Abstract
The University of Wisconsin Neighborhood Health Partnerships Program used electronic health record and influenza vaccination data to estimate COVID-19 relative mortality risk and potential barriers to vaccination in Wisconsin ZIP Code Tabulation Areas. Data visualization revealed four groupings to use in planning and prioritizing vaccine outreach and communication based on ZIP Code Tabulation Area characteristics. The program provided data, visualization, and guidance to health systems, health departments, nonprofits, and others to support planning targeted outreach approaches to increase COVID-19 vaccination uptake. (Am J Public Health. 2021;111(12):2111–2114. https://doi.org/10.2105/AJPH.2021.306524)
COVID-19 vaccine outreach is critical to overcoming barriers to vaccination. Vaccine hesitancy, including concerns about side effects and doubts about effectiveness,1 is persistent despite proven safety and efficacy among millions of people. Successful outreach requires understanding the characteristics, needs, and challenges of communities so that investments are targeted to promote rapid vaccination.
INTERVENTION
In December 2020, the University of Wisconsin Neighborhood Health Partnerships Program and Health Innovation Program partnered with the Wisconsin Collaborative for Healthcare Quality (WCHQ) to build an outreach prioritization tool, using electronic health record (EHR) and influenza vaccination uptake data to support community-level understanding of COVID-19 mortality risk and vaccination barriers. Throughout the pandemic, quantifying COVID-19 mortality risk by geographic area has been useful for planning and directing resources to vulnerable communities.2 The tool estimates relative mortality risk and potential barriers to vaccination for COVID-19 in Wisconsin ZIP Code Tabulation Areas (ZCTAs) and characterizes each ZCTA according to a rural–urban geodisparity model (see the supplemental material, available as a supplement to the online version of this article at http://www.ajph.org). Rather than a continuous score that assumes a rural disadvantaged area is the same as an urban disadvantaged area, this model accounts for differences in the sources of variation in and between rural and urban populations and goes beyond economic factors to incorporate information on health care capacity and health needs.
We calculated COVID-19 relative mortality risk using EHR data submitted to WCHQ by 22 health systems in June 2018. These data include 3.75 million patient records representing 65% of primary care providers in the state. We derived mortality risk using a model published in Nature Medicine3 that incorporated sociodemographic, behavioral, and health condition factors.
Potential barriers to COVID-19 vaccination include hesitancy, access, and trust in health care. We estimated these barriers by using ZCTA-level 2019–2020 seasonal influenza vaccination data from the Wisconsin Department of Health Services Immunization Registry. We divided each ZCTA’s influenza vaccination rate by the average rate for all ZCTAs to derive relative vaccination rates. Although there are distinctions between COVID-19 and influenza vaccination, influenza vaccination rates are a useful proxy to anticipate potential barriers to COVID-19 vaccination.4 A nationwide survey in June 2020 found that being previously vaccinated for influenza was a “potent predictor of intent to obtain a COVID-19 vaccine.”1(p1082)
PLACE AND TIME
We designed the tool in December 2020 and made it available via a public Web site in February 2021. We developed and validated it with experts in EHR and public health data and biostatistics. Before launch, staff at WCHQ, the Wisconsin Department of Health Services, and local health departments through the Wisconsin Public Health Research Network reviewed the tool.
PERSON
We directed the tool and guidance to decision makers from health systems, health departments, nonprofits, and other organizations.
PURPOSE
The purpose of the tool was to understand where and how to prioritize COVID-19 vaccination outreach efforts in Wisconsin communities.
IMPLEMENTATION
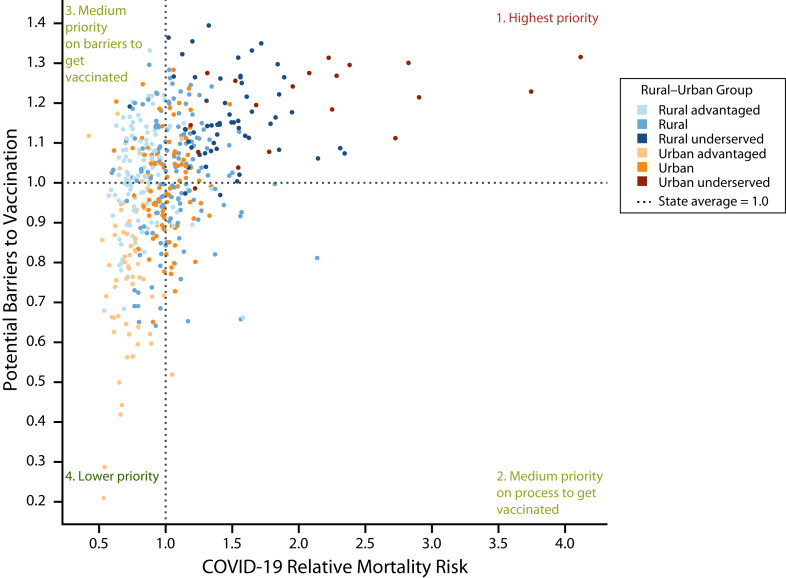
When we plotted the Wisconsin ZCTAs by COVID-19 relative mortality risk and potential barriers to vaccination, we identified four unique groupings of ZCTAs relative to state averages. These groupings (Figure 1; https://nhp.wisc.edu/covid-19) can be used to target and prioritize outreach investments; plan communication timing, volume, and channel; and develop messaging to increase vaccine uptake among ZCTA residents.
FIGURE 1—
COVID-19 Relative Mortality Risk and Barriers to Vaccination by Wisconsin ZIP Code Tabulation Area: February 2021
Group 1, “highest priority,” comprised 151 ZCTAs, representing 95% of underserved communities. They have the highest estimated COVID-19 relative mortality risk and highest barriers to vaccination. They would benefit from rapid vaccination and early targeting with the highest volume of communications from multiple channels and sources to overcome barriers while also making vaccination processes and timelines clear. Investing in partnerships with trusted organizations and individuals (e.g., churches, employers, and community organizations) may be a powerful action that builds trust and overcomes potential barriers in these communities.5
Group 2, “medium priority on process to get vaccinated,” comprised 60 ZCTAs, representing primarily rural and urban communities that are neither advantaged nor disadvantaged. They have higher than average COVID-19 relative mortality risk but lower than average barriers to vaccination. These communities should be vaccinated as quickly as possible but have fewer barriers and may require a more moderate volume of communications focusing primarily on vaccination processes.
Group 3, “medium priority on barriers to get vaccinated,” comprised 116 ZCTAs, representing 50% of rural advantaged communities. They have lower than average COVID-19 relative mortality risk but higher than average barriers to vaccination. Moderate communications addressing potential barriers could be beneficial, especially through partnerships with trusted individuals and organizations.
Group 4, “lower priority,” comprised 151 ZCTAs, representing 84% of urban advantaged communities. Their COVID-19 relative mortality risks and barriers to vaccination are both lower than average. These communities need basic communications on processes and timelines but may not require extra effort to motivate vaccination.
To disseminate the tool and guidance, we issued a press release and social media communications. The Wisconsin Public Health Research Network assisted in dissemination to local health departments. Two webinars and a downloadable toolkit with the webinar recording and materials were available at http://www.hipxchange.org/COVID-19VaccineOutreach.
EVALUATION
The two webinars had more than 150 attendees from various health systems, local and state health departments, community organizations, universities, and businesses. The Web site had 563 views in February 2021, which was a 54% increase in traffic compared with the previous six months. As of July 2021, there have been 1410 webinar views, and individuals from state, national, and international health organizations and universities have downloaded the toolkit.
Based on follow-up with webinar attendees, they used the tool to gain insights into populations served, plan programs supporting vaccine administration to vulnerable populations, and advocate community health workers’ involvement in vaccination education in high-mortality, high-barrier neighborhoods. We also supplied data to researchers and community organizations to support grant applications for COVID-19 vaccination and testing outreach.
In addition, the Wisconsin Department of Health Services recently released COVID-19 vaccination data at the ZCTA level. There was a strong correlation (0.81) between flu vaccination and receiving one or more doses of the COVID-19 vaccine.
ADVERSE EFFECTS
There were no adverse effects associated with the outreach prioritization tool, but there are some limitations to our tool. Not every person is reflected in the WCHQ data, so mortality risk for a ZCTA may be over- or underreported. Individuals with barriers to accessing health care are especially likely to be missing from the data. Only a single year of influenza vaccination data was available at the ZCTA level; data over several years could enhance understanding of potential barriers and trends related to vaccine uptake.
SUSTAINABILITY
The use of EHR data and seasonal influenza vaccination data could be applied to future vaccination campaigns to target those with the highest relative mortality risk from an infectious disease and higher barriers to vaccination. Other states with regional health improvement collaboratives could similarly use their data to inform public health decision making.
PUBLIC HEALTH SIGNIFICANCE
Communicating about new vaccines is challenging. Using local data to understand the characteristics of communities can inform targeting, message development, appropriate channels to maximize impact,6 and investment allocation. It may also provide a basis for collaboration and consistency in messaging across stakeholders (e.g., public health, health care, the press, community organizations) contributing to vaccine outreach and communications.
Increasing vaccine uptake is critical to saving lives and improving the social and economic conditions affected by the COVID-19 pandemic. There is also an opportunity to invest in underserved communities to increase trust in health officials, improve uptake of other vaccines, and benefit health beyond the scope of COVID-19.7
ACKNOWLEDGMENTS
The work reported in this article was funded through two Wisconsin Partnership Program grants (principal investigator: M. A. S.; principal investigator: J. M. W.). The project was supported by contributions from the University of Wisconsin Collaborative Center for Health Equity, the University of Wisconsin Population Health Institute, and the University of Wisconsin Health Innovation Program (HIP). HIP contributions were supported through the Wisconsin Partnership Program at the University of Wisconsin School of Medicine and Public Health and the Community–Academic Partnerships core of the University of Wisconsin Institute for Clinical and Translational Research through the National Center for Advancing Translational Sciences (grant UL1TR002373).
The authors would like to thank the members of the Accountable Care Organization Collaborative Working Group at HIP who provided support and direction throughout the data analysis process. The authors also thank the Wisconsin Department of Health Services for providing the seasonal influenza vaccination data.
Note. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare.
HUMAN PARTICIPANT PROTECTION
Institutional review board review was not required because the project does not constitute research as defined under 45 CFR 46.102(d). This project was certified as quality improvement through the University of Wisconsin-Madison Health Sciences institutional review board self-certification tool.
REFERENCES
- 1. Ruiz JB, Bell RA. Predictors of intention to vaccinate against COVID-19: results of a nationwide survey. Vaccine. . 2021;39(7):1080–1086. doi: 10.1016/j.vaccine.2021.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Smith CD, Mennis J. Incorporating geographic information science and technology in response to the COVID-19 pandemic. Prev Chronic Dis. . 2020;17:E58. doi: 10.5888/pcd17.200246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jin J, Agarwala N, Kundu P, et al. Individual and community-level risk for COVID-19 mortality in the United States. Nat Med. . 2021;27(2):264–269. doi: 10.1038/s41591-020-01191-8. [DOI] [PubMed] [Google Scholar]
- 4.Rouw A, Wexler A, Dawson L, Kates J, Artiga S.2020. https://www.kff.org/coronavirus-covid-19/issue-brief/state-variation-in-seasonal-flu-vaccination-implications-for-a-covid-19-vaccine
- 5.National Academies of Sciences Engineering and Medicine. Strategies for Building Confidence in the COVID-19 Vaccines. Washington, DC: National Academies Press; 2021. [DOI] [PubMed] [Google Scholar]
- 6. Quinn SC, Jamison AM, Freimuth V. Communicating effectively about emergency use authorization and vaccines in the COVID-19 pandemic. Am J Public Health. . 2021;111(3):355–358. doi: 10.2105/AJPH.2020.306036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ojikutu BO, Stephenson KE, Mayer KH, Emmons KM. Building trust in COVID-19 vaccines and beyond through authentic community investment. Am J Public Health. . 2021;111(3):366–368. doi: 10.2105/AJPH.2020.306087. [DOI] [PMC free article] [PubMed] [Google Scholar]