Abstract
Our brain is constantly shaped by our immediate environments, and while some effects are transient, some have long-term consequences. Therefore, it is critical to identify which environmental risks have evident and long-term impact on brain development. To expand our understanding of the environmental context of each child, the Adolescent Brain Cognitive Development (ABCD) Study® incorporates the use of geospatial location data to capture a range of individual, neighborhood, and state level data based on the child’s residential location in order to elucidate the physical environmental contexts in which today’s youth are growing up. We review the major considerations and types of geocoded information incorporated by the Linked External Data Environmental (LED) workgroup to expand on the built and natural environmental constructs in the existing and future ABCD Study data releases. Understanding the environmental context of each youth furthers the consortium’s mission to understand factors that may influence individual differences in brain development, providing the opportunity to inform public policy and health organization guidelines for child and adolescent health.
Abbreviations: ABCD, Adolescent Brain Cognitive Development; ACS, American Community Survey; CDC, Centers for Disease Control and Prevention; CT, U.S. Census Bureau Census Tract; DAIRC, Data Analytic and Information Resource Center; LED, Linked External Data; PII, Personal Identifiable Information
Keywords: Environmental neuroscience, Environmental health, Neighborhood, Built environment, Natural environment
Highlights
-
•
ABCD Study® includes a Linked External Data (LED) Environmental working group.
-
•
Residential geocodes linked to physical environmental contextual variables.
-
•
External data sources include residential, census, and state-level variables.
-
•
These data may allow for important gene-by-environment effects to be examined.
1. Introduction
The physical environment encompasses both built and natural factors that can be a major determinant of our health and wellbeing (Braveman et al., 2011, Evans and Stoddart, 1990, Dahlgren and Whitehead, 1991, Keating, Daniel and Hertzman, 1999). The built environment includes man-made spaces as well as state- and community-level conditions in which we live, learn, work, and play (e.g. homes, buildings, streets, infrastructure, neighborhood conditions, access to resources, policy). The natural environment on the other hand includes land, air, and water, and includes aspects of our physical surroundings such as oceans, forests, greenspace, and climate (Woolf and Aron, 2013). These natural environments can also include potentially harmful substances, including exposure to air pollution and other toxins.
Within the realm of environmental health, an extensive literature has emerged implicating the importance of the physical environment in which individuals grow up on human neurodevelopment. For example, living in an urban setting has been associated with mental health risk, including schizophrenia and post-traumatic stress disorder (Costa e Silva and Steffen, 2019, Fan et al., 2011, Haddad et al., 2015, Lambert et al., 2015, Pedersen and Mortensen, 2001b), whereas neighborhood conditions, such as growing up in lower socioeconomic neighborhoods, have been linked with children’s verbal and emotional behavioral outcomes (Christian et al., 2015, Minh et al., 2017). As for the natural environment, emerging literature has also implicated greenspace as a potential protective factor, with links to better childhood neurodevelopmental outcomes and lower risk of psychiatric disorders in adolescents and adulthood (Engemann et al., 2019, Liao et al., 2019, Younan et al., 2016). In terms of exposure to harmful substances, air pollution and lead exposure have been widely linked to cognitive functioning during childhood and adolescents (Cecil, 2011, Clifford et al., 2016, Lanphear et al., 2005, Volk et al., 2021) as well as increased the risk of mental health problems (Antonsen et al., 2020, Daneshparvar et al., 2016, Khan et al., 2019, Pedersen and Mortensen, 2006, Thurston et al., 2017) More recently, studies have begun to show these built and natural environmental factors during childhood and adolescence influencing brain structure and function (Bell et al., 2021, Herting et al., 2019, Rakesh et al., 2021a, Rakesh et al., 2021b). Indeed, these strong links between various physical environmental factors and health outcomes has led to the strong impetus for elucidating how an individual’s exposome, or the totality of exposure experienced by an individual over their lives, may affect one’s health (Wild, 2012). Thus, questions remain as to when during development and how these various exposures may exert their unique or interactive effects on neurodevelopment and what children may be most vulnerable to such exposures. Moreover, although evidence has been mounting on the impact of the physical environment on neurodevelopment outcomes, these studies have primarily focused on single exposures, cross-sectional behavioral measurements or implemented neuroimaging methods in smaller samples and have largely focused on study participants from a single limited geographical location. Thus, future research requiring large scale, population neuroimaging and longitudinal studies are needed to identify the potential biological mechanisms that may underlie the link between physical environmental exposures and brain development.
The Adolescent Brain Cognitive Development (ABCD) Study® provides a unique opportunity to investigate the links between exposure to multiple built and natural environmental factors and the developing child and adolescent brain in a population-based study of U.S. children. The large, diverse sample (i.e. N~11,800 children enrolled at 9–10 years of age) and a longitudinal design, including annual follow-up for 9 years, allows researchers to examine environmental impacts on cognitive, behavioral, and multimodal neuroimaging measurements in youth across 21 metropolitan areas in America. By linking information about the physical environment of ABCD participants through geocoding of their residential locations, the ABCD Study® holds great potential in contributing to our understanding of environmental-based changes in human brain development. Although the process of identifying and linking physical environmental exposures is an ever-evolving process, the LED Environment Working Group within the consortium has already begun to map several residential-, census-, and state-level variables to better understand the built and natural environment of ABCD participants. Thus, the goal of the current manuscript is to serve as a resource for the field regarding the existing LED Environment measures in the ABCD Study in hopes of facilitating open science and the use of these data by researchers who are interested in how the built and natural environment impacts neurodevelopment. In the following sections, we first discuss key aspects to geospatial mapping and data linkage efforts in the ABCD Study, including: (1) describing our workflow for linking environmental measurements in the ABCD Study while maintaining privacy protection for our participants; (2) reviewing the currently linked environmental measurements obtained by geospatial mapping in detail, and (3) discussing strengths and limitations of these data, including outlining how the current environmental data may be useful towards understanding social determinants of health using the ABCD Study dataset as well as considerations for the user and future directions of the geospatial mapping and data linkage efforts in the ABCD Study.
2. Estimating the physical environment through geospatial mapping
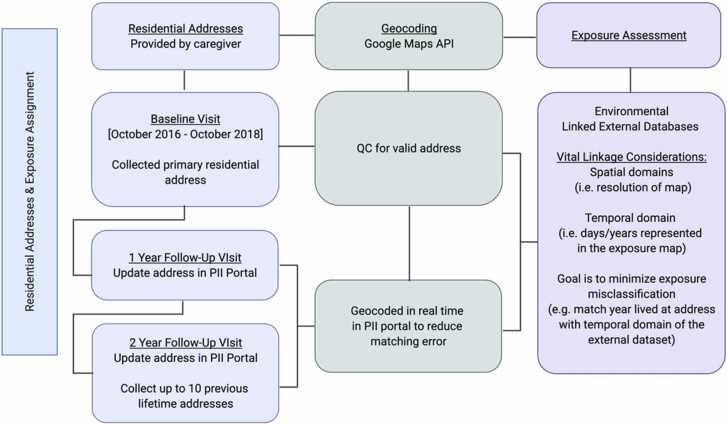
Fig. 1 shows an overview of the collection of residential addresses, geocoding process, and linkage to external data sources. Below, we outline each step of the process in greater detail.
Fig. 1.
Collection and linking of residential address information in the ABCD Study. Current residential data include both retrospectively collected primary residential addresses as well as prospective data collection at each annual study visit. Exposure assessment comes from linking geocodes to external data resources. Linkage has primarily focused on addresses collected at baseline. In future releases, retrospective and prospective data will be linked with special consideration to the spatial and temporal domains to minimize misclassification between when and where a child resided and the contextual variables of any given environmental dataset. API = application programming interface. QC = quality control. PII = personally identifiable information.
2.1. Collection of residential addresses
After parents/caregivers and children completed written informed consent and written assent, respectively, primary residential addresses were collected in-person from the participant’s caregiver during both the baseline study visit (October 2016 to October 2018) and at each follow-up study visit occurring approximately every 12 months. At the baseline visit, the parent or caregiver was asked, “At what address does your child live?” by the Research Assistant (RA); the RA recorded the answer in the secure personal identifiable information (PII) portal. If a child spent less than 80% of their time at the primary address, the RA was able to record up to 2 additional current addresses in the PII to capture time spent at several home locations. Address 1 is treated as the primary address, with the percentages of time spent in primary, secondary, and tertiary addresses also recorded if the child split their time between multiple home addresses. At the follow-up in-person visits, the RA updated the current addresses as needed. As part of the second-year follow-up visit, the RA also collected up to 10 previous lifetime addresses for the child.
2.2. Data processing for residential addresses
As pointed out in prior reviews on the applications of geocoding on health sciences (Goldberg et al., 2013), converting residential addresses to the latitude and longitude is the most basic and critical step for the subsequent geospatial data linkage. To achieve this, the latitude and longitude of baseline residential addresses were geocoded by the ABCD Data Analysis Informatics and Resource Center (DAIRC) using the Google Maps Application Programming Interface (API) (“Google Maps Static API Documentation,” 2021), and each address was assigned a Status Code and/or Error Message. Status codes included “OK” (no errors occurred in geocoding the address) or “ZERO_RESULTS” (the geocode was successful but returned no results indicating the geocoder passed a non-existent address). Error messages of the geocoding issues included: “city not found”, “state not found”, “street not found”, “zip code not found”, or “geocode zip code does not match typed zip code”. Only addresses that generated an “OK” status were used for exposure assignment. Of all addresses collected at the baseline visit, 98.99% were successfully geocoded. For follow-up address data collection (including collecting up to 10 lifetime addresses), the Google API was used in real-time to ensure address validity (Status code “OK”) and generate a map of the location in Google Maps so the participant could verify the address’s general location ensuring appropriate longitude and latitude.
2.3. PII and ethics
One critical task for geospatial mapping in the ABCD Study is to ensure the protection of privacy of the participating individuals and their families. The policy of the ABCD Study strictly prohibits the identification of participants; therefore, we took precautions in designing our geospatial mapping pipelines.
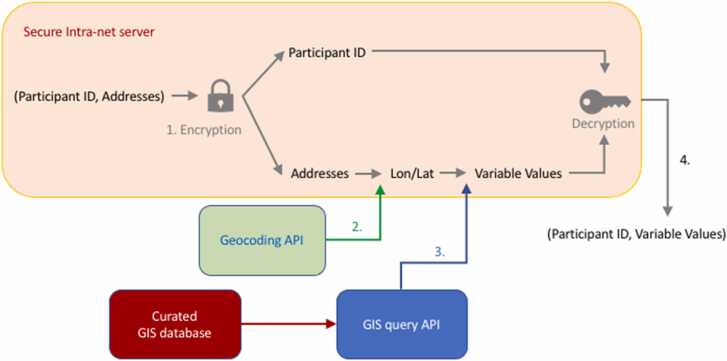
We modularized and compartmentalized the pipeline, as illustrated in Fig. 2. After PII were recorded and validated by the on-site researchers, data were automatically encrypted and stored in a secured, firewall-protected intranet server. Participants’ identification (ID) and addresses were then dissociated and separately encrypted. The encrypted addresses were then exposed to the geocoding API for converting into longitude and latitude (Step 2 in Fig. 2). In parallel, the ABCD Study researchers curated a geographic information system (GIS) database, based on the initial scientific inputs from the community and the feasibility of the datatype (described below). GIS is a general framework used for capturing, storing, managing, and displaying data related to geospatial locations on the Earth’s surface (Campbell and Shin, 2011). An example of the LED Environment GIS curation and the corresponding query functions can be found in the ABCD Study’s Github page (https://github.com/ABCD-STUDY/geocoding). The curated GIS database was imported into the secured server and used to query the corresponding values given longitude and latitude (Step 3 in Fig. 2). After the values were assigned, the longitude and latitude were removed from the subsequent process, avoiding the leakage of PII. The assigned values and the corresponding encrypted keys were then linked back to the participant ID, producing a decrypted dataset without any PII (Step 4 in Fig. 2). While the encryption and decryption in the PII server were unique to ABCD, as it was developed to bridge the need between maintaining the PII of ABCD Study as a whole and the geocoding process, the geocoding data linkage is built upon the existing code bases for assigning values given the spatial coordinates and GIS database (Goldberg et al. 2013). Currently, we adopt deterministic value assignment without considering mapping uncertainties. Although this would limit the statistical modeling for spatial inference, it was a practical solution given a wide swath of environmental variables with different spatial resolutions were requested for geocoding.
Fig. 2.
Conceptual workflow of modularized geocoding pipeline of ABCD Study. Colored rectangles represent different compartmentalized modules, while the geocoding processes are labeled numerically (Step 1–4, further detailed in the maintext).
Finally, we imposed rounding for continuous geocoded variables to avoid identifiability as some GIS maps can have resolution fine enough to have one single unique value for one particular ABCD participant. Although it might be theoretically possible to identify individuals using multiple variables as triangulation, the data use agreement that governs the responsibility of the approved researchers prohibit such usage.
2.4. Types of geospatial data
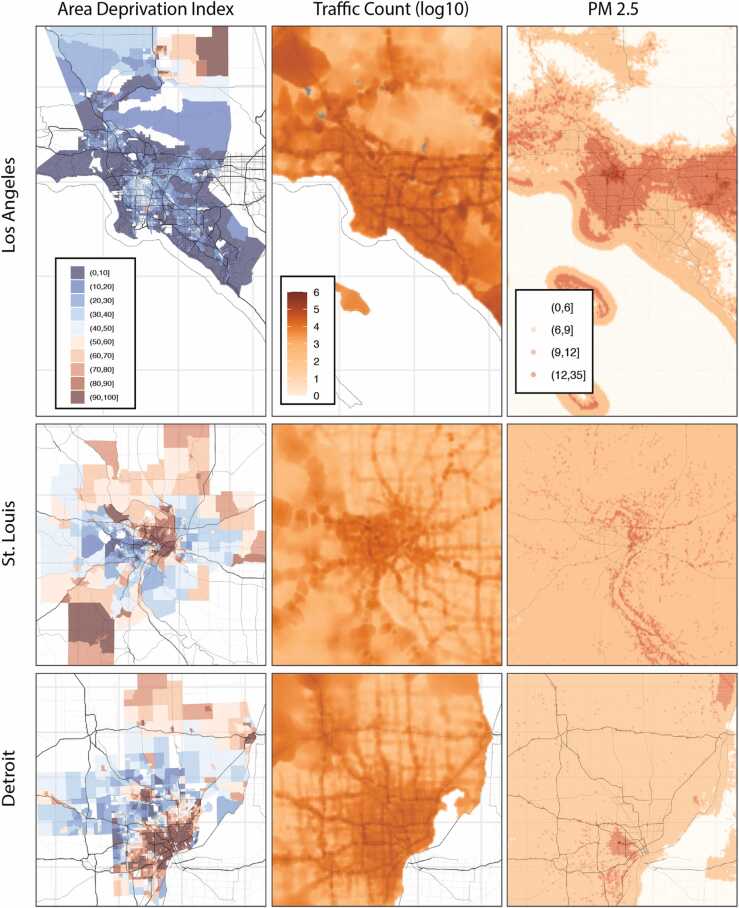
With every address, census tract, and city having its own longitude and latitude, GIS data can be linked to estimate participants’ physical environments. There are two primary spatial data types in GIS: (1) vector data, which is comprised of either points, lines, or spatial polygons with associated values, and (2) spatial data (or raster data), which is represented by grid cells (also referred to as pixels). Examples of vector geospatial data are shown in the first two columns of Fig. 3. Spatial polygons may be associated with data aggregated at various spatial levels, and are irregular polygonal regions defined by historical, statistical, legal, and/or administerial reasons. Example data of spatial polygons include the census tracts used by the US Census, zip codes used by the United States Postal Service, or counties by local governments. The census tracts are polygons created with the intention of having about 4000 people in each of them, although the actual number ranges (Bureau of the Census, 2018). Zip codes on the other hand are clusters of lines with more than 41,000 zip codes with some populations of a single zip code exceeding 100,000. The first column of Fig. 3 illustrates this data type using the Area Deprivation Index, a measurement of neighborhood deprivation derived from the American Community Survey. The second column in Fig. 3 illustrates traffic counts, which are point data that were obtained by surveying stations at various geographical locations. In contrast, raster data are usually obtained by model estimation, incorporating multiple sources such as satellite imaging and ground station surveys, as is seen for fine particulate matter (PM2.5) in the third column of Fig. 3.
Fig. 3.
Example of three types of geospatial data used for linkage, including spatial polygons, point data, and raster data. Area Deprivation Index (spatial polygon), traffic counts (point data), and fine particulate air pollution (PM2.5) plotted for 3 different recruitment areas in the U.S., including Los Angeles, California (top row), St. Louis, Missouri (middle row), and Ann-Arbor-Detroit region, Michigan (bottom row).
3. Physical environment assessments
The curated GIS database compiled by the ABCD Study LED Environment Working Group includes both vector and raster data of multiple built and natural environmental contextual variables. As shown in Table 1 and outlined in greater detail below, various environmental datasets have been used to map environmental factors to the state-, census-, residential-level for ABCD Study participants to date.
Table 1.
Environmental Context Variables Currently Linked in the ABCD Study for baseline data(Year 1). Asterisk (*) indicates that this measure is available starting in Release 4.0.
| Domain | Measure | Description | Temporal Domain of Data | Spatial Resolution of Data | Citation or Data Source | Descriptive Statistics of ABCD |
|---|---|---|---|---|---|---|
| Built Environment Variables | ||||||
| Laws and Biases | Race Bias | Composite of multiple multi decade surveys tapping implicit and explicit attitudes at a state-wide level. | 2016 | State | Hatzenbuehler et al. (2021) | Range: -1.98–1.11 Mean (SD): -0.18 (0.74) |
| Gender Bias | Composite of multiple multi decade surveys tapping implicit and explicit attitudes as well as data on women’s economic and political status. | 2016 | State | Hatzenbuehler et al. (2021) | Range: -1.84–1.27 Mean (SD): -0.25 (0.90) |
|
| Ethnicity Bias | Composite of multiple multi decade surveys tapping implicit and explicit attitudes as well as data on state-level immigration policies. | 2016 | State | Hatzenbuehler et al. (2021) | Range: -1.75–0.64 Mean (SD): -0.48 (0.69) |
|
| Marijuana Laws | Categorization of current marijuana status as recreational, medicinal, low THC/CBD, or no legal access. | 2016 | State | http://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx and https://www.mpp.org/states/ | Proportion: 0.25 recreational 0.45 medical 0.29 low T/C 0.01 not legal |
|
| Urbanization | Gross Residential Density | Housing units per acre from EPA’s Smart Location Database. | Estimate from 2010 | Census Tract | Ramsey and Bell, 2014a2014, Ramsey and Bell, 2014b | Range: 0–219 Mean (SD): 3.96 (7.00) |
| Population Density | Population Count Adjusted to Match 2015 Revision of UN WPP Country Totals in persons per 1 km2. | Estimate from 2010 | Census Tract | https://beta.sedac.ciesin.columbia.edu/data/set/gpw-v4-population-density-adjusted-to-2015-unwpp-country-totals | Range: 0–60283 Mean (SD): 2189 (2658) |
|
| Urban Area | Categorical measure of whether a census block is “urban” (2500 or more people) or “rural” (less than 2500 people). | Estimate from 2010 | Census Tract | https://www.census.gov/programs-surveys/geography/about/faq/2010-urban-area-faq.html | Proportion: 0.09 Rural 0.03 Urban Clusters 0.87 Urbanized |
|
| National Walkability Index | Composite index ranking census block groups according to their walkability. | Estimate from 2010 | Census Tract | https://www.epa.gov/smartgrowth/smart-location-mapping#walkability | Range: 1.17–19.83 Mean (SD): 10.67 (4.07) |
|
| Traffic | Traffic counts modeled at the 1 km2 resolution. | Estimate from 2016 | Address Point | https://downloads.esri.com/esri_content_doc/dbl/us/Kalibrate_TrafficMetrixManual_Version140.pdf | Range: 0–157,145 Mean (SD): 12793 (11869) |
|
| Proximity to Roads | Number of meters away from major road or highway. | Estimate from 2016 | Address Point | https://nationalmap.gov/small_scale/mld/1roadsl.html | Range: 0.01–34314.62 Mean (SD): 1187 (1283) |
|
| Neighborhood Quality | Area Deprivation Index (ADI) | Composite index of a census tract’s socioeconomic disadvantage based on income, education, employment, and housing quality using data from the American Community Survey. | Average of annual estimates spanning 2010–2014 | Census Tract | Kind et al. (2014) | Weighted Sum - Range: 0–125.8 Mean (SD): 93.73 (23.22) |
| Social Vulnerability Index (SVI)* | Composite index of 15 census variables indicating an area’s potential need for support following a disaster. | Average of annual estimates spanning 2014–2018 | Census Tract | Flanagan et al. (2011) | Total Score - Range: 0–1 Mean (SD): 0.42 (0.30) |
|
| Opportunity Atlas (OA)* | Estimate of income in adulthood based on the Opportunity Atlas childhood census blocks for children born 1978–1983. | Average of annual estimates between 2014 and 2015 | Census Tract | https://www.opportunityatlas.org/ | Avg Score - Range: 0.22–0.78 Mean (SD): 0.52 (0.10) |
|
| Child Opportunity Index (COI) 2.0 * | Composite index of 29 variables tapping neighborhood conditions relevant to healthy child development. | Estimate from 2015 | Census Tract | Acevedo-Garcia et al. (2020) | Nationally normed overall COI - Range: 1–100 Mean (SD): 60.4 (30.5) |
|
| Crime | County level counts of arrests and offences from Uniform Crime Reporting Program Data. | 3 years average from 2010 | County | http://doi.org/10.3886/ICPSR33523.v2 | Grand total - Range: 0–348049 Mean (SD): 53268 (86316) |
|
| Lead Risk | Imputed estimate of lead exposure based on age of homes and poverty levels in census tract. | Average of annual estimates spanning 2010–2014 | Census Tract | Washington Tracking Network, Washington State Department of Health. Childhood lead risk map. https://fortress.wa.gov/doh/wtn/WTNPortal/ | Range: 0–10 Mean (SD): 5 (3.1) |
|
| Natural Environment Variables | ||||||
| Air Quality | Fine particulate (PM2.5) | Spatio-temporal model predictions measured in μg/m3 at 1 km2 resolution. | Annual average of daily estimates, maximum and minimum daily level in 2016 | Address Point | Di et al. (2019) | Range: 1.72–15.90 Mean (SD): 7.65 (1.58) |
| Nitrous dioxide (NO2) | Spatio-temporal model predictions measured in ppb (parts per billion) at 1 km2 resolution. | Annual average of daily estimates, maximum and minimum daily level in 2016 | Address Point | Di et al. (2020) | Range: 1.99–37.94 Mean (SD): 18.87 (6.03) |
|
| Ozone (O3) | Spatio-temporal model predictions measured in ppb (parts per billion) at 1 km2 resolution. | Annual average of daily estimates, maximum and minimum daily level in 2016 | Address Point | Requia et al. (2020) | Range: 29.85–54.27 Mean (SD): 41.66 (4.40) |
|
| Elevation and Climate | Elevation | Meters above sea level. | 2016 | Address Point | https://developers.google.com/maps/documentation/elevation/overview | Range: 0–2621 Mean (SD): 341.1 (501.7) |
| Temperature* | Maximum daily temperature (degrees Celsius) of seven days prior to MRI scan at 4 m2 resolution. | Daily estimates linked to multiple days prior to visit from January 2016 – June 2020 | Address Point | Daly et al. (2015) | Range: -19–45.6 Mean (SD): 21.7 (9.9) |
|
| Humidity* | Maximum daily vapor pressure deficit (hectopascals, hPa) of seven days prior to MRI scan at 4 m2 resolution. | Daily estimates linked to multiple days prior to visit from January 2016 – June 2020 | Address Point | Daly et al. (2015) | Range: 0–93.3 Mean (SD): 15.8 (10.6) |
|
3.1. Evidence of stigma and potential biases
Youth grow up in overlapping circles of cultural and socio-political contexts, from their local family and neighborhoods to the states and countries in which they live. We typically focus on the experience of stigma and bias at a relatively local level (e.g., family, local community members, peers). Critically, there are also important indicators of more systemic or structural bias reflected in social norms at the community or institutionalized laws, policies and practices that may either reflect the behavior of individuals or shape the behavior of individuals in youths’ local environment(s). However, we rarely directly examine the relationship between objective measures of systemic/structural bias and function in youth. The ABCD Study provides a novel opportunity to address such critical questions with empirical data, given the geographic variability of the sites involved in the ABCD Study, which affords significant divergence across youth in their exposure to such systemic biases. To address such questions, colleagues at Harvard University created state-level indicators of three types of structural stigma (Hatzenbuehler et al., 2021): gender (i.e., potential bias about women), race (i.e., potential bias about Black individuals), and ethnicity (i.e., potential bias about Latinx individuals). This information was linked to each youth in the ABCD Study as a function of their baseline site (state) of participation and does not yet include information about whether the child moved to a different state, which may have different state level indicators, at later visits.
To create these state-level measures, they used several types of data (described in detail in (Hatzenbuehler et al., 2021)). First, they obtained data about implicit and explicit attitudes about each of these three identity groups aggregated at the state-level, derived from large-scale projects that spanned several years: Project Implicit (years 2003–2018), the General Social Survey (years 1974–2014), and the American National Election Survey (1992–2016). Second, for information on gender, they obtained state-level data of women’s economic and political statuses (e.g., earning ratios, participation in the labor market and political office, business ownership, etc.) and information about reproductive policies, such as information about availability of abortion providers. Third, for information on attitudes towards Latinx individuals, they examined state-level policies on immigration, recognizing that many Latinx individuals are not immigrants but that such state-level policies likely influence the experience of all individuals in the community with that identity. These data can be used to examine how these state level biases interact with youth’s identities to predict a range of factors, such as educational experience, mental health, brain development, and substance use/abuse.
3.2. Marijuana laws
In the United States, public acceptance of cannabis use has increased (Johnston et al. 2020) alongside increased access because of broader cannabis legalization. Currently, 36 states have legalized either recreational or medical cannabis use. Early research suggests that cannabis legalization does not lead to increases in adolescent cannabis use (Cerdá et al., 2018, Sarvet et al., 2018). However, among younger adolescents (7th and 8th grade), greater exposure to cannabis advertisements was associated with greater use, intention to use, and positive expectancies (D’Amico et al. 2018). The difference in results as a function of age highlights the importance of understanding how cannabis regulations affect younger cohorts of children and adolescents who may have greater exposure to cannabis advertisement after living in an environment with legal access to cannabis for a longer period. Furthermore, the ABCD Study is an ideal dataset to examine the effects of cannabis legalization because there are 21 sites located in 17 states with various state cannabis policies. In addition, the ABCD Study is collecting detailed substance use data unlike other national surveys. Cannabis legalization categories were assigned to participants based on their state of residence. The four cannabis legalization categories are: 1. Recreational – allows adults to use cannabis for recreational purposes, 2. Medical – allows adults to use cannabis for medical conditions, 3. Low THC/CBD – allows adults to use cannabis that is low in THC and high in CBD for medical conditions, and 4. No legal access to cannabis – forbids access to cannabis. Information about states current cannabis laws were obtained from two websites: http://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx and https://www.mpp.org/states/.
3.3. Urbanicity
Urbanicity can provide information as to the impact of living in urban areas. Urbanicity indices may reflect the presence of environmental and social conditions that are more common in urban areas, such as pollution, congestion, and increased rates of social interactions. To date, various health factors have been linked to urbanicity, such as increases in overweight/obesity, increased calorie intake, decreased physical activity, increased drug and alcohol use, and mental health disorders, among many others (Evans et al., 2020, Rudolf et al., 2014; Stowe et al. 2019). In the ABCD Study, we have linked five measures of urbanicity to residential addresses, including two density measures (population and gross residential), census-tract derived metrics classifying the locations as urban or non-urban areas, walkability, and motor vehicle information including distance to roadway and traffic volumes.
Population density refers to the number of people living in a given unit of area (i.e., crowding). Differences in population density have been linked to psychological and environmental quality of life (Fassio et al., 2013), and has been shown to moderate relationships between the built environment and health outcomes (Liu et al. 2007). Thus, information about variability of population density (low versus high) may be important for contextualizing relationships between the build environment and health outcomes in the ABCD Study. As such, the population density from the Gridded Population of the World (GPW), provided by the Socioeconomic Data and Applications Center (SEDAC), has been linked to ABCD individual participant address information. National-level population estimates from 2010 used in this metric have been adjusted to the United Nations World Population estimates, which can often be corrected for over- or under-reporting (United Nations, 2021) and mapped to an ~1-km grid. Population density values represent persons per km2. Similarly, gross residential density is a measure of housing units per acre on unprotected land and is an alternative measure of crowding. This measure was obtained from the Smart Location Database created by the United States Environmental Protection Agency based on the 2010 Census Data (Ramsey and Bell, 2014b, Ramsey and Bell, 2014a2014) and also linked to ABCD Study individual addresses.
While many studies have documented the effects of increased urbanicity on child and adolescent health outcomes, few studies have focused on differential risk associated with living in a rural area relative to an urban area (Crouch et al., 2019, Curtis et al., 2011). Although the number of studies devoted to this topic are few, linking this information to the ABCD Study may provide an opportunity to further investigate both positive (Crouch et al. 2021) and negative (Crouch et al. 2020) impacts of living in an rural area. To classify individuals as living in a rural or urban area, urban-rural census tract variables from 2010 were mapped to each address. Based on this external database, the Census Bureau identifies two types of urban areas, including Urbanized Areas (UAs) of 50,000 or more people and Urban Clusters (UCs) of at least 2500, but less than 50,000 people. Rural areas are those that encompass all population, housing, and territory not included within an urban area (“Federal Register” 2011).
In urban places, city planning designs have limited the walkability between work, home, and recreational spaces, with distances too great to walk (Frank et al. 2006). Such reduction in walkability leads to fewer opportunities for physical activity and a risk for health. Understanding potential links between the walkability of the built environment of the child and physical and mental health outcomes is important in the context of the ABCD Study (Frank et al. 2006). A measure of walkability was linked to ABCD participant addresses using the National Walkability Index from the Smart Location Database created by the United States Environmental Protection Agency (https://www.epa.gov/smartgrowth/smart-location-mapping#walkability) based on 2010 census data. Walkability scores were calculated at the census-tract level, ranking each census tract on a range from 1 to 20 according to relative walkability. The walkability score is based on a weighted formula that uses ranked indicators as related to the propensity of walk trips. The ranked-indicator scores used in the weighted formula include a combination of diversity of employment types plus the number of occupied housing, pedestrian-oriented intersections, and proportion of workers who carpool.
Beyond population density and walkability, epidemiological studies have also reported associations between road proximity and brain health. Various neurodevelopment, cognitive functioning, and mental health outcomes have been linked to living near major roadways (Brunst et al., 2019, Ha et al., 2019, Pedersen and Mortensen, 2001a, Reuben et al., 2021, Wang et al., 2017). As such, the ABCD Study may be valuable to help understand how the distance of a child's home to major roadways as well as the daily traffic patterns on nearby roadways impacts cognitive and neurodevelopmental trajectories over time. Therefore, we have mapped road proximity and traffic volume estimates to residential addresses of the child in the ABCD Study to provide insight into both the major roadways nearby and how many cars and trucks typically utilize these roads. the geospatial coordinates of the major roads were obtained through the North American Atlas for roads, as last updated July 2012 (https://demographics5.arcgis.com/arcgis/rest/services/USA_Traffic_Counts/MapServer/0), and the shortest distance to a major roadway in meters was linked to participant’s residential addresses. Traffic count data linked to the residential address includes average annual daily traffic as published and managed from Kalibate and Esri for the 2018 calendar year and summarized at the 1-km2 spatial resolution (https://demographics5.arcgis.com/arcgis/rest/services/USA_Traffic_Counts/MapServer/0). These traffic counts are taken Sunday thru Saturday and seasonally adjusted to represent the average day of the year (https://demographics5.arcgis.com/arcgis/rest/services/USA_Traffic_Counts/MapServer/0).
3.4. Neighborhood quality
In the field of developmental cognitive neuroscience, socioeconomic status has traditionally been treated as an individual-level variable, specific to each family or person. However, socioeconomic status can also be attributed to neighborhoods and communities, which may represent an independent construct from family-level socioeconomic status (Taylor et al., 2020, Gibson et al., 2020, Wolf et al., 2017) with considerable effects on child development (Leventhal and Brooks-Gunn, 2000). In the ABCD Study, detailed questions are asked about socioeconomic and social factors at the family-level. Thus, the ABCD Study is an ideal dataset to examine the independent and multiplicative associations of family- and neighborhood-level socioeconomic status on adolescent health. Investigations with these ABCD data can elucidate the underlying mechanisms by which various contexts (i.e., family and neighborhood poverty or opportunity) uniquely influence development and potential emerging health disparities (Braveman and Barclay, 2009). Accordingly, the ABCD Study has incorporated the Area Deprivation Index measure of neighborhood-level socioeconomic status in past data releases, as well as information on crime and risk of lead (Pb) exposure. Moving forward, three additional metrics, including the Social Vulnerability Index, Opportunity Atlas, and the Child Opportunity Index, have been linked in the 4.0 annual data release.
3.4.1. Area deprivation index (ADI)
The ADI represents a composite multivariable metric of neighborhood disadvantage (i.e., socioeconomic status), with higher values representing greater disadvantage. Developed and popularized by Singh (2003), the ADI was initially constructed to determine how area deprivation was associated with mortality. However, as more pertinent to ABCD, per studies of related measures of neighborhood disadvantage, increased disadvantage is indirectly associated with children’s developmental outcomes (Elliot et al., 1996, Kohen et al., 2008) and adult health problems (Ross and Mirowsky, 2001) through other neighborhood- and/or family-level variables. The ABCD Study includes the composite ADI metrics, including the weighted ADI score and its national percentile, along with the 17 component variables used to create the composite scores at the census-tract level for participants’ primary, secondary, and tertiary addresses at baseline, all of which were derived from the 2011–2015 American Community Survery (ACS; https://www.census.gov/programs-surveys/acs). A description of the 17 component variables is included in Supplemental Table 2. The code used by the ABCD Study to compute the ADI is also available (https://github.com/ABCD-STUDY/geocoding/blob/master/Gen_data_proc.R).
3.4.2. Social vulnerability index (SVI)
The SVI, published by the Center for Disease Control (CDC), is a composite metric that can be used to identify which communities are most vulnerable to stressors such as natural disasters, human-caused disasters, and disease outbreaks (CDC/ATSDR’s Social Vulnerability Index (SVI), 2021; Flanagan et al. 2011). Like the ADI, the SVI incorporates 15 variables from the ACS, which are described in Supplemental Table 3. These 15 items are grouped into 4 themes: socioeconomic status (1−4), household composition and disability (5−8), minority status and language (9−10), and housing type and transportation (11−15). SVI is calculated by deriving percentiles of each variable (at the county or census-tract level), summing the percentiles within the theme, and summing these totals across themes, with higher values of SVI representing greater vulnerability to disaster and disease. Here, linking SVI to ABCD data provides the opportunity to better understand not only how environmental contexts are interrelated with adolescent development, but how environmental vulnerability to external stressors (and the presence of such stressors) may invoke downstream effects on developmental outcomes. The 4.0 annual release for the ABCD Study includes the census-tract level SVI for participants’ primary, secondary, and tertiary addresses.
3.4.3. Opportunity atlas
The neighborhoods in which children in America grow up can influence outcomes in adulthood. As such, the Opportunity Atlas (Chetty et al. 2018) estimates measures of average outcomes across 20,000 people in adulthood (born 1978–1983) according to the census tracts in which they grew up (i.e., childhood census tracts). The ABCD Study includes scores from the Opportunity Atlas that indicate the predicted 2014–2015 mean income earnings of adults aged 31–37 years that grew up in that census tract as children. Scores are provided based on the childhood census tracts of the Opportunity Atlas cohort, but we also provide the adult mean earnings disaggregated by parental household income percentiles based on the national income distribution during their childhood. For example, the mean income earnings at the 25th percentile rank correspond to the mean income earnings of adults whose parents were at the 25th percentile of the national income distribution. More information on the Opportunity Atlas can be found at https://opportunityinsights.org/policy/frequently-asked-questions/. Although the outcomes for census tracts are based on children who were born in those tracts between 1978 and 1983, Chetty et al. (2018) suggest that these longitudinal outcomes are best suited for measuring stable outcomes in earnings in adulthood. Linking measures from the Opportunity Atlas to the ABCD Study allows for objective measures of neighborhood economic opportunity (i.e., upward mobility) to study in relation to health outcomes in ABCD youth. However, while the Opportunity Atlas estimates can be used as predictors of economic opportunity for children today, it is important to combine these estimates with additional data to determine applicability to neighborhoods that have undergone substantial change in the last several decades.
3.4.4. Child opportunity index (COI) 2.0
There are vast differences in neighborhood access to opportunities and quality of conditions for children across America, including access to good schools and healthy foods, green spaces such as safe parks and playgrounds, safe housing and cleaner air. These inequitable neighborhood differences can negatively influence the current living conditions of a child, as well as development throughout childhood and subsequent health outcomes in adulthood (Acevedo-Garcia et al. 2014). Children who grow up in neighborhoods with access to more educational and health opportunities are more likely to grow up to be healthy adults. The COI 2.0 is a national contemporary measure of neighborhood opportunity, comprising a comprehensive dataset that aggregates 29 indicators of neighborhood conditions for 72,000 census tracts in the United States. Beginning with the ABCD 4.0 data release, the ABCD Study provides scores for the COI 2.0 overall index, and the three domain indices that comprise the overall index: (1) education (e.g., third grade reading and math proficiency, school poverty), (2) health and environment (e.g., access to green space and healthy food), and (3) social and economic opportunities (Acevedo-Garcia et al. 2020). We have also included scores for the 29 indicators that comprise the three domains. Detailed documentation describing the indicators that comprise each of the domains as well as the dataset source and year for each of the 29 indicators can be found in Supplemental Table 4 and the COI 2.0 technical documentation (Acevedo-Garcia et al. 2014). Given the diverse demographics of the ABCD Study participants, linking the COI 2.0 gives us objective measures of neighborhood opportunities for participants so that we can assess the influence of neighborhood quality on adolescent health and potential emerging health disparities.
3.4.5. Crime
Crime rates are an important neighborhood characteristic that can cause distress on individuals' mental well-being (Dustmann and Fasani, 2016) and has been linked with various children's developmental outcomes (Sharkey, 2010, Baranyi et al., 2021). However, the impact of crime within the context of other neighborhood variables and how these impact neural mechanisms during children’s development is less clear. To empower researchers to investigate the impact of local crime rates in the broader context of the built environment, we obtained county-level crime statistics from Uniform Crime Reporting Data (https://doi.org/10.3886/ICPSR33523.v2). In addition to the total crime rates, we also provided subcategories of the crime, including violent crimes, drug violations, drug sales, marijuana sales, drug possessions, and DUIs.
3.4.6. Risk of lead exposure
The removal of lead from gasoline (for on-road vehicles) and house paint has been associated with dramatic declines in childhood lead exposure, which, given lead’s effects on child development (Lanphear et al. 2005), has been regarded as one of the greatest public health achievements of the 20th century (Gilbert and Weiss, 2006). Unfortunately, exposure to lead remains a dire public health concern, as risk of exposure persists through lead-contaminated water pipes and ingestion of lead-contaminated dust and soil per leaded gas vehicular emissions and non-remediated lead-based paint (Gibson et al., 2020, Jacobs et al., 2002, Lanphear and Roghmann, 1997, Mielke et al., 2019; Roy and Edwards 2019). Collectively, children living in older homes are at greater risk of exposure (Jacobs et al. 2002). In 2016, Rad Cunningham at the Washington State Department of Health developed a nationwide map quantifying risk of lead exposure at the census-tract level, in which risk of lead exposure was a function of housing age and poverty rates (Frostenson, 2016). More specifically, “housing age” reflected the estimated number of homes in each census tract with lead-paint hazards based on decades of construction (e.g., lead-paint hazards would be more likely in homes built before 1940 than in homes built in the 1970 s). Marshall et al., 2020, Evans et al., 2020, Wheeler et al., 2019 reported that these lead-risk estimates were valid proxies of childhood lead exposure, in that, across several states and cities, there was a greater prevalence of elevated blood lead levels in census tracts with higher risk scores; further research will permit determining the extent to which these lead-risk scores are predictive of individuals’ observed blood-lead levels. Accordingly, the ABCD Study incorporated the aforementioned lead-risk scores using code freely available on GitHub (https://github.com/voxmedia/data-projects/blob/master/vox-lead-exposure-risk/calculate-lead-risk.py), to estimate census tract lead-risk scores of participants’ primary, secondary, and tertiary residential addresses.
3.5. Air quality
Air pollution, or the presence of toxic particulates and gases within the atmosphere, is one of the most widespread environmental issues affecting global health today. Adverse effects of air pollution exposure on mortality (Stieb, Judek, and Burnett, 2002), and morbidity (Anderson et al., 2012), as well as respiratory and cardiovascular health are well documented (Brunekreef and Holgate 2002), but a growing body of evidence suggests that air pollution exposure may also compromise brain development (Block and Calderón-Garcidueñas, 2009, Calderón-Garcidueñas et al., 2015) with long lasting effects on cognition (Guxens et al., 2014, Guxens et al., 2018) and mental health (Buoli et al., 2018, Gu et al., 2020, Khan et al., 2019, Power et al., 2015, Roberts et al., 2019). However, because of challenges to accurately model air pollution exposure and a dearth of well-powered longitudinal neuroimaging studies that span adolescence, much remains unknown regarding the effects of air pollution on neurocognitive development during adolescence (Herting et al. 2019). ABCD provides a unique opportunity to investigate the effects of air pollution exposure during critical developmental periods on adolescent brain development and behavior.
Using state-of-the-art air pollution modeling at high spatial resolution created by colleagues at Harvard University, ABCD provides a number of measures capturing participant’s residential exposure to three criteria ambient air pollutants: fine particulate (PM2.5), nitrous dioxide (NO2), and ozone (O3). These ambient air pollutant exposure estimates are derived from a hybrid spatiotemporal model at the 1 × 1 km2 spatial resolution (Di, 2020, Di et al., 2019, Requia et al., 2020). This hybrid model combines the strengths of satellite-based aerosol optical depth models, land-use regression, and chemical transport models. This model has previously been trained for the continental United States from 2000 to 2016 and tested with left-out monitors. Daily 1 × 1 km2 ambient exposure estimates were then averaged across the 2016 calendar year and linked to the nearest estimate of the 1 × 1 km2 grid for the latitude and longitudinal of the baseline residential addresses. In addition to computing average annual estimates for PM2.5, NO2, and O3, ABCD includes the minimum and maximum levels of all three pollutants in 2016 in the 4.0 annual release, as well as the number of days that PM2.5 levels exceeded the National Ambient Air Quality Standards (NAAQS) threshold of 35 µg/m3. By including this array of measures, researchers have the opportunity to gain insight into differential effects of long-term (i.e., annual average) versus focal (i.e., max level in a year) air pollution exposure, as well as the degree to which National Ambient Air Quality Standards’ thresholds are meaningful in terms of preventing adverse effects of air pollution exposure on the adolescent brain.
3.6. Elevation and climate
The existing literature suggests that temperature, including heat and cold stress, can negatively impact how the human body functions, and cognitive functioning is no exception (Laurent et al. 2018). Studies suggest heat waves can impact test scores across American high school students (Goodman et al. 2018) and that fluctuations in temperature may also increase symptom severity in individuals affected by certain neurological conditions (Obradovich et al. 2018). Moreover, climate change has already made temperatures hotter, producing more intensive heat waves in the U.S. (Patz et al. 2014). Thus, characterizing the climate that participants may have experienced at home prior to ABCD Study visits may be useful to determine how seasons or weather may relate to individual differences in brain functioning. By considering the climate, the ABCD Study holds the potential to answer pertinent questions regarding potential effects of hotter and/or greater fluctuations in temperature on brain function in today’s youth. Thus, to account for potential differences in climate, the ABCD Study has mapped temperature, humidity, and elevation to residential addresses as part of the 4.0 ABCD data release. Maximum daily temperature (℃) and vapor pressure deficit (VPD; hPa) data derived at the 30-arcsec (~800 m) spatial resolution from 1981 through June of 2020 (Daly et al., 2015), were mapped to the residential address for the 7 days prior to each individual’s baseline study visit. Given that temperature and air pressure also decrease as a function of elevation, for completeness, elevation was also mapped to the residential address using the Google Maps Elevation API (https://developers.google.com/maps/documentation/elevation/overview).
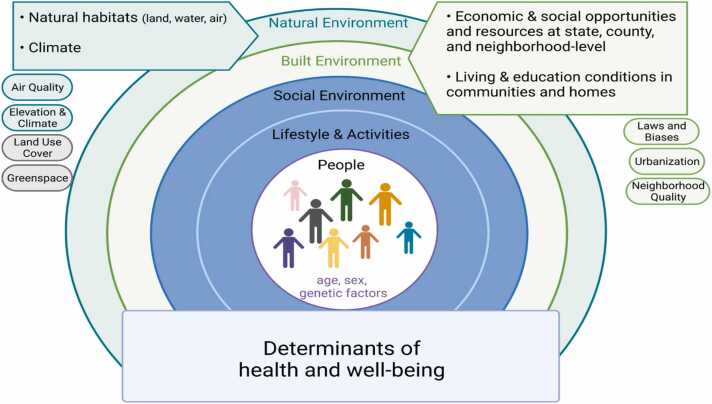
4. Strengths and limitations: considerations for the end user
The LED Environment Working Group strives to include additional information about the built and natural environments of all participants in the ABCD Study. These data provide an additional perspective about differences both between study sites and individual differences among children within even a single given study site location. Integrating these external environmental factors are likely important in considering both mediating and moderating effects and allows for important questions to be asked with implications for policies that may help ensure all children can thrive. That is, given the wealth of additional data collected in the ABCD Study, the addition of understanding the built and natural environment in ABCD provides the opportunity to think more broadly about how these factors may influence neurodevelopment of children within the established social determinants of health framework of public health (Fig. 4)(Dahlgren and Whitehead, 1991). Specifically, health outcomes, including neurodevelopment, cognition, and mental health as measured extensively by the ABCD Study, have been recognized to be influenced by complex interactions among environmental, social, and economic factors that are ultimately closely tied to one another (Mahler, 1980). Dahlgren and Whitehead (1991) provided a visual representation of such complex processes as a model of the main determinants of health and well-being in public health, which has since helped shape public health policy at both national and global scales (Braveman et al., 2011, Graham, 2010). Thus, capturing the broader physical environment makes the ABCD Study an ideal resource for researchers interested in studying how various distal and proximal factors may impact developing children and their health. While a number of development cognitive research studies have focused on individual factors, including socio-demographic factors (i.e. age, sex, genes, family-level socioeconomic status), lifestyle (e.g. physical activity, diet), and social environments (i.e. social relationships, social networks, cultural factors), additional natural and built environmental factors including neighborhood quality, community-level access to resources and opportunities, and exposure to harmful substances, provides an additional layer as to understanding and identifying key factors of neurodevelopment and to promote policies that lead to better health outcomes for all children across America. Specifically, these data can allow for researchers to examine if upstream built and natural factors (i.e. lack of greenspace, poor neighborhood walkability) might account for and/or moderate associations between physical activity and brain development, understanding the link between screen-time and mental health, determining how neighborhood conditions may impact the formation of peer groups, or exploring how recreational activities may moderate the relationship between adverse neighborhood conditions and mental health. In doing so, not only may we have a better understanding of the complex associations between the various factors contributing to neurodevelopment across childhood and adolescence, but research findings may also point to possible public health targets for intervention and treatment.
Fig. 4.
Adapted social determinants of health framework from (Barton and Grant, 2006) as first proposed by (Dahlgren and Whitehead, 1991) to visualize the role of how the natural and built environment are part of a larger complex process by which health and well-being are affected. Health outcomes, such as brain and cognitive development as measured in the ABCD Study, is influenced by a set of multi-faceted and interlocking factors, running from the broad physical environment (green) through more proximal measures including social environment, lifestyle factors (blue). For the physical environment, the LED Environment Working Group is tasked with identifying and linking residential geocodes to various external databases in hopes of characterizing these natural and built environmental contextual variables in the ABCD Study. Categories of the various existing types of environmental factors already linked to each child’s baseline residential address are illustrated in green and blue bubbles and correspond with those datasets described in detail in Table 1. Gray bubbles are planned natural environmental variables that will be linked in the future. Figure created with BioRender.com
While there are clear strengths in mapping the environmental context of today’s youth in the ABCD Study, there are also several important technical limitations as well as considerations for researchers planning to use and interpret these data. A vital consideration to this type of geospatial research and the variables derived from it, is the accuracy of the assignment of the exposure assessment at any given time. Several challenges arise in trying to maximize this accuracy. Any given geospatial database has both a spatial and temporal component. How these data were derived, and the degree of resolution is important to consider. For example, census tracts can be rather large, whereas in urban areas drastic differences in the environment can sometimes be noted to vary from street to street. Furthermore, individuals who live in the same census tract should not be considered to have the same experiences or the same amount of exposure in the neighborhood as others with similar demographics. Moreover, many times, geospatial databases are compiled after data is available from other sources, such as the American Community Survey or the Environmental Protection Agency. Thus, exposure estimates can often reflect a snapshot in time that may or may not overlap directly with the time period that the child was at that residential location; requiring the researcher to consider if the exposure of interest can or cannot be assumed to be stable beyond the temporal domains of the dataset. For example, many databases may create variables using 5-year averages (i.e. 2010–2014 calendar year data) that have then been linked to the baseline residential addresses which were collected in 2016–2018. Another technical challenge is that retrospective address collection is hindered by recall bias, or the differences in the accuracy or completeness of caregivers in the ABCD Study to recall address details over the 9–10 years prior to study enrollment. In addition, exposure assessment based on residential geospatial location also fails to capture individual data on percentage of time in which children in the current study spend time at their primary address versus other daily activities and/or various locations, such as in school. Of course, it is important to note that misclassification of exposure may be lower for children in that they may spend more of their time around the home, as compared to other populations such as adults who may spend more time commuting, time at work, or so forth. Although children do spend a substantial period of time at school, which may or may not be in a similar geographical location to that of their primary residence. Lastly, there is not a direct correlation between external environmental exposures to chemicals and internal exposure doses. For some environmental toxins, internal biomarkers exist to determine internal dose (e.g., metal exposures), whereas others, like air pollution, do not. Nonetheless, these geospatial factors can lead to misclassification, or information bias, which can severely affect observed associations between the exposure and the outcome. Therefore, given these limitations, it is important to note that while the current LED Environment measures may help provide a snapshot as to the built and natural environment surrounding ABCD participants’ residential homes, the current data fall short of fully characterizing participant exposomes. Thus, while continued efforts by the LED Environment Working Group aim to mitigate these challenges, findings should be interpreted considering these potential pitfalls, and misclassification should be acknowledged and discussed when necessary.
Another potential challenge for researchers using these data is conceptual and/or statistical collinearity and potential confounders. Environmental variables included from various databases can greatly overlap in terms of theoretical construct. For example, various factors may represent broad constructs of economic advantage, and many variables from the same databases may be highly collinear. It is also important to note that although some estimates may draw from similar linked databases (i.e. census-tract estimates from the US Census or the American Community Survey), they may implement any number of transformations or operations when computing measures. In addition to considering the exposure of interest from these data, a number of spatial contextual variables may also be important to consider as source(s) of confounding. For example, ecological variables, such as air pollution, may be an important spatial confounder in examining associations between neighborhood socioeconomic factors and child health outcomes in ABCD. Some models of exposures may also include other important geospatial or socioeconomic factors in establishing estimates of exposure, such as temperature and humidity in estimating ambient air pollution, or age of housing in compiling a metric for lead risk. Therefore, it is vital in the early stages of planning analyses with these data to consider the choice of which variables to use for a given construct, identifying potential ecological or spatial confounders, and understanding the raw datasets that were utilized in calculating various environmental and societal variables included in the ABCD Study. Additional sensitivity analyses should always be considered to evaluate the impact of potential confounds and the specificity of the tested environments.
Lastly, researchers should note that the environmental estimates do not represent the ‘lived’ or subjective experience of these exposures, with careful consideration given to the potential interpretation of any effects seen between these variables and brain and cognitive outcomes of interest. For example, these data are derived from outside databases that may capture an objective perspective of a given geospatial location, as they do not rely on the subjective report of the participants. However, these objective constructs do not necessarily reflect any individual’s subjective experience in a given state, census tract, or even residential neighborhood. It is likely that subjective experiences may moderate or mediate associations of external estimates of exposures. Further, neighborhood socioeconomic factors, environmental exposures, and potential health and behavioral outcomes should also be considered in light of local, state, and federal policies of racism, segregation, and inequality that has resulted in persistent inequalities in social, economic, and educational opportunities (Rothstein, 2017; Taylor, 2014; Washington, 2019; Zimring, 2017). For these reasons, socioeconomic and other family-level factors are likely to also be highly correlated to various built and natural exposure variables. Thus, thoughtful consideration is vital in reporting on potential exposure and outcome associations but also the nexus of neighborhoods, communities, and environmental justice and equity.
5. Future directions
The LED Environmental Working Group has primarily focused on baseline residential addresses to provide additional contextual information about the places where ABCD Study participants are growing up. In this process, we continually aim to implement ways to reduce exposure misclassification. Current efforts include historical reconstruction of each child’s residential history, which offers the opportunity to create a better understanding about each child’s physical environmental exposures across their lifespan. In doing so, quality assurance of retrospective residential addresses using commercial credit-reporting data is underway to help reduce recall bias (Hurley et al. 2017). Further, efforts are under way to improve syncing the temporal domains of linked database estimates with temporal changes in residential information for retrospective and prospective addresses. The ABCD Study’s Physical Health Working Group is also collecting biomarkers (i.e., blood, baby teeth, etc.) to measure exposure to some chemical toxins. Beyond improving exposure assessment, both the working group and its discussions with the greater larger scientific community has identified additional important linkage databases with other information regarding environmental toxins, urban settings, and neighborhood factors, such as greenspace and food deserts. The ABCD LED Environment Working Group envisions an ever-increasing resource for researchers who are keen to understand environmental impacts on the human brain.
Funding
Authors involved in the preparation of this article are supported by the Adolescent Brain Cognitive Development (ABCD) Study (https://abcdstudy.org). This is a multisite, longitudinal study designed to recruit more than 10,000 children age 9–10 and follow them over 10 years into early adulthood. The ABCD Study® is supported by the National Institutes of Health and Additional Federal Partners under award numbers U01DA041048, U01DA050989, U01DA051016, U01DA041022, U01DA051018, U01DA051037, U01DA050987, U01DA041174, U01DA041106, U01DA041117, U01DA041028, U01DA041134, U01DA050988, U01DA051039, U01DA041156, U01DA041025, U01DA041120, U01DA051038, U01DA041148, U01DA041093, U01DA041089, U24DA041123, U24DA041147. A full list of supporters is available at https://abcdstudy.org/federal-partners.html. A listing of participating sites and a complete listing of the study investigators can be found at https://abcdstudy.org/consortium_members/. ABCD consortium investigators designed and implemented the study and/or provided data but did not necessarily participate in analysis or writing of this report. Dr. Gayathri Dowling was substantially involved in all of the cited grants. The views and opinions expressed in this manuscript are those of the authors only and do not necessarily represent the views, official policy or position of the U.S. Department of Health and Human Services or any of its affiliated institutions or agencies or ABCD consortium investigators.
Additional support for portions of these data, including the estimates and assignment of ambient air pollution exposure and other neighborhood metrics to each subject’s residential address, was provided by the National Institutes of Health [NIEHS P30ES007048–23S1, 3P30ES000002–55S1, P01ES022845, R01 ES032295, R01 ES031074].
CRediT authorship contribution statement
Chun Chieh Fan: Conceptualization, Data curation, Funding acquisition, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft. Andrew Marshall: Data curation, Methodology, Validation, Visualization, Writing – original draft. Harry Smolker: Data curation, Methodology, Validation, Visualization, Writing – original draft. Marybel R. Gonzalez: Data curation, Methodology, Validation, Visualization, Writing – original draft. Susan F. Tapert: Investigation, Writing – review & editing. Deanna M. Barch: Data curation, Investigation, Methodology, Validation, Writing – review & editing. Elizabeth Sowell: Investigation, Writing – review & editing. Gayathri J. Dowling: Investigation, Writing – review & editing. Carlos Cardenas-Iniguez: Investigation, Writing – review & editing. Jessica Ross: Data curation, Writing – original draft. Wesley K. Thompson: Data curation, Investigation, Methodology, Validation. Megan M. Herting: Conceptualization, Data curation, Funding acquisition, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The LED Environment Working group readily relies on outside expertise in environmental exposure, environmental health, sociology, and spatial sciences to inform protocol development and linkage of exposure to geocoded data. Expertise and guidance on the topics of geocoding of residential address has come from Daniel Goldberg; air pollution exposure has come from JC Chen, Rob McConnell, and Joel Schwartz; Traffic counts were collated by Heresh Amini and provided by Joel Schwartz; Child Opportunity Atlas expertise is provided by Daniel Hackman; temperature and humidity data have been obtained and curated for data linkage by Scott Delaney, and the Social Vulnerability Index from those at the CDC. State level bias information was provided by Mark Hatzenbuehler and Katie McGlaughlin at Harvard.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.dcn.2021.101030.
Contributor Information
Chun Chieh Fan, Email: c9fan@ucsd.edu.
Megan M. Herting, Email: herting@usc.edu.
Appendix A. Supplementary material
Supplementary material
.
References
- Acevedo-Garcia D., McArdle N., Hardy E.F., Crisan U.I., Romano B., Norris D., Baek M., Reece J. The child opportunity index: improving collaboration between community development and public health. Health Aff. 2014;33(11):1948–1957. doi: 10.1377/hlthaff.2014.0679. [DOI] [PubMed] [Google Scholar]
- Anderson Jonathan O., Thundiyil Josef G., Stolbach Andrew. Clearing the air: a review of the effects of particulate matter air pollution on human health. J. Med. Toxicol. 2012;8(2):166–175. doi: 10.1007/s13181-011-0203-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antonsen Sussie, Mok Pearl L.H., Webb Roger T., Mortensen Preben B., McGrath John J., Agerbo Esben, Brandt J.ørgen, Geels Camilla, Jesper, Christensen H., Pedersen Carsten B. Exposure to air pollution during childhood and risk of developing schizophrenia: a national cohort study. Lancet Planet. Health. 2020;4(2):e64–e73. doi: 10.1016/S2542-5196(20)30004-8. [DOI] [PubMed] [Google Scholar]
- Baranyi Gergő., Di Marco Martín Hernán, Russ Tom C., Dibben Chris, Pearce Jamie. The impact of neighbourhood crime on mental health: a systematic review and meta-analysis. Soc. Sci. Med. 2021;282(August) doi: 10.1016/j.socscimed.2021.114106. [DOI] [PubMed] [Google Scholar]
- Barton Hugh, Grant Marcus. A health map for the local human habitat. J. R. Soc. Promot. Health. 2006;126(6):252–253. doi: 10.1177/1466424006070466. [DOI] [PubMed] [Google Scholar]
- Bell Kristina L., Purcell Juliann B., Harnett Nathaniel G., Goodman Adam M., Mrug Sylvie, Schuster Mark A., Elliott Marc N., Tortolero Emery Susan, Knight David C. White matter microstructure in the young adult brain varies with neighborhood disadvantage in adolescence. Neuroscience. 2021;466(July):162–172. doi: 10.1016/j.neuroscience.2021.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Block Michelle L., Calderón-Garcidueñas Lilian. Air pollution: mechanisms of neuroinflammation and CNS disease. Trends Neurosci. 2009;32(9):506–516. doi: 10.1016/j.tins.2009.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman Paula, Barclay Colleen. Health disparities beginning in childhood: a life-course perspective. Pediatrics. 2009;124(Supplement 3):S163–S175. doi: 10.1542/peds.2009-1100D. [DOI] [PubMed] [Google Scholar]
- Braveman Paula, Egerter Susan, Williams David R. The social determinants of health: coming of age. Ann. Rev. Public Health. 2011;32:381–398. doi: 10.1146/annurev-publhealth-031210-101218. [DOI] [PubMed] [Google Scholar]
- Brunekreef Bert, Holgate Stephen T. Air pollution and health. Lancet. 2002;360(9341):1233–1242. doi: 10.1016/S0140-6736(02)11274-8. [DOI] [PubMed] [Google Scholar]
- Brunst Kelly J., Ryan Patrick H., Altaye Mekibib, Yolton Kimberly, Maloney Thomas, Beckwith Travis, LeMasters Grace, Cecil Kim M. Myo-inositol mediates the effects of traffic-related air pollution on generalized anxiety symptoms at age 12 years. Environ. Res. 2019;175(August):71–78. doi: 10.1016/j.envres.2019.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buoli Massimiliano, Grassi Silvia, Caldiroli Alice, Silvia Carnevali Greta, Mucci Francesco, Iodice Simona, Cantone Laura, Pergoli Laura, Bollati Valentina. Is there a link between air pollution and mental disorders? Environ. Int. 2018;118:154–168. doi: 10.1016/j.envint.2018.05.044. [DOI] [PubMed] [Google Scholar]
- Bureau of the Census Census tracts for the 2020 census-final criteria. Fed. Regist. 2018;83(219):56277–56284. [Google Scholar]
- Calderón-Garcidueñas Lilian, Calderón-Garcidueñas Ana, Torres-Jardón Ricardo, Avila-Ramírez José, Kulesza Randy J., Angiulli Amedeo D. Air pollution and your brain: what do you need to know right now. Prim. Health Care Res. Dev. 2015;16(4):329–345. doi: 10.1017/S146342361400036X. [DOI] [PubMed] [Google Scholar]
- Campbell, J. , Michael , S. , 2011. Essentials of Geographic Information Systems. Open Textbook Library. 2011. https://open.umn.edu/opentextbooks/textbooks/67.
- CDC/ATSDR’s Social Vulnerability Index (SVI) , 2021. April 28, 2021. https://www.atsdr.cdc.gov/placeandhealth/svi/index.html.
- Cecil K.M. Effects of early low-level lead exposure on human brain structure, organization and functions. J. Dev. Origins Health Dis. 2011;2(1):17–24. doi: 10.1017/S2040174410000486. [DOI] [Google Scholar]
- Cerdá Magdalena, Sarvet Aaron L., Wall Melanie, Feng Tianshu, Keyes Katherine M., Galea Sandro, Hasin Deborah S. Medical marijuana laws and adolescent use of marijuana and other substances: alcohol, cigarettes, prescription drugs, and other illicit drugs. Drug Alcohol Depend. 2018;183(February):62–68. doi: 10.1016/j.drugalcdep.2017.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chetty Raj, Friedman John N., Hendren Nathaniel, Jones Maggie R., Porter Sonya R. National Bureau of Economic Research; 2018. The Opportunity Atlas: Mapping the Childhood Roots of Social Mobility. [DOI] [Google Scholar]
- Christian Hayley, Zubrick Stephen R., Foster Sarah, Giles-Corti Billie, Bull Fiona, Wood Lisa, Knuiman Matthew, Brinkman Sally, Houghton Stephen, Boruff Bryan. The influence of the neighborhood physical environment on early child health and development: a review and call for research. Health Place. 2015;33(May):25–36. doi: 10.1016/j.healthplace.2015.01.005. [DOI] [PubMed] [Google Scholar]
- Clifford Angela, Lang Linda, Chen Ruoling, Anstey Kaarin J., Seaton Anthony. Exposure to air pollution and cognitive functioning across the life course--a systematic literature review. Environ. Res. 2016;147(May):383–398. doi: 10.1016/j.envres.2016.01.018. [DOI] [PubMed] [Google Scholar]
- Costa e Silva Jorge Alberto, Steffen Ricardo E. Urban environment and psychiatric disorders: a review of the neuroscience and biology. Metabolism. 2019;100(November) doi: 10.1016/j.metabol.2019.07.004. [DOI] [PubMed] [Google Scholar]
- Crouch Elizabeth, Radcliff Elizabeth, Merrell Melinda A., Bennett Kevin J. Rural-urban differences in positive childhood experiences across a national sample. J. Rural Health. 2021;37(3):495–503. doi: 10.1111/jrh.12493. [DOI] [PubMed] [Google Scholar]
- Crouch Elizabeth, Probst Janice C., Radcliff Elizabeth, Bennett Kevin J., Hunt McKinney Selina. Prevalence of adverse childhood experiences (ACEs) among US children. Child Abuse Negl. 2019;92(June):209–218. doi: 10.1016/j.chiabu.2019.04.010. [DOI] [PubMed] [Google Scholar]
- Crouch Elizabeth, Radcliff Elizabeth, Probst Janice C., Bennett Kevin J., McKinney Selina Hunt. Rural-urban differences in adverse childhood experiences across a national sample of children. J. Rural Health. 2020;36(1):55–64. doi: 10.1111/jrh.12366. Official J. Am. Rural Health Assoc. Nat. Rural Health Care Assoc. [DOI] [PubMed] [Google Scholar]
- Curtis Alexa C., Waters Catherine M., Brindis Claire. Rural adolescent health: the importance of prevention services in the rural community. J. Rural Health. 2011;27(1):60–71. doi: 10.1111/j.1748-0361.2010.00319.x. [DOI] [PubMed] [Google Scholar]
- D’Amico Elizabeth J., Rodriguez Anthony, Tucker Joan S., Pedersen Eric R., Shih Regina A. Planting the seed for marijuana use: changes in exposure to medical marijuana advertising and subsequent adolescent marijuana use, cognitions, and consequences over seven years. Drug Alcohol Depend. 2018;188(July):385–391. doi: 10.1016/j.drugalcdep.2018.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly Christopher, Smith Joseph I., Olson Keith V. Mapping atmospheric moisture climatologies across the conterminous united states. PLoS One. 2015;10(10) doi: 10.1371/journal.pone.0141140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daneshparvar Maryam, Mostafavi Seyed-Ali, Jeddi Maryam Zare, Yunesian Masud, Mesdaghinia Alireza, Mahvi Amir Hossein, Akhondzadeh Shahin. The role of lead exposure on attention-deficit/ hyperactivity disorder in children: a systematic review. Iran. J. Psychiatry. 2016;11(1):1–14. [PMC free article] [PubMed] [Google Scholar]
- Di Q., Amini H., Shi L., Kloog I., Silvern R., Kelly J., M.B, Choirat C., Koutrakis P., Lyapustin A., Wang Y., Mickley L.J., Sabath Schwartz J. An ensemble-based model of PM2.5 concentration across the contiguous united states with high spatiotemporal resolution. Environ. Int. 2019;130(September) doi: 10.1016/j.envint.2019.104909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Qian, et al. Assessing NO2 concentration and model uncertainty with high spatiotemporal resolution across the contiguous United States using ensemble model averaging. Environ. Sci. Technol. 2020;54(3):1372–1384. doi: 10.1021/acs.est.9b03358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolores , A.G., Noelke , C. , McArdle , N. , Sofer , N. , Huntington , N. , Hardy , E., Huber, R., Baek, M., Reece, J. , 2020. “The Geography of Child Opportunity: Why Neighborhoods Matter for Equity.” [DOI] [PubMed]
- Dustmann Christian, Fasani Francesco. The effect of local area crime on mental health. Econ. J. 2016;126(593):978–1017. [Google Scholar]
- Elliot Delbert S., Julius Wilson William, Huizinga David, Sampson Robert J., Elliot Amanda, Rankin Bruce. The effects of neighborhood disadvantage on adolescent development. J. Res. Crime Delinq. 1996;33(4):389–426. doi: 10.1177/0022427896033004002. [DOI] [Google Scholar]
- Engemann Kristine, Bøcker Pedersen Carsten, Arge Lars, Tsirogiannis Constantinos, Mortensen Preben Bo, Svenning Jens-Christian. Residential green space in childhood is associated with lower risk of psychiatric disorders from adolescence into adulthood. Proc. Natl. Acad. Sci. 2019;116(11):5188–5193. doi: 10.1073/pnas.1807504116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans Brittany E., Huizink Anja C., Greaves-Lord Kirstin, Tulen Joke H.M., Roelofs Karin, der Ende Jan van. Urbanicity, biological stress system functioning and mental health in adolescents. PLoS One. 2020 doi: 10.1371/journal.pone.0228659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans Robert G., Stoddart Gregory L. Producing health, consuming health care. Soc. Sci. Med. 1990;31(12):1347–1363. doi: 10.1016/0277-9536(90)90074-3. [DOI] [PubMed] [Google Scholar]
- Fan Yingling, Das Kirti V., Chen Qian. Neighborhood green, social support, physical activity, and stress: assessing the cumulative impact. Health Place. 2011;17(6):1202–1211. doi: 10.1016/j.healthplace.2011.08.008. [DOI] [PubMed] [Google Scholar]
- Fassio Omar, Rollero Chiara, Piccoli Norma De. Health, quality of life and population density: a preliminary study on ‘contextualized’ quality of life. Soc. Indic. Res. 2013;110(2):479–488. doi: 10.1007/s11205-011-9940-4. [DOI] [Google Scholar]
- Federal Register, 2011. Urban Area Criteria for the 2010 Census. August 24, 2011. https://www.federalregister.gov/documents/2011/08/24/2011–21647/urban-area-criteria-for-the-2010-census.
- Flanagan Barry E., Gregory Edward W., Hallisey Elaine J., Heitgerd Janet L., Lewis Brian. A social vulnerability index for disaster management. J. Home. Security Emerg. Manag. 2011;8(1) doi: 10.2202/1547-7355.1792. [DOI] [Google Scholar]
- Frank Lawrence D., Sallis James F., Conway Terry L., Chapman James E., Saelens Brian E., Bachman William. Many pathways from land use to health: associations between neighborhood walkability and active transportation, body mass index, and air quality. J. Am. Plan. Assoc. 2006;72(1):75–87. doi: 10.1080/01944360608976725. [DOI] [Google Scholar]
- Frostenson, S. , 2016. Where Is the Lead Exposure Risk in Your Community?” Vox.Com. 2016. http://www.vox.com/a/lead-exposure-risk-map.
- Gibson Jacqueline MacDonald, Fisher Michael, Clonch Allison, MacDonald John M., Cook Philip J. Children drinking private well water have higher blood lead than those with city water. Proc. Nat. Acad. Sci. 2020;117(29):16898–16907. doi: 10.1073/pnas.2002729117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert Steven G., Weiss Bernard. A rationale for lowering the blood lead action level from 10 to 2μg/DL. Neuro Toxicol. Environ. Neurodev. Disord. 2006;27(5):693–701. doi: 10.1016/j.neuro.2006.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg Daniel W., Ballard Morven, Boyd James H., Mullan Narelle, Garfield Carol, Rosman Diana, Ferrante Anna M., Semmens James B. An evaluation framework for comparing geocoding systems. Int. J. Health Geogr. 2013;12(1):50. doi: 10.1186/1476-072X-12-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman, J. , Hurwitz , M. , Park , J. , Smith , J. 2018. Heat and Learning.” SSRN Scholarly Paper ID 3180724. Rochester, NY: Social Science Research Network. 10.2139/ssrn.3180724. [DOI]
- Göran , D. , Whitehead, M. , 1991. Policies and Strategies to Promote Social Equity in Health. Background Document to WHO - Strategy Paper for Europe. Institute for Futures Studies. https://ideas.repec.org/p/hhs/ifswps/2007_014.html.
- Graham Hilary. Where is the future in public health? Milbank Q. 2010;88(2):149–168. doi: 10.1111/j.1468-0009.2010.00594.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu Hejun, Yan Weiran, Elahi Ehsan, Cao Yuxia. Air pollution risks human mental health: an implication of two-stages least squares estimation of interaction effects. Environ. Sci. Pollut. Res. 2020;27(2):2036–2043. doi: 10.1007/s11356-019-06612-x. [DOI] [PubMed] [Google Scholar]
- Guxens M., Lubczyńska M.J., Muetzel R.L., Bueno A.D., Jaddoe V.W.V., Hoek G., van-der-Lugt A., Verhulst F.C., White T., Brunekreef B., Tiemeier H., El-Marroun H. Air pollution exposure during fetal life, brain morphology, and cognitive function in school-age children. Biol. Psychiatry. 2018;84(4):295–303. doi: 10.1016/j.biopsych.2018.01.016. [DOI] [PubMed] [Google Scholar]
- Guxens M.ònica, Garcia-Esteban Raquel, Giorgis-Allemand Lise, Forns Joan, Badaloni Chiara, Ballester Ferran, Beelen Rob, Cesaroni Giulia, Chatzi Leda, Agostini Maria de. Air pollution during pregnancy and childhood cognitive and psychomotor development: six european birth cohorts. Epidemiology. 2014;25:636–647. doi: 10.1097/EDE.0000000000000133. [DOI] [PubMed] [Google Scholar]
- Ha Sandie, Yeung Edwina, Bell Erin, Insaf Tabassum, Ghassabian Akhgar, Bell Griffith, Muscatiello Neil, Mendola Pauline. Prenatal and early life exposures to ambient air pollution and development. Environ. Res. 2019;174(July):170–175. doi: 10.1016/j.envres.2019.03.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haddad Leila, Schäfer Axel, Streit Fabian, Lederbogen Florian, Grimm Oliver, Wüst Stefan, Deuschle Michael, Kirsch Peter, Tost Heike, Meyer-Lindenberg Andreas. Brain structure correlates of urban upbringing, an environmental risk factor for schizophrenia. Schizophr. Bull. 2015;41(1):115–122. doi: 10.1093/schbul/sbu072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler Mark L., Weissman David G., McKetta Sarah, Lattanner Micah R., Ford Jessie V., Barch Deanna M., McLaughlin Katie A. Smaller hippocampal volume among black and latinx youth living in high-stigma contexts. BioRxiv. 2021 doi: 10.1101/2020.10.09.333328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herting Megan M., Younan Diana, Campbell Claire E., Chen Jiu-Chiuan. Outdoor air pollution and brain structure and function from across childhood to young adulthood: a methodological review of brain mri studies. Front. Public Health. 2019;7:332. doi: 10.3389/fpubh.2019.00332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurley Susan, Hertz Andrew, Nelson David O., Layefsky Michael, Von Behren Julie, Bernstein Leslie, Deapen Dennis, Reynolds Peggy. Tracing a path to the past: exploring the use of commercial credit reporting data to construct residential histories for epidemiologic studies of environmental exposures. Am. J. Epidemiol. 2017;185(3):238–246. doi: 10.1093/aje/kww108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs David E., Clickner Robert P., Zhou Joey Y., Viet Susan M., Marker David A., Rogers John W., Zeldin Darryl C., Broene Pamela, Friedman Warren. The prevalence of lead-based paint hazards in US housing. Environ. Health Perspect. 2002;110(10):A599–A606. doi: 10.1289/ehp.021100599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston, L., Miech , R. A. , O’Malley , P. , Bachman, J.G. , Schulenberg, J.E. , Patrick, M.E. , 2020. Monitoring the Future National Survey Results on Drug Use, 1975–2019: Overview, Key Findings on Adolescent Drug Use. Institute for Social Research. Institute for Social Research. https://eric.ed.gov/?id=ED604018.
- Keating, Daniel P., Hertzman Clyde. Guilford Press; New York: 1999. Developmental Health and the Wealth of Nations: Social, Biological, and Educational Dynamics. [Google Scholar]
- Khan Atif, Plana-Ripoll Oleguer, Antonsen Sussie, Brandt J.ørgen, Geels Camilla, Landecker Hannah, Sullivan Patrick F., Bøcker Pedersen Carsten, Rzhetsky Andrey. Environmental pollution is associated with increased risk of psychiatric disorders in the US and denmark. PLoS Biol. 2019;17(8) doi: 10.1371/journal.pbio.3000353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohen Dafna E., Leventhal Tama, Dahinten V.Susan, McIntosh Cameron N. Neighborhood disadvantage: pathways of effects for young children. Child Dev. 2008;79(1):156–169. doi: 10.1111/j.1467-8624.2007.01117.x. [DOI] [PubMed] [Google Scholar]
- Lambert Kelly G., Nelson Randy J., Jovanovic Tanja, Cerdá Magdalena. Brains in the city: neurobiological effects of urbanization. Neurosci. Biobehav. Rev. 2015;58(November):107–122. doi: 10.1016/j.neubiorev.2015.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanphear Bruce P., Roghmann Klaus J. Pathways of lead exposure in urban children. Environ. Res. 1997;74(1):67–73. doi: 10.1006/enrs.1997.3726. [DOI] [PubMed] [Google Scholar]
- Lanphear Bruce P., Hornung Richard, Khoury Jane, Yolton Kimberly, Baghurst Peter, Bellinger David C., Canfield Richard L., Dietrich Kim N., Bornschein Robert, Greene Tom. Low-level environmental lead exposure and children’s intellectual function: an international pooled analysis. Environ. Health Perspect. 2005;113(7):894–899. doi: 10.1289/ehp.7688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laurent Jose Guillermo Cedeño, Williams Augusta, Oulhote Youssef, Zanobetti Antonella, Allen Joseph G., Spengler John D. Reduced cognitive function during a heat wave among residents of non-air-conditioned buildings: an observational study of young adults in the summer of 2016. PLoS Med. 2018;15(7) doi: 10.1371/journal.pmed.1002605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal Tama, Brooks-Gunn Jeanne. The neighborhoods they live in: the effects of neighborhood residence on child and adolescent outcomes. Psychol. Bull. 2000;126(2):309–337. doi: 10.1037/0033-2909.126.2.309. [DOI] [PubMed] [Google Scholar]
- Liao Jiaqiang, Zhang Bin, Xia Wei, Cao Zhongqiang, Zhang Yimin, Liang Shengwen, Hu Ke, Xu Shunqing, Li Yuanyuan. Residential exposure to green space and early childhood neurodevelopment. Environ. Int. 2019;128(July):70–76. doi: 10.1016/j.envint.2019.03.070. [DOI] [PubMed] [Google Scholar]
- Liu Gilbert C., Wilson Jeffrey S., Qi Rong, Ying Jun. Green neighborhoods, food retail and childhood overweight: differences by population density. Am. J. Health Promot. AJHP. 2007;21(4 Suppl):317–325. doi: 10.4278/0890-1171–21.4 s.317. [DOI] [PubMed] [Google Scholar]
- Mahler H. Hospitals and health for all by the year 2000. Can. J. Public Health Rev. Canad. Sante Publique. 1980;71(5):347–349. [PubMed] [Google Scholar]
- Marshall Andrew T., Betts Samantha, Kan Eric C., McConnell Rob, Lanphear Bruce P., Sowell Elizabeth R. Association of lead-exposure risk and family income with childhood brain outcomes. Nat. Med. 2020;26(1):91–97. doi: 10.1038/s41591-019-0713-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mielke Howard W., Gonzales Christopher R., Powell Eric T., Laidlaw Mark A.S., Berry Kenneth J., Mielke Paul W., Egendorf Sara Perl. The concurrent decline of soil lead and children’s blood lead in new orleans. Proc. Nat. Acad. Sci. 2019;116(44):22058–22064. doi: 10.1073/pnas.1906092116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minh Anita, Muhajarine Nazeem, Janus Magdalena, Brownell Marni, Guhn Martin. A review of neighborhood effects and early child development: how, where, and for whom, do neighborhoods matter? Health Place. 2017;46(July):155–174. doi: 10.1016/j.healthplace.2017.04.012. [DOI] [PubMed] [Google Scholar]
- Obradovich Nick, Migliorini Robyn, Paulus Martin P., Rahwan Iyad. Empirical evidence of mental health risks posed by climate change. Proc. Nat. Acad. Sci. 2018;115(43):10953–10958. doi: 10.1073/pnas.1801528115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patz Jonathan A., Frumkin Howard, Holloway Tracey, Vimont Daniel J., Haines Andrew. Climate change: challenges and opportunities for global health. JAMA. 2014;312(15):1565–1580. doi: 10.1001/jama.2014.13186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen Carsten Bøcker, Mortensen Preben Bo. Family history, place and season of birth as risk factors for schizophrenia in denmark: a replication and reanalysis. Br. J. Psychiatry. 2001;179(1):46–52. doi: 10.1192/bjp.179.1.46. [DOI] [PubMed] [Google Scholar]
- Pedersen Carsten Bøcker, Mortensen Preben Bo. Evidence of a dose-response relationship between urbanicity during upbringing and schizophrenia risk. Arch. Gen. Psychiatry. 2001;58(11):1039–1046. doi: 10.1001/archpsyc.58.11.1039. [DOI] [PubMed] [Google Scholar]
- Pedersen Carsten Bøcker, Mortensen Preben Bo. Urbanization and traffic related exposures as risk factors for schizophrenia. BMC Psychiatry. 2006;6:2. doi: 10.1186/1471-244X-6-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Power Melinda C., Kioumourtzoglou Marianthi-Anna, Hart Jaime E., Okereke Olivia I., Laden Francine, Weisskopf Marc G. The relation between past exposure to fine particulate air pollution and prevalent anxiety: observational cohort study. BMJ. 2015:h1111. doi: 10.1136/bmj.h1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rakesh Divyangana, Seguin Caio, Zalesky Andrew, Cropley Vanessa, Whittle Sarah. Associations between neighborhood disadvantage, resting-state functional connectivity, and behavior in the adolescent brain cognitive development study: the moderating role of positive family and school environments. Biol. Psychiatry Cogn. Neurosci. Neuroimag. 2021;6(9):877–886. doi: 10.1016/j.bpsc.2021.03.008. [DOI] [PubMed] [Google Scholar]
- Rakesh Divyangana, Cropley Vanessa, Zalesky Andrew, Vijayakumar Nandita, Allen Nicholas B., Whittle Sarah. Neighborhood disadvantage and longitudinal brain-predicted-age trajectory during adolescence. Dev. Cogn. Neurosci. 2021;51(October) doi: 10.1016/j.dcn.2021.101002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramsey, K. , Bell, A. 2014a. Smart Location Database, Environmental Protection Agency. 2014.
- Ramsey Kevin, Bell Alexander. The smart location database: a nationwide data resource characterizing the built environment and destination accessibility at the neighborhood scale. Cityscape. 2014;16(2):145–162. [Google Scholar]
- Requia W.J., Di Q., Sivern R., Kelly J.T., Kautrakis P., Mickley L.J., Sulprizio M.P., Amini H., Shi L., Schwartz J. An ensemble learning approach for estimating high spatiotemporal resolution of ground-level ozone in the contiguous United States. Environ. Sci. Technol. 2020;54(18) doi: 10.1021/acs.est.0c01791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reuben A., Arseneault L., Beddows A., Beevers S.D., Moffitt T.E., Ambler A., R.M, Newbury J.B., Odgers C.L., Schaefer J.D., Latham Fisher H.L. Association of air pollution exposure in childhood and adolescence with psychopathology at the transition to adulthood. JAMA Network Open. 2021;4(4) doi: 10.1001/jamanetworkopen.2021.7508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts Susanna, Arseneault Louise, Barratt Benjamin, Beevers Sean, Danese Andrea, Odgers Candice L., Moffitt Terrie E., Reuben Aaron, Kelly Frank J., Fisher Helen L. Exploration of NO2 and PM2.5 air pollution and mental health problems using high-resolution data in london-based children from a UK longitudinal cohort study. Psychiatry Res. 2019;272(February):8–17. doi: 10.1016/j.psychres.2018.12.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross Catherine E., Mirowsky John. Neighborhood disadvantage, disorder, and health. J. Health Soc. Behav. 2001;42(3):258–276. doi: 10.2307/3090214. [DOI] [PubMed] [Google Scholar]
- Rothstein Richard. Liveright Publishing; 2017. The Color of Law: A Forgotten History of How Our Government Segregated America. [Google Scholar]
- Roy Siddhartha, Edwards Marc A. Preventing another lead (Pb) in drinking water crisis: lessons from the washington DC and flint MI contamination events. Curr. Opinion Environ. Sci. Health. 2019;7:34–44. [Google Scholar]
- Rudolf K.E., Stuart E.A., Glass T.A., Merikangas K.R. Neighborhood disadvantage in context: the influence of urbanicity on the association between neighborhood disadvantage and adolescent emotional disorders. Soc. Psychiatry Psychiatr. Epidemiol. 2014;49:467–475. doi: 10.1007/s00127-013-0725-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarvet Aaron L., Wall Melanie M., Keyes Katherine M., Cerdá Magdalena, Schulenberg John E., O’Malley Patrick M., Johnston Lloyd D., Hasin Deborah S. Recent rapid decrease in Adolescents’ perception that marijuana is harmful, but no concurrent increase in use. Drug Alcohol Depend. 2018;186(May):68–74. doi: 10.1016/j.drugalcdep.2017.12.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharkey P. The acute effect of local homicides on children’s cognitive performance. Proc. Nat. Acad. Sci. 2010;107(26):11733–11738. doi: 10.1073/pnas.1000690107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh Gopal K. Area deprivation and widening inequalities in US mortality, 1969–1998. Am. J. Public Health. 2003;93(7):1137–1143. doi: 10.2105/ajph.93.7.1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stieb David M., Judek Stan, Burnett Richard T. Meta-analysis of time-series studies of air pollution and mortality: effects of gases and particles and the influence of cause of death, age, and season. J. Air Waste Manag. Assoc. 2002;52(4):470–484. doi: 10.1080/10473289.2002.10470794. [DOI] [PubMed] [Google Scholar]
- Stowe Ellen W., Hughey S.Morgan, Hallum Shirelle H., Kaczynski Andrew T. Associations between walkability and youth obesity: differences by urbanicity. Child. Obes. 2019;15(8):555–559. doi: 10.1089/chi.2019.0063. [DOI] [PubMed] [Google Scholar]
- Taylor Dorceta. NYU Press; 2014. Toxic Communities: Environmental Racism, Industrial Pollution, and Residential Mobility. [Google Scholar]
- Taylor Rita L., Cooper Shelly R., Jackson Joshua J., Barch Deanna M. Assessment of neighborhood poverty, cognitive function, and prefrontal and hippocampal volumes in children. JAMA Netw. Open. 2020;3(11) doi: 10.1001/jamanetworkopen.2020.23774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thurston G.D., Kipen H., Annesi-Maesano I., Balmes J., Brook R.D., Cromar K., S, Forastiere F., Forsberg B., Frampton M.W., Grigg J., Heederik D., Kelly F.J., Kuenzli N., Laumbach R., Peters A., Rajagopalan S.T., Rich D., Ritz B., Samet J.M., Sandstrom T., Sigsgaard T., Sunyer J., De Matteis Brunekreef B. A joint ERS/ATS policy statement: what constitutes an adverse health effect of air pollution? An analytical framework. Eur. Respir. J. 2017;49(1) doi: 10.1183/13993003.00419-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations . n.d. World Population Prospects in 2011, United Nations. (Accessed 1 June 2021). https://population.un.org/wpp/.
- Volk H.E., Perera F., Braun J.M., Kingsley S.L., Gray K., Buckley J., J.E, Croen L.A., Eskenazi B., Herting M., Just A.C., Kloog I., Margolis A., McClure L.A., Miller R., Levine S., Wright R., Clougherty Environmental influences on Child Health O. Prenatal air pollution exposure and neurodevelopment: a review and blueprint for a harmonized approach within ECHO. Environ. Res. 2021;196(May) doi: 10.1016/j.envres.2020.110320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Pan, Tuvblad Catherine, Younan Diana, Franklin Meredith, Lurmann Fred, Wu Jun, Baker Laura A., Chen Jiu-Chiuan. Socioeconomic disparities and sexual dimorphism in neurotoxic effects of ambient fine particles on youth iq: a longitudinal analysis. PLoS One. 2017;12(12) doi: 10.1371/journal.pone.0188731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washington, Harriet A. 2019. A Terrible Thing to Waste: Environmental Racism and Its Assault on the American Mind. Hachette UK.
- Wheeler David C., Resa M.Jones, Schootman Mario, Nelson Erik J. Explaining variation in elevated blood lead levels among children in minnesota using neighborhood socioeconomic variables. Sci. Total Environ. 2019;650:970–977. doi: 10.1016/j.scitotenv.2018.09.088. [DOI] [PubMed] [Google Scholar]
- Wild Christopher Paul. The exposome: from concept to utility. Int. J. Epidemiol. 2012;41(1):24–32. doi: 10.1093/ije/dyr236. [DOI] [PubMed] [Google Scholar]
- Wolf, S. , Katherine , A. Magnuson, Kimbro, R.T, 2017. Family Poverty and Neighborhood Poverty: Links with Children’s School Readiness before and after the Great Recession. Children and Youth Services Review 79 (August): 368–384. 10.1016/j.childyouth.2017.06.040. [DOI] [PMC free article] [PubMed]
- Woolf Steven H., Aron Laudan Y. U.S. Health in International Perspective: Shorter Lives, Poorer Health. The National Academies Press; Washington, D.C: 2013. National Academies (U.S.), and Institute of Medicine (U.S.). Physical and Social Environmental Factors.〈https://www.ncbi.nlm.nih.gov/books/NBK154491/〉 [PubMed] [Google Scholar]
- Younan D., Tuvblad C., Li L., Wu J., Lurmann F., Franklin M., K, McConnell R., Wu A.H., Baker L.A., Berhane Chen J.C. Environmental determinants of aggression in adolescents: role of urban neighborhood greenspace. J. Am. Acad. Child Adolesc. Psychiatry. 2016;55(7):591–601. doi: 10.1016/j.jaac.2016.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimring Carl A. NYU Press; 2017. Clean and White: A History of Environmental Racism in the United States. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material