Abstract
Background
Although the emotional and psychological impact of nurses’ work had been identified before the COVID-19 pandemic, the pandemic aggravated risk indicators for their mental health.
Aim
The objective of this study was to analyse the levels of anxiety, depression, post-traumatic stress and burnout of nurses in the Balearic Islands (Spain) during the pandemic to identify possible sociodemographic and related occupational factors.
Design
A cross-sectional study of 892 nurses was conducted during four weeks from February to March 2021.
Methods
Sociodemographic data related to the pandemic were collected and anxiety, depression, burnout and post-traumatic stress were measured with validated scales. A multivariate and predictive analysis was carried out with risk estimates.
Findings
About 75.6% of the nurses had experience in COVID-19 units, and 49.1% had worked for more than 10 months in a COVID-19 unit. Nurses in COVID-19 units (hospital ward or ICU) were more likely to report emotional fatigue (OR 1.9, p < 0.001) and anxiety (OR 1.5, p = 0.021). In general, moderate post-traumatic stress was evident in general nurses (p = 0.027), and severe post-traumatic stress was evident in ICU nurses (p = 0.027). A 1.24-month reduction in COVID-19 patient care predicted reduced levels of emotional fatigue (5.45 points), depersonalisation (1.87 points) and post-traumatic stress (4.65 points) in nurses.
Conclusion
Given the occurrence of new waves of COVID-19, the need to establish preventive strategies that focus on the personal and occupational characteristics related to these indicators and to implement urgent psychological support strategies is demonstrated.
Impact
Given these findings, it is imperative solutions are urgently applied in order to prevent compounding risk to the health system.
Keywords: Nurses, Stress disorders, Post-traumatic, Anxiety, Depression, Burnout, Psychological, COVID-19
Summary of relevance
Problem
The COVID-19 pandemic and the high demand for care have overwhelmed health professionals, aggravating risk indicators for their mental health.
Studies are needed to evaluate emotional indicators to understand these effects before, during, and after the pandemic.
What is already known
Nurses manifest behavioural patterns characterised by fatigue, loss of motivation, and symptoms consistent with anxiety and depression as a consequence of high and extensive workloads during the COVID-19 pandemic.
Many work shifts, high number of hours worked, being older and little professional experience seem to be associated with increased risk of developing burnout among nurses.
What this paper adds
Nurses present more post-traumatic stress, anxiety, depression, and burnout syndrome during the pandemic than before.
The levels of stress, anxiety, and depression are affected by the type of unit where the nurse works and whether or not they are in contact with COVID-19 patients.
Immediate psychological care for nurses is necessary during the pandemic and the number of days caring for COVID-19 patients must be reduced to reduce the emotional impact.
A system of rotation of nurses to decrease time caring for patients with COVID-19 may reduce distress. Rotating non-COVID-19-units nurses with COVID-19-units may be an option to achieve this.
Alt-text: Unlabelled box
1. Introduction
In March 2020, the World Health Organization declared the COVID-19 outbreak a pandemic. This situation has challenged not only the stability of social and economic structures but also health systems and the mental health of the population, including health professionals.
While the data on the psychological responses to the pandemic are alarming in the general population (González-Sanguino et al., 2020; Mazza et al., 2020; Wang et al., 2020), these results are doubly so for frontline health professionals such as nurses, especially in terms of anxiety, post-traumatic stress and depression. In most studies, nurses have shown higher levels of post-traumatic stress and physical and emotional fatigue than other health professionals due to their increased workload, the difficulty of the work tasks and traumatic events resulting from the pandemic (Anmella et al., 2020; Lai et al., 2020; Luceño-Moreno et al., 2020; Zerbini et al., 2020)
Although the emotional and psychological impact of nurses’ work had been identified before the COVID-19 pandemic (Mesa Castro, 2019), the pandemic and high demand for care have overwhelmed these health professionals, aggravating risk indicators for their mental health. Direct personal contact, high levels of responsibility and exposure to near-death situations have increased, worsening the work situation of these professionals and increasing the risk to their health (Luceño-Moreno et al., 2020; Nowicki et al., 2020; Zakeri, Hossini Rafsanjanipoor, Zakeri, & Dehghan, 2021). This situation further exacerbates the outcomes predicted by studies, such as that of Fornés-Vives (2019), which estimated before the pandemic that one in five nurses would suffer high levels of work stress that led them to abandon the profession (Fornés-Vives et al., 2019).
1.1. Literature review
As a result of work and emotional overload pre-pandemic, nurses manifest behavioural patterns characterised by fatigue, loss of motivation and symptoms consistent with anxiety and depression, which place patients at risk (Aiken et al., 2012). In direct relation to these behaviours, nurses commonly experience burnout syndrome, which includes high levels of emotional fatigue, high depersonalisation and low personal fulfilment at work. This three-dimensional syndrome usually occurs due to continued exposure to work stressors such as insufficient training, equipment problems, workloads or rotations (Gutiérrez & Arias-Herrera, 2018).
In a pandemic situation like the one we have experienced; nurses' mental health may have been affected. Studies are needed to evaluate emotional indicators to understand these effects before, during and after the pandemic. However, it is necessary to consider the importance of exposure to stressors related not only to the nurse but also to the patient, and above all, the institution and health system, in the development of this syndrome (Baldonedo-Mosteiro et al., 2019; Gómez-Urquiza et al., 2017; Gutiérrez & Arias-Herrera, 2018). Therefore, several authors warn of the importance of addressing environmental or organisational stressors and taking into account the related sociodemographic variables to strengthen the actions needed to protect groups at highest risk (Baldonedo-Mosteiro et al., 2019; Fornés-vives, 2020; Orgambídez-Ramos et al., 2018).
In this regard, work shifts (especially shifts in rotation morning, afternoon and night), number of hours worked (more hours per month), age (older), and professional experience (between 10 and 20 years of experience in the same service) seem to be associated with an increased risk of developing burnout among nurses (Luceño-Moreno et al., 2020). These data highlight the importance of describing and monitoring before the pandemic the emotional, psychological and social impact of the different dimensions that comprise burnout, as well as anxiety, depression and post-traumatic stress, on nurses.
Such efforts are even more necessary during the current pandemic situation to illuminate the new environments and conditions that nurses face, identify the factors that present the greatest risk and design and develop strategies that help reduce the impact of these factors on nurses’ mental health.
2. Participants, ethics, and methods
2.1. Aim
The objective of this study was to describe the levels of anxiety, depression, post-traumatic stress and burnout that nursing professionals experienced during the COVID-19 pandemic and to identify potentially related sociodemographic and occupational factors.
2.2. Design
A descriptive, cross-sectional and observational study was conducted via the distribution of a self-administered questionnaire to nurses at the socio-health centres of the Balearic Islands (Spain) during 4 weeks from February to March 2021.
2.3. Participants
The Balearic Islands is a region of Spain located in an archipelago in the Mediterranean made up of 4 islands with approximately one million inhabitants in total. The health system is mixed, mostly public and universal care. It is made up of 4 public hospitals and more than 5 private ones, more than 50 primary care centres and more than 30 socio-health care centres.
The total number of COVID-19 cases in the Balearic Islands in February 2021 was 55,816 patients, of which about 144 were hospitalised and 60 in intensive care units. It was considered the third wave, the most intense in the region.
About 6122 nurses from the Balearic Islands were invited to participate via email and the internal information systems of all public and private socio-health centres. The questionnaire collected information on the nurses’ sociodemographic characteristics, factors related to care during the COVID-19 pandemic and three validated scales on burnout, anxiety and depression and post-traumatic stress (Costa Requena & Gil Moncayo, 2007; Maslach et al., 1986; Terol Cantero et al., 2007; Zigmond & Snaith, 1983).
2.4. Data collection
The questionnaire was carried out online through a virtual platform. It was distributed through the intranet of the health centres. The questionnaire collected the following information:
Regarding sociodemographic variables, information was obtained regarding the nurses’ age, gender, health centre, unit or service, educational level, marital status, cohabitants, dependents, children, professional role, work shifts, contract, places of work, years of professional experience and experience caring for patients with COVID-19.
Regarding variables related to the pandemic, information was collected on the number of months that the nurses had cared for COVID-19 patients, workload, unit changes due to lack of personnel, increases in work hours, suspension of requested time off during the pandemic, number of PCR tests performed, whether the nurses had been positive for COVID-19, days of isolation and quarantine, hospitalisation due to COVID-19, after-effects, sick leave and whether close contacts had been infected with COVID-19.
To analyse the management of the pandemic, information was collected on PPE and attitudes regarding restrictive measures, management by the health system, information on COVID-19, vaccination and its side effects and concerns and fears regarding vaccination. In addition, information was obtained regarding whether the nurses had received psychological support and whether they believed they needed such support now or would need it in the near future due to the pandemic.
For the measurement of burnout syndrome, anxiety, depression and post-traumatic stress, the following scales were used:
Burnout: The Spanish adaptation of the Maslach Burnout Inventory (MBI-HSS) instrument was applied to evaluate burnout syndrome (Aguayo et al., 2011; Seisdedos, 1997) with license number FPUEYCMRD. It consists of 22 items with seven response options on a Likert scale from 0 (never) to 6 (every day). The scale has three dimensions: (i) emotional fatigue, for which scores less than 0-18 points are considered low, scores between 19 and 26 points are considered moderate and scores more than 27 points are considered high; (ii) depersonalisation (low < 5, medium 6-9, high > 10); and (iii) personal fulfilment (low < 33, medium 34-39, high > 40). This scale presents adequate psychometric characteristics, which show an appropriate fit for the three-factor solution and a consistency greater than 0.71 for all subscales (Aguayo et al., 2011; Cañadas-de la Fuente et al., 2014).
Anxiety and depression: The Spanish adaptation of the Hospital Anxiety and Depression Scale (HADS) was used (Terol Cantero et al., 2007; Zigmond & Snaith, 1983). It consists of 14 items that correspond to two subscales of anxiety and depression. Each subscale comprises seven items scored on a Likert scale ranging from 0-4. The HADS evaluates symptoms of anxiety and depression in patients and in the general population. The cutoff values are <7, absent; 8-10 points, doubtful or possible; and > 11, serious. The higher the score is, the higher the prevalence of symptoms of anxiety and depression is. The Spanish adaptation showed adequate psychometric properties that confirm the validity of two factors, with an internal consistency of 0.77 for the anxiety subscale and 0.71 for the depression subscale (Maslach et al., 1986).
Post-traumatic stress: The Impact of Event Scale–Revised (IES-R) was used (Costa Requena & Gil Moncayo, 2007) to evaluate the emotional distress accompanying a stressful life event, such as the pandemic or the death of a patient from COVID-19. It comprises 22 items distributed in three scales: (a) intrusion (7 items), (b) avoidance (8 items) and (c) hyperarousal (7 items). Regarding post-traumatic stress, a score of 20 was considered the cutoff point. A total score greater than or equal to 20 on the IES-R suggests a possible psychiatric disorder, and a mean score less than or equal to 14 suggests that the presence of a psychiatric disorder is unlikely (Costa Requena & Gil Moncayo, 2007). Symptoms can be classified as subclinical at 0-8 points, mild at 9-25 points, moderate clinically significant post-traumatic stress at 26-43 points and severe clinically significant post-traumatic stress at more than 43 points. The Spanish adaptation of this scale shows adequate psychometric properties that confirm the three-factor solution, and the reliability is greater than 0.70 for all subscales.
2.5. Data analysis
The statistical program IBM SPSS Statistics version 26 was used. Statistical significance was considered at p < 0.05. The data were subjected to an exploratory analysis using the Kolmogorov-Smirnov test to determine whether the variables fit a normal distribution. A descriptive (univariate) analysis of each of the study variables was performed, and the data were filtered to rule out outliers or extremes. For qualitative variables, the absolute frequency and distribution of responses were calculated. For quantitative variables with a normal distribution, the mean was used as a measure of central tendency, and the standard deviation was used as a measure of dispersion if the distribution of the data met the normality requirement. Bivariate association analysis was performed. Possible associations between the variables were explored. The chi-square test was used for the analysis of categorical variables. For comparisons between dichotomous categorical variables and quantitative variables, we used Student's t test for independent groups, with the requirement of normality and equality of variances. To explore the possible association between categorical variables with three or more levels and quantitative variables, we used ANOVA. The type of association between continuous quantitative variables was examined with the Pearson correlation coefficient. To study the relationship between the confounding factors (sociodemographic characteristics) and the different outcome measurements, a bivariate or multiple linear regression model was applied using the variables that had a significance levels of < 0.2 in the univariate comparisons, and different risk estimates were obtained (odds ratios: OR). Linear regression equations were used to evaluate the relationship of each of the variables (demographic characteristics, work characteristics, COVID-19-related factors and burnout) regardless of the symptoms (post-traumatic stress, anxiety and depression) using the R2 value and the standardised coefficient. Finally, models were used to determine which variables (demographic characteristics, work characteristics, COVID-19-related factors and burnout) were related to symptoms of post-traumatic stress, anxiety and depression. The model was estimated by least squares using the forward stepwise selection method.
2.6. Validity and reliability/rigour
To ensure methodological rigor, all the scales used are scientifically validated. Normality and homogeneity of the variances analyses have been included. Possible limitations of the study have been explored and included in the manuscript. The results have been contrasted with similar studies before and during the pandemic to compare the significant changes produced. Confirmation intervals have been established and a significance of 95% has been considered.
3. Findings
3.1. Sociodemographic characteristics and information on the COVID-19 pandemic
A total of 892 nurses from all centres in the Balearic Islands (Spain) out of a total of 6122 nurses who participated in the study. A total of 67.4% (n = 601) worked in specialised care centres (hospitals), 14.8% (n = 132) worked in primary health care and nursing homes, 5.8% (n = 52) worked in emergency care centres, and 8.4% (n = 75) worked in private centres.
A total of 82.6% (n = 737) were women, and 69% (n = 614) were between 29 and 48 years of age. A total of 39.9% (n = 356) had postgraduate training. The majority (n = 625; 71%) lived with their partners, and 186 (20.9%) had dependents in their care. A total of 94.1% (n = 839) are healthcare nurses. Only 34.8% (n = 309) were permanent staff, 83.6% were full-time staff, and 57% (n = 507) were on rotating shifts (7-hour morning or afternoon shifts and 10-hour night shifts). A total of 61.3% (n = 546) had between 10 and 30 years of professional experience. A total of 49.2% (n = 358) had one to 15 years of experience in a single unit. The units in which they conducted their professional activity can be found in Table 1 .
Table 1.
Association between scales and demographic variables.
| Variable | Emotional fatigue n(%) |
0R/p | Anxiety n(%) |
OR/p | Depression n(%) |
OR/p | Post-traumatic stress n(%) |
OR/p | Burnout n(%) |
OR/p | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low | Moderate | High | Absent | Probable | Present | Absent | Probable | Present | Mild | Moderate. | Severe | NO | YES | ||||||
| GENDER | |||||||||||||||||||
| Male | 43(15.4) | 29(15.8) | 80(18.8) | ⁎⁎1.7 | 56(25.1) | 33(14.2) | 62(14.5) | ⁎⁎1.2 | 49(18.3) | 81(18.4) | 22(12.2) | ⁎⁎1.7 | 49(17.8)) | 55(14.3) | 22(17.5) | ⁎⁎0.97 | 107(18.3) | 45(14.9) | ⁎⁎1.1 |
| Female | 237(84.6) | 154(84.2) | 346(81.2) | 0.438 | 167(74.9) | 200(85.8) | 370(85.5) | 0.001* | 219(81.7) | 360(81.6) | 158(87.8) | 0.151 | 226(82.2) | 329(85.7) | 104(82.5) | 0.079 | 479(81.7) | 258(85.1) | 0.201 |
| AGE | |||||||||||||||||||
| 18-28 years | 25(8.9) | 21(11.5) | 70(16.4) | 18(8) | 24(10.3) | 74(17.1) | 17(6.3) | 65(14.7) | 34(18.9) | 44(16) | 51(13.3) | 13(10.3) | 77(13.1) | 39(12.8) | |||||
| 29-38 years | 95(33.8) | 62(33.9) | 144(33.8) | ⁎⁎0.7 | 81(36.2) | 93(39.9) | 127(29.3) | ⁎⁎1.1 | 96(37.5) | 139(31.5) | 66(36.7) | ⁎⁎0.6 | 101(36.7) | 118(30.7) | 36(28.6) | ⁎⁎1.3 | 199(34) | 102(33.6) | ⁎⁎1 |
| 39-48 years | 108(38.4) | 65(35.5) | 140(32.9) | 0.242 | 88(39.3) | 79(33.9) | 146(33.7) | 0.010* | 97(36.1) | 158(35.8) | 58(32.2) | 0.002* | 93(33.8) | 142(37) | 45(35.7) | 0.007* | 204(34.8) | 109(35.9) | 0.962 |
| 49-58 years | 39(13.9) | 28(15.3) | 55(12.9) | 29(12.9) | 27(11.6) | 66(15.2) | 45(16.7) | 58(13.2) | 19(10.6) | 28(10.2) | 50(13) | 29(23) | 79(13.5) | 43(14.1) | |||||
| 59-66 years | 14(5) | 7(3.8) | 17(4) | 8(3.6) | 10(4.3) | 20(4.6) | 14(5.2) | 21(4.8) | 3(1.7) | 9(3.3) | 23(6) | 3(2.4) | 27(4.6) | 11(3.6) | |||||
| SERVICE | |||||||||||||||||||
| ICU adult | 11(3.9) | 8(4.4) | 40(9.5) | 14(6.3) | 16(6.9) | 29(6.8) | 23(8.6) | 21(4.8) | 15(8.4) | 18(6.6) | 26(6.8) | 11(8.9) | 49(8.5) | 10(3.3) | |||||
| ICU ped | 12(4.3) | 3(1.6) | 7(1.7) | 4(1.8) | 7(3) | 11(2.6) | 4(1.5) | 11(2.5) | 7(3.9) | 10(3.7) | 9(2.4) | 2(1.6) | 10(1.7) | 12(4) | |||||
| Consultation | 13(4.7) | 4(2.2) | 19(4.5) | 9(4.1) | 8(3.4) | 19(4.4) | 9(3.4) | 17(3.9) | 10(5.6) | 11(4) | 15(3.9) | 7(5.6) | 25(4.3) | 11(3.6) | |||||
| O. room2 | 18(6.5) | 9(4.9) | 21(5) | 10(4.5) | 14(6) | 24(5.6) | 17(6.3) | 23(5.3) | 8(4.5) | 11(4) | 27(7.1) | 5(4) | 30(5.2) | 18(6) | |||||
| COVID-Ce1 | 4(1.4) | 7(3.8) | 7(1.7) | ⁎⁎1.9 | 2(0.9) | 8(3.4) | 8(1.9) | ⁎⁎1.5 | 6(2.2) | 8(1.8) | 4(2.2) | ⁎⁎1 | 3(1.1) | 11(2.9) | 4(3.2) | ⁎⁎1.3 | 9(1.6) | 9(3) | ⁎⁎0.8 |
| Hosp adult | 41(14.7) | 38(20.9) | 74(17.7) | 0.000* | 39(17.6) | 35(15.1) | 79(18.5) | 0.021* | 45(16.8) | 75(17.3) | 33(18.5) | 0.585 | 29(10.6) | 58(15.2) | 22(17.7) | 0.077 | 101(17.5) | 52(17.2) | 0.019* |
| Urg ped | 10(3.6) | 1(0.5) | 1(0.2) | 5(2.3) | 5(2.2) | 2(0.5) | 3(1.1) | 6(1.4) | 3(1.7) | 52(19) | 3(0.8) | 1(0.8) | 9(1.6) | 3(1) | |||||
| Urg adult | 24(8.6) | 19(10.4) | 45(10.7) | 21(9.5) | 29(12.5) | 38(8.9) | 22(8.2) | 51(11.8) | 15(8.4) | 6(2.2) | 44(11.5) | 13(10.5) | 53(9.2) | 35(11.6) | |||||
| H COVID3 | 19(6.8) | 16(8.8) | 38(9.1) | 13(5.9) | 19(8.2) | 41(9.6) | 25(9.3) | 38(8.8) | 19(5.6) | 20(7.3) | 46(12.1) | 5(4) | 49(8.5) | 24(7.9) | |||||
| Hosp ped | 11(3.9) | 4(2.2) | 4(1) | 8(3.6) | 4(1.7) | 7(1.6) | 6(2.2) | 11(2.5) | 2(1.1) | 18(6.6) | 8(2.1) | 2(1.6) | 12(2.1) | 7(2.3) | |||||
| SUAP4 | 11(3.9) | 6(3.3) | 7(1.7) | 8(3.6) | 5(2.2) | 11(2.6) | 9(3.4) | 11(2.5) | 4(2.2) | 5(1.8) | 9(2.4) | 3(2.4) | 15(2.6) | 9(3) | |||||
| Health Cen | 33(11.8) | 18(9.9) | 57(13.6) | 21(9.5) | 27(11.6) | 60(14.1) | 27(10.1) | 57(13.1) | 24(13.5) | 11(4) | 42(11) | 18(14.5) | 83(14.4) | 25(8.3) | |||||
| 061 | 18(6.5) | 5(2.7) | 5(1.2) | 17(8.6) | 6(2.6) | 5(1.2) | 14(5.2) | 13(3) | 1(0.6) | 31(11.4) | 6(1.6) | 2(1.6) | 18(3.1) | 10(3.3) | |||||
| COVID UCI | 9(2.2) | 16(8.8) | 48(11.5) | 19(8.6) | 12(5.2) | 42(9.8) | 23(8.6) | 33(7.6) | 17(9.6) | 15(5.5) | 31(8.1) | 14(11.3) | 46(8) | 27(8.9) | |||||
| Nurs home | 6(2.2) | 10(5.5) | 12(2.9) | 7(3.2) | 9(3.9) | 12(2.8) | 7(2.6) | 17(3.9) | 4(2.2) | 23(8.4) | 11(2.9) | 2(1.6) | 20(3.5) | 8(2.6) | |||||
| SHIFTS | |||||||||||||||||||
| Rotating | 136(48.2) | 93(50.8) | 278(65.6) | 116(52.9) | 127(54) | 264(61.3) | 153(56.5) | 246(55.9) | 108(60.7) | 57(54.3) | 144(52.4) | 229(59.8) | 353(60.3) | 154(50.7) | |||||
| 12 hours | 47(16.7) | 32(17.5) | 52(12.3) | ⁎⁎0.7 | 34(15.2) | 38(16.2) | 59(13.7) | ⁎⁎0.9 | 36(13.3) | 69(15.7) | 26(14.6) | ⁎⁎0.9 | 8(7.6) | 45(16.4) | 58(15.1) | ⁎⁎0.9 | 77(13.2) | 54(17.8) | ⁎⁎1.2 |
| Fixed M/A5 | 71(25.2) | 44(24) | 86(20.3) | 0.000* | 48(21.5) | 58(24.7) | 95(22) | 0.004* | 58(21.4) | 103(23.4) | 40(22.5) | 0.122 | 33(31.4) | 61(22.2) | 79(20.6) | 0.013* | 126(21.5) | 75(24.7) | 0.078 |
| 24 hours | 22(7.8) | 9(4.9) | 7(1.7) | 20(9) | 9(3.8) | 9(2.1) | 17(6.3) | 19(4.3) | 2(1.1) | 5(4.8) | 21(7.6) | 11(2.9) | 22(3.8) | 16(5.3) | |||||
| Fixed night | 6(2.1) | 5(2.7) | 1(0.2) | 5(2.2) | 3(1.3) | 4(0.9) | 7(2.6) | 3(0.7) | 2(16.7) | 2(1.9) | 4(1.5) | 6(1.6) | 7(1.2) | 5(1.6) | |||||
| COVID-At6 | |||||||||||||||||||
| No | 101(35.7) | 34(18.7) | 78(18.4) | 66(29.5) | 54(23) | 93(2.6) | ⁎⁎1.2 | 64(23.6) | 121(27.6) | 28(15.6) | 63(22.9) | 82(21.4) | 18(14.4) | ⁎⁎1.8 | 135(23.1) | 78(25.6) | |||
| Yes, daily | 66(23.3) | 72(39.6) | 183(43.2) | ⁎⁎1.8 | 77(34.4) | 82(34.9) | 62(37.7) | 0.229 | 8(36.2) | 158(36) | 65(36.3) | ⁎⁎1.9 | 93(33.8) | 159(41.4) | 8(38.4) | 0.000* | 217(37.2) | 104(34.1) | ⁎⁎0.9 |
| Yes, once a week | 116(41) | 76(41.8) | 163(38.4) | 0.000* | 81(36.2) | 99(42.1) | 175(40.7) | 109(40.2) | 160(36.4) | 86(24.2) | 0.018* | 119(43.3) | 143(37.2) | 59(47.2) | 232(39.8) | 123(40.3) | 0.594 | ||
| COVID EXPERIENCE | |||||||||||||||||||
| 0-2 months | 48(26.7) | 36(24.2) | 77(22.3) | ⁎⁎0.6 | 40(24.4) | 43(24.6) | 78(23.3) | ⁎⁎0.8 | 44(21.2) | 81(25.4) | 36(24.5) | ⁎⁎0.5 | 46(23) | 68(22.2) | 26(25.7) | ⁎⁎0.6 | 111(24.4) | 50(22.8) | ⁎⁎1.4 |
| 3-4 months | 13(7.2) | 15(10.1) | 37(10.7) | 0.822 | 12(7.3) | 20(11.4) | 33(9.9) | 0.738 | 18(8.7) | 27(8.5) | 20(13.6) | 0.514 | 23(11.5) | 27(8.8) | 7(6.9) | 0.459 | 45(9.9) | 20(9.1) | 0.526 |
| 5-7 months | 12(6.7) | 15(10.1) | 270(7.8) | 10(6.1) | 15(8.6) | 29(8.7) | 15(7.2) | 28(8.8) | 11(7.5) | 20(10) | 21(6.9) | 11(10.9) | 31(6.8) | 23(10.5) | |||||
| 8-10 months | 16(8.9) | 12(8.1) | 35(10.1) | 13(7.9) | 14/8) | 36(10.7) | 17(8.2) | 33(10.3) | 13(8.8) | 17(8.5) | 30(9.8) | 12(11.9) | 45(9.9) | 18(8.2) | |||||
| + 10 months | 91(50.6) | 71(47.7) | 169(49.0) | 89(54.3) | 83(47.4) | 159(47.5) | 114(54.8) | 150(47) | 67(45.6) | 94(47) | 160(52.3) | 45(44.6) | 223(49) | 108(49.3) | |||||
Note.
COVID Centre
Operation room
Hospitalisation Units COVID-19
Primary Care Emergency Service (SUAP)
Fixed Morning/Afternoon;
Direct care of COVID patients.
P value for chi square
OR: odds ratio
Regarding factors related to the pandemic, 76% (n = 676) of the nurses had contact with COVID-19 patients daily or at least once a week. Some 18.3% (n = 161) had to change units or services to serve COVID-19 patients; this affected work days, vacations, leave and time off in 62.2% (n = 555) of the respondents, and 495 of the nurses had to increase their weekly working hours (55.7%).
A total of 75.6% (n = 674) had experience in COVID-19 units; 49.1% (n = 331) had been caring for COVID-19 patients for more than 10 months, and 80.6% had performed two or more PCR tests at the time of the study.
A total of 152 of the nurses had contracted COVID-19 (16.9%); of these, 66.9% had to self-isolate for 11 to 30 days. A total of 50.3% (n = 76) suffered after-effects, including muscular conditions, loss of strength, headaches, loss of smell and taste and lung involvement. For 85.4% (n = 65), the after-effects were less severe, but they were persistent in 60.2% (n = 46) of the cases.
Regarding time off work for isolation because of COVID-19, 24.9% (n = 222) were quarantined due to close contact with other professionals, and 39.5% (n = 352) were quarantined due to relatives who were positive for COVID-19. A total of 27.5% (n = 73) had to be quarantined two or more times. A total of 5.5% (n = 47) of the nurses had to leave their family home due to risk of infection, and another 5.5% (n = 47) did not do so due to lack of means but felt that they should have.
Regarding the resources and management of the pandemic, 72.9% (n = 639) of the nurses reported having had a shortage of personal protective equipment (PPE) at the beginning of the pandemic, a factor that is currently not a general issue. A total of 94.2% (n = 835) of the nurses were very concerned about the pandemic situation, compared with only 68.1% (606) of their relatives. A total of 78.4% (n = 693) admitted that they felt there was an excessive amount of information about the COVID-19 in the media.
Regarding vaccination, as of 20 March 2021, 84.1% (n = 749) had been vaccinated, with 89.3% (n = 679) receiving the Pfizer vaccine. A total of 51.6% (n = 351) were indifferent regarding which vaccine they would receive, but the majority would have chosen Pfizer because of the results of published studies. The most common side effect was headache, and in some cases, local pain, malaise, low-grade fever and chills were common. A total of 90.9% (n = 801) considered vaccination indispensable to reduce the incidence of infection and protect their patients. It is noteworthy that 15.1% (n = 128) of the nurses had doubts about being vaccinated due to uncertainty about the efficacy, and 18.6% (n = 158) had doubts related to the fear of secondary reactions. The vaccine did not provide a sense of security against the risk of infection in 22.1% (n = 172) of the nurses.
At the time of the survey, only 5.6% (n = 49) of the nurses were receiving psychological support, although 23.5% (n = 205) believed that they needed it, and 36.7% (n = 320) thought that they would need it in future.
A total of 54.8% (n = 488) and 23.8% (n = 212) were partially or not satisfied, respectively, with the management of the pandemic by their health centre: 58% (n = 517) felt that the restriction measures were taken too late, and 98.7% identified this delay as the main cause of contagion.
3.2. Emotional impact and mental health of nurses
3.2.1. Burnout
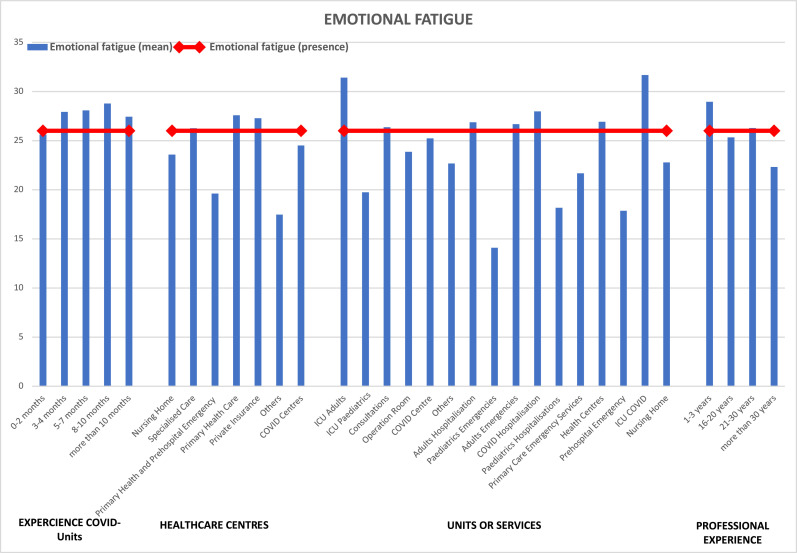
COVID-19 hospitalisation nurses had high levels of emotional fatigue according to the Maslach Burnout Inventory-MBI-HSS scale (mean = 27.97; p < 0.001). This figure was even higher in nurses working in the COVID-19 ICU, who had a mean score of 31.67 (p < 0.001). According to the risk estimation analysis, COVID-19 units nurses were 1.9 (OR; p < 0.001) times more likely to experience fatigue than nurses in non-COVID-19 units.
The results show statistically significant variations in emotional fatigue according to the unit, years of professional experience, health centre and experience in COVID-19 units (p < 0.001; F ANOVA, chi square).
The findings indicated that after 2 months of working in units with COVID-19 patients, nurses began to experience emotional fatigue, which increased over the course of month. The greatest emotional fatigue occurred among nurses in specialised care, primary care and private care.
The high fatigue values noted among nurses working in the adult ICU and in ICUs with COVID-19 patients are of concern; they exceeded the mean of 31 points out of 26, which is the detection cutoff for fatigue. However, nurses in adult emergency units, adult hospitalisation and COVID-19 units and health centres also had high fatigue values. We should also highlight that nurses in the lowest and middle ranges of professional experience were the most affected by fatigue ( Fig. 1).
Fig. 1.
Mean emotional fatigue by unit, age, experience, and health centre.
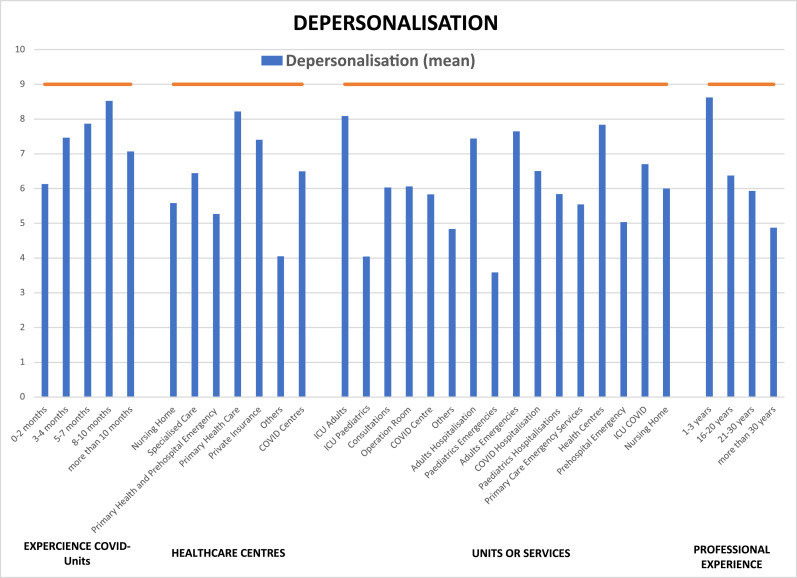
There was no evidence of depersonalisation of patients by nurses in any case, including by unit or centre, age or professional experience. Nonetheless, in some cases, the nurses approached 9 points on average, a value that indicates the emergence of depersonalisation ( Fig. 2).
Fig. 2.
Mean depersonalisation by unit, age, experience, and health centre.
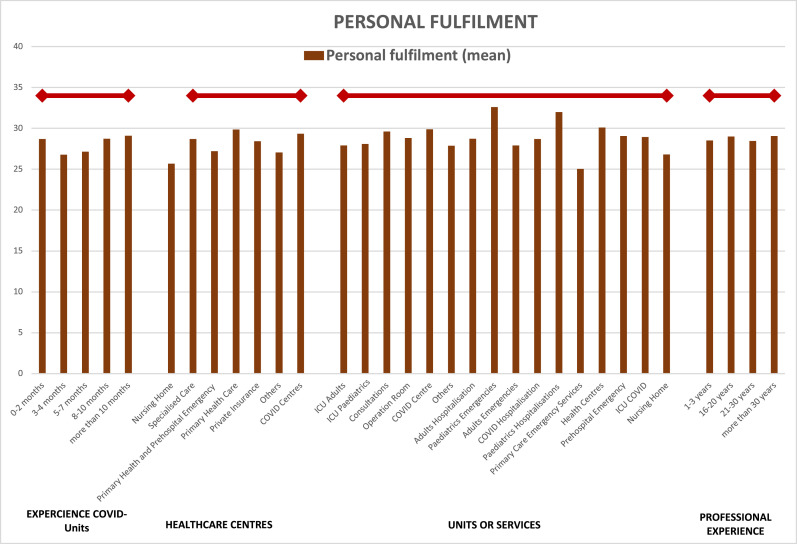
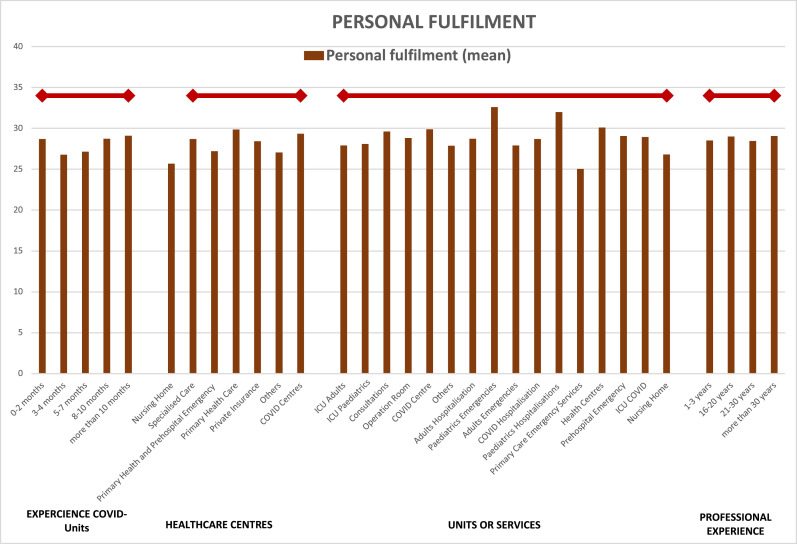
Regardless of the nurses’ unit, centre and experience, the average values for personal fulfilment were below 34 points, and the association was statistically significant (p < 0.05; Fig. 3).
Fig. 3.
Average personal fulfilment by unit, age, experience, and health centre.
3.2.2. Anxiety
Anxiety symptoms were present according to the Hospital Anxiety and Depression Scale (HADS) scale (mean = 11.24; p = 0.013). A 1.5 (OR; p = 0.021) additional risk of anxiety was associated with working in COVID-19 units.
The emergence of clear symptoms of anxiety in nurses who had been working in COVID-19 units for more than two months stood out. High average levels of anxiety were observed in nursing home and primary care professionals for all years of professional experience except the 16-20 year range. Although there were no disaggregated mean symptoms of depression, the values were within the range of possible symptoms in all cases ( Fig. 4).
Fig. 4.
Mean anxiety and depression by unit, age, experience, and health centre.
3.2.3. Post-traumatic stress
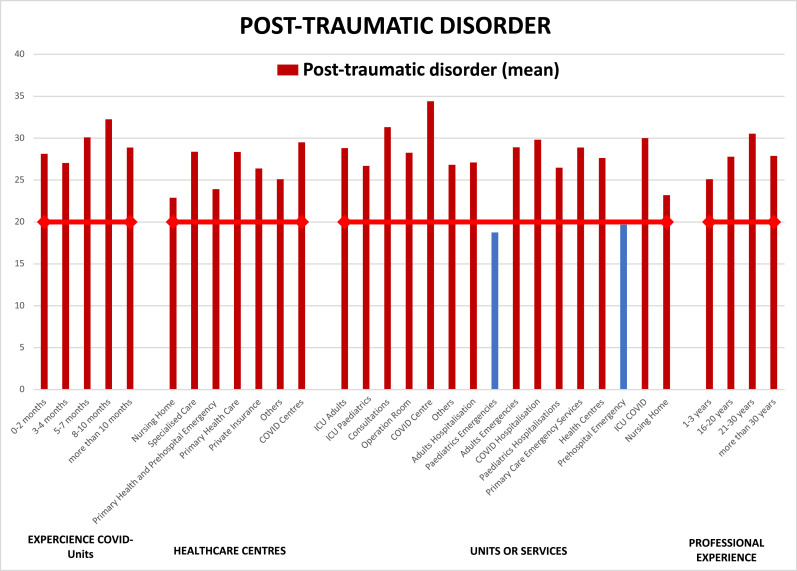
The presence of moderate post-traumatic stress disorder in among nurses who worked with hospitalised COVID-19 patients (mean of 29.82; p = 0.027) and levels of post-traumatic stress disorder that approached severe in nurses who worked in the ICU mean of 30.01 points; p = 0.027) was evidenced by scores on the Impact of Event Scale–Revised (IES-R).
The existence of post-traumatic stress disorder related to the pandemic or deaths of patients by COVID-19 among nurses who worked in all units and at health centres, those with all durations of experience with COVID-19 patients and all levels of experience was confirmed. More than 49% (n = 443) of the nurses had moderate post-traumatic stress disorder ( Fig. 5).
Fig. 5.
Mean post-traumatic stress by unit, age, experience, and health centre.
These results are shown in Tables 1 and 2 .
Table 2.
Comparison of means between scales and demographic variables.
| Emotional fatigue | Depersonalisation | Personal fulfilment | Anxiety | Depression | Post-traumatic stress | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean | SD | p value | N | Mean | SD | p value | N | Mean | SD | p value | N | Mean | SD | p value | N | Mean | SD | p value | N | Mean | SD | p value | |
| Experience in COVID units | ||||||||||||||||||||||||
| 0-2 months | 161 | 25.60 | 13.80 | 0.000a | 161 | 6.13 | 6.03 | 0.000a | 161 | 28.69 | 8.47 | 0.232 | 161 | 10.86 | 4.76 | 0.218 | 161 | 9.05 | 2.38 | 0.283 | 161 | 28.13 | 14.94 | 0.001a |
| 3-4 months | 65 | 27.92 | 11.50 | 65 | 7.46 | 6.30 | 65 | 26.78 | 7.12 | 65 | 11.03 | 3.67 | 65 | 9.05 | 2.13 | 65 | 27.03 | 13.98 | ||||||
| 5-7 months | 54 | 28.07 | 12.00 | 54 | 7.87 | 5.29 | 54 | 27.13 | 8.21 | 54 | 11.11 | 4.20 | 54 | 9.11 | 2.77 | 54 | 30.09 | 13.53 | ||||||
| 8-10 months | 63 | 28.78 | 14.20 | 63 | 8.52 | 7.03 | 63 | 28.71 | 8.60 | 63 | 11.68 | 4.93 | 63 | 8.71 | 2.25 | 63 | 32.25 | 14.28 | ||||||
| More than 10 months | 331 | 27.43 | 13.60 | 331 | 7.07 | 6.20 | 331 | 29.08 | 6.97 | 331 | 10.60 | 4.37 | 331 | 8.67 | 2.17 | 331 | 28.89 | 13.91 | ||||||
| Total | 674 | 25.88 | 13.60 | 674 | 6.62 | 5.94 | 674 | 28.64 | 7.83 | 674 | 10.69 | 4.39 | 674 | 8.74 | 2.23 | 674 | 27.80 | 14.60 | ||||||
| Type of health centre | ||||||||||||||||||||||||
| Nursing home | 19 | 23.58 | 9.10 | 0.001a | 19 | 5.58 | 5.43 | 0.009a | 19 | 25.68 | 9.14 | 0.23 | 19 | 11.37 | 3.74 | 0.019a | 19 | 8.79 | 1.78 | 0.087 | 19 | 22.89 | 15.97 | 0.207 |
| Specialised | 601 | 26.26 | 13.40 | 601 | 6.45 | 5.89 | 601 | 28.69 | 7.65 | 601 | 10.67 | 4.38 | 601 | 8.77 | 2.21 | 601 | 28.38 | 14.32 | ||||||
| PC emergency and prehospital | 52 | 19.62 | 13.20 | 52 | 5.27 | 5.38 | 52 | 27.21 | 10.48 | 52 | 8.83 | 4.54 | 52 | 7.83 | 2.35 | 52 | 23.92 | 14.28 | ||||||
| Primary care | 113 | 27.58 | 14.10 | 113 | 8.22 | 6.74 | 113 | 29.86 | 7.48 | 113 | 11.62 | 4.32 | 113 | 8.96 | 2.18 | 113 | 28.35 | 15.88 | ||||||
| Private | 75 | 27.28 | 12.80 | 75 | 7.40 | 5.68 | 75 | 28.43 | 7.19 | 75 | 10.57 | 4.35 | 75 | 8.71 | 2.35 | 75 | 26.39 | 14.73 | ||||||
| Other | 19 | 17.47 | 14.80 | 19 | 4.05 | 4.18 | 19 | 27.05 | 9.43 | 19 | 10.37 | 4.36 | 19 | 8.53 | 2.52 | 19 | 25.11 | 15.38 | ||||||
| COVID centre | 12 | 24.50 | 25.80 | 12 | 6.50 | 3.29 | 12 | 29.33 | 5.05 | 12 | 10.50 | 3.42 | 12 | 9.33 | 1.92 | 12 | 29.50 | 10.32 | ||||||
| Total | 891 | 25.85 | 13.40 | 891 | 6.61 | 5.93 | 891 | 28.64 | 7.84 | 891 | 10.68 | 4.38 | 891 | 8.74 | 2.23 | 891 | 27.78 | 14.59 | ||||||
| Units/services | ||||||||||||||||||||||||
| ICU adult | 59 | 31.41 | 12.10 | 0.000a | 59 | 8.08 | 5.45 | 0.003a | 59 | 27.92 | 7.21 | 0.143 | 59 | 11.02 | 4.13 | 0.013a | 59 | 8.88 | 2.36 | 0.258 | 59 | 28.81 | 12.85 | 0.027a |
| ICU/REA paed/neonatal | 22 | 19.73 | 12.50 | 22 | 4.05 | 4.73 | 22 | 28.09 | 6.47 | 22 | 10.77 | 3.89 | 22 | 9.27 | 2.62 | 22 | 26.68 | 14.40 | ||||||
| Consultation | 36 | 26.36 | 14.70 | 36 | 6.03 | 6.35 | 36 | 29.61 | 7.79 | 36 | 11.28 | 4.95 | 36 | 9.17 | 2.57 | 36 | 31.31 | 15.09 | ||||||
| Operating room | 48 | 23.85 | 13.40 | 48 | 6.06 | 5.68 | 48 | 28.81 | 7.88 | 48 | 11.06 | 4.42 | 48 | 8.67 | 1.91 | 48 | 28.25 | 12.95 | ||||||
| COVID centre | 18 | 25.22 | 10.20 | 18 | 5.83 | 4.59 | 18 | 29.89 | 6.48 | 18 | 11.11 | 3.39 | 18 | 9.00 | 2.14 | 18 | 34.39 | 11.53 | ||||||
| Other | 91 | 22.67 | 13.40 | 91 | 4.84 | 5.10 | 91 | 27.88 | 8.70 | 91 | 10.35 | 4.61 | 91 | 8.81 | 2.35 | 91 | 26.82 | 16.04 | ||||||
| Hosp adult | 153 | 26.86 | 13.40 | 153 | 7.44 | 6.48 | 153 | 28.73 | 7.66 | 153 | 10.94 | 4.57 | 153 | 8.80 | 2.03 | 153 | 27.11 | 15.20 | ||||||
| Ped emergency | 12 | 14.08 | 11.60 | 12 | 3.58 | 3.48 | 12 | 32.58 | 8.01 | 12 | 7.50 | 3.97 | 12 | 8.75 | 1.60 | 12 | 18.75 | 14.25 | ||||||
| Adult emergency | 88 | 26.67 | 13.40 | 88 | 7.65 | 6.38 | 88 | 27.91 | 6.60 | 88 | 10.20 | 3.71 | 88 | 8.63 | 2.10 | 88 | 28.90 | 13.64 | ||||||
| COVID hospitalisation | 73 | 27.97 | 12.30 | 73 | 6.51 | 5.48 | 73 | 28.71 | 6.63 | 73 | 11.25 | 4.21 | 73 | 8.49 | 2.14 | 73 | 29.82 | 10.97 | ||||||
| Ped hospitalisation | 19 | 18.16 | 14.00 | 19 | 5.84 | 5.81 | 19 | 32.00 | 7.05 | 19 | 9.32 | 4.32 | 19 | 8.42 | 1.71 | 19 | 26.47 | 17.13 | ||||||
| SUAP | 24 | 21.67 | 13.70 | 24 | 5.54 | 6.15 | 24 | 25.04 | 10.72 | 24 | 10.13 | 4.34 | 24 | 8.46 | 2.41 | 24 | 28.88 | 13.95 | ||||||
| Health centre | 108 | 26.92 | 14.30 | 108 | 7.83 | 6.66 | 108 | 30.09 | 7.43 | 108 | 11.38 | 4.28 | 108 | 8.91 | 2.19 | 108 | 27.63 | 16.00 | ||||||
| 0-61 | 28 | 17.86 | 12.70 | 28 | 5.04 | 4.73 | 28 | 29.07 | 10.10 | 28 | 7.71 | 4.50 | 28 | 7.29 | 2.19 | 28 | 19.68 | 13.37 | ||||||
| COVID ICU | 73 | 31.67 | 11.50 | 73 | 6.70 | 5.39 | 73 | 28.95 | 7.57 | 73 | 11.01 | 4.76 | 73 | 8.90 | 2.77 | 73 | 30.01 | 14.15 | ||||||
| Residence | 28 | 22.79 | 10.10 | 28 | 6.00 | 5.89 | 28 | 26.82 | 8.63 | 28 | 10.64 | 3.74 | 28 | 8.68 | 1.93 | 28 | 23.21 | 15.70 | ||||||
| Total | 880 | 25.90 | 10.13 | 880 | 6.63 | 5.95 | 880 | 28.71 | 7.74 | 880 | 10.70 | 4.38 | 880 | 8.74 | 2.23 | 880 | 27.84 | 14.55 | ||||||
| Professional experience | ||||||||||||||||||||||||
| 0-12 months | 13 | 28.15 | 10.10 | 0.085 | 13 | 10.85 | 5.27 | 0.000a | 13 | 28.54 | 5.47 | 0.397 | 13 | 13.08 | 3.93 | 0.023a | 13 | 9.38 | 2.93 | 0.008a | 13 | 32.15 | 10.07 | 0.007a |
| 1-3 years | 64 | 28.95 | 12.40 | 64 | 8.63 | 6.88 | 64 | 28.50 | 7.10 | 64 | 11.16 | 4.39 | 64 | 9.23 | 1.95 | 64 | 25.11 | 14.05 | ||||||
| 4-6 years | 108 | 28.51 | 12.80 | 108 | 9.66 | 6.09 | 108 | 26.79 | 7.32 | 108 | 11.55 | 3.82 | 108 | 9.24 | 2.02 | 108 | 29.45 | 12.75 | ||||||
| 7-8 years | 46 | 23.87 | 15.00 | 46 | 6.20 | 6.40 | 46 | 29.24 | 6.94 | 46 | 9.43 | 4.06 | 46 | 8.83 | 2.11 | 46 | 22.67 | 15.89 | ||||||
| 9-10 years | 48 | 26.27 | 12.80 | 48 | 6.04 | 4.44 | 48 | 28.08 | 7.64 | 48 | 11.04 | 4.21 | 48 | 9.19 | 2.41 | 48 | 28.75 | 14.59 | ||||||
| 11-15 years | 194 | 25.01 | 194 | 5.70 | 5.11 | 194 | 29.39 | 7.11 | 194 | 10.02 | 4.37 | 194 | 8.42 | 2.25 | 194 | 25.78 | 14.98 | |||||||
| 16-20 years | 172 | 25.34 | 12.90 | 172 | 6.37 | 6.07 | 172 | 28.99 | 8.78 | 172 | 10.38 | 4.90 | 172 | 8.63 | 4.90 | 172 | 27.78 | 14.66 | ||||||
| 21-30 years | 180 | 26.28 | 14.60 | 180 | 5.93 | 5.96 | 180 | 28.47 | 8.02 | 180 | 10.98 | 4.34 | 180 | 8.78 | 4.34 | 180 | 30.54 | 15.10 | ||||||
| More than 30 years | 65 | 22.31 | 13.40 | 65 | 4.88 | 5.08 | 65 | 29.06 | 9.23 | 65 | 11.02 | 4.13 | 65 | 8.06 | 4.13 | 65 | 27.88 | 13.68 | ||||||
| Total | 890 | 25.88 | 13.40 | 890 | 6.62 | 5.94 | 890 | 28.64 | 7.83 | 890 | 10.69 | 4.39 | 890 | 10.69 | 4.39 | 890 | 27.80 | 14.60 | ||||||
| Age | ||||||||||||||||||||||||
| 18-28 years | 116 | 29.63 | 11.90 | 0.018a | 116 | 10.16 | 6.50 | 0.000a | 116 | 26.87 | 6.74 | 0.075 | 116 | 11.69 | 3.95 | 0.013a | 116 | 9.43 | 2.14 | 0.003a | 116 | 27.86 | 12.63 | 0.015a |
| 29-38 years | 301 | 25.80 | 13.40 | 301 | 6.63 | 5.53 | 301 | 28.78 | 7.29 | 301 | 10.35 | 4.49 | 301 | 8.77 | 2.35 | 301 | 26.00 | 14.73 | ||||||
| 39-48 years | 313 | 25.27 | 13.70 | 313 | 6.11 | 5.86 | 313 | 29.05 | 7.88 | 313 | 10.37 | 4.34 | 313 | 8.63 | 2.04 | 313 | 27.89 | 14.45 | ||||||
| 49-58 years | 122 | 25.32 | 13.60 | 122 | 5.37 | 5.82 | 122 | 28.56 | 9.06 | 122 | 11.34 | 4.51 | 122 | 8.53 | 2.32 | 122 | 31.16 | 16.45 | ||||||
| 59-66 years | 38 | 22.84 | 14.20 | 38 | 4.32 | 4.07 | 38 | 30.24 | 9.81 | 38 | 11.16 | 4.41 | 38 | 8.13 | 2.47 | 38 | 30.42 | 12.84 | ||||||
| Total | 890 | 25.92 | 13.43 | 890 | 6.64 | 5.94 | 890 | 28.66 | 7.83 | 890 | 10.70 | 4.39 | 890 | 8.75 | 2.23 | 890 | 27.80 | 14.62 | ||||||
| Shift | ||||||||||||||||||||||||
| 12 hours | 131 | 24.63 | 13.20 | 0.000a | 131 | 6.43 | 5.58 | 0.012a | 131 | 29.07 | 7.16 | 0.006a | 131 | 10.48 | 4.38 | 0.001a | 131 | 8.74 | 2.12 | 0.001a | 131 | 28.68 | 13.71 | 0.021a |
| 24 hours | 38 | 18.34 | 12.10 | 38 | 4.74 | 4.63 | 38 | 25.74 | 11.94 | 38 | 7.84 | 4.14 | 38 | 7.50 | 2.01 | 38 | 20.89 | 12.69 | ||||||
| Fixed morning | 190 | 23.91 | 13.20 | 190 | 5.71 | 5.62 | 190 | 30.16 | 7.57 | 190 | 10.52 | 4.33 | 190 | 8.66 | 2.23 | 190 | 26.18 | 15.44 | ||||||
| Fixed night | 12 | 16.50 | 13.00 | 12 | 5.83 | 6.19 | 12 | 32.08 | 6.93 | 12 | 9.17 | 3.30 | 12 | 7.75 | 2.01 | 12 | 24.50 | 12.74 | ||||||
| Fixed afternoon | 11 | 27.27 | 15.10 | 11 | 9.55 | 5.87 | 11 | 26.82 | 9.59 | 11 | 12.82 | 4.90 | 11 | 10.09 | 2.98 | 11 | 31.64 | 17.44 | ||||||
| Rotating | 507 | 27.65 | 13.30 | 507 | 7.14 | 6.17 | 507 | 28.12 | 7.60 | 507 | 11.01 | 4.36 | 507 | 8.85 | 2.23 | 507 | 28.67 | 14.51 | ||||||
| Total | 889 | 25.88 | 13.50 | 889 | 6.62 | 5.94 | 889 | 28.64 | 7.83 | 889 | 10.69 | 4.39 | 889 | 8.74 | 2.23 | 889 | 27.80 | 14.60 | ||||||
| Increase in working hours | ||||||||||||||||||||||||
| No | 393 | 22.64 | 13.20 | 0.000a | 393 | 5.42 | 5.21 | 0.000a | 393 | 29.23 | 8.24 | 0.119 | 393 | 9.84 | 4.32 | 0.000a | 393 | 8.39 | 2.13 | 0.000a | 393 | 25.08 | 14.70 | 0.000a |
| Yes, to cover leave due to COVID-19 | 246 | 27.75 | 12.90 | 246 | 7.40 | 6.28 | 246 | 28.63 | 7.35 | 246 | 11.35 | 4.47 | 246 | 9.02 | 2.07 | 246 | 29.23 | 14.50 | ||||||
| Yes, due to lack of personnel | 249 | 29.78 | 13.10 | 249 | 7.80 | 6.35 | 249 | 27.78 | 7.57 | 249 | 11.45 | 4.15 | 249 | 9.03 | 2.39 | 249 | 30.96 | 13.65 | ||||||
| Total | 888 | 25.88 | 13.40 | 888 | 6.62 | 5.94 | 888 | 28.64 | 7.83 | 888 | 10.69 | 4.39 | 888 | 8.74 | 2.23 | 888 | 27.80 | 14.60 | ||||||
Abbreviations: SUAP = Primary Care Emergency Service; REA = Recovery and Anaesthetic Room.
aStatistically significant according to the F of ANOVA.
3.3. Predictive regression models and correlations between scales
All of the scales were significantly correlated (p < 0.001), with strong positive correlations between emotional fatigue and anxiety (r = .680; p < 0.001) and post-traumatic stress (r = .623; p < 0.001) and anxiety and stress (r = .714; p < 0.001), as shown in Table 3 .
Table 3.
Correlations between the burnout, anxiety, depression, and post-traumatic stress scales.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|
| 1 | Emotional fatigue | - | |||||
| 2 | Depersonalisation | .559a | - | ||||
| 3 | Personal fulfilment | -.318a | -.236a | - | |||
| 4 | Anxiety | .680a | .420a | -.339a | - | ||
| 5 | Depression | .497a | .330a | -.220a | .558a | - | |
| 6 | Post-traumatic disorder | .623a | .388a | -.249a | .714a | .558a | - |
p < 0.01 (two tailed).
There were significant relationships between age and depersonalisation, depression and post-traumatic stress; between COVID-19 unit and emotional fatigue and low personal fulfilment; between primary care and low personal fulfilment and anxiety; and between specialised COVID-19 care and emotional fatigue. In addition, months of experience caring for COVID-19 patients and direct contact with these patients were correlated with emotional fatigue, anxiety and post-traumatic stress. The latter was also related to being positive for COVID-19 (Table 4 )
Table 4.
Binary regression models for demographic variables, unit, and COVID-19.
| Dependent variable | Predictor variable | B | SE | Exp (β) | Wald/t | p |
|---|---|---|---|---|---|---|
| Age | (Constant) | .745 | .283 | 2.106 | 6.933 | 0.008 |
| Depersonalisation | -.053 | .013 | .931 | 28.485 | 0.000 | |
| Depression | -.116 | 0.036 | -.890 | 10.388 | 0.000 | |
| Post-traumatic stress | 0.032 | 0.006 | 1.032 | 29.977 | 0.000 | |
| Model statistics: Cox and Snell R2 = 0.059; Nagelkerke's R2 = 0.079; chi-square = 54.205; df = 3; p < 0.001b | ||||||
| COVID-19 unit | (Constant) | -1.945 | .389 | .143 | 24.973 | 0.000 |
| Emotional fatigue | .021 | 0.006 | 1.022 | 13.832 | 0.000 | |
| Personal fulfilment | .025 | .010 | 1.025 | 5.934 | 0.000 | |
| Model statistics: Cox and Snell R2 = 0.018; Nagelkerke's R2 = 0.024; chi-square = 15.669; df = 2; p < 0.001b | ||||||
| Primary care | (Constant) | 4.231 | 1.025 | 17.041 | 0.000 | |
| Personal fulfilment | -.046 | .016 | .955 | 8.547 | 0.003 | |
| Anxiety | -.084 | .037 | .920 | 5.139 | 0.023 | |
| Model statistics: Cox and Snell R2 = 0.020; Nagelkerke's R2 = 0.088; chi-square = 17.60; df = 7; p < 0.014a | ||||||
| COVID-19 specialisation | (Constant) | 33.039 | 2.296 | 14.38 | 0.000 | |
| Emotional fatigue | -3.261 | 1.253 | -1.0 | -2.602 | 0.009 | |
| Model statistic: R2 = 0.01; adjusted R2 = 0.009; F (6.772); p < 0.009a | ||||||
| Experience with direct care for COVID-19 patients | (Constant) | -.632 | .207 | .531 | 9.354 | 0.002 |
| Emotional fatigue | -.039 | .009 | 0.962 | 20.496 | 0.000 | |
| Anxiety | .096 | .029 | 1.101 | 10.985 | 0.001 | |
| Post-traumatic stress | -.021 | .008 | .979 | 6.994 | 0.008 | |
| Model statistic: R2 = 0.044; Nagelkerke's R2 = 0.065; chi-square = 54.693; df = 3; p < 0.001b | ||||||
| Contact with COVID-19 patients | (Constant) | .544 | .209 | 1.724 | 6.779 | 0.009 |
| Emotional fatigue | .046 | .009 | 1.047 | 26.612 | 0.000 | |
| Anxiety | -.111 | .030 | .895 | 13.965 | 0.000 | |
| Post-traumatic stress | .026 | .008 | 01.026 | 10.138 | 0.001 | |
| Model statistic: Cox and Snell R2 = 0.060; adjusted R2 = 0.089; chi-square = 54.693; df = 3; p < 0.001b | ||||||
| COVID-19 positive | (Constant) | -1.940 | .202 | .144 | 91.967 | 0.000 |
| Post-traumatic stress | .013 | .006 | 1.013 | 4.676 | 0.031 | |
| Model statistic: Cox and Snell R2 = 0.005; Nagelkerke's R2 = 0.009; chi-square = 4.733; df = 1; p < 0.030a | ||||||
Note. B = unstandardised B coefficient or SE = standard error, Exp(β) = standardised beta coefficient, Wald or t = test statistic, R2 = coefficient of determination, p = probability value.
ap < 0.05.
bp < 0.001
The results obtained in the linear regression model predicted that emotional fatigue would decrease to 5.45 points when the duration of COVID-19 patient care was decreased by 1.24 months. Similarly, with the same reduction of care by 1.24 months, depersonalisation decreased by 1.87 points, and post-traumatic stress decreased by 4.65 points.
There was a 1.35 (OR; p < 0.001) times greater risk of experiencing post-traumatic stress among nurses who cared for COVID-19 patients or experienced the death of a COVID-19 patient compared with those who were not involved in direct care (Tables 5 and 6 ).
Table 5.
Multiple regression model of emotional fatigue, depersonalisation, personal fulfilment, anxiety, depression, and post-traumatic stress.
| Dependent variable | Independent variables | B | Std. error | Beta | t | Sig. | 95% CI | R2 | R2 adjusted | F | p | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (Constant) | 7.494 | 2.672 | 2.804 | 0.005a | 2.244 | 12.745 | 0.503 | 0.497 | 83.258 | 0.000b | ||
| Anxiety | 5.435 | 0.699 | 0.333 | 7.78 | 0.000b | 4.062 | 6.807 | |||||
| Emotional fatigue | Poststress | 4.771 | 0.647 | 0.302 | 7.37 | 0.000b | 3.499 | 6.043 | ||||
| Burnout symptoms | -6.346 | 0.931 | -0.22 | -6.815 | 0.000b | -8.176 | -4.517 | |||||
| Shift | -1.208 | 0.446 | -0.087 | -2.71 | 0.007a | -2.083 | -0.332 | |||||
| Depression | 1.94 | 0.706 | 0.103 | 2.747 | 0.006a | 0.552 | 3.328 | |||||
| Specialisation COVID | -2.66 | 1.128 | -0.076 | -2.359 | 0.019a | -4.876 | -0.445 | |||||
| Contact COVID | -2.847 | 1.17 | -0.177 | -2.433 | 0.015a | -5.144 | -0.549 | |||||
| Primary care | -2.811 | 1.398 | -0.074 | -2.011 | 0.045a | -5.555 | -0.067 | |||||
| (Constant) | 3.037 | 1.027 | 2.956 | 0.003a | 1.019 | 5.055 | 0.539 | 0.284 | 50.585 | 0.000b | ||
| Anxiety | 1.787 | 0.377 | 0.23 | 4.739 | 0.000b | 1.046 | 2.528 | |||||
| Depersonalisation | Burnout symptoms | -3.495 | 0.526 | -0.254 | -6.647 | 0.000b | -4.529 | -2.462 | ||||
| Emotional fatigue | -1.238 | 0.232 | -0.206 | -5.342 | 0.000b | -1.694 | -0.783 | |||||
| Poststress | 1.644 | 0.369 | 0.219 | 4.457 | 0.000b | 0.919 | 2.369 | |||||
| Primary care | -1.488 | 0.611 | -0.088 | -2.438 | 0.015a | -2.687 | -0.29 | |||||
| Contact COVID | 1.026 | 0.482 | 0.078 | 2.129 | 0.034a | 0.08 | 1.972 | |||||
| (Constant) | 40.624 | 1.985 | 20.464 | 0.000b | 36.72 | 44.525 | 0.47 | 0.21 | 19.982 | 0.000b | ||
| Anxiety | -1.893 | 0.489 | -0.209 | -3.87 | 0.000b | -2.854 | -0.932 | |||||
| Personal fulfilment | Poststress | -1.757 | 0.461 | -0.201 | -3.809 | 0.000b | -2.664 | -0.851 | ||||
| Emotional fatigue | 0.683 | 0.301 | 0.097 | 2.27 | 0.024a | 0.092 | 1.274 | |||||
| Contact COVID | -2.359 | 0.789 | -0.121 | -2.991 | 0.003a | -3.909 | -0.81 | |||||
| Shift | 2.087 | 0.774 | 0.112 | 2.696 | 0.007a | 0.566 | 3.608 | |||||
| Burnout symptoms | -1.491 | 0.648 | -0.093 | -2.302 | 0.022a | -2.764 | -0.218 | |||||
| DepressionCLAS | -1.117 | 0.499 | -0.106 | -2.24 | 0.026a | -2.096 | -0.137 | |||||
| Contact COVID | -0.866 | 0.343 | -0.094 | -2.527 | 0.012a | -1.539 | -0.193 | |||||
| Primary care | -1.706 | 0.806 | -0.079 | -2.118 | 0.035a | -3.288 | -0.125 | |||||
| (Constant) | -0.901 | 0.397 | -2.269 | 0.024a | -1.681 | -0.121 | 0.888 | 0.786 | 366.9 | 0.000b | ||
| Poststress | 1.478 | 0.181 | 0.284 | 8.173 | 0.000b | 1.123 | 1.834 | |||||
| Anxiety | Depression | 0.619 | 0.153 | 0.099 | 4.052 | 0.000b | 0.319 | 0.919 | ||||
| Burnout symptoms | -0.553 | 0.2 | -0.058 | -2.758 | 0.006a | -0.947 | -0.159 | |||||
| Post-traumatic stress disorder | -0.723 | 0.31 | -0.075 | -2.332 | 0.020a | -1.332 | -0.114 | |||||
| Shift | -0.542 | 0.163 | -0.127 | -3.325 | 0.001a | -0.862 | -0.222 | |||||
| Contact COVID | 0.469 | 0.195 | 0.089 | 2.41 | 0.016a | 0.087 | 0.851 | |||||
| Primary care | -0.982 | 0.472 | -0.079 | -2.081 | 0.038a | -1.908 | -0.056 | |||||
| (Constant) | 3.383 | 0.17 | 19.865 | 0.000b | 3.048 | 3.718 | 0.915 | 0.836 | 637.1 | 0.000b | ||
| Poststress | 0.384 | 0.075 | 0.15 | 5.142 | 0.000b | 0.237 | 0.531 | |||||
| Depression | Post-traumatic stress disorder | -0.324 | 0.131 | -0.069 | -2.479 | 0.014a | -0.581 | -0.067 | ||||
| Burnout symptoms | -0.195 | 0.086 | -0.042 | -2.274 | 0.023a | -0.364 | -0.027 | |||||
| Emotional fatigue | -0.233 | 0.077 | -0.112 | -3.017 | 0.003a | -0.384 | -0.081 | |||||
| Contact COVID | 0.217 | 0.097 | 0.083 | 2.247 | 0.025a | 0.027 | 0.407 | |||||
| (Constant) | -18.804 | 0.972 | -19.341 | 0.000b | -20.71 | -16.894 | 0.95 | 0.901 | 911.1 | 0.000b | ||
| Anxiety | 0.969 | 0.335 | 0.056 | 2.896 | 0.004a | 0.312 | 1.626 | |||||
| Post-traumatic stress | Emotional fatigue | 0.569 | 0.195 | 0.043 | 2.925 | 0.004a | 0.187 | 0.952 | ||||
| Depression | 0.935 | 0.337 | 0.047 | 2.777 | 0.006a | 0.273 | 1.596 | |||||
| Contact COVID | 6.644 | 1.195 | 0.204 | 5.562 | 0.000b | 4.299 | 8.99 | |||||
| Shift | -1.645 | 0.546 | -0.114 | -3.011 | 0.003a | -2.717 | -0.572 | |||||
Note. B = unstandardised B coefficient; SE = standard error, Beta = standardised beta coefficient, t = test statistic, R2 = coefficient of determination, p = probability.
p < 0.05.
p < 0.001.
Table 6.
Predictive models for the correlation between emotional fatigue, depersonalisation, and post-traumatic stress and months of experience in COVID-19 units.
| B | SD | Beta | t | p | 95% CI | R2 | F | p | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Emotional fatigue and experience in COVID-19 units | ||||||||||
| (Constant) | 32.666 | 1.36 | 24.026 | 0 | 29.997 | 35.334 | 0.03 | 27.871 | 0.000 | |
| Experience COVID months | -5.452 | 1.033 | -0.174 | -5.279 | 0 | -7.479 | -3.425 | |||
| Equation | e= 32.67-(5.452*Exp1.24 months COVID) | |||||||||
| Emotional depersonalisation and experience in COVID units | ||||||||||
| (Constant) | 8.952 | 0.604 | 14.822 | 0 | 7.767 | 10.138 | 0.018 | 16.626 | 0.000 | |
| Experience 2 months | -1.871 | 0.459 | -0.135 | -4.077 | 0 | -2.771 | -0.97 | |||
| Equation | e=8.952+(1.250*Exp1.24 monthsCOVID) | |||||||||
| Post-traumatic stress and experience in COVID units | ||||||||||
| (Constant) | 33.588 | 1.485 | 22.622 | 0 | 30.674 | 36.502 | 0.018 | 16.979 | 0.000 | |
| Experience 2 months | -4.647 | 1.128 | -0.137 | -4.121 | 0 | -6.86 | -2.434 | |||
| Equation | e=33.588-(1.250*Exp1.24 monthsCOVID) | |||||||||
4. Discussion
The main findings of this study highlight the multidimensional impact of the COVID-19 on the professional, emotional, psychological, and social environment of most of the participating nurses. Among the respondents, 76% had daily or weekly contact with COVID-19 patients, and almost 50% had treated COVID-19 patients for more than 10 months. Based on these findings, our study identified the main professional conditions and sociodemographic characteristics that institutions and nurse managers should target for intervention to reduce this impact.
Among professional factors, the nursing professionals identified that their workloads had increased and/or vacations and days off had been changed or eliminated due to COVID-19-related issues. Along these lines, more than 50% of the nursing personnel felt low or not satisfied with the health management of COVID-19, and 72% perceived a lack of resources and restrictions, mainly in the beginning of pandemic. In agreement with our data, previous studies in other demographic regions have confirmed the nurses’ perceptions of organisational barriers related to heavier workloads (Manzano García & Ayala Calvo, 2021), more working hours, lack of resources (Barello et al., 2021) and more risky and stressful environment, which were related to professional commitment (Duran, Celik, Ertugrul, Ok, & Albayrak, 2021) and burnout syndrome (Galanis, Vraka, Fragkou, Bilali, & Kaitelidou, 2021; Giménez-Espert, del, Prado-Gascó, & Soto-Rubio, 2020). Although the lack of protective resources and professional training in the management of COVID-19 patients seems to have been resolved, job demands continue to be overwhelming. This finding reflects the need for institutions and nursing leaders to prioritise the establishment of strategies for improving occupational issues in addition to providing transparent information, communication and resources for healthcare providers to protect nurses (Giménez-Espert, del, Prado-Gascó, & Soto-Rubio, 2020; Shah et al., 2021).
Given that burnout syndrome is a direct consequence of professional factors (Maslach & Leiter, 2008), we found a high level of emotional fatigue in nurses working in COVID-19 hospital wards and ICUs; the respondents had scores of more than 31 points in this burnout dimension. A score of 26 points, which is the cutoff for risky levels of emotional fatigue (Maslach et al., 1986), was reached after two months of professional contact with COVID-19 units, and the respondents’ scores continued to increase with increasing months of contact. We also observed higher emotional fatigue among nurses with lower levels of experience. Although high levels of emotional fatigue were identified in nurses before the COVID-19 pandemic, our results indicated that nurses in COVID-19 units and ICUs were 1.9 times more prone to emotional fatigue (Gómez-Urquiza et al., 2017). Before the pandemic, the prevalence high levels of emotional fatigue in nurses was already between 23 and 30%, and the highest score observed was 27 points; in contrast, we found a prevalence of more than 47% scores higher than 31 points in nurse who worked in COVID-19 units and ICUs (Gómez-Urquiza et al., 2017). A systematic review and meta-analysis just before the pandemic describing burnout among nurses confirmed that younger age and lower experience were related to burnout, as were factors related to workload and work environment. This systematic review reported data that were similar to ours regarding high levels of emotional fatigue, which had a prevalence of 34%.
In line with emotional fatigue as the core dimension and first symptom of the burnout process (Maslach & Jackson, 1981), the nurses in our study scored less than 34 points on the personal fulfilment construct. A value below 34 indicates a lack of personal fulfilment and a high risk to mental health in nurses (Lim et al., 2010). This situation was independent of age, nursing unit and experience but was closely related to work shift. Galanis et al. showed in their meta-analysis which aimed to examine the nurses' burnout and associated risk factors during the COVID-19 pandemic, that 15.2% of the total sample scored low on personal fulfilment, while in the present study, low scores were observed in 94.3% of the respondents, with 28.6 points as the average score (Galanis, Vraka, Fragkou, Bilali, & Kaitelidou, 2021). In disagreement with our results, Luceño-Moreno et al. (2020), in their study on psychosocial risks at work level and creation of the Multidimensional Questionnaire DECORE (Demand, Control, Reward), observed low personal fulfilment in 8.4% of Spanish health personnel. A major difference is that those studies took place during the first weeks of the pandemic situation, so it was not possible to assess the emotional impact due to the short time that had elapsed.
In contrast, we observed relatively positive findings for the depersonalisation dimension; none of the professionals had a high score, although some of the nurses were close to the 9-point cutoff that is considered high for this dimension. Higher values were observed in younger nurses and those with less experience, similarly to previous studies (Galanis, Vraka, Fragkou, Bilali, & Kaitelidou, 2021; Luceño-Moreno et al., 2020; Zhang et al., 2020). Although this construct did not show high levels prior in nursing professionals to the pandemic, with an 8% of prevalence (Parola et al., 2017), a meta-analysis of this dimension during COVID-19 pandemic reported a prevalence of less than 13% (Galanis, Vraka, Fragkou, Bilali, & Kaitelidou, 2021). Nurses who had contact with COVID-19 patients do not demonstrate low depersonalisation, and their levels are similar to those of professionals working in other units, such as mental health (Galanis, Vraka, Fragkou, Bilali, & Kaitelidou, 2021). Due to the frightening situation and contact with COVID-19 patients, nurses have developed consequent empathy strategies and feeling capable to emotionally connect with patients in a deeper way.
As a result of professional issues, the nurses experienced other emotional and psychological impairments, such as anxiety, depression and post-traumatic stress. In line with findings regarding the burnout dimensions, high levels of anxiety were observed after two months of continuous professional contact with COVID-19 patients, mainly among nurses at residences for the elderly and in primary care. This anxiety level diminished among professionals who had between 16 and 20 years of experience, similar to previous reports that experience was a protective factor for mental health in nurses during the COVID-19 pandemic (Galanis, Vraka, Fragkou, Bilali, & Kaitelidou, 2021). Although a high level of depression was not observed, we found values close to those indicative of risk, which could mean that subclinical or short-term depression was present in many cases.
We found moderate levels of post-traumatic stress, an especially worrying psychological impairment, among nurses due to deaths and/or other health issues related to COVID-19 patients. This result was independent of age, nursing experience and unit, and mild, moderate and high levels of post-traumatic stress were found in 35%, 43.0% and 14.1% of the respondents, respectively; in other words, 82.2% of the total sample in the present study reported some degree of post-traumatic stress. Despite these alarming results, our data contrast with results of Luceño-Moreno et al. (2020), who described symptoms of post-traumatic stress in Spanish health personnel at the very beginning of the COVID-19 pandemic. These authors reported high post-traumatic stress levels, with 56.6% of the sample showing high scores (Luceño-Moreno et al., 2020), similar to the findings of other studies that evaluated the early stages of the COVID-19 pandemic in Spain (Luo et al., 2021). In this regard, we should consider the great impact of the beginning of the COVID-19 pandemic in Spain and the possibility that post-traumatic stress decreased in subsequent months among healthcare professionals. However, no longitudinal studies of post-traumatic stress in nurses coping with COVID-19 exist to confirm this possibility.
These data offer information regarding the high risk of mental health disorders in nurses who are coping with the pandemic situation and the need to provide psychological support. We found that only 5.6% of our respondents had received psychological help, although 24% and 37% of nurses considered that they currently needed such help or felt that they would need it in the immediate future, respectively. Similarly, previous studies recommended mental health interventions for high-risk nurses and immediate access to mental health services, in addition to rest periods (Galanis, Vraka, Fragkou, Bilali, & Kaitelidou, 2021).
It is also important to highlight the social impact of the pandemic situation on nurses. In addition to those who developed COVID-19 and were placed in isolation or lockdown, 25% and 40% of the respondents were quarantined due to close contact with infected health care professionals or family members, respectively. Importantly, 5.5% of nurses reported that they had to leave their homes temporarily due to the fear of spreading the disease to family members. These issues are directly related to the development of anxiety and burnout, as previous studies have confirmed (Morgantini et al., 2020; Shreffler et al., 2020).
In general, we observed that professional contact with COVID-19 increased the risk of burnout syndrome and post-traumatic stress (by up to 1.4 times), and this risk increased after two months of continuous and direct contact. These data reflect the urgent need to establish protective strategies for nurses. Regarding immunisation as the main protective strategy, 84% of the nurses had received any type of vaccine against COVID-19, although 22% indicated that they did not feel completely safe, and 17% became sick. Nonetheless, more than 90% considered the vaccine an essential method to protect against the pandemic. This result is in line with data reported by previous studies from other European countries in which more than 94% of the sample indicated willingness to obtain the vaccine (Szmyd et al., 2021).
The parameters and characteristics that could help reduce the psychological and emotional impact of COVID-19 include breaks from caring for COVID-19 patients, reduced professional contact with COVID-19 units, emotional coping strategies, increase in breaks, days off or rotations to other units.
Considering these findings and suggestions from previous studies (Galanis, Vraka, Fragkou, Bilali, & Kaitelidou, 2021), institutions and nurse leaders should limit continuous contact with COVID-19 patients to 3-4 months to reach pre-pandemic levels at least and breaks from working with COVID-19 patients should last at least 1.2 months. Shorter periods of COVID-19 contact and breaks from COVID-19 units could diminish the psychological and emotional impact of the pandemic on nurses.
The consequent reduction in economic costs derived from reductions in sick leave and related treatments could be leveraged to augment the personnel resources and allow the incorporation of this primary strategy. Supporting our suggestions, Cunningham & Çayi (2021) evaluated the impact of brief resilience retreats on healthcare workers’ anxiety during the COVID-19 pandemic and reported reductions in anxiety scores among nurses. In this study, nurse leadership achieved well-being among nurses by offering 10 daylong retreats that promoted mindfulness practices (Cunningham & Çayir, 2021). Because greater emotional and psychological impact has been observed in professionals with less experience and younger nurses, measures to manage the impact of the COVID-19 pandemic should be reinforced in these groups.
4.1. The present study has limitations
Our sample comprised nurses in the Balearic Health System at public, private and social health centres. Although this represents a significant sample, it may differ from samples from other health systems in terms of aspects of pandemic management; however, the data regarding the emotional impact of the pandemic may be similar. There may be a response bias, with nurses who have tested positive for COVID-19 or are caring for COVID-19 patients more likely to answer the questionnaire.
5. Conclusion
In conclusion, our results confirmed the professional, psychological, emotional and social impact of the COVID-19 pandemic on nurses and identified the demographic characteristics and professional situations that increase nurses’ likelihood of being affected.
The emotional impact on nurses during the pandemic increased in those who work for more than two months in COVID-19 units, especially in the ICU, and also in those with fewer years of professional experience and who work in clinical settings of primary and specialised care.
With this information, institutions and nurse managers should establish primary strategies that recognise the importance of personal and occupational characteristics, such as adjusting work shifts, hiring temporary replacements and rotating nurses on COVID-19 units to protect nurses in similar situations or future COVID-19 waves; furthermore, psychological support strategies are urgently needed.
Author contributions
Jesús Molina-Mula: Conceptualisation, Methodology, Software, Validation, Formal analysis, Investigation, Resources, Data curation, Writing - original draft, Writing - review & editing, Visualisation, Supervision, Project administration, Funding acquisition; Antonio González-Trujillo: Methodology, Validation, Writing - original draft, Writing - review & editing; Catalina Perelló-Campaner: Writing - original draft, Writing - review & editing; Sergio Tortosa-Espínola: Conceptualisation, Investigation, Resources, Project administration, Funding acquisition; Jorge Tera-Donoso: Conceptualisation, Project administration, Funding acquisition; Litha Otero De la Rosa: Investigation, Resources, Project administration, Funding acquisition; Natalia Romero-Franco: Methodology, Validation, Writing - original draft, Writing - review & editing
Funding
Innovation and Development Center in Nursing and Physiotherapy of the Balearic Islands (SATSE-CIDEFIB).
Ethical statement
The study was reviewed by an Ethics committee who deemed approval of the ethics committee was not required because the data collected was anonymised with personally identifiable data collected according to European regulation 2016/679 and current Spanish legislation. The study has followed the code of good practice in research and the Declaration of Helsinki.
Conflict of interest
None.
Acknowledgements
We are grateful to the Center for Innovation and Development in Nursing and Physiotherapy of the Balearic Islands of SATSE Baleares for the support and dissemination of the research and to the nurses of the Balearic Islands for their involvement and commitment. To the nurses of the Balearic Islands for their commitment and dedication in times of pandemic and to Innovation and Development Center in Nursing and Physiotherapy of the Balearic Islands (SATSE-CIDEFIB) for the economic and technical support.
References
- Aguayo R., Vargas C., Emilia I., Lozano L.M. A meta-analytic reliability generalization study of the Maslach Burnout Inventory. International Journal of Clinical and Health Psychology. 2011;11(2):343–361. [Google Scholar]
- Aiken L.H., Sermeus W., Van den Heede K., Sloane D.M., Busse R., McKee M., et al. Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ. 2012;344(mar20 2):e1717. doi: 10.1136/bmj.e1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anmella G., Fico G., Roca A., Gómez-Ramiro M., Vázquez M., Murru A., et al. Unravelling potential severe psychiatric repercussions on healthcare professionals during the COVID-19 crisis. Journal of Affective Disorders. 2020;273:422–424. doi: 10.1016/j.jad.2020.05.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldonedo-Mosteiro M., Almeida M.C., dos S., Baptista P.C.P., Sánchez-Zaballos M., Rodriguez-Diaz F.J., et al. Burnout syndrome in Brazilian and Spanish nursing workers. Revista Latino-Americana de Enfermagem. 2019;27:e3192. doi: 10.1590/1518-8345.2818.3192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barello S., Caruso R., Palamenghi L., Nania T., Dellafiore F., Bonetti L., et al. Factors associated with emotional exhaustion in healthcare professionals involved in the COVID-19 pandemic: an application of the job demands-resources model. International Archives of Occupational and Environmental Health. 2021;94(8):1751–1761. doi: 10.1007/s00420-021-01669-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cañadas-de la Fuente G.A., San Luis C., Lozano L.M., Vargas C., García I., de la Fuente E.I. Evidence for factorial validity of Maslach Burnout Inventory and burnout levels among health workers. Revista Latinoamericana de Psicología. 2014;46(1):44–52. [Google Scholar]
- Costa Requena G., Gil Moncayo F.L. Propiedades psicométricas de la escala revisada del impacto del evento estresante (IES-R) en una muestra espanola de pacientes con cancer. Análisis y Modificación de Conducta. 2007;33(149):311–331. doi: 10.33776/amc.v33i149.1218. [DOI] [Google Scholar]
- Cunningham T., Çayir E. Nurse leaders employ contemplative practices to promote healthcare professional well-being and decrease anxiety. JONA: The Journal of Nursing Administration. 2021;51(3):156–161. doi: 10.1097/NNA.0000000000000987. [DOI] [PubMed] [Google Scholar]
- Duran S., Celik I., Ertugrul B., Ok S., Albayrak S. Factors affecting nurses’ professional commitment during the COVID-19 pandemic: a cross-sectional study. Journal of Nursing Management. 2021;29(7):1906–1915. doi: 10.1111/jonm.13327. jonm.13327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fornés-vives J. Estrés laboral en enfermería : un reto a combatir. Revista Española de Enfermería de Salud Mental. 2020;11:8–10. [Google Scholar]
- Fornés-Vives J., García-Banda G., Frias-Navarro D., Pascual-Soler M. Longitudinal study predicting burnout in Spanish nurses: the role of neuroticism and emotional coping. Personality and Individual Differences. 2019;138(October 2018):286–291. doi: 10.1016/j.paid.2018.10.014. [DOI] [Google Scholar]
- Galanis P., Vraka I., Fragkou D., Bilali A., Kaitelidou D. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: a systematic review and meta-analysis. Journal of Advanced Nursing. 2021;77(8):3286–3302. doi: 10.1111/jan.14839. jan.14839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giménez-Espert M., del C., Prado-Gascó V., Soto-Rubio A. Psychosocial risks, work engagement, and job satisfaction of nurses during COVID-19 pandemic. Frontiers in Public Health. 2020;8:566896. doi: 10.3389/fpubh.2020.566896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gómez-Urquiza J.L., Monsalve-Reyes C.S., San Luis-Costas C., Fernández-Castillo R., Aguayo-Estremera R., Cañadas-de la Fuente G.A. Factores de riesgo y niveles de burnout en enfermeras de atención primaria: una revisión sistemática. Atención Primaria. 2017;49(2):77–85. doi: 10.1016/j.aprim.2016.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Sanguino C., Ausín B., Castellanos M.Á., Saiz J., López-Gómez A., Ugidos C., et al. Mental health consequences during the initial stage of the 2020 coronavirus pandemic (COVID-19) in Spain. Brain, Behavior, and Immunity. 2020;87(May):172–176. doi: 10.1016/j.bbi.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutiérrez J.J.B., Arias-Herrera A. Síndrome de burnout en personal de enfermería: asociación con estresores del entorno hospitalario, Andalucía, España. Enfermería Universitaria. 2018;15(1):30–44. doi: 10.22201/eneo.23958421e.2018.1.62903. [DOI] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim N., Kim E.K., Kim H., Yang E., Lee S.M. individual and work-related factors influencing burnout of mental health professionals: a meta-analysis. Journal of Employment Counseling. 2010;47(2):86–96. doi: 10.1002/j.2161-1920.2010.tb00093.x. [DOI] [Google Scholar]
- Luceño-Moreno L., Talavera-Velasco B., García-Albuerne Y., Martín-García J. Symptoms of posttraumatic stress, anxiety, depression, levels of resilience and burnout in Spanish health personnel during the COVID-19 pandemic. International Journal of Environmental Research and Public Health. 2020;17(15):5514. doi: 10.3390/ijerph17155514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo D., Liu Q., Chen Q., Huang R., Chen P., Yang B.X., et al. Mental health status of the general public, frontline, and non-frontline healthcare providers in the early stage of COVID-19. Frontiers in Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.553021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manzano García G., Ayala Calvo J.C. The threat of COVID-19 and its influence on nursing staff burnout. Journal of Advanced Nursing. 2021;77(2):832–844. doi: 10.1111/jan.14642. [DOI] [PubMed] [Google Scholar]
- Maslach C., Jackson S.E. The measurement of experienced burnout. Journal of Organizational Behavior. 1981;2(2):99–113. doi: 10.1002/job.4030020205. [DOI] [Google Scholar]
- Maslach C., Jackson S.E., Leiter M.P., Schaufeli W.B., Schwab R.L. 3rd ed. Vol. 21. Consulting Psychologists Press; Palo Alto, CA: 1986. (Maslach burnout inventory). [Google Scholar]
- Maslach C., Leiter M.P. Early predictors of job burnout and engagement. Journal of Applied Psychology. 2008;93(3):498–512. doi: 10.1037/0021-9010.93.3.498. [DOI] [PubMed] [Google Scholar]
- Mazza C., Ricci E., Biondi S., Colasanti M., Ferracuti S., Napoli C., et al. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. International Journal of Environmental Research and Public Health. 2020;17(9):3165. doi: 10.3390/ijerph17093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mesa Castro N. Influencia De La Inteligencia Emocional Percibida En La Ansiedad Y El Estrés Laboral De Enfermería. ENE Revista de Enfermeria. 2019;13(3):1–26. [Google Scholar]
- Morgantini L.A., Naha U., Wang H., Francavilla S., Acar Ö., Flores J.M., et al. Factors contributing to healthcare professional burnout during the COVID-19 pandemic: a rapid turnaround global survey. PLoS One. 2020;15(9) doi: 10.1371/journal.pone.0238217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nowicki G.J., Ślusarska B., Tucholska K., Naylor K., Chrzan-Rodak A., Niedorys B. The severity of traumatic stress associated with covid-19 pandemic, perception of support, sense of security, and sense of meaning in life among nurses: research protocol and preliminary results from Poland. International Journal of Environmental Research and Public Health. 2020;17(18):1–18. doi: 10.3390/ijerph17186491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orgambídez-Ramos A., Borrego-Alés Y., Ruiz-Frutos C. Empowerment, vulnerabilidad al estrés y burnout en enfermeros portugueses. Ciência & Saúde Coletiva. 2018;23(1):259–266. doi: 10.1590/1413-81232018231.15522015. [DOI] [PubMed] [Google Scholar]
- Parola V., Coelho A., Cardoso D., Sandgren A., Apóstolo J. Prevalence of burnout in health professionals working in palliative care: a systematic review. JBI Database of Systematic Reviews and Implementation Reports. 2017;15(7):1905–1933. doi: 10.11124/JBISRIR-2016-003309. [DOI] [PubMed] [Google Scholar]
- Seisdedos N. TEA; MadridSpain: 1997. MBI human services. [Google Scholar]
- Shah M., Roggenkamp M., Ferrer L., Burger V., Brassil K. Mental health and COVID-19: the psychological implications of a pandemic for nurses. Clinical Journal of Oncology Nursing. 2021;25(1):69–75. doi: 10.1188/21.CJON.69-75. [DOI] [PubMed] [Google Scholar]
- Shreffler J., Huecker M., Petrey J. The impact of COVID-19 on healthcare worker wellness: a scoping review. Western Journal of Emergency Medicine. 2020;21(5):1059–1066. doi: 10.5811/westjem.2020.7.48684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szmyd B., Karuga F.F., Bartoszek A., Staniecka K., Siwecka N., Bartoszek A., et al. Attitude and behaviors towards SARS-CoV-2 vaccination among healthcare workers: a cross-sectional study from Poland. Vaccines. 2021;9(3):218. doi: 10.3390/vaccines9030218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terol Cantero M.C., López-Roig S., Rodríguez-Marín J., Martín-Aragón M., Pastor M.-Á., Reig M.T. Propiedades psicométricas de la Escala Hospitalaria de Ansiedad y Estrés (HAD) en población española. Ansiedad y Estrés. 2007;13:163–176. [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zakeri M.A., Hossini Rafsanjanipoor S.M., Zakeri M., Dehghan M. The relationship between frontline nurses’ psychosocial status, satisfaction with life and resilience during the prevalence of COVID-19 disease. Nursing Open. 2021;8(4):1829–1839. doi: 10.1002/nop2.832. January, nop2.832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zerbini G., Ebigbo A., Reicherts P., Kunz M., Messman H. Psychosocial burden of healthcare professionals in times of covid-19 – a survey conducted at the university hospital Augsburg. GMS German Medical Science. 2020;18:1–9. doi: 10.3205/000281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Wang C., Pan W., Zheng J., Gao J., Huang X., et al. Stress, burnout, and coping strategies of frontline nurses during the COVID-19 epidemic in Wuhan and Shanghai, China. Frontiers in Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.565520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zigmond A.S., Snaith R.P. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]