Abstract
Background
There is little argument that COVID-19 is potentially highly stressful for many people, however, little research has broken down COVID-19-related distress into different aspects clustering together, and how these clusters differ in terms of the vulnerability of the individuals.
Objective
The primary aim of the present study was to identify distinct profiles of individuals' reactions to COVID-19-related stress, and analyze potential differences and risk and protective factors associated with these profiles in relation to childhood abuse, psychopathology, and interpersonal relationships.
Participants and setting
Data was collected online among a convenience sample of 914 men and women in Israel.
Methods
A Latent Profile Analysis (LPA) for estimating distinct profiles in people's COVID-19-related distress was applied. Next, profiles were compared in childhood abuse, psychopathology, perceived social support and relationship satisfaction.
Results
Five distinct profiles were identified: The distressed (23.75%), the worried (38.96%), the financially and socially distressed (15.20%), the caregivers (13.65%), and the untroubled (8.44Profiles in which individuals had more COVID-19 related distress are characterized by more childhood abuse, psychopathology, and less social support and relationship satisfaction.
Conclusion
An assessment of the psychological implications of COVID-19 (when screening the population and creating prevention/intervention programs) should take into account the different responses individuals have when facing COVID-19, and their vulnerability, including their history of abuse, psychopathology, social support and relationship satisfaction, so that these programs will be better tailored to each type of distress experienced.
Keywords: COVID-19 distress, Latent Profile Analysis (LPA), Psychopathology, Childhood abuse, Relationship satisfaction, Social support
1. Introduction
In December 2019, SARS-CoV-2, the virus that causes COVID-19, appeared in Wuhan, China, expanding rapidly and affecting countries worldwide (Huang et al., 2020). Today, COVID-19 has become a global health crisis. In addition to its significant physical implications, COVID-19 has serious effects on individuals' well-being and mental health (Salari et al., 2020). As the pandemic continues to drag on, it is likely that widespread negative mental health consequences will be reported with the potential for long-lasting effects (Brooks et al., 2020; Salari et al., 2020; Serafini et al., 2020). In the present study, we sought to identify different profiles of individuals that can be distinguished by their COVID-19-related stress. Further, we wished to examine the differences between the profiles in terms of mental health, history of childhood abuse, current relationship satisfaction, and perceived social support.
1.1. COVID-19-related distress
With the outbreak of COVID-19, national polls have indicated sharp increases in fear and worries relating to the virus (Asmundson & Taylor, 2020). Although previous research has indicated that fear of COVID-19 and COVID-19-related stress are relatively common (Fitzpatrick, Harris, & Drawve, 2020; Taylor et al., 2020), research has only begun to explore the differential levels of COVID-19-related anxiety and stress (Fernández, Crivelli, Guimet, Allegri, & Pedreira, 2020; Maaravi & Heller, 2020). The current pandemic is at very least-highly stressful for most people and is likely to be traumatic for many others (Horesh & Brown, 2020). Individuals are facing increased stress, prompted by worries about their own and their loved ones' health, as well as about job security and financial hardship. However, there might be a great difference in how stressful COVID-19 is perceived by different individuals. Perceived stress pertains to the degree to which life situations are appraised as stressful (Cohen, Kamarck, & Mermelstein, 1983) and this subjective perception can further play a meaningful role in predicting post stress-exposure psychopathology (e.g., Lassri, Soffer-Dudek, Lerman, Rudich, & Shahar, 2013). The present study sought to examine who are the individuals who are the most stressed by COVID-19? In the first stage, we will analyze different aspects of COVID-19-related distress, and how they cluster together, based on individuals' reactions. In the second stage, we will examine the role of childhood abuse, psychopathology, and interpersonal relationships in the different reaction profiles to COVID-19-related distress.
1.2. The role of childhood abuse, psychopathology, and interpersonal relationships in COVID-19-related distress
The research on how survivors of childhood abuse experienced the stress in the current pandemic is scarce. In a recent study, individuals with a history of childhood abuse were found to be at higher risk for experiencing COVID-19 acute stress disorder (Tsur & Abu-Raiya, 2020). Although childhood abuse was found to directly increase COVID-19 acute stress disorder, it was also mediated by complex posttraumatic stress disorder (CPTSD; Tsur & Abu-Raiya, 2020). In the same vein, two studies found a significant association between adverse childhood experiences and poor mental health during the COVID-19 pandemic (Doom & Fox, 2020; Guo et al., 2020).
A wide range of mental health outcomes have been observed during the virus outbreak, at the individual, community, national, and international levels. The psychological disorders that have been reported during this pandemic include various symptoms of psychological trauma, such as emotional distress, depression, stress, mood swings, irritability, insomnia, attention deficit hyperactivity disorder, posttraumatic stress, and anger (Brooks et al., 2020; Salari et al., 2020; Serafini et al., 2020). Higher levels of mental health issues during the pandemic were found among individuals who had to quarantine (Jeong et al., 2016; Zhao et al., 2020), individuals living in areas with high rates of infection, and individuals who were divorced/widowed (Zhao et al., 2020), with higher risks related to being female and living alone (Kelly, 2020). Survivors of COVID-19 (Taquet, Luciano, Geddes, & Harrison, 2020), individuals with prior mental health issues (Li, Li, Fortunati, & Krystal, 2020), and people who consumed a great deal of media during the pandemic (Bendau et al., 2020; Gao et al., 2020) also appeared to be at increased risk of mental health sequelae. While the aforementioned studied contributed to the understanding of populations that are in risk for mental health problems during COVID-19, the relationship between a history of childhood abuse and mental health consequences during the COVID-19 outbreak is still uncharted territory. However, based on previous research indicating that adverse childhood experiences, including abuse experiences, have been found to predict lower mental health outcomes in trauma contexts (e.g., Inoue et al., 2019), it can be assumed that COVID-19 places survivors of childhood abuse at higher risk for distress.
Social support plays a key role in well-being, and yet social distancing represents one of the major preventative efforts for reducing the spread of COVID-19 (Saltzman, Hansel, & Bordnick, 2020). Social supports moderated the relationship between COVID-19 and loneliness, anxiety (Xu et al., 2020) and psychopathology (Szkody, Stearns, Stanhope, & McKinney, 2020). While COVID-19 made social support even more unavailable due to lockdowns and isolations restrictions, survivors of childhood abuse are known to have limited social support systems to begin with (Gewirtz-Meydan, 2020).
Finally, ever since the COVID-19 outbreak and associated lockdowns, couples have experienced escalations in relational stress and conflict in their romantic partnerships (Pietromonaco & Overall, 2020). Indeed, in a study conducted in Germany, relationship satisfaction decreased for 40% of respondents (Schmid, Wörn, Hank, Sawatzki, & Walper, 2020). The decrease in relationship satisfaction was found to be significant for men and women alike, and almost irrespective of whether they experienced COVID-19-related changes in their employment situation (Schmid et al., 2020). As childhood abuse is associated with lower relationship quality in men and women in general (Zamir, 2021), their relationships are at higher risk for distress when an external threat as COVID-19 is presented.
1.3. The present study
Most previous studies on fear and distress regarding COVID-19 examined these psychological reactions as unidimensional. Little research has broken down COVID-19-related distress into different aspects or examined how these aspects cluster together. Such clustering can enable a more precise understanding of COVID-19 distress, and potential differences between the clusters can thus be assessed. The primary aim of the present study was to assess and identify distinct profiles of COVID-19 distress, and analyze potential differences and risk and protective factors associated with these profiles in relation to childhood abuse, psychopathology, and interpersonal relationships. Based on the literature reviewed, we hypothesized that COVID-19-related distress would be predicted by a history of childhood abuse, higher levels of psychopathology, and lower levels of current relationship satisfaction and perceived social support.
2. Methods
2.1. Participants and procedure
We conducted an online survey, accessible through Qualtrics (a secured web-based survey data collection system), among a convenience sample of men and women in Israel. The survey took an average of 20 min to complete and was open from May through August 2020. It was anonymous, and no data were collected that linked participants to recruitment sources. The [masked for review] institutional review board approved all procedures and instruments. Clicking on the link to the survey guided potential respondents to a page that provided information about the purpose of the study, the nature of the questions, and a consent form (stating that the survey was voluntary, respondents could stop at any time, and responses would be anonymous). Each participant was given the opportunity to take part in a lottery that included five $30 gift vouchers. At the end of the survey, we provided a list of online resources, telephone hotlines for mental health issues, and the researchers' contact information.
A total of 914 people participated in the study. Of them, 88.4% identified as women and 9.85% as men. The majority of the sample defined themselves as Jewish (94.1%), non-religious (67.9%), with a college/university degree (70.7%), earning an above-average income (51.1%), and with very good or excellent health. (85.7%). More than half (69.5%) reported being in a romantic relationship, and most of them (68.6%) did not have children.
2.2. Measures
COVID-19 distress was assessed using ten questions specifically tailored for the COVID-19 experience. Participants were asked to rate on a five-point Likert scale, ranging between 1 (not at all) to 5 (very much), the extent to which they feared or worried about the situations presented to them. The scale included ten questions: 1) How worried are you about being infected with COVID-19? 2) How worried are you that someone you know will be infected with COVID-19? 3) How lonely have you felt during the COVID-19 outbreak? 4) How worried are you about the spread of COVID-19? 5) How worried are you about the long-term effects of COVID-19? 6) How much do you fear that COVID-19 will have a negative impact on your life? 7) How scared are you about another COVID-19 outbreak in the near future? 8) How worried are you about your economic situation during COVID-19? 9) How stressed have you been during the COVID-19 outbreak? 10) How worried are you because of the new routine you have to abide by?
2.2.1. COVID-19-related measures
Participants were asked how badly their income was affected by COVID-19 on a scale from 1 (not at all) to 4 (very badly). Participants were also asked to indicate how much time they had been spending consuming regular or social media related to COVID-19 per day (not at all, 15 min a day, between 30 min and 2 h, and over 2 h). Media exposure was assessed with 5 items, asking respondents how many COVID-19 news broadcasts they watched on television or via social media during this period. Following this question, participants were asked to indicate whether they felt sad, scared, irritated, and/or angry (yes or no) when consuming regular or social media related to COVID-19. These items were based on measures assessing media exposure to terror-related news and were adapted to align with COVID-19 exposure (see Lassri et al., 2013; Pfefferbaum et al., 2003).
Childhood abuse was measured using the Childhood Trauma Questionnaire (CTQ-28), which has demonstrated good criterion-related validity (Bernstein et al., 2003). This 28-item questionnaire uses a 5-point Likert scale ranging from 1 (never true) to 5 (very often true), and captures three forms of childhood abuse: emotional, physical, and sexual abuse. Total scores range from 15 to 45, with higher scores indicating greater severity of abuse. The CTQ has been found to be valid for use in clinical and nonclinical populations (Scher, Stein, Asmundson, McCreary, & Forde, 2001) and has been shown to have high internal consistency and test–retest reliability, as well as a strong convergence with the Childhood Trauma Interview, demonstrating that reports of child abuse based on the CTQ are highly stable over time and across types of measurements (Bernstein et al., 2003; Bernstein & Putnam, 1986). In the present study, the calculated three scales had high reliability (α = 0.92).
Psychopathology was assessed using the short version of the Brief Symptom Inventory (BSI-18; Derogatis & Melisaratos, 2004), an 18-item scale used to assess a wide range of self-reported psychopathological symptoms. Individuals are asked to indicate on a 5-point Likert scale how often (0 = not at all to 4 = frequently) they had experienced a symptom within the past month. These items yield three subscales of psychological distress, including depression, anxiety, and somatization, as well as a global BSI scale computed by averaging all 18 items. The BSI-18 has shown very good reliability and validity for the assessment of psychological distress (Franke et al., 2017). In this sample, Cronbach's alpha = 0.92.
Relationship satisfaction was assessed using the Relationship Assessment Scale (RAS; (Hendrick, 1988). The RAS is a seven-item measure of global relationship satisfaction. Responses are given on a five-point Likert scale. Items are calculated by average scores ranging from 1 to 5 with higher scores indicate greater relationship satisfaction. Cronbach's alpha in our study was 0.91.
Social support was measured using the brief form of the Perceived Social Support Questionnaire (F-SozU; Kliem et al., 2015). The F-SozU contains six items which are rated on a 5-point Likert scale, with response categories ranging from 1 (not true at all) to 5 (very true). Higher scores reflect higher perceived social support. Previous research supports the reliability and validity of the scale (Kliem et al., 2015; Lin, Hirschfeld, & Margraf, 2019), and the reliability was very high (α = 0.87) in this sample.
Background variables included information about gender, age, marital status, education, religious affiliation, physical well-being, and income.
2.3. Data analysis
Initially, we applied Latent Profile Analysis (LPA) for estimating distinct profiles in people's COVID-19-related distress (based on their responses on the 10 items related to COVID-19 distress). To do so, we used tidyLPA R package (Rosenberg, Beymer, Anderson, van Lissa, & Schmidt, 2018) with MPlus (Muthén & Muthén, 2019) integration. We examined 1 to 7 possible profiles. The optimal number of profiles was determined by Akogul and Erisoglu's (2017) Analytic Hierarchy Process (AHP), bootstrapped likelihood ratio test (BLRT), sample size of each profile, and theoretical plausibility. The AHP uses the following information criteria in its decision tree: Akaike's Information Criterion (AIC), Approximate Weight of Evidence (AWE), Bayesian Information Criterion (BIC), Classification Likelihood Criterion (CLC), and Kullback Information Criterion (KIC).
Next, profiles were compared in a series of measures. Specifically, using chi-square tests for independence of measures with Cramer's V (assessing effect size) and Pearson standardized residuals post hoc tests with Holm-Bonferroni adjustment (Agresti, 2018), we estimated differences in gender, religious status (secular, religious), marital status (married, unmarried), children (yes, no), fear of COVID-19 prolonged outcomes (yes, no), use of facial masks (yes, no), and media exposure-related mood (sad, afraid, irritated, angry; yes, no). Finally, using one-way analyses of variance (ANOVA) with ω2 (omega squared; assessing effect size) and Tukey's Honestly Significant Difference (HSD) post hoc tests, we estimated differences in age, education level, income, self-rated health, COVID-19-related implications for financial situation, COVID-19-related media exposure, childhood abuse, psychopathology global severity index (GSI), relationship satisfaction, and perceived social support. We did not perform multivariate analysis of variance (MANOVA) because the dependent variables were not related to the same theoretical construct. All analyses were performed in R (R Core Team, 2020).
3. Results
3.1. Latent profile analysis
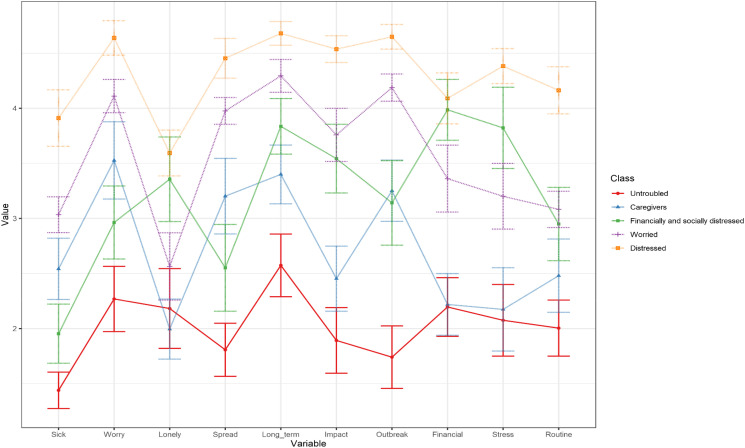
Results are summarized in Table 1 . The analysis indicates that a 5-profile solution is ideal to describe people with different profiles of COVID-19-related distress (see Fig. 1 ). Specifically, the five profiles are: “untroubled” (n = 76), “caregivers” (n = 123), “financially and socially distressed” (n = 137), “worried” (n = 351), and “distressed” (n = 214). Untroubled describes individuals with low levels of distress on all the items of the COVID-19 distress questionnaire. Caregivers refers to individuals with high levels of distress in items related to worries about others and loved ones. Financially and socially distressed describes individuals whose main concerns refer to increased loneliness and economic concerns. Worried are people who have relatively high levels of COVID-19 distress, and are concerned about the virus spreading and affecting them in the short and long term. Finally, distressed describes people with significantly high levels of COVID-19 distress (on all items). Results of chi-square tests for assessing differences in qualitative measures between these profiles are presented in Table 2 . Results of ANOVAs for assessing differences in quantitative measures are presented in Table 3 .
Table 1.
Results of latent profile analysis.
| AIC | AWE | BIC | CLC | KIC | BLRT | Entropy | |
|---|---|---|---|---|---|---|---|
| 1 profile | 28,180.73 | 28,470.87 | 28,276.80 | 28,142.73 | 28,203.73 | 1839.47⁎⁎⁎ | 1.00 |
| 2 profile | 26,363.25 | 26,814.37 | 26,512.16 | 26,302.95 | 26,397.25 | 490.31⁎⁎⁎ | 0.85 |
| 3 profile | 25,894.94 | 26,506.82 | 26,096.69 | 25,812.56 | 25,939.94 | 291.19⁎⁎⁎ | 0.81 |
| 4 profile | 25,625.74 | 26,398.32 | 25,880.33 | 25,521.34 | 25,681.74 | 202.36⁎⁎⁎ | 0.80 |
| 5 profile | 25,445.37 | 26,378.64 | 25,752.80 | 25,318.96 | 25,512.37 | 131.51⁎⁎⁎ | 0.80 |
| 6 profile | Model did not compile | ||||||
| 7 profile | Model did not compile | ||||||
Note. AIC = Akaike's Information Criterion; AWE = Approximate Weight of Evidence; BIC = Bayesian Information Criterion; CLC = Classification Likelihood Criterion; KIC = Kullback Information Criterion; BLRT = bootstrapped likelihood ratio test.
Values in bold are the lowest values and refer to the best fit according to the specific indices.
p < 0.001.
Fig. 1.
5-profile solution of the latent profile analysis.
Table 2.
Differences in percentage of background and COVID-19-related measures as a function of distress profiles.
| Untroubled |
Caregivers |
Financially and socially distressed |
Worried |
Distressed |
χ2(4) | Cramer's V (95% CI) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | N | % | N | % | N | % | N | % | N | |||
| Gender (men) | 21.3a | 16 | 8.1b | 10 | 10.4b | 14 | 6.3b | 22 | 12.7b | 27 | 18.33⁎⁎ | 0.14 (0.06, 0.20) |
| Religious status (secular) | 88.2 | 67 | 81.3 | 100 | 89.1 | 122 | 79.8 | 280 | 86.4 | 184 | 9.58⁎ | 0.10 (0.00, 0.16) |
| Married | 26.3b | 20 | 25.2b | 31 | 39.4a | 54 | 24.5b | 86 | 36.4a | 78 | 16.95⁎⁎ | 0.14 (0.05, 0.19) |
| Children (yes) | 41.3b | 31 | 36.9b | 45 | 33.6b | 46 | 30.9b | 108 | 19.6a | 42 | 19.13⁎⁎⁎ | 0.15 (0.06, 0.20) |
| Fear of prolonged outcome (yes) | 47.3a | 35 | 56.1b | 69 | 72.1c | 98 | 75.5c | 262 | 91.1d | 194 | 80.21⁎⁎⁎ | 0.30 (0.23, 0.36) |
| Use mask (yes) | 68.4a | 52 | 90.2c,b | 111 | 83.0b | 112 | 94.8c | 329 | 98.1d | 206 | 76.41⁎⁎⁎ | 0.29 (0.22, 0.35) |
| Sad (yes) | 28.4a | 21 | 41.0b | 50 | 47.4b | 64 | 64.0c | 222 | 72.5d | 153 | 70.28⁎⁎⁎ | 0.28 (0.21, 0.34) |
| Afraid (yes) | 21.6a | 16 | 47.9b | 58 | 53.0c | 71 | 76.7d | 266 | 91.1e | 194 | 173.67⁎⁎⁎ | 0.44 (0.37, 0.50) |
| Irritated (yes) | 42.5a | 31 | 29.5b | 36 | 64.9c | 87 | 59.4c | 206 | 71.8d | 153 | 67.36⁎⁎⁎ | 0.28 (0.20, 0.34) |
| Angry (yes) | 46.6 | 34 | 32.2a | 39 | 65.9 | 89 | 59.5 | 207 | 68.5b | 146 | 50.36⁎⁎⁎ | 0.24 (0.16, 0.30) |
Note. 95% CI = 95% confidence interval for Cramer's V. Percentages with different letters are significantly different at p < 0.05.
p < 0.05.
p < 0.01.
p < 0.001.
Table 3.
Differences in quantitative measures as a function of distress profiles.
| Untroubled |
Caregivers |
Financially and socially distressed |
Worried |
Distressed |
F(4, 845) | ω2 (90% CI) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | M | SD | M | SD | |||
| Age | 34.83a | 11.77 | 33.55a | 12.00 | 32.41a | 10.38 | 30.59a | 9.71 | 28.93b | 8.29 | 7.23⁎⁎⁎ | 0.03 (0.01, 0.05) |
| Level of education | 2.39 | 1.52 | 2.16 | 1.43 | 2.55 | 1.63 | 2.45 | 1.60 | 2.53 | 1.71 | 1.31 | 0.00 (0.00, 0.00) |
| Income | 2.50b | 1.18 | 2.90a | 1.23 | 2.51b | 1.13 | 2.50b | 1.18 | 2.30b | 1.15 | 5.06⁎⁎⁎ | 0.02 (0.00, 0.03) |
| Self-rated health | 4.23a | 0.65 | 4.32a | 0.68 | 4.16a | 0.73 | 4.22a | 0.63 | 3.86b | 0.85 | 12.07⁎⁎⁎ | 0.05 (0.02, 0.07) |
| Implications for financial situation | 1.95a | 1.01 | 1.73b | 0.92 | 2.50c | 1.07 | 2.25c | 1.05 | 2.62d | 1.14 | 16.84⁎⁎⁎ | 0.07 (0.04, 0.09) |
| Media exposure | 1.73a | 0.77 | 1.91a | 0.67 | 2.04b,a | 0.86 | 2.18b | 0.74 | 2.35b | 0.77 | 13.19⁎⁎⁎ | 0.05 (0.03, 0.07) |
| Childhood abuse | 6.53a | 1.97 | 6.17a | 1.74 | 7.83b | 3.06 | 6.79a | 2.35 | 7.38b | 2.95 | 9.08⁎⁎⁎ | 0.04 (0.02, 0.06) |
| Psychopathology | 0.80a | 0.54 | 0.74a | 0.48 | 1.43b | 0.73 | 1.14c | 0.62 | 1.88d | 0.75 | 77.19⁎⁎⁎ | 0.27 (0.23, 0.31) |
| Relationship satisfaction | 5.66 | 0.99 | 5.88 | 0.97 | 5.63 | 1.10 | 5.91a | 0.98 | 5.60b | 1.19 | 3.04⁎⁎⁎ | 0.01 (0.00, 0.03) |
| Perceived social support | 4.01a | 0.81 | 4.01a | 0.76 | 3.56b | 0.90 | 3.87 | 0.78 | 3.70b | 0.91 | 6.12⁎⁎⁎ | 0.03 (0.01, 0.04) |
Note. 95% CI = 90% confidence interval for ω2. Means with different letters are significantly different at p < 0.05.
p < 0.05.
p < 0.01.
p < 0.001.
3.2. Differences in background measures
The analyses revealed several unique characteristics. The untroubled group had significantly more men in it than did all the other groups. The distressed group had significantly fewer children, was younger, and had lower self-rated health than did all the other groups. The caregiver group reported that their income was significantly higher than the income of all the other groups. Aside from these unique differences, we found that the financially and socially distressed group, and the distressed group, had significantly more married participants in them than did the untroubled, caregiver, and worried groups. Other differences were not significant.
3.3. Differences in COVID-19-related measures
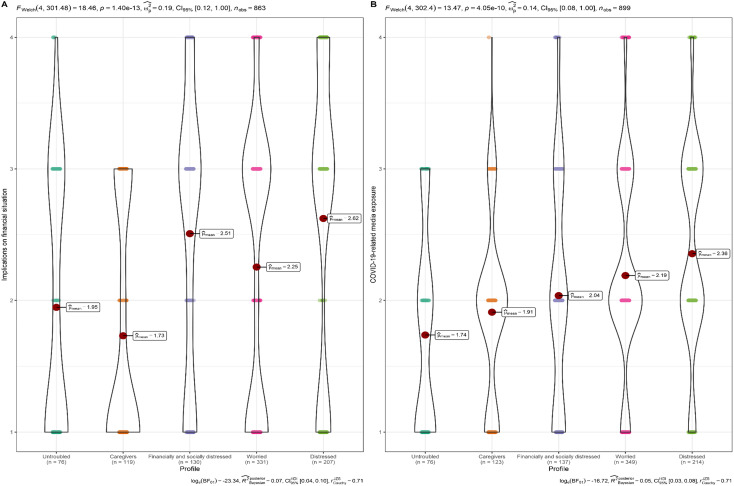
Results of quantitative measures are presented in Fig. 2 . The analyses revealed several unique characteristics. The untroubled group had a lower percentage of participants with fear of prolonged COVID-19-related outcomes, a lower use of protective facial masks, and a lower percentage of feeling sad and afraid as compared with all the other groups. The caregiver group had the fewest number of people who felt irritated, and they were the least troubled regarding COVID-19's implications for their financial situation. The distressed group had significantly more participants who were afraid of prolonged COVID-19-related outcomes, a higher use of protective facial masks, and a higher percentage of sadness, fear, and irritation. The distressed group was also the most troubled regarding COVID-19's implications for their financial situation. Finally, the financially and socially distressed group and the worried group had moderate levels (i.e., higher than those of the untroubled and financially and socially distressed groups, yet lower than those of the distressed group) of fear of prolonged COVID-19-related outcomes, feelings of irritation, and distress about COVID-19's implications for their financial situation. Aside from these unique differences, we found that the untroubled group and the caregiver group were less exposed to the media than were the worried group and the distressed group, and that the caregiver group had a lower percentage of “feeling angry” than did the distressed group. Other differences were not significant.
Fig. 2.
Differences in implications for financial situation (A) and COVID-19-related media exposure (B).
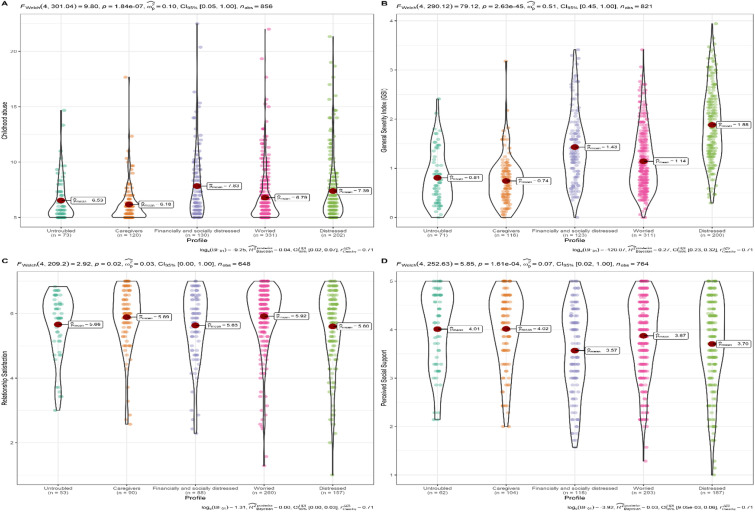
3.4. Differences in childhood abuse history, psychopathology, relationship satisfaction, and perceived social support
Results are presented in Fig. 3 . The analyses indicated that the financially and socially distressed group and the distressed group had significantly higher rates of childhood abuse than did the other groups. Regarding the GSI, we found the following pattern: untroubled, caregivers < worried < financially and socially distressed < distressed. In addition, we found that relationship satisfaction of the worried group was significantly higher than that of the distressed group. Finally, the analyses revealed that perceived social support of the untroubled and caregiver groups was higher than that of the financially and socially distressed and distressed groups.
Fig. 3.
Differences in childhood abuse (A), psychopathology — GSI (B), relationship satisfaction (C) and perceived social support (D).
4. Discussion
The goals of this study were to identify distinct profiles of COVID-19 distress, and to examine how these profiles differed in terms of childhood abuse, psychopathology, perceived social support, and relationship satisfaction. Five distinct profiles were identified. The largest group in the study was the worried group (38.96%), representing those who were preoccupied with COVID-19-related worries (i.e., the virus spreading and affecting them in the short and long term) and had high levels of COVID distress. The second largest group was the distressed group (23.75%) and included people with extremely high COVID-19 distress in all aspects. The third largest group was the financially and socially distressed group (15.20%), which consisted of people with high concerns over loneliness and economic restraints. The fourth largest group, the caregivers (13.65%), had great concerns over the well-being of their loved ones and others, with less concern regarding their own well-being in terms of being infected by the virus. The smallest group was the untroubled group (8.44%), representing individuals who reported very low levels of COVID-19 distress in all aspects measured.
These profiles are alarming as they indicate that 63% of people are experiencing high levels of distress in regard to the pandemic. Although these rates could be indicative of an immediate reaction, it is also possible that this distress will continue for years after the acute phase of the disease has passed. The possible long-term mental health impact of COVID-19 has been termed “the silent pandemic” (Graham Thornicroft, 2020) as the threat to the population's mental health has not been discussed in any meaningful way and remains unclear. Psychiatrists therefore recommend building research capacity to test COVID-19-related mental health problems (Holmes et al., 2020).
Our study describes the potential risk and protective factors associated with the profiles identified. The distressed profile seemed to have the highest cumulative distress and adversity. The distressed group was significantly more afraid of prolonged COVID-19-related outcomes, experienced higher levels of sadness, fear, and irritation when exposed to COVID-19-related news via the media, was the most troubled by COVID-19's implications for their financial situation. The distressed group had high levels of childhood abuse, had extremely high levels of psychopathology, and had the lowest level of relationship satisfaction and perceived social support. This profile is in line with previous studies indicating that a higher emotional response to COVID-19 is associated with mental disorders (García-Fernández et al., 2021), low relationship satisfaction (Luetke, Hensel, Herbenick, & Rosenberg, 2020; Pieh, Budimir, Probst, & O′Rourke, 2020), and lower levels of perceived social support (Zysberg & Zisberg, 2020). Particular attention should be given to the distressed group, as their COVID-19 distress is extremely high, and intersects with various other adversities.
The worried group had almost the same COVID-19 distress patterns, but these patterns were lower in intensity than they were in the distressed group. The worried group had moderate levels of fear of prolonged COVID-19-related outcomes and psychopathology. Perhaps the lower intensity of distress can be attributed to the relatively higher relationship satisfaction and perceived social support among this group. In other words, despite the high levels of COVID-19-related distress, the worried group did not seem to be as affected by COVID-19 distress as was the distressed group, presumably due to significant protective factors such as high relationship satisfaction and high perceived social support. This profile corresponds with previous studies indicating that social support (Szkody et al., 2020; Yu et al., 2020) and relationship satisfaction (Pieh et al., 2020) have been associated with less psychological distress during the pandemic.
The findings of the current study also raise a number of concerns about the financially and socially distressed group. In terms of COVID-19-related distress, this group was definitely not the most distressed; however, they had specific concerns about their financial situation and they also reported feeling very lonely. The financially and socially distressed group reported relatively high levels of childhood abuse, a well-documented risk factor for psychopathology (Kessler et al., 2010; Spataro, Mullen, Burgess, Wells, & Moss, 2004; Sperry & Widom, 2013), which might also explain their higher levels of COVID-19 distress. This finding corresponds with a recent study that found that individuals with a history of childhood abuse tended to experience more CPTSD symptoms, and that these symptoms, in turn, were implicated in elevated levels of both fear of COVID-19, as well as COVID-19 acute stress disorder, as compared to participants who did not experience childhood abuse (Tsur & Abu-Raiya, 2020). In addition, the financially and socially distressed group have reported low perceived social support. This group perhaps best exemplifies the non-medical implications of COVID-19.
As for their financial worries, economic hardship has long been documented as a predictive factor of psychological distress (Althouse, Allem, Childers, Dredze, & Ayers, 2014). During this pandemic, many individuals, couples, and families have faced increased financial pressure due to job loss or reduced work hours and the downsizing of social services and business activities (Godinic, Obrenovic, & Khudaykulov, 2020). Not surprisingly, economic status has been found to be negatively associated with mental stress during this pandemic (Godinic et al., 2020; Obrenovic, Jianguo, Khudaykulov, & Khan, 2020). Previous studies indicated that feeling lonely has been extremely common during this global crisis (Groarke et al., 2020; Killgore, Cloonan, Taylor, & Dailey, 2020), but this is perhaps even more true for survivors of childhood abuse. During the pandemic, survivors of child abuse may not be able to engage in their usual coping mechanisms (e.g., going to the gym), but they may also be using a more avoidant coping mechanism (e.g., being around people, keeping busy), and the lockdowns brought things to the fore as they were left alone with their thoughts and memories (Justice in Covid-19 for Sexual Abuse and Violence (JiCSAV), 2021). In other cases, trials of abuse cases were delayed due to the shut-down of the criminal justice system, leaving survivors who were waiting for their trial for many years, in uncertainty and anxiety (JiCSAV, 2021).
The caregivers were characterized by one specific concern: They feared not for themselves, but for others, and their loved ones. The caregivers reported having a higher income than all the other groups, comprised the fewest number of people who felt irritated, and were the least troubled about COVID-19's implications for their financial situation. The caregiver group was typified by significantly less psychopathology and lowest level of history of childhood abuse, and had relatively high social support, as well as the highest income reported. We would cautiously suggest that this group's relatively high financial, interpersonal, and emotional resources perhaps made them more resilient in the face of COVID-19-related distress. It is possible that as this group did not endure too much personal distress, economic hardship, or other such worries, they were more emotionally available to care for others.
Finally, the untroubled group was the group that reported the least COVID-19 distress. The untroubled group had significantly less psychopathology and history of childhood abuse, and relatively high levels of social support. This group had potential protective factors (e.g., social support) and low risk factors (e.g., psychopathology and history of childhood abuse). With regard to gender, this group had significantly more men. Previous studies have all pointed to a difference between women's and men's distress during the pandemic, with women reporting higher levels of stress than men (Kowal et al., 2020; Limcaoco, Mateos, Fernández, & Roncero, 2020; Wang et al., 2020). During the current pandemic, women have also reported both higher levels of work-family conflict than have men (Minello, 2020) and assuming more responsibility for domestic chores and childcare (Kowal et al., 2020). It can thus be assumed that women are more overwhelmed and stressed than are men by the need to adapt to various changes elicited by COVID-19 lockdowns and quarantines. In line with the finding regarding high media consumption among the distressed and worried groups, both the untroubled and the caregiver groups were significantly less exposed to the media.
Although the caregiver and the untroubled groups seemed to cope well with COVID-19-related distress, it should be noted that these groups were the smallest groups in our sample, and together comprised only 22% of participants. That said, it seems that the vast majority of people experience moderate to high levels of COVID-19-related distress. Our study contributes to a better understanding of the factors associated with the different profiles of COVID-19-related distress. In this sense, COVID-19 distress severity could be mapped as a function of different adversities, mental health, social support, relationship satisfaction, and sociodemographic factors.
4.1. Clinical implications
The five profiles identified in this study raise many clinical considerations for clinicians and policymakers. First, the current study enables us to classify people by their COVID-19-related distress. In other words, people can be identified by their main areas of distress (e.g., worry over others, financial worries, contracting the disease, etc.). As such, more suitable strategies and mental health recommendations or programs can be offered to different people, in order to reduce their specific fears, allow them to develop better coping strategies, and improve their well-being by addressing the specific aspects causing them distress. Moreover, this study identified different populations at risk for specific COVID-19-related distress (e.g., those with a history of childhood abuse, higher levels of psychopathology, less social support, and low relationship satisfaction). These at-risk populations should be carefully attended to, as the pandemic is expected to have long-term consequences for their well-being.
4.2. Limitations and future research
The current study had a few limitations. First, self-reported rates may not fully reflect the true prevalence of the reported measures. Despite the large sample used (n = 914), most of our respondents were women, were highly educated, and had very good general health (according to their self-rated health). Second, there was no comparison group, nor were there baseline measures. As the currents study is cross-sectional, bi-directional effects of social support, psychopathology and interpersonal relationships in the model are possible. Thus, we are unable to determine whether these aspects preceded the pandemic response or was caused by it. Future research should include more representative samples and track COVID-19 distress in longitudinal studies, to analyze its consequences over time. Finally, the sample was not nationally representative, and it was recruited online. Thus, it is possible that the name of the study and its description attracted individuals who were highly sensitive to and worried about the pandemic, and also those who tended to use social media more regularly. Further research is required to determine the association between COVID-19 and various other relevant mental health aspects, including posttraumatic stress disorder, suicidal behaviors, and dissociation. Although we inquired about relationship satisfaction, a more comprehensive understanding of relational aspects during the pandemic could have been obtained by evaluating both partners, using an actor-partner independent model.
5. Conclusion
The current study demonstrates the importance of identifying unique responses to COVID-19 distress by identifying five distinct profiles: distressed, worried, financially and socially distressed, caregivers, and untroubled. The findings also revealed that individuals that have more COVID-19 related distress report more childhood abuse, psychopathology, and less social support and relationship satisfaction. An assessment of the psychological implications of COVID-19 (when screening the population and creating prevention/intervention programs) should consider taking into account the different responses individuals have when facing COVID-19, and their vulnerability, including their history of abuse, psychopathology, social support and relationship satisfaction, so that these programs can be better tailored to each type of distress experienced.
Role of the funding source
Haruv Institute did not take any part in the study except of providing seed money.
Declaration of competing interest
The authors have no conflicts of interest to disclose.
Acknowledgements
This project received funding from the Haruv Institute.
Footnotes
Author's note: Dr. Gewirtz Meydan is an affiliated researcher at The Crimes against Children Research Center and at Haruv Institute, and Dr. Lassri is affiliated researcher at the Research Department of Clinical, Educational and Health Psychology, UCL (University College London) and at Haruv Institute.
References
- Agresti A. John Wiley & Sons; 2018. An introduction to categorical data analysis. [Google Scholar]
- Akogul S., Erisoglu M. An approach for determining the number of clusters in a model-based cluster analysis. Entropy. 2017;19(9):1–15. doi: 10.3390/e19090452. [DOI] [Google Scholar]
- Althouse B.M., Allem J.P., Childers M.A., Dredze M., Ayers J.W. Population health concerns during the United States’ great recession. American Journal of Preventive Medicine. 2014;46(2):166–170. doi: 10.1016/j.amepre.2013.10.008. [DOI] [PubMed] [Google Scholar]
- Asmundson G.J.G., Taylor S. Coronaphobia: Fear and the 2019-nCoV outbreak. Journal of Anxiety Disorders. 2020;70:1–2. doi: 10.1016/j.janxdis.2020.102196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendau A., Petzold M.B., Pyrkosch L., Mascarell Maricic L., Betzler F., Rogoll J., Große J., Ströhle A., Plag J. Associations between COVID-19 related media consumption and symptoms of anxiety, depression and COVID-19 related fear in the general population in Germany. European Archives of Psychiatry and Clinical Neuroscience. 2020;1:3. doi: 10.1007/s00406-020-01171-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein D.P., Stein J.A., Newcomb M.D., Walker E., Pogge D., Ahluvalia T., Stokes J., Handelsman L., Medrano M., Desmond D., Zule W. Development and validation of a brief screening version of the childhood trauma questionnaire. Child Abuse and Neglect. 2003;27(2):169–190. doi: 10.1016/S0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Bernstein E.M., Putnam F.W. Development, reliability, and validity of a child dissociation scale. The Journal of Nervous and Mental Disease. 1986;174(12):727–735. doi: 10.1016/S0145-2134(08)80004-X. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24(4):385–396. [PubMed] [Google Scholar]
- Derogatis L.R., Melisaratos N. In: The use of psychological testing for treatment planning and outcomes assessment: Instruments for adults. Maruish M.E., editor. Lawrence Erlbaum Associates Publishers; 2004. The SCL-90-R, the brief symptom inventory (BSI), and the BSI-18; pp. 1–41. [Google Scholar]
- Doom J., Fox K. 2020. Adverse and benevolent childhood experiences predict mental health during the COVID-19 pandemic. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernández R.S., Crivelli L., Guimet N.M., Allegri R.F., Pedreira M.E. Psychological distress associated with COVID-19 quarantine: Latent profile analysis, outcome prediction and mediation analysis. Journal of Affective Disorders. 2020;277(1):75–84. doi: 10.1016/j.jad.2020.07.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick K.M., Harris C., Drawve G. Fear of COVID-19 and the mental health consequences in America. Psychological Trauma: Theory, Research, Practice, and Policy. 2020;12:17–21. doi: 10.1037/tra0000924. [DOI] [PubMed] [Google Scholar]
- Franke G.H., Jaeger S., Glaesmer H., Barkmann C., Petrowski K., Braehler E. Psychometric analysis of the brief symptom inventory 18 (BSI-18) in a representative German sample. BMC Medical Research Methodology. 2017;17(1):1–7. doi: 10.1186/s12874-016-0283-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao J., Zheng P., Jia Y., Chen H., Mao Y., Chen S., Wang Y., Fu H., Dai J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE. 2020;15(4) doi: 10.1371/journal.pone.0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-Fernández L., Romero-Ferreiro V., Padilla S., López-Roldán P.D., Monzó- García M., Rodriguez-Jimenez R. The impact on mental health patients of COVID-19 outbreak in Spain Lorena. Journal of Psychiatric Research. 2021 doi: 10.1016/j.jpsychires.2021.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gewirtz-Meydan A. The relationship between child sexual abuse, self-concept and psychopathology: The moderating role of social support and perceived parental quality. Children and Youth Services Review. 2020;113(March) doi: 10.1016/j.childyouth.2020.104938. [DOI] [Google Scholar]
- Godinic D., Obrenovic B., Khudaykulov A. Effects of economic uncertainty on mental health in the COVID-19 pandemic context: Social identity disturbance, job uncertainty and psychological well-being model. International Journal of Innovation and Economic Development. 2020;6(1):61–74. doi: 10.18775/ijied.1849-7551-7020.2015.61.2005. [DOI] [Google Scholar]
- Graham Thornicroft S. King’s College London; 2020. The silent pandemic: Covid-19 and mental health.https://www.kcl.ac.uk/the-silent-pandemic-covid-19-and-mental-health (King’s College London). [Google Scholar]
- Groarke J.M., Berry E., Graham-Wisener L., McKenna-Plumley P.E., McGlinchey E., Armour C. Loneliness in the UK during the COVID-19 pandemic: Cross-sectional results from the COVID-19 psychological wellbeing study. PLoS ONE. 2020;15:1–18. doi: 10.1371/journal.pone.0239698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo J., Fu M., Liu D., Zhang B., Wang X., Van Ijzendoorn M.H. Is the psychological impact of exposure to COVID-19 stronger in adolescents with pre-pandemic maltreatment experiences? A survey of rural Chinese adolescents. Child Abuse & Neglect. 2020;110:1–10. doi: 10.1016/j.chiabu.2020.104667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendrick S.S. A generic measure of relationship satisfaction. Journal of Marriage and Family. 1988;50(1):93–98. [Google Scholar]
- Holmes E.A., O’Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., Bullmore E.… Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry. 2020;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horesh D., Brown A.D. Covid-19 response: Traumatic stress in the age of Covid-19: A call to close critical gaps and adapt to new realities. Psychological Trauma: Theory, Research, Practice, and Policy. 2020;12(4):331–335. doi: 10.1037/TRA0000592. [DOI] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., Cheng Z., Yu T., Xia J., Wei Y., Wu W., Xie X., Yin W., Li H., Liu M., Cao B.… Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inoue Y., Stickley A., Yazawa A., Aida J., Kawachi I., Kondo K., Fujiwara T. Adverse childhood experiences, exposure to a natural disaster and posttraumatic stress disorder among survivors of the 2011 great east Japan earthquake and tsunami. Epidemiology and Psychiatric Sciences. 2019;28(1):45–53. doi: 10.1017/S2045796017000233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeong H., Yim H.W., Song Y.J., Ki M., Min J.A., Cho J., Chae J.H. Mental health status of people isolated due to Middle East respiratory syndrome. Epidemiology and Health. 2016;38 doi: 10.4178/epih.e2016048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Justice in Covid-19 for Sexual Abuse and Violence (JiCSAV) 2021. Independent Sexual Violence Advisors and Third Sector Support Services. [Google Scholar]
- Kelly B.D. Impact of covid-19 on mental health in Ireland: Evidence to date. Irish Medical Journal. 2020;113(10):1–6. [Google Scholar]
- Kessler R.C., McLaughlin K.A., Green J.G., Gruber M.J., Sampson N.A., Zaslavsky A.M., Aguilar-Gaxiola S., Alhamzawi A.O., Alonso J., Angermeyer M., Benjet C., Bromet E., Chatterji S., De Girolamo G., Demyttenaere K., Fayyad J., Florescu S., Gal G., Gureje O., Williams D.R.… Childhood adversities and adult psychopathology in the WHO world mental health surveys. British Journal of Psychiatry. 2010;197(5):378–385. doi: 10.1192/bjp.bp.110.080499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore W.D.S., Cloonan S.A., Taylor E.C., Dailey N.S. Loneliness: A signature mental health concern in the era of COVID-19. Psychiatry Research. 2020;290 doi: 10.1016/j.psychres.2020.113117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kliem S., Mößle T., Rehbein F., Hellmann D.F., Zenger M., Brähler E. A brief form of the perceived social support questionnaire (F-SozU) was developed, validated, and standardized. Journal of Clinical Epidemiology. 2015;68(5):551–562. doi: 10.1016/j.jclinepi.2014.11.003. [DOI] [PubMed] [Google Scholar]
- Kowal M., Coll-Martín T., Ikizer G., Rasmussen J., Eichel K., Studzinska A., Ahmed O. 2020. Who is the most stressed during COVID-19 isolation? Data from 27 countries. Unpublished manuscript. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lassri D., Soffer-Dudek N., Lerman S.F., Rudich Z., Shahar G. Self-criticism confers vulnerability to psychopathology in the face of perceived stress related to missile attacks: Three longitudinal studies. International Journal of Cognitive Therapy. 2013;6(3):221–234. doi: 10.1521/ijct.2013.6.3.221. [DOI] [Google Scholar]
- Li L., Li F., Fortunati F., Krystal J.H. Association of a prior psychiatric diagnosis with mortality among hospitalized patients with coronavirus disease 2019 (COVID-19) infection. JAMA Network Open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.23282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Limcaoco R.S.G., Mateos E.M., Fernández J.M., Roncero C. Anxiety, worry and perceived stress in the world due to the COVID-19 pandemic, March 2020. Preliminary results. MedRxiv. 2020 doi: 10.1101/2020.04.03.20043992. [DOI] [Google Scholar]
- Lin M., Hirschfeld G., Margraf J. Brief form of the perceived social support questionnaire (F-SozU K-6): Validation, norms, and cross-cultural measurement invariance in the USA, Germany, Russia, and China. Psychological Assessment. 2019;31(5):609–621. doi: 10.1037/pas0000686. [DOI] [PubMed] [Google Scholar]
- Luetke M., Hensel D., Herbenick D., Rosenberg M. Romantic relationship conflict due to the COVID-19 pandemic and changes in intimate and sexual behaviors in a nationally representative sample of American adults. Journal of Sex and Marital Therapy. 2020;46(8):747–762. doi: 10.1080/0092623X.2020.1810185. [DOI] [PubMed] [Google Scholar]
- Maaravi Y., Heller B. Not all worries were created equal: The case of COVID-19 anxiety. Public Health. 2020;185:243–245. doi: 10.1016/j.puhe.2020.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minello A. The pandemic and the female academic. Nature. 2020:17. doi: 10.1038/d41586-020-01135-9. [DOI] [PubMed] [Google Scholar]
- Muthén L.K., Muthén B. (8th ed.). Muthén & Muthén; 2019. Mplus User’s guide. [Google Scholar]
- Obrenovic B., Jianguo D., Khudaykulov A., Khan M.A.S. Work-family conflict impact on psychological safety and psychological well-being: A job performance model. Frontiers in Psychology. 2020;11:1–18. doi: 10.3389/fpsyg.2020.00475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum B., Seale T.W., Brandt E.N., Pfefferbaum R.L., Doughty D.E., Rainwater S.M. Media exposure in children one hundred miles from a terrorist bombing. Annals of Clinical Psychiatry. 2003;15(1):1–8. doi: 10.1023/A:1023293824492. [DOI] [PubMed] [Google Scholar]
- Pieh C., Budimir S., Probst T., O′Rourke T. Relationship quality and mental health during COVID-19 lockdown. PLoS ONE. 2020;15:1–10. doi: 10.1371/journal.pone.0238906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietromonaco P.R., Overall N.C. Applying relationship science to evaluate how the COVID-19 pandemic may impact couples’ relationships. American Psychologist. 2020;1–13 doi: 10.1037/amp0000714. [DOI] [PubMed] [Google Scholar]
- R Core Team . 2020. R: A language and environment for statistical computing. [Google Scholar]
- Rosenberg J., Beymer P., Anderson D., van Lissa C.J., Schmidt J. tidyLPA: An R package to easily carry out Latent Profile Analysis (LPA) using open-source or commercial software. Journal of Open Source Software. 2018;3(30):978. doi: 10.21105/joss.00978. [DOI] [Google Scholar]
- Salari N., Hosseinian-Far A., Jalali R., Vaisi-Raygani A., Rasoulpoor S., Mohammadi M., Rasoulpoor S., Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Globalization and Health. 2020;16(1):1–11. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saltzman L.Y., Hansel T.C., Bordnick P.S. Loneliness, isolation, and social support factors in post-COVID-19 mental health. Psychological Trauma: Theory, Research, Practice, and Policy. 2020;12:55–57. doi: 10.1037/tra0000703. [DOI] [PubMed] [Google Scholar]
- Scher C.D., Stein M.B., Asmundson G.J.G., McCreary D.R., Forde D.R. The childhood trauma questionnaire in a community sample: Psychometric properties and normative data. Journal of Traumatic Stress. 2001;14(4):843–857. doi: 10.1023/A:1013058625719. [DOI] [PubMed] [Google Scholar]
- Schmid L., Wörn J., Hank K., Sawatzki B., Walper S. Changes in employment and relationship satisfaction in times of the COVID-19 pandemic: Evidence from the German family panel. European Societies. 2020;1–16 doi: 10.1080/14616696.2020.1836385. [DOI] [Google Scholar]
- Serafini G., Parmigiani B., Amerio A., Aguglia A., Sher L., Amore M. The psychological impact of COVID-19 on the mental health in the general population. QJM: An International Journal of Medicine. 2020;113(8):229–235. doi: 10.1093/qjmed/hcaa201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spataro J., Mullen P.E., Burgess P.M., Wells D.L., Moss S.A. Impact of child sexual abuse on mental health: Prospective study in males and females. British Journal of Psychiatry. 2004;184(MAY):416–421. doi: 10.1192/bjp.184.5.416. [DOI] [PubMed] [Google Scholar]
- Sperry D.M., Widom C.S. Child abuse and neglect, social support, and psychopathology in adulthood: A prospective investigation. Child Abuse and Neglect. 2013;37(6):415–425. doi: 10.1016/j.chiabu.2013.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szkody E., Stearns M., Stanhope L., McKinney C. Stress-buffering role of social support during COVID-19. Family Process. 2020;1–14 doi: 10.1111/famp.12618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taquet M., Luciano S., Geddes J.R., Harrison P.J. Bidirectional associations between COVID-19 and psychiatric disorder: Retrospective cohort studies of 62 354 COVID-19 cases in the USA. The Lancet Psychiatry. 2020;0366(20):1–11. doi: 10.1016/S2215-0366(20)30462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S., Landry C.A., Paluszek M.M., Fergus T.A., McKay D., Asmundson G.J.G. Development and initial validation of the COVID stress scales. Journal of Anxiety Disorders. 2020;72(May) doi: 10.1016/j.janxdis.2020.102232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsur N., Abu-Raiya H. COVID-19-related fear and stress among individuals who experienced child abuse: The mediating effect of complex posttraumatic stress disorder. Child Abuse and Neglect. 2020;110(P2) doi: 10.1016/j.chiabu.2020.104694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health. 2020;17(5):1729–1754. doi: 10.1093/qjmed/hcaa110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu J., Ou J., Luo S., Wang Z., Chang E., Novak C., Shen J., Zheng S., Wang Y. Perceived social support protects lonely people against COVID-19 anxiety: A three-wave longitudinal study in China. Frontiers in Psychology. 2020;11:1–12. doi: 10.3389/fpsyg.2020.566965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu H., Li M., Li Z., Xiang W., Yuan Y., Liu Y., Li Z., Xiong Z. Coping style, social support and psychological distress in the general Chinese population in the early stages of the COVID-19 epidemic. BMC Psychiatry. 2020;20(1):1–11. doi: 10.1186/s12888-020-02826-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zamir O. Childhood maltreatment and relationship quality: A review of type of abuse and mediating and protective factors. Trauma, Violence, and Abuse. 2021 doi: 10.1177/1524838021998319. [DOI] [PubMed] [Google Scholar]
- Zhao H., He X., Fan G., Li L., Huang Q., Qiu Q., Kang Z., Du T., Han L., Ding L., Xu H. COVID-19 infection outbreak increases anxiety level of general public in China: Involved mechanisms and influencing factors. Journal of Affective Disorders. 2020;276(July):446–452. doi: 10.1016/j.jad.2020.07.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zysberg L., Zisberg A. Days of worry: Emotional intelligence and social support mediate worry in the COVID-19 pandemic. Journal of Health Psychology. 2020 doi: 10.1177/1359105320949935. [DOI] [PubMed] [Google Scholar]