Abstract
Purpose of review:
The present review focuses on the epidemiology of type 2 diabetes (T2D) in Indigenous communities in the continental United States (U.S.)—including disease prevention and management—and discusses special considerations in conducting research with Indigenous communities.
Recent findings:
Previous studies have reported the disparately high prevalence of diabetes, especially T2D, among Indigenous peoples in the U.S. The high prevalence and incidence of early-onset T2D in Indigenous youth relative to that of all youth in the U.S. population poses challenges to the prevention of complications of diabetes.
Summary:
Behavioral, dietary, lifestyle and genetic factors associated with T2D in Indigenous communities are often investigated. More limited is discussion of the historical and ongoing consequences of colonization and displacement that impact the aforementioned risk factors. Future research is necessary to assess community-specific needs with respect to diabetes prevention and management across the diversity of Indigenous communities in the U.S.
Introduction: Considerations on terminology with respect to Indigenous peoples
Indigenous peoples in the present-day United States (U.S.), including members of 574 federally recognized tribes and other first peoples of the U.S. and territories, have experienced historical and ongoing challenges to health and its determinants. Due to the tumultuous and complicated relationships between Indigenous nations and the rest of the U.S., increasing participation in research studies among these populations is complex. The dynamic between Indigenous populations in the U.S. and the federal government is often described by “colonization,” a term that encompasses the physical and theoretical framework of interactions among the entities, beginning at first contact between Indigenous peoples and European settlers.[1] Post-contact, European settlers and their descendants who largely took ownership of lands inhabited by Indigenous peoples and power in colonial, federal, and state governments in what became the U.S. used Eurocentric arguments to support forced assimilation and cultural genocide of Indigenous peoples.[2] At the most basic level, careful consideration of engagement with Indigenous individuals and communities begins with terminology. As a result of the complex history of terminology that is rooted in erroneous geography, racism and stereotypes, name designation with respect to Indigenous communities is especially convoluted.[3]
There has been a considerable debate regarding appropriate terminology in discussing and engaging with Indigenous peoples; historically in the U.S., such terminology has included “Indian,” “American Indian,” and “Native American.” Name preferences vary depending on the individual and community, although the general consensus among communities is to ask each their preference, which might utilize their native tongue (e.g. Diné for Navajo). The present review will use a range of terms based on the context. The terms “Indian,” “American Indian (AI)” and “Native American” are based on inaccurate declarations and applied inconsistently (e.g. toward Indigenous peoples of Alaska, Hawaii, Guam, Puerto Rico, U.S. Virgin Islands, etc.); however, these terms are often used in bureaucratic spaces. In the present review, these terms will be used when discussing existing laws and institutions, for consistency; when not discussing these topics, “Indigenous” will be used to concisely include, and honor sovereignty of, first peoples in the U.S., and subgroups included in relevant studies will be specified. This review will focus on the epidemiology of diabetes, especially T2D, in Indigenous communities within the present-day continental U.S.
Prevalence of diagnosed diabetes among adults
According to the 2020 National Diabetes Statistics Report published by the Centers for Disease Control and Prevention, 34.2 million people in the U.S. are estimated to have diabetes (10.5% of the population); of this figure, 7.3 million people (21.4%) are estimated to have undiagnosed diabetes.[4] In the U.S., the prevalence of diabetes in Indigenous populations tends to be higher than in other American ethnic groups. In the National Health Interview Survey (NHIS), in 2011–2015, the age-standardized prevalence of self-reported diagnosed diabetes was 2.2 times higher in Indigenous (American Indian/Alaska Native, AI/AN) than in non-Hispanic white (NHW) men, and 2.5 times higher in Indigenous than in NHW women (Table 1).[5] In the NHIS, age-sex standardized prevalence of diagnosed diabetes in adults aged at least 20 years was 19.1% in Indigenous populations compared with 9.5% in the general population.[5]
Table 1.
Age standardized prevalence of diagnosed diabetes in adults in the U.S. in the NHIS, 2011–2015. From reference 5.
| Ethnic group | Diabetes prevalence in men (95% CI) | Diabetes prevalence in women (95% CI) |
|---|---|---|
| Non-Hispanic Indigenous | 19.7% (15.9–24.1) | 18.8% (13.7–25.2) |
| Non-Hispanic Black | 14.0% (13.7–14.8) | 14.3% (13.6–15.0) |
| Hispanic | 13.9% (13.1–14.8) | 13.2% (12.4–14.0) |
| Non-Hispanic Asian | 10.4% (9.3–11.7) | 8.3% (7.5–9.1) |
| Non-Hispanic White | 9.0% (8.7–9.3) | 7.6% (7.3–7.9) |
The NHIS did not perform testing to identify undiagnosed diabetes. However, studies that have performed glycemic testing to identify undiagnosed—as well as previously diagnosed—diabetes have also found diabetes prevalence to be higher in Indigenous populations than in the general US population, as assessed by the National Health and Nutrition Examination Survey.[6, 7]
According to a nationwide, population-based, cross-sectional survey among adults in the U.S. in 2016 and 2017, approximately 5% of prevalent diabetes comprised type 1 diabetes (T1D), 92% comprised T2D, and 3% comprised other subtypes of diabetes.[8] Previous studies on cardiometabolic health outcomes in certain Indigenous communities in the U.S. have reported that nearly all cases of diabetes in participants were clinically characterized as T2D.[9] Few studies have classified diabetes in Indigenous populations via assessment of T1D-related autoantibodies. Studies in Indigenous communities in the Southwestern U.S. and Alaska have suggested that nearly all diabetes was T2D, based on the absence of T1D-related autoantibodies, as well as clinical characteristics.[10, 11]
Documented cases of diabetes among Indigenous communities in the U.S., approximately 5.2 million individuals (1.6% of the U.S. population), began to increase drastically in the 20th century.[12] A recent observational study on the incidence and prevalence of diagnosed diabetes (T1D and T2D combined) was conducted on Indian Health Service (IHS) health records of Indigenous (AI/AN) adults from 2006–2017. The prevalence of diagnosed diabetes increased significantly from 2006 (14.4%) to 2013 (15.4%) and decreased significantly from 2013 to 2017 (14.6%).[13] These trends were consistent across all age groups (18–44 years, 45–64 years, 65–74 years and ≥ 75 years).[13] There are limited data on prevalence of prediabetes, but several studies have indicated that prevalence of prediabetes in Indigenous populations is similar to, or slightly lower than, in the general population.[14] For example, in a consortium of U.S. health care systems including nearly five million individuals, over 25,000 individuals who identified themselves in health records, or who were identified on their birth certificate, as AI/AN, had lower prevalence of prediabetes (31.1%) as compared with the overall study population (33.4%).[14] In this study, the prevalence of diabetes was 19.6% in AI/AN individuals (15.9% in the overall population), so the prevalence of dysglycemia (prediabetes and diabetes) was 50.7%.
The aforementioned trends in the prevalence of diagnosed diabetes in Indigenous adults (2006–2017) are similar to adults in the general U.S. population as reported in the National Health Interview Survey (2000–2018). Several nationwide changes with respect to diabetes diagnostic criteria, testing practices and ICD coding occurred during the aforementioned study period, which could have affected its results. There are fewer reports of diabetes incidence (as opposed to prevalence), because incidence estimates require longitudinal studies. Among adults in the general U.S. population, the age-adjusted incidence of diagnosed diabetes was similar in 2000 (6.2 per 1000 adults) and 2018 (6.7 per 1000 adults), with an increase in incidence between 2000 and 2008, and a significant decreasing trend in incidence from 2008 (8.4 per 1000 adults) to 2018.[4] Additionally, data from a study of diabetes incidence in an Indigenous community from the Southwestern U.S. demonstrated that, once ascertainment bias was taken into account, incidence of diabetes in the community remained stable throughout the study period (1965–2003), with significant increases occurring only in youth.[15]
Youth-onset diabetes
The relatively high prevalence of T2D in Indigenous populations is particularly pronounced in youth. In the SEARCH for Diabetes in Youth study, which was a population-based assessment of prevalence in youth aged 10–19 years across 5 different American centers as well as several reservation communities, the prevalence of diagnosed T2D was 1.20 per 1000 in Indigenous populations compared with 0.34 per 1000 in NHW counterparts (Table 2).[16]
Table 2.
Prevalence of diagnosed type 2 diabetes in youth aged 10–19 years in the SEARCH for Diabetes in Youth Study. From reference 15.
| Ethnic group | Prevalence of T2D per 1000 (‰) children age 10–19 (95% CI) |
|---|---|
| Indigenous | 1.20‰ (0.96–1.51) |
| Black | 1.06‰ (0.93–1.22) |
| Hispanic | 0.79‰ (0.70–0.88) |
| Asian/Pacific Islander | 0.34‰ (0.26–0.46) |
| White | 0.17‰ (0.15–0.20) |
A trend analysis of diagnosed diabetes (including type 1 and type 2) prevalence among American Indian and Alaska Native young adults (aged 18–34 years) between 1994 and 2007 found statistically significant increasing trends in annual prevalence estimates of diagnosed diabetes among Indigenous (AI/AN, including those from within the 50 United States and Puerto Rico, Guam and the Virgin Islands) and NHW young adults. Indigenous young adults were, on average, 1.7 times more likely than NHW young adults to be diagnosed with diabetes during 1994–2000 and 2.5 times more likely during 2001–2007.[17] Most previous studies have found that the incidence of young-onset T2D in Indigenous children, adolescents and young adults was greater than that of the overall U.S. population in that given time period. The increased incidence of youth-onset T2D in Indigenous children, adolescents, and young adults relative to the overall population poses challenges to the prevention of complications of diabetes.
Complications of diabetes
People with early-onset diabetes have a greater risk of premature development of microvascular and macrovascular complications, as well as psychological comorbidities, over the life course.[18, 19] Diabetic nephropathy (DN) is a major cause of morbidity and mortality. While the prevalence of DN is relatively high in Indigenous communities in the U.S., its incidence has decreased in this demographic group in recent years.[19] However, in the U.S., the incidence of nephropathy remains higher than in the non-Indigenous white population: according to the U.S. Renal Disease Data Systems, incidence of end-stage renal disease (ESRD) among Indigenous populations was 504.4 cases per million individuals in 2018, 1.6 times higher than in the non-Indigenous white population.[20] The public health impact of diabetes on kidney disease is particularly severe in Indigenous communities; diabetes is the primary cause of 67% of the ESRD that occurs in Indigenous (AI/AN) populations, as compared with 39% in the general U.S. population.[20] In a longitudinal population-based study among members of an Indigenous community in the Southwest U.S., early-onset T2D was associated with substantially increased incidence of ESRD and mortality in middle age (25–55 years); the longer duration of T2D experienced by individuals diagnosed with T2D at under 20 years of age predominantly accounted for this burden.[21]
Diabetic retinopathy (DR) is a leading cause of vision loss among adults globally; among Indigenous peoples with diabetes in the U.S., the limited published evidence on DR includes prevalence estimates of 35% to 49% for non-proliferative DR and 3% to 10% for proliferative DR.[22–24] According to a multi-site, cross-sectional study including participants recruited at Indian Health Service-Joslin Vision Network Teleophthalmology Program clinics between 2011 and 2016, 20.0% of patients had DR—approximately half of the estimates from previous literature regarding multiple different Indigenous communities in the U.S.—with 17.7% having non-proliferative DR and 2.3% having proliferative DR.[25]
Risk factors for T2D and considerations with respect to Indigenous communities
Obesity
According to the National Health Interview Survey in the U.S., Indigenous (AI/AN) adults are 50% more likely to have obesity than are non-Hispanic white adults, and Indigenous adolescents are 30% more likely to have obesity than NHW adolescents.[26] While further research on fat distribution and cardiometabolic risk is needed and BMI is not necessarily the optimal predictor of disease risk, there is strong evidence for the association between obesity and hypertension, dyslipidemia, hypercholesterolemia, insulin resistance, and glucose intolerance.[27] One’s risk of obesity, caused by an excess of energy intake relative to energy expenditure, can be influenced by genetic variants and/or lifestyle factors and overnutrition in utero.[28] Longitudinal studies in Indigenous populations have shown that obesity, as measured by body mass index, is strongly and linearly associated with incidence of diabetes and that diabetes incidence is low in those with BMI < 25 kg/m2 (Figure 1).[29]
Figure 1. Age-sex standardized incidence of type 2 diabetes by body mass index in a longitudinal study of Indigenous adults in an Indigenous study population in the Southwest U.S. Adapted from reference 28.
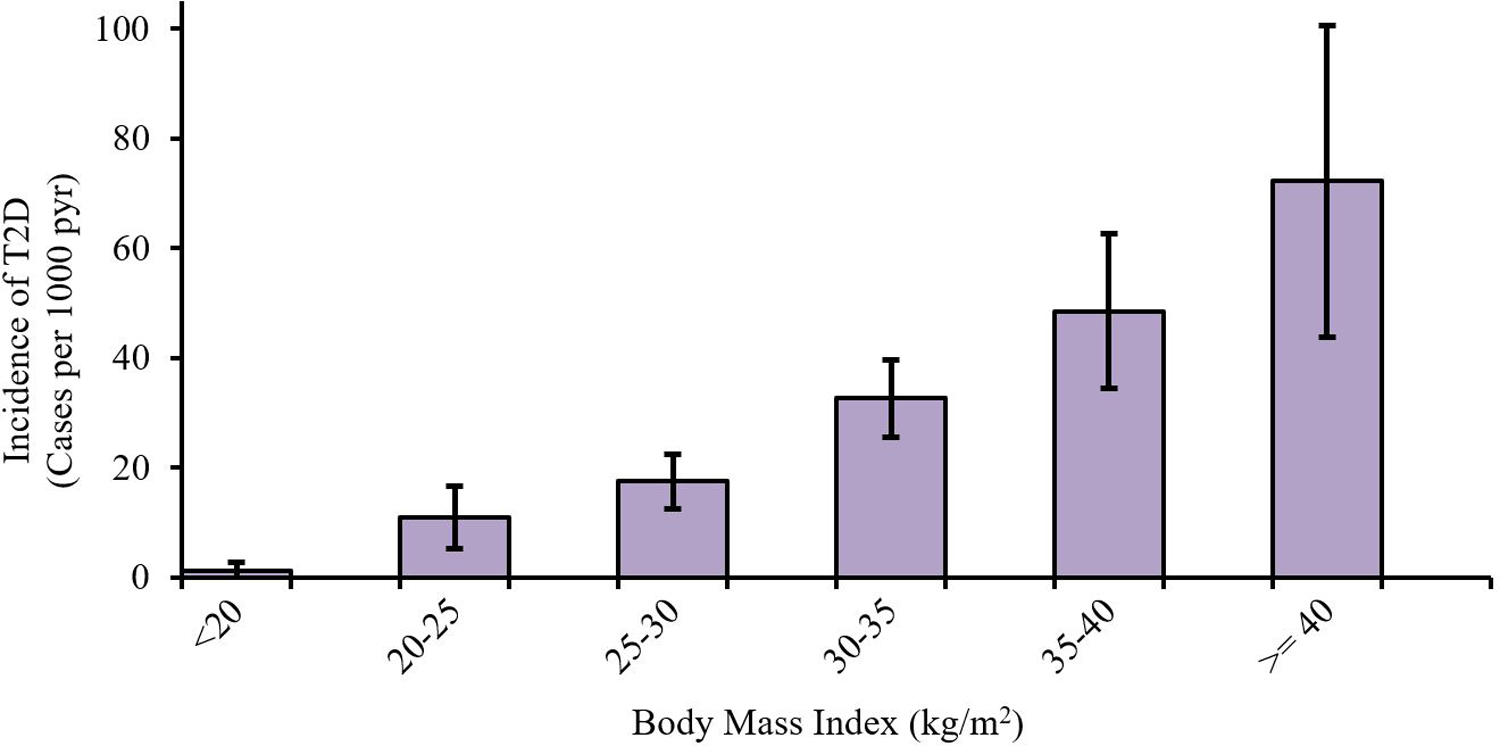
According to a longitudinal study, obesity (as measured by body mass index) is strongly and linearly associated with incidence of diabetes and diabetes incidence is low in those with BMI < 25 kg/m2.
A longitudinal study of Indigenous young adults within a larger general U.S. study population found that Indigenous young adults had higher hemoglobin A1c levels, higher self-reported blood glucose, self-reported diabetes, and obesity. They also had higher rates of structural risk factors (e.g. residing in poorer and more transient neighborhoods and having greater levels of stress) than NHW young adults.[30]
Food security and nutrition
Food insecurity is broadly defined as unpredictable access to healthy foods including fruits, vegetables, refrigerated meats, and dairy items.[31] Nutrition status is directly impacted by food security, which is one external mechanism by which food insecurity confers elevated risks of developing obesity (a major risk factor for T2D) and T2D.[32, 33] Thus, the efficacy of interventions that aim to reduce risk of T2D is reduced by the food security and nutrition status of participants.[34] Food insecurity is a dynamic and often transient experience for individuals and households and becomes particularly complex in Indigenous communities, whose food environment has been impacted by historical events and trauma.[35]
Food environments common in and nearby tribal reservations, including the relatively low number of supermarkets and great number of gas station and other convenience stores (which have limited availability of fresh produce and acceptance of food stamps), can affect residents’ risk of obesity.[36] Approximately 76.7% of the population on tribal reservations live more than 1 mile from a grocery store, as opposed to 41.2% of the general U.S. population. Nearly 50% of individuals living on tribal reservations have an income at or below 200% of the federal poverty level, as opposed to 28.9% of the general U.S. population.[37] In a cross-sectional study of Indigenous adults living within the Chickasaw Nation and the Choctaw Nation of Oklahoma, using nontraditional food retailers (e.g. convenience stores, gas stations and discount stores) was significantly associated with obesity and diabetes.[38]
Colonization and the formation of the present-day U.S. displaced Indigenous peoples already residing on these lands, creating environmental inequities and dependence on the U.S. Federal Government.[39, 40] Although the U.S. Department of Agriculture’s Food Assistance Programs (e.g. Commodity Supplemental Food Programs) were established to mitigate the issues caused by colonization, the issues of food sovereignty, reclamation of traditions and access to nutritious foods remain challenges for Indigenous communities in the U.S.[41, 42] Collectively, food insecurity and colonization have contributed to health disparities, including increased prevalence of T2D, among Indigenous communities.[43, 44]
Behavioral risk factors
Within Indigenous populations, the influence of behavioral and psychosocial factors is compounded by existing environmental risks and low socioeconomic status. The role of mental health and stress in the development and management of T2D in Indigenous communities is not well understood. In a longitudinal health study in an Indigenous community in the Southwest U.S., the prevalence of depression was slightly but not significantly higher among adult participants with diabetes than those without diabetes.[45] Another study involving Indigenous individuals with T2D from two reservation communities reported that individuals with greater numbers of reported mental and emotional health issues had greater risk of self-reported hyperglycemia, comorbidities and physical activity impairment.[46] In a study of Indigenous adults in the U.S. with T2D, reports of adverse childhood experiences were common and associated in a dose-response manner with increased odds of screening positive for current depression.[47] Other studies in Indigenous communities report a sense of fatalism and inevitability with respect to diabetes among community members.[48, 49] Further empirical research on the association between mental health issues, chronic stress, and T2D is needed.
Intergenerational trauma—a term capturing the broad impacts of genocidal forced loss of lands, languages and cultures[50, 51]—is well-recognized among Indigenous communities globally and has been associated with risk of anxiety and affective disorders.[52] While risk factors are important to identify and address, some researchers have found that support from cultural and familial entities have assisted in management of chronic diseases (e.g. T2D) and mitigated detrimental effects of adverse childhood experiences.[53] Furthermore, individuals who experienced more apathy were at increased risk for high blood sugar while individuals who were more involved in cultural and traditional activities, such as integration of more traditional foods,[54] were significantly less likely to have feelings of apathy and to have high blood sugar.[55] Emerging solutions increasingly address disparities in food security and nutrition affecting Indigenous communities through interventions that focus on regaining food sovereignty through increased integration of traditional foods and severance of diets linked to cardiometabolic diseases.[56]
Smoking has been shown to increase risk for T2D and to increase risk for macrovascular complications in people with diabetes.[57, 58] Estimates of the prevalence of cigarette smoking among Indigenous peoples in the U.S. vary across communities. A cross-sectional study found that 32% of American Indians currently smoked at the time of the study, over double the general U.S. smoking rate (15.5%).[59] According to a cross-sectional survey of IHS patients, AI/AN individuals with diabetes were more likely than those without diabetes to be current smokers (30% vs. 19%, p<0.01), and current smokers with diabetes were more likely than nonsmokers with diabetes to have HbA1c > 8.0% (p<0.05).[60] Many Indigenous communities use tobacco for ceremonial purposes.[61] Cessation programs and tribal health campaigns to “keep tobacco sacred” have been tailored to Indigenous communities, to distinguish the ceremonial use of traditional tobacco from the habitual use of commercial forms of tobacco; however, researchers often conflate the two.[62, 63] Research and prevention efforts must be informed by this context in addressing current smoking disparities and health risks among Indigenous communities.
Physical activity—including leisure-time and occupational activity—is associated with lower risk of incident diabetes and obesity in Indigenous communities as well as in the general population in the U.S.[64, 65] One study reported that a relatively low proportion (14.7%) of Indigenous adults in the U.S. met current recommendations for physical activity and that this proportion did not substantially change between 1998 and 2017.[66] A systematic review published in 2013 found that Indigenous adults in Canada and the U.S. reported lower activity levels since 2000 as compared with the 1990s, although recent activity levels were similar to those in the 1980s.[67] According to a cross-sectional analysis of over 10,000 Indigenous adults in the U.S., characteristics that were positively and significantly associated with time spent performing vigorous activity per week included: male sex, age < 40 years, and living in a rural area.[68] Further research is needed to assess the reasons for disparities in physical exercise and to develop and evaluate lifestyle intervention programs to promote physical activity among Indigenous peoples in the U.S.
Genetic factors
Estimates of the heritability of type 2 diabetes, derived from twin and family studies, range from 20–80%, and T2D results from the complex interplay of genetic and environmental factors.[69, 70] Studies in Indigenous populations in the U.S. have reported similar estimates of heritability for T2D—ranging from 22–62%.[71, 72] These heritability estimates reflect phenotypic resemblance among family members, and they illustrate potential genetic effects on T2D, although they can also reflect clustering of environmental risk factors within families. Over 400 independent single-nucleotide polymorphisms have been associated with T2D at a genome-wide significant level, though these explain a small proportion of the heritability.[73]
Genome-wide association studies, candidate gene and linkage-based studies of type 2 diabetes that have identified these genetic variants have predominantly included European-ancestry study populations.[74] Studies that have examined the effects of these established T2D-susceptibility variants have found that, while there is some modest heterogeneity in effects across populations, the variants generally associate with diabetes in Indigenous populations in a way consistent with the effects in Europeans.[7, 75] While common variants are largely shared across ancestral groups, certain genetic variants that strongly and significantly associate with type 2 diabetes have greater risk allele frequencies in certain study populations than others. Some genetic variants with strong effects on diabetes risk, are common or at low frequency in certain Indigenous study populations, but are rare in other continental ancestry groups (e.g. ABCC8 R1420H, HNF1A G319S).[76, 77] Certain variants in the gene KCNQ1—which are established as associated with T2D across multiple ancestry groups—exhibit parent-of-origin effects and have particularly strong effects on diabetes in an Indigenous community from the Southwest U.S.[78]
The extent to which genetic differences among populations explain the high risk for T2D experienced by Indigenous populations remains undetermined. Studies comparing the frequencies of established T2D-susceptibility alleles across populations have been inconsistent; some have found higher frequencies in Indigenous populations than in populations at lower risk for T2D, while others have not.[7, 79, 80] Differences may lie in which populations are analyzed and how markers are ascertained: the ascertainment of diabetes-susceptibility variants remains incomplete and the extent to which the currently ascertained variants capture effects of causal variants across populations is unpredictable due to variation in linkage disequilibrium patterns.
The “thrifty genotype hypothesis” has played a prominent role as a potential explanation for the high risk of T2D and obesity in Indigenous populations in the U.S. This hypothesis was originally created to offer an explanation for the then-increasing global burden of diabetes, proposing that genetically-conferred metabolic “thriftiness” is maladaptive to “Westernized” lifestyles, but was advantageous in the “feast-or-famine days” of human ancestors.[81] Several investigators have proposed that such selection, operating more strongly in the population history of Indigenous peoples, may explain their higher risk of T2D in the present day.[82, 83] However, analyses of molecular signatures of selection at established diabetes risk alleles have provided little evidence for such selection.[84, 85] Furthermore, the differences in diabetes prevalence among Indigenous Americans and other ancestry groups (African Americans, European Americans) are consistent with expectations under evolutionary neutrality, given genetic distances and heritability.[86]
Intergenerational transmission of risk for diabetes
Parental diabetes has been associated with elevated risk of subsequent diabetes in offspring. Maternal diabetes (i.e. in utero exposure to a diabetic environment) has also been associated with subsequent risk of T2D and accelerated weight gain and T2D in offspring.[87, 88] In an Indigenous population in the Southwestern U.S., maternal diabetes was associated with greater birth weight and greater risk of diabetes in offspring; by contrast, paternal diabetes was associated with lower birth weight and greater risk of diabetes in offspring.[89] In this population, as compared with offspring of women who developed diabetes after pregnancy or who remained diabetic, the offspring of women who had diabetes during pregnancy had greater risk of obesity and higher plasma glucose concentrations.[90] A systematic review of gestational diabetes (GDM) in study populations in the U.S., Australia, New Zealand and Canada showed that Indigenous subgroups had varying rates of GDM that were frequently greater than those of non-Indigenous subgroups.[91]
Many studies have investigated the complex relationships among parental genotype and diabetes; and offspring genotype, birth weight, obesity and T2D. In multiple study populations, including certain Indigenous populations, the association between birth weight and the risk of T2D forms a U-shaped curve, in which lower and higher birth weights are associated with greater risk of T2D later in life.[92,93] Genetic and non-genetic factors contribute in a complex interplay to elevated risk of subsequent T2D in individuals with lower versus higher birth weights.
The disproportionately high prevalence of T2D, a complex disease resulting from environmental and genetic factors, in Indigenous children and adults suggests increased risk of diabetes in future generations if prevention efforts are not successful. Notably, the Stopping Gestational Diabetes Mellitus in Daughters and Mothers intervention was a preconception counseling and diabetes risk reduction program culturally tailored to Indigenous (AI/AN) women.[94] A study of qualitative data from the program found that Indigenous women were aware of topics including nutrition and healthy weight gain during pregnancy, and expressed the need for specific education on GDM risk reduction and the challenges of healthful eating during and before pregnancy for Indigenous women.[95] In addition to diabetes prevention efforts, further research should specifically address the mechanisms through which parental diabetes, in utero exposure to a diabetic environment, offspring birth weight and offspring diabetes relate.
IHS and diabetes-related health care services
The IHS was established in 1955 when the responsibility of meeting the health needs of American Indians and Alaska Natives was transferred from the Department of the Interior to the U.S. Public Health Service.[96,97] Since 1955, 28 IHS facilities across 8 states in both urban and rural locations have been established, serving approximately 2.6 million members of 574 currently federally recognized American Indian and Alaska Native Tribes.[98] IHS coverage does not account for numerous tribal communities that are not federally recognized, as well as Indigenous peoples in U.S. territories. Many IHS facilities engage in pediatric screening for T2D and focus on implementing a clinical model of patient-centered care (PCC). This model shifts the traditional authoritarian physician paradigm to one in which patients are engaged in their health-related decisions. IHS facilities also offer preconception care as well as screening for diabetes during and after pregnancy.[99]
The Diabetes Prevention Program and Special Diabetes Program for Indians
Notably, the Diabetes Prevention Program (DPP) was a landmark randomized controlled trial that assessed the effect of an intensive lifestyle intervention (ILI) on prevention or delay of diabetes onset, relative to the drug metformin, or placebo.[100] The latter two groups received standard health lifestyle advice. 3234 participants were randomized to the three-arm trial in the DPP, with an average age of 51 years at baseline and 68% women; five percent of participants were American Indian. The ILI decreased the incidence of diabetes by 58% and randomization to metformin decreased diabetes incidence by 31% compared with the placebo group.[101] There were no significant differences in diabetes incidence or treatment effects according to racial/ethnic group.
The IHS has established the Special Diabetes Program for Indians (SDPI) Community Directed Program, which provides grant funding to 301 IHS and tribal entities in 35 states that are solely dedicated to prevention and treatment of T2D. Mandated and funded by U.S. Congress as part of SDPI, the SDPI Diabetes Prevention (SDPI-DP) project assessed the translational effectiveness of the DPP intensive lifestyle intervention in preventing T2D across 36 rural, reservation and urban Indigenous communities in the U.S.[102] This study, implementing community-based participatory research principles, implemented the Lifestyle Balance Curriculum intervention, a goal-based curriculum adapted from the DPP that addressed food choices, food preparation, physical activity, stress management and self-motivation. Because the lifestyle intervention from the DPP was demonstrably so effective, the institutional review board for SDPI-DP did not allow for a control group; however, the crude incidence among all SDPI-DP participants was 4.0% per year, that for those who finished all 16 classes was 3.5% per year, and that for those who did not finish all the classes was 7.5% per year.[102]
A previous literature review highlighted 15 studies of culturally-influenced diabetes prevention interventions that were conducted with Indigenous youth and adults published between 1990 and 2008: three demonstrated long-term effectiveness in T2D prevention and two did not; ten described the interventions without reporting outcomes.[103] Such limited published research suggests a need for further community-based participatory research studies with Indigenous communities to identify their specific needs with respect to the prevention of T2D, as well as long-term interventions and assessment of longitudinal health outcomes.
Conclusions
Indigenous communities have high prevalence of T2D as compared with other demographic groups in the U.S. T2D is a complex disease that is associated with a host of risk factors in the domains of nutrition and food security, behavioral health, mental health, genetic epidemiology, parental diabetes, and the intrauterine environment. For centuries, Indigenous peoples in the U.S. have endured loss of land and traditional foodways that could contribute to this disparity and merit consideration beyond race being a simple heuristic for risk of T2D.
Future research to address these issues will require engagement with Indigenous communities, fostering community involvement throughout all processes; and receptiveness to innovative, possibly unconventional, techniques.[104] Such research is necessary to assess community-specific needs with respect to diabetes prevention and management across the diversity of Indigenous communities in the U.S.
Footnotes
Indexing in PubMed: All co-authors are employees of the U.S. Government (National Institutes of Health), so this article is not subject to copyright and will be indexed in PubMed.
References
- 1.Alfred GT. Colonialism and State Dependency. Int J Indig Heal 2009:5:42–60. 10.3138/IJIH.V5I2.28982. [DOI] [Google Scholar]
- 2.Braun KL, Browne CV., Ka’Opua LS, et al. Research on indigenous elders: From positivistic to decolonizing methodologies. Gerontologist 2014:54:117–126. 10.1093/geront/gnt067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Davis-Delano LR, Gone JP, Fryberg SA. The psychosocial effects of Native American mascots: a comprehensive review of empirical research findings. Race Ethn Educ 2020:23:613–633. 10.1080/13613324.2020.1772221. [DOI] [Google Scholar]
- 4.Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2020. Atlanta, GA: 2020. [Google Scholar]
- 5.Cowie CC, Casagrande SS, Geiss LS. Prevalence and incidence of type 2 diabetes and prediabetes. In: Cowie CC, Casagrande SS, Menke A (eds) Diabetes in America, 3rd ed. National Institute of Diabetes and Digestive and Kidney Diseases (US), Bethesda, MD. [PubMed] [Google Scholar]; •• Cowie et al review results of the National Health Interview Survey (NHIS), which has shown that in the U.S., the prevalence of diabetes in Indigenous populations tends to be higher than in other American ethnic groups. In 2011–2015, the age-standardized prevalence of self-reported diagnosed diabetes was 2.2 times higher in Indigenous (American Indian/Alaska Native, AI/AN) than in non-Hispanic white (NHW) men, and 2.5 times higher in Indigenous than in NHW women.
- 6.Sugarman JR, Gilbert TJ, Weiss NS. Prevalence of diabetes and impaired glucose tolerance among Navajo Indians. Diabetes Care 1992:15:114–120. 10.2337/diacare.15.1.114. [DOI] [PubMed] [Google Scholar]
- 7.Hanson RL, Rong R, Kobes S, et al. Role of established type 2 diabetes-susceptibility genetic variants in a high prevalence American Indian population. Diabetes 2015:64:2646–57. 10.2337/db14-1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xu G, Liu B, Sun Y, et al. Prevalence of diagnosed type 1 and type 2 diabetes among US adults in 2016 and 2017: Population based study. BMJ 2018:362:1497. 10.1136/bmj.k1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dabelea D, Pettitt DJ, Jones KL, Arslanian SA. Type 2 diabetes mellitus in minority children and adolescents: An emerging problem. Endocrinol Metab Clin North Am 1999:28:709–729. 10.1016/S0889-8529(05)70098-0. [DOI] [PubMed] [Google Scholar]
- 10.Mohatt J, Gilliam LK, Bekris L, et al. Type 1 diabetes-related autoantibodies are rare in Alaska native populations. Int J Circumpolar Health 2002:61:21–31. 10.3402/ijch.v61i1.17402. [DOI] [PubMed] [Google Scholar]
- 11.Knowler WC, Bennett PH, Bottazzo GF, Doniach D. Islet cell antibodies and diabetes mellitus in Pima Indians. Diabetologia 1979:17:161–164. 10.1007/BF01219743. [DOI] [PubMed] [Google Scholar]
- 12.Will JC, Strauss KF, Mendlein JM, et al. Diabetes mellitus among Navajo Indians: Findings from the Navajo Health and Nutrition Survey. J Nutr 1997:127:. 10.1093/jn/127.10.2106s. [DOI] [PubMed] [Google Scholar]
- 13.Bullock A, Sheff K, Hora I, et al. Prevalence of diagnosed diabetes in American Indian and Alaska Native adults, 2006–2017 What are the new findings? BMJ Open Diab Res Care 2020:8:1218. 10.1136/bmjdrc-2020-001218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhu Y, Sidell MA, Arterburn D, et al. Racial/ethnic disparities in the prevalence of diabetes and prediabetes by BMI: Patient Outcomes Research To Advance Learning (PORTAL) multisite cohort of adults in the U.S. Diabetes Care 2019:42(12):2211–2219. 10.2337/dc19-0532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pavkov ME, Hanson RL, Knowler WC, et al. Changing patterns of type 2 diabetes incidence among Pima Indians. Diabetes Care 2007:30:1758–1763. 10.2337/dc06-2010. [DOI] [PubMed] [Google Scholar]
- 16.Dabelea D, Mayer-Davis EJ, Saydah S, et al. Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA - J Am Med Assoc 2014:311:1778–1786. 10.1001/jama.2014.3201. [DOI] [PMC free article] [PubMed] [Google Scholar]; •• Dabalea et al describe the results of the SEARCH for Diabetes in Youth study, which was a population-based assessment of prevalence in youth aged 10–19 years across 5 different American centers as well as several reservation communities. The prevalence of T2D was 1.20 per 1000 in Indigenous populations, substantially greater with the prevalence in non-Hispanic white counterparts (0.34 per 1000 in NHW counterparts).
- 17.Roberts H, Jiles R, Mokdad A, et al. Trend analysis of diagnosed diabetes prevalence among American Indian/Alaska Native young adults - United States, 1994–2007. Ethn Dis 2009:19:276–279 [PubMed] [Google Scholar]
- 18.Haines L, Wan KC, Lynn R, et al. Rising incidence of type 2 diabetes in children in the U.K. Diabetes Care 2007:30:1097–1101. 10.2337/dc06-1813. [DOI] [PubMed] [Google Scholar]
- 19.Pavkov ME, Knowler WC, Hanson RL, Nelson RG. Diabetic nephropathy in American Indians, with a special emphasis on the Pima Indians. Curr. Diab. Rep 2008:8:486–493. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Pavkov et al describe the prevalence and incidence of diabetic nephropathy (DN) in Indigenous communities, with a focus on an Indigenous community from the Southwest U.S. While the prevalence of DN is relatively high in Indigenous communities in the U.S., its incidence was found to have decreased in this demographic group in recent years.
- 20.Saran R, Robinson B, Abbott KC, et al. US Renal Data System 2019 Annual Data Report: Epidemiology of kidney disease in the United States. Am J Kidney Dis 2020:75:A6–A7. 10.1053/j.ajkd.2019.09.003. [DOI] [PubMed] [Google Scholar]
- 21.Pavkov ME, Bennett PH, Knowler WC, et al. Effect of youth-onset type 2 diabetes mellitus on incidence of end-stage renal disease and mortality in young and middle-aged Pima Indians. J Am Med Assoc 2006:296:421–426. 10.1001/jama.296.4.421. [DOI] [PubMed] [Google Scholar]
- 22.Nagi DK, Pettitt DJ, Bennett PM, et al. Diabetic retinopathy assessed by fundus photography in pima indians with impaired glucose tolerance and NIDDM. Diabet Med 1997:14:449–456. . [DOI] [PubMed] [Google Scholar]
- 23.Rate RG, Knowler WC, Morse HG, et al. Diabetes mellitus in Hopi and Navajo Indians. Prevalence of microvascular complications. Diabetes 1983:32:894–899. 10.2337/diab.32.10.894. [DOI] [PubMed] [Google Scholar]
- 24.Berinstein DM, Stahn RM, Welty TK, et al. The prevalence of diabetic retinopathy and associated risk factors among Sioux Indians. Diabetes Care 1997:20:757–759. 10.2337/diacare.20.5.757. [DOI] [PubMed] [Google Scholar]
- 25.Bursell SE, Fonda SJ, Lewis DG, Horton MB. Prevalence of diabetic retinopathy and diabetic macular edema in a primary care-based teleophthalmology program for American indians and alaskan natives. PLoS One 2018:13:. 10.1371/journal.pone.0198551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. Summary health statistics: National Health Interview Survey, 2018. Atlanta, GA: 2018. [Google Scholar]
- 27.Saxton SN, Clark BJ, Withers SB, et al. Mechanistic links between obesity, diabetes, and blood pressure: Role of perivascular adipose tissue. Physiol Rev 2019:99:1701–1763. 10.1152/physrev.00034.2018. [DOI] [PubMed] [Google Scholar]
- 28.Romieu I, Dossus L, Barquera S, et al. Energy balance and obesity: what are the main drivers? Cancer Causes Control 2017:28:247–258. 10.1007/s10552-017-0869-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Knowler WC, Pettitt DJ, Savage PJ, Bennett PH. Diabetes incidence in Pima Indians: Contributions of obesity and parental diabetes. Am J Epidemiol 1981:113:144–156. 10.1093/oxfordjournals.aje.a113079. [DOI] [PubMed] [Google Scholar]
- 30.Marley TL, Metzger MW. A longitudinal study of structural risk factors for obesity and diabetes among American Indian young adults, 1994–2008. Prev Chronic Dis 2015:12:. 10.5888/pcd12.140469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bickel G, Nord M, Price C, et al. Measuring food security in the United States Guide to Measuring Household Food Security, Revised 2000. Washington, DC: 2000. [Google Scholar]
- 32.Jernigan VBB, Huyser KR, Valdes J, Simonds VW. Food insecurity among American Indians and Alaska Natives: A national profile using the Current Population Survey–Food Security Supplement. J Hunger Environ Nutr 2017:12:1–10. 10.1080/19320248.2016.1227750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Seligman HK, Bindman AB, Vittinghoff E, et al. Food insecurity is associated with diabetes mellitus: Results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999–2002. J Gen Intern Med 2007:22:1018–1023. 10.1007/s11606-007-0192-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dinour LM, Bergen D, Yeh MC. The food insecurity-obesity paradox: A review of the literature and the role food stamps may play. J Am Diet Assoc 2007:107:1952–1961. 10.1016/j.jada.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 35.Warne D, Wescott S. Social determinants of American Indian nutritional health. Curr Dev Nutr 2019:3:12–18. 10.1093/cdn/nzz054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gittelsohn J, Sharma S. Physical, consumer, and social aspects of measuring the food environment among diverse low-income populations. Am J Prev Med 2009:36:S161. 10.1016/j.amepre.2009.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kaufman P, Dicken C, Williams R. Measuring access to healthful, affordable food in American Indian and Alaska Native tribal areas, EIB-131, U.S. Department of Agriculture, Economic Research Service, 2014. [Google Scholar]
- 38.Love CV, Taniguchi TE, Williams MB, et al. Diabetes and obesity associated with poor food environments in American Indian communities: The Tribal Health and Resilience in Vulnerable Environments (THRIVE) Study. Curr Dev Nutr 2019:3:63–68. 10.1093/cdn/nzy099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.White KP. Indigenous food systems, environmental justice, and settler-industrial states. In: Rawlinson MC, Ward C (eds) Global Food, Global Justice: Essays on Eating under Globalization. Cambridge Scholars Publishing, pp 143–156. [Google Scholar]
- 40.Newton NJ. Winters v. United States, 207 U.S. 564 (1908). In: Cohen’s Handbook of Federal Indian Law 1207.
- 41.Lynn K, Daigle J, Hoffman J, et al. The impacts of climate change on tribal traditional foods. Clim Change 2013:120:545–556. 10.1007/s10584-013-0736-1. [DOI] [Google Scholar]
- 42.Levy S To combat diabetes, native peoples rediscover traditional plants. Bioscience 2019:69:689–696. 10.1093/biosci/biz081. [DOI] [Google Scholar]
- 43.Gracey M, King M. Indigenous health part 1: determinants and disease patterns. Lancet 2009:374:65–75. 10.1016/S0140-6736(09)60914-4. [DOI] [PubMed] [Google Scholar]
- 44.King M, Smith A, Gracey M. Indigenous health part 2: the underlying causes of the health gap. Lancet 2009:374:76–85. 10.1016/S0140-6736(09)60827-8. [DOI] [PubMed] [Google Scholar]
- 45.Sahota PKC, Knowler WC, Looker HC. Depression, diabetes, and glycemic control in an American Indian community. J Clin Psychiatry 2008:69:800–809. 10.4088/JCP.v69n0513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Walls ML, Sittner KJ, Aronson BD, et al. Stress exposure and physical, mental, and behavioral health among american Indian adults with type 2 diabetes. Int J Environ Res Public Health 2017:14:. 10.3390/ijerph14091074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Elm JHL. Adverse childhood experiences and internalizing symptoms among American Indian adults with type 2 diabetes. J Racial Ethn Heal Disparities 2020:7:958–966. 10.1007/s40615-020-00720-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mechanick JI, Adams S, Davidson JA, et al. Transcultural diabetes care in the United States – A position statement by the American Association of Clinical Endocrinologists. Endocr Pract 2019:25:729–765. 10.4158/PS-2019-0080. [DOI] [PubMed] [Google Scholar]
- 49.Cavanaugh CL, Taylor CA, Keim KS, et al. Cultural perceptions of health and diabetes among Native American men. J Health Care Poor Underserved 2008:19:1029–1043. 10.1353/hpu.0.0083. [DOI] [PubMed] [Google Scholar]
- 50.Maple-Brown LJ, Graham S, McKee J, Wicklow B. Walking the path together: incorporating Indigenous knowledge in diabetes research. Lancet Diabetes Endocrinol 2020:8:559–560. 10.1016/S2213-8587(20)30188-1. [DOI] [PubMed] [Google Scholar]
- 51.Warne D, Lajimodiere D. American Indian health disparities: Psychosocial influences. Soc Personal Psychol Compass 2015:9:567–579. 10.1111/spc3.12198. [DOI] [Google Scholar]
- 52.Ehlers CL, Gizer IR, Gilder DA, et al. Measuring historical trauma in an American Indian community sample: Contributions of substance dependence, affective disorder, conduct disorder and PTSD. Drug Alcohol Depend 2013:133:180–187. 10.1016/j.drugalcdep.2013.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Brockie TN, Elm JHL, Walls ML. Examining protective and buffering associations between sociocultural factors and adverse childhood experiences among American Indian adults with type 2 diabetes: a quantitative, community-based participatory research approach. BMJ Open 2018:8:e022265. 10.1136/bmjopen-2018-022265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sarkar D, Walker-Swaney J, Shetty K. Food diversity and indigenous food systems to combat diet-linked chronic diseases. Curr Dev Nutr 2020:4:3–11. 10.1093/CDN/NZZ099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Carlson AE, Aronson BD, Unzen M, et al. Apathy and type 2 diabetes among American Indians: Exploring the protective effects of traditional cultural involvement. J Health Care Poor Underserved 2017:28:770–783. 10.1353/hpu.2017.0073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wicklow BA, Sellers EAC. Maternal health issues and cardio-metabolic outcomes in the offspring: A focus on Indigenous populations. Best Pract Res Clin Obstet Gynaecol 2015:29:43–53. 10.1016/j.bpobgyn.2014.04.017. [DOI] [PubMed] [Google Scholar]
- 57.Eliasson B Cigarette smoking and diabetes. Prog Cardiovasc Dis 2003:45:405–413. 10.1053/pcad.2003.00103. [DOI] [PubMed] [Google Scholar]
- 58.Pan A, Wang Y, Talaei M, et al. Relation of active, passive, and quitting smoking with incident type 2 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol 2015:3:958–967. 10.1016/S2213-8587(15)00316-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Jamal A, Phillips E, Gentzke AS, et al. Current cigarette smoking among adults -- United States, 2016. MMWR Morb Mortal Wkly Rep 2018:67:53–59. 10.15585/mmwr.mm6702a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Morton DJ, Garrett M, Reid J, Wingard DL. Current smoking and type 2 diabetes among patients in selected Indian Health Service clinics, 1998–2003. Am J Public Health 2008:98:560–565. 10.2105/AJPH.2006.104042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Walls ML, Hautala D, Gonzalez M, et al. Perceptions and prevalence of alcohol and cigarette use among American Indian adults with type 2 diabetes. Clin Diabetes 2019:37:260–268. 10.2337/cd18-0078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Smith SS, Rouse LM, Caskey M. Culturally tailored smoking cessation for adult American Indian smokers: a clinical trial. Couns Psychol 2014:42:852–886. 10.1177/0011000014542601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Daley CM, James AS, Barnoskie RS, et al. “Tobacco has a purpose, not just a past”: feasibility of developing a culturally appropriate smoking cessation program for a pan-tribal native population. Med Anthropol Q 2006:20:421–440. 10.1525/maq.2006.20.4.421. [DOI] [PubMed] [Google Scholar]
- 64.Fretts AM, Howard BV., Kriska AM, et al. Physical activity and incident diabetes in American Indians. Am J Epidemiol 2009:170:632–639. 10.1093/aje/kwp181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kriska AM, Saremi A, Hanson RL, et al. Physical activity, obesity, and the incidence of type 2 diabetes in a high-risk population. Am J Epidemiol 2003:158:669–675. 10.1093/aje/kwg191. [DOI] [PubMed] [Google Scholar]
- 66.Benjamin EJ, Muntner P, Alonso A, et al. Heart Disease and Stroke Statistics-2019 Update: A report from the American Heart Association. Circulation 2019:139:e56–e528. 10.1161/CIR.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 67.Foulds HJA, Warburton DER, Bredin SSD. A systematic review of physical activity levels in Native American populations in Canada and the United States in the last 50 years. Obes Rev 2013:14:593–603. 10.1111/obr.12032. [DOI] [PubMed] [Google Scholar]
- 68.Redwood D, Schumacher MC, Lanier AP, et al. Physical activity patterns of American Indian and Alaskan Native people living in Alaska and the Southwestern United States. Am J Heal Promot 2009:23:388–395. 10.4278/ajhp.071211130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ali O. Genetics of type 2 diabetes. World J Diabetes 2013:4:114. 10.4239/wjd.v4.i4.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Willemsen G, Ward KJ, Bell CG, et al. The concordance and heritability of type 2 diabetes in 34,166 twin pairs from international twin registers: The Discordant Twin (DISCOTWIN) Consortium. Twin Res Hum Genet 2015:18:762–771. 10.1017/thg.2015.83. [DOI] [PubMed] [Google Scholar]
- 71.North KE, Williams JT, Welty TK, et al. Evidence for joint action of genes on diabetes status and CVD risk factors in American Indians: The strong heart family study. Int J Obes 2003:27:491–497. 10.1038/sj.ijo.0802261. [DOI] [PubMed] [Google Scholar]
- 72.Baier LJ, Hanson RL. Genetic studies of the etiology of type 2 diabetes in Pima Indians: Hunting for pieces to a complicated puzzle. Diabetes 2004:53:1181–1186. 10.2337/diabetes.53.5.1181. [DOI] [PubMed] [Google Scholar]
- 73.Udler MS, McCarthy MI, Florez JC, Mahajan A. Genetic risk scores for diabetes diagnosis and precision medicine. Endocr Rev 2019:40:1500–1520. 10.1210/er.2019-00088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Martin AR, Kanai M, Kamatani Y, et al. Clinical use of current polygenic risk scores may exacerbate health disparities. Nat Genet 2019:51:584–591. 10.1038/s41588-019-0379-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Carlson CS, Matise TC, North KE, et al. Generalization and dilution of association results from European GWAS in populations of non-European ancestry: The PAGE Study. PLoS Biol 2013:11:1001661. 10.1371/journal.pbio.1001661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Baier LJ, Muller YL, Remedi MS, et al. ABCC8 R1420H loss-of-function variant in a Southwest American Indian community: Association with increased birth weight and doubled risk of type 2 diabetes. Diabetes 2015:64:4322–4332. 10.2337/db15-0459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hegele RA, Cao H, Harris SB, et al. The hepatic nuclear factor-1α G319S variant is associated with early-onset type 2 diabetes in Canadian Oji-Cree. J Clin Endocrinol Metab 1999:84:1077–1082. 10.1210/jcem.84.3.5528. [DOI] [PubMed] [Google Scholar]
- 78.Hanson RL, Guo T, Muller YL, et al. Strong parent-of-origin effects in the association of KCNQ1 variants with type 2 diabetes in American Indians. Diabetes 2013:62:2984–2991. 10.2337/db12-1767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Chen R, Corona E, Sikora M, et al. Type 2 diabetes risk alleles demonstrate extreme directional differentiation among human populations, compared to other diseases. PLoS Genet 2012:8:. 10.1371/journal.pgen.1002621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chande AT, Rishishwar L, Conley AB, et al. Ancestry effects on type 2 diabetes genetic risk inference in Hispanic/Latino populations. BMC Med Genet 2020:21:. 10.1186/s12881-020-01068-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Neel JV. Diabetes mellitus: A “thrifty” genotype rendered detrimental by “progress”? Am J Hum Genet 1962:14:353–362 [PMC free article] [PubMed] [Google Scholar]
- 82.Wendorf M, Goldfine ID. Archaeology of NIDDM: Excavation of the “thrifty” genotype. Diabetes 1991:40:161–165. 10.2337/diab.40.2.161. [DOI] [PubMed] [Google Scholar]
- 83.Gerstein HC, Waltman L. Why don’t pigs get diabetes? Explanations for variations in diabetes susceptibility in human populations living in a diabetogenic environment. CMAJ 2006:174:25–26. 10.1503/cmaj.050649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Southam L, Soranzo N, Montgomery SB, et al. Is the thrifty genotype hypothesis supported by evidence based on confirmed type 2 diabetes- and obesity-susceptibility variants? Diabetologia 2009:52:1846–1851. 10.1007/s00125-009-1419-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wang G, Speakman JR. Analysis of positive selection at single nucleotide polymorphisms associated with body mass index does not support the “thrifty gene” hypothesis. Cell Metab 2016:24:531–541. 10.1016/j.cmet.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 86.Hanson RL, Van Hout CV, Hsueh WC, et al. Assessment of the potential role of natural selection in type 2 diabetes and related traits across human continental ancestry groups: comparison of phenotypic with genotypic divergence. Diabetologia 2020:63:2616–2627. 10.1007/s00125-020-05272-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Pettitt DJ, Baird HR, Aleck KA, et al. Excessive obesity in offspring of Pima Indian women with diabetes during pregnancy. N Engl J Med 1983:308:242–245. 10.1056/nejm198302033080502. [DOI] [PubMed] [Google Scholar]
- 88.Pettitt DJ, Aleck KA, Baird HR, et al. Congenital susceptibility to NIDDM. Role of intrauterine environment. Diabetes 1988:37:622–628. 10.2337/diab.37.5.622. [DOI] [PubMed] [Google Scholar]
- 89.Lindsay RS, Dabelea D, Roumain J, et al. Type 2 diabetes and low birth weight: The role of paternal inheritance in the association of low birth weight and diabetes. Diabetes 2000:49:445–449. 10.2337/diabetes.49.3.445. [DOI] [PubMed] [Google Scholar]
- 90.Pettitt DJ, Nelson RG, Saad MF, et al. Diabetes and obesity in the offspring of Pima Indian women with diabetes during pregnancy. Diabetes Care 1993:16:310–314. 10.2337/diacare.16.1.310. [DOI] [PubMed] [Google Scholar]
- 91.Voaklander B, Rowe S, Sanni O, et al. Prevalence of diabetes in pregnancy among Indigenous women in Australia, Canada, New Zealand, and the USA: a systematic review and meta-analysis. Lancet Glob Health 2020:8:e681–e698. 10.1016/S2214-109X(20)30046-2. [DOI] [PubMed] [Google Scholar]
- 92.McCance DR, Pettitt DJ, Hanson RL, et al. Birth weight and non-insulin dependent diabetes: Thrifty genotype, thrifty phenotype, or surviving small baby genotype? BMJ 1994:308:942. 10.1136/bmj.308.6934.942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Olaiya MT, Wedekind LE, Hanson RL, et al. Birthweight and early-onset type 2 diabetes in American Indians: differential effects in adolescents and young adults and additive effects of genotype, BMI and maternal diabetes. Diabetologia 2019:62:1628–1637. 10.1007/s00125-019-4899-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Nadeau KJ, Stotz SA, Moore K, et al. Beta testing of a gestational diabetes risk reduction intervention for American Indian and Alaska Native teens. J Pediatr Health Care 2020:34:418–423. 10.1016/j.pedhc.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Stotz SA, Charron-Prochownik D, Terry MA, et al. Stopping gestational diabetes in American Indian and Alaska Native girls: nutrition as a key component to gestational diabetes risk reduction. Curr Dev Nutr 2020:5:13–21. 10.1093/cdn/nzaa081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bergman AB, Grossman DC, Erdrich AM. A political history of the Indian Health Service. Milbank Q 1999:77:571–604. 10.1111/1468-0009.00152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Sequist TD, Cullen T, Acton KJ. Indian Health Service innovations have helped reduce health disparities affecting American Indian and Alaska Native people. Health Aff 2011:30:1965–1973. 10.1377/hlthaff.2011.0630. [DOI] [PubMed] [Google Scholar]
- 98.Levinson DR. Indian Health Service hospitals: Longstanding challenges warrant focused attention to support quality care. Washington, DC: 2016. [Google Scholar]
- 99.Ho J, Bachman-Carter K, Thorkelson S, et al. Glycemic control and healthcare utilization following pregnancy among women with pre-existing diabetes in Navajo Nation. BMC Health Serv Res 2018:18:1–8. 10.1186/s12913-018-3434-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.The Diabetes Prevention Program Research Group. The Diabetes Prevention Program. Design and methods for a clinical trial in the prevention of type 2 diabetes. Diabetes Care 1999:22:623–634. 10.2337/diacare.22.4.623. Erratum in: Diabetes Care 1999:22:1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002:346:393–403. 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Jiang L, Manson SM, Beals J, et al. Translating the diabetes prevention program into American Indian and Alaska Native communities: Results from the Special Diabetes Program for Indians diabetes prevention demonstration project. Diabetes Care 2013:36:2027–2034. 10.2337/dc12-1250. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Jiang et al review the results of the Special Diabetes Program for Indians Diabetes Prevention project (SDPI-DP), which implemented the Lifestyle Balance Curriculum intervention, a goal-based curriculum adapted from the original Diabetes Prevention Program (DPP). The crude incidence of diabetes among all SDPI-DP participants was 4.0% per year, that for those who finished all 16 classes was 3.5% per year, and that for those who did not finish all the classes was 7.5% per year.
- 103.Edwards K, Patchell B. State of the science: A cultural view of Native Americans and diabetes prevention. J Cult Divers 2009:16:32–35 [PMC free article] [PubMed] [Google Scholar]
- 104.Walls ML, Whitesell NR, Barlow A, Sarche M. Research with American Indian and Alaska Native populations: Measurement matters. J Ethn Subst Abuse 2019:18:129–149. 10.1080/15332640.2017.1310640. [DOI] [PMC free article] [PubMed] [Google Scholar]


