in the community (Molnar 2020a). Although the Support Group provided PC personnel access to the highest echelons of the MoH, by September 2020 questions were being raised by members as to whether the group had duplicated other efforts. Specifically, many of the same AHS-PHCP staff sat both on that group and the Task Force and the Working Group (Participant 82). As such, we focus on the Task Force and the Working Group as the ad hoc independent responses to the activation of the IMS and its centralized vision of resilience. We show how the Task Force and the Working Group, operating outside the IMS, were seen by PC stakeholders as ensuring not just a place for PC in the broader response but also resilience in PC operations.
The Task Force was created in March 2020 after personnel in the PHCP realized “We're missing primary care” (Participant 01) in the emergency response system. The Task Force's explicit objective was to align the PCN response with that being rolled out by the MoH and AHS via the IMS (PCNs and AHS 2020). It was thus also an attempt to give PC stakeholders visibility and access into the ECC's deliberations and decision making. The Task Force was composed of executive directors from some of the PCNs, as well as AHS- and community-based physicians.
The Working Group was established as a complementary body to the Task Force, with its mission being to conduct operational activities arising from the pandemic, generally, and the work of the Task Force, specifically. The Working Group was staffed by AHS-PHCP staff. Both the Task Force and the Working Group included crossover members, with this redundancy aimed at ensuring the “effective and efficient transfer of information and communication in both directions” (Participant 74).
Although the Task Force and the Working Group operated smoothly in their PC-focused contexts, their relationship with the IMS, and thus the central system, was more challenging. The bidirectional communications that the groups' members experienced in the AHS-PC and PCN ecosystem became unidirectional when they interacted with the ECC at the pinnacle of the IMS. As a PCN-based member of the Task Force described it, the ratio of downward to upward information flow was “probably 90–10” in the sense that
[the meetings were] all about [ECC] planning, and then, once the community started to be hit with [COVID-19, our] questions and [feedback became about] 10% [of the focus]. (Participant 01)
As such, the Task Force predominantly became a point of information outflow from the administrative AHS-ECC to the provision-oriented PCNs. An AHS-PHCP member described how the emphasis on downward communication was not an aberration of the pandemic:
[AHS] is [a] single healthcare provider on the acute [care] side, and just now starting to think about how to integrate [with community-based PC.] But we still have primary care on the outside looking in. Situations like [COVID-19 reveal] where all the gaps still exist in making it a unified system … there's nothing like a crisis to really tell you where you're at. (Participant 74)
A community-based PC physician echoed this, noting how the pandemic was a lesson about the need "to integrate the way that family physicians and walk-in clinics work with the operations of AHS (Participant 16).
Indeed, the Task Force and the Working Group were formed from competing visions of resilience in which PC was an insider rather than an outsider to the IMS structure, specifically, and to the AHS system more broadly.
In forming the Task Force, members of the PHCP took up an accustomed role of advocacy within their larger organization. PHCP staff in the early days of the pandemic sought out meetings with AHS colleagues:
[R]attling cages like we always do – that's a pretty standard approach that we have to take, even [during] non-COVID [times]. It's like, “Have you considered primary care? Where does primary care fit in there? We think it [has] got to be an important component. Here's what happened last time with H1N1. We need to get and have membership on ECC.” (Participant 74)
Despite this appeal to historical experience and arguments that equated PC involvement with system resilience, a more centralized vision of what was required for resilience prevailed, and the PHCP was ultimately denied a seat at the ECC table.
In response, and following their own vision of resilience, PCHP personnel joined with PCN staff to form the Task Force, which would sit just outside the ECC. Prior to a redesign of the reporting and response structures in November 2020, a single member of the Task Force played a pivotal role and was the personification of an alternative PC-based vision of resilience. This member – who also interacted consistently with the Working Group – happened, also, to sit on the ECC. This was not by accident. Although the member did not sit on the ECC in a PC capacity, they were nonetheless embedded in the administrative and service provision linkage points between central AHS and independent PC. Their presence at the highest levels of both the central response (ECC) and independent PC response (Task Force) was intended to provide a “crosswalk” between the elements. Rather than vying for voice in crowded ZEOC meetings that were intended to be the formal mechanism for ensuring PC resilience in the pandemic, this lone member was able to secure access, albeit informal, to a higher rung of the IMS.
If the Task Force relied on a single crossover member to gain access to the ECC for PC, the PCNs – positioned even further from the central IMS and system – felt even less integrated in the central response. Neither the executive directors of the PCNs – some of whom sat directly on the Task Force – nor the majority of senior PCN operational staff had access to the “lower rung” ZEOCs. A Calgary zone PCN staffer described it:
Our executive director absolutely wasn't integrated into ZEOC calls. I was not part of those [either]. (Participant 56)
This account of the central IMS response to the pandemic, and independent PC stakeholders' replies, has emphasized the adaptive actions of those stakeholders. With their vision of resilience competing with the one embedded in the central response, independent PC developed “work-around” solutions. In the next section, we present evidence that underscores the importance of this ingenuity in ensuring PC resilience during the pandemic. The focus of this section is on the flow of resilience-focused IPC guidance from the central system to independent PC clinics.
Implementation guidance
Even as Alberta's PC physicians began using newly developed VCBCs (CIHI 2021; Government of Alberta 2020b) and shifted to virtual visits for the majority of their patients, some community-managed COVID-19 patients still needed in-person visits. This population – along with a backlog of non-COVID-19 patients who had avoided in-person visits – focused attention on the need for PC-specific guidance on IPC best practices. Without robust IPC measures in place, in-person PC could not be safely carried out. Across Canada, formal responses to this need had seen a range of stakeholders publish guidance on how best to provide IPC in PC and thus ensure resilience in its operations (Pinto et al. 2020).
Specifically, document-based guides were published by the provincial medical association (AMA and ACTT 2020), the provincial regulatory body (CPSA 2021), national public health and IPC agencies (Government of Canada 2021; IPAC 2020), with quality improvement-focused researchers also providing IPC implementation guidance (Blaak et al. 2020). In Alberta, the Task Force and the Working Group – themselves workarounds to the IMS – sought to work with a number of these externally produced recommendations to develop a webpage that would be “the source of truth for community physicians” (Participant 13) as they looked for IPC best practices.
Notwithstanding these efforts, many PC stakeholders described challenges with the IPC guidance that was made available on the website. Specifically, the resources were described as fragmentary, delayed or out of date, difficult to interpret and inadequately mindful of the PC context as they had been developed originally for acute care (Pinto et al. 2020).
As a PC physician noted:
There is no specific guidance [for primary care. We're] supposed to be able to go to the increasingly jumbled AHS website and find stuff, and then translate it [for our] world. (Participant 71)
Another PC physician described this “jumbling” as a problem not just for the AHS IPC guidance website:
Most of the communication [from AHS] is really just a list of websites that we should access. You get 25 different websites … You have to sort through [them] and see what's relevant, [editing out what] is just general information until you hit something that's really pertinent to you. (Participant 16)
The reaction to the jumble and the informational overload of the resilience-seeking website was localized interpretation. An AHS-PHCP staffer described feeling constantly out of sync as independent PC began interpreting centrally supplied guidance to achieve resilience on its own terms. They and their colleagues would
go scrambling to make a bunch of documents and update the website and all that stuff. And then in the meantime, [the PC physicians have] already interpreted [things] themselves because they have to. They need an answer today. They don't need an answer in four days … So they immediately start translating. (Participant 13)
Faced with IPC guidance that was filled with “some vague wording and ‘use your best judgment' type of thing” (Participant 37), many PC physicians felt they were improvising their IPC protocols. Similarly, a PCN staffer described combing the internet for specific guidance on environmental cleaning but finding little:
There's no real specific guidelines saying, “You must clean the bathroom X number of times a day; you must wipe this [surface] X number of times a day” so we just created processes dependent [on our situation]. (Participant 56)
Taking the intricacies of donning and doffing personal protective equipment (PPE) in PC clinics rather than hospital conditions as an example, one PC physician noted:
It takes very intense training and supervision and people need to watch [you don and doff] and make sure that you're doing it right. You have [those people] in a hospital setting. But basically [what the guidance was saying to us in PC was]: “Watch this video. This is how you do donning. This is how you do doffing. Here's some stuff.” (Participant 16)
Translating and improvising amid this ambiguity, many PC personnel came to “wonder who is driving the ship, if anyone at all” (Participant 31).
While most PC clinics navigated and operationalized guidance documents on their own, some clinics and PCNs (n = 15) also participated in novel “tabletop simulation” exercises created over the course of the pandemic by our applied research team (Blaak and Fadaak 2020a, 2020b; Blaak et al. 2021). The appetite for these PPE and IPC implementation simulations was identified in the interviews that elicited the quotations found in the preceding paragraphs. We leveraged our connections with the AHS’ IPC team to draw together PC personnel with questions and IPC professionals with practical answers. The resulting self-declared “community of practice” (Participant 49) continued to meet until May 2021 as a forum for questions on how to use PPE and enact IPC best practices on the front lines of PC. Commenting on the baseline knowledge of PC-based members of the community of practice, one of the AHS-IPC professionals answering the questions noted:
It's a real gap in knowledge and a gap in access to knowledge. Should [PC] have to pay over and above for [IPC expertise]? The challenge is that [my team inside the AHS is] already stretched so thin covering acute care and long-term care, and supported living sites, that to add PC [would be a real challenge]. (Participant 53)
The search for practical guidance on the use of PPE and implementation of IPC best practices culminated in the following: 1) local PC interpretations of guidance developed remotely for acute care contexts; 2) the creation of tabletop simulations for PC by our university-based research team; and 3) a self-started, IPC-focused community of practice within PC. Across these three replies to the central pandemic response, IPC activity inside AHS remained relatively constant, with a member of the AHS-IPC making themselves available to the community of practice as necessary.
Discussion
The COVID-19 pandemic has had a “seismic effect” on the delivery of care by family physicians (Alsnes et al. 2020; Coombes 2020; Schneider and Shah 2020), who are grappling with the uncertainties of their patients' immediate and long-term issues (Greenhalgh et al. 2020). As this test of PC resilience unfolds, governments have sought even greater inclusion of family medicine into the next phase of the pandemic response, with PC deployed to deliver mass vaccination programs (Kanani et al. 2020; Mueller 2020; Weintraub et al. 2020) or positioned as a major resource in overcoming vaccine hesitancy (Griggs 2021). In this context, the ways that pandemic-induced disturbances have led to shared resilience goals, but competing visions of what ought to continue and what ought to change, as well as how to attain those outcomes in PC, are worthy of close policy attention.
The IMS and competing visions of resilience
As a response to the pandemic, Alberta's IMS was intended to streamline decision making and information flow. The IMS embedded a resilience vision in which the central system was superordinate to independent PC just as it was to other services. Indeed, the central system's vision was, in important ways, “blind” to PC's potential for action (Newton et al. 2021). Maintaining this hierarchical relationship and the command-and-control capacities it afforded was, for those activating the IMS and sitting on the ECC, central to ensuring resilience in the healthcare system's operations. In contrast, PC stakeholders maintained a sense that even if they were one among many services, their voice and operational concerns deserved prioritization. This is to say that they expressed a competing resilience vision that was grounded in efforts to raise the profile and status of independent PC that predated the pandemic. Where the central system sought to ensure the continuation of not just operations but also PC's outsider status, PC stakeholders sought continuity of operations and to press home a long sought-after change in PC's relationship with the centre.
For both groups, then, resilience was not only a technical exercise in maintaining operational capacity, but a political exercise in asserting that the pandemic was, on the one hand, a disturbance to be mitigated and, on the other, an opportunity to embrace change. These competing visions suggest that policy makers planning for future pandemics will profitably spend time not just in considering the technical challenges of resilience but also in understanding the political efforts and institutional relationship arcs that subtend discussions of what ought to be protected and what ought to be changed as operational capacity is safeguarded. More specifically, the resilience vision expressed by PC stakeholders in Alberta included the “workaround” creation of a range of groups just outside the gravitational pull of the central system. With the Task Force and the Working Group built on the fly and in reaction to the IMS, these ad hoc resilience-focused structures relied on specific people – in particular a single physician with the cross-over capacity to access the ECC – to succeed.
While improvisation, trust and mutual respect will inevitably play important roles in any system's resilience successes, the opportunity here is to formally integrate PC into the highest levels of an IMS. Finding solutions that sustainably formalize and integrate PC into resilience-focused emergency management policies is a priority for health systems pursuing massive vaccine delivery programs and other PC integration into future public health responses to pandemics. Rather than relying on workaround ingenuity, IMS plans, in whatever form they currently exist, can profitably be revisited with an eye to preventing PC from remaining “on the outside looking in.” Potential benefits to be realized here include improved co-ordination across PC and acute care facilities, as well as cost savings, as more cases are managed more effectively in the community (Newton et al. 2021).
Implementation guidance
As is always the case, PC clinicians needed to translate high-level policy directives into practical changes to their workflow. In the case of IPC guidance, this translation and implementation work was complicated not just in Alberta, but across Canada, by the fact that the available material was minimally reflective of PC realities and difficult to access (Pinto et al. 2020). Replying to this central response, independent PC personnel and researchers moved resiliently to create a patchwork of solutions that ranged from local interpretations of the available guidance, to participating in tabletop simulations, to forming an IPC-focused community of practice and to building a community-facing website. Each of these replies exposed gaps in knowledge, capacity and reach.
Focused policy attention from government and stakeholders is required to get the right guidance to the right people at the right time. The consistent delivery of expert IPC knowledge in an easily digestible and PC-customized form is a resilience-focused policy challenge that will need to be addressed collaboratively by the government and the regulatory and professional organizations in each province. The patchwork of solutions we have described may well provide starting points for policy conversations and further research, but agreeing on common, scalable ways forward is policy work that remains, in many cases, to be done.
Conclusion
The responses of Alberta's central health system to the COVID-19 pandemic led to replies from independent PC stakeholders, with all parties aiming for technical resilience but expressing competing visions for how that ought to be achieved. On the one hand, the central system sought resilience in the continuation of not just care delivery operations but PC's status as an outsider among other services. On the other, independent PC sought both the advancement of ongoing reforms aimed at better integrating PC into the central system, as well as greater influence in the provincial response to a predominantly community-based disease. Attention to the gaps between resilience visions – what ought to be protected and what ought to be altered to ensure continuity of operations – is a key focus for policy planners moving forward.
In this context, planning aimed at maximizing the benefits and minimizing the downsides of improvisational efforts to meet pandemic challenges is necessary. Focal points here include the (re)design of central IMS and IPC guidance distribution structures to include independent PC as robustly as possible without over-relying on workarounds. As this policy planning and structure design occurs, the goal is to leverage existing linkages between central service delivery systems and independent PC in ways that avoid the inconsistencies and potential burnout of responses that rely too heavily on individuals and improvisation.
Acknowledgement
The authors wish to thank the anonymous participants in this study, not just for their time and perspectives on the unfolding pandemic as it has shaped their work, but also for their tireless efforts to deliver care in the face of unprecedented uncertainty and demand.
Contributor Information
Myles Leslie, Director of Research, School of Public Policy, University of Calgary; Associate Professor, Department of Community Health Sciences, Cumming School of Medicine, University of Calgary, Calgary, AB.
Raad Fadaak, Research Associate, School of Public Policy, University of Calgary, Calgary, AB.
Nicole Pinto, Research Associate, School of Public Policy, University of Calgary, Calgary, AB.
Jan Davies, Professor of Anesthesia, Cumming School of Medicine, University of Calgary; Anesthesiologist, Department of Anesthesiology, Perioperative and Pain Medicine, Alberta Health Services, Calgary, AB.
Lee Green, Professor and Chair, Faculty of Medicine and Dentistry Department of Family Medicine, University of Alberta, Edmonton, AB.
Judy Seidel, Adjunct Associate Professor, Department of Community Health Sciences, Cumming School of Medicine, University of Calgary; Scientific Director, Primary Healthcare Integration Network, Alberta Health Services, Calgary, AB.
John Conly, Professor, Department of Microbiology, Immunology and Infectious Diseases, Cumming School of Medicine, University of Calgary, Infection Prevention and Control, Alberta Health Services, Calgary, AB.
Pierre-Gerlier Forest, Director, School of Public Policy, Department of Community Health Sciences, Cumming School of Medicine, University of Calgary, Calgary, AB.
Funding
This work was supported by the Social Sciences and Humanities Research Council and Canadian Institutes for Health Research under the COVID-19 Rapid Response operating grant program dated February 18, 2020, and the World Health Organization's R&D Blueprint Infection Prevention and Control Pillar.
References
- Alberta Health Services (AHS). n.d. Emergency Coordination Centre: COVID-19. Retrieved October 18, 2021. <https://www.albertahealthservices.ca/topics/Page17116.aspx>.
- Alberta Health Services (AHS). 2019. Emergency/Disaster Management: 5. Retrieved October 18, 2021. <https://fhd.athabascau.ca/programs/undergrad/lpn-bn/docs/ahs_emergency.pdf?>.
- Alberta Medical Association (AMA) and Accelerating Change Transformation Team (ACTT). 2020, November 24. Community Physician Provincial Readiness Checklist for COVID-19. Retrieved December 2, 2020. <https://www.albertadoctors.org/COVID-19-info-resources/community-health-clinic-prov-relaunch-re.pdf>.
- Alsnes I.V., Munkvik M., Flanders W.D., Øyane N.. 2020. How Well Did Norwegian General Practice Prepare to Address the COVID-19 Pandemic? Family Medicine and Community Health 8(4): e000512. doi:10.1136/fmch-2020-000512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auditor General of Alberta. 2017. Alberta Health – Primary Care Networks. Retrieved December 1, 2020. <https://www.oag.ab.ca/reports/health-primary-care-networks-oct-2017/>.
- Bhatia R.S., Chu C., Pang A., Tadrous M., Stamenova V., Cram P.. 2021. Virtual Care Use before and during the COVID-19 Pandemic: A Repeated Cross-Sectional Study. CMAJ Open 9(1): E107–E114. doi:10.9778/cmajo.20200311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blaak J., Fadaak R.. 2020a. Adapting Tabletop Simulations to Support Primary Care Teams in the COVID-19 Response [YouTube video]. 48th Annual Meeting, Virtual – NAPCRG. Retrieved October 18, 2021.<https://www.youtube.com/watch?v=Bh1iZuyrXD8&t=3s>. [Google Scholar]
- Blaak J., Fadaak R.. 2020b. Deploying Tabletop Simulations to Improve Primary Care Preparedness for COVID-19 [YoutTube video]. NAPCRG 2020 Workshop – Tabletop Simulations for COVID-19 in Primary Care – Alberta, Canada. Retrieved October 18, 2021. <https://www.youtube.com/watch?v=TxMIyT2GQvo>. [Google Scholar]
- Blaak J., Davies J., Fadaak R., Leslie M., Ferdous M., Cheng M.. 2020. Key Learning & Recommendations for COVID-19 in Primary Care. Retrieved December 2, 2020. <https://www.w21c.org/file/Iterative-Key-Learnings-Recommendations.pdf>.
- Blaak M.J., Fadaak R., Davies J.M., Pinto N., Conly J., Leslie M.. 2021. Virtual Tabletop Simulations for Primary Care Pandemic Preparedness and Response. BMJ Simulation & Technology Enhanced Learning 7(6): 487–93. doi:10.1136/bmjstel-2020-000854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanchet K., Nam S.L., Ramalingam B., Pozo-Martin F.. 2017. Governance and Capacity to Manage Resilience of Health Systems: Towards a New Conceptual Framework. International Journal of Health Policy and Management 6(8): 431–35. doi:10.15171/ijhpm.2017.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boothby L. 2020, March 20. COVID-19 Could Bankrupt Clinics Because of Low Fees for Virtual Visits, Edmonton Doctors' Group Says. Edmonton Journal. Retrieved October 25, 2021. <https://edmontonjournal.com/news/politics/covid-19-edmonton-doctors-group-says-virtual-visits-could-close-clinics-because-of-low-fees>.
- Braithwaite J., Wears R.L., Hollnagel E.. 2015. Resilient Health Care: Turning Patient Safety on Its Head. International Journal for Quality in Health Care 27(5): 418–20. doi:10.1093/intqhc/mzv063. [DOI] [PubMed] [Google Scholar]
- Canadian Institute for Health Information (CIHI). 2021. Physician Billing Codes in Response to COVID-19. Retrieved December 3, 2020. <https://www.cihi.ca/en/physician-billing-codes-in-response-to-covid-19>.
- Canadian Institutes of Health Research (CIHR). 2020. Policy Implementation and Communication Lessons from Alberta's Acute and Primary Care Environments during the COVID-19 Response. Government of Canada. Retrieved December 17, 2020. <https://webapps.cihr-irsc.gc.ca/decisions/p/project_details.html?applId=422611&lang=en>. [Google Scholar]
- Castleden M., McKee M., Murray V., Leonardi G.. 2011. Resilience Thinking in Health Protection. Journal of Public Health 33(3): 369–77. doi:10.1093/pubmed/fdr027. [DOI] [PubMed] [Google Scholar]
- College of Physicians and Surgeons of Alberta (CPSA). 2021. Guidance for Community Medical Clinics: Stage 3 Reopening. Retrieved October 18, 2021. <https://cpsa.ca/wp-content/uploads/2021/07/IPAC-Guidance-for-Community-Medical-Clinics-Stage-3.pdf>.
- Coombes R. 2020. Covid-19: This Time It's Personal for GPs. BMJ 371: m3898. doi:10.1136/bmj.m3898. [Google Scholar]
- El Bcheraoui C., Weishaar H., Pozo-Martin F., Hanefeld J.. 2020. Assessing COVID-19 through the Lens of Health Systems' Preparedness: Time for a Change. Globalization and Health 16(1): 112. doi:10.1186/s12992-020-00645-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forest P.G. 2019. Cutting through the Ice …. Healthcare Quarterly 22(2): 13–14. doi:10.12927/hcq.2019.25911. [DOI] [PubMed] [Google Scholar]
- Glazier R.H., Green M.E., Wu F.C., Frymire E., Kopp A., Kiran T.. 2021. Shifts in Office and Virtual Primary Care during the Early COVID-19 Pandemic in Ontario, Canada. CMAJ 193(6): E200–E210. doi:10.1503/cmaj.202303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Government of Alberta. 2014, January. Alberta's Primary Health Care Strategy. Alberta Health. Retrieved October 18, 2021. <https://open.alberta.ca/dataset/1cac62b5-a383-4959-8187-1b2a6798d0ac/resource/2ff5246a-bdd9-428a-ab04-62e5475c90ed/download/6849603-2014-albertas-primary-health-care-strategy-2014-01.pdf>. [Google Scholar]
- Government of Alberta. 2020a. Fiscal Plan: A Plan for Jobs and the Economy 2020–23. Retrieved October 25, 2021. <https://open.alberta.ca/dataset/05bd4008-c8e3-4c84-949e-cc18170bc7f7/resource/79caa22e-e417-44bd-8cac-64d7bb045509/download/budget-2020-fiscal-plan-2020-23.pdf>.
- Government of Alberta. 2020b, June 9. Alberta Health Care insurance Plan: Virtual Care Codes Made Permanent. Retrieved October 18, 2021. <https://open.alberta.ca/dataset/58a224a2-0fed-4b1e-b8d5-9f6cf70450c6/resource/8323480b-939c-4099-ab76-bdb5147bde9c/download/health-ahcip-bulletin-med-231-virtual-care-codes-permanent.pdf>.
- Government of Canada. 2021, June 28. Infection Prevention and Control for COVID-19: Interim Guidance for Outpatient and Ambulatory Care Settings. Retrieved October 18 2021. <https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/guidance-documents/interim-guidance-outpatient-ambulatory-care-settings.html>.
- Greenhalgh T., Knight M., A'Court C., Buxton M., Husain L.. 2020. Management of Post-Acute Covid-19 in Primary Care. BMJ 370: m3026. doi:10.1136/bmj.m3026. [DOI] [PubMed] [Google Scholar]
- Griggs J. 2021. Leveraging Trust in Primary Care to Promote Behavior Change during COVID-19 [Blog post]. Milbank Memorial Fund. Retrieved October 18, 2021. <https://www.milbank.org/2021/03/leveraging-trust-in-primary-care-to-promote-behavior-change-during-covid-19/>. [Google Scholar]
- Haldane V., Ong S.-E., Chuah F.L.-H., Legido-Quigley H.. 2017. Health Systems Resilience: Meaningful Construct or Catchphrase? The Lancet 389(10078): 1513. doi:10.1016/S0140-6736(17)30946-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanefeld J., Mayhew S., Legido-Quigley H., Martineau F., Karanikolos M., Blanchet K. et al. 2018. Towards an Understanding of Resilience: Responding to Health Systems Shocks. Health Policy and Planning 33(3): 355–67. doi:10.1093/heapol/czx183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Infection Prevention and Control Canada (IPAC). 2020. Coronavirus (COVID-19) Guidance for Acute, Long Term, Community and Dentistry Care. Retrieved December 2, 2020. <https://ipac-canada.org/guidance-for-ltc-community-and-dentistry.php>.
- Kanani N., Lawson E., Waller E.. 2020, November 9. Urgent Preparing for General Practice to Contribute to a Potential COVID-19 Vaccination Programme. NHS. Retrieved October 18, 2021. <https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/C0856_COVID-19-vaccineletter_9-Novrevb.pdf>. [Google Scholar]
- Leach M., Scoones I., Stirling A.. 2010. Governing Epidemics in an Age of Complexity: Narratives, Politics and Pathways to Sustainability. Global Environmental Change 20(3): 369–77. doi:10.1016/j.gloenvcha.2009.11.008. [Google Scholar]
- Legido-Quigley H., Asgari N., Teo Y.Y., Leung G.M., Oshitani H., Fukuda K. et al. 2020. Are High-Performing Health Systems Resilient against the COVID-19 Epidemic? The Lancet 395(10227): 848–50. doi:10.1016/S0140-6736(20)30551-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leslie M., Fadaak R., Davies J., Blaak J., Forest P.G., Green L. et al. 2020a. Integrating the Social Sciences into the COVID-19 Response in Alberta, Canada. BMJ Global Health 5(7): e002672. doi:10.1136/bmjgh-2020-002672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leslie M., Khayatzadeh-Mahani A., Birdsell J., Forest P.G., Henderson R., Gray R.P. et al. 2020b. An Implementation History of Primary Health Care Transformation: Alberta's Primary Care Networks and the People, Time and Culture of Change. BMC Family Practice 21: 258. doi:10.1186/s12875-020-01330-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin M., Beliavsky A., Katz K., Powis J.E., Ng W., Williams V. et al. 2020. What Can Early Canadian Experience Screening for COVID-19 Teach Us about How to Prepare for a Pandemic? CMAJ 192(12): E314–18. doi:10.1503/cmaj.200305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mejdahl C.T., Schougaard L.M.V., Hjollund N.H., Riiskjær E., Lomborg K.. 2018. "Exploring Organisational Mechanisms in PRO-Based Follow-Up in Routine Outpatient Care – An Interpretive Description of the Clinician Perspective. BMC Health Services Research 18: 546. doi:10.1186/s12913-018-3352-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molnar C.P. 2020a, April 17. Embattled. Alberta Medical Association. Retrieved October 18, 2021. <https://www.albertadoctors.org/services/media-publications/presidents-letter/pl-archive/Embattled>. [Google Scholar]
- Mueller B. 2020, December 31. Some Doctors in Britain Plan to Defy Instructions to Delay Vaccine Booster Shots. The New York Times. Retrieved October 18, 2021. <https://www.nytimes.com/2020/12/31/world/uk-britain-covid-coronavirus.html>.
- Newton W.P., Baxley E., Magill M.. 2021. Learning from COVID-19: System Blindness to Primary Care. The Annals of Family Medicine 19(3): 282–84. doi:10.1370/afm.2705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinto N., Fadaak R., Leslie M.. 2020, October 8. COVID-19 Infection Prevention and Control: A Rapid Review of Primary Care Resources across Canada [Blog post]. Canadian Family Physician. Retrieved October 18, 2021. <https://www.cfp.ca/news/2020/10/08/10-8>.
- Primary Care Networks (PCNs) and Alberta Health Services (AHS). 2020, February 27. Overview of COVID-19 PCN Incident Response Task Force. Retrieved December 1, 2020. <https://www.albertahealthservices.ca/assets/info/ppih/if-ppih-covid-19-primary-care-task-force-overview.pdf>.
- Rawaf S., Allen L.N., Stigler F.L., Kringos D., Yamamoto H.Q., van Weel C.. 2020. Lessons on the COVID-19 Pandemic, for and by Primary Care Professionals Worldwide. European Journal of General Practice 26(1): 129–33. doi:10.1080/13814788.2020.1820479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider E.C., Shah T.. 2020, May 20. Pandemic Shock Threatens to Undermine Outpatient Care [Blog]. The Commonwealth Fund. Retrieved October 18, 2021. <https://www.commonwealthfund.org/blog/2020/pandemic-shock-threatens-undermine-outpatient-care>. [Google Scholar]
- Thorne S., Kirkham S.R., MacDonald-Emes J.. 1997. Interpretive Description: A Noncategorical Qualitative Alternative for Developing Nursing Knowledge. Research in Nursing & Health 20(2): 169–77. doi:10.1002/(sici)1098-240x(199704)20:2<169::aid-nur9>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- Thorne S., Stephens J., Traunt T.. 2016. Building Qualitative Study Design Using Nursing's Disciplinary Epistemology. Journal of Advanced Nursing 72(2): 451–60. doi:10.1111/jan.12822. [DOI] [PubMed] [Google Scholar]
- Turenne C.P., Gautier L., Degroote S., Guillard E., Chabrol F., Ridde V.. 2019. Conceptual Analysis of Health Systems Resilience: A Scoping Review. Social Science & Medicine 232: 168–80. doi:10.1016/j.socscimed.2019.04.020. [DOI] [PubMed] [Google Scholar]
- Weintraub R., Koller C.F., Bitton A. 2020, December 1. Why Primary Care Can Make COVID-19 Vaccine Distribution More Successful [Blog post]. Milbank Memorial Fund. Retrieved October 18, 2021. <https://www.milbank.org/2020/12/why-primary-care-can-make-covid-19-vaccine-distribution-more-successful/>. [Google Scholar]
- Wiig S., Aase K., Billett S., Canfield C., Røise O., Nja O. et al. 2020. Defining the Boundaries and Operational Concepts of Resilience in the Resilience in Healthcare Research Program. BMC Health Services Research 20(1): 330. doi:10.1186/s12913-020-05224-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan C., Rose S., Rothberg M.B., Mercer M.B., Goodman K., Misra-Hebert A.D.. 2016. Physician, Scribe, and Patient Perspectives on Clinical Scribes in Primary Care. Journal of General Internal Medicine 31(9): 990–95. doi:10.1007/s11606-016-3719-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yazdizadeh B., Majdzadeh R., Ahmadi A., Mesgarpour B.. 2020. Health Research System Resilience: Lesson Learned from the COVID-19 Crisis. Health Research Policy and Systems 18(1): 136. doi:10.1186/s12961-020-00667-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young J., Donahue M., Farquhar M., Simpson C., Rocker G.. 2012. Using Opioids to Treat Dyspnea in Advanced COPD. Canadian Family Physician 58(7): e401–07. [PMC free article] [PubMed] [Google Scholar]


