Version Changes
Revised. Amendments from Version 1
Based on reviewer feedback, changes that have been incorporated as part of the revised version: 1. Additional clarification provided for 'unit occupancy' under section 'methods' and sub-section 'variables'. 2. Under the section 'methods', sub-section 'analysis' , a sentence added on why interrupted time series was not used. 3. Figure 1- color of lines changes to 'orange' for clarity 4. All p values reported in the format recommended by the reviewer 5. 'Discussion' section updated to add reasons for possible increase in mortality during the pandemic period and an additional point around the lack of granularity of information on 'case-mix' added to limitations.
Abstract
Background: Coronavirus disease 2019 (COVID-19) has been responsible for over 3.4 million deaths globally and over 25 million cases in India. As part of the response, India imposed a nation-wide lockdown and prioritized COVID-19 care in hospitals and intensive care units (ICUs). Leveraging data from the Indian Registry of IntenSive care, we sought to understand the impact of the COVID-19 pandemic on critical care service utilization, case-mix, and clinical outcomes in non-COVID ICUs.
Methods: We included all consecutive patients admitted between 1 st October 2019 and 27 th September 2020. Data were extracted from the registry database and included patients admitted to the non-COVID or general ICUs at each of the sites. Outcomes included measures of resource-availability, utilisation, case-mix, acuity, and demand for ICU beds. We used a Mann-Whitney test to compare the pre-pandemic period (October 2019 - February 2020) to the pandemic period (March-September 2020). In addition, we also compared the period of intense lockdown (March-May 31 st 2020) with the pre-pandemic period.
Results: There were 3424 patient encounters in the pre-pandemic period and 3524 encounters in the pandemic period. Comparing these periods, weekly admissions declined (median [Q1 Q3] 160 [145,168] to 113 [98.5,134]; p<0.001); unit turnover declined (median [Q1 Q3] 12.1 [11.32,13] to 8.58 [7.24,10], p<0.001), and APACHE II score increased (median [Q1 Q3] 19 [19,20] to 21 [20,22] ; p<0.001). Unadjusted ICU mortality increased (9.3% to 11.7%, p=0.015) and the length of ICU stay was similar (median [Q1 Q3] 2.11 [2, 2] vs. 2.24 [2, 3] days; p=0.151).
Conclusion: Our registry-based analysis of the impact of COVID-19 on non-COVID critical care demonstrates significant disruptions to healthcare utilization during the pandemic and an increase in the severity of illness.
Keywords: COVID-19, registries, critical care, severity of illness
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has been responsible for over 3.4 million deaths globally as of 26 th May 2021 ( WHO COVID-19 Dashboard). In India, there have been over 25 million cases and approximately 300000 deaths ( WHO COVID-19 Dashboard for India). As part of the early pandemic response in the first wave, India and several other countries imposed nation-wide lockdowns and restrictions to control the spread of the disease ( The Hindu, BBC). Health-services were restructured with prioritization of COVID-19 care ( The Economic Times, The Times of India) including in hospitals and intensive care units (ICUs). The lockdown also disrupted public transport, limiting access to healthcare facilities. In addition, fears of contracting the infection dissuaded patients from seeking care for non-COVID-19 illnesses ( The Wire Science, TOI Plus).
In past smaller epidemics, health systems have struggled to maintain routine services and non-pandemic healthcare and public health services suffered 1, 2 . During the ongoing COVID-19 pandemic, there is limited information on how the outbreak has impacted acute and critical care service provision in India and other low- and middle-income countries (LMICs).
Even in non-pandemic times, India has a limited supply of critical care capacity with bed availability estimated at 2.6 per 100,000 population compared with much higher capacity in most high-income countries, for example 12.9 ICU beds per 100,000 population in Canada 3 , and other LMICs in the region, for example 11.7 beds per 100,000 population in Mongolia 4 . Other well-described challenges to the delivery of critical care in India include the limited number of beds with capacity for oxygen delivery, ventilators, and importantly, healthcare professionals 5 . All these challenges are further amplified by the disparities in distribution of these resources between urban and rural India 6 and between the public and private sector.
In this context, critical care registries, by continually evaluating service provision, case-mix and outcomes, can be used to describe the impact of pandemic on critical care service provision and inform health-capacity strengthening efforts. The Indian Registry of IntenSive care (IRIS) prospectively collects information on service utilisation, case mix, and outcomes 7 . Leveraging the registry platform, we sought to understand the impact of the COVID-19 pandemic on critical care service utilization, case-mix, severity of illness and clinical outcomes in non-COVID ICUs.
Methods
Data sources
All data for this analysis was available from IRIS. IRIS, a cloud-based registry established in January 2019, prospectively collects information on service utilisation, case-mix, and outcomes. 13 hospitals (13 ICUs) currently participate in the registry and details of implementation have previously been published 7 .
For this report, we included all consecutive cases admitted between 1 st October 2019 and 27 th September 2020. Patients admitted before 27 th September 2020, but not discharged at time of analysis (2 nd November 2020) were excluded. Data was extracted from the registry database and included patients admitted to the non-COVID or general ICUs at each of the sites. In all participating hospitals, COVID-19 patients were managed in designated locations and as such, not included in the registry. No additional variables, other than those already available in the registry, were included in the study design.
Variables
The main exposure was time, defined as the pre-pandemic period (October 2019-February 2020), pandemic period (March-September 2020), and period of intense lockdown (March-May 31 st 2020) within the pandemic period. Outcomes of interest included admission rates, unit occupancy, unit turnover, bed availability, use of resources at admission (invasive and non-invasive ventilation, vasoactive medications, renal replacement therapy), number of surgical admissions, route to admission (i.e. from operating room, emergency room, ward etc.) and case mix (diagnosis, APACHE II score 8 ).
Unit occupancy was defined in the registry as ( weekly number of admissions × mean weekly length of stay)/(number of beds available × 7). Unit turnover was defined in the registry as weekly number of discharges/(number of beds available × 7) and bed availability was defined as (weekly number of admissions × mean length of stay)-(bed capacity × 7).
Analysis
We used a Mann-Whitney test to compare baseline data from the pre-pandemic period to the pandemic period. In addition, we also compared the period of intense lockdown with the pre-pandemic period. October 2019 was chosen as the reference starting point as most units in the registry were contributing data by then (the registry was established in January 2019). While interrupted time series(ITS) would have been an ideal method for analysing temporal trends, we did not pursue this approach as the assumptions for ITS (linearity) were not met in our dataset and also due to the inability to control for covariates.
Data is presented as median (Q1, Q3) using weekly recorded numbers. We plotted 2020 data points with a loess smoothing line and standard error bars. Statistical analysis was conducted using RStudio v3.6.1 (R Foundation, Vienna, Austria). Full R code are provided (see Code availability) 9 and raw data are available with restrictions on access (see Data availability).
Ethics and consent
This analysis has been approved by the Institutional Ethics Committee (Apollo Main Hospital-C-S-010/02-21) centrally at the study coordinating centre. The consent model for IRIS has been previously described 7 . As this was a secondary analysis of deidentified registry data, no further individual patient-level consent was considered necessary or sought.
Patient and public involvement
Given the nature of this analysis, no patient or public involvement was sought.
Results
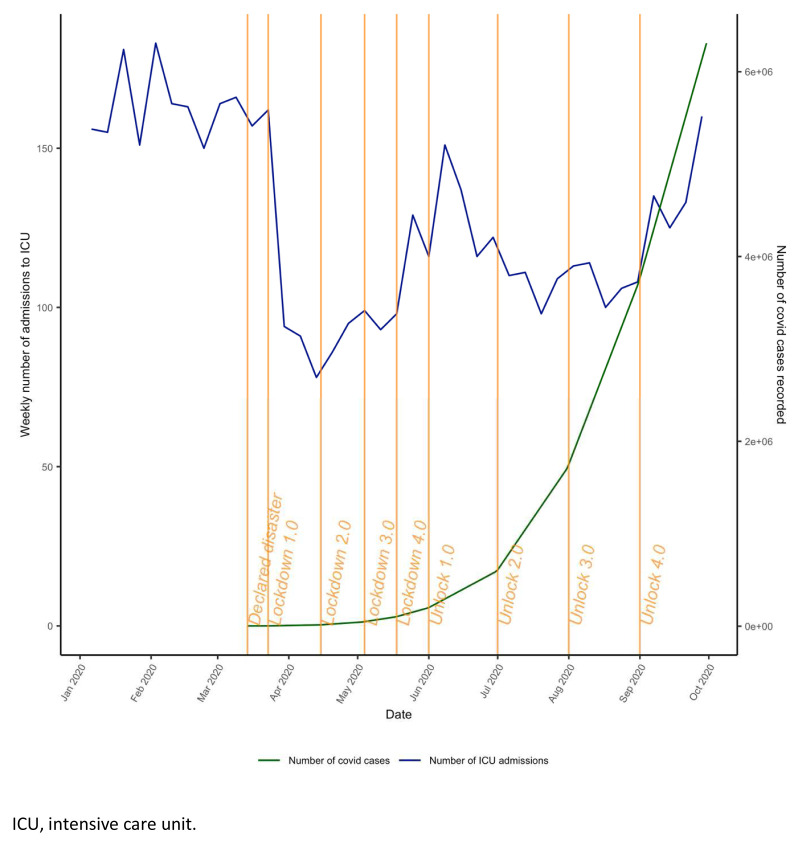
A total of 6948 patient encounters from 13 hospitals (13 ICUs) were reported between 1 st October 2019 and 27 th September 2020, with 3424 encounters in the pre-pandemic period and 3524 encounters in the pandemic period ( Figure 1). All variables had <6% missing data. National lockdown commenced in India on the 24 th March 2020, and the first phase of unlocking started on 1 st June 2020 ( Figure 2).
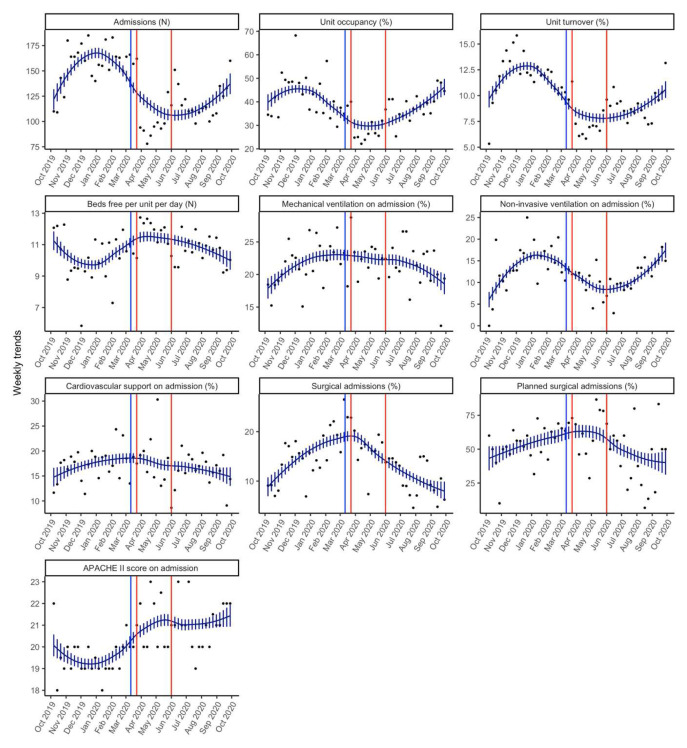
Figure 1. Smoothed weekly trends.
The dots are the original data, and the lines and bars are loess predictions and standard errors. The blue line represents March 11 th 2020, the date the WHO declared Covid a pandemic. The orange lines indicate the intense lockdown period in India from 23 rd March 2020– 1 st June 2020.
Figure 2. Phases of lockdown in India.
ICU, intensive care unit.
Number of admissions, case-mix and turnover
Weekly admissions declined from a median (Q1, Q3) of 160 (145, 168) admissions from the pre-pandemic period to 113 (98.5, 134.0) for the pandemic period (p<0.001) ( Table 1). For this same comparison period there was also a significant decline in the unit turnover from a median (Q1, Q3) of 12.1% (11.3, 13.1) to 8.6% (7.2, 10.0) (p<0.001) and unit occupancy from a median (Q1, Q3) of 43.2% (35.2, 49.0) to 35.1% (29.0, 40.0) ( Table 1).
Table 1. Comparison of pre and pandemic period.
All variables are reported as weekly median (Q1, Q3). A Mann-Whitney test was performed to statistically test the difference between the two time periods.
| Variable | Oct 2019 to Feb 2020 | Mar to Sep 2020 | p-value |
|---|---|---|---|
| Admissions (N) | 160 (145, 168) | 113 (98.5, 134) | <0.001 |
| Unit occupancy (%) | 43.19 (35.23, 49) | 35.12 (29.01, 40) | <0.003 |
| Unit turnover (%) | 12.1 (11.32, 13) | 8.58 (7.24, 10) | <0.001 |
| Beds free per unit per day (N) | 10.13 (9.3, 11) | 11.01 (10.35, 12) | 0.034 |
| Mechanical ventilation on admission (%) | 22.01 (19.01, 24) | 22.37 (19.49, 24) | 0.852 |
| Non-invasive ventilation on admission (%) | 14.56 (11.57, 17) | 11.43 (9.41, 13) | 0.013 |
| Cardiovascular support on admission (%) | 17.65 (14.57, 19) | 16.98 (14.56, 19) | 0.648 |
| Surgical admissions (%) | 14.59 (12.18, 18) | 14.29 (9.05, 16) | 0.634 |
| Planned surgical admissions (%) | 51.85 (46.43, 60) | 56.25 (37.5, 69) | 0.751 |
| APACHE II score on admission | 19 (19, 20) | 21 (20, 22) | <0.001 |
In terms of case-mix, there were no differences in the proportion of surgical admissions between these periods.
Comparing the pre-pandemic phase to the intense lockdown phase (March-May 2020), the median (Q1, Q3) weekly admissions declined to 98 (93, 157) admissions (p=0.003). In addition, for this comparison period, the percentage unit occupancy as well as unit turnover were also significantly lower during the intense lockdown period as compared to the pre-pandemic period ( Table 2). The number of beds free per day per week increased from a median (Q1, Q3) of 10.13 (9.3, 11) to 11.92 (11.01, 12) (p=0.005) during the intense lockdown phase ( Table 2).
For this comparison period, the proportion of surgical admissions increased from a median (Q1, Q3) of 14.6% (12.18, 18) to 17.4% (16.13, 20).
Severity of illness
The median APACHE II score (Q1, Q3) increased significantly from 19 (19, 20) in the pre-pandemic period to 21 (20, 22) during the pandemic period (p<0.001) ( Table 1). However, the median percentage of patients needing mechanical ventilation at admission was not different (22.01 vs. 22.37; p=0.852). There was a decline in the median percentage of patients needing non-invasive ventilation at admission from 14.56 (11.57, 17) to 11.43 (9.41, 13) (p=0.013). Need for cardiovascular support at admission was not different between the two periods (17.65% vs. 16.98%; p=0.648) ( Table 1).
Comparing the pre-pandemic period to the intense lockdown phase, the median APACHE II was significantly higher (19 vs. 20) (p<0.001) ( Table 2). The median proportion of patients needing mechanical ventilation was not different between these two periods ( Table 2). Similar to the previous comparison period, the median proportion of patients needing non-invasive ventilation was lower during the intense lockdown phase (14.56 vs. 11.58; p=0.021).
Table 2. Comparison of pre pandemic and intense lockdown periods.
All variables are reported as median (Q1, Q3). A Mann-Whitney test was performed to statistically test the difference between the two time periods.
| Variable | Oct 2019 to Feb 2020 | Mar to May 2020 | p-value |
|---|---|---|---|
| Admissions (N) | 160 (145, 168) | 98 (93, 157) | 0.003 |
| Unit occupancy (%) | 43.19 (35.23, 49) | 26.66 (25.02, 35) | <0.001 |
| Unit turnover (%) | 12.1 (11.32, 13) | 7.1 (6.59, 10) | <0.001 |
| Beds free per unit per day (N) | 10.13 (9.3, 11) | 11.92 (11.01, 12) | 0.005 |
| Mechanical ventilation on admission (%) | 22.01 (19.01, 24) | 22.48 (21.05, 24) | 0.595 |
| Non-invasive ventilation on admission (%) | 14.56 (11.57, 17) | 11.58 (10.2, 12) | 0.021 |
| Cardiovascular support on admission (%) | 17.65 (14.57, 19) | 18.52 (14.74, 19) | 0.736 |
| Surgical admissions (%) | 14.59 (12.18, 18) | 17.44 (16.13, 20) | 0.024 |
| Planned surgical admissions (%) | 51.85 (46.43, 60) | 65.38 (56.25, 73) | 0.029 |
| APACHE II score on admission | 19 (19, 20) | 20 (20, 22) | <0.001 |
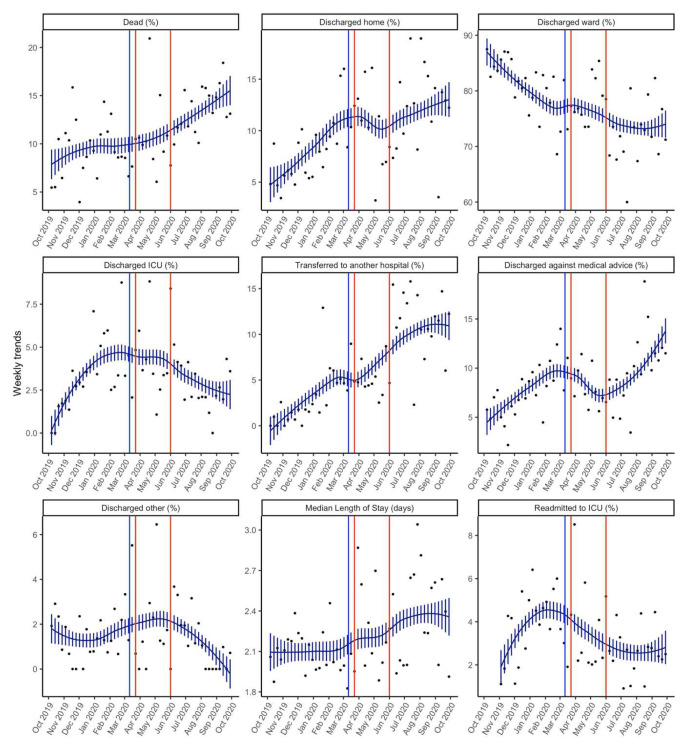
Outcomes
Table 3 and Figure 3 presents details of the key outcomes in the pandemic and pre-pandemic periods. There was a higher overall unadjusted ICU mortality during the pandemic period as compared to the pre-pandemic period (11.7% vs 9.3%, p=0.015). There was no difference in the median length of stay between the two periods.
Figure 3. Smoothed weekly trends of outcomes.
The dots are the original data, and the lines and bars are loess predictions and standard errors. The blue line represents March 11 th 2020, the date the WHO declared COVID-19 as a pandemic. The brown lines indicate the intense lockdown period in India from 23 rd March 2020– 1 st June 2020.
Table 3. Key outcomes: pre-pandemic and pandemic period.
All variables are reported as the weekly median with interquartile range. A Mann-Whitney test was performed to statistically test the difference between the two time periods.
| Variable | Oct 2019 to Feb 2020 | Mar to Sep 2020 | p-value |
|---|---|---|---|
| Dead (%) | 9.29 (7.5, 11) | 11.68 (9.91, 15) | 0.015 |
| Discharged home (%) | 6.45 (5.51, 9) | 12.23 (8.4, 14) | <0.001 |
| Discharged ward (%) | 82.52 (78.82, 84) | 73.56 (71.79, 79) | <0.001 |
| Discharged ICU (%) | 2.94 (1.88, 4) | 3.45 (2.09, 4) | 0.709 |
| Transferred to another hospital (%) | 1.76 (0.68, 3) | 8.7 (4.67, 12) | <0.001 |
| Discharged against medical advice (%) | 7.03 (5.29, 9) | 9.38 (7.18, 11) | 0.014 |
| Discharged other (%) | 1.29 (0.75, 2) | 1.15 (0, 2) | 0.910 |
| Readmitted to ICU (%) | 4.27 (2.76, 5) | 2.65 (2.17, 4) | 0.051 |
| Median length of stay (days) | 2.11 (2, 2) | 2.24 (2, 3) | 0.151 |
ICU, intensive care unit.
Discussion
Our registry-based analysis of the impact of COVID-19 on non-COVID critical care services shows a significant reduction in the median number of admissions to the ICUs during the pandemic period as compared to the pre-pandemic period. This reduction was most prominent during the intense lockdown phase. We also noted an increase in the median APACHE II score and a significant decline in the ICU turnover for comparison periods. While the median severity of illness was higher, we did not see an increase in the proportion of patients needing mechanical ventilation or cardio-vascular support at admission. Additionally, the proportion of planned surgical admissions declined over this period but was not statistically significant. Unadjusted ICU mortality was higher during the pandemic period, but the median length of stay was similar.
To our knowledge, our study is the first to demonstrate the collateral impact of the pandemic on non-COVID acute and critical care. In previous epidemics, similar findings have been reported. However, the scale and the extended timeline of the current pandemic means that such disruption is likely of much a larger magnitude than previously witnessed. Lee and colleagues reported a 33% reduction in emergency room visits during the MERS-CoV outbreak in South Korea 10 . Similarly, during the SARS outbreak, Huang and colleagues showed a mean reduction of 92.5±8.3 patients in emergency room visits 11 .
Such disruptions to other components of healthcare delivery have been reported during previous outbreaks and epidemics such as the impact of Ebola on maternal and child health services in Guinea 12 and of SARS on ambulatory and in-patient care 13 . During the current pandemic, concerns have been expressed about the impact on hematopoietic stem cell transplant 14 , on outcomes from cancer surgery 15 , on maternal and neonatal care 16 , and tuberculosis control programs 17, 18 .
There are several reasons for such disruptions, including the necessary and inevitable prioritization of pandemic healthcare services, obstacles to access of healthcare triggered by lockdown and suspension of public transport, fear of contracting infection whilst trying to access care, among others. Such medical avoidance behaviours have also been described during past outbreaks 19 . In India, a nationwide lockdown was imposed on 24 th March 2020 with an immediate disruption of public transport and the imposition of a curfew across the country. Additionally, hospitals were explicitly asked to prioritize COVID-19 care by increasing capacity, by redirecting resources (manpower, equipment etc.), and reducing or suspending non-emergency services.
In a recent survey of healthcare worker perceptions on the impact of the pandemic led by our group 20 , respondents reported a decline in acute care service utilisation and a delay in time-sensitive procedures such as percutaneous coronary angioplasties. In the view of the respondents, fear of contracting infection and lockdown were seen as having contributed the most to such disruptions. The results of the current study provide objective data to complement the perceptions of the survey respondents.
There are several possible reasons for the increase in mortality observed during the pandemic period. This could represent a real effect due to patients presenting late (and sicker) due to the fear of contracting COVID-19 when they come in contact with the healthcare system or due to pandemic imposed restrictions on access to healthcare facilities. Alternately, this could be a chance finding reflecting secular trends. We tried to limit this by extending the time periods of the analyses but cannot be confident that we have fully excluded such effects. This observed increase also be due to lack of adjustment for potential confounders.
Strengths and limitations
Our study has several important strengths. We compared the service utilisation during the pandemic and the intense lockdown phase with an extended pre-pandemic period to overcome any limitations arising from secular trends. Missingness for our dataset was less than 6% for all variables and the reported changes are therefore not due to systematic differences in data availability for the pre and pandemic periods. In addition, our study, to the best of our knowledge, is the first to provide objective data on disruptions to acute and critical care.
Our report has several limitations. Our network includes only a fraction of ICUs within India and may not be epidemiologically representative of the impact of the pandemic on critical care service utilisation across the country or wider region. The impact on ICU service utilisation described may be due to other agents external to the registry’s surveillance and are not described here. In addition, we did not include data from COVID ICUs nor did we compare the service utilization between the COVID and non-COVID areas. Mortality in our cohort is low (9.3 and 11.7%) as compared to other registries (for example 31% for the year 2019 in the Linking Of Global Intensive Care or LOGIC initiative) and this may be explained by a combination of reasons including the mix of ICUs represented in IRIS and the overall small number of ICUs currently participating. In addition, the registry collects information on broad diagnostic categories and does not have granular information on case-mix; as such, we were unable to describe changes in the case-mix during the pre and pandemic periods. We are also unable to comment on the effect of the pandemic on population-level health indicators. Nonetheless, we think this report provides valuable insights into the impact of public health decision and policy making during the pandemic and the impact of the pandemic on healthcare resource utilisation.
Conclusion
Our registry-based analysis of the impact of COVID-19 on non-COVID critical care demonstrates significant disruptions to healthcare utilization during the pandemic and an increase in the severity of illness. Our findings are likely to inform future healthcare planning during pandemics to minimise disruptions to other aspects of healthcare delivery.
Data availability
Underlying data
Pooled data from IRIS are available from the IRIS Dashboard at https://nicst.com/picu-iris-public/. The IRIS collaboration supports and welcomes data sharing. Our agreement with participating sites in the registry is only for the sharing of deidentified data between them and the registry coordinating centre for the purposes of audit, quality improvement and specific research questions. We are not allowed to post data on a repository or any other public database. However, raw data will be made available to qualified researchers who provide a detailed and methodologically sound proposal with specific aims that are clearly outlined. Such proposals will be screened by the IRIS Steering committee for approval.
Data sharing will be for the purposes of medical research and under the auspices of the consent under which the data were originally gathered. To gain access, qualified researchers will need to sign a data sharing and access agreement and will need to confirm that data will only be used for the agreed upon purpose for which data access was granted. Researchers can contact the corresponding author through electronic mail ( bharath@icuconsultants.com) for such access; alternatively, IRIS can be contacted at info@irisicuregistry.org and joinus@irisicuregistry.org.
Code availability
Analysis code available from: https://github.com/NICST-PROTECT/ICU-service-utilisation-public/tree/v1.0.1
Archived analysis code at time of publication: https://doi.org/10.5281/zenodo.4939947 9
License: MIT
Funding Statement
This work is partially supported by the Wellcome Trust and Mahidol Oxford Tropical Research Unit. Authors RH and AB were co-applicants on the Wellcome Innovations grant 215522.
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
[version 2; peer review: 2 approved]
References
- 1. Brolin Ribacke KJ, Saulnier DD, Eriksson A, et al. : Effects of the West Africa Ebola Virus Disease on Health-Care Utilization - A Systematic Review. Front Public Health. 2016;4:222. 10.3389/fpubh.2016.00222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lu TH, Chou YJ, Liou CS: Impact of SARS on healthcare utilization by disease categories: implications for delivery of healthcare services. Health Policy. 2007;83(2–3):375–81. 10.1016/j.healthpol.2007.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Phua J, Faruq MO, Kulkarni AP, et al. : Critical Care Bed Capacity in Asian Countries and Regions. Crit Care Med. 2020;48(5):654–62. 10.1097/CCM.0000000000004222 [DOI] [PubMed] [Google Scholar]
- 4. Mendsaikhan N, Begzjav T, Lundeg G, et al. : A Nationwide Census of ICU Capacity and Admissions in Mongolia. PLoS One. 2016;11(8):e0160921. 10.1371/journal.pone.0160921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tirupakuzhi Vijayaraghavan BK, Myatra SN, Mathew M, et al. : Challenges in the delivery of critical care in India during the COVID-19 pandemic. J Intensive Care Soc. 2020;1–7. 10.1177/1751143720952590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Saigal S, Sharma JP, Pakhare A, et al. : Mapping the Characteristics of Critical Care Facilities: Assessment, Distribution, and Level of Critical Care Facilities from Central India. Indian J Crit Care Med. 2017;21(10):625–33. 10.4103/ijccm.IJCCM_193_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Adhikari NKJ, Arali R, Attanayake U, et al. : Implementing an intensive care registry in India: preliminary results of the case-mix program and an opportunity for quality improvement and research [version 2; peer review: 2 approved]. Wellcome Open Res. 2020;5:182. 10.12688/wellcomeopenres.16152.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Knaus WA, Draper EA, Wagner DP, et al. : APACHE II: A severity of disease classification system. Crit Care Med. 1985;13(10):818–29. 10.1097/00003465-198603000-00013 [DOI] [PubMed] [Google Scholar]
- 9. Rashan A: NICST-PROTECT/ICU-service-utilisation-public: Added license.(Version v1.0.1). Zenodo. 2021. 10.5281/zenodo.4939947 [DOI] [Google Scholar]
- 10. Lee SY, Khang YH, Lim HK: Impact of the 2015 Middle East Respiratory Syndrome Outbreak on Emergency Care Utilization and Mortality in South Korea. Yonsei Med J. 2019;60(8):796–803. 10.3349/ymj.2019.60.8.796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Huang CC, Yen DH, Huang HH, et al. : Impact of severe acute respiratory syndrome (SARS) outbreaks on the use of emergency department medical resources. J Chin Med Assoc. 2005;68(6):254–59. 10.1016/S1726-4901(09)70146-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Delamou A, El Ayadi AM, Sidibe S, et al. : Effect of Ebola virus disease on maternal and child health services in Guinea: a retrospective observational cohort study. Lancet Glob Health. 2017;5(4):e448–e457. 10.1016/S2214-109X(17)30078-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chang HJ, Huang N, Lee CH, et al. : The Impact of the SARS Epidemic on the Utilization of Medical Services: SARS and the Fear of SARS. Am J Public Health. 2004;94(4):562–64. 10.2105/ajph.94.4.562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sahu KK, Siddiqui AD, Cerny J: COVID-19 pandemic and impact on hematopoietic stem cell transplantation. Bone Marrow Transplant. 2020;55(11):2193–95. 10.1038/s41409-020-0913-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sud A, Jones ME, Broggio J, et al. : Collateral damage: the impact on outcomes from cancer surgery of the COVID-19 pandemic. Ann Oncol. 2020;31(8):1065–74. 10.1016/j.annonc.2020.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kc A, Gurung R, Kinney MV, et al. : Effect of the COVID-19 pandemic response on intrapartum care, stillbirth, and neonatal mortality outcomes in Nepal: a prospective observational study. Lancet Glob Health. 2020;8(10):E1273–E1281. 10.1016/S2214-109X(20)30345-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fei H, Yinyin X, Hui C, et al. : The impact of the COVID-19 pandemic on tuberculosis control in China. Lancet Reg Health West Pac. 2020;3:100032. 10.1016/j.lanwpc.2020.100032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Husain AA, Monaghan TM, Kashyap RS: Impact of COVID-19 pandemic on tuberculosis care in India. Clin Microbiol Infect. 2021;27(2):293–294. 10.1016/j.cmi.2020.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lau JT, Griffiths S, Choi KC, et al. : Avoidance behaviors and negative psychological responses in the general population in the initial stage of the H1N1 pandemic in Hong Kong. BMC Infect Dis. 2010;10:139. 10.1186/1471-2334-10-139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tripathy S, Vijayaraghavan BK, Panigrahi MK, et al. : Collateral Impact of the COVID-19 Pandemic on Acute Care of Non-COVID Patients: An Internet-based Survey of Critical Care and Emergency Personnel. Indian J Crit Care Med. 2021;25(4):374–381. 10.5005/jp-journals-10071-23782 [DOI] [PMC free article] [PubMed] [Google Scholar]