Abstract
Background:
Highly-potent cannabis products, e.g., concentrates, entail greater risks of cannabis-related harms than lower-potency products such as plant or flower material. However, little information is available on whether individuals in U.S. states with recreational cannabis laws (RCL) or medical cannabis laws (MCL) are more likely than individuals in U.S. states without cannabis legalization (no-CL) to use highly-potent forms of cannabis.
Methods:
Cannabis-using adults in a 2017 online survey (N=4,064) provided information on state of residence and past-month cannabis use, including types of products used, categorized as low-potency (smoked or vaped plant cannabis) or high-potency (vaping or dabbing concentrates). Multivariable logistic regression models generated adjusted odds ratios (aOR) and 95% confidence intervals (CI) for use of high-potency cannabis products by state cannabis legalization status (RCL, MCL, no-CL).
Results:
Compared to participants in no-CL states, participants in RCL states had greater odds of using high-potency concentrate products (aOR=2.61;CI=1.77–3.86), as did participants in MCL-only states (aOR=1.55;CI=1.21–1.97). When participants in RCL states and MCL states were directly compared, those in RCL states had greater odds of using high-potency concentrate products (aOR=1.69;CI=1.27–2.42).
Discussion:
Although the sample was not nationally representative and the cross-sectional data precluded determining the direction of effect, results suggest that use of high-potency cannabis concentrates is more likely among those in RCL states. Clinicians in RCL states should screen cannabis users for harmful patterns of use. Policymakers in states that do not yet have RCL should consider these findings when drafting new cannabis laws, including the specific products permitted and how best to regulate them.
Keywords: Cannabis, marijuana, potency, legalization, vaping, concentrates
1. Introduction
In the United States (US), laws and attitudes towards cannabis are changing, as evidenced by the legalization of medical cannabis use in 36 states since 1996, and recreational cannabis use in 18 states since 2012. Although Americans increasingly believe that cannabis use is harmless (Chiu et al., 2021; Compton et al., 2016), a meta-analysis shows that ~20% of cannabis users develop cannabis use disorder (CUD) (Leung et al., 2020), with greatest risk among frequent users (Leung et al., 2020), while CUD is associated with considerable impairment, as shown on a widely used functional impairment scale (Hasin et al., 2016), and CUD is also with multiple psychosocial and health problems (Gutkind et al., In Press). Cannabis use is also associated with other problems, including impaired driving (Dahlgren et al., 2020; Preuss et al., 2021; Sevigny, 2021), mental disorders (Hasin et al., 2016; Hines et al., 2020), hyperemesis syndrome (Perisetti et al., 2020) and cardiovascular events (Sun et al., 2020; Yang et al., 2021). Frequent adult cannabis use and related problems have increased in recent years (Brown et al., 2017; Chiu et al., 2021; Compton et al., 2016; Hasin et al., 2015). These increases are greater in states that legalized cannabis for medical or recreational use (Cerda et al., 2020; Chiu et al., 2021; Cook et al., 2020; Fink et al., 2020; Hasin et al., 2017). Determining the factors underlying these increases is an important public health priority.
One potential underlying factor is the potency of the products used. While cannabis is composed of many compounds, the potency of cannabis products is typically characterized by concentration of delta 9-tetrahydrocannabinol (THC), the major psychoactive compound (ElSohly et al., 2021; Radwan et al., 2021). Studies consistently show that on average, cannabis concentrates have substantially higher THC potency than plant/flower cannabis products (Daniulaityte et al., 2017; ElSohly et al., 2016; Mehmedic et al., 2010; Smart et al., 2017), including a recent meta-analysis of 12 studies conducted in 7 countries (Freeman et al., 2021). Further, while cannabis concentrates could theoretically contain predominantly cannabidiol (CBD) rather than THC, CBD products constituted only 5% of the cannabis market (BDS Analytics, 2019) as recently as 2017, most CBD products are not marketed as concentrates, and while CBD product use has increased since 2017, THC products remain the dominant product in the cannabis market (Research and Markets, 2021). Thus, reported use of a cannabis concentrate is very likely to involve use of a high-THC product. Cannabis products with higher THC concentrations (i.e., higher-potency products) are associated with greater risk of harms (Brunette et al., 2018; Chiu et al., 2021; Englund et al., 2017; Freeman and Winstock, 2015; Rigucci et al., 2016), including more rapid progression to first symptoms of CUD (Arterberry et al., 2019), CUD severity(Freeman and Winstock, 2015), anxiety disorders(Hines et al., 2020), psychotic disorders(Di Forti et al., 2015), and other cannabis-related problems (e.g., with memory (Freeman and Winstock, 2015; Hines et al., 2020), family or friends(Hines et al., 2020)). Although flower products remain the most commonly used, cannabis concentrates are increasing in popularity (Bidwell et al., 2021; Schaneman, 2021; Spindle et al., 2019). Thus, determining whether state cannabis legalization status is associated with use of cannabis concentrate products, with their high likelihood of having higher THC potency than plant/flower cannabis, is an important element in understanding the public health impact of changing cannabis laws.
Surprisingly little is known about adult likelihood of using a high-potency product by state cannabis legalization status, i.e., states with a recreational cannabis law (RCL), a medical cannabis law (MCL) or neither (no-CL). Instead, most studies examined RCL/MCL and route of administration (e.g., smoking vs. vaping). For example, in a 2014–2015 online national survey of cannabis users (Borodovsky et al., 2016), those in MCL states (but not RCL states) were more likely to report that they ever vaped cannabis than those in no-CL states. In a 2016 12-state survey (Schauer et al., 2020) (including 3 RCL states), living in a MCL or RCL state was not consistently associated with routes of administration. A 2020 US study of routes of administration showed that vaping was more likely in RCL and MCL states than in no-CL states (Shi, 2021). A 2018 study in Canada and the US (Goodman et al., 2020) did differentiate products used from routes of administration, showing that participants in US RCL states were more likely to vape plant cannabis than those in other US states, although they did not differ in their use of concentrates. However, this study grouped MCL states together with no-CL states. Because MCL and no-CL states have been shown to differ on many cannabis outcomes (Fink et al., 2020; Hasin et al., 2017; Martins et al., 2016; Mauro et al., 2019; Wen et al., 2015), grouping MCL with no-CL states may have obscured some distinctions. Finally, a Twitter-based survey found that those residing in RCL or MCL-only states were more likely than others to use cannabis concentrates (Daniulaityte et al., 2018). Thus, while studies suggest that MCL or RCL alter the likelihood of different routes of administration, only one study addressed whether living in RCL or MCL-only states affected the likelihood of using high-potency concentrate cannabis products. Because different Web-based platforms for survey recruitment can introduce differences in participant selection and characteristics (Daniulaityte et al., 2018), additional studies are needed about state cannabis legalization and use of high-potency cannabis products such as concentrates. Accordingly, we analyzed data from cannabis users in a large U.S. adult online sample recruited via Facebook to provide more information about the relationship of RCL, MCL and no-CL to adult use of high-potency cannabis products, i.e., those involving concentrates.
2. Methods
2.1. Recruitment and Sample
As described elsewhere (Borodovsky et al., 2020), adults age ≥18 years in the 50 U.S. states and Washington, D.C. (DC) were recruited to participate in an online survey between 08/14/2017 and 10/01/2017 via targeted Facebook social media advertisements (see Supplementary Appendix 1). The Dartmouth Committee for the Protection of Human Subjects approved the survey. Two different advertisement strategies were used to increase the proportion of cannabis users in the survey (Borodovsky et al., 2018). The first advertised a cannabis-specific research study without mentioning any incentive to recruit more frequent users. The second strategy advertised generic information about a research study and a chance to be randomly selected to win a $10 Amazon gift code upon survey completion to recruit less frequent users. Via a URL in the advertisement, potential participants were directed to an electronic consent page that briefly explained the study and confidentiality. After consenting, participants completed an anonymous questionnaire covering demographic characteristics, state and ZIP code of residence, and cannabis use behaviors. Of the original sample (Borodovsky et al., 2020), the present analytic subset included the 4,064 participants who used cannabis at least once in the prior 30 days, had complete information on control variables (2 were excluded due to incomplete information) and provided responses on routes of administration involving plant cannabis or concentrates.
2.2. Measures
2.2.1. State Cannabis Law Status
Our main predictors consisted of state cannabis laws at the time data were collected. Participants were asked their current state of residence, and effective state law status was coded based on whether legislation had gone into effect by the time of the survey in 2017. RCL and MCL enactment was determined by publicly available state legislative policies (Ballotpedia; Britannica ProCon, 2017; Marijuana Policy Project; National Organization for the Reform of Marijuana Laws; Prescription Drug Abuse Policy System, February 1 2017). Only states with laws permitting use of cannabis products containing THC for medical purposes were classified as MCL states; states with CBD-only laws were not considered MCL states. Note that all states with RCL also had MCL. Two variables were created to operationalize state law status. The first indicated the presence or absence of RCL: participants living in states with an RCL were coded as positive, and all others as negative. The second was a 3-level variable. Participants were categorized as living in a state with an RCL, living in a state with an MCL but no RCL (MCL-only), or living in a state without RCL or MCL (no-CL).
2.2.2. Classification of Cannabis Products Used
Initial survey questions on cannabis use covered lifetime use of particular cannabis products and their routes of administration (see Supplementary Appendix 2), including four categories: smoking; vaping plant material; vaping concentrates; and using concentrates with a dab rig, referred to hereafter as dabbing. Because the question on smoking did not specify that the product smoked was plant/flower, but smoking concentrates is a very atypical method of using them, we classified participants who endorsed smoking as users of plant/flower. Among all participants acknowledging lifetime use of smoking, vaping plant material, vaping concentrates, or dabbing concentrates, questions covered the frequency of their use within the past 30 days. For example, participants who endorsed lifetime smoking and lifetime vaping of concentrates were asked about the frequency of both smoking and vaping of concentrates within the past 30 days. The 30-day period was used to improve recall by covering a recent period. Endorsement of use of any concentrate in the prior 30 days, either by vaping or dabbing, was considered an indicator of high-potency use. Endorsement of any smoking or vaping of plant/flower was considered an indicator of low-potency use. All participants who had any use of concentrates (vaping or dabbing) in the prior 30 days were classified as users of high-potency products. All others were classified as users of low-potency products only.
We created variables for a sensitivity analysis designed to provide a more nuanced indicator of prior-month high-potency use by indicating the proportion of all use that was high-potency. For this, we constructed an outcome variable as follows. Frequency of any prior-month use was assessed by asking “How many days have you used cannabis (marijuana) in the past 30 days?”, with 8 response options: 0 days, 1–2 days, 3–5 days, 6–9 days, 10–19 days, 20–25 days, 26–29 days, or 30 days, assigned values of 0–7, respectively. Analogous questions assessed the frequency of vaping or dabbing concentrates. To calculate the proportion of participants’ total prior-month use that was high-potency, the frequency of high-potency use was divided by the frequency of any prior-month use. For example, a respondent with high-potency use for 3–5 days in the prior month (category 2), and any prior-month use of 20–25 days (category 5) was assigned a value of 2/5=0.4. The values of this variable could range from 0.0–1.0. Among participants reporting more frequent high-potency use than any prior-month use (n=59), the proportion of high-potency use was capped at 1.0.
2.2.3. Covariates
Individual-level sociodemographic control variables included age (18–20; 21–29; 30–44; 45–64; 65+), race/ethnicity (White; Black; Hispanic; other), gender (male; female; other), employment status (any full or part-time job; none), and education level (some high school or less; high school graduate or more). As in prior studies using these data (Borodovsky et al., 2020), advertising recruitment strategy was also included as a covariate. We also included a dichotomized age variable to explore the effect of being underage (i.e., age 18–20) vs. age 21 and older in sensitivity analyses.
State-level control variables created with 2017 U.S. census data from the American Community Survey provided by Geolytics (Geolytics, 2021) included gender (% of state population that was male); race/ethnicity (% non-Hispanic While); age (% aged <30 years); and urbanicity (state population density). Additional state-level control variables included % of population in poverty (United States Census Bureau, 2018); state unemployment rate, 2017 (United States Department of Labor, 2018); and percent used cannabis in the past month (average of 2016–2017 and 2017–2018 estimates from the National Survey on Drug Use and Health) (Substance Abuse and Mental Health Data Archive).
2.2.4. Analysis
After generating descriptive statistics of the sample characteristics, logistic regression was used to assess the association of state cannabis laws with use of high-potency cannabis products/concentrates by modeling the state law variables as predictors. Separate analyses were conducted for the 2-level RCL predictor (yes/no) and for the 3-level predictor (RCL, MCL-only, no-CL). Unadjusted models were run, and then models adjusted for the individual- and state-level control covariates, producing unadjusted odds ratios (OR) or adjusted odds ratios (aOR) and 95% confidence intervals (CI). For analyses involving the 3-level cannabis law predictor, to determine if the effects of RCL vs. no-CL and MCL-only vs. no-CL differed, contrasts were conducted using Wald tests. All analyses used SAS 9.4 software (SAS Institute Inc, Copyright © 2013).
In one sensitivity analysis, the proportion of use that was high-potency was analyzed as an alternative outcome. Since the proportional measure best fit the normal distribution, linear regression was used. Regression coefficients are reported, with 95% CIs, considered significant if not overlapping with 0. To determine if the effects of RCL vs. no-CL and MCL-only vs. no-CL differed, contrasts were conducted using F-tests.
In additional sensitivity analyses regarding age, we first removed all participants who were underage for legal use, i.e., age 18–20, and re-ran the analyses on the subset of remaining participants. Next, in models of CL effects in the full sample (all ages included), we added interaction (age 18–20 vs. 21 and older) by state law predictor terms in order to determine whether the state cannabis laws had significantly different effects in these age groups.
3. Results
3.1. Sample characteristics
Participants lived in all 50 states and Washington, D.C., with a range of 3 participants in D.C. to 442 participants in California (Figure 1). Of the sample (Table 1), 52.0% were male, 68.2% aged <30 years, 21.3% non-White, 54.2% unemployed, and 36.7% had high school education or less. Over a quarter (26.5%) resided in an RCL state, 41.1% in an MCL-only state, and 32.4% in a no-CL state. Nearly all (98.4%) reported using smoking or vaping plant cannabis (Table 2), with 96.9% reporting smoking and 29.1% reporting vaping. Use of concentrates was reported by 54.2%, with 44.9% reporting vaping concentrates, and 35.7% reporting dabbing. Of those using concentrates, the vast majority (97.2%) also reported using low-potency products. Prevalence of daily cannabis use was 40.3%, with 66.2% using 20 or more days a month.
Figure 1. Legal status of cannabis by state in 2017.
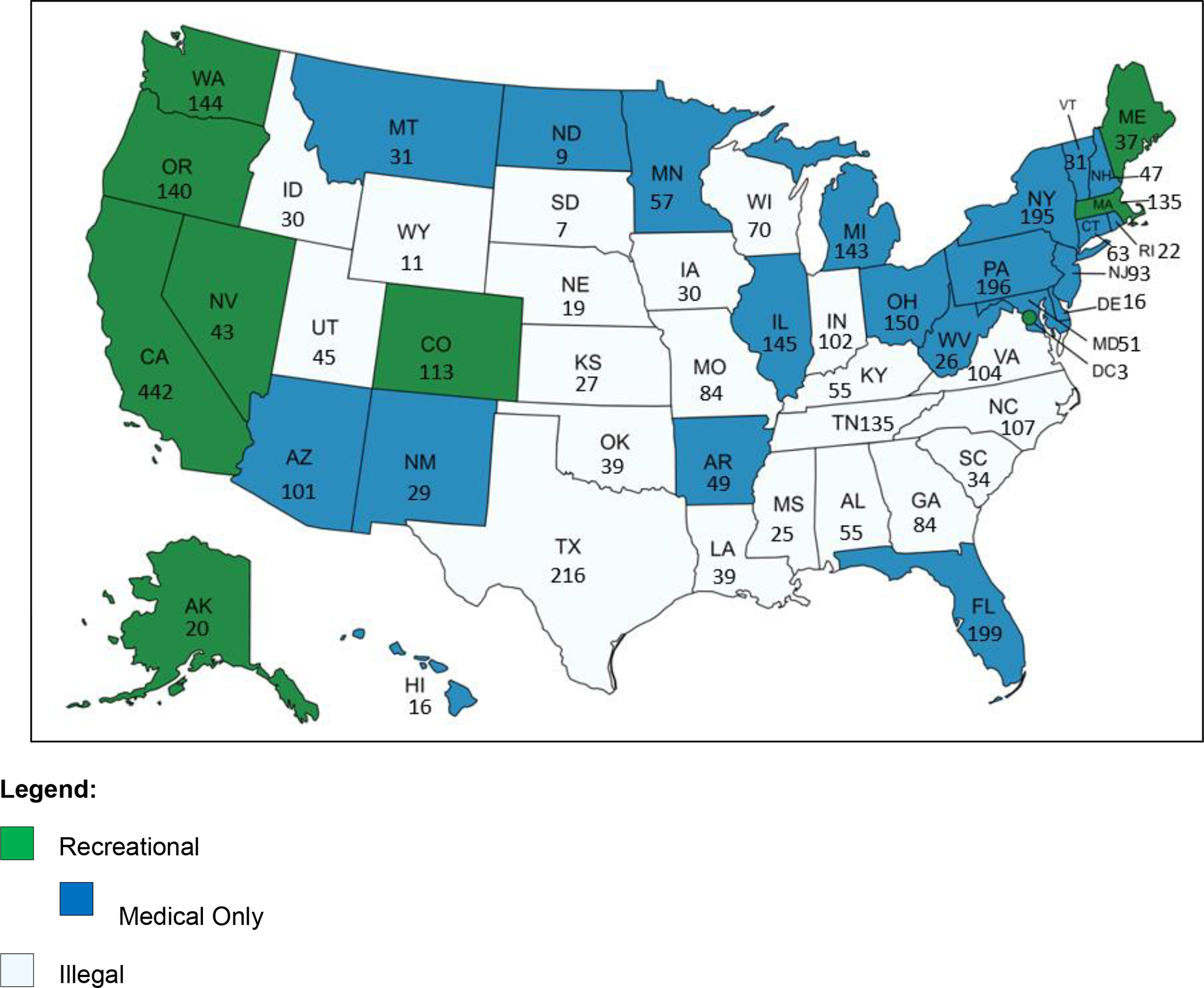
*Ns correspond to number of participants analyzed in that state.
Table 1.
Sample characteristics (N=4,064)
| n | % | |
|---|---|---|
| Sociodemographic | ||
| Age | ||
| 18–20 | 1,533 | 37.7 |
| 21–29 | 1,240 | 30.5 |
| 30–44 | 655 | 16.1 |
| 45–64 | 549 | 13.5 |
| 65+ | 87 | 2.1 |
| Gender | ||
| Male | 2,116 | 52.1 |
| Female | 1,874 | 46.1 |
| Other | 74 | 1.8 |
| Race/ethnicity | ||
| White | 3,201 | 78.8 |
| Black | 127 | 3.1 |
| Hispanic | 311 | 7.7 |
| Other | 425 | 10.5 |
| Employment | ||
| Any | 1,860 | 45.8 |
| None | 2,204 | 54.2 |
| Education | ||
| High school or less | 1,494 | 36.8 |
| More than high school | 2,570 | 63.2 |
| Advertising/recruitment strategy | ||
| Focused on non-frequent usersa | 1,032 | 25.4 |
| Focused on frequent usersb | 3,032 | 74.6 |
| State cannabis law status | ||
| Recreational cannabis law (RCL)c | 1,077 | 26.5 |
| Medical cannabis law (MCL-only)d | 1,669 | 41.1 |
| No cannabis law (no-CL) | 1,318 | 32.4 |
Generic advertisement to Facebook accounts of less-frequent cannabis users that incentivized survey completion with an online raffle for a $10 Amazon gift code.
Cannabis-specific advertisements directed to Facebook accounts of frequent cannabis users
Respondent was living in a state with a recreational cannabis law enacted by 2017: Alaska, California, Colorado, DC, Maine, Massachusetts, Nevada, Oregon, Washington. All these states also had an MCL enacted by 2017.
Respondent was living in a state with a medical cannabis law enacted by 2017: Arizona, Arkansas, Connecticut, Delaware, Florida, Hawaii, Illinois, Maryland, Michigan, Minnesota, Montana, New Hampshire, New Jersey, New Mexico, New York, North Dakota, Ohio, Pennsylvania, Rhode Island, Vermont, West Virginia
Table 2:
Characteristics of past-month cannabis use (N=4,064)
| Frequency of any past-month cannabis use | n | % |
|---|---|---|
| 1–2 days | 368 | 9.1 |
| 3–5 days | 292 | 7.2 |
| 6–9 days | 240 | 5.9 |
| 10–19 days | 472 | 11.6 |
| 20–25 days | 494 | 12.2 |
| 26–29 days | 559 | 13.8 |
| 30 days (daily) | 1,639 | 40.3 |
| Daily/near dailya | 2,198 | 54.1 |
| Frequentlyb | 2,692 | 66.2 |
| Frequency of smoking plant material | ||
| Daily | 1,396 | 34.4 |
| Daily/near dailya | 1,859 | 45.7 |
| Frequentlyb | 2,341 | 57.6 |
| Frequency of vaping plant material | ||
| Daily | 77 | 1.9 |
| Daily/near dailya | 109 | 2.7 |
| Frequentlyb | 165 | 4.1 |
| Frequency of vaping concentrates | ||
| Daily | 167 | 4.1 |
| Daily/near dailya | 227 | 5.6 |
| Frequentlyb | 358 | 8.8 |
| Frequency of dabbing concentrates | ||
| Daily | 170 | 4.2 |
| Daily/near dailya | 224 | 5.5 |
| Frequentlyb | 337 | 8.3 |
| Cannabis product potency and method of administration | ||
| Low-potency (plant material) | ||
| Vaping | 1,185 | 29.2 |
| Smoking | 3,939 | 96.9 |
| Any use of plant material | 3,999 | 98.4 |
| High-potency (concentrates) | ||
| Vaping | 1,825 | 44.9 |
| Dabbing | 1,451 | 35.7 |
| Any use of concentrates | 2,203 | 54.2 |
| Combined potency | ||
| Used high-potency concentrates only | 65 | 1.6 |
| Used both high and low potency products | 2,138 | 52.6 |
| Used low-potency plant products only | 1,861 | 45.8 |
26–30 days in the past month
20 or more days in the past month
3.2. State cannabis law status and high-potency use (Table 3)
Table 3.
Recreational cannabis laws (RCL), medical cannabis laws (MCL) and use of high-potency cannabis concentrate products in the past month (n=4,064)
| Participants with use of high-potency products | Odds ratio (95% CI) | ||
|---|---|---|---|
| 2-level cannabis law variable | % (SE) | Unadjusted | Adjusteda |
| RCLb | 65.9 (1.44) | 1.94 (1.68, 2.24) | 1.61 (1.22, 2.13) |
| No RCL | 50.0 (0.91) | reference | reference |
| 3-level cannabis law variable | |||
| RCLb | 65.9 (1.44) | 2.41 (2.04, 2.85) | 2.61 (1.77, 3.86) |
| MCL-onlyc | 54.3 (1.22) | 1.48 (1.28, 1.71) | 1.55 (1.21, 1.97) |
| No-CL (no RCL or MCL) | 44.5 (1.37) | reference | reference |
| Contrasts between RCL and MCL effects | Wald χ2 (dof=1), p-value | ||
| 36.38, <0.0001 | 13.24, 0.0003 | ||
CI=confidence interval; RCL=recreational cannabis law; MCL=medical cannabis law; dof = degrees of freedom
Adjusted for: individual-level (age, gender, race/ethnicity, employment, education, advertising strategy) and state-level (past month cannabis use, age, gender, race/ethnicity, unemployment, poverty, population density). oRs with 95% CI above 1 are significant at the p<0.05 level.
Respondent was living in a state with a recreational cannabis law (and medical cannabis law) enacted by 2017: Alaska, California, Colorado, DC, Maine, Massachusetts, Nevada, Oregon, Washington
Respondent was living in a state with a medical cannabis law enacted by 2017: Arizona, Arkansas, Connecticut, Delaware, Florida, Hawaii, Illinois, Maryland, Michigan, Minnesota, Montana, New Hampshire, New Jersey, New Mexico, New York, North Dakota, Ohio, Pennsylvania, Rhode Island, Vermont, West Virginia
Analysis of the 2-level cannabis law predictor indicated that compared to participants in states with no RCL, participants in RCL states had greater odds of using high-potency concentrates in unadjusted (OR=1.94; CI=1.68, 2.24) and adjusted models (aOR=1.61;CI=1.22, 2.13). Using the 3-level cannabis law predictor, compared to participants in no-CL states, participants in RCL states had greater odds of using high-potency concentrates in unadjusted (OR=2.41;CI=2.04, 2.85) and adjusted models (aOR=2.61;CI=1.77, 3.86) as did participants in MCL-only states in unadjusted (OR=1.48; 95% CI=1.28, 1.71) and adjusted models (aOR=1.55; CI=1.21, 1.97). Wald tests indicated that the RCL effect was stronger than the MCL-only effect (unadjusted: χ2= 36.38; p<0.0001; adjusted: χ2=13.24; p=0.0003), and compared to participants in MCL-only states, participants in RCL states had greater odds of using high-potency concentrates in unadjusted (OR=1.63;CI=1.39, 1.91) and adjusted models (aOR=1.69;CI=1.27, 2.42).
3.3. Sensitivity analyses
In models of the proportion of past 30-day use that involved use of high-potency concentrates (Table 4), analysis of the 2-level cannabis law predictor indicated that compared to participants in states with no RCL, the proportion of high-potency use was greater among participants in RCL states (adjusted beta=0.09, 95% CI=0.04, 0.13). In analysis of the 3-level cannabis law predictor, compared to participants in no-CL states, the proportion of high-potency use was greater among participants in RCL states (adjusted beta=0.16, 95% CI=0.09, 0.22) and greater among those in MCL-only states (adjusted beta=0.06, 95% CI=0.02, 0.10). F-tests showed that the effect of RCL was greater than MCL-only (f=16.74,p=<0.0001). The proportion of high-potency concentrate use was greater among participants in RCL states than in MCL-only states (adjusted beta=0.09, 95% CI=0.04, 0.14).
Table 4.
Recreational cannabis laws (RCL), medical cannabis laws (MCL) and proportion of all cannabis use in the past 30 days that was of high-potency cannabis concentrate products (n=4,064)
| Proportion of days used cannabis involving high potency usea, past 30 days | Regression coefficient (95% CI) | ||
|---|---|---|---|
| 2-level cannabis law variable | Mean (SE) | Unadjusted | Adjustedb |
| RCLc | 0.41 (0.01) | 0.15 (0.12, 0.17) | 0.09 (0.04, 0.13) |
| No RCL | 0.26 (0.01) | reference | reference |
| 3-level cannabis law variable | |||
| RCLc | 0.41 (0.01) | 0.19 (0.16, 0.22) | 0.16 (0.09, 0.22) |
| MCL-onlyd | 0.30 (0.01) | 0.07 (0.05, 0.10) | 0.06 (0.02, 0.10) |
| No-CL (no RCL or MCL) | 0.23 (0.01) | reference | reference |
| Contrasts between RCL and MCL effects | F-test (dof=1), p-value | ||
| 72.96, <0.0001 | 16.74, <0.0001 | ||
CI=confidence interval; RCL=recreational cannabis law; MCL=medical cannabis law; dof = degrees of freedom
Prior-month days of using a high-potency cannabis concentrate divided by prior-month days of any cannabis use
Adjusted for: individual-level (age, gender, race/ethnicity, employment, education, advertising strategy) and state-level (past month cannabis use, age, gender, race/ethnicity, unemployment, poverty, population density). Regression coefficients with 95% CI above 0 are significant at the p<0.05 level.
Respondent was living in a state with a recreational cannabis law (and medical cannabis law) enacted by 2017: Alaska, California, Colorado, DC, Maine, Massachusetts, Nevada, Oregon, Washington
Respondent was living in a state with a medical cannabis law enacted by 2017: Arizona, Arkansas, Connecticut, Delaware, Florida, Hawaii, Illinois, Maryland, Michigan, Minnesota, Montana, New Hampshire, New Jersey, New Mexico, New York, North Dakota, Ohio, Pennsylvania, Rhode Island, Vermont, West Virginia
Of the participants, 37.7% (n=1,533) were age 18–20 and 62.3% (n=2,531) were 21 years or older. Removing the participants who were age 18–20 had essentially no effect on the results (Supplementary Tables 1 and 2). There was no significant interaction between state law predictors and age (18–20 vs 21+) for any use of a high-potency cannabis concentrate product (Supplementary Table 3) or the proportion of cannabis use that involved high-potency concentrates (Supplementary Table 4), indicating that being underage did not modify the effects of the state cannabis laws.
4. Discussion
This study is the first to examine the relationship of state recreational cannabis laws (RCL) and medical cannabis laws (MCL-only) to the use of high-potency cannabis concentrate products in a large sample of cannabis users. Data were analyzed from 4,064 adult cannabis users age ≥18 years in the 50 U.S. states and D.C. who participated in a 2017 online survey. Study measures differeniated smoking, vaping plant material, vaping concentrates, and dabbing concentrates in the prior 30 days, with participants with any use of concentrates characterized as users of high-potency cannabis products. Overall, participants living in states with an RCL at the time of the survey were more likely than others to use high-potency cannabis concentrates, results that were robust to control for multiple individual- and state-level control covariates, including whether participants were underage (age 18–20) or not. Further, when participants in RCL states, MCL-only states, and states with no cannabis legalization (no-CL) were compared, participants in RCL as well as MCL-only states were more likely to use high-potency concentrates than those in no-CL states. Further, participants in RCL states were more likely to use high-potency concentrates than participants in MCL-only states.
Previous studies of adults suggested that legalization of cannabis use for medical or recreational purposes is associated with routes of administration, but few studies specified the products used and their potencies. Results were somewhat inconsistent. A Canadian/US study did not show a difference in use of concentrates between residents of RCL and other states (Goodman et al., 2020), but this study combined participants in MCL-only and no-CL states. A Twitter-based survey found that those in both RCL and MCL-only states were more likely than others to use cannabis concentrates (Daniulaityte et al., 2018). Our results are consistent with this latter study. The many studies showing differences between MCL and no-CL states on multiple cannabis outcomes (Fink et al., 2020; Hasin et al., 2017; Martins et al., 2016; Mauro et al., 2019; Wen et al., 2015) suggest the importance of continuing to differentiate MCL-only from no-CL states, and of conducting additional studies using a variety of sample designs.
Policy experts have speculated that the emergence of a legal cannabis retail market via RCLs would provide wider access to more potent cannabis products (Hall and Lynskey, 2020; Matheson and Le Foll, 2020), but noted current gaps in knowledge and the need for more studies (Hall et al., 2019). The present study takes a step in the direction of filling these gaps by exploring differences in high-potency cannabis use among those living in RCL, MCL and no-CL states.
In interpreting our results, an important consideration is that the associations are based on cross-sectional data from a single year (2017) and do not indicate the direction of effect (i.e., did state laws lead to high-potency use, or did increasingly common high-potency use within certain states lead to public support for RCL passage and enactment?). A more informative design would involve multiple years of data analyzed with difference-in-difference or synthetic control statistical methods. These would allow comparing pre-post change in prevalence of using high-potency products in states that changed their laws to contemporaneous changes in states that did not change their laws. Future studies should utilize such methods as data become available. In the meantime, the present study provides novel and important information on an issue that is highly salient to evaluating potential health effects of the rapidly changing legal status of cannabis in the U.S.
Studies have shown that individuals can partially titrate their THC exposure from higher-potency products by varying their cannabis self-administration behaviors to limit the dose to which they are exposed (Freeman et al., 2014; van der Pol et al., 2014). If such dose-reducing behaviors always occurred, this would reduce the public health relevance of state laws as a factor in state-level variation in use of high-potency products. However, such behaviors do not fully compensate for variation in THC concentrations, and therefore, greater THC concentrations deliver higher THC doses to the user (Freeman et al., 2021). Further, users of concentrates have been shown to select these products for reasons such as “stronger intoxication effect”, “effects last longer” and “fewer hits are necessary” (Loflin and Earleywine, 2014), suggesting that many concentrate users are not only exposed to higher doses of THC but in fact, deliberately seek out these products because of their potency. Given that high-potency products are associated with higher risk of cannabis-related harms, state-level factors associated with use of high-potency concentrates such as state cannabis laws are thus highly relevant to public health.
Potential mechanisms can be posited for both possible directions of effect for our findings. RCL could have led to increased use of high-potency concentrate use by stimulating growth of an active, commercialized industry that developed and marketed novel, high-potency cannabis products (Chiu et al., 2021; Hall and Lynskey, 2020; Hall et al., 2019). Such a mechanism is plausible since state RCLs have often been followed by a proliferation of online and retail outlets and dispensaries that make high-potency products more easily accessible (Smart et al., 2017) and possibly normalize their use, increasing their popularity with consumers. Even MCL-only in the absence of RCL may impact use of specific cannabis products through increased availability due to the proliferation of cannabis dispensaries (Borodovsky et al., 2017; Shi, 2021). Alternatively, the other direction of effect could be explained if a growing demand for high-potency types of cannabis within certain states prior to MCL or RCL (perhaps due to influences of informal social networks or social media) contributed to the likelihood of enacting MCL or RCL within those states, leading to a higher supply of these products to meet the demand. Additional data are needed to answer these questions.
Study limitations are noted. Participants came from an online sample recruited through two distinct social media advertisements and targeting strategies (Borodovsky et al., 2020). This permitted assembling a large sample efficiently at relatively low cost. However, the mechanics underlying algorithmically-based dissemination of social media advertisements are unclear, and thus the nature of the selection biases that produced this sample are also unclear. Note that the study was not designed or funded to produce a nationally representative sample, and its demographic distribution differed from that of a nationally representative sample of frequent cannabis users in 2017 (see Supplementary Table 5), e.g., our sample had greater representation of females and those age 18–20, but lower representation of Black, Hispanic, and employed persons. Findings should be interpreted accordingly. Additional limitations include that reasons for use of higher- and lower-potency products, where or how participants obtained them, or whether participants had received medical authorizations were not ascertained; future studies should do so. Further, we made the assumption that “smoking” involved the use of plant/flower products, since smoking concentrates is a very atypical way to use them, and we also assumed that use of concentrates represented use of high-potency THC products, because only 5% of the 2017 cannabis market consisted of CBD products25 and CBD products are typically not marketed as concentrates. Future studies should use questionnaires that carefully delineate what is smoked, and whether products used were primarily THC, primarily CBD, or some combination. In addition, the study did not ascertain further nuances in the state cannabis laws or their enactment, e.g., whether the states had retail stores in 2017, but future studies should address such issues. Finally, quantities of cannabis used were not assessed. Although our study was not focused on amounts of use, additional information on quantity could be useful. Measuring cannabis quantity accurately is challenging, especially in non-laboratory studies, but this is an important aspect of future cannabis research. Studies should implement improved, validated quantity measures as soon as they become available.
5. Conclusions
Use of highly potent cannabis products is rapidly gaining in popularity (Bidwell et al., 2021; Schaneman, 2021; Spindle et al., 2019), and our results suggest that use of such products is especially likely in RCL and MCL-only states. Because high-potency products are associated with greater risk of CUD and other harms, states and localities should consider this accumulating evidence when formulating laws, policies and public health messaging about the potency of permitted products. Policies to consider that may promote the sale and purchase of less-potent cannabis products include minimum unit pricing and taxes driven by potency rather than price (Caulkins et al., 2015; Shover and Humphreys, 2019; Smart et al., 2017). Clinicians in outpatient and emergency settings (Bollom et al., 2018) should be alert to these issues, especially in RCL states, regularly screening for potentially harmful cannabis products analogous to the screening for harmful or binge drinking that is now widely recommended (Heather, 2010; National Institute on Alcohol Abuse and Alcoholism, 2005). The increasingly common belief that cannabis is harmless may be based (at least partially) on assumptions arising from the weak, low-potency forms that were most commonly used in the 20th century. However, these beliefs may no longer be tenable given the increasing use of higher-potency forms. The U.S. is currently in a period of rapidly expanding public support for legalization of cannabis use, and additional states are likely to legalize recreational or medical cannabis use in the next few years. How these legal changes will affect the use of highly-potent forms of cannabis, their potential health harms and which policies will best promote public health requires careful ongoing public health research and monitoring.
Supplementary Material
Highlights.
The potency of cannabis products used (high-potency concentrates or low-potency plant/flower) was compared between adults living in U.S. states with recreational, medical or no cannabis laws (RCL, MCL, no-CL).
Adults in RCL and MCL states were more likely to use high-potency cannabis than those in no-CL states.
Adults in RCL states were more likely than those in MCL states to use high-potency cannabis.
Acknowledgments
Role of Funding Source
The funding organizations and sponsoring agencies had no further role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Funding:
Support acknowledged from R01DA R01DA048860, 1R01DA050032, T32DA031099, and the New York State Psychiatric Institute
Footnotes
Author Disclosures
Conflict of Interest
Dr. Alan Budney reports funding from NIDA as well as being a member of the Scientific Review Board of Canopy Growth and a consultant for Jazz Pharmaceuticals. All other authors of this manuscript have no conflicts of interest to report.
Declaration of Interests:
None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Arterberry BJ, Treloar Padovano H, Foster KT, Zucker RA, Hicks BM, 2019. Higher average potency across the United States is associated with progression to first cannabis use disorder symptom. Drug Alcohol Depend 195, 186–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballotpedia, Encyclopedia of American Politics.
- BDS Analytics, 2019. The Global Cannabinoids Market: Will CBD Overtake THC?
- Bidwell LC, Martin-Willett R, Karoly HC, 2021. Advancing the science on cannabis concentrates and behavioural health. Drug Alcohol Rev 40(6), 900–913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollom A, Austrie J, Hirsch W, Nee J, Friedlander D, Iturrino J, Ballou S, Lembo A, 2018. Emergency Department Burden of Nausea and Vomiting Associated With Cannabis Use Disorder: US Trends From 2006 to 2013. J Clin Gastroenterol 52(9), 778–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borodovsky JT, Crosier BS, Lee DC, Sargent JD, Budney AJ, 2016. Smoking, vaping, eating: Is legalization impacting the way people use cannabis? Int J Drug Policy 36, 141–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borodovsky JT, Lee DC, Crosier BS, Gabrielli JL, Sargent JD, Budney AJ, 2017. U.S. cannabis legalization and use of vaping and edible products among youth. Drug Alcohol Depend 177, 299–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borodovsky JT, Marsch LA, Budney AJ, 2018. Studying Cannabis Use Behaviors With Facebook and Web Surveys: Methods and Insights. JMIR Public Health Surveill 4(2), e48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borodovsky JT, Marsch LA, Scherer EA, Grucza RA, Hasin DS, Budney AJ, 2020. Perceived safety of cannabis intoxication predicts frequency of driving while intoxicated. Prev Med 131, 105956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britannica ProCon, 2017. Legal Recreational Marijuana States and DC.
- Brown QL, Sarvet AL, Shmulewitz D, Martins SS, Wall MM, Hasin DS, 2017. Trends in Marijuana Use Among Pregnant and Nonpregnant Reproductive-Aged Women, 2002–2014. JAMA 317(2), 207–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunette MF, Mueser KT, Babbin S, Meyer-Kalos P, Rosenheck R, Correll CU, Cather C, Robinson DG, Schooler NR, Penn DL, Addington J, Estroff SE, Gottlieb J, Glynn SM, Marcy P, Robinson J, Kane JM, 2018. Demographic and clinical correlates of substance use disorders in first episode psychosis. Schizophr Res 194, 4–12. [DOI] [PubMed] [Google Scholar]
- Caulkins JP, Kilmer B, Kleiman MAR, MacCoun RJ, Midgette G, Oglesby P, Pacula RL, Reuter P, 2015. Considering Marijuana Legalization: Insights for Vermont and Other Jurisdictions. RAND Corporation, Santa Monica, CA. [Google Scholar]
- Cerda M, Mauro C, Hamilton A, Levy NS, Santaella-Tenorio J, Hasin D, Wall MM, Keyes KM, Martins SS, 2020. Association Between Recreational Marijuana Legalization in the United States and Changes in Marijuana Use and Cannabis Use Disorder From 2008 to 2016. JAMA Psychiatry 77(2), 165–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu V, Leung J, Hall W, Stjepanovic D, Degenhardt L, 2021. Public health impacts to date of the legalisation of medical and recreational cannabis use in the USA. Neuropharmacology 193, 108610. [DOI] [PubMed] [Google Scholar]
- Compton WM, Han B, Jones CM, Blanco C, Hughes A, 2016. Marijuana use and use disorders in adults in the USA, 2002–14: analysis of annual cross-sectional surveys. Lancet Psychiatry 3(10), 954–964. [DOI] [PubMed] [Google Scholar]
- Cook AC, Leung G, Smith RA, 2020. Marijuana Decriminalization, Medical Marijuana Laws, and Fatal Traffic Crashes in US Cities, 2010–2017. Am J Public Health 110(3), 363–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahlgren MK, Sagar KA, Smith RT, Lambros AM, Kuppe MK, Gruber SA, 2020. Recreational cannabis use impairs driving performance in the absence of acute intoxication. Drug Alcohol Depend 208, 107771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniulaityte R, Lamy FR, Barratt M, Nahhas RW, Martins SS, Boyer EW, Sheth A, Carlson RG, 2017. Characterizing marijuana concentrate users: A web-based survey. Drug Alcohol Depend 178, 399–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniulaityte R, Zatreh MY, Lamy FR, Nahhas RW, Martins SS, Sheth A, Carlson RG, 2018. A Twitter-based survey on marijuana concentrate use. Drug Alcohol Depend 187, 155–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Forti M, Marconi A, Carra E, Fraietta S, Trotta A, Bonomo M, Bianconi F, Gardner-Sood P, O’Connor J, Russo M, Stilo SA, Marques TR, Mondelli V, Dazzan P, Pariante C, David AS, Gaughran F, Atakan Z, Iyegbe C, Powell J, Morgan C, Lynskey M, Murray RM, 2015. Proportion of patients in south London with first-episode psychosis attributable to use of high potency cannabis: a case-control study. Lancet Psychiatry 2(3), 233–238. [DOI] [PubMed] [Google Scholar]
- ElSohly MA, Chandra S, Radwan M, Majumdar CG, Church JC, 2021. A Comprehensive Review of Cannabis Potency in the United States in the Last Decade. Biol Psychiatry Cogn Neurosci Neuroimaging 6(6), 603–606. [DOI] [PubMed] [Google Scholar]
- ElSohly MA, Mehmedic Z, Foster S, Gon C, Chandra S, Church JC, 2016. Changes in Cannabis Potency Over the Last 2 Decades (1995–2014): Analysis of Current Data in the United States. Biol Psychiatry 79(7), 613–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Englund A, Freeman TP, Murray RM, McGuire P, 2017. Can we make cannabis safer? Lancet Psychiatry 4(8), 643–648. [DOI] [PubMed] [Google Scholar]
- Fink DS, Stohl M, Sarvet AL, Cerda M, Keyes KM, Hasin DS, 2020. Medical marijuana laws and driving under the influence of marijuana and alcohol. Addiction 115(10), 1944–1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman TP, Craft S, Wilson J, Stylianou S, ElSohly M, Di Forti M, Lynskey MT, 2021. Changes in delta-9-tetrahydrocannabinol (THC) and cannabidiol (CBD) concentrations in cannabis over time: systematic review and meta-analysis. Addiction 116(5), 1000–1010. [DOI] [PubMed] [Google Scholar]
- Freeman TP, Morgan CJ, Hindocha C, Schafer G, Das RK, Curran HV, 2014. Just say ‘know’: how do cannabinoid concentrations influence users’ estimates of cannabis potency and the amount they roll in joints? Addiction 109(10), 1686–1694. [DOI] [PubMed] [Google Scholar]
- Freeman TP, Winstock AR, 2015. Examining the profile of high-potency cannabis and its association with severity of cannabis dependence. Psychol Med 45(15), 3181–3189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geolytics, 2021. Estimates and Projections Variables
- Goodman S, Wadsworth E, Leos-Toro C, Hammond D, International Cannabis Policy Study t., 2020. Prevalence and forms of cannabis use in legal vs. illegal recreational cannabis markets. Int J Drug Policy 76, 102658. [DOI] [PubMed] [Google Scholar]
- Gutkind S, Fink D, Shmulewitz D, Stohl M, Hasin DS, In Press. Psychosocial and health problems associated with alcohol use disorder and cannabis use disorder in U.S. adults. Drug Alcohol Depend. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall W, Lynskey M, 2020. Assessing the public health impacts of legalizing recreational cannabis use: the US experience. World Psychiatry 19(2), 179–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall W, Stjepanovic D, Caulkins J, Lynskey M, Leung J, Campbell G, Degenhardt L, 2019. Public health implications of legalising the production and sale of cannabis for medicinal and recreational use. Lancet 394(10208), 1580–1590. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Kerridge BT, Saha TD, Huang B, Pickering R, Smith SM, Jung J, Zhang H, Grant BF, 2016. Prevalence and Correlates of DSM-5 Cannabis Use Disorder, 2012–2013: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions-III. Am J Psychiatry 173(6), 588–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Saha TD, Kerridge BT, Goldstein RB, Chou SP, Zhang H, Jung J, Pickering RP, Ruan WJ, Smith SM, Huang B, Grant BF, 2015. Prevalence of Marijuana Use Disorders in the United States Between 2001–2002 and 2012–2013. JAMA Psychiatry 72(12), 1235–1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Sarvet AL, Cerda M, Keyes KM, Stohl M, Galea S, Wall MM, 2017. US Adult Illicit Cannabis Use, Cannabis Use Disorder, and Medical Marijuana Laws: 1991–1992 to 2012–2013. JAMA Psychiatry 74(6), 579–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heather N, 2010. Breaking new ground in the study and practice of alcohol brief interventions. Drug Alcohol Rev 29(6), 584–588. [DOI] [PubMed] [Google Scholar]
- Hines LA, Freeman TP, Gage SH, Zammit S, Hickman M, Cannon M, Munafo M, MacLeod J, Heron J, 2020. Association of High-Potency Cannabis Use With Mental Health and Substance Use in Adolescence. JAMA Psychiatry 77(10), 1044–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung J, Chan GCK, Hides L, Hall WD, 2020. What is the prevalence and risk of cannabis use disorders among people who use cannabis? a systematic review and meta-analysis. Addict Behav 109, 106479. [DOI] [PubMed] [Google Scholar]
- Loflin M, Earleywine M, 2014. A new method of cannabis ingestion: the dangers of dabs? Addict Behav 39(10), 1430–1433. [DOI] [PubMed] [Google Scholar]
- Marijuana Policy Project.
- Martins SS, Mauro CM, Santaella-Tenorio J, Kim JH, Cerda M, Keyes KM, Hasin DS, Galea S, Wall M, 2016. State-level medical marijuana laws, marijuana use and perceived availability of marijuana among the general U.S. population. Drug Alcohol Depend 169, 26–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matheson J, Le Foll B, 2020. Cannabis Legalization and Acute Harm From High Potency Cannabis Products: A Narrative Review and Recommendations for Public Health. Front Psychiatry 11, 591979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mauro CM, Newswanger P, Santaella-Tenorio J, Mauro PM, Carliner H, Martins SS, 2019. Impact of Medical Marijuana Laws on State-Level Marijuana Use by Age and Gender, 2004–2013. Prev Sci 20(2), 205–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehmedic Z, Chandra S, Slade D, Denham H, Foster S, Patel AS, Ross SA, Khan IA, ElSohly MA, 2010. Potency trends of Delta9-THC and other cannabinoids in confiscated cannabis preparations from 1993 to 2008. J Forensic Sci 55(5), 1209–1217. [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism, 2005. A Pocket Guide For Alcohol Screening and Brief Intervention. [Google Scholar]
- National Organization for the Reform of Marijuana Laws.
- Perisetti A, Gajendran M, Dasari CS, Bansal P, Aziz M, Inamdar S, Tharian B, Goyal H, 2020. Cannabis hyperemesis syndrome: an update on the pathophysiology and management. Ann Gastroenterol 33(6), 571–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prescription Drug Abuse Policy System, February 1 2017. Medical Marijuana Laws for Patients. [Google Scholar]
- Preuss UW, Huestis MA, Schneider M, Hermann D, Lutz B, Hasan A, Kambeitz J, Wong JWM, Hoch E, 2021. Cannabis Use and Car Crashes: A Review. Front Psychiatry 12, 643315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radwan MM, Chandra S, Gul S, ElSohly MA, 2021. Cannabinoids, Phenolics, Terpenes and Alkaloids of Cannabis. Molecules 26(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Research and Markets, 2021. Global Cannabis Market by Application (Medical, Recreational), Product Type (Flowers, Concentrates), Compound (THC-dominant, CBD-dominant, Balanced THC & CBD), and Region (North America, South America, Europe, RoW) - Forecast to 2026.
- Rigucci S, Marques TR, Di Forti M, Taylor H, Dell’Acqua F, Mondelli V, Bonaccorso S, Simmons A, David AS, Girardi P, Pariante CM, Murray RM, Dazzan P, 2016. Effect of high-potency cannabis on corpus callosum microstructure. Psychol Med 46(4), 841–854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAS Institute Inc, Copyright © 2013. SAS® 9.4. Cary, NC. [Google Scholar]
- Schaneman B, 2021. Marijuana concentrate sales up 40% as more consumers turn to the product category. MJBizDaily. [Google Scholar]
- Schauer GL, Njai R, Grant-Lenzy AM, 2020. Modes of marijuana use - smoking, vaping, eating, and dabbing: Results from the 2016 BRFSS in 12 States. Drug Alcohol Depend 209, 107900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sevigny EL, 2021. Cannabis and driving ability. Curr Opin Psychol 38, 75–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi Y, 2021. Heterogeneities in administration methods among cannabis users by use purpose and state legalization status: findings from a nationally representative survey in the United States, 2020. Addiction 116(7), 1782–1793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shover CL, Humphreys K, 2019. Six policy lessons relevant to cannabis legalization. Am J Drug Alcohol Abuse 45(6), 698–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smart R, Caulkins JP, Kilmer B, Davenport S, Midgette G, 2017. Variation in cannabis potency and prices in a newly legal market: evidence from 30 million cannabis sales in Washington state. Addiction 112(12), 2167–2177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spindle TR, Bonn-Miller MO, Vandrey R, 2019. Changing landscape of cannabis: novel products, formulations, and methods of administration. Curr Opin Psychol 30, 98–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Data Archive, NSDUH State Estimates. [Google Scholar]
- Sun Y, Liu B, Wallace RB, Bao W, 2020. Association of Cannabis Use With All-Cause and Cause-Specific Mortality Among Younger- and Middle-Aged U.S. Adults. Am J Prev Med 59(6), 873–879. [DOI] [PubMed] [Google Scholar]
- United States Census Bureau, 2018. Income and Poverty in the United States: 2017.
- United States Department of Labor, 2018. REGIONAL AND STATE UNEMPLOYMENT — 2017 ANNUAL AVERAGES.
- van der Pol P, Liebregts N, Brunt T, van Amsterdam J, de Graaf R, Korf DJ, van den Brink W, van Laar M, 2014. Cross-sectional and prospective relation of cannabis potency, dosing and smoking behaviour with cannabis dependence: an ecological study. Addiction 109(7), 1101–1109. [DOI] [PubMed] [Google Scholar]
- Wen H, Hockenberry JM, Cummings JR, 2015. The effect of medical marijuana laws on adolescent and adult use of marijuana, alcohol, and other substances. J Health Econ 42, 64–80. [DOI] [PubMed] [Google Scholar]
- Yang PK, Odom EC, Patel R, Loustalot F, Coleman King S, 2021. Nonmedical Marijuana Use and Cardiovascular Events : A Systematic Review. Public Health Rep, 33354920988285. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


