Abstract
Objective
Primary biliary cholangitis (PBC) is a progressive, autoimmune, cholestatic liver disease affecting approximately 15 000 individuals in the UK. Updated guidelines for the management of PBC were published by The European Association for the Study of the Liver (EASL) in 2017. We report on the first national, pilot audit that assesses the quality of care and adherence to guidelines.
Design
Data were collected from 11 National Health Service hospitals in England, Wales and Scotland between 2017 and 2020. Data on patient demographics, ursodeoxycholic acid (UDCA) dosing and key guideline recommendations were captured from medical records. Results from each hospital were evaluated for target achievement and underwent χ2 analysis for variation in performance between trusts.
Results
790 patients’ medical records were reviewed. The data demonstrated that the majority of hospitals did not meet all of the recommended EASL standards. Standards with the lowest likelihood of being met were identified as optimal UDCA dosing, assessment of bone density and assessment of clinical symptoms (pruritus and fatigue). Significant variations in meeting these three standards were observed across UK, in addition to assessment of biochemical response to UDCA (all p<0.0001) and assessment of transplant eligibility in high-risk patients (p=0.0297).
Conclusion
Our findings identify a broad-based deficiency in ‘real-world’ PBC care, suggesting the need for an intervention to improve guideline adherence, ultimately improving patient outcomes. We developed the PBC Review tool and recommend its incorporation into clinical practice. As the first audit of its kind, it will be used to inform a future wide-scale reaudit.
Keywords: autoimmune biliary disease, autoimmune liver disease, liver cirrhosis, chronic liver disease, cholestatic liver diseases
Significance of this study.
What is already known on this topic
Guidelines on management and diagnosis of primary biliary cholangitis (PBC) were published in 2017 and 2018. They emphasised on long-term, individualised treatment with consideration for the symptom burden of the disease.
What this study adds
In the first audit of its kind, we have demonstrated significant shortcomings, across the 11 UK-based hospitals involved, in meeting recommended targets published in European Association for the Study of the Liver guidelines for PBC. This indicates the need for widespread analysis of PBC care in UK and improvement of services.
How might it impact on clinical practice in the foreseeable future
This study will inform future quality improvement projects in PBC and promote awareness of existing management guidelines, ultimately improving the quality of PBC services and patient outcomes.
Introduction
Primary biliary cholangitis (PBC) is an autoimmune, cholestatic liver disease characterised by destruction of intrahepatic cholangiocytes and progressive fibrosis.1–3 The chronic disease course culminates in end-stage biliary cirrhosis and its associated complications such as portal hypertension.1–3 The UK prevalence of PBC is estimated to be 15 000.2
Clinical features and the impact of PBC on the quality of life (QoL) are highly variable.4 5 Common features include pruritus, fatigue, memory problems and decreased bone mineral density.6 The aims of life-long treatment are to minimise the symptom burden, slow down disease progression and manage complications.1 4 Individuals with inadequate biochemical response to first-line therapy, ursodeoxycholic acid (UDCA), following 1 year of treatment, are regarded as high risk of progressive disease.1 2 7
Updated guidelines for PBC management were published in 2017 by European Association for the Study of the Liver (EASL) and in 2018 by the British Society of Gastroenterology (BSG) in collaboration with UK-PBC—both recommend the utilisation of audit tools.1 2 At the time of writing, no formal analysis has been undertaken on the management of PBC nationally.
This pilot audit aims to gain insight into the performance within the UK National Health Service (NHS). We aim to identify whether key targets are being met on an individual and national level.
Materials and methods
This study is a multicentre, retrospective pilot audit of PBC management across UK.
Site recruitment
Site recruitment was undertaken through electronic emailing and collaborative efforts between clinicians. All hospitals in the UK managing patients with PBC were eligible. The recruitment process commenced in May 2017 until March 2020. Appointed audit leads used a clinical audit tool for data collection—a Microsoft Excel spreadsheet with predefined standards based on EASL guidelines.1 The accompanying audit proforma is provided in online supplemental materials.
flgastro-2020-101713supp001.pdf (3.3MB, pdf)
A total of 11 NHS hospitals from England, Wales and Scotland contributed data towards this audit. Their trusts are listed below:
Royal Free London NHS Foundation Trust.
Imperial College Healthcare NHS Trust London.
London North West University Healthcare NHS Trust.
York Teaching Hospital NHS Foundation Trust.
University Hospitals of Derby and Burton NHS Foundation Trust.
Aneurin Bevan University Health Board.
Betsi Cadwaladr University Health Board.
Swansea Bay University Health Board
Hywel Dda University Health Board.
Cardiff & Vale University Health Board.
NHS Grampian.
The involved hospitals have been anonymised for publication purposes and will be referred by their corresponding number in table 1 where they are summarised.
Table 1.
Summary of the NHS hospitals involved in this audit
| NHS hospital | Data collection period | Number of patients | Number of patients with concurrent AIH (% of total patients) | % of female patients (number) | Mean age (SD) |
| Hospital 1* | June–July 2018 | 122 | 43 (35.3) | - | - |
| Hospital 2* | October–November 2018 | 75 | 17 (22.7) | - | 66.9 (10.43) |
| Hospital 3* | 2017–2018 | 10 | 1 (10.00) | 100.0 (10) | 57.2 (13.52) |
| Hospital 4 | February–March 2020† | 19 | 2 (10.5) | 94.7 (18) | 62.5 (17.95) |
| Hospital 5* | December 2017–January 2018 | 166 | 6 (4.00) | 95.0 (151/159)‡ | 58.3 (11.44) |
| Hospital 6* | August–December 2019 | 69 | 10 (14.00) | 95.7 (66) | 68.7 (12.82) |
| Hospital 7* | 2017–2018 | 123 | - | - | - |
| Hospital 8 | 2017–2018 | 18 | 3 (16.7) | 77.8 (14) | 69.4 (14.83) |
| Hospital 9* | 2017–2018 | 82 | 15 (18.3) | - | - |
| Hospital 10 | September–October 2017 | 18 | 2 (11.1) | - | - |
| Hospital 11* | 2017–2018 | 88 | 12 (13.6) | - | 60.9 (13.89) |
| Total dataset | 790 | 111 (14.1) | 62.1 (13.16) |
Incomplete or absent datasets are indicated with a hyphen (-).
Data on number of patients, concurrent autoimmune hepatitis (AIH) diagnosis, percentage of women and mean age for the cohorts from each hospital is shown where available.
*Indicates hospitals with dedicated hepatology clinics. Hospitals with general gastroenterology clinics are unmarked.
†The patient list was obtained in December 2017, however, data collection was delayed due to staffing disruption. Data collection in 2020 was undertaken using the same list of patients obtained in 2017 to ensure consistency with other datasets.
‡Data on sex were absent for seven patients who were therefore omitted from the percentage calculation.
AIH, autoimmune hepatitis; NHS, National Health Service.
Audit standards
Audit standards were developed according to the 2017 EASL guidelines for PBC management. BSG/UK-PBC guidelines were published following the development of the audit standards and did not directly contribute.2 Standards were chosen according to guideline recommendations and feasibility of data collection from electronic records.
Specific audit standards with their respective EASL recommended targets shown in brackets, which include1:
Prescription of the recommended UDCA dose (13–15 mg/kg/day) (90%).
Assessment of biochemical response to UDCA following 1 year of treatment (80%).
Recorded symptom assessment of pruritus and/or fatigue (90%).
Assessment of bone density via a dual-energy X-ray absorptiometry (DEXA) scan within 5 years since diagnosis (80%) and appropriate medical intervention for patients with abnormal results such as supplementation with vitamin D (no recommended target).
Assessment of patients with severe disease for liver transplant eligibility (90%).
Patient recruitment, exclusion criteria and data collection
All patients over the age of 18, diagnosed with PBC and managed at each site, with available medical records were included. Patient lists were generated via coding departments; hospital biochemistry labs (patients positively testing for antimitochondrial antibodies (AMA) or PBC-specific antinuclear antibodies (ANA)); local databases and/or histopathology results. Patients who were under investigation for suspected PBC, had missing records or had been transferred to a different site at the time of data collection were excluded.
Collected data included age, sex, weight, UDCA dosage, UDCA discontinuation, record of assessment of UDCA response at 1 year from initial UDCA prescription, record of assessment of pruritus, fatigue and bone density within 5 years of diagnosis, intervention for abnormal bone density findings and record of assessment of transplant eligibility for high-risk patients.
Symptom assessment was evaluated via information in clinic letters. Assessment involved subjective evaluation in the majority of cases, however, a few clinicians used objective assessments such as the PBC-40 questionnaire.4
Data analysis and statistics
Data were combined into a single master-audit database. Hospitals were omitted from comparisons if data sets were missing or inputted incorrectly. Data were grouped according to country (England, Scotland, Wales) and the level of hepatology service provided, general gastroenterology clinic (GGC) or dedicated hepatology clinic (DHC). Averages were calculated using mean and SD. χ2 analysis was undertaken to enable assessment of variation in compliance to EASL guidelines between hospitals. For the comparison of GGC versus DHC, Fisher’s exact test was undertaken in preference to χ2 due to increased accuracy. Statistical analysis was performed using GraphPad Prism V.8. As the study design did not include analysis of factors contributing to discrepancies in performance—such as the local clinical service structure, patients’ comorbidities, compliance and ethnic background—no regression models were applied.
Governance and support
Approval was obtained from each site as per local policy. No patient-identifying information was collected and patient management was not affected. This project was supported by the PBC Foundation. Dr Falk Pharma UK supported local audits with materials such as the audit proforma. No funding was received. Neither Dr Falk Pharma nor PBC Foundation was involved in data analysis or report writing.
Results
Population
Data from 790 patients at 11 hospitals were obtained from May 2017 to March 2020. The number of patients involved in data collection at each site ranged from 10 patients (hospital 3) to 166 patients (hospital 5). The mean age at the time of data collection was 62.1 years (SD, 13.16). Across the five hospitals that provided data on sex distribution, the percentage of female patients was 94.2% (259 of 275 patients). table 1 details each hospital involved in the audit. Supplementary data are presented in online supplemental materials.
UDCA dosing and assessment of response at 1 year
Across all 11 hospitals, 670 of 790 (84.8%) patients had records of UDCA prescription, with 65 of 670 (9.7%) patients discontinuing treatment (figure 1A). Documentation of reasoning behind discontinuation was limited and inconsistent. The most frequent reasons were intolerance—notably nausea, vomiting and diarrhoea—or that the patient had received a liver transplant.
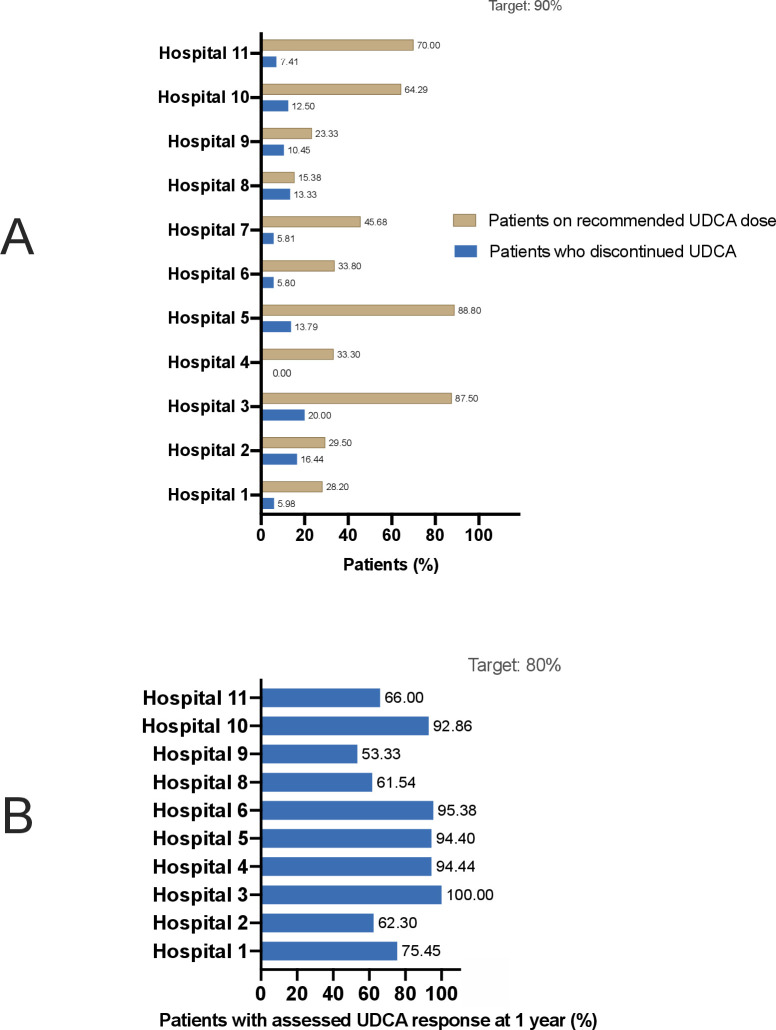
Figure 1.
(A) Bar chart showing (a) percentages of the total number of patients with PBC initially prescribed UDCA who discontinued treatment and (b) percentages of the patients with ongoing UDCA treatment who were prescribed the recommended dose of 13–15 mg/kg daily. Data were available from all 11 hospitals, as displayed on the y axis. (B) Bar chart showing the percentages of patients with PBC with ongoing UDCA treatment that underwent a biochemical assessment of UDCA response following 1 year of treatment. Data were available from 10 hospitals, as displayed on the y axis. PBC, primary biliary cholangitis; UDCA, ursodeoxycholic acid.
Of the patients remaining on UDCA treatment, 292 of 605 (48.3%) patients had been prescribed the recommended UDCA dose of 13–15 mg/kg/day, 288 of 605 (47.6%) patients were prescribed an alternative dose and 25 of 605 (4.1%) patients were prescribed an unspecified dose. None of the 11 hospitals met the EASL target of 90% for prescription of the recommended UDCA dose. Significant variation was observed between hospitals, ranging from 15.8% (hospital 8) to 88.8% (hospital 5) (p<0.0001) (figure 1A).
Data on assessment of UDCA response were available from 10 hospitals, comprising of 524 patients remaining on UDCA treatment (86.6% of 605 patients remaining on UDCA in all 11 hospitals). Assessment of UDCA response at 1 year was recorded in 414 of 524 (79.0%) patients. Five of the 10 assessed hospitals met the EASL target of 80%. A significant variation was observed between hospitals, ranging from 53.3% (hospital 9) to 100% (hospital 3) (p<0.0001) (figure 1B).
Symptom assessment
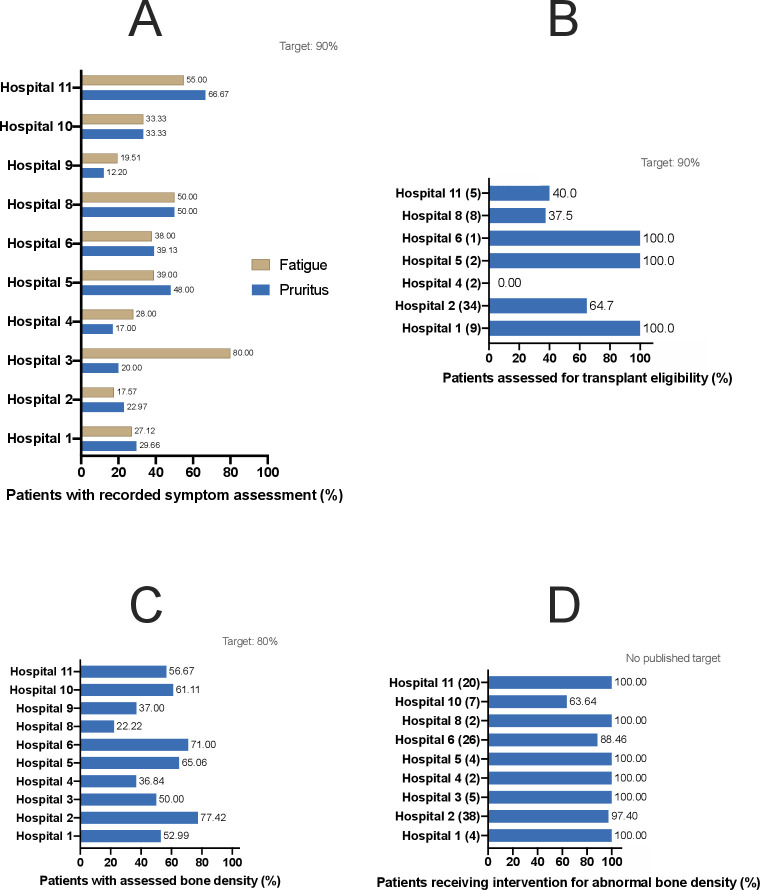
Data on symptom assessment were available from 592 of 667 (88.8%) patients across 10 hospitals. Pruritus assessment was recorded in 209 of 592 (35.3%) patients and fatigue assessment in 197 of 592 (33.3%) patients. None of the hospitals met the EASL target of 90%. Significant variation was observed between hospitals for recorded assessments of both pruritus and fatigue (ranges: pruritus—12.2%–66.7%, fatigue— 17.6%–80.0%) (p<0.0001) (figure 2A).
Figure 2.
(A) Bar chart showing percentages of all patients with PBC with a recorded assessment of (a) fatigue and (b) pruritus. Data were available from 10 hospitals, as displayed on the y axis. (B) Bar chart showing the percentages of high-risk patients undergoing assessment for liver transplant eligibility. Data were available from seven hospitals, as displayed on the y axis. The number of patients classified as high-risk is shown in brackets for individual hospitals. (C) Bar chart showing the percentages of all patients with PBC undergoing assessment of bone density within 5 years of PBC diagnosis. Data were available from 10 hospitals, as displayed on the y axis. (D) Bar chart showing the percentages of patients with PBC with abnormal bone density findings that received an appropriate intervention. Data were available from nine hospitals, as displayed on the y axis. Number of patients with abnormal bone density readings is shown in brackets for individual hospitals. PBC, primary biliary cholangitis.
Transplant consideration
Data on transplant consideration were available from seven hospitals. Sixty-one of 557 (11%) patients were recorded as high risk. Thirty-nine of 61 (63.9%) high-risk patients underwent assessment for liver transplant eligibility. Four of the seven assessed hospitals met the EASL target of 90%. Significant variation was observed between hospitals, ranging from 0% (hospital 4) to 100% (multiple hospitals) (p=0.0297) (figure 2B).
Bone density assessment
Bone density assessment within 5 years of PBC diagnosis was recorded in 358 of 621 (57.6%) patients across 10 hospitals. None of the hospitals met the EASL target of 80%. Significant variation was observed between hospitals, ranging from 22.2% (hospital 8) to 77.4% (hospital 2) (p<0.0001) (figure 2C). The proportions of patients with abnormal bone density that were provided an appropriate intervention ranged from 88.5% (hospital 6) to 100% (multiple hospitals). There was no significant variation observed among hospitals (p=0.6148) ( figure 2D ).
Comparison between England, Wales and Scotland
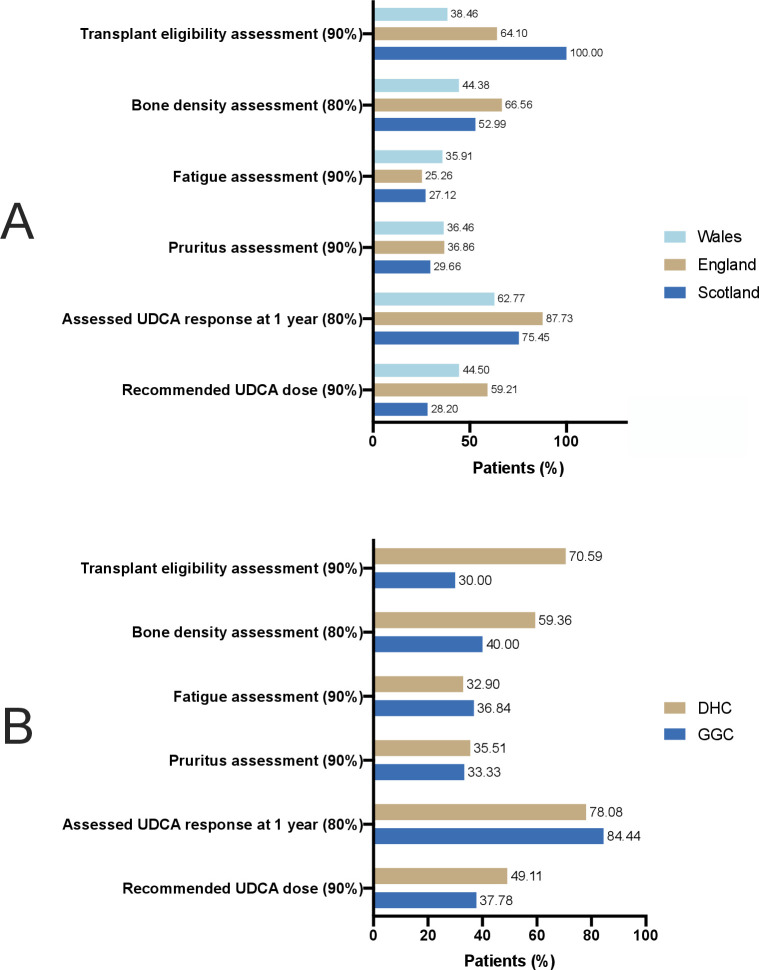
Significant variation in performance was observed between England (five hospitals, 339 patients), Wales (five hospitals, 329 patients) and Scotland (one hospital, 122 patients) in all recorded standards except pruritus assessment (figure 3A). Adherence to the guidelines in England was greater for recommended UDCA dosing (59.2% vs 44.5% Wales, 28.2% Scotland), assessment of UDCA response (87.7% vs 62.8% Wales, 75.5% Scotland) and assessment of bone density within 5 years (66.6% vs 44.4% Wales, 53.0% Scotland). Raw data and statistical analysis are shown in online supplemental materials.
Figure 3.
(A) Bar chart showing the performance of England (five hospitals), Wales (four to five hospitals) and Scotland (one hospital) for all assessed targets, as displayed on the y axis. One Welsh hospital provided data for recommended UDCA dosing only and for no other standards. Data on assessment of transplant eligibility were available from four English and two Welsh hospitals. (B) Bar chart showing the performance of GGC (two to three hospitals) and DHC (eight hospitals) for all assessed targets, as displayed on the y axis. One DHC hospital provided data for recommended UDCA dosing only and for no other standards. Data on assessment of transplant eligibility were available from two GGC hospitals and five DHC hospitals. DHC, dedicated hepatology clinics; GGC, general gastroenterology clinics; PBC, primary biliarycholangitis; UDCA, ursodeoxycholic acid.
Comparison between DHC and GGC
Depending on the hospital, patients with PBC were either seen in DHC or GGC. For two of the six assessed standards—assessments of bone density and transplant eligibility— significantly greater performance was observed in DHC (eight hospitals, 735 patients) compared with GGC (three hospitals, 55 patients) (figure 3B). The 80% target for assessment of UDCA response at 1 year was met by GGC only (84.4%). Raw data and statistical analysis are shown in online supplemental materials.
Discussion
In the first nationwide pilot audit of PBC management, our primary aim was to gain an indication of the quality of PBC care to inform a potential widespread audit. We obtained a large sample size, treated across 11 large hospitals. This is representative of the population of patients with PBC managed within the NHS and enables examination of care quality and nationwide variability. Real-world data were captured, ensuring that our findings are reflective of clinical practice.
None of the hospitals met all the recommended EASL targets, and targets were often substantially missed. The poor adherence to recommended UDCA dosing is a cause for concern. Surprisingly, 50% of hospitals met the target for assessment of UDCA response, which may reflect an emphasis on risk stratification in PBC education.8 Poor survival has been reported in individuals responding poorly to UDCA.9 10 The early identification of high-risk individuals and provision of second-line treatments could significantly improve disease outcomes.11 12 Undertreatment of UDCA via sub-optimal dosing has been suggested as a predictive factor in the development of cirrhosis, HCC and liver failure.13–16
No hospital met the target for symptom screening or bone density assessment. Regular assessment of symptom burden has been highlighted as a key aspect of lifelong PBC management.17 One study observed that approximately 51% of patients develop PBC symptoms within 5 years after diagnosis.18 Furthermore, up to 44% of patients with PBC are affected by osteoporosis, with the majority having osteopenia.2 This pilot audit was based on EASL guidelines alone, which recommend the use of DEXA scan in all patients with PBC. BSG/UK-PBC guidelines recommend risk assessment—using the FRAX or QFracture score—and a subsequent DEXA scan when scores indicate treatment.2 This disparity may explain the poor performance for this target across hospitals.
This audit has identified statistically significant variation in performance across individual hospitals, between countries and between GGC and DHC. Caution should be undertaken when interpreting the GGC versus DHC comparison due to the differences in population sizes between the assessed groups (55 vs 735 patients, respectively). This may be due to the increased availability of PBC-related databases within DHC. For this reason, not every hospital was able to participate and hospitals with DHC were more willing to contribute to the study. Geographic variation in UDCA use has been reported.19 Additionally, a global cohort study—which included the UK—previously reported a large number of patients who were underdosed with UDCA.16
An intervention is necessary to improve clinical practice. Simple techniques, such as the implementation of a short review form or checklist to use at follow-up, may provide a promising strategy.20 21 Until recently, the only PBC-specific health-related QoL assessment was the PBC-40 questionnaire.4 22 Guidelines recommend symptom assessment but do not specify tools to score symptoms objectively. The PBC-10 questionnaire has recently been developed and validated for this purpose.23
We have developed a PBC Review tool—based on guideline recommendations and the PBC-10—for use in hospitals. This is provided in online supplemental materials. A copy of this tool, with our findings, will be provided to the contributing hospitals. We aim to establish a national PBC registry for data collection to facilitate future quality improvement projects.
There are some limitations to our pilot audit. Audits were initially intended to be carried out for local purposes. Compilation of data into a national aggregate and subsequent analysis was undertaken by different authors. As a result, there is potential variation in the quality and consistency of data collection between sites. We did not report on the use of second-line treatments, such as obeticholic acid, as they were not widely prescribed at the time of audit development. Hospitals that reported second-line prescription are shown in online supplemental materials. At the time of writing, EASL and BSG-UK-PBC guidelines have been established for at least 2 years; however, most hospitals collected data in 2017 and 2018. Improvement in PBC management may have occurred since, thus, results may not accurately reflect current practice.
This pilot audit was not designed to assess the causes of deficiencies in PBC care. Consideration should be made for the likely influence of potential conflict between patient choice and recommended guidelines on target failures. Data from a limited number of involved hospitals included notes such as ‘poor tolerance of recommended UDCA dosage’, ‘reluctance to increase UDCA dose’ after years on a lower-than-recommended dose and ‘failure to attend appointments’. Data have not been obtained for individual consultants, such as specialism into hepatology or luminal gastroenterology, which may influence knowledge of existing guidelines and quality of care. Formal analysis of these factors should be considered in a future audit to investigate the extent of their influence on guideline non-adherence. Analysis should also include explicit documentation of reasons for failure in guideline adherence and include data on second-line therapies, referral to tertiary care and biochemistry.
We have revealed clear gaps in quality of national PBC care, with notable failures in UDCA dosing and symptom assessment. Our findings justify the recommendation of incorporating a PBC review tool into clinical practice. We recommend that managing clinicians review clinical guidelines and ensure departmental practice are up to date. Optimal patient management is crucial to minimising disease progression and maximising QoL. A refined, wide-scale national reaudit will be developed in the near future.
Acknowledgments
Dr Falk Pharma UK, PBC Foundation, Gastroenterology Trainees’ Research Collaboration—Cymru (GASTRIC-C).
Footnotes
Correction notice: This article has been corrected since it published Online First. A typographical error has been corrected in the materials and methods section.
Contributors: All persons who meet authorship criteria are listed as authors, and all authors certify that they have participated sufficiently in the work to take public responsibility for the content, including participation in the concept, design, analysis, writing or revision of the manuscript. All authors have reviewed the final manuscript and have confirmed their inclusion in the authorship list. Furthermore, each author certifies that this material or similar material has not been and will not be submitted to or published in any other publication. Guarantor of article: LA; specific contributions are listed below: MS—investigation, data curation, formal analysis, writing—original draft, writing—review and editing, visualisation. First and corresponding author. AG—writing—review and editing, supervision. Joint first author. LA—conceptualisation, data acquisition, formal analysis, supervision, writing—review and editing, approval of final version. Senior author and guarantor. DJ—conceptualisation, supervision, writing—review and editing, approval of final version. Senior author. The following authors were involved in investigation and data acquisition: ES, YML, NS, BC-S, AM, LT, AM, HKT, HNH, RV.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
No ethical approval was required, in keeping with all projects on the programme of UK national audits.
References
- 1. European Association for the Study of the Liver. Electronic address: easloffice@easloffice.eu, European Association for the Study of the Liver . EASL clinical practice guidelines: the diagnosis and management of patients with primary biliary cholangitis. J Hepatol 2017;67:145–72. 10.1016/j.jhep.2017.03.022 [DOI] [PubMed] [Google Scholar]
- 2. Hirschfield GM, Dyson JK, Alexander GJM, et al. The British Society of Gastroenterology/UK-PBC primary biliary cholangitis treatment and management guidelines. Gut 2018;67:1568–94. 10.1136/gutjnl-2017-315259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Onofrio FQ, Hirschfield GM, Gulamhusein AF. A practical review of primary biliary cholangitis for the gastroenterologist. Gastroenterol Hepatol 2019;15:145–54. [PMC free article] [PubMed] [Google Scholar]
- 4. Jacoby A, Rannard A, Buck D, et al. Development, validation, and evaluation of the PBC-40, a disease specific health related quality of life measure for primary biliary cirrhosis. Gut 2005;54:1622–9. 10.1136/gut.2005.065862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mells GF, Pells G, Newton JL, et al. Impact of primary biliary cirrhosis on perceived quality of life: the UK-PBC national study. Hepatology 2013;58:273–83. 10.1002/hep.26365 [DOI] [PubMed] [Google Scholar]
- 6. Galoosian A, Hanlon C, Zhang J, et al. Clinical updates in primary biliary cholangitis: trends, epidemiology, diagnostics, and new therapeutic approaches. J Clin Transl Hepatol 2020;8:49–60. 10.14218/JCTH.2019.00049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lindor KD, Bowlus CL, Boyer J, et al. Primary biliary cholangitis: 2018 practice guidance from the American association for the study of liver diseases. Hepatology 2019;69:394–419. 10.1002/hep.30145 [DOI] [PubMed] [Google Scholar]
- 8. Corrigan M, Hirschfield G, Greenfield S, et al. Barriers to implementation of stratified care in primary biliary cholangitis: a scoping exercise. BMJ Open Gastroenterol 2019;6:e000226. 10.1136/bmjgast-2018-000226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Parés A, Caballería L, Rodés J. Excellent long-term survival in patients with primary biliary cirrhosis and biochemical response to ursodeoxycholic acid. Gastroenterology 2006;130:715–20. 10.1053/j.gastro.2005.12.029 [DOI] [PubMed] [Google Scholar]
- 10. Corpechot C, Abenavoli L, Rabahi N, et al. Biochemical response to ursodeoxycholic acid and long-term prognosis in primary biliary cirrhosis. Hepatology 2008;48:871–7. 10.1002/hep.22428 [DOI] [PubMed] [Google Scholar]
- 11. Bowlus CL, Pockros PJ, Kremer AE, et al. Long-Term obeticholic acid therapy improves histological endpoints in patients with primary biliary cholangitis. Clin Gastroenterol Hepatol 2020;18:1170–8. 10.1016/j.cgh.2019.09.050 [DOI] [PubMed] [Google Scholar]
- 12. Trauner M, Nevens F, Shiffman ML, et al. Long-term efficacy and safety of obeticholic acid for patients with primary biliary cholangitis: 3-year results of an international open-label extension study. Lancet Gastroenterol Hepatol 2019;4:445–53. 10.1016/S2468-1253(19)30094-9 [DOI] [PubMed] [Google Scholar]
- 13. Prince M, Chetwynd A, Newman W, et al. Survival and symptom progression in a geographically based cohort of patients with primary biliary cirrhosis: follow-up for up to 28 years. Gastroenterology 2002;123:1044–51. 10.1053/gast.2002.36027 [DOI] [PubMed] [Google Scholar]
- 14. Corpechot C, Chazouillères O, Poupon R. Early primary biliary cirrhosis: biochemical response to treatment and prediction of long-term outcome. J Hepatol 2011;55:1361–7. 10.1016/j.jhep.2011.02.031 [DOI] [PubMed] [Google Scholar]
- 15. Corpechot C, Carrat F, Bahr A, et al. The effect of ursodeoxycholic acid therapy on the natural course of primary biliary cirrhosis. Gastroenterology 2005;128:297–303. 10.1053/j.gastro.2004.11.009 [DOI] [PubMed] [Google Scholar]
- 16. Harms MH, van Buuren HR, Corpechot C, et al. Ursodeoxycholic acid therapy and liver transplant-free survival in patients with primary biliary cholangitis. J Hepatol 2019;71:357–65. 10.1016/j.jhep.2019.04.001 [DOI] [PubMed] [Google Scholar]
- 17. Tripathi D, Stanley AJ, Hayes PC, et al. U.K. guidelines on the management of variceal haemorrhage in cirrhotic patients. Gut 2015;64:1680–704. 10.1136/gutjnl-2015-309262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Prince MI, Chetwynd A, Craig WL, et al. Asymptomatic primary biliary cirrhosis: clinical features, prognosis, and symptom progression in a large population based cohort. Gut 2004;53:865–70. 10.1136/gut.2003.023937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lu M, Li J, Haller IV, et al. Factors associated with prevalence and treatment of primary biliary cholangitis in United States health systems. Clin Gastroenterol Hepatol 2018;16:1333–41. 10.1016/j.cgh.2017.10.018 [DOI] [PubMed] [Google Scholar]
- 20. Ebben RHA, Siqeca F, Madsen UR, et al. Effectiveness of implementation strategies for the improvement of guideline and protocol adherence in emergency care: a systematic review. BMJ Open 2018;8:e017572. 10.1136/bmjopen-2017-017572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Treadwell JR, Lucas S, Tsou AY. Surgical checklists: a systematic review of impacts and implementation. BMJ Qual Saf 2014;23:299–318. 10.1136/bmjqs-2012-001797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Newton JL, Hudson M, Tachtatzis P, et al. Population prevalence and symptom associations of autonomic dysfunction in primary biliary cirrhosis. Hepatology 2007;45:1496–505. 10.1002/hep.21609 [DOI] [PubMed] [Google Scholar]
- 23. Alrubaiy L, Mells G, Flack S, et al. PBC-10: a short quality of life measure for clinical screening in primary biliary cholangitis. Aliment Pharmacol Ther 2019;50:1223–31. 10.1111/apt.15554 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
flgastro-2020-101713supp001.pdf (3.3MB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.