Abstract
The COVID-19 pandemic caused substantial disruptions in the field operations of all 3 major components of the Medical Expenditure Panel Survey (MEPS). The MEPS is widely used to study how policy changes and major shocks, such as the COVID-19 pandemic, affect insurance coverage, access, and preventive and other health care utilization and how these relate to population health.
We describe how the MEPS program successfully responded to these challenges by reengineering field operations, including survey modes, to complete data collection and maintain data release schedules. The impact of the pandemic on response rates varied considerably across the MEPS. Investigations to date show little effect on the quality of data collected. However, lower response rates may reduce the statistical precision of some estimates.
We also describe several enhancements made to the MEPS that will allow researchers to better understand the impact of the pandemic on US residents, employers, and the US health care system. (Am J Public Health. 2021;111(12):2157–2166. https://doi.org/10.2105/AJPH.2021.306534)
The Medical Expenditure Panel Survey (MEPS) is a family of large-scale federal health surveys conducted annually since 1996 by the Agency for Healthcare Research and Quality (AHRQ). The MEPS is widely used to study health care utilization and costs, health insurance coverage and premiums, access, and quality of health care in the United States.1–3 The MEPS-Household Component (MEPS-HC) collects detailed information on individuals in approximately 14 000 households through multiple rounds of in-person interviews. The MEPS-HC is closely linked to the National Health Interview Survey (NHIS), conducted annually by the National Center for Health Statistics, deriving its sample from the NHIS. The MEPS-HC provides less detail on health status and medical conditions than the NHIS but substantially greater detail on income, health insurance coverage, and, especially, health care utilization and spending, with information about every health care encounter and prescription drug fill for each household member over a 2-year period. This detail can be used to assess the consequences of health policy changes and major shocks, like the Great Recession and the COVID-19 pandemic, on health insurance coverage, access to care, patterns of preventive and other health care utilization, and how these all relate to population health. The MEPS-HC is also unique among major federal health surveys in collecting information on every household member to provide a more complete picture of the effects of policy changes and shocks on families.
The closely related MEPS-Medical Provider Component (MEPS-MPC) collects payment data from an annual sample of hospitals, doctors, home health agencies, and pharmacies that provided treatment to MEPS-HC households in the previous calendar year. It is designed to produce more detailed and accurate information on spending for health care encounters and prescription drug fills reported in the MEPS-HC than MEPS-HC respondents can typically provide. MEPS-MPC data are not separately released but instead are used as the principal source of expenditures in the person-level and event-level MEPS-HC calendar-year public use files (PUFs).
The MEPS-Insurance Component (MEPS-IC) is a separate, large-scale multimode (telephone, mail, Web) annual survey of more than 40 000 private-sector employers and more than 3000 state and local governments. The survey produces national and state-level estimates on topics such as health insurance offerings, enrollments, types of coverage, premium amounts, and employee out-of-pocket contributions in tabular format and in an annual chartbook.4
Field interviews for the MEPS-HC, MEPS-MPC, and MEPS-IC components are conducted, respectively, by Westat (www.westat.com), RTI International (www.rti.org), and the US Census Bureau (www.census.gov/programs-surveys/meps.html). AHRQ itself maintains a large, interdisciplinary staff of statisticians, economists, sociologists, and other researchers to provide overall direction for the MEPS, develop sampling strategies, design survey instruments, monitor data collection, develop and oversee data editing and imputation with contractors, perform quality control, and produce statistical reports. In keeping with recommendations of the National Academy of Sciences Committee on National Statistics,5 a robust intramural research program is an integral part of the MEPS program, with researchers involved in all aspects of survey work, in addition to producing peer-reviewed publications. AHRQ and the National Center for Health Statistics coordinate efforts on the MEPS and NHIS through the Department of Health and Human Services Data Council, which oversees surveys and other data collection efforts across the department. Additional information about the MEPS programs, including survey questionnaires, summary data tables, publications, and PUFs, can be found at https://www.meps.ahrq.gov/mepsweb.
The COVID-19 pandemic caused substantial disruptions in the field operations of all 3 MEPS components, as with all federal surveys. The countrywide shutdowns that began in mid-March 2020 led to the immediate suspension of all in-person and call center–based interviewing at the height of data collection. The MEPS program responded by reengineering, often radically, many aspects of field operations to complete data collection. We describe these disruptions and the program responses in detail for each of the MEPS components, including their effects on response rates and data quality. The challenges of conducting the MEPS during the COVID-19 pandemic also led to innovations in content, providing new opportunities for analyses. We describe these enhancements, including content specifically added to study the impact of the pandemic on the health care system, employers, and US residents.
FIELDING THE SURVEY DURING COVID-19
We outline how the MEPS program managed the disruptions in field operations caused by the COVID-19 pandemic in each of the 3 major components of the survey.
Household Component
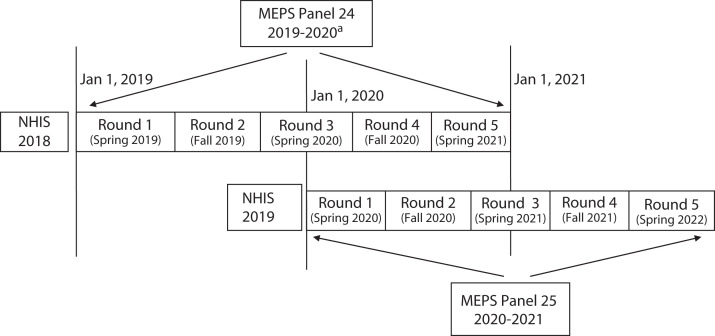
The MEPS-HC uses an overlapping panel design to make nationally representative estimates for the civilian, noninstitutionalized population. Each year, a new panel of households is drawn from a subsample of households responding to the NHIS and interviewed in person 5 times (“rounds”) using computer-assisted personal interviewing (CAPI) to collect 2 full calendar years of data. Normally, 2 overlapping panels are fielded at the same time and combined to make calendar-year estimates and PUFs (Figure 1). In the “spring” field period running from January to June 2020, 3 panels were fielded simultaneously: round 1 of the new panel—panel 25—which began that calendar year; round 3 of panel 24, which began the previous year; and round 5 of panel 23, which began 2 years previously. The round 5 reference period normally ends December 31 of the previous year.
FIGURE 1—
Overlapping Panel Design of the Medical Expenditure Panel Survey (MEPS)-Household Component: United States, 2019–2020
Note. NHIS = National Health Interview Survey. The figure depicts the standard 2-panel overlapping design of the MEPS used since 1996 and originally planned for the 2020 data collection year. Annually released full-year PUFs from 1997 through 2019 combine data from multiple rounds from each of 2 panels, as depicted. Subsequently, panel 23 was extended 4 additional rounds covering 2 additional calendar years, 2020 and 2021. As a result, the 2020 full-year PUFs will be composed of data from 3 panels (the Appendix and Figure A, available as supplements to the online version of this article at http://www.ajph.org, provide additional details).
aPanel 24 was subsequently extended 4 additional rounds covering 2 calendar years, 2021 and 2022 (the Appendix and Figure A provide additional details).
In response to the COVID-19 pandemic, Westat suspended all in-person field activities on March 17, 2020 (Box 1).6 The MEPS-HC field staff immediately pivoted to conducting remaining spring interviews entirely by telephone. Interviewers were already familiar with telephone-based interviewing procedures because a small percentage (6%–7%) of interviews were conducted by telephone in prior years.
BOX 1—
Medical Expenditure Panel Survey (MEPS) Data Collection Modes Before and After the COVID-19 Pandemic Hit, by Major Component
| MEPS Component | Usual Data Collection Mode | COVID-19 Data Collection Mode |
| MEPS-HC: nationally representative panel survey of households (5 rounds covering 2 calendar years each panel) with detailed demographic characteristics, health care utilization and spending, and health insurance coverage | Main instrument: in-person CAPI interviews | • Spring 2020: All telephone-based CAPI after March 17 • Fall 2020: almost all telephone-based CAPI interviewing; limited in-person interviews, some door-to-door contacts to schedule telephone interviews |
| Supplemental paper and pencil SAQs and other forms: interviewers collect during interview or returned by mail by respondent | • Spring 2020: respondents returned survey by mail only • Fall 2020: respondents returned survey mostly by mail, some pickup by field interviewers |
|
| MEPS-MPC: follow-back surveys of hospitals, office-based doctors, home health agencies, and pharmacies identified by MEPS-HC respondents where signed authorization forms were obtained | Call-center based CATI | Home-based telework CATI |
| Abstraction from hard copy medical and billing records in RTI call center and entered into CATI system | Home-based telework abstraction from electronic records or scanned from hard copy records received at call centers | |
| MEPS-IC: annual, nationally representative employer surveys of business locations and of state and local governments covering health insurance offerings, number of enrolled employees, and average health insurance premiums, copays and deductible amounts. | • Telephone (CATI) prescreener • Self-administered paper forms • Self-administered web form • Telephone (paper and CATI) follow-up • Personal visits • Respondents were offered a choice between mail (paper) response and web response. Most cases were sent paper forms with a link to the survey website. |
• Telephone (CATI) prescreener • Self-administered paper forms • Self-administered web form • Telephone (paper and CATI) follow-up • 2020 respondents were initially only offered web response. Once the survey processing facility (NPC) opened some survey form packages were mailed, completed and returned. No personal visits were conducted in 2020. |
Note. CAPI = computer-assisted personal interviewing; CATI = computer-assisted telephone interviewing; HC = Household Component; IC = insurance component; MPC = Medical Provider Component; NPC = US Census Bureau’s National Processing Center; RTI = RTI International; SAQ = self-administered questionnaires.
Before the suspension of in-person interviewing, 73% of round 5 interviews had been completed, and additional telephone-based interviewing achieved the usual high (98%) response rate (Table 1) conditional on households completing previous interviews. Respondents contacted for round 5 interviews previously participated in both the NHIS and 4 rounds of MEPS, so high levels of cooperation and ease of locating respondents were expected. A conditional response rate of 91% was achieved for round 3, with 35% of the interviews completed after the in-person field suspension. This was slightly lower than the usual 95% response rates for round 3. Because of the success in completing the round 3 and 5 interviews by telephone, the impact on the overall response rate for the 2019 full-year PUFs of the MEPS was minimal.
TABLE 1—
Survey Response Rates by Medical Expenditure Panel Survey (MEPS) Component and Data Collection Year: United States, 2018–2020
| MEPS Component | Data Collection Year | ||
| 2018 | 2019 | 2020 | |
| Conditional response ratea | |||
| MEPS-HC | |||
| Round 1 (spring) | 72.9 | 71.2 | 61.7 |
| Round 3 (spring) | 95.0 | 94.6 | 91.3 |
| Round 5 (spring) | 97.8 | 98.3 | 97.7 |
| Round 2 (fall) | 92.9 | 92.5 | 78.5 |
| Round 4 (fall) | 96.7 | 96.2 | 85.5 |
| Conditional response rateb | |||
| MEPS-MPCc | |||
| Hospital | 87.0 | 87.7 | 57.3 |
| Office-based doctors | 82.0 | 82.4 | 65.3 |
| Home health agencies | 85.0 | 84.9 | 80.2 |
| Noncorporate pharmacies | 84.8 | 83.3 | 65.8 |
| Corporate pharmacies | 86.1 | 89.2 | 80.7 |
| Unconditional response rated | |||
| MEPS-IC | |||
| Private sector | 67.8 | 59.2 | 56.3 |
| State and local governments | 83.0 | 82.1 | 75.2 |
Note. HC = Household Component; IC = Insurance Component; MPC = Medical Provider Component.
aThe round-specific household response rate is conditional on the household having responded previously to either the National Health Interview Survey (round 1) or previous MEPS-HC rounds (rounds 2–5; Table A, available as a supplement to the online version of this article at http://www.ajph.org, provides sample sizes).
bThe provider response rate is conditional on having signed the authorization form from the MEPS-HC sample member and case fielded in the MPC. The denominator for the response rate calculation is the unique combination of the provider and the MEPS sample person.
cMEPS-MPC collects data for health care encounters and prescription fills that occurred in the previous calendar year. Because of budget limitations, a stratified subsample of office-based doctors is fielded each year.
dThe response rate was calculated using unique private-sector establishments (a single firm may have multiple establishments) or unique state and local government entities.
By contrast, the round 1 response rate fell substantially below normal (Table 1). The greater drop in round 1 response rate was likely because of both greater difficulty in locating some respondents by telephone only and greater reluctance of new sample members to respond during the COVID-19 crisis. Response rates for the 2 rounds normally fielded during the fall MEPS-HC data collection (panel 25, round 2 and panel 24, round 4), which runs from July through December, also fell in 2020 (Table 1). As a result, the overall response rate in the 2020 full-year PUFs of the MEPS-HC is expected to be lower than in previous years.
The spring 2021 data collection (Figure A, available as a supplement to the online version of this article at http://www.ajph.org) proceeded mostly by telephone, with in-person interviewing limited to lower risk areas and where respondents and interviewers felt comfortable. Even in safer areas, interviewers mostly made contact in person to arrange a subsequent telephone interview. A greater proportion of interviews were conducted in person beginning in May 2021, with Westat planning to return to in-person interviewing in fall 2021.
Initial analyses found little evidence of nonresponse bias because of the drops in response rates, including the large drop in round 1. There were no differences in response rates by age, race/ethnicity, sex, and health status, but there were small differences by education in round 1. Standard reweighting procedures will account for this when producing the 2020 annual weights. The switch from in-person to telephone interviewing affected the conditional response rates of other key aspects of the MEPS-HC. Most importantly, at the end of the in-person interview, sample members (or their parents) complete authorization forms (AFs), allowing the MEPS-MPC contractor to contact providers and pharmacies to collect more complete payment and other information. The signed AFs are often just handed to the interviewer. Telephone-based interviewing precludes this simple route for distributing and collecting AFs. Consequently, Westat developed mail-based alternatives to distribute and collect the AFs from households,6 subsequently adding contactless in-person drop-offs to improve response rates. Supplemental self-administered questionnaires (SAQs) are also mailed to adult household members ahead of scheduled interviews during certain rounds. These are often collected by interviewers during in-person interviews. Again, the switch to telephone interviewing put more of the onus on MEPS-HC households, and response rates suffered accordingly. Because some forms are still being collected and receipted, final response rates for both the AFs and SAQs for 2020 are not yet available.
Medical Provider Component
The MEPS-MPC collects billing and medical record information for office-based doctors, hospitals, home health agencies, and pharmacies for MEPS-HC sample members with signed AFs. In 2020, the MEPS-MPC collected data for encounters that occurred in 2019. Before the pandemic, this work was conducted exclusively in call centers using a combination of computer-assisted telephone interviewing (CATI) and abstraction from hard copy records mailed, faxed, or sent electronically by providers (Box 1). Some data collection is completed entirely through telephone interviews. Mostly, however, initial telephone contacts request records, and data collection is completed through abstraction. The hospital records abstraction is particularly labor intensive and often requires subsequent telephone contacts. Abstractors generally complete hard copy summary sheets from the records they are abstracting, which are then entered into the CATI system.
RTI shut down all telephone and abstraction activities on March 17, 2020, in response to the pandemic, and the call centers remain closed.7 RTI developed new procedures for staff to complete the MEPS-MPC while teleworking through remote access to RTI systems. The more complicated issue was billing and medical record abstraction, which could not be completed by hard copy review in employees’ homes for logistical and confidentiality reasons. Instead, hard copy records were scanned by a few employees at the call center. Abstractors then electronically highlighted key information in PDF documents and then entered them into the CATI system. This electronic highlighting and abstraction proved more cumbersome than hard copy abstraction.
Historically, MEPS-MPC obtains high rates of cooperation from providers, but providers were also hard hit by the COVID-19 pandemic, further slowing production (Table 1). Many doctor offices temporarily closed, and some provider staff working from home could not immediately access records. Hospitals were especially overwhelmed, with staff simply not having time to respond. Although the MEPS-MPC data collection picked up considerably through the summer and fall 2020, response rates were still substantially lower in 2020 (Table 1). The final MEPS-MPC sample from 2020 (covering events that occurred in 2019) has proportionally fewer cases with Medicaid coverage compared with earlier years. However, this is accounted for in the expenditure editing and imputation processes and, in extensive reviews of the final 2019 MEPS expenditure estimates, no systematic biases were uncovered.
Insurance Component
The MEPS-IC collects information about health insurance offered by both private and nonfederal public sector employers. We focus discussion on the private sector, but data collection from governments is similar.
MEPS-IC data are collected and processed by the US Census Bureau in stages: research, telephone prescreener, mailout, personal visits, and telephone follow-up. After the 2020 sample was drawn from the US Census Bureau’s Business Register, research to update telephone numbers and other contact information was to commence. In mid-March 2020, the pandemic forced the closure of the Census Bureau telephone centers, and the research operation was canceled. After a delay, the Census Bureau distributed laptops to their analysts, enabling them to complete research from home (April 2020–June 2020).8
The brief telephone prescreener calls (June 2020–August 2020)8 to determine whether a business offered health insurance to its employees were similarly conducted from home. If the business did not offer insurance, characteristics of the business were collected, and the survey ended. To facilitate communication with businesses operating remotely, interviewers collected e-mail addresses for future contacts with businesses that offered insurance.
From June through October, businesses that offered insurance or did not respond to the prescreener would typically be mailed an advanced letter and would subsequently receive survey forms along with a letter indicating an option to respond via the Web.8 Because of COVID-19, the Census Bureau’s National Processing Center was temporarily closed on March 18, 2020 and was unable to mail hard copy forms. By early May, automated processes were available that allowed the National Processing Center to mail advance letters notifying businesses of their inclusion in the survey and asking them to respond by Web. A similar “eBlast” e-mail was also sent to businesses. Later in the summer, the National Processing Center was finally able to mail some survey forms. However, emphasis in data collection shifted from a choice of paper or Web to primarily Web.
Personal visits (normally conducted August–December)8 were canceled because of COVID-19. These visits are expensive and reserved for the largest nonresponders. Although the response rate for the largest employers was higher in 2020 compared to 2019, it might have been even higher had personal visits not been eliminated. The final response rate for the largest employers was still substantially below the rates of 2018 and earlier years.
The telephone follow-up operation, normally fielded from September 2020 through February 2021, was extended several weeks to compensate for lower response rates to the prescreener and e-mails.8 The combined mitigation efforts resulted in a surprisingly small drop in the private-sector response rate from 59.2% in 2019 to 56.3% in 2020 (Table 1).
NEW SURVEY CONTENT
We describe the new content added to the MEPS in direct response to the disruptions in the field operations, as well as new MEPS content relevant for understanding the effects of the COVID-19 pandemic.
Longer Panels
Because of the substantial drop in round 1 response rates in 2020 and the anticipated effects of similar drops in the NHIS response rates on the MEPS-HC, Westat proposed extending data collection for the panel that was originally scheduled to rotate out of the survey after the round 5 interviews (panel 23, which started in 2018). Westat rapidly developed and tested a round 6 instrument that could be fielded in fall 2020. Because of the high likelihood that the COVID-19 pandemic would continue to limit in-person field operations and concerns about response rates in newer panels, AHRQ subsequently decided to extend the MEPS panels that began in 2018 (panel 23) and 2019 (panel 24) to 4 full years of data collection instead of the normal 2, budget permitting (Figure A and the Appendix provide additional details, available as supplements to the online version of this article at http://www.ajph.org). These extended panels have the dual benefits of increasing MEPS-HC sample sizes and allowing entirely new analyses to take advantage of the longer panels. Because data were collected for these panels before the COVID-19 pandemic, these extended panels will be particularly important for studying the consequences of the pandemic, including longer-run effects on health care utilization and the health of US residents.
Telehealth Visits
Many hospitals, doctor offices, and other health care providers transitioned to deliver some or all health care virtually by telephone or Internet in response to the pandemic even before the countrywide shutdowns in mid-March 2020. Supporting this move to telehealth-based care, Medicare, Medicaid, and most private insurers substantially relaxed previously tight restrictions on payment for telehealth visits,9,10 but the MEPS-HC instrument had not previously explicitly probed respondents on telehealth visits. For 2020, interviewers were prompted to probe for visits that occurred by telephone or video (the Appendix provides additional details). Starting with 2021 interviews, the event reporting modules in the MEPS were substantially redesigned to include better probes for telehealth encounters and allow explicit identification of telehealth visits, including mode (telephone, video, or other). Data on these telehealth visits will be available beginning with the 2020 full-year PUFs for the MEPS-HC (Appendix).
COVID-19–Specific Content
Three questions were added to the MEPS-HC instrument for the fall 2020, spring 2021, and fall 2021 interviews that asked whether any medical care, dental care, or prescription drugs were delayed “because of the coronavirus pandemic.” Beginning in fall 2021, MEPS-HC respondents will also be asked whether each person in the household had received a COVID-19 vaccination.
Two new questions were added to the 2021 MEPS-IC survey to further measure the consequences of the pandemic. The first asks about the teleworking capabilities of the employer’s staff. The second asks employers if their business had a net increase or net decrease in the number of employees because of the pandemic. The MEPS-IC is pretesting additional questions about incentives employers offered to employees to receive COVID-19 vaccinations and the impact of the pandemic on employers and employees.
Other Content
A new Social and Health Experiences SAQ was fielded in spring 2021 through a budget supplement for the MEPS-HC. A Web option was provided and strongly encouraged to improve response rates. The questionnaire asks each adult about social and behavioral determinants of health, including housing security, quality and affordability, food security, transportation challenges, general well-being, family and community support, personal safety, and adverse circumstances during childhood. This SAQ was planned long before the COVID-19 pandemic but will provide additional context for understanding the effect of the pandemic and how it varied across the population. Likewise, the main MEPS-HC instruments for 2020 and 2021 contain a US Department of Agriculture–funded supplement on food security that was previously included in the 2016 and 2017 MEPS.
DATA QUALITY COLLECTED ON THE COVID-19 PANDEMIC
Initial investigations of the effects of COVID-19 on data quality focused on MEPS-HC reports of health care utilization for 2 main reasons. First, household reports of every office-based visit, hospital stay or visit, home health, prescription drug fill, and all other health care utilization serve as the basic building blocks of expenditure estimates, the most important domain in the MEPS-HC.
Second, reporting of health care events may be particularly sensitive to a switch from in-person to telephone-based interviews. The process of eliciting all health care encounters and prescription drugs and recording details—including dates, health care conditions associated with visits or medications, and payment details—is complex. To speed this process and improve recall, MEPS-HC respondents are encouraged to keep records and have them available during interviews. These records include bills, explanation of benefit forms, pill bottles, and special calendars to record the dates of all visits. Past validation studies demonstrate a strong correlation between use of records and the quality of MEPS-HC reports.11–14 Telephone-based interviewing likely makes using these records during interviews more cumbersome. For example, the respondent cannot simply hand a pill bottle to the interviewer to record an unusual or complicated drug name. Respondents may also be more reluctant to collect or use records during a telephone-based interview or may not have had access to them because of the pandemic.6 Indeed, there is evidence that use of records declined overall.6
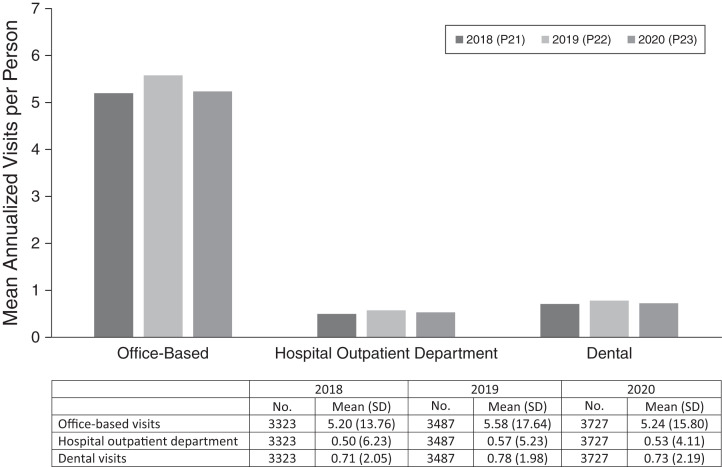
We examined whether the switch from in-person to telephone-based interviewing affected the quality of health care utilization data by comparing the number of visits reported in interviews conducted exclusively by telephone after March 17, 2020, to interviews conducted by standard MEPS procedures after March 17 of the 2 previous spring interview cycles. Figure 2 compares the mean number of visits reported in the spring 2020, round 5 interviews conducted after March 17 to round 5 interviews conducted after March 17 the 2 previous years. The round 5 reference period ends on December 31, 2019, for the spring 2020 interviews, so the pandemic should not affect actual health care utilization. We found that the mean annualized number of office-based visits, visits to hospital outpatient departments, and dental visits were all comparable across all 3 years with no statistically significant differences. We similarly found no evidence of a mode effect in the switch from in-person to strictly telephone-based interviewing in rounds 1 and 3 and in multivariable regression models of all 3 rounds (see Appendix for additional details). Separate analyses performed by the MEPS-HC contractor, Westat, confirm these results.6 In separate assessments, AHRQ and RTI found that the quality of the payment data collected in the MEPS-MPC in 2020 was like previous years (Appendix).
FIGURE 2—
Household Reporting of Pre–COVID-19 Visits in Medical Expenditure Panel Survey (MEPS)-Household Component Round 5 Interviews Conducted After March 17 by Data Collection Year: United States, 2018–2020
Note. The figure represents the authors’ analyses of confidential MEPS-household component files. Usual reference period is from the date of round 4 interview to December 31 of the year before round 5 data collection. Adjusted Wald test of 2020 vs 2019 means: P = .50 office-based; P = .78 hospital outpatient department; P = .39 dental visits. Visits were annualized to account for slightly unequal average.
Our evaluations of both household reports of health care utilization and the quality of payment data from the MEPS-MPC are encouraging. However, challenges remain. In particular, the lower response rates in the MEPS-MPC (Table 1) mean that fewer events and prescription drugs reported by MEPS-HC households for 2019 have complete payment information available from providers. As a result, more payment data must be imputed, reducing the accuracy of MEPS-HC 2019 expenditure variables and estimates released in 2021. RTI reports that the 2021 data collection is going more smoothly, with higher response rates than in 2020. However, because of the challenges of collecting the necessary AFs from MEPS-HC sample members, the number of providers RTI can contact is smaller than in past years. Thus, there will again be fewer events with complete payment data available from the MEPS-MPC, and more imputation will likely occur in the 2020 PUFs of the MEPS-HC.
Investigation of the quality of reporting in these and all other domains of the MEPS is ongoing (see Appendix for more details).
CONCLUSIONS
The COVID-19 pandemic created and continues to create many challenges for the MEPS program. Our contractors and partners worked creatively to revamp field operations in each of the main MEPS components by switching data collection modes, staffing operations with teleworkers, or both. That they were able to achieve the response rates they did during 2020 and maintain the data release schedules for data already collected is a testament to their hard work and dedication. We have also been encouraged by the quality of the data obtained despite substantial changes in data collection. At the same time, the statistical precision of some estimates may be reduced because of lower response rates in 2020 than in previous years, which continued in 2021. Of particular concern, the difficulties created by the pandemic increased the amount of imputation that was required to produce the expenditure variables in the 2019 full-year PUFs of the MEPS-HC and will do so again in the 2020 PUFs. AHRQ and its contractors are continuing intensive efforts to assess the quality of MEPS data collected during the pandemic using both qualitative and quantitative methods and to develop any necessary mitigation strategies for producing PUFs and other products.
The challenges of collecting data during the pandemic have also accelerated work on developing new methods and technologies for the MEPS of households, providers, and employers. For example, the MEPS-HC contractor is working on a system of collecting AFs electronically with electronic signatures to improve AF response rates whether MEPS-HC interviews are conducted in person or by telephone. Similarly, the MEPS is expanding the use of machine-learning methods to automate portions of the labor-intensive record abstraction in each of its surveys. The encouraging results of our analyses of the quality of MEPS-HC data collected through less costly telephone interviews opens new possibilities for extending MEPS panels on an ongoing basis. We are also examining whether additional portions of the MEPS-HC can be moved to the Web. A major lesson of the pandemic is that the MEPS, like other federal surveys, must become more flexible to better anticipate and respond to similar challenges in the future, while maintaining its core strengths that justify a continued large public investment.
Since its inception in 1996, the MEPS has been used in a wide range of economic, health services research, clinical, and public health studies, including those published in AJPH.15–19 The MEPS is designed to support in-depth analyses of how socioeconomic characteristics, health insurance coverage, access to care, patterns of preventive and other health care utilization and spending, and population health all relate to one another. Meeting the challenges of the COVID-19 pandemic has created additional opportunities for analyses using the MEPS. We are particularly excited about the possibilities created by the planned 4-year panels. The 2-year duration in all previous panels of the MEPS-HC constrains both the topics that can be studied and the statistical methods that can be successfully applied to the MEPS-HC. In particular, the longer panels support examining the longer-run impacts of policy changes and shocks on access, health care utilization, health behaviors, and health of individuals and families and thus will allow analyses of sample members before, during, and after the COVID-19 pandemic.
Explicitly adding telehealth events to the MEPS-HC is also long overdue and particularly important for understanding health care utilization during the pandemic. Finally, the new COVID-19 questions and other new content in conjunction with the extended panels will greatly enhance the ability of the MEPS to study the consequences of the COVID-19 pandemic on US residents, their employers, and the health care system.
ACKNOWLEDGMENTS
We wish to thank Joel Cohen, Karen Davis, Kathryn Dowd, Steven Hill, Ed Miller, Erica Saleksa, Marie Stagnitti, Jeffrey Rhoades, and Peter Tice for their many helpful comments and suggestions. We also wish to thank the staff of Westat, RTI International, and the US Census Bureau for their hard work and dedication to the Medical Expenditure Panel Survey throughout the COVID-19 pandemic and for providing us with data and information used within.
Note. The views expressed in this article are those of the authors, and no official endorsement by the Agency for Healthcare Research and Quality or the US Department of Health and Human Services is intended or should be inferred.
CONFLICTS OF INTEREST
The authors report no conflicts of interest.
HUMAN PARTICIPANT PROTECTION
All analyses were conducted under the protocol “Secondary Analysis of Confidential Data from the Medical Expenditure Panel Survey” (CRRI 0504015) and approved by the Advarra institutional review board.
Footnotes
See also Lau et al., p. 2085.
REFERENCES
- 1.Weil A.2015. https://www.healthaffairs.org/do/10.1377/hblog20151015.051225/full
- 2. Cohen SB, Cohen JW. The capacity of the Medical Expenditure Panel Survey to inform the Affordable Care Act. Inquiry. . 2013;50(2):124–134. doi: 10.1177/0046958013513678. [DOI] [PubMed] [Google Scholar]
- 3. Cohen JW, Cohen SB, Banthin JS. The Medical Expenditure Panel Survey: a national information resource to support healthcare cost research and inform policy and practice. Med Care. . 2009;47(7 supp 1):S44–S50. doi: 10.1097/MLR.0b013e3181a23e3a. [DOI] [PubMed] [Google Scholar]
- 4.Agency for Healthcare Research and Quality. MEPS insurance component chartbook. 2020. https://www.meps.ahrq.gov/data_files/publications/cb24/cb24.pdf
- 5.National Academies of Sciences, Engineering, and Medicine. Principles and Practices for a Federal Statistical Agency. 7th ed. Washington, DC: National Academies Press; 2021. [DOI] [PubMed] [Google Scholar]
- 6.Westat. MEPS COVID-19 Data Quality Report. Contract# HHSA-290-2016-00004I. Task Order# 75Q80119F32016, Deliverable # 1A.01 Final Report. Rockville, MD: Westat; 2021. [Google Scholar]
- 7.Dowd D, Saleska E, Bell S, et al. 2021.
- 8.Livesay M, Tarsia B, Winder S, Davis K.2021.
- 9.US Department of Health and Human Services. 2020. https://www.hhs.gov/coronavirus/telehealth/index.html#waivers [DOI] [PubMed]
- 10. Patel SY, Mehrotra A, Huskamp HA, Uscher-Pines L, Ganguli I, Barnett ML. Variation in telemedicine use and outpatient care during the COVID-19 pandemic in the United States. Health Aff (Millwood). . 2021;40(2):349–358. doi: 10.1377/hlthaff.2020.01786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zuvekas S, Biener A, Hicks W. The effects of survey enhancements on the quality of reporting in the Medical Expenditure Panel Survey, 2008–2015. J Surv Stat Methodol. . 2020;8(3):589–616. doi: 10.1093/jssam/smz014. [DOI] [Google Scholar]
- 12. Zuvekas SH. The effects of recall length and reporting aids on household reporting of health care events in the Medical Expenditure Panel Survey. J Econ Soc Meas. . 2011;36(4):321–343. doi: 10.3233/JEM-2011-0348. [DOI] [Google Scholar]
- 13. Hill SC, Zuvekas SH, Zodet MW. Implications of the accuracy of MEPS prescription drug data for health services research. Inquiry. . 2011;48(3):242–259. doi: 10.5034/inquiryjrnl_48.03.04. [DOI] [PubMed] [Google Scholar]
- 14.Kashihara D, Wobus D.2021. http://www.asasrms.org/Proceedings/y2007/Files/JSM2007-000563.pdf
- 15. Bachhuber MA, Hennessy S, Cunningham CO, Starrels JL. Increasing benzodiazepine prescriptions and overdose mortality in the United States, 1996–2013. Am J Public Health. . 2016;106(4):686–688. doi: 10.2105/AJPH.2016.303061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Caldwell JT, Ford CL, Wallace SP, Wang MC, Lois M, Takahashi LM. Intersection of living in a rural versus urban area and race/ethnicity in explaining access to health care in the United States. Am J Public Health. . 2016;106(8):1463–1469. doi: 10.2105/AJPH.2016.303212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Aldridge MD, Kelley AS. The myth regarding the high cost of end-of-life care. Am J Public Health. . 2015;105(12):2411–2415. doi: 10.2105/AJPH.2015.302889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Abdus S, Mistry KB, Selden TM. Racial and ethnic disparities in services and the Patient Protection and Affordable Care Act. Am J Public Health. . 2015;105(suppl 5):S668–S675. doi: 10.2105/AJPH.2015.302892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lau DT, Kirby JB. The relationship between living arrangement and preventive care use among community-dwelling elderly persons. Am J Public Health. . 2009;99(7):1315–1321. doi: 10.2105/AJPH.2008.151142. [DOI] [PMC free article] [PubMed] [Google Scholar]