Abstract
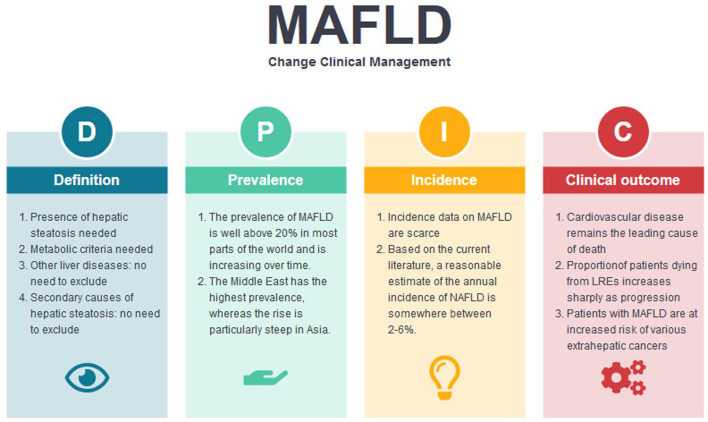
Metabolic (dysfunction)-associated fatty liver disease (MAFLD) is currently the most common chronic liver disease and affects at least a quarter of the global adult population. It has rapidly become one of the leading causes of hepatocellular carcinoma and cirrhosis in Western countries. In this review, we discuss the nomenclature and definition of MAFLD as well as its prevalence and incidence in different geographical regions. Although cardiovascular disease remains the leading cause of death in MAFLD patients, the proportion of patients dying from hepatic complications increases sharply as the disease progresses to advanced liver fibrosis and cirrhosis. In addition, patients with MAFLD are at increased risk of various extrahepatic cancers. Although a causal relationship between MAFLD and extrahepatic cancers has not been established, clinicians should recognize the association and consider cancer screening (e.g., for colorectal cancer) as appropriate.
Keywords: Nonalcoholic fatty liver disease, Nonalcoholic steatohepatitis, Obesity, Prevalence, Incidence, Hepatocellular carcinoma, Cirrhosis
Graphical abstract
Introduction
Metabolic (dysfunction)-associated fatty liver disease (MAFLD) is the most common chronic liver disease, affecting at least a quarter of the global adult population.1 In the Western world, MAFLD has already become one of the leading causes of cirrhosis, end-stage liver disease, and hepatocellular carcinoma (HCC).2 Although the same has not happened in Asia yet, studies from Japan and Korea have clearly documented a rapid rise in non-viral hepatitis-related HCC.3 Modeling studies also suggest that HCC, hepatic decompensation and liver-related death from MAFLD would increase significantly from 2015 to 2030 in essentially all countries.4,5
Because of the strong association between MAFLD and the metabolic syndrome, cardiovascular disease (CVD) is the leading cause of death in MAFLD patients.6 Nonetheless, the relative importance of various causes of death depends on the severity of MAFLD. In a multicenter retrospective cohort study, Vilar-Gomez et al.7 showed that liver disease was the leading cause of death in MAFLD patients with F3-4 fibrosis.
In this review, we first describe the concept of MAFLD, followed by the global prevalence and incidence of the disease. We also discuss the various hepatic and non-hepatic clinical outcomes in patients with MAFLD.
MAFLD vs. nonalcoholic fatty liver disease (NAFLD)
In 2020, Mohammed Eslam, Jacob George and hepatologists from various countries proposed to change the nomenclature of NAFLD to MAFLD.8 This was to address a number of limitations of the term NAFLD. For a disease that affects at least a quarter of the general population, it would be reasonable to have a positive diagnosis by describing what it is instead of a negative diagnosis by stating what it is not.9 The new term is also supposed to describe the heterogeneous pathophysiology of fatty liver disease better. In addition, professional societies and patient advocacy groups highlighted potential stigmatization with a name that includes the term “alcoholic”, and the prefix “non” may trivialize the condition.10
After the publication of the proposal, a number of professional societies have declared support for the name change.11–13 The Asian Pacific Association for the Study of the Liver issued the first management guidelines of MAFLD.14 Nonetheless, some hepatologists opposed the proposal, highlighting the potential negative impact on disease awareness and drug development as well as the ambiguity of metabolic dysfunction.15,16 A recent review article, on the other hand, reminds us of the importance of focusing on evidence in this debate.17 In addition, feedback from representatives of patient advocacy groups, primary care physicians and non-hepatologists does not suggest that the name change would negatively impact disease awareness.10,18–20 Currently, the European and American liver associations are organizing a platform to discuss this issue.
It is important to note that the MAFLD proposal changes not only the name but also the definition of the disease (Table 1). In the original definition, one may diagnose NAFLD when a patient has hepatic steatosis and no other liver diseases or secondary causes of hepatic steatosis. In contrast, to make the diagnosis of MAFLD, the patient should have hepatic steatosis as well as overweight or obesity, type 2 diabetes mellitus (T2D), or two or more other metabolic risk factors.8 On the other hand, a patient may have MAFLD and other chronic liver diseases at the same time. Thus, the terms MAFLD and NAFLD are not interchangeable, and this would in turn impact our understanding of the epidemiology of the disease.
Table 1. Definitions of MAFLD and NAFLD.
| MAFLD | NAFLD | |
|---|---|---|
| Presence of hepatic steatosis | Yes | Yes |
| Metabolic criteria | The diagnosis is made if a patient has hepatic steatosis and is overweight or obese, has T2D, or two or more of the following: Central obesity by ethnic-specific waist circumference cutoffs; Blood pressure ≥135/85 mmHg or specific drug treatment; Plasma triglycerides ≥150 mg/dL or specific drug treatment; Plasma HDL-cholesterol <40 mg/dL for men and <50 mg/dL for women or specific drug treatment; Fasting plasma glucose ≥100 mg/dL, 2-h post-load glucose ≥140 mg/dL, or hemoglobin A1c ≥5.7%; Homeostasis model assessment of insulin resistance ≥2.5; Plasma high-sensitivity C-reactive protein >2 mg/L | Not required |
| Other liver diseases | No need to exclude; a patient can have MAFLD and another liver disease at the same time | By definition, the presence of another liver disease (e.g., chronic viral hepatitis, autoimmune liver disease) would lead to the exclusion of NAFLD |
| Secondary causes of hepatic steatosis | No need to exclude; also use the term “alternative causes” instead of “secondary causes” | By definition, the presence of secondary causes of hepatic steatosis (e.g., use of systemic steroids, total parenteral nutrition) would lead to the exclusion of NAFLD |
HDL, high density lipoprotein; MAFLD, metabolic (dysfunction)-associated fatty liver disease; NAFLD, nonalcoholic fatty liver disease; T2D, type 2 diabetes.
For the purpose of this review series, we distinguish studies on MAFLD from those on NAFLD, wherever possible. Nonetheless, for historical reasons, most studies were on NAFLD and did not include the metabolic criteria.
Prevalence of MAFLD/NAFLD
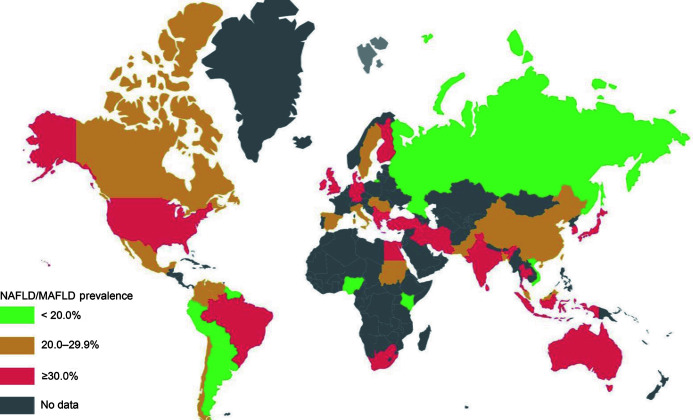
In this section, we review the prevalence of MAFLD in different regions (Fig. 1, Table 2). It is noteworthy that it is potentially misleading to compare studies directly as they differ in study methods (e.g., imaging studies are more sensitive than abnormal liver enzymes for the detection of MAFLD), settings (healthy volunteers, random selection from the general population, special groups) and period. In particular, as the prevalence of MAFLD is on the rise in almost all regions, recent data can differ a lot from those obtained 20 years ago. Furthermore, because MAFLD and NAFLD have different definitions, they include similar but slightly different individuals in epidemiological studies. In a few prevalence studies, around 90% of people with fatty liver would fulfill both the MAFLD and NAFLD criteria.21,22 Around 5% of fatty liver patients would not fulfill the metabolic criteria of MAFLD, whereas around 5% of patients would not be considered to have NAFLD because of concomitant liver diseases or excessive alcohol consumption.
Fig. 1. Global prevalence of MAFLD/NAFLD.
MAFLD, metabolic (dysfunction)-associated fatty liver disease; NAFLD, nonalcoholic fatty liver disease.
Table 2. Prevalence and incidence of NAFLD in different regions.
| Continent | Country/region | Prevalence, % | Incidence, per 1,000 person-years |
|---|---|---|---|
| North America | 11.1–46.0 | Not available | |
| USA | 11.1–46.0 | Not available | |
| Mexico | 14.3 | Not available | |
| South America | 23.4–35.3 | Not available | |
| Brazil | 35.3 | Not available | |
| Colombia | 26.6 | Not available | |
| Chile | 23.4 | Not available | |
| Europe | 4.0–49.6 | 18.5 | |
| UK | 26.4 | Not available | |
| France | 26.8 | Not available | |
| Spain | 25.8 | Not available | |
| Italy | 4.0–49.6 | 18.5 | |
| Germany | 30.0 | Not available | |
| Romania | 20.0 | Not available | |
| Hungary | 22.6 | Not available | |
| Finland | 41.2 | Not available | |
| Netherlands | 33.9 | Not available | |
| Asia | 23.3–31.9 | 44.8–57.4 | |
| China | 12.5–29.9 | 47.0–81.3 | |
| Japan | 17.3–19.6 | 26.3–31.7 | |
| South Korea | 27.0–28.8 | 37.9–52.9 | |
| India | 10.0–25.0 | Not available | |
| Taiwan | 11.5–50.1 | Not available | |
| Hong Kong | 23.1–28.5 | 30.0–47.0 | |
| Singapore | 22.0–29.4 | Not available | |
| Malaysia | 22.7–49.6 | Not available | |
| Sri Lanka | 31.0–34.3 | Not available | |
| Middle East | 13.5–58.2 | Not available | |
| Saudi Arabia | 16.6–22.5 | Not available | |
| Turkey | 51.1–59.1 | Not available | |
| Israel | 23.9–39.5 | 19.34–40.57 | |
| Iran | 12.9–17.9 | Not available | |
| Africa | 5.7–28.7 | Not available | |
| Nigeria | 1.2–16.7 | Not available | |
| Sudan | 12.7–29.2 | Not available |
NAFLD, nonalcoholic fatty liver disease.
North America
Several studies used the National Health and Nutrition Examination Survey (NHANES) data to determine the prevalence of MAFLD in the USA. One study used data in 2011–2018 and reported a prevalence of MAFLD of 34.8%.23 Another study focused on data in 2017–2018 and reported a prevalence of 39.1%.24 The difference was due to the method used to diagnose fatty liver. The first study used the fatty liver index (FLI) but the second one used the controlled attenuation parameter measurement by vibration-controlled transient elastography. The prevalence of MAFLD varied by ethnicity, with the highest prevalence seen among Hispanic Americans (51.4%) and the lowest among African Americans (21.5%).23
In the past decades, extensive studies have been conducted to accurately determine the prevalence of NAFLD in the North America. These data were summarized in a recent meta-analysis, which reported the global prevalence of NAFLD.25 In this paper, the prevalence of NAFLD in North America was about 24.1%, which was lower than that of MAFLD. The prevalence of nonalcoholic steatohepatitis (NASH) among NAFLD patients in North America was about 21%. Most of the studies included in the meta-analysis used imaging methods (mostly ultrasonography) to estimate the prevalence of NAFLD. The prevalence of NAFLD in Americans as estimated by any other methods (including FLI, International Classification of Diseases [ICD] codes) was about 21.1%, which suggested that the diagnosis of NAFLD based on blood test or ICD code alone can lead to underestimation. Studies on the prevalence of NAFLD from other North American countries are scarce. A retrospective study from Mexico that included 2,503 subjects reported a prevalence of NAFLD of 14.3%.26 Differences in the genetic background, environment, presence of metabolic syndrome and other factors account for the varying prevalence of NAFLD in North America. The prevalence of NAFLD is reported to be highest in Hispanic Americans, followed by Americans of European descent, and lowest in African Americans.27 The prevalence of NAFLD might also be different within certain ethnic groups among Americans, according to the country of origin.28 Additionally, the regional and ethnic differences in terms of obesity prevalence were significant in the USA; African Americans exhibited a higher prevalence of severe obesity than other ethnicities, and obesity is more prevalent in Texas than the rest of the country.29
South America
So far, there has been no report on the prevalence of MAFLD in South America, and data on the epidemiology of NAFLD are also scant. In the meta-analysis of Younossi et al.,25 the prevalence of NAFLD in South America was about 30.5%, which was among the highest worldwide. The inclusion population reporting the prevalence of NAFLD in South America varied greatly. A Brazilian study that enrolled middle-aged and older adults showed that NAFLD was present in 35.2% of the subjects.30 Studies from other South American countries reported somewhat lower prevalences. A study from Colombia that included 263 young males reported a prevalence of 26.6%.31 Another study from Chile showed that 23.4% of the subjects was suspected of NAFLD.32 However, most of these studies were performed over a decade ago and cannot reflect the current situation.
Europe
Epidemiological studies of MAFLD in Europe are scant. One study published with the UK biobank data, involving 423,252 participants, showed the prevalence of MAFLD was 38.0%.33 The prevalence of NAFLD in Europe varied widely from 4% to more than 40%.25 The study of Younossi et al.25 reported an average prevalence of 23.7% in Europe. Most of the studies were from Western Europe. Unlike studies in the USA, few studies have investigated the ethnicity discrepancies in Europe. The studies on the prevalence of NAFLD were mainly conducted by different countries. The prevalence of NAFLD was 25.8% in the adult population of Spain.34 The prevalence of NAFLD in Italy was reported to be 22.6%, from the study by Bedogni et al.35 NAFLD prevalences in the UK and France were similar. A large prospective primary care cohort in the UK indicated that the prevalence of NAFLD was 26.4%.36 The study from France included 272 patients undergoing liver biopsy, and simple steatosis was present in 26.8% of the patients.37 Haring and colleagues38 reported a prevalence of ultrasonographic hepatic steatosis of around 30% among 4,160 subjects. Data of the epidemiology of NAFLD in Eastern Europe is scant. In a prospective cohort of 3,005 hospitalized patients in Romania, 20% had NAFLD by ultrasonography.39 A similar prevalence was observed in a study from Hungary; indeed, Tarnoki et al.40 reported a 22.6% prevalence of ultrasonographic fatty liver.
Asia-Pacific region
The prevalence of MAFLD has been increasing in the Asia-Pacific region over the past few decades. A recent systematic review and meta-analysis of 237 studies and 13,044,518 participants from Asia suggested that the overall prevalence of NAFLD in adults in Asia, regardless of diagnostic method, was 29.62%.41 NAFLD prevalence varies widely within the Asia-Pacific region with disparities in economic, political and educational development, and also with variations in nutrition and lifestyle behavior.27 In China, the MAFLD prevalence in Xinxiang, Henan Province (central China) was 29.85% in 2017;42 in other regions of China, NAFLD prevalences in Shanghai (east China), Guangdong (south China) and Chengdu (southwest China) were 15.35%, 15.0% and 12.5%, respectively.43–45 The prevalence rate was significantly higher in urban areas (23.0%) than in rural areas (12.9%) in South China. In Hong Kong, Wong et al.21 reported that the population prevalence of MAFLD and NAFLD was 25.9% (95% confidence interval [CI]: 23.2–28.7%) and 25.7% (95% CI: 23.1–28.5%), respectively. In Taiwan, the prevalence of NAFLD was reported to be 11.5% in the general community, but much higher in the elderly (50.1% prevalence).46 In South Korea, the prevalences of NAFLD and MAFLD were 28.0% and 37.3% respectively from a nationwide health screening database that included 9,584,399 participants.47 In Japan, the NAFLD prevalence rate was 17.9% among all ages in 2016.4
In rural India, the prevalence of NAFLD was around 10% in community-based epidemiological data, while the prevalence rate in urban populations was higher (17–25%).48–50 This is similar to the prevalence rate published by the west. In some countries of Southeast Asia, such as Sri Lanka, Malaysia and Singapore, there were also dramatic variations in NAFLD prevalence between urban and rural regions (5–35%).5,51,52
Africa
There are limited data on the burden of NAFLD in Africa. Globally, the highest prevalence of NAFLD was reported from South America and the Middle East, whereas the lowest rate was reported from Africa.25 However, this is likely to be underestimated because of rising rates of obesity, T2D, human immunodeficiency virus (HIV) infection, and change in dietary habits in Africa. In Nigeria, the prevalence of NAFLD was reported to be 9.5–16.7% in individuals with diabetes and 1.2–4.5% in individuals without diabetes.53,54 The estimated prevalence of NAFLD in the non-diabetic Sudanese population is reportedly around 20%,55 and the prevalence of NAFLD among Sudanese individuals with T2D is 30%.56 NAFLD prevalence is also higher in obese individuals. One study in South Africa reported a prevalence of NAFLD of 47.6% among overweight and obese adults.57 The African region has the highest burden of HIV infection worldwide and accounts for over two-thirds of the global total of new HIV infections.58 However, there are limited data for NAFLD among HIV-infected patients in Africa. One is a retrospective South African study which reported a prevalence of 28% on liver biopsy, and the other is a prospective cross-sectional study with a prevalence of 13.3% by ultrasound from Nigeria.59,60
Summary
The prevalence of MAFLD/NAFLD is well above 20% in most parts of the world and is increasing over time. The Middle East has the highest prevalence, whereas the rise is particularly steep in Asia. Although the prevalence of MAFLD/NAFLD appears lower in Africa, there have been few large epidemiological studies in this region, and data need to be updated.
Incidence of MAFLD/NAFLD
Studies on the incidence of MAFLD are uncommon and are largely based on serial ultrasound scans with limited control on the agreement among different operators (Table 2). Thus, the interpretation might be affected by intraobserver and interobserver variability, not to mention the limited reliability of ultrasound scan to detect mild steatosis and quantify the degree of steatosis.61 Besides, studies using registries or health examination cohorts suffer from selection bias, as patients who had serial examinations are likely different from those who did not. To our knowledge, only one study from Hong Kong used proton-magnetic resonance spectroscopy, an objective measurement of hepatic steatosis, to determine the incidence of NAFLD in the general population.62 Because people without fatty liver at baseline are less likely to have metabolic diseases during follow-up, they may not fulfill the metabolic criteria of MAFLD even when they begin to develop fatty liver. Thus, the incidence of MAFLD can be substantially lower than the incidence of NAFLD in the same population.21
North and South Americas
There are no incidence data of MAFLD in North and South Americas for the general population. In the meta-analysis of Younossi et al.,25 the incidence data of NAFLD were only available in Asia. Kanwal et al.63 analyzed the national Veterans Administration databases from 2003 to 2011 for the age-adjusted incidence of NAFLD. The annual incidence rates of NAFLD remained stable (from 2.2% to 3.2%) during the study duration. Compared with older patients, the incidence of patients younger than 45 years-old had a greater increase. The incidence of NAFLD will likely continue to increase because of a steady overall incidence coupled with a rising incidence in younger individuals.
Europe
There are no incidence data of MAFLD in Europe for the general population. Only few studies have explored the incidence of NAFLD. A study from Italy used the general population of the Dionysos Study which included 144 subjects without fatty liver to study the incidence and natural course of NAFLD.64 After a median follow-up of 8.5 years, the incidence of fatty liver was 18.5 per 1,000 person-years. NAFLD is emerging as the leading chronic liver disease in Europe. A study conducted in Northeast England found that NAFLD-related HCC accounted for 35% of all HCC cases in 2010, an increase of more than 10-fold in 10 years.65
Asia-Pacific region
Few studies have evaluated the incidence of NAFLD in Asia. A recent systematic review and meta-analysis of 18 studies showed that the pooled annual NAFLD incidence rate was 50.9 cases per 1,000 person-years (95% CI: 44·8–57·4) in Asia.41 The incidence of NAFLD was the highest in mainland China (63.0 per 1,000 person-years [47.0–81.3]) and lowest in Japan (29.0 per 1,000 person-years [26.3–31.7]). In a population study of Hong Kong, the incidence of MAFLD was 2.8 per 100 person-years at a median interval of 47 months (range: 34–60 months).21 A prospective observational study from Japan which followed 4,401 healthy Japanese found a 10% annual incidence rate.66 Another Japanese study evaluated elevated aminotransferase levels, weight gain and insulin resistance development over 5 years, and reported that the incidence of NAFLD was 31 per 1,000 person-years.67 Among patients with T2D in Hong Kong, 52% had incident MAFLD as determined by controlled attenuation parameter using transient elastography in a 3-year period.68 However, current data on incidence for NAFLD are still limited in Asia, due to the limited number of studies. Further studies seem warranted to determine the true incidence in general population.
Africa
We did not identify any incidence study from Africa. Nonetheless, data on ethnic differences may shed light on this issue. Studies from the USA have demonstrated distinct disparities in the prevalence of NAFLD by race and ethnicity. Compared to Hispanics or Whites, African Americans have a lower prevalence of elevated aminotransferase levels and NAFLD.69 Genetic and metabolic factors are suggested as underlying causes for these differences.70 In particular, the PNPLA3 gene polymorphism is uncommon among Africans. Although African-Americans have a higher rate of obesity and insulin resistance compared to Caucasians and Hispanics, they have lower serum concentrations of triglycerides.71 The prevalence of steatosis as assessed by magnetic resonance spectroscopy was highest in Hispanics (45%), followed by Whites (33%) and African Americans (24%), in over 2,000 participants in the Dallas Heart Study.69 Another study by Kallwitz et al.72 consisted of 238 patients who had a routine liver biopsy at the time of obesity surgery, and reported that African Americans had significantly lower rates of steatosis, NASH, and fibrosis score than non-Hispanic Whites and Hispanics. However, African-Americans have one of the highest overall incidence rates of HCC and HCC mortality, which may be explained by contributing factors, including hepatitis C virus infection, alcohol abuse, or obesity.73
Summary
Incidence data on MAFLD/NAFLD are scarce, mainly because of the difficulty to determine new-onset fatty liver reliably using inexpensive noninvasive tests, such as abdominal ultrasonography and serum formulae. Nonetheless, based on the current literature, a reasonable estimate of the annual incidence of NAFLD is somewhere between 2–6%. Similar to the prevalence data, the incidence of MAFLD/NAFLD is strongly associated with older age and metabolic risk factors.
Clinical outcomes
MAFLD is strongly associated with metabolic diseases and their complications. On the whole, CVD remains the leading cause of death in MAFLD patients. Nonetheless, MAFLD is also associated with increased risk of extrahepatic malignancies. Liver-related death is also important in patients with advanced liver disease.7 Recent data suggest that MAFLD but not NAFLD is associated with increased overall and cardiovascular mortality, again highlighting the importance of metabolic dysfunction in the natural history of the disease.47,74 For example, in the NHANES III 1988–1994 cohort, subjects with MAFLD had a 17% increase in overall mortality at a median follow-up of 23 years.74 Likewise, subjects who had MAFLD but not NAFLD in the same cohort were more likely to have increased fibrosis-4 index, suggestive of significant liver fibrosis, than those who had NAFLD but not MAFLD.75 In this section, we discuss the various clinical outcomes in patients with MAFLD.
Cardiovascular events
CVD is the leading cause of death in NAFLD patients, accounting for 40–45% of the total deaths in NAFLD.14,76,77 In a Korean nationwide cohort study involving more than 9 million patients, Lee et al.47 reported that MAFLD was associated with a higher risk of cardiovascular events compared to NAFLD. Composite cardiovascular events, defined as myocardial infarction, stroke and heart failure, were analyzed in different definitions of fatty liver disease (MAFLD and NAFLD). The cumulative incidence of cardiovascular events was higher in patients with MAFLD or NAFLD than those without. Importantly, patients with MAFLD had higher cardiovascular risk than those with NAFLD but not MAFLD. These results support the notion that the new MAFLD definition identifies higher risk patients.47 In addition, in a cross-sectional study of more than 1,000 Brazilians undergoing liver biopsies, Guerreiro et al.78 found that MAFLD patients with concomitant hepatitis C virus and hepatitis B virus infection had a higher cardiovascular risk than those without viral infection.
The pathophysiological mechanisms of MAFLD and CVD include systemic insulin resistance, systemic inflammation, endothelial dysfunction, altered lipid metabolism and oxidative stress.79 Multiple mechanisms contribute to the occurrence and progression of MAFLD. Currently, therapy concerning these mechanisms is under development. Primary prevention of MAFLD is lifestyle modification, including weight loss through healthy diet and physical activity, which is also the primary prevention of CVD indicated by the American College of Cardiology/American Heart Association (ACC/AHA).80 Hypocaloric diet and moderate exercise can effectively benefit both MAFLD and CVD.14,80
For secondary prevention, although statins do not improve the histological features of MAFLD, they are key to preventing cardiovascular events.81 Unfortunately, because of an unfounded fear for drug-induced liver injury and inadequate assessment of cardiovascular risk, statins are underused in MAFLD patients.82 Athyros et al.81 conducted a post-hoc analysis of the GREek Atorvastatin and Coronary heart disease Evaluation (GREACE) cohort of 1,600 patients with coronary heart disease. Among 437 patients with abnormal liver tests at baseline, improvement in liver enzymes was observed in the atorvastatin group but not the control group after 3 years of follow-up. Cardiovascular events occurred 10% in treatment group (3.2 events per 100 patient-years) and 30% in control group (10.0 events per 100 patient-years), translating into a 68% relative risk reduction in cardiovascular events.83 Semaglutide is a glucagon-like peptide-1 receptor (GLP1) agonist for the treatment of T2D, which is also one of the CVD risk factors. A recent multinational placebo-controlled phase 2 trial showed that NASH resolution without worsening of fibrosis could be achieved in 59% of the patients receiving semaglutide at 0.4 mg daily for 72 weeks, compared with 17% in the placebo group. The drug also demonstrated good cardiovascular safety and tolerability.84 Another class of antidiabetic drug, the sodium-glucose cotransporter 2 inhibitors, also improves cardiovascular and renal outcomes.85 It may also reduce liver fat and improve liver histology.
In patients with severe obesity, bariatric surgery can significantly reduce liver steatosis, necroinflammation, and fibrosis as well as the risk of cardiovascular events.86 However, there has been no randomized controlled trial on the use of bariatric surgery in MAFLD. The indication of bariatric surgery in MAFLD patients needs to be defined.
Hepatic events
Hepatic events are defined as any occurrence of cirrhosis complications (ascites, upper gastrointestinal variceal hemorrhage, spontaneous bacterial peritonitis, hepatic encephalopathy, and hepatorenal syndrome), HCC, and liver-related mortality. In a retrospective cohort with 619 NAFLD patients, the annual incidence of hepatic events was 1.6%, 2.8%, 7.1%, 13.7%, and 23.5% in patients with F0, F1, F2, F3, and F4 fibrosis, respectively.87 In a multinational cohort study with 458 NAFLD patients, Vilar-Gomez et al.7 demonstrated that incidence of cirrhotic complications was 3.1% in patients with bridging fibrosis, 16.7% in cirrhosis with Child-Turcotte-Pugh (CTP) A5, 57.1% in cirrhosis with CTP A6. Among hepatic decompensations, ascites (70%) and variceal hemorrhage (24%) were the most common hepatic events.
Demographic factors of HCC include age, male sex, and race. In a retrospective study with 296,707 NAFLD patients, patients with age ≥65 years had a higher risk for HCC (incidence rate=0.41 per 1,000 person-years), compared to age <65 years (incidence rate=0.22 per 1,000 person-years). Male sex was significantly associated with HCC, with 11.05 annual incidence per 1,000 person-years compared to female sex, with 1.62 annual incidence per 1,000 person-years. Patients of Hispanic race had 23.76 annual incidence per 1,000 person-years compared to those of White race and African Americans, with 11.94.88
Metabolic factors, including T2D, obesity, dyslipidemia, and hypertension, are considered as risk factors of hepatic events in NAFLD patients.89 Among these, T2D is the most significant risk factor. In a cohort of 18 million people from four European centers, baseline T2D was highly associated with incident liver-related events in patients with NASH or NAFLD cohort after 3.3 years of follow-up (hazard ratio [HR]=2.3, 95% CI=1.9–2.78).90 In addition, in a prospective study of 0.5 million people in China, individuals with diabetes had significantly higher risk of cirrhosis and HCC after 10 years of follow-up (HR=1.49, 95% CI=1.30–1.70). Plasma glucose had a positive association with HCC (each 1 mmol/L higher at baseline associated with an adjusted HR of 1.04, 95% CI=1.03–1.06) and cirrhosis (with an adjusted HR of 1.07, 95% CI=1.05–1.09).91 A meta-analysis including 12 studies with 22.8 million patients and a median follow-up of 10 years showed that T2D increased the risk of incident severe liver disease by more than 2-fold (random effect HR=2.25, 95% CI=1.83–2.76). In 14 studies with 49,000 patients with a median of 13.8 years follow-up, obesity was associated with the increased risk of incident liver-related events (random effect HR=1.20, 95% CI=1.12–1.28).89 In a retrospective study of 271,000 NAFLD patients, Kanwal et al.92 showed that metabolic traits including diabetes (HR=1.31, 95% CI=1.27–1.35), obesity (HR=1.10, 95% CI=1.07–1.13), hypertension (HR=1.59, 95% CI=1.50–1.68) and hyperlipidemia (HR=1.24, 95% CI=1.19–1.28) were independently associated with the risk of cirrhosis or HCC. Besides, compared with patients with one or no metabolic traits, risk of cirrhosis or HCC increased to 1.33 (95% CI=1.26–1.40), 1.61 (95% CI=1.53–1.69) and 2.03 (95% CI=1.93–2.13) for having 2, 3 and 4 metabolic traits.
For NAFLD patients, genetic factors play an important role in incidence of hepatic events. In the UK Biobank database, three genetic variants (PNPLA3, TM6SF2, MBOAT7) were found to be associated with hepatic events. The PNPLA3 rs738409 GG genotype had an adjusted HR of 2.85 (95% CI=1.85–4.39) for liver cancer, 3.13 (95% CI=2.29–4.27) for cirrhosis, and 2.13 (95%CI=1.85–2.46) for other hepatic events. Likewise, the TM6SF2 rs58542926 CC/TT genotypes had an adjusted HR of 2.12 (95% CI=1.57–2.86) for HCC in NAFLD patients.33
The definition of MAFLD can include patients with viral hepatitis and excessive alcohol consumption, which are considered as significant risk factors in HCC or cirrhosis. Chronic HBV infection is the leading cause of HCC in Eastern Asia, with lifetime risk of 10–25% for HBV patients progressing to HCC.93,94 Although MAFLD appears to be less common in HBV-infected individuals than uninfected controls,95 the presence of metabolic risk factors and hepatic steatosis increases the risk of cirrhosis and HCC in patients with chronic hepatitis B.96,97 Patients with chronic hepatitis B and MAFLD have higher serum alanine aminotransferase and liver stiffness than those without MAFLD.98 On the flip side, even prior or occult HBV infection, as suggested by positive anti-hepatitis B core antibody, increases the risk of cirrhosis and HCC in patients with MAFLD.99 A meta-analysis providing data from 2,629,272 patients showed that long-term alcohol consumption was associated with increasing risk for liver cirrhosis, with a relative risk of 10.70 (95% CI=2.95–38.78) for consumption of seven drinks or more per day and women had a higher risk compared to men (Table 3).85
Table 3. Risk factors of hepatocellular carcinoma and cirrhosis in MAFLD patients.
| Risk factors |
|---|
| Demographic factors |
| Older age |
| Male sex |
| Hispanic race |
| Family history of cirrhosis |
| Alcohol consumption |
| Metabolic factors |
| T2D |
| Obesity |
| Hypertension |
| Dyslipidemia |
| Genetic factors |
| PNPLA3 rs738409 |
| TM6SF2 rs58542926 |
| MBOAT7 rs641738 |
| HSD17B13 rs6834314 (protective) |
| Chronic infections |
| Chronic hepatitis B |
| Chronic hepatitis C |
| HIV |
MAFLD, metabolic (dysfunction)-associated fatty liver disease; HIV, human immunodeficiency virus; T2D, type 2 diabetes.
Extrahepatic malignancies
Owing to the increasing global prevalence of MAFLD, the association between MAFLD and risk of some extrahepatic cancers (especially colorectal cancer) has gained considerable interest.100 Recent cohort studies and meta-analyses showed that NAFLD is associated with an increased prevalence and incidence of colorectal cancer and adenomas.101,102 A systematic review and meta-analysis of 26 studies showed that the pooled odds ratio (OR) values of the risk of colorectal cancer and adenomas in patients with NAFLD were 1.72 (95% CI: 1.40–2.11) and 1.37 (95% CI: 1.29–1.46), respectively.103 Wong et al.104 found that NAFLD patients had a higher prevalence of colorectal adenomas (34.7% vs. 21.5%, p=0.043) and advanced neoplasms (18.6% vs. 5.5%, p=0.002) than healthy controls.102 A large cross-sectional study of 26,540 asymptomatic individuals from South Korea also showed that the risk for any colorectal neoplasia and advanced colorectal neoplasia increased in patients with NAFLD.
Apart from colorectal cancer and adenomas, NAFLD was reported to be associated with other cancers. A longitudinal cohort study in a US population reported that NAFLD was associated with higher risk of uterine, gastric and pancreatic cancers.105 A retrospective study also found that NAFLD (FLI ≥60) was significantly associated with the development of esophageal cancer (HR=2.10, 95% CI: 1.88–2.35).106 Another large prospective cohort study from China showed that NAFLD was associated with increased risk of thyroid cancer (HR=2.79, 95% CI: 1.25–6.21, p=0.01) and lung cancer (HR=1.23, 95% CI: 1.02–1.49, p=0.03).101 Breast cancer is now the most common cancer in women and is the leading cause of cancer deaths among women. A cohort study included subjects who were followed up for >1 year after having a heath checkup at a tertiary hospital in Korea and showed that NAFLD was associated with the development of breast cancer in females.107 Growing data support that prostate cancer is a metabolic syndrome-related cancer and the second most commonly diagnosed cancer among men worldwide.108 A nationwide study with 10,516,985 Korean men indicated that NAFLD based on FLI and hepatic steatosis index was independently associated with the development of prostate cancer, particularly in the elderly.109 Cholangiocarcinoma, including intra- and extrahepatic cholangiocarcinoma, is a rare but highly lethal cancer. Several studies showed that the risk of developing cholangiocarcinoma was significantly higher in patients with NAFLD than in patients without NAFLD.110–112 A meta-analysis also reported that NAFLD was associated with a nearly 30% increased risk of urinary system cancers.113
Renal outcomes
End-stage renal disease causes significant morbidity and mortality in patients with metabolic syndrome. In particular, diabetic nephropathy is currently the leading cause of end-stage renal disease worldwide. Among patients with T2D, Asians are more likely to develop end-stage renal disease, while Caucasians are more likely to develop coronary artery disease.114 Because of shared risk factors, patients with MAFLD/NAFLD have increased risk of chronic kidney disease.115–117 Like other complications, it appears that the severity of fatty liver disease does matter. In a study using transient elastography to examine 1,763 Chinese patients with T2D, increased liver stiffness (a surrogate for fibrosis) but not controlled attenuation parameter (a surrogate for steatosis) was independently associated with albuminuria.118
Summary
CVD remains the leading cause of death in patients with MAFLD/NAFLD. In patients with advanced liver fibrosis or cirrhosis, however, liver-related complications are much more common and account for the majority of deaths. Recent data suggest that the MAFLD definition identifies patients at risk of complications better than the original NAFLD definition, likely because of the presence of metabolic risk factors. Although the association between MAFLD/NAFLD and CVD as well as some extrahepatic cancers is well established, it remains unclear if it represents a causal relationship. The bottom line is that clinicians should be aware of the association and be vigilant of the development of new comorbidities and complications.
Management implications
Detailed discussion on the management of MAFLD is outside the scope of this article and has been covered by various management guidelines and reviews.1,119 The rising incidence of MAFLD around the world and the strong association with metabolic disorders highlight the importance of healthy lifestyle as a prevention and treatment of MAFLD.120 Based on data from numerous clinical trials, guidelines have endorsed vitamin E and pioglitazone as potential treatments for selected patients with steatohepatitis. A number of metabolic drugs, such as obeticholic acid, semaglutide, aramchol and resmetirom, have entered phase 3 development and may transform the management of NASH.121 In particular, some metabolic drugs, such as GLP1 receptor agonists and sodium-glucose co-transporter-2 inhibitors, have been shown to improve not only glycemia but also body weight and cardiovascular outcomes.85,122 Hopefully, an upstream treatment will be able to mitigate different metabolic disorders, including MAFLD, at the same time.
Conclusions
There is no doubt that MAFLD/NAFLD is increasingly important worldwide. It remains highly prevalent in the West, while its prevalence in the East is catching up and has reached over 30% in some Asia-Pacific regions. The incidence of MAFLD/NAFLD is hard to study because of the lack of systematic screening programs and accurate tools. The most commonly used screening tools, like ultrasonography, are not sensitive enough and may miss some subtle changes in liver fat content.
MAFLD/NAFLD is not just common but potentially life-threatening in a significant proportion of patients. MAFLD/NAFLD kills not just by hepatic events but more often through cardiovascular events and non-liver malignancies. This is even more challenge in the low- and middle-income countries, as MAFLD/NAFLD is not yet a priority in their public healthcare systems. An integrated approach involving social, behavioral and medical efforts are the keys to decelerate the rising prevalence and incidence, and hence the adverse clinical outcomes of MAFLD/NAFLD, around the world.
Abbreviations
- CI
confidence interval
- CTP
Child-Turcotte-Pugh
- CVD
cardiovascular disease
- FLI
fatty liver index
- GLP1
glucagon-like peptide-1
- HCC
hepatocellular carcinoma
- HR
hazard ratio
- ICD
International Classification of Diseases
- MAFLD
metabolic (dysfunction)-associated fatty liver disease
- NAFLD
nonalcoholic fatty liver disease
- NASH
nonalcoholic steatohepatitis
- NHANES
National Health and Nutritional Examination Survey
- T2D
type 2 diabetes
References
- 1.Powell EE, Wong VW, Rinella M. Non-alcoholic fatty liver disease. Lancet. 2021;397(10290):2212–2224. doi: 10.1016/S0140-6736(20)32511-3. [DOI] [PubMed] [Google Scholar]
- 2.Younossi Z, Stepanova M, Ong JP, Jacobson IM, Bugianesi E, Duseja A, et al. Nonalcoholic steatohepatitis is the fastest growing cause of hepatocellular carcinoma in liver transplant candidates. Clin Gastroenterol Hepatol. 2019;17(4):748–755. doi: 10.1016/j.cgh.2018.05.057. e743. [DOI] [PubMed] [Google Scholar]
- 3.Tateishi R, Uchino K, Fujiwara N, Takehara T, Okanoue T, Seike M, et al. A nationwide survey on non-B, non-C hepatocellular carcinoma in Japan: 2011-2015 update. J Gastroenterol. 2019;54(4):367–376. doi: 10.1007/s00535-018-1532-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Estes C, Anstee QM, Arias-Loste MT, Bantel H, Bellentani S, Caballeria J, et al. Modeling NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016-2030. J Hepatol. 2018;69(4):896–904. doi: 10.1016/j.jhep.2018.05.036. [DOI] [PubMed] [Google Scholar]
- 5.Estes C, Chan HLY, Chien RN, Chuang WL, Fung J, Goh GB, et al. Modelling NAFLD disease burden in four Asian regions-2019-2030. Aliment Pharmacol Ther. 2020;51(8):801–811. doi: 10.1111/apt.15673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wong VW, Wong GL, Yeung JC, Fung CY, Chan JK, Chang ZH, et al. Long-term clinical outcomes after fatty liver screening in patients undergoing coronary angiogram: a prospective cohort study. Hepatology. 2016;63(3):754–763. doi: 10.1002/hep.28253. [DOI] [PubMed] [Google Scholar]
- 7.Vilar-Gomez E, Calzadilla-Bertot L, Wai-Sun Wong V, Castellanos M, Aller-de la Fuente R, Metwally M, et al. Fibrosis severity as a determinant of cause-specific mortality in patients with advanced nonalcoholic fatty liver disease: a multi-national cohort study. Gastroenterology. 2018;155(2):443–457.e417. doi: 10.1053/j.gastro.2018.04.034. [DOI] [PubMed] [Google Scholar]
- 8.Eslam M, Newsome PN, Sarin SK, Anstee QM, Targher G, Romero-Gomez M, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol. 2020;73(1):202–209. doi: 10.1016/j.jhep.2020.03.039. [DOI] [PubMed] [Google Scholar]
- 9.Wai-Sun Wong V, Kanwal F. On the proposed definition of metabolic-associated fatty liver disease. Clin Gastroenterol Hepatol. 2021;19(5):865–870. doi: 10.1016/j.cgh.2021.01.017. [DOI] [PubMed] [Google Scholar]
- 10.Shiha G, Korenjak M, Eskridge W, Casanovas T, Velez-Moller P, Hogstrom S, et al. Redefining fatty liver disease: an international patient perspective. Lancet Gastroenterol Hepatol. 2021;6(1):73–79. doi: 10.1016/S2468-1253(20)30294-6. [DOI] [PubMed] [Google Scholar]
- 11.Mendez-Sanchez N, Arrese M, Gadano A, Oliveira CP, Fassio E, Arab JP, et al. The Latin American Association for the Study of the Liver (ALEH) position statement on the redefinition of fatty liver disease. Lancet Gastroenterol Hepatol. 2021;6(1):65–72. doi: 10.1016/S2468-1253(20)30340-X. [DOI] [PubMed] [Google Scholar]
- 12.Shiha G, Alswat K, Al Khatry M, Sharara AI, Ormeci N, Waked I, et al. Nomenclature and definition of metabolic-associated fatty liver disease: a consensus from the Middle East and north Africa. Lancet Gastroenterol Hepatol. 2021;6(1):57–64. doi: 10.1016/S2468-1253(20)30213-2. [DOI] [PubMed] [Google Scholar]
- 13.Spearman CW, Desalegn H, Ocama P, Awuku YA, Ojo O, Elsahhar M, et al. The sub-Saharan Africa position statement on the redefinition of fatty liver disease: from NAFLD to MAFLD. J Hepatol. 2021;74(5):1256–1258. doi: 10.1016/j.jhep.2021.01.015. [DOI] [PubMed] [Google Scholar]
- 14.Eslam M, Sarin SK, Wong VW, Fan JG, Kawaguchi T, Ahn SH, et al. The Asian Pacific Association for the Study of the Liver clinical practice guidelines for the diagnosis and management of metabolic associated fatty liver disease. Hepatol Int. 2020;14(6):889–919. doi: 10.1007/s12072-020-10094-2. [DOI] [PubMed] [Google Scholar]
- 15.Ratziu V, Rinella M, Beuers U, Loomba R, Anstee QM, Harrison S, et al. The times they are a-changin’ (for NAFLD as well) J Hepatol. 2020;73(6):1307–1309. doi: 10.1016/j.jhep.2020.08.028. [DOI] [PubMed] [Google Scholar]
- 16.Younossi ZM, Rinella ME, Sanyal AJ, Harrison SA, Brunt EM, Goodman Z, et al. From NAFLD to MAFLD: implications of a premature change in terminology. Hepatology. 2021;73(3):1194–1198. doi: 10.1002/hep.31420. [DOI] [PubMed] [Google Scholar]
- 17.Fouad Y, Elwakil R, Elsahhar M, Said E, Bazeed S, Ali Gomaa A, et al. The NAFLD-MAFLD debate: eminence vs evidence. Liver Int. 2021;41(2):255–260. doi: 10.1111/liv.14739. [DOI] [PubMed] [Google Scholar]
- 18.Fouad Y, Gomaa A, Semida N, Ghany WA, Attia D. Change from NAFLD to MAFLD increases the awareness of fatty liver disease in primary care physicians and specialists. J Hepatol. 2021;74(5):1254–1256. doi: 10.1016/j.jhep.2020.12.035. [DOI] [PubMed] [Google Scholar]
- 19.Alem SA, Gaber Y, Abdalla M, Said E, Fouad Y. Capturing patient experience: a qualitative study of change from NAFLD to MAFLD real-time feedback. J Hepatol. 2021;74(5):1261–1262. doi: 10.1016/j.jhep.2021.01.022. [DOI] [PubMed] [Google Scholar]
- 20.Mendez-Sanchez N, Diaz-Orozco L, Cordova-Gallardo J. Redefinition of fatty liver disease from NAFLD to MAFLD raised disease awareness: Mexican experience. J Hepatol. 2021;75(1):221–222. doi: 10.1016/j.jhep.2021.04.021. [DOI] [PubMed] [Google Scholar]
- 21.Wong VW, Wong GL, Woo J, Abrigo JM, Chan CK, Shu SS, et al. Impact of the new definition of metabolic associated fatty liver disease on the epidemiology of the disease. Clin Gastroenterol Hepatol. 2020 doi: 10.1016/j.cgh.2020.10.046. [DOI] [PubMed] [Google Scholar]
- 22.Lin S, Huang J, Wang M, Kumar R, Liu Y, Liu S, et al. Comparison of MAFLD and NAFLD diagnostic criteria in real world. Liver Int. 2020;40(9):2082–2089. doi: 10.1111/liv.14548. [DOI] [PubMed] [Google Scholar]
- 23.Wong RJ, Cheung R. Trends in the prevalence of metabolic dysfunction-associated fatty liver disease in the United States, 2011-2018. Clin Gastroenterol Hepatol. 2021 doi: 10.1016/j.cgh.2021.01.030. [DOI] [PubMed] [Google Scholar]
- 24.Ciardullo S, Perseghin G. Prevalence of NAFLD, MAFLD and associated advanced fibrosis in the contemporary United States population. Liver Int. 2021;41(6):1290–1293. doi: 10.1111/liv.14828. [DOI] [PubMed] [Google Scholar]
- 25.Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84. doi: 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 26.Lizardi-Cervera J, Laparra DI, Chávez-Tapia NC, Ostos ME, Esquivel MU. Prevalence of NAFLD and metabolic syndrome in asymtomatics subjects. Rev Gastroenterol Mex. 2006;71(4):453–459. [PubMed] [Google Scholar]
- 27.Younossi Z, Anstee QM, Marietti M, Hardy T, Henry L, Eslam M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15(1):11–20. doi: 10.1038/nrgastro.2017.109. [DOI] [PubMed] [Google Scholar]
- 28.Fleischman MW, Budoff M, Zeb I, Li D, Foster T. NAFLD prevalence differs among hispanic subgroups: the Multi-Ethnic Study of Atherosclerosis. World J Gastroenterol. 2014;20(17):4987–4993. doi: 10.3748/wjg.v20.i17.4987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.González-Muniesa P, Mártinez-González MA, Hu FB, Després JP, Matsuzawa Y, Loos RJF, et al. Obesity. Nat Rev Dis Primers. 2017;3:17034. doi: 10.1038/nrdp.2017.34. [DOI] [PubMed] [Google Scholar]
- 30.Karnikowski M, Córdova C, Oliveira RJ, Karnikowski MG, Nóbrega Ode T. Non-alcoholic fatty liver disease and metabolic syndrome in Brazilian middle-aged and older adults. Sao Paulo Med J. 2007;125(6):333–337. doi: 10.1590/s1516-31802007000600006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.López-Velázquez JA, Silva-Vidal KV, Ponciano-Rodríguez G, Chávez-Tapia NC, Arrese M, Uribe M, et al. The prevalence of nonalcoholic fatty liver disease in the Americas. Ann Hepatol. 2014;13(2):166–178. [PubMed] [Google Scholar]
- 32.Riquelme A, Arrese M, Soza A, Morales A, Baudrand R, Pérez-Ayuso RM, et al. Non-alcoholic fatty liver disease and its association with obesity, insulin resistance and increased serum levels of C-reactive protein in Hispanics. Liver Int. 2009;29(1):82–88. doi: 10.1111/j.1478-3231.2008.01823.x. [DOI] [PubMed] [Google Scholar]
- 33.Liu Z, Suo C, Shi O, Lin C, Zhao R, Yuan H, et al. The health impact of MAFLD, a novel disease cluster of NAFLD, is amplified by the integrated effect of fatty liver disease-related genetic variants. Clin Gastroenterol Hepatol. 2020 doi: 10.1016/j.cgh.2020.12.033. [DOI] [PubMed] [Google Scholar]
- 34.Caballería L, Pera G, Auladell MA, Torán P, Muñoz L, Miranda D, et al. Prevalence and factors associated with the presence of nonalcoholic fatty liver disease in an adult population in Spain. Eur J Gastroenterol Hepatol. 2010;22(1):24–32. doi: 10.1097/MEG.0b013e32832fcdf0. [DOI] [PubMed] [Google Scholar]
- 35.Bedogni G, Miglioli L, Masutti F, Tiribelli C, Marchesini G, Bellentani S. Prevalence of and risk factors for nonalcoholic fatty liver disease: the Dionysos nutrition and liver study. Hepatology. 2005;42(1):44–52. doi: 10.1002/hep.20734. [DOI] [PubMed] [Google Scholar]
- 36.Armstrong MJ, Houlihan DD, Bentham L, Shaw JC, Cramb R, Olliff S, et al. Presence and severity of non-alcoholic fatty liver disease in a large prospective primary care cohort. J Hepatol. 2012;56(1):234–240. doi: 10.1016/j.jhep.2011.03.020. [DOI] [PubMed] [Google Scholar]
- 37.de Lédinghen V, Ratziu V, Causse X, Le Bail B, Capron D, Renou C, et al. Diagnostic and predictive factors of significant liver fibrosis and minimal lesions in patients with persistent unexplained elevated transaminases. A prospective multicenter study. J Hepatol. 2006;45(4):592–599. doi: 10.1016/j.jhep.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 38.Haring R, Wallaschofski H, Nauck M, Dörr M, Baumeister SE, Völzke H. Ultrasonographic hepatic steatosis increases prediction of mortality risk from elevated serum gamma-glutamyl transpeptidase levels. Hepatology. 2009;50(5):1403–1411. doi: 10.1002/hep.23135. [DOI] [PubMed] [Google Scholar]
- 39.Radu C, Grigorescu M, Crisan D, Lupsor M, Constantin D, Dina L. Prevalence and associated risk factors of non-alcoholic fatty liver disease in hospitalized patients. J Gastrointestin Liver Dis. 2008;17(3):255–260. [PubMed] [Google Scholar]
- 40.Tarnoki AD, Tarnoki DL, Bata P, Littvay L, Osztovits J, Jermendy G, et al. Heritability of non-alcoholic fatty liver disease and association with abnormal vascular parameters: a twin study. Liver Int. 2012;32(8):1287–1293. doi: 10.1111/j.1478-3231.2012.02823.x. [DOI] [PubMed] [Google Scholar]
- 41.Li J, Zou B, Yeo YH, Feng Y, Xie X, Lee DH, et al. Prevalence, incidence, and outcome of non-alcoholic fatty liver disease in Asia, 1999-2019: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2019;4(5):389–398. doi: 10.1016/S2468-1253(19)30039-1. [DOI] [PubMed] [Google Scholar]
- 42.Li H, Guo M, An Z, Meng J, Jiang J, Song J, et al. Prevalence and risk factors of metabolic associated fatty liver disease in Xinxiang, China. Int J Environ Res Public Health. 2020;17(6):1818. doi: 10.3390/ijerph17061818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Li H, Wang YJ, Tan K, Zeng L, Liu L, Liu FJ, et al. Prevalence and risk factors of fatty liver disease in Chengdu, Southwest China. Hepatobiliary Pancreat Dis Int. 2009;8(4):377–382. [PubMed] [Google Scholar]
- 44.Fan JG, Zhu J, Li XJ, Chen L, Li L, Dai F, et al. Prevalence of and risk factors for fatty liver in a general population of Shanghai, China. J Hepatol. 2005;43(3):508–514. doi: 10.1016/j.jhep.2005.02.042. [DOI] [PubMed] [Google Scholar]
- 45.Zhou YJ, Li YY, Nie YQ, Ma JX, Lu LG, Shi SL, et al. Prevalence of fatty liver disease and its risk factors in the population of South China. World J Gastroenterol. 2007;13(47):6419–6424. doi: 10.3748/wjg.v13.i47.6419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chen CH, Huang MH, Yang JC, Nien CK, Yang CC, Yeh YH, et al. Prevalence and risk factors of nonalcoholic fatty liver disease in an adult population of taiwan: metabolic significance of nonalcoholic fatty liver disease in nonobese adults. J Clin Gastroenterol. 2006;40(8):745–752. doi: 10.1097/00004836-200609000-00016. [DOI] [PubMed] [Google Scholar]
- 47.Lee H, Lee YH, Kim SU, Kim HC. Metabolic dysfunction-associated fatty liver disease and incident cardiovascular disease risk: a nationwide cohort study. Clin Gastroenterol Hepatol. 2020 doi: 10.1016/j.cgh.2020.12.022. [DOI] [PubMed] [Google Scholar]
- 48.Amarapurkar D, Kamani P, Patel N, Gupte P, Kumar P, Agal S, et al. Prevalence of non-alcoholic fatty liver disease: population based study. Ann Hepatol. 2007;6(3):161–163. [PubMed] [Google Scholar]
- 49.Das K, Das K, Mukherjee PS, Ghosh A, Ghosh S, Mridha AR, et al. Nonobese population in a developing country has a high prevalence of nonalcoholic fatty liver and significant liver disease. Hepatology. 2010;51(5):1593–1602. doi: 10.1002/hep.23567. [DOI] [PubMed] [Google Scholar]
- 50.Singh SP, Nayak S, Swain M, Rout N, Mallik RN, Agrawal O, et al. Prevalence of nonalcoholic fatty liver disease in coastal eastern India: a preliminary ultrasonographic survey. Trop Gastroenterol. 2004;25(2):76–79. [PubMed] [Google Scholar]
- 51.Dassanayake AS, Kasturiratne A, Rajindrajith S, Kalubowila U, Chakrawarthi S, De Silva AP, et al. Prevalence and risk factors for non-alcoholic fatty liver disease among adults in an urban Sri Lankan population. J Gastroenterol Hepatol. 2009;24(7):1284–1288. doi: 10.1111/j.1440-1746.2009.05831.x. [DOI] [PubMed] [Google Scholar]
- 52.Goh SC, Ho EL, Goh KL. Prevalence and risk factors of non-alcoholic fatty liver disease in a multiracial suburban Asian population in Malaysia. Hepatol Int. 2013;7(2):548–554. doi: 10.1007/s12072-012-9359-2. [DOI] [PubMed] [Google Scholar]
- 53.Olusanya TO, Lesi OA, Adeyomoye AA, Fasanmade OA. Non alcoholic fatty liver disease in a Nigerian population with type II diabetes mellitus. Pan Afr Med J. 2016;24:20. doi: 10.11604/pamj.2016.24.20.8181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Onyekwere CA, Ogbera AO, Balogun BO. Non-alcoholic fatty liver disease and the metabolic syndrome in an urban hospital serving an African community. Ann Hepatol. 2011;10(2):119–124. [PubMed] [Google Scholar]
- 55.Almobarak AO, Barakat S, Khalifa MH, Elhoweris MH, Elhassan TM, Ahmed MH. Non alcoholic fatty liver disease (NAFLD) in a Sudanese population: what is the prevalence and risk factors? Arab J Gastroenterol. 2014;15(1):12–15. doi: 10.1016/j.ajg.2014.01.008. [DOI] [PubMed] [Google Scholar]
- 56.Almobarak AO, Barakat S, Suliman EA, Elmadhoun WM, Mohamed NA, Abobaker IO, et al. Prevalence of and predictive factors for nonalcoholic fatty liver disease in Sudanese individuals with type 2 diabetes: Is metabolic syndrome the culprit? Arab J Gastroenterol. 2015;16(2):54–58. doi: 10.1016/j.ajg.2015.06.001. [DOI] [PubMed] [Google Scholar]
- 57.Kruger FC, Daniels C, Kidd M, Swart G, Brundyn K, Van Rensburg C, et al. Non-alcoholic fatty liver disease (NAFLD) in the Western Cape: a descriptive analysis. S Afr Med J. 2010;100(3):168–171. doi: 10.7196/samj.1422. [DOI] [PubMed] [Google Scholar]
- 58.Pustil R. Global AIDS. AIDS. 2003;17(Suppl 4):S3–11. [PubMed] [Google Scholar]
- 59.Hoffmann CJ, Hoffmann JD, Kensler C, van der Watt M, Omar T, Chaisson RE, et al. Tuberculosis and hepatic steatosis are prevalent liver pathology findings among HIV-infected patients in South Africa. PLoS One. 2015;10(2):e0117813. doi: 10.1371/journal.pone.0117813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lesi OA, Soyebi KS, Eboh CN. Fatty liver and hyperlipidemia in a cohort of HIV-positive Africans on highly active antiretroviral therapy. J Natl Med Assoc. 2009;101(2):151–155. doi: 10.1016/s0027-9684(15)30828-2. [DOI] [PubMed] [Google Scholar]
- 61.Wong VW, Adams LA, de Lédinghen V, Wong GL, Sookoian S. Noninvasive biomarkers in NAFLD and NASH - current progress and future promise. Nat Rev Gastroenterol Hepatol. 2018;15(8):461–478. doi: 10.1038/s41575-018-0014-9. [DOI] [PubMed] [Google Scholar]
- 62.Wong VW, Wong GL, Yeung DK, Lau TK, Chan CK, Chim AM, et al. Incidence of non-alcoholic fatty liver disease in Hong Kong: a population study with paired proton-magnetic resonance spectroscopy. J Hepatol. 2015;62(1):182–189. doi: 10.1016/j.jhep.2014.08.041. [DOI] [PubMed] [Google Scholar]
- 63.Kanwal F, Kramer JR, Duan Z, Yu X, White D, El-Serag HB. Trends in the burden of nonalcoholic fatty liver disease in a United States cohort of veterans. Clin Gastroenterol Hepatol. 2016;14(2):301–308.e301-302. doi: 10.1016/j.cgh.2015.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bedogni G, Miglioli L, Masutti F, Castiglione A, Crocè LS, Tiribelli C, et al. Incidence and natural course of fatty liver in the general population: the Dionysos study. Hepatology. 2007;46(5):1387–1391. doi: 10.1002/hep.21827. [DOI] [PubMed] [Google Scholar]
- 65.Dyson J, Jaques B, Chattopadyhay D, Lochan R, Graham J, Das D, et al. Hepatocellular cancer: the impact of obesity, type 2 diabetes and a multidisciplinary team. J Hepatol. 2014;60(1):110–117. doi: 10.1016/j.jhep.2013.08.011. [DOI] [PubMed] [Google Scholar]
- 66.Hamaguchi M, Kojima T, Takeda N, Nakagawa T, Taniguchi H, Fujii K, et al. The metabolic syndrome as a predictor of nonalcoholic fatty liver disease. Ann Intern Med. 2005;143(10):722–728. doi: 10.7326/0003-4819-143-10-200511150-00009. [DOI] [PubMed] [Google Scholar]
- 67.Suzuki A, Angulo P, Lymp J, St Sauver J, Muto A, Okada T, et al. Chronological development of elevated aminotransferases in a nonalcoholic population. Hepatology. 2005;41(1):64–71. doi: 10.1002/hep.20543. [DOI] [PubMed] [Google Scholar]
- 68.Lee HW, Wong GL, Kwok R, Choi KC, Chan CK, Shu SS, et al. Serial transient elastography examinations to monitor patients with type 2 diabetes: a prospective cohort study. Hepatology. 2020;72(4):1230–1241. doi: 10.1002/hep.31142. [DOI] [PubMed] [Google Scholar]
- 69.Browning JD, Szczepaniak LS, Dobbins R, Nuremberg P, Horton JD, Cohen JC, et al. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology. 2004;40(6):1387–1395. doi: 10.1002/hep.20466. [DOI] [PubMed] [Google Scholar]
- 70.Romeo S, Kozlitina J, Xing C, Pertsemlidis A, Cox D, Pennacchio LA, et al. Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nat Genet. 2008;40(12):1461–1465. doi: 10.1038/ng.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Forde KA, Tanapanpanit O, Reddy KR. Hepatitis B and C in African Americans: current status and continued challenges. Clin Gastroenterol Hepatol. 2014;12(5):738–748. doi: 10.1016/j.cgh.2013.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kallwitz ER, Guzman G, TenCate V, Vitello J, Layden-Almer J, Berkes J, et al. The histologic spectrum of liver disease in African-American, non-Hispanic white, and Hispanic obesity surgery patients. Am J Gastroenterol. 2009;104(1):64–69. doi: 10.1038/ajg.2008.12. [DOI] [PubMed] [Google Scholar]
- 73.Altekruse SF, McGlynn KA, Reichman ME. Hepatocellular carcinoma incidence, mortality, and survival trends in the United States from 1975 to 2005. J Clin Oncol. 2009;27(9):1485–1491. doi: 10.1200/JCO.2008.20.7753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kim D, Konyn P, Sandhu KK, Dennis BB, Cheung AC, Ahmed A. Increased all-cause mortality with metabolic dysfunction-associated fatty liver disease in the United States. J Hepatol. 2021 doi: 10.1016/j.jhep.2021.07.035. [DOI] [PubMed] [Google Scholar]
- 75.Nguyen VH, Le MH, Cheung RC, Nguyen MH. Differential clinical characteristics and mortality outcomes in persons with NAFLD and/or MAFLD. Clin Gastroenterol Hepatol. 2021 doi: 10.1016/j.cgh.2021.05.029. [DOI] [PubMed] [Google Scholar]
- 76.Anstee QM, Mantovani A, Tilg H, Targher G. Risk of cardiomyopathy and cardiac arrhythmias in patients with nonalcoholic fatty liver disease. Nat Rev Gastroenterol Hepatol. 2018;15(7):425–439. doi: 10.1038/s41575-018-0010-0. [DOI] [PubMed] [Google Scholar]
- 77.Targher G, Day CP, Bonora E. Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. N Engl J Med. 2010;363(14):1341–1350. doi: 10.1056/NEJMra0912063. [DOI] [PubMed] [Google Scholar]
- 78.Guerreiro GTS, Longo L, Fonseca MA, de Souza VEG, Álvares-da-Silva MR. Does the risk of cardiovascular events differ between biopsy-proven NAFLD and MAFLD? Hepatol Int. 2021;15(2):380–391. doi: 10.1007/s12072-021-10157-y. [DOI] [PubMed] [Google Scholar]
- 79.Stahl EP, Dhindsa DS, Lee SK, Sandesara PB, Chalasani NP, Sperling LS. Nonalcoholic fatty liver disease and the heart: JACC state-of-the-art review. J Am Coll Cardiol. 2019;73(8):948–963. doi: 10.1016/j.jacc.2018.11.050. [DOI] [PubMed] [Google Scholar]
- 80.Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. Circulation. 2019;140(11):e596–e646. doi: 10.1161/cir.0000000000000678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Athyros VG, Tziomalos K, Gossios TD, Griva T, Anagnostis P, Kargiotis K, et al. Safety and efficacy of long-term statin treatment for cardiovascular events in patients with coronary heart disease and abnormal liver tests in the Greek Atorvastatin and Coronary Heart Disease Evaluation (GREACE) Study: a post-hoc analysis. Lancet. 2010;376(9756):1916–1922. doi: 10.1016/s0140-6736(10)61272-x. [DOI] [PubMed] [Google Scholar]
- 82.Khoo S, Wong VW, Goh GB, Fan J, Chan WK, Seto WK, et al. Suboptimal treatment of dyslipidemia in patients with nonalcoholic fatty liver disease. J Gastroenterol Hepatol. 2020;35(2):320–325. doi: 10.1111/jgh.14794. [DOI] [PubMed] [Google Scholar]
- 83.Newsome PN, Buchholtz K, Cusi K, Linder M, Okanoue T, Ratziu V, et al. A placebo-controlled trial of subcutaneous semaglutide in nonalcoholic steatohepatitis. N Engl J Med. 2021;384(12):1113–1124. doi: 10.1056/NEJMoa2028395. [DOI] [PubMed] [Google Scholar]
- 84.Kahl S, Gancheva S, Straßburger K, Herder C, Machann J, Katsuyama H, et al. Empagliflozin effectively lowers liver fat content in well-controlled type 2 diabetes: a randomized, double-blind, phase 4, placebo-controlled trial. Diabetes Care. 2020;43(2):298–305. doi: 10.2337/dc19-0641. [DOI] [PubMed] [Google Scholar]
- 85.Hsiang JC, Wong VW. SGLT2 inhibitors in liver patients. Clin Gastroenterol Hepatol. 2020;18(10):2168–2172. doi: 10.1016/j.cgh.2020.05.021. e2162. [DOI] [PubMed] [Google Scholar]
- 86.Lee Y, Doumouras AG, Yu J, Brar K, Banfield L, Gmora S, et al. Complete resolution of nonalcoholic fatty liver disease after bariatric surgery: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2019;17(6):1040–1060.e1011. doi: 10.1016/j.cgh.2018.10.017. [DOI] [PubMed] [Google Scholar]
- 87.Angulo P, Kleiner DE, Dam-Larsen S, Adams LA, Bjornsson ES, Charatcharoenwitthaya P, et al. Liver fibrosis, but no other histologic features, is associated with long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology. 2015;149(2):389–397.e310. doi: 10.1053/j.gastro.2015.04.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kanwal F, Kramer JR, Mapakshi S, Natarajan Y, Chayanupatkul M, Richardson PA, et al. Risk of hepatocellular cancer in patients with non-alcoholic fatty liver disease. Gastroenterology. 2018;155(6):1828–1837.e1822. doi: 10.1053/j.gastro.2018.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Jarvis H, Craig D, Barker R, Spiers G, Stow D, Anstee QM, et al. Metabolic risk factors and incident advanced liver disease in non-alcoholic fatty liver disease (NAFLD): a systematic review and meta-analysis of population-based observational studies. PLoS Med. 2020;17(4):e1003100. doi: 10.1371/journal.pmed.1003100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Alexander M, Loomis AK, van der Lei J, Duarte-Salles T, Prieto-Alhambra D, Ansell D, et al. Risks and clinical predictors of cirrhosis and hepatocellular carcinoma diagnoses in adults with diagnosed NAFLD: real-world study of 18 million patients in four European cohorts. BMC Med. 2019;17(1):95. doi: 10.1186/s12916-019-1321-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Pang Y, Kartsonaki C, Turnbull I, Guo Y, Clarke R, Chen Y, et al. Diabetes, plasma glucose, and incidence of fatty liver, cirrhosis, and liver cancer: a prospective study of 0.5 million people. Hepatology. 2018;68(4):1308–1318. doi: 10.1002/hep.30083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kanwal F, Kramer JR, Li L, Dai J, Natarajan Y, Yu X, et al. Effect of metabolic traits on the risk of cirrhosis and hepatocellular cancer in nonalcoholic fatty liver disease. Hepatology. 2020;71(3):808–819. doi: 10.1002/hep.31014. [DOI] [PubMed] [Google Scholar]
- 93.Yang JD, Hainaut P, Gores GJ, Amadou A, Plymoth A, Roberts LR. A global view of hepatocellular carcinoma: trends, risk, prevention and management. Nat Rev Gastroenterol Hepatol. 2019;16(10):589–604. doi: 10.1038/s41575-019-0186-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.McGlynn KA, Petrick JL, El-Serag HB. Epidemiology of hepatocellular carcinoma. Hepatology. 2021;73(Suppl 1):4–13. doi: 10.1002/hep.31288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Wong VW, Wong GL, Chu WC, Chim AM, Ong A, Yeung DK, et al. Hepatitis B virus infection and fatty liver in the general population. J Hepatol. 2012;56(3):533–540. doi: 10.1016/j.jhep.2011.09.013. [DOI] [PubMed] [Google Scholar]
- 96.Yip TC, Wong VW, Chan HL, Tse YK, Kong AP, Lam KL, et al. Effects of diabetes and glycemic control on risk of hepatocellular carcinoma after seroclearance of hepatitis B surface antigen. Clin Gastroenterol Hepatol. 2018;16(5):765–773. doi: 10.1016/j.cgh.2017.12.009. e762. [DOI] [PubMed] [Google Scholar]
- 97.Chan AW, Wong GL, Chan HY, Tong JH, Yu YH, Choi PC, et al. Concurrent fatty liver increases risk of hepatocellular carcinoma among patients with chronic hepatitis B. J Gastroenterol Hepatol. 2017;32(3):667–676. doi: 10.1111/jgh.13536. [DOI] [PubMed] [Google Scholar]
- 98.Mak LY, Yuen MF, Seto WK. Letter regarding “a new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement”. J Hepatol. 2020;73(6):1573–1574. doi: 10.1016/j.jhep.2020.07.008. [DOI] [PubMed] [Google Scholar]
- 99.Chan TT, Chan WK, Wong GL, Chan AW, Nik Mustapha NR, Chan SL, et al. Positive hepatitis B core antibody is associated with cirrhosis and hepatocellular carcinoma in nonalcoholic fatty liver disease. Am J Gastroenterol. 2020;115(6):867–875. doi: 10.14309/ajg.0000000000000588. [DOI] [PubMed] [Google Scholar]
- 100.Mantovani A, Scorletti E, Mosca A, Alisi A, Byrne CD, Targher G. Complications, morbidity and mortality of nonalcoholic fatty liver disease. Metabolism. 2020;111S:154170. doi: 10.1016/j.metabol.2020.154170. [DOI] [PubMed] [Google Scholar]
- 101.Wang Z, Zhao X, Chen S, Wang Y, Cao L, Liao W, et al. Associations between nonalcoholic fatty liver disease and cancers in a large cohort in China. Clin Gastroenterol Hepatol. 2021;19(4):788–796. doi: 10.1016/j.cgh.2020.05.009. e784. [DOI] [PubMed] [Google Scholar]
- 102.Wong VW, Wong GL, Tsang SW, Fan T, Chu WC, Woo J, et al. High prevalence of colorectal neoplasm in patients with non-alcoholic steatohepatitis. Gut. 2011;60(6):829–836. doi: 10.1136/gut.2011.237974. [DOI] [PubMed] [Google Scholar]
- 103.Liu SS, Ma XF, Zhao J, Du SX, Zhang J, Dong MZ, et al. Association between nonalcoholic fatty liver disease and extrahepatic cancers: a systematic review and meta-analysis. Lipids Health Dis. 2020;19(1):118. doi: 10.1186/s12944-020-01288-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ahn JS, Sinn DH, Min YW, Hong SN, Kim HS, Jung SH, et al. Non-alcoholic fatty liver diseases and risk of colorectal neoplasia. Aliment Pharmacol Ther. 2017;45(2):345–353. doi: 10.1111/apt.13866. [DOI] [PubMed] [Google Scholar]
- 105.Allen AM, Hicks SB, Mara KC, Larson JJ, Therneau TM. The risk of incident extrahepatic cancers is higher in non-alcoholic fatty liver disease than obesity - a longitudinal cohort study. J Hepatol. 2019;71(6):1229–1236. doi: 10.1016/j.jhep.2019.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lee JM, Park YM, Yun JS, Ahn YB, Lee KM, Kim DB, et al. The association between nonalcoholic fatty liver disease and esophageal, stomach, or colorectal cancer: National population-based cohort study. PLoS One. 2020;15(1):e0226351. doi: 10.1371/journal.pone.0226351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kim GA, Lee HC, Choe J, Kim MJ, Lee MJ, Chang HS, et al. Association between non-alcoholic fatty liver disease and cancer incidence rate. J Hepatol. 2018;68(1):140–146. doi: 10.1016/j.jhep.2017.09.012. [DOI] [PubMed] [Google Scholar]
- 108.Center MM, Jemal A, Lortet-Tieulent J, Ward E, Ferlay J, Brawley O, et al. International variation in prostate cancer incidence and mortality rates. Eur Urol. 2012;61(6):1079–1092. doi: 10.1016/j.eururo.2012.02.054. [DOI] [PubMed] [Google Scholar]
- 109.Choi YJ, Lee DH, Han KD, Yoon H, Shin CM, Park YS, et al. Is nonalcoholic fatty liver disease associated with the development of prostate cancer? A nationwide study with 10,516,985 Korean men. PLoS One. 2018;13(9):e0201308. doi: 10.1371/journal.pone.0201308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Chang JS, Tsai CR, Chen LT. Medical risk factors associated with cholangiocarcinoma in Taiwan: a population-based case-control study. PLoS One. 2013;8(7):e69981. doi: 10.1371/journal.pone.0069981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Lee BS, Cha BH, Park EC, Roh J. Risk factors for perihilar cholangiocarcinoma: a hospital-based case-control study. Liver Int. 2015;35(3):1048–1053. doi: 10.1111/liv.12618. [DOI] [PubMed] [Google Scholar]
- 112.Welzel TM, Graubard BI, El-Serag HB, Shaib YH, Hsing AW, Davila JA, et al. Risk factors for intrahepatic and extrahepatic cholangiocarcinoma in the United States: a population-based case-control study. Clin Gastroenterol Hepatol. 2007;5(10):1221–1228. doi: 10.1016/j.cgh.2007.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Mantovani A, Petracca G, Beatrice G, Csermely A, Tilg H, Byrne CD, et al. Non-alcoholic fatty liver disease and increased risk of incident extrahepatic cancers: a meta-analysis of observational cohort studies. Gut. 2021 doi: 10.1136/gutjnl-2021-324191. [DOI] [PubMed] [Google Scholar]
- 114.Ma RCW. Epidemiology of diabetes and diabetic complications in China. Diabetologia. 2018;61(6):1249–1260. doi: 10.1007/s00125-018-4557-7. [DOI] [PubMed] [Google Scholar]
- 115.Musso G, Gambino R, Tabibian JH, Ekstedt M, Kechagias S, Hamaguchi M, et al. Association of non-alcoholic fatty liver disease with chronic kidney disease: a systematic review and meta-analysis. PLoS Med. 2014;11(7):e1001680. doi: 10.1371/journal.pmed.1001680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Sun DQ, Jin Y, Wang TY, Zheng KI, Rios RS, Zhang HY, et al. MAFLD and risk of CKD. Metabolism. 2021;115:154433. doi: 10.1016/j.metabol.2020.154433. [DOI] [PubMed] [Google Scholar]
- 117.Zhang HJ, Wang YY, Chen C, Lu YL, Wang NJ. Cardiovascular and renal burdens of metabolic associated fatty liver disease from serial US national surveys, 1999-2016. Chin Med J (Engl) 2021;134(13):1593–1601. doi: 10.1097/CM9.0000000000001513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Yeung MW, Wong GL, Choi KC, Luk AO, Kwok R, Shu SS, et al. Advanced liver fibrosis but not steatosis is independently associated with albuminuria in Chinese patients with type 2 diabetes. J Hepatol. 2018;68(1):147–156. doi: 10.1016/j.jhep.2017.09.020. [DOI] [PubMed] [Google Scholar]
- 119.Wong VW, Chan WK, Chitturi S, Chawla Y, Dan YY, Duseja A, et al. Asia-Pacific Working Party on non-alcoholic fatty liver disease guidelines 2017-Part 1: definition, risk factors and assessment. J Gastroenterol Hepatol. 2018;33(1):70–85. doi: 10.1111/jgh.13857. [DOI] [PubMed] [Google Scholar]
- 120.Wong VW, Wong GL, Chan RS, Shu SS, Cheung BH, Li LS, et al. Beneficial effects of lifestyle intervention in non-obese patients with non-alcoholic fatty liver disease. J Hepatol. 2018;69(6):1349–1356. doi: 10.1016/j.jhep.2018.08.011. [DOI] [PubMed] [Google Scholar]
- 121.Wong VW, Chitturi S, Wong GL, Yu J, Chan HL, Farrell GC. Pathogenesis and novel treatment options for non-alcoholic steatohepatitis. Lancet Gastroenterol Hepatol. 2016;1(1):56–67. doi: 10.1016/S2468-1253(16)30011-5. [DOI] [PubMed] [Google Scholar]
- 122.Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jodar E, Leiter LA, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016;375(19):1834–1844. doi: 10.1056/NEJMoa1607141. [DOI] [PubMed] [Google Scholar]