Abstract
This paper provides new evidence on the role of city planning, urban form, and built environment characteristics in health and well-being during the coronavirus disease (COVID-19) pandemic. Based on survey and geographic information systems (GIS) data from Oslo and Viken in Norway, the paper investigates changes in health and well-being due to COVID-19 and how the compact city and its characteristics relate to these changes. Findings indicate that self-reported measures of health and well-being worsened due to COVID-19. The most substantial changes were reported for life satisfaction, anxiety, and satisfaction with leisure, personal relationships, and vacations. General health, happiness, and satisfaction with income also declined during COVID-19 in comparison with pre-COVID-19 times. Overall, residents of compact neighborhoods reported lower well-being during COVID-19 compared to residents of lower-density neighborhoods. Important compact city characteristics – higher neighborhood density, reliance on public transport, smaller dwellings, and less green space – were negatively associated with well-being and health outcomes during COVID-19. In contrast, another compact city attribute, the presence of numerous local facilities, was positively linked to well-being and health during COVID-19. Based on these findings, the paper presents possible implications for sustainable urban planning and compact cities.
Keywords: Compact cities, Urban sprawl, Coronavirus disease (COVID-19) pandemic, Sustainable city planning, Urban sustainability, Pandemic-resilient cities
Graphical abstract
1. Introduction
The coronavirus disease (COVID-19) pandemic has caused numerous deaths worldwide but has also indirectly affected physical and mental health, and most, if not all, domains of life (Brooks et al., 2020; Fiorillo and Gorwood, 2020; Li et al., 2020; Moreno et al., 2020; Patrick et al., 2020; White and Van Der Boor, 2020). This indirect impact of COVID-19 on health and well-being can be attributed to measures that were implemented to slow down infection rates: lockdowns, quarantines, social distancing measures, travel restrictions, and closing of businesses and facilities. The risk of infection together with these unforeseen measures contributed to stress and fear of infection, unemployment, loss of income, economic instability, insecurity for the future, lack of social connectedness, feelings of isolation, problems in social relationships, lack of participation in favorite activities, limited options for doing sports and physical exercise, and inability to travel for leisure.
The role of cities, city planning, and built environment characteristics in the changes in health and well-being occurring due to COVID-19 has not been sufficiently investigated yet. Urban form and built environment characteristics can contribute to health and well-being in several ways (Hamidi et al., 2018; Litman, 2020b; Mouratidis, 2021b; Stevenson et al., 2016). But more knowledge is needed on how compact versus sprawled urban forms and their characteristics might have contributed to health and well-being during the COVID-19 times. The compact city is a type of urban form and public policy that offers multiple environmental, societal, and economic benefits compared to urban sprawl (Dye, 2008; Glaeser, 2011; Meyer, 2013; Mouratidis, 2018b), and is therefore widely considered the preferred model in the quest for sustainable urban planning and policy (Bibri et al., 2020; OECD, 2018). Studying the links between urban form compactness (and its characteristics) and health and well-being during COVID-19 times in diverse contexts can shed light on a timely, critical issue for sustainable urban planning and offer evidence-based knowledge for possible policy recommendations for compact cities in times of pandemic crises.
This study provides new evidence on changes in self-reported health and well-being due to COVID-19 and investigates how the compact city relates to these changes. It is one of the first studies to combine survey data with geographic information systems (GIS) data on the built environment in order to examine links between compact city planning and health/well-being changes due to COVID-19. Two research questions are addressed: (1) How did self-reported health and well-being change before versus during COVID-19? (2) How do compact city characteristics relate to health and well-being before and during COVID-19? The study focuses on the region of Oslo and Viken in Norway. This region includes both compact and low-density urban environments with diverse spatial characteristics, thus offering a useful case for exploring the research questions of the study.
2. Literature review
2.1. Compact city planning and well-being
The links between compact city characteristics and health and well-being have been widely studied in the period before COVID-19 (e.g. Ala-Mantila et al., 2018; Cao, 2016; Ettema and Schekkerman, 2016; Howley et al., 2009; Ihlebæk et al., 2021; Kyttä et al., 2016; Markevych et al., 2017; Mouratidis, 2018a, Mouratidis, 2019a; Mouratidis, 2019b; Wang and Wang, 2016). Compact cities – cities of short distances enabled by higher densities – offer both advantages and disadvantages in relation to health and well-being. They provide greater access to destinations, enable the use of efficient public transport systems, provide walkable access to a wider range of facilities, and provide access to the public realm. Thereby, they have been linked to increased walking, lower obesity, higher life expectancy, increased overall social activity, increased travel satisfaction, and higher residential satisfaction (Cosby et al., 2019; Dye, 2008; Hamidi et al., 2018; Litman, 2020b; Melis et al., 2015; Mouratidis, 2018a, Mouratidis, 2018b; Mouratidis et al., 2019; Saelens and Handy, 2008; Stevenson et al., 2016). Increased overall social activity in compact cities not only contributes to social capital and well-being but also to resilience during adverse events such as pandemics (Sharifi, 2019). On the other hand, compact urban forms have some considerable disadvantages. They cannot provide the benefits that low-density suburbs can offer, as they typically lack ample green space and private gardens, while they tend to be noisier and to have higher air pollution at a local level (Howley et al., 2009; Tao et al., 2020). Dwellings in compact urban forms are also typically smaller than the ones found in suburban detached housing, with possible negative implications for well-being. Furthermore, although compact urban form enables social activity at a city level, social relationships at a neighborhood level tend to be weaker than those in low-density suburban areas (French et al., 2014; Mouratidis and Poortinga, 2020). Disadvantages of compact cities might be responsible for some negative mental health outcomes reported in the literature, although causality should be further examined (Gruebner et al., 2017; Litman, 2020b).
2.2. Compact cities and well-being under COVID-19
Human health, including physical and mental health, and human well-being, including quality of life domains and overall subjective well-being, declined due to COVID-19 in several, if not most, parts of the world (e.g. Brooks et al., 2020; Fiorillo and Gorwood, 2020; Moreno et al., 2020). Although early evidence suggests that health and well-being declined due to COVID-19, little empirical knowledge exists on how this change is linked to city planning and the compact city model in specific. Several studies have already discussed issues around city planning and COVID-19 (Barak et al., 2021; Connolly et al., 2020; Florida et al., 2021; Hamidi et al., 2020; Honey-Rosés et al., 2020; Litman, 2020a; Mouratidis, 2021a; Sharifi and Khavarian-Garmsir, 2020; Trasberg and Cheshire, 2021), but empirical evidence on how compact urban form relates to changes in health and well-being due to COVID-19 is limited (McFarlane, 2021). A synthesis of existing knowledge of how compact city characteristics could contribute to health and well-being during COVID-19 is presented in Table A1 (Appendix A).
Based on what is known about how and where the virus SARS-CoV-2 typically spreads, we could reasonably expect that some of the established benefits of compact urban form might have attenuated during the pandemic. Indeed, early evidence suggests that denser neighborhoods were associated with lower well-being outcomes during COVID-19 (Mouratidis and Yiannakou, 2021). Quarantines, social distancing, risk of infection, the closing of facilities and businesses, and travel restrictions might have substantially reduced some compact city benefits such as the use of lively public spaces, walking activity, use of public transport, socializing in cafes and restaurants, and easy access to other parts of the city or the airport (Bucsky, 2020; de Haas et al., 2020; Gössling et al., 2021; Honey-Rosés et al., 2020).
Although some compact city benefits might have attenuated during COVID-19, the high accessibility to local facilities (typical for compact urban forms) that remained open during the pandemic could still prove to be important to perform certain activities (Litman, 2020a). For example, good access to high-quality healthcare facilities and services have provided health benefits during the pandemic and has been linked to lower mortality from COVID-19 (Hamidi et al., 2020; Lieberman-Cribbin et al., 2020; Peto, 2020). Other potential compact city benefits during COVID-19 could be the possibly better internet access which was crucial during the pandemic, better access to food deliveries and other forms of online shopping (Mouratidis and Papagiannakis, 2021), and the access to public spaces when restrictions allowed (Honey-Rosés et al., 2020). Compact cities and compact neighborhoods, that are typically more noisy and more polluted than low density areas, might have benefited more from the reduced noise and air pollution (Sharifi and Khavarian-Garmsir, 2020) due to reduced urban mobility during COVID-19 (Politis et al., 2021; Shakibaei et al., 2021). Nevertheless, poor air quality, found in certain compact cities, might have increased the risk of infection, mortality, and fatality due to COVID-19 (Mondal et al., 2022; Sarkodie and Owusu, 2021).
The importance of certain advantages of low-density development might have increased during COVID-19. Lockdowns, quarantines, and social distancing measures have forced large parts of the population to spend most of the time at home. Thus, living in a larger dwelling, typically found in the suburbs, facilitated daily life activities and possibly provided well-being and mental health benefits (Ahmad et al., 2020; Amerio et al., 2020; Mouratidis and Yiannakou, 2021; Tinson and Clair, 2020). In addition, private gardens attached to dwellings typically found in low-density sprawled development and large green spaces found in low-density areas (but also in some compact areas) seem to be particularly important during COVID-19 as they provide space for performing activities with a low risk of infection (Poortinga et al., 2021; Pouso et al., 2021; Shoari et al., 2020; Slater et al., 2020; Ugolini et al., 2020; Venter et al., 2020; Xie et al., 2020). Another attribute of suburban living that has been strengthened during COVID-19 is related to mobility. The mobility of residents of low-density suburbs is to a high degree dependent on the private car. Private cars have been safer to use (when driving alone) during COVID-19 than public transport especially for long commutes (Hu et al., 2021; Sun and Zhai, 2020), and this contributed to a more substantial decrease in the use of public transport compared to other transport modes (Bucsky, 2020; Jenelius and Cebecauer, 2020). Thereby, residents of low-density neighborhoods might have experienced lower risk and less fear of infection related to daily-life travel but also more opportunities for safe mobility compared to residents of compact areas, for whom public transport may be the only option for traveling medium or long distances. Those transit-dependent residents, especially those employed in professions requiring a physical presence, continued to travel to work during COVID-19 (Hu and Chen, 2021) and might have experienced negative feelings and stress while using public transport due to the associated risk of infection (Shamshiripour et al., 2020).
In this paper, the aim is to provide evidence that sheds more light on the relationship between compact city characteristics and health/well-being changes due to COVID-19. Then findings are discussed considering the theoretical background and possible mechanisms presented here. It should be however noted that the analysis presented in this paper is exploratory and not confirmatory, as theory and empirical research on the built environment and COVID-19-related changes in health/well-being are still rather immature.
3. Data and methods
3.1. Data sources
Data collection was carried out in the counties of Oslo and Viken in Norway (Fig. A1, Appendix A) for a research project on mobility and quality of life. In 2019, Oslo county had approximately 670,000 inhabitants and Viken, the region surrounding Oslo, had approximately 1,230,000 inhabitants. The area of Oslo and Viken is highly monocentric and has a center-periphery gradient. The city center of Oslo is the main economic and cultural center of the area. Population densities tend to be higher the closer one gets to Oslo city center (Fig. A1, Appendix A). Residents of Oslo and Viken may travel to central parts of Oslo on a regular basis to access workplaces and educational, cultural, and commercial facilities.
An overview of the methodology of the study is displayed in Fig. A2 (Appendix A). Data were collected via a population-based questionnaire survey and analysis with GIS. The survey was conducted in Oslo and Viken during June–August 2020, some months after COVID-19 was declared a pandemic by the World Health Organization. Survey participants were asked to consider the period with the strictest COVID-19-related measures (this was March–May 2020) when answering questions concerning COVID-19 (see Section 3.2). Norway had less severe restrictions compared to certain European countries. While several establishments were temporarily closed (e.g. businesses, restaurants, fitness centers, and cultural venues), some businesses and facilities remained open. However, overall, restrictions had a strong impact on the society and economy in Norway.
The final survey sample comprises 1796 residents of Oslo and Viken aged 19–95 years. Participants resided in a variety of locations in Oslo and Viken as seen in Fig. A1 (Appendix A). Before distributing the survey, ethics approval was received for the research project (reference number 869419) by the Norwegian Center for Research Data (NSD). Next, an application was sent to the Norwegian Tax Administration for obtaining a list of the residential addresses of all the residents of Oslo and Viken. Then 20,000 letters were sent by post inviting residents to participate in a web-based survey. The letters included a web address that needed to be typed in an internet browser to access the online survey. Only one member per household and only adult residents were invited. Oslo and Viken were divided into four different zones and then random sample selection was performed within each of these zones. The distribution of invitation letters comprised 12,000 letters in the county of Oslo (8000 letters in the inner city and 4000 letters in the outer city) and 8000 letters in the county of Viken (4000 letters in outer suburbs of Oslo and 4000 letters in peripheral towns and rural areas). The aim of this selection process was to obtain diversity in urban form and residential locations in the sample. The first aim was to obtain a balance between compact and lower density urban forms. Since only about a third of Oslo residents lives in compact neighborhoods (typically located in the inner city), these residents had to be oversampled (8000 letters) to produce a more balanced sample that includes a good representation of residents of compact neighborhoods and residents of lower density neighborhoods. Indeed, about half of the residents in the obtained sample reside in apartment blocks typically located in denser neighborhoods and the other half reside in housing types found in lower density urban forms, e.g. detached houses, duplexes, and row houses (see Table A2, Appendix A). The second aim of the sampling process was related to residential location. Oslo inner city was oversampled for the aforementioned reasons, while an equal number of letters was sent to inner suburbs, outer suburbs, and peripheral areas (4000 letters in each type of area) to ensure a good representation of these different residential locations. The invitation letter and the survey questions were in both Norwegian and English languages. Prior to sending the final survey, a pilot test was performed, and the survey was revised accordingly. Participation in the survey did not include monetary or other incentives. Excluding letters distributed to wrong addresses, the survey response rate was 9.4%. Table A3 in Appendix A compares the sample's sociodemographic characteristics with those of the population.
3.2. Variable descriptions
Table A2 (Appendix A) presents descriptive statistics on the built environment characteristics examined in the study. These characteristics are all related to urban form compactness. The geospatial analysis for the following built environment characteristics was performed with GIS. Survey participants filled in their residential addresses when completing the survey. The residential addresses were georeferenced and then built environment characteristics were measured in GIS for each residential location individually: distance to city center, neighborhood density, public transport, local facilities, and green space. Distance to city center was calculated in kilometers along the walking network. This measure was used to assess the location of each participant's dwelling in relation to the city center of Oslo. Neighborhood density was assessed as the population density within a 1000 m buffer from each participant's dwelling. It was measured in persons per hectare based on the 2019 population dataset for statistical grids (250 m × 250 m) from Statistics Norway. Public transport accessibility was calculated as the number of bus, tram, metro, and train stops within a 1000 m buffer from each participant's dwelling. This analysis was based on OpenStreetMap data. Local facilities were assessed as the number of facilities within a 1000 m buffer from each participant's dwelling. This analysis was based on “amenity” OpenStreetMap data. The analysis included all types of facilities in the dataset such as: restaurants, cafés, cinemas, theaters, post offices, schools, libraries, hospitals, and banks. Green space was measured as the percentage of green space area within a 1000 m buffer from each participant's dwelling, based on 2019 data by Hansen et al. (2013). Two additional characteristics of the built environment were captured via the survey. These are attributes of the dwelling of each participant. The survey included a question on the type of dwelling that the participant lives in. This item was later coded as 1 = apartment and 0 = other (e.g. detached house, duplex). The second dwelling attribute obtained via the survey is the size of each participant's dwelling, measured in square meters. This question was optional, for privacy reasons, so the sample size is smaller for this variable due to missing data. Table A4 in Appendix A presents a correlation matrix showing bivariate correlations between built environment characteristics.
Health and well-being variables and individual sociodemographic characteristics were obtained via the survey. Descriptive statistics for health and well-being data are presented in Table A5 in Appendix A. The survey questions are presented in detail in Appendix B. For the questions on health and well-being, survey participants were asked to consider their “life during the lockdown (the period with the most restrictions) due to the coronavirus pandemic (COVID-19)” and their “life right before the COVID-19 pandemic”. The questions on health and well-being are based on questions from the European Social Survey (2012) and OECD (2013). Participants responded to the question “How satisfied are/were you with your...?” for different items: “life as a whole”, “health status”, “leisure activities”, “vacations”, “personal income”, and “personal relationships”. The scale used ranged from “extremely dissatisfied” (0) to “extremely satisfied” (10). To evaluate their general health (self-reported health) participants were asked “How would you describe your health in general?”. The scale ranged from “extremely poor” (0) to “extremely good” (10). Participants were also asked “Please tell us how much of the time you felt…” for the items: “happiness”, “anxiety”, “headache”, and “back pain”. The scale used ranged from “very rarely or never” (1) to “very often or always” (5). All health and well-being variables were evaluated for both “before COVID-19” and “during COVID-19”.
3.3. Analytical methods
For the analysis addressing the first research question – how health and well-being changed before and during COVID-19 – paired t-tests and Wilcoxon signed-rank tests were performed. This analysis tested for significant differences in each health/well-being measure before versus during COVID-19. The paired t-test and the Wilcoxon signed-rank test are used to examine the difference between two variables for the same subject. Since health and well-being were measured at two different times, before and during COVID-19, for the same individuals, with a “natural intervention” (i.e. COVID-19) occurring between the two, these two tests are suitable for detecting significant differences.
For the second research question – how compact city characteristics relate to health and well-being before and during COVID-19 – multiple linear regression was used. Built environment and sociodemographic characteristics were the independent variables. Since built environment and sociodemographic characteristics and health and well-being were all measured at the individual level, there was no need for multilevel modeling approaches. Health and well-being variables were examined as dependent variables, each one with a different regression model. These variables were: life satisfaction, personal relationships satisfaction, leisure satisfaction, general health, happiness, and anxiety. The other health and well-being variables in the dataset were excluded from this analysis to reduce complexity and keep the study more focused on basic health and well-being indicators. Based on previous theoretical models on the built environment in monocentric areas such as the one of Oslo and Viken (Mouratidis and Poortinga, 2020; Næss, 2019), a two-step approach was followed for the inclusion of built environment characteristics in the models. The first step examines the variables neighborhood density and distance to city center, while the second step additionally examines variables influenced by density and distance to city center: local facilities, green space, public transport, and dwelling characteristics. All models include individual sociodemographic variables as covariates: age, gender, unemployment, cohabitation status, citizenship, income, education level, presence of children in household, religiosity, and disability. Models on life satisfaction and happiness additionally include an “age squared” variable to capture their U-shaped relationship with age. Finally, to understand the relationships between compact city characteristics, bivariate correlation analyses were conducted (Table A4, Appendix A).
4. Results
4.1. Health and well-being before versus during COVID-19
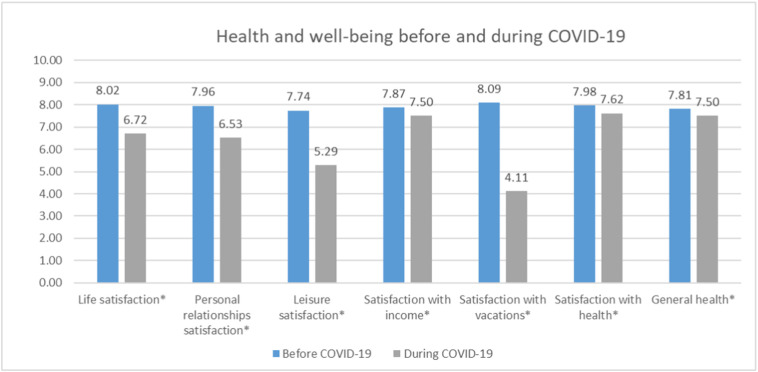
The first part of the analysis compares health and well-being before and during COVID-19. The distributions of health and well-being variables are presented in Figs. A3 and A4 (Appendix A). The means of health and well-being variables before and during COVID-19 and comparisons with paired t-tests and Wilcoxon signed-rank tests are presented in Figs. 1 and 2 . Results show that all health and well-being variables significantly worsened during COVID-19 compared to before COVID-19. Differences are all statistically significant at the p < 0.001 level. The most substantial changes are reported for well-being measures: life satisfaction (16% decrease), anxiety (25% increase), personal relationships satisfaction (18% decrease), leisure satisfaction (32% decrease), and satisfaction with vacations (49% decrease). The changes in general health (4% decrease), satisfaction with health (5% decrease), headache (3% increase), back pain (6% increase), happiness (9% decrease), and satisfaction with income (5% decrease) are smaller in size, but still statistically significant.
Fig. 1.
Health and well-being (mean values) before and during COVID-19 in Oslo and Viken (1/2). Notes: *p < 0.001: significant differences based on paired t-tests as well as Wilcoxon signed-rank tests. Variables are measured on a scale from 0 to 10.
Fig. 2.

Health and well-being (mean values) before and during COVID-19 in Oslo and Viken (2/2). Notes: *p < 0.001: significant differences based on paired t-tests as well as Wilcoxon signed-rank tests. Variables are measured on a scale from 1 to 5.
Next, the relationships between individual characteristics and the changes in health and well-being before-during COVID-19 were examined with multiple linear regression models that include all sociodemographic variables shown in Table A2 (Appendix A) as independent variables and the change for each health and well-being variable before-during COVID-19 as the dependent variable. Since these relationships are not the main focus of the paper, their regression tables are not presented here to reduce the number of tables. The main findings are as follows. Females experienced larger decreases in life satisfaction, happiness, personal relationships satisfaction, leisure satisfaction, and satisfaction with vacations, and a larger increase in anxiety and frequency of back pain. Older adults experienced a larger decrease in personal relationships satisfaction, smaller decreases in general health and satisfaction with income, and a smaller increase in the frequency of back pain. Non-Norwegians and unemployed individuals had a larger decrease in satisfaction with income. Highly educated individuals had smaller decreases in life satisfaction, personal relationships satisfaction, satisfaction with income, and satisfaction with vacations. Those living with a spouse or partner experienced smaller decreases in happiness and personal relationships satisfaction. Those with children in their household had smaller decreases in life satisfaction, personal relationships satisfaction, and leisure satisfaction and a smaller increase in the frequency of back pain. Individuals with higher household incomes had a larger decrease in satisfaction with vacations. Religious individuals had a larger decrease in general health and a larger increase in anxiety. Individuals with serious health problems or a disability had a smaller decrease in life satisfaction.
4.2. Compact city, health, and well-being before-during COVID-19
The second part of the analysis investigates how the compact city and its characteristics relate to health and well-being. Table 1, Table 2, Table 3, Table 4, Table 5, Table 6 present the results of linear regression models. Each table examines a different health or well-being measure as the dependent variable. The analysis was performed for health and well-being: before COVID-19, during COVID-19, and for the change before-during COVID-19. The analysis for before COVID-19 examines associations between compact city characteristics and health/well-being for the pre-COVID-19 period, the analysis for during COVID-19 examines these associations for the COVID-19 period, the analysis for the change before-during COVID-19 investigates whether and how compact city characteristics relate to the increase or decrease of a health/well-being variable due to COVID-19. Each table consists of Models 1 and 2 (columns 1 and 2) corresponding to the two steps explained in Section 3.3. All the analyses include individual sociodemographic characteristics as covariates. Their coefficients are not presented here to reduce the size of the tables.
Table 1.
Regression models of life satisfaction before and during COVID-19.
| Variables |
Life satisfaction |
|||||
|---|---|---|---|---|---|---|
| Before COVID-19 |
During COVID-19 |
Change (Before − During COVID-19) |
||||
| 1 |
2 |
1 |
2 |
1 |
2 |
|
| Built environment | β (B, SE) |
β (B, SE) |
β (B, SE) |
β (B, SE) |
β (B, SE) |
β (B, SE) |
| Distance to city center | 0.042 (0.0024, 0.0015) |
0.045 (0.0025, 0.0016) |
0.009 (0.0007, 0.0020) |
−0.013 (−0.0009, 0.0022) |
0.025 (0.0017, 0.0019) |
0.051 (0.0035, 0.0021) |
| Neighborhood density | −0.028 (−0.0008, 0.0008) |
−0.071 (−0.0021, 0.0016) |
−0.085⁎⁎ (−0.0033, 0.0011) |
−0.098 (−0.0038, 0.0022) |
0.069⁎ (0.0025, 0.0011) |
0.047 (0.0017, 0.0021) |
| Public transport | 0.010 (0.0003, 0.0015) |
−0.035 (−0.0016, 0.0020) |
0.045 (0.0019, 0.0019) |
|||
| Local facilities | −0.039 (−0.0002, 0.0003) |
0.065 (0.0004, 0.0004) |
−0.102 (−0.0006, 0.0003) |
|||
| Green space | −0.064⁎ (−0.0069, 0.0034) |
−0.002 (−0.0003, 0.0046) |
−0.051 (−0.0065, 0.0043) |
|||
| Apartment | 0.040 (0.1229, 0.1027) |
−0.004 (−0.0153, 0.1374) |
0.037 (0.1382, 0.1301) |
|||
| Dwelling size | 0.010 (0.0002, 0.0007) |
0.073⁎ (0.0021, 0.0010) |
−0.071⁎ (−0.0019, 0.0009) |
|||
| Summary statistics | ||||||
| N | 1796 | 1760 | 1796 | 1760 | 1796 | 1760 |
| Adjusted R-squared | 0.143 | 0.145 | 0.077 | 0.078 | 0.037 | 0.042 |
Notes: Coefficients out of the parenthesis are standardized beta coefficients. The parenthesis includes the unstandardized coefficient and the standard error of the estimate. The models include individual sociodemographic variables as covariates (coefficients not shown here to reduce complexity): age, age squared, gender, unemployment, cohabitation status, citizenship, income, education level, presence of children in household, religiosity, and disability.
p < 0.05.
p < 0.01.
Table 2.
Regression models of personal relationships satisfaction before and during COVID-19.
| Variables |
Personal relationships satisfaction |
|||||
|---|---|---|---|---|---|---|
| Before COVID-19 |
During COVID-19 |
Change (Before − During COVID-19) |
||||
| 1 |
2 |
1 |
2 |
1 |
2 |
|
| Built environment | β (B, SE) |
β (B, SE) |
β (B, SE) |
β (B, SE) |
β (B, SE) |
β (B, SE) |
| Distance to city center | 0.040 (0.0024, 0.0016) |
0.040 (0.0024, 0.0017) |
0.029 (0.0024, 0.0023) |
0.003 (0.0002, 0.0025) |
−0.001 (−0.0001, 0.0021) |
0.028 (0.0021, 0.0023) |
| Neighborhood density | 0.003 (0.0001, 0.0009) |
−0.073 (−0.0023, 0.0017) |
−0.021 (−0.0009, 0.0013) |
−0.087 (−0.0038, 0.0025) |
0.026 (0.0010, 0.0012) |
0.038 (0.0015, 0.0023) |
| Public transport | 0.028 (0.0010, 0.0016) |
−0.030 (−0.0015, 0.0023) |
0.055 (0.0026, 0.0021) |
|||
| Local facilities | 0.009 (0.0000, 0.0003) |
0.121⁎ (0.0009, 0.0004) |
−0.125⁎ (−0.0008, 0.0004) |
|||
| Green space | −0.045 (−0.0049, 0.0036) |
−0.013 (−0.0020, 0.0052) |
−0.021 (−0.0030, 0.0048) |
|||
| Apartment | 0.041 (0.1304, 0.1085) |
−0.023 (−0.1034, 0.1563) |
0.057 (0.2338, 0.1435) |
|||
| Dwelling size | 0.034 (0.0008, 0.0008) |
0.054 (0.0017, 0.0011) |
−0.032 (−0.0010, 0.0010) |
|||
| Summary statistics | ||||||
| N | 1796 | 1760 | 1796 | 1760 | 1796 | 1760 |
| Adjusted R-squared | 0.104 | 0.107 | 0.050 | 0.053 | 0.052 | 0.052 |
Notes: Coefficients shown out of the parenthesis are standardized beta coefficients. The parenthesis includes the unstandardized coefficient and the standard error of the estimate. The models include individual sociodemographic variables as covariates (coefficients not shown here to reduce complexity): age, gender, unemployment, cohabitation status, citizenship, income, education level, presence of children in household, religiosity, and disability.
p < 0.05.
Table 3.
Regression models of leisure satisfaction before and during COVID-19.
| Variables |
Leisure satisfaction |
|||||
|---|---|---|---|---|---|---|
| Before COVID-19 |
During COVID-19 |
Change (Before − During COVID-19) |
||||
| 1 |
2 |
1 |
2 |
1 |
2 |
|
| Built environment | β (B, SE) |
β (B, SE) |
β (B, SE) |
β (B, SE) |
β (B, SE) |
β (B, SE) |
| Distance to city center | 0.018 (0.0012, 0.0018) |
0.005 (0.0003, 0.0019) |
0.033 (0.0032, 0.0027) |
0.011 (0.0011, 0.0029) |
−0.020 (−0.0020, 0.0029) |
−0.008 (−0.0008, 0.0031) |
| Neighborhood density | −0.008 (−0.0003, 0.0010) |
−0.026 (−0.0009, 0.0019) |
−0.071⁎ (−0.0037, 0.0015) |
−0.070 (−0.0036, 0.0029) |
0.064⁎ (0.0034, 0.0016) |
0.051 (0.0027, 0.0031) |
| Public transport | −0.058 (−0.0023, 0.0018) |
−0.013 (−0.0008, 0.0027) |
−0.024 (−0.0015, 0.0029) |
|||
| Local facilities | 0.030 (0.0002, 0.0003) |
0.064 (0.0005, 0.0005) |
−0.043 (−0.0004, 0.0005) |
|||
| Green space | −0.046 (−0.0055, 0.0040) |
0.040 (0.0074, 0.0062) |
−0.068⁎ (−0.0129, 0.0065) |
|||
| Apartment | 0.000 (−0.0008, 0.1190) |
−0.020 (−0.1080, 0.1847) |
0.020 (0.1072, 0.1940) |
|||
| Dwelling size | 0.027 (0.0007, 0.0008) |
0.050 (0.0019, 0.0013) |
−0.031 (−0.0012, 0.0013) |
|||
| Summary statistics | ||||||
| N | 1796 | 1760 | 1796 | 1760 | 1796 | 1760 |
| Adjusted R-squared | 0.077 | 0.075 | 0.048 | 0.051 | 0.007 | 0.008 |
Notes: Coefficients shown out of the parenthesis are standardized beta coefficients. The parenthesis includes the unstandardized coefficient and the standard error of the estimate. The models include individual sociodemographic variables as covariates (coefficients not shown here to reduce complexity): age, gender, unemployment, cohabitation status, citizenship, income, education level, presence of children in household, religiosity, and disability.
p < 0.05.
Table 4.
Regression models of general health before and during COVID-19.
| Variables |
General health |
|||||
|---|---|---|---|---|---|---|
| Before COVID-19 |
During COVID-19 |
Change (Before − During COVID-19) |
||||
| 1 |
2 |
1 |
2 |
1 |
2 |
|
| Built environment | β (B, SE) |
β (B, SE) |
β (B, SE) |
β (B, SE) |
β (B, SE) |
β (B, SE) |
| Distance to city center | 0.011 (0.0007, 0.0016) |
0.011 (0.0007, 0.0017) |
0.032 (0.0023, 0.0018) |
0.015 (0.0011, 0.0020) |
−0.040 (−0.0016, 0.0011) |
−0.010 (−0.0004, 0.0012) |
| Neighborhood density | −0.016 (−0.0005, 0.0009) |
−0.039 (−0.0013, 0.0017) |
−0.014 (−0.0005, 0.0010) |
−0.047 (−0.0018, 0.0020) |
0.000 (−0.0000, 0.0006) |
0.022 (0.0005, 0.0012) |
| Public transport | 0.024 (0.0009, 0.0016) |
−0.032 (−0.0014, 0.0018) |
0.094⁎ (0.0023, 0.0011) |
|||
| Local facilities | 0.017 (0.0001, 0.0003) |
0.099 (0.0006, 0.0003) |
−0.149⁎⁎ (−0.0005, 0.0002) |
|||
| Green space | 0.008 (0.0010, 0.0035) |
0.030 (0.0040, 0.0041) |
−0.040 (−0.0030, 0.0026) |
|||
| Apartment | 0.007 (0.0253, 0.1057) |
−0.001 (−0.0040, 0.1228) |
0.014 (0.0293, 0.0770) |
|||
| Dwelling size | 0.008 (0.0002, 0.0007) |
0.030 (0.0008, 0.0009) |
−0.041 (−0.0006, 0.0005) |
|||
| Summary statistics | ||||||
| N | 1796 | 1760 | 1796 | 1760 | 1796 | 1760 |
| Adjusted R-squared | 0.248 | 0.244 | 0.208 | 0.208 | 0.009 | 0.015 |
Notes: Coefficients shown out of the parenthesis are standardized beta coefficients. The parenthesis includes the unstandardized coefficient and the standard error of the estimate. The models include individual sociodemographic variables as covariates (coefficients not shown here to reduce complexity): age, gender, unemployment, cohabitation status, citizenship, income, education level, presence of children in household, religiosity, and disability.
p < 0.05.
p < 0.01.
Table 5.
Regression models of happiness before and during COVID-19.
| Variables |
Happiness |
|||||
|---|---|---|---|---|---|---|
| Before COVID-19 |
During COVID-19 |
Change (Before − During COVID-19) |
||||
| 1 |
2 |
1 |
2 |
1 |
2 |
|
| Built environment | β (B, SE) |
β (B, SE) |
β (B, SE) |
β (B, SE) |
β (B, SE) |
β (B, SE) |
| Distance to city center | 0.022 (0.0006, 0.0008) |
0.020 (0.0006, 0.0008) |
0.021 (0.0007, 0.0009) |
0.006 (0.0002, 0.0010) |
−0.002 (−0.0001, 0.0008) |
0.013 (0.0004, 0.0008) |
| Neighborhood density | −0.003 (−0.0000, 0.0004) |
−0.082 (−0.0012, 0.0008) |
−0.077⁎⁎ (−0.0013, 0.0005) |
−0.177⁎⁎ (−0.0031, 0.0010) |
0.089⁎⁎ (0.0013, 0.0004) |
0.128⁎ (0.0019, 0.0008) |
| Public transport | −0.060 (−0.0010, 0.0008) |
−0.074 (−0.0015, 0.0009) |
0.028 (0.0005, 0.0008) |
|||
| Local facilities | 0.121⁎ (0.0003, 0.0001) |
0.154⁎⁎ (0.0004, 0.0002) |
−0.060 (−0.0001, 0.0001) |
|||
| Green space | 0.016 (0.0008, 0.0017) |
0.002 (0.0001, 0.0021) |
0.014 (0.0007, 0.0018) |
|||
| Apartment | 0.078⁎ (0.1176, 0.0522) |
0.075⁎ (0.1336, 0.0616) |
−0.011 (−0.0160, 0.0529) |
|||
| Dwelling size | 0.032 (0.0004, 0.0004) |
0.074⁎ (0.0009, 0.0004) |
−0.056 (−0.0006, 0.0004) |
|||
| Summary statistics | ||||||
| N | 1796 | 1760 | 1796 | 1760 | 1796 | 1760 |
| Adjusted R-squared | 0.078 | 0.078 | 0.067 | 0.069 | 0.021 | 0.020 |
Notes: Coefficients shown out of the parenthesis are standardized beta coefficients. The parenthesis includes the unstandardized coefficient and the standard error of the estimate. The models include individual sociodemographic variables as covariates (coefficients not shown here to reduce complexity): age, age squared, gender, unemployment, cohabitation status, citizenship, income, education level, presence of children in household, religiosity, and disability.
p < 0.05.
p < 0.01.
Table 6.
Regression models of anxiety before and during COVID-19.
| Variables |
Anxiety |
|||||
|---|---|---|---|---|---|---|
| Before COVID-19 |
During COVID-19 |
Change (During – Before COVID-19) |
||||
| 1 |
2 |
1 |
2 |
1 |
2 |
|
| Built environment | β (B, SE) |
β (B, SE) |
β (B, SE) |
β (B, SE) |
β (B, SE) |
β (B, SE) |
| Distance to city center | −0.005 (−0.0002, 0.0009) |
−0.005 (−0.0002, 0.0010) |
0.020 (0.0008, 0.0011) |
0.041 (0.0016, 0.0012) |
0.028 (0.0009, 0.0010) |
0.053 (0.0018, 0.0010) |
| Neighborhood density | 0.028 (0.0005, 0.0005) |
0.016 (0.0003, 0.0010) |
0.037 (0.0008, 0.0006) |
0.060 (0.0013, 0.0012) |
0.015 (0.0003, 0.0005) |
0.054 (0.0010, 0.0010) |
| Public transport | 0.047 (0.0010, 0.0009) |
0.123⁎⁎ (0.0030, 0.0011) |
0.097⁎ (0.0020, 0.0010) |
|||
| Local facilities | 0.012 (0.0000, 0.0002) |
−0.077 (−0.0003, 0.0002) |
−0.102 (−0.0003, 0.0002) |
|||
| Green space | 0.023 (0.0015, 0.0021) |
0.055 (0.0041, 0.0024) |
0.041 (0.0026, 0.0022) |
|||
| Apartment | −0.036 (−0.0661, 0.0628) |
−0.012 (−0.0253, 0.0727) |
0.022 (0.0408, 0.0649) |
|||
| Dwelling size | −0.028 (−0.0004, 0.0004) |
−0.019 (−0.0003, 0.0005) |
0.007 (0.0001, 0.0005) |
|||
| Summary statistics | ||||||
| N | 1796 | 1760 | 1796 | 1760 | 1796 | 1760 |
| Adjusted R-squared | 0.111 | 0.108 | 0.094 | 0.094 | 0.012 | 0.011 |
Notes: Coefficients shown out of the parenthesis are standardized beta coefficients. The parenthesis includes the unstandardized coefficient and the standard error of the estimate. The models include individual sociodemographic variables as covariates (coefficients not shown here to reduce complexity): age, gender, unemployment, cohabitation status, citizenship, income, education level, presence of children in household, religiosity, and disability.
p < 0.05.
p < 0.01.
Table 1 presents regression models on life satisfaction. Results show that neighborhood density is negatively associated with life satisfaction during COVID-19. It is also observed that neighborhood density is associated with a larger change (decrease) in life satisfaction before-during COVID-19. These results indicate that residents of denser neighborhoods experienced a larger decline in life satisfaction during the pandemic. Dwelling size is positively associated with life satisfaction during COVID-19 and is associated with a smaller change (decrease) in life satisfaction before-during COVID-19. These results indicate that residents living in smaller dwellings experienced a larger decline in life satisfaction during the pandemic. Green space is found to be negatively associated with life satisfaction before COVID-19.
Table 2 presents regression models on personal relationships satisfaction. The main finding from this analysis is that local facilities are associated with higher personal relationships satisfaction during COVID-19 and are also associated with a smaller change (decrease) in personal relationships satisfaction before-during COVID-19. These results indicate that residents living in proximity to many local facilities experienced a smaller decline in personal relationships satisfaction during the pandemic.
Table 3 displays regression models on leisure satisfaction. Results indicate a negative association between neighborhood density and leisure satisfaction during COVID-19. Neighborhood density is also associated with a larger change (decrease) in leisure satisfaction before-during COVID-19. These results indicate that residents living in denser neighborhoods experienced a larger decline in leisure satisfaction during the pandemic. Green space is associated with a smaller change (decrease) in leisure satisfaction before-during COVID-19, indicating that residents with access to more green space experienced a smaller decline in leisure satisfaction during the pandemic.
Table 4 displays regression models on general health. The most significant and substantial finding is that local facilities are associated with a smaller change (decrease) in general health before-during COVID-19. This finding indicates that those living in proximity to numerous local facilities experienced a smaller decline in general health during the pandemic. On the other hand, public transport is associated with a larger change (decrease) in general health before-during COVID-19, indicating that residents living in transit-oriented neighborhoods experienced a larger decline in general health during the pandemic.
Table 5 presents regression models on happiness. Neighborhood density is found to be negatively associated with happiness, while it is also associated with a larger change (decrease) in happiness before-during COVID-19. These results indicate that residents of denser neighborhoods experienced a larger decline in happiness during the pandemic. Local facilities are positively associated with happiness both before COVID-19 and during COVID-19. Living in an apartment is positively associated with happiness both before COVID-19 and during COVID-19. A larger dwelling size is associated with higher happiness during COVID-19.
Table 6 presents regression models on anxiety. The main finding is that higher public transport accessibility is associated with higher anxiety during COVID-19. Public transport accessibility is also associated with a larger change (increase) in anxiety before-during COVID-19. These results indicate that residents of transit-oriented neighborhoods experienced a more substantial increase in anxiety during the pandemic.
5. Discussion and conclusions
5.1. Discussion of results
The analysis addressing the first research question of the paper compared health and well-being before versus during COVID-19 (Section 4.1). Findings suggest that health and well-being worsened during COVID-19 compared to the before COVID-19 period. The worsening of health and well-being due to COVID-19 is in line with previous findings from other contexts (Li et al., 2020; Moreno et al., 2020; Mouratidis and Yiannakou, 2021; Patrick et al., 2020; White and Van Der Boor, 2020). Factors that have contributed to the decline of health and well-being due to COVID-19 could have been the COVID-19 health-related risks, quarantine, social distancing, isolation at home, travel restrictions, loss of economic activity, unemployment, and closing of or lack of access to various types of facilities. The decline in health and well-being due to COVID-19 was also analyzed for its relationship with individual characteristics (Section 4.1). The most notable findings were that health and well-being before-during COVID-19 worsened considerably more for females, for individuals who do not have higher education, and for individuals who live alone.
The second research question of the paper was examined with regression models on how the compact city and its characteristics relate to health and well-being outcomes before and during COVID-19 (Section 4.2). The study extends previous research on city planning and COVID-19 (e.g. Connolly et al., 2020; Hamidi et al., 2020; Mouratidis, 2021a; Sharifi and Khavarian-Garmsir, 2020). It is among the first to combine survey data with GIS data on the built environment in order to shed light on the role of the compact city and its characteristics in health and well-being changes due to COVID-19. Results suggest that, overall, residents of compact neighborhoods experienced lower well-being during COVID-19 compared to residents of low-density neighborhoods. Several compact city characteristics – higher neighborhood density, transit-oriented neighborhoods, smaller dwellings, and less green space – were associated with negative well-being and health outcomes during COVID-19. On the other hand, results indicate that another characteristic of the compact city, the presence of numerous local facilities, was associated with positive well-being and health outcomes during COVID-19.
Higher neighborhood density was found to be associated with lower life satisfaction, lower happiness, and lower leisure satisfaction during COVID-19. Residents of denser neighborhoods typically live in smaller dwellings, rely more on public transport, have lower access to green space, and have access to a greater number of local facilities (see correlation analyses in Table A4, Appendix A). Since smaller dwellings, public transport reliance, and lack of access to green space seem to have negative implications for health and well-being during COVID-19, neighborhood density may contribute, overall, to negative health and well-being outcomes during COVID-19. The seemingly positive implications of local facilities for health and well-being found in the study do not completely counterbalance the possible negative implications of smaller dwellings, public transport reliance, and less green space. Moreover, it was difficult for residents of denser neighborhoods to avoid urban stressors during the pandemic, which might have additionally contributed to lower well-being. Travel restrictions, lockdowns, and quarantines made it difficult to visit nature and rural areas or travel abroad for leisure (Gössling et al., 2021). The finding of denser neighborhoods being associated with lower well-being during COVID-19 is in line with earlier evidence from a study in Greek cities (Mouratidis and Yiannakou, 2021).
Public transport accessibility was found to be associated with a larger increase in anxiety and with a larger decline in general health before-during COVID-19. Public transport exposed passengers to a high risk of infection during the pandemic and therefore its use greatly declined compared to other transport modes (Bucsky, 2020; Hadjidemetriou et al., 2020; Jenelius and Cebecauer, 2020; Teixeira and Lopes, 2020). However, some residents living in transit-oriented neighborhoods who had to travel during COVID-19 did not have the option to use travel modes other than public transport. These residents might have been infected to a larger extent but might have also experienced stress from the fear of infection during travel by public transport. The high risk of infection associated with public transport is also likely to have decreased the mobility of residents of compact, transit-oriented neighborhoods, compared to residents of low-density neighborhoods who could have used their private car to access destinations and participate in activities. All these considerations may explain the negative association between public transport and health and well-being outcomes.
Living in a smaller dwelling was associated with lower life satisfaction and lower happiness during COVID-19. The importance of the dwelling dramatically increased during COVID-19 since residents had to spend more time and perform more, if not most, of their activities at home. Numerous teleactivities replaced out-of-home activities during COVID-19 (de Haas et al., 2020; Pierce et al., 2021; Shamshiripour et al., 2020; Wijesooriya et al., 2020). For that purpose, larger dwellings were likely to be more pleasant, less stressful, and more functional, since they were more likely to allow members of the same household to perform different activities at home. This finding is in line with the link between poor housing and increased risk of depression during COVID-19 found by Amerio et al. (2020) and with the link between smaller dwellings and increased anxiety found by Mouratidis and Yiannakou (2021).
Living in an apartment (versus living in a detached/semi-detached house or row house) was not adversely linked to health and well-being during COVID-19, when dwelling size and the amount of green space were included in the statistical models. On the contrary, living in an apartment was associated with greater happiness before and during COVID-19. These findings may suggest that it was the size of the dwelling and the surrounding green space that mattered for health and well-being during COVID-19, and not the type of dwelling per se. However, since apartments tend to be generally smaller and to lack outdoor green space, residents living in apartments likely experienced more negative health and well-being impacts during the pandemic.
Access to numerous local facilities was associated with higher happiness and higher personal relationships satisfaction during COVID-19. A higher number of local facilities was also associated with a smaller decrease in general health before-during COVID-19. The presence of numerous facilities within walkable distance is likely to have allowed residents to participate in certain activities by using facilities that remained open during COVID-19. In Norway, several facilities were open during the COVID-19 period. In areas with many facilities, it is possible that the sheer number and variety of existing facilities made it more likely that at least some facilities were open and accessible, while in other areas with fewer facilities almost everything was shut down besides grocery stores. The presence of numerous local facilities might have also reduced the risk of infection and the fear of infection associated with using public transport to access facilities that are not within walkable distance. Good access to high-quality healthcare facilities could have also provided health-related benefits and might be linked to lower mortality from COVID-19 as suggested by Hamidi et al. (2020).
Green space was found to have some possibly positive well-being implications as it was associated with a smaller reduction in leisure satisfaction before-during COVID-19. In other words, the leisure satisfaction of residents of areas with more green space in close proximity decreased to a smaller extent during the pandemic than the leisure satisfaction of residents of areas with less green space in close proximity. This finding suggests that access to green space was important for performing leisure activities during COVID-19. This is in line with earlier studies on COVID-19 and green space (e.g. Ugolini et al., 2020; Venter et al., 2020; Xie et al., 2020). Although the present study does not include specific data on private versus public green space, the analysis included a variable on dwelling type: apartment versus detached house or duplex. Detached houses and duplexes in Oslo and Viken typically have private gardens while apartments do not. Detached houses or duplexes were not found to be associated with more positive health and well-being outcomes during COVID-19 in the present study. However, it might be the gardening activity that contributes to positive well-being outcomes during COVID-19 (Corley et al., 2021), and not just the presence of a private green space itself.
5.2. COVID-19, sustainable urban planning, and compact cities
Findings from this study challenge the compact city as a model for sustainable urban planning and policy, providing insights for reflection and improvement during COVID-19 but also post-COVID-19. The compact city provides multiple societal and environmental (e.g. for urban sustainability and climate change mitigation and adaptation) benefits (Ahlfeldt et al., 2018; Tonne et al., 2021), and, therefore, it is important that societies and policymakers do not lose interest in compact city policies. Measures need to be taken so that events such as the COVID-19 pandemic will not lead to further sprawl, suburbanization, and an abandonment of compact city policies.
Some possible implications for the compact city and sustainable urban planning and policy are presented here. Public transport accessibility – one of the strengths of the compact city – was found to be negatively linked to some health and well-being outcomes during COVID-19, possibly due to increased risk of infection and related stress. To mitigate this issue, public transport departures need to be frequent enough to guarantee safe social distancing during pandemic crises. In addition, alternative transport options need to be available in compact, transit-oriented neighborhoods, especially during pandemic events. Such options may include active travel modes as well as affordable and accessible carsharing in case residents need to travel longer distances. All these may provide safer alternatives in terms of virus transmission. Results from this study also suggest that dwelling size mattered for well-being during COVID-19, as living in a smaller dwelling – often characterizing compact city living – was associated with lower life satisfaction and lower happiness during COVID-19. As teleactivities are expected to be increasingly adopted in the post-COVID-19 period, and several of them may take place at home, a minimum dwelling size might need to be established in compact cities in order to avoid negative impacts on health and well-being from overcrowded or tight dwellings. This would be particularly important for families with children as well as poorer households that are more likely to live in smaller, overcrowded dwellings. Another alternative is the development of multifunctional shared spaces where local residents can perform a variety of activities and teleactivities. Such spaces would need to be appropriately designed if they are to be used during pandemic events. Access to green space was found to be possibly important for leisure activities during COVID-19, as larger green space was associated with a smaller reduction in leisure satisfaction before-during COVID-19. Using green spaces for several purposes, including social and physical activities and connecting with nature, is particularly important during pandemics, and especially in more urban, compact areas (Douglas et al., 2020; Hamidi and Zandiatashbar, 2021; Shoari et al., 2020; Xie et al., 2020). The importance of easy access to numerous local facilities (enabled by compact cities) during COVID-19 was also illustrated by the study's findings, as it was associated with higher happiness and personal relationships satisfaction during COVID-19. Proximity to a wide range of facilities is key during pandemic crises (Litman, 2020a) as it allows participation in activities and access to healthcare provision. Finally, outcomes from this study suggest that the worsening of health and well-being due to COVID-19 was more severe for certain groups of people such as females and individuals who live alone. Urban policies, but also country-level policies, should provide greater support for these groups of people during and post-COVID-19. Relevant measures could aim at reducing transport-related gender inequalities (e.g. Uteng et al., 2020) and improving social cohesion at a local community level to reduce loneliness and social isolation (e.g. Anderson et al., 2017).
5.3. Limitations and future research
This study has some limitations that should be taken into consideration when interpreting the results. The overview of changes in health and well-being due to COVID-19 concerns the context of Oslo and Viken, in Norway. Studies could explore these changes in other contexts with different social, cultural, and spatial characteristics. The study employed retrospective data measuring respondents' evaluations of health and well-being before and during COVID-19. Due to the retrospective nature of the data, individual recall of health and well-being evaluations may be imprecise and subject to biases. It is also possible that the survey's timing itself, in the middle of the pandemic and therefore in an extraordinary situation, might have created bias. Future research could additionally investigate possible links between these health and well-being variables with more complex statistical approaches such as structural equation modeling. Results from the present analysis on compact city characteristics and health/well-being should be interpreted with caution since they indicate associations but not necessarily causal relationships. Qualitative research findings could be particularly useful for shedding more light on the complex pathways behind the relationships examined in this paper. Prospective longitudinal designs would also help identify possible causal relationships.
CRediT authorship contribution statement
Kostas Mouratidis: Conceptualization, Methodology, Investigation, Formal analysis, Visualization, Writing – original draft, Writing – review & editing, Funding acquisition, Project administration.
Declaration of competing interest
The author declares that he has no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The study is part of the research project “App Cities: New urban technologies, daily travel, and quality of life” (project number: 1850051060), funded by the Norwegian University of Life Sciences. Additional support for the data collection of the project was provided by Viken County Municipality (Viken Fylkeskommune) and the Norwegian Public Roads Administration (Statens Vegvesen). I am grateful to Sebastian Peters for valuable feedback on an earlier draft of the paper and for the collaboration throughout this research project. I would also like to thank the three anonymous reviewers for their insightful comments and suggestions.
Editor: Jay Gan
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.scitotenv.2021.152332.
Appendices. Supplementary data
Appendices
References
- Ahlfeldt G., Pietrostefani E., Schumann A., Matsumoto T. Demystifying compact urban growth: evidence from 300 studies from across the world. 2018. Retrieved from. [DOI]
- Ahmad K., Erqou S., Shah N., Nazir U., Morrison A.R., Choudhary G., Wu W.-C. Association of poor housing conditions with COVID-19 incidence and mortality across US counties. PLoS ONE. 2020;15(11) doi: 10.1371/journal.pone.0241327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ala-Mantila S., Heinonen J., Junnila S., Saarsalmi P. Spatial nature of urban well-being. Reg. Stud. 2018;52(7):959–973. doi: 10.1080/00343404.2017.1360485. [DOI] [Google Scholar]
- Amerio A., Brambilla A., Morganti A., Aguglia A., Bianchi D., Santi F., Capolongo S. COVID-19 lockdown: housing built environment’s effects on mental health. Int. J. Environ. Res. Public Health. 2020;17(16) doi: 10.3390/ijerph17165973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson J., Ruggeri K., Steemers K., Huppert F. Lively social space, well-being activity, and urban design: findings from a low-cost community-led public space intervention. Environ. Behav. 2017;49(6):685–716. doi: 10.1177/0013916516659108. [DOI] [Google Scholar]
- Barak N., Sommer U., Mualam N. Urban attributes and the spread of COVID-19: the effects of density, compliance and socio-political factors in Israel. Sci. Total Environ. 2021;793 doi: 10.1016/j.scitotenv.2021.148626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bibri S.E., Krogstie J., Kärrholm M. Compact city planning and development: emerging practices and strategies for achieving the goals of sustainability. Dev. Built Environ. 2020;4 doi: 10.1016/j.dibe.2020.100021. [DOI] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucsky P. Modal share changes due to COVID-19: the case of Budapest. Transp. Res. Interdiscip. Perspect. 2020;8 doi: 10.1016/j.trip.2020.100141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao X. How does neighborhood design affect life satisfaction? Evidence from twin cities. Travel Behav. Soc. 2016;5:68–76. doi: 10.1016/j.tbs.2015.07.001. [DOI] [Google Scholar]
- Connolly C., Keil R., Ali S.H. Extended urbanisation and the spatialities of infectious disease: demographic change, infrastructure and governance. Urban Stud. 2020 doi: 10.1177/0042098020910873. 0042098020910873. [DOI] [Google Scholar]
- Corley J., Okely J.A., Taylor A.M., Page D., Welstead M., Skarabela B., Russ T.C. Home garden use during COVID-19: associations with physical and mental wellbeing in older adults. J. Environ. Psychol. 2021;73 doi: 10.1016/j.jenvp.2020.101545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cosby A.G., McDoom-Echebiri M.M., James W., Khandekar H., Brown W., Hanna H.L. Growth and persistence of place-based mortality in the United States: the rural mortality penalty. Am. J. Public Health. 2019;109(1):155–162. doi: 10.2105/AJPH.2018.304787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Haas M., Faber R., Hamersma M. How COVID-19 and the dutch ‘intelligent lockdown’ change activities, work and travel behaviour: evidence from longitudinal data in the Netherlands. Transp. Res. Interdiscip. Perspect. 2020;6 doi: 10.1016/j.trip.2020.100150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douglas M., Katikireddi S.V., Taulbut M., McKee M., McCartney G. Mitigating the wider health effects of covid-19 pandemic response. BMJ. 2020;369 doi: 10.1136/bmj.m1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dye C. Health and urban living. Science. 2008;319(5864):766. doi: 10.1126/science.1150198. [DOI] [PubMed] [Google Scholar]
- Ettema D., Schekkerman M. How do spatial characteristics influence well-being and mental health? Comparing the effect of objective and subjective characteristics at different spatial scales. Travel Behav. Soc. 2016;5(Supplement C):56–67. doi: 10.1016/j.tbs.2015.11.001. [DOI] [Google Scholar]
- European Social Survey . Centre for Comparative Social Surveys, City University London; London: 2012. ESS Round 6 Source Questionnaire. [Google Scholar]
- Fiorillo A., Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur. Psychiatry. 2020;63(1) doi: 10.1192/j.eurpsy.2020.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Florida R., Rodríguez-Pose A., Storper M. Cities in a post-COVID world. Urban Stud. 2021 doi: 10.1177/00420980211018072. 00420980211018072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- French S., Wood L., Foster S.A., Giles-Corti B., Frank L., Learnihan V. Sense of community and its association with the neighborhood built environment. Environ. Behav. 2014;46(6):677–697. doi: 10.1177/0013916512469098. [DOI] [Google Scholar]
- Glaeser E. Penguin Books; New York: 2011. Triumph of the City: How Our Greatest Invention Makes Us Richer, Smarter, Greener, Healthier, and Happier. [Google Scholar]
- Gruebner O., Rapp M.A., Adli M., Kluge U., Galea S., Heinz A. Cities and mental health. Dtsch. Arztebl. Int. 2017;114(8):121–127. doi: 10.3238/arztebl.2017.0121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gössling S., Scott D., Hall C.M. Pandemics, tourism and global change: a rapid assessment of COVID-19. J. Sustain. Tour. 2021;29(1):1–20. doi: 10.1080/09669582.2020.1758708. [DOI] [Google Scholar]
- Hadjidemetriou G.M., Sasidharan M., Kouyialis G., Parlikad A.K. The impact of government measures and human mobility trend on COVID-19 related deaths in the UK. Transp. Res. Interdiscip. Perspect. 2020;6 doi: 10.1016/j.trip.2020.100167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamidi S., Ewing R., Tatalovich Z., Grace J.B., Berrigan D. Associations between urban sprawl and life expectancy in the United States. Int. J. Environ. Res. Public Health. 2018;15(5):861. doi: 10.3390/ijerph15050861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamidi S., Sabouri S., Ewing R. Does density aggravate the COVID-19 pandemic? J. Am. Plan. Assoc. 2020;86(4):495–509. doi: 10.1080/01944363.2020.1777891. [DOI] [Google Scholar]
- Hamidi S., Zandiatashbar A. Compact development and adherence to stay-at-home order during the COVID-19 pandemic: a longitudinal investigation in the United States. Landsc. Urban Plan. 2021;205 doi: 10.1016/j.landurbplan.2020.103952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen M.C., Potapov P.V., Moore R., Hancher M., Turubanova S.A., Tyukavina A., Townshend J.R.G. High-resolution global maps of 21st-century forest cover change. Science. 2013;342(6160):850–853. doi: 10.1126/science.1244693. [DOI] [PubMed] [Google Scholar]
- Honey-Rosés J., Anguelovski I., Chireh V.K., Daher C., Konijnendijk van den Bosch C., Litt J.S., Nieuwenhuijsen M.J. The impact of COVID-19 on public space: an early review of the emerging questions – design, perceptions and inequities. Cities Health. 2020;1–17 doi: 10.1080/23748834.2020.1780074. [DOI] [Google Scholar]
- Howley P., Scott M., Redmond D. Sustainability versus liveability: an investigation of neighbourhood satisfaction. J. Environ. Plan. Manag. 2009;52(6):847–864. doi: 10.1080/09640560903083798. [DOI] [Google Scholar]
- Hu M., Roberts J.D., Azevedo G.P., Milner D. The role of built and social environmental factors in Covid-19 transmission: a look at America’s capital city. Sustain. Cities Soc. 2021;65 doi: 10.1016/j.scs.2020.102580. [DOI] [Google Scholar]
- Hu S., Chen P. Who left riding transit? Examining socioeconomic disparities in the impact of COVID-19 on ridership. Transp. Res. Part D: Transp. Environ. 2021;90 doi: 10.1016/j.trd.2020.102654. [DOI] [Google Scholar]
- Ihlebæk C., Næss P., Stefansdottir H. Are compact cities a threat to public health? Eur. Plan. Stud. 2021;29(6):1021–1049. doi: 10.1080/09654313.2020.1775790. [DOI] [Google Scholar]
- Jenelius E., Cebecauer M. Impacts of COVID-19 on public transport ridership in Sweden: analysis of ticket validations, sales and passenger counts. Transp. Res. Interdiscip. Perspect. 2020;8 doi: 10.1016/j.trip.2020.100242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kyttä M., Broberg A., Haybatollahi M., Schmidt-Thomé K. Urban happiness: context-sensitive study of the social sustainability of urban settings. Environ. Plann. B. Plann. Des. 2016;43(1):34–57. [Google Scholar]
- Li J., Yang Z., Qiu H., Wang Y., Jian L., Ji J., Li K. Anxiety and depression among general population in China at the peak of the COVID-19 epidemic. World Psychiatry. 2020;19(2):249–250. doi: 10.1002/wps.20758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieberman-Cribbin W., Tuminello S., Flores R.M., Taioli E. Disparities in COVID-19 testing and positivity in New York City. Am. J. Prev. Med. 2020;59(3):326–332. doi: 10.1016/j.amepre.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litman T. Pandemic-resilient community planning. 2020. https://www.vtpi.org/PRCP.pdf Retrieved from Victoria, Canada:
- Litman T. Urban sanity: understanding urban mental health impacts and how to create saner, happier cities. 2020. https://www.vtpi.org/urban-sanity.pdf Retrieved from Victoria, Canada:
- Markevych I., Schoierer J., Hartig T., Chudnovsky A., Hystad P., Dzhambov A.M., Fuertes E. Exploring pathways linking greenspace to health: theoretical and methodological guidance. Environ. Res. 2017;158:301–317. doi: 10.1016/j.envres.2017.06.028. [DOI] [PubMed] [Google Scholar]
- McFarlane C. Repopulating density: COVID-19 and the politics of urban value. Urban Stud. 2021 doi: 10.1177/00420980211014810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melis G., Gelormino E., Marra G., Ferracin E., Costa G. The effects of the urban built environment on mental health: a cohort study in a large northern Italian City. Int. J. Environ. Res. Public Health. 2015;12(11):14898–14915. doi: 10.3390/ijerph121114898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer W.B. MIT Press; Cambridge, MA: 2013. The Environmental Advantages of Cities: Countering Commonsense Antiurbanism. [Google Scholar]
- Mondal S., Chaipitakporn C., Kumar V., Wangler B., Gurajala S., Dhaniyala S., Sur S. COVID-19 in New York state: effects of demographics and air quality on infection and fatality. Sci. Total Environ. 2022;807 doi: 10.1016/j.scitotenv.2021.150536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreno C., Wykes T., Galderisi S., Nordentoft M., Crossley N., Jones N., Arango C. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. 2020;7(9):813–824. doi: 10.1016/S2215-0366(20)30307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mouratidis K. Built environment and social well-being: how does urban form affect social life and personal relationships? Cities. 2018;74:7–20. doi: 10.1016/j.cities.2017.10.020. [DOI] [Google Scholar]
- Mouratidis K. Is compact city livable? The impact of compact versus sprawled neighbourhoods on neighbourhood satisfaction. Urban Stud. 2018;55(11):2408–2430. doi: 10.1177/0042098017729109. [DOI] [Google Scholar]
- Mouratidis K. Built environment and leisure satisfaction: the role of commute time, social interaction, and active travel. J. Transp. Geogr. 2019;80 doi: 10.1016/j.jtrangeo.2019.102491. [DOI] [Google Scholar]
- Mouratidis K. Compact city, urban sprawl, and subjective well-being. Cities. 2019;92:261–272. doi: 10.1016/j.cities.2019.04.013. [DOI] [Google Scholar]
- Mouratidis K. How COVID-19 reshaped quality of life in cities: a synthesis and implications for urban planning. Land Use Policy. 2021;111 doi: 10.1016/j.landusepol.2021.105772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mouratidis K. Urban planning and quality of life: a review of pathways linking the built environment to subjective well-being. Cities. 2021;115 doi: 10.1016/j.cities.2021.103229. [DOI] [Google Scholar]
- Mouratidis K., Ettema D., Næss P. Urban form, travel behavior, and travel satisfaction. Transp. Res. A Policy Pract. 2019;129:306–320. doi: 10.1016/j.tra.2019.09.002. [DOI] [Google Scholar]
- Mouratidis K., Papagiannakis A. COVID-19, internet, and mobility: the rise of telework, telehealth, e-learning, and e-shopping. Sustain. Cities Soc. 2021;74 doi: 10.1016/j.scs.2021.103182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mouratidis K., Poortinga W. Built environment, urban vitality and social cohesion: do vibrant neighborhoods foster strong communities? Landsc. Urban Plan. 2020;204 doi: 10.1016/j.landurbplan.2020.103951. [DOI] [Google Scholar]
- Mouratidis K., Yiannakou A. COVID-19 and urban planning: built environment, health, and well-being in greek cities before and during the pandemic. Cities. 2021;103491 doi: 10.1016/j.cities.2021.103491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Næss P. 2019. Meta-Analyses of Built Environment Effects on Travel: No New Platinum Standard. [DOI] [Google Scholar]
- OECD . OECD Better Life Initiative; Washington, DC: 2013. OECD Guidelines on Measuring Subjective Well-Being. [PubMed] [Google Scholar]
- OECD Governance: compact cities: the way of the future. 2018. http://www.oecd.org/newsroom/governancecompactcitiesthewayofthefuture.htm
- Patrick S.W., Henkhaus L.E., Zickafoose J.S., Lovell K., Halvorson A., Loch S., Davis M.M. Well-being of parents and children during the COVID-19 pandemic: a National Survey. Pediatrics. 2020;146(4) doi: 10.1542/peds.2020-016824. [DOI] [PubMed] [Google Scholar]
- Peto J. Covid-19 mass testing facilities could end the epidemic rapidly. BMJ. 2020;368 doi: 10.1136/bmj.m1163. [DOI] [PubMed] [Google Scholar]
- Pierce B.S., Perrin P.B., Tyler C.M., McKee G.B., Watson J.D. The COVID-19 telepsychology revolution: a national study of pandemic-based changes in U.S. Mental health care delivery. Am. Psychol. 2021;76(1):14–25. doi: 10.1037/amp0000722. [DOI] [PubMed] [Google Scholar]
- Politis I., Georgiadis G., Papadopoulos E., Fyrogenis I., Nikolaidou A., Kopsacheilis A., Verani E. COVID-19 lockdown measures and travel behavior: the case of Thessaloniki, Greece. Transp. Res. Interdiscip. Perspect. 2021;10 doi: 10.1016/j.trip.2021.100345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poortinga W., Bird N., Hallingberg B., Phillips R., Williams D. The role of perceived public and private green space in subjective health and wellbeing during and after the first peak of the COVID-19 outbreak. Landsc. Urban Plan. 2021;211 doi: 10.1016/j.landurbplan.2021.104092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pouso S., Borja Á., Fleming L.E., Gómez-Baggethun E., White M.P., Uyarra M.C. Contact with blue-green spaces during the COVID-19 pandemic lockdown beneficial for mental health. Sci. Total Environ. 2021;756 doi: 10.1016/j.scitotenv.2020.143984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saelens B.E., Handy S.L. Built environment correlates of walking: a review. Med. Sci. Sports Exerc. 2008;40(7 Suppl):S550. doi: 10.1249/MSS.0b013e31817c67a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkodie S.A., Owusu P.A. Global effect of city-to-city air pollution, health conditions, climatic & socio-economic factors on COVID-19 pandemic. Sci. Total Environ. 2021;778 doi: 10.1016/j.scitotenv.2021.146394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shakibaei S., de Jong G.C., Alpkökin P., Rashidi T.H. Impact of the COVID-19 pandemic on travel behavior in Istanbul: a panel data analysis. Sustain. Cities Soc. 2021;65 doi: 10.1016/j.scs.2020.102619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shamshiripour A., Rahimi E., Shabanpour R., Mohammadian A. How is COVID-19 reshaping activity-travel behavior? Evidence from a comprehensive survey in Chicago. Transp. Res. Interdiscip. Perspect. 2020;7 doi: 10.1016/j.trip.2020.100216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharifi A. Urban form resilience: a meso-scale analysis. Cities. 2019;93:238–252. doi: 10.1016/j.cities.2019.05.010. [DOI] [Google Scholar]
- Sharifi A., Khavarian-Garmsir A.R. The COVID-19 pandemic: impacts on cities and major lessons for urban planning, design, and management. Sci. Total Environ. 2020;749 doi: 10.1016/j.scitotenv.2020.142391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shoari N., Ezzati M., Baumgartner J., Malacarne D., Fecht D. Accessibility and allocation of public parks and gardens in England and Wales: a COVID-19 social distancing perspective. PLOS ONE. 2020;15(10) doi: 10.1371/journal.pone.0241102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slater S.J., Christiana R.W., Gustat J. Recommendations for keeping parks and green space accessible for mental and physical health during COVID-19 and other pandemics. Prev. Chronic Dis. 2020;17:E59. doi: 10.5888/pcd17.200204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevenson M., Thompson J., de Sá T.H., Ewing R., Mohan D., McClure R., Woodcock J. Land use, transport, and population health: estimating the health benefits of compact cities. Lancet. 2016;388(10062):2925–2935. doi: 10.1016/S0140-6736(16)30067-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun C., Zhai Z. The efficacy of social distance and ventilation effectiveness in preventing COVID-19 transmission. Sustain. Cities Soc. 2020;62 doi: 10.1016/j.scs.2020.102390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tao Y., Zhang Z., Ou W., Guo J., Pueppke S.G. How does urban form influence PM2.5 concentrations: insights from 350 different-sized cities in the rapidly urbanizing Yangtze River Delta region of China, 1998–2015. Cities. 2020;98 doi: 10.1016/j.cities.2019.102581. [DOI] [Google Scholar]
- Teixeira J.F., Lopes M. The link between bike sharing and subway use during the COVID-19 pandemic: the case-study of New York's citi bike. Transp. Res. Interdiscip. Perspect. 2020;6 doi: 10.1016/j.trip.2020.100166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinson A., Clair A. Better Housing is Crucial for Our Health and the COVID-19 Recovery. The Health Foundation; 2020. pp. 1–25. [Google Scholar]
- Tonne C., Adair L., Adlakha D., Anguelovski I., Belesova K., Berger M., Adli M. Defining pathways to healthy sustainable urban development. Environ. Int. 2021;146 doi: 10.1016/j.envint.2020.106236. [DOI] [PubMed] [Google Scholar]
- Trasberg T., Cheshire J. Spatial and social disparities in the decline of activities during the COVID-19 lockdown in greater London. Urban Stud. 2021 doi: 10.1177/00420980211040409. doi:10.1177/00420980211040409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ugolini F., Massetti L., Calaza-Martínez P., Cariñanos P., Dobbs C., Ostoić S.K., Sanesi G. Effects of the COVID-19 pandemic on the use and perceptions of urban green space: an international exploratory study. Urban For. Urban Green. 2020;56 doi: 10.1016/j.ufug.2020.126888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uteng T.P., Christensen H.R., Levin L. Routledge; London: 2020. Gendering Smart Mobilities. [Google Scholar]
- Venter Z.S., Barton D.N., Gundersen V., Figari H., Nowell M. Urban nature in a time of crisis: recreational use of green space increases during the COVID-19 outbreak in Oslo, Norway. Environ. Res. Lett. 2020;15(10) doi: 10.1088/1748-9326/abb396. [DOI] [Google Scholar]
- Wang F., Wang D. Mobility, Sociability and Well-being of Urban Living. Springer; Berlin: 2016. Place, geographical context and subjective well-being: state of art and future directions; pp. 189–230. [Google Scholar]
- White R.G., Van Der Boor C. Impact of the COVID-19 pandemic and initial period of lockdown on the mental health and well-being of adults in the UK. BJPsych. Open. 2020;6(5) doi: 10.1192/bjo.2020.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wijesooriya N.R., Mishra V., Brand P.L.P., Rubin B.K. COVID-19 and telehealth, education, and research adaptations. Paediatr. Respir. Rev. 2020;35:38–42. doi: 10.1016/j.prrv.2020.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie J., Luo S., Furuya K., Sun D. Urban parks as green buffers during the COVID-19 pandemic. Sustainability. 2020;12(17):6751. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendices