Abstract
Background:
A majority of surgical patients are prescribed opioids for pain management. Many patients have pre-existing chronic pain managed with opioids and/or opioid use disorders (OUD) which can complicate peri-operative management. Patients who use opioids prior to surgery are at increased risk of developing OUD after surgery. To date, no studies have examined the prevalence of opioid screening and electronic medical record (EMR) documentation prior to surgery.
Materials and methods:
A 40-item survey was administered to 268 patients at their first post-operative care visit at a single tertiary academic center from October 2017–July 2018. A chart review of a random sample of 100 patients was performed to determine provider opioid screening prevalence in the pre-surgical setting. Log-binomial models were used to calculate prevalence ratios (PR) to determine provider role (surgeon, advanced practice clinicians, surgical trainee) association with opioid screening documentation. Exploratory qualitative interviews were conducted with surgical providers to identify barriers to screening and screening documentation.
Results:
Only 7% of patients were screened preoperatively for opioid use. A total of 38% of patients self-reported that they had used opioids in the past year. Of that group, only 3% had screening by a surgical provider prior to surgery documented in their EMR. Provider role was not associated with likelihood of opioid screening (surgeon versus trainee, PR =1.2, 95% CI 0.2–8.5) (surgeons versus APCs, PR=1.05, 95% CI 0.17–8.53). EMRs were discordant with patient survey results for patients with no ICD-10 codes for opioid use. The most common perceived barriers to pre-operative screening were insufficient clinic time; logistics of who should screen/not required as part of their clinical workflow; not perceiving screening as a priority; and lack of expertise in the area of chronic opioid use and OUD.
Conclusion:
Pre-operative screening for opioid use is uncommon and EMRs are often discordant with patient self-reported use. Efforts to increase pre-operative screening will need to address barriers screening practices and increasing health system support by incorporating screening into the clinical workflow and adding it to documentation templates.
Keywords: Opioids, screening, education, prescribing providers
Introduction
Surgeons commonly prescribe opioids for pain management after surgery and account for at least 10% of all opioids prescribed in the United States (US)1. The prescribing practices of surgeons have been under scrutiny as nearly 100 million Americans undergo surgery each year1. Prior studies have shown over-prescribing of opioids among surgical patients is common2–6. An estimated 3–11% of opioid-naïve patients who use opioids after surgery will transition to chronic use and this risk is even higher in patients with prior or existing opioid use2, 3, 5, 7.
Amidst the worsening U.S. opioid epidemic, providers are being encouraged to tailor opioid prescribing to individual patient needs. While the CDC guidelines8 are intended for primary care physicians managing chronic pain, many of the tenets are applicable to prescribing for acute pain. For example, screening for prior opioid use can assess both tolerance and potential risk of developing dependence9. However, to date, no studies have examined the rate of, or barriers to, routine screening by surgeons.
Public health interventions have done much to decrease rates of alcohol and tobacco use in past decades including changing the conversation surrounding their use and seeking treatment10. In many instances of social issues including as is the case for alcohol and tobacco, public health campaigns can help reframe the issue of misuse and dependence in a way that allows for patients to seek treatment options and receive necessary care11. Therefore, when looking at opioids and patient’s self-reporting of opioids, other substance misuse such as tobacco and alcohol act as an important control12. Providers are also more accustomed to asking about alcohol and tobacco and so it is more likely to be found in the medical record13. However, the stigma surrounding opioid misuse and dependence11, 14, 15 can prevent surgical and other providers from screening and properly prescribing pain management options for their patients.
The objectives of this study were to 1) assess how often patients were pre-operatively screened for prior opioid use in the past year, 2) compare patient-reported opioid, tobacco, and alcohol use with EMR documentation, and 3) explore barriers and facilitators to routine pre-operative screening for opioids. We hypothesized that routine screening is rarely done and that one contributing factor is that electronic medical records (EMR) are often inaccurate in describing a history of opioid misuse or abuse for a patient. To test this, we used socially accepted substance use of alcohol and tobacco as controls and examined the consistency between patient-reported tobacco and alcohol use with recorded values in the EMR. To put our findings in context, we conducted exploratory interviews with surgeons, advanced practice clinicians (APCs), and surgical trainees to identify potential barriers to routine screening.
Materials and methods
Study Design
We conducted a mixed-methods study to 1) determine how frequently patients are pre-operatively screened for opioid use, 2) whether patient-reported use of opioids, alcohol, and tobacco match EMRs, 3) explore potential barriers and facilitators to routine pre-operative opioid screening. The University of Utah Institutional Review Board approved this study.
At the University of Utah, we have been prospectively collecting patient-reported data on post-operative satisfaction, pain management, and opioid use since October 2017. Patients who underwent general, vascular, and plastic surgery operations are asked to complete a 40-item survey instrument at their first post-operative clinic visit. Patient are also asked about potential risk factors for developing chronic opioid use after surgery such as pre-operative opioid use, mental health disorders, smoking, and alcohol use. Our completion rate is 91.7% as patients are asked to complete the survey while they are waiting for providers in the clinic rooms. Patient responses are stored in a Research Electronic Data Capture (REDCap) database16. The pain management survey was developed through an iterative process in collaboration with survey design experts at the University of Utah Center for Clinical and Translational Science (CCTS). At the time of this study, we had survey data on 268 patients.
Chart review
We selected a random sample of 100 charts for in-depth review. The sampled patient list of medical record numbers was linked to patient’s electronic medical records and a complete chart review was then performed by a single reviewer (HT). Pre-operative clinical notes, anesthesia notes, and history and physical documents were systematically reviewed for documentation of pre-operative screening for opioid use. As a teaching institution, all notes are cosigned by attending surgeons. However, for our analysis, we assigned the role of the provider to the person who first wrote the note (trainee, APC, or surgeon). Notes written by medical students were considered to be written by the surgeon.
Patients were identified as having been screened for opioid use if there was any documentation in the pre-operative clinical record describing discussions held with the patient regarding opioid use, or if patients were categorized with chronic opioid use/dependence ICD-10 codes (F11.21; F11.2). Alcohol and tobacco use were also gathered from the EMR by use of ICD-10 codes (F10; F17.2). Patients with a pain management plan were considered to have been screened. Provider and patient sex were recorded.
Chart review data was then compared with patient’s self-reported responses for pre-operative opioid use along with more socially desirable substance abuse controls of tobacco, and alcohol use. This was done to ensure that the social stigma surrounding opioids did not create a barrier for discussion between patient and provider in acknowledging these social habits.
Statistical analysis
Descriptive statistics were performed on continuous and categorical variables to characterize the study population. Univariate associations were produced using chi-squared or Fisher’s exact tests. For our primary objective to assess if providers documented opioid misuse in their patient’s electronic medical record (EMR), we used log-binomial models to generage adjusted prevalence ratios (aPR) adjusting for provider age and sex. Data analysis was completed using Stata 15.1 software (College Station, TX).
Provider interviews
Exploratory qualitative interviews were conducted from a purposive sample with five surgical providers in the Department of Surgery at the University of Utah in order to better understand provider perspective regarding pre-operative screening for opioid use and identify barriers associated with screening. Providers consisted of two surgeons with more than a five-year history at the facility, a senior level general surgery resident, and two advanced practice clinicians with five and twenty years of experience, respectively. Providers were asked about their pre-operative opioid screening practices Questions included whether they screen patients and if so, where do they document a patient’s pre-operative opioid use; how they decide who to screen; provider and organizational barriers to screening and documentation; and how a history of pre-operative opioid use guides their clinical decision making for pain management options for their patients following surgery.
Results
Demographics
The demographics of the 100 patients sampled for chart review are shown in Table 1. Male and female patients were equally represented. The median patient age was 56 years old [IQR: 40–67]. The most common surgical specialties of the operations performed were vascular surgery (35%), breast (plastic) surgery (30%), and colorectal surgery (26%). A total of 87 patients had data for the primary endpoint of opioid use with 33 (38%) patients affirming that they used opioids in the past year. A total of 24 (24%) patients acknowledged alcohol use. Another 3 (3%) patients reported tobacco use. Out of 94 patients that responded to the question about chronic pain, 36 (37%) answered affirmatively (Table 1, Figure 1).
Table 1:
Patient demographics
| Demographics | Responses | N= (%) |
|---|---|---|
| Patient gender | ||
| Males | N=100 | 51 (51%) |
| Females | 49 (49%) | |
| Patient age | N=100 | Median 56 (IQR 40–67) |
| Surgical specialty | ||
| Breast (plastic surgery) | N=100 | 30 (30%) |
| Cancer (not other categories) | 6 (6%) | |
| Colorectal | 26 (26%) | |
| General | 3 (3%) | |
| Vascular | 35 (35%) | |
| Self-reported Opioid use in the past year | ||
| Yes | N=87 | 33 (38%) |
| No | 54 (62%) | |
| Self-reported Chronic pain | ||
| Yes | N=94 | 36 (37%) |
| No | 58 (59%) | |
Figure 1:
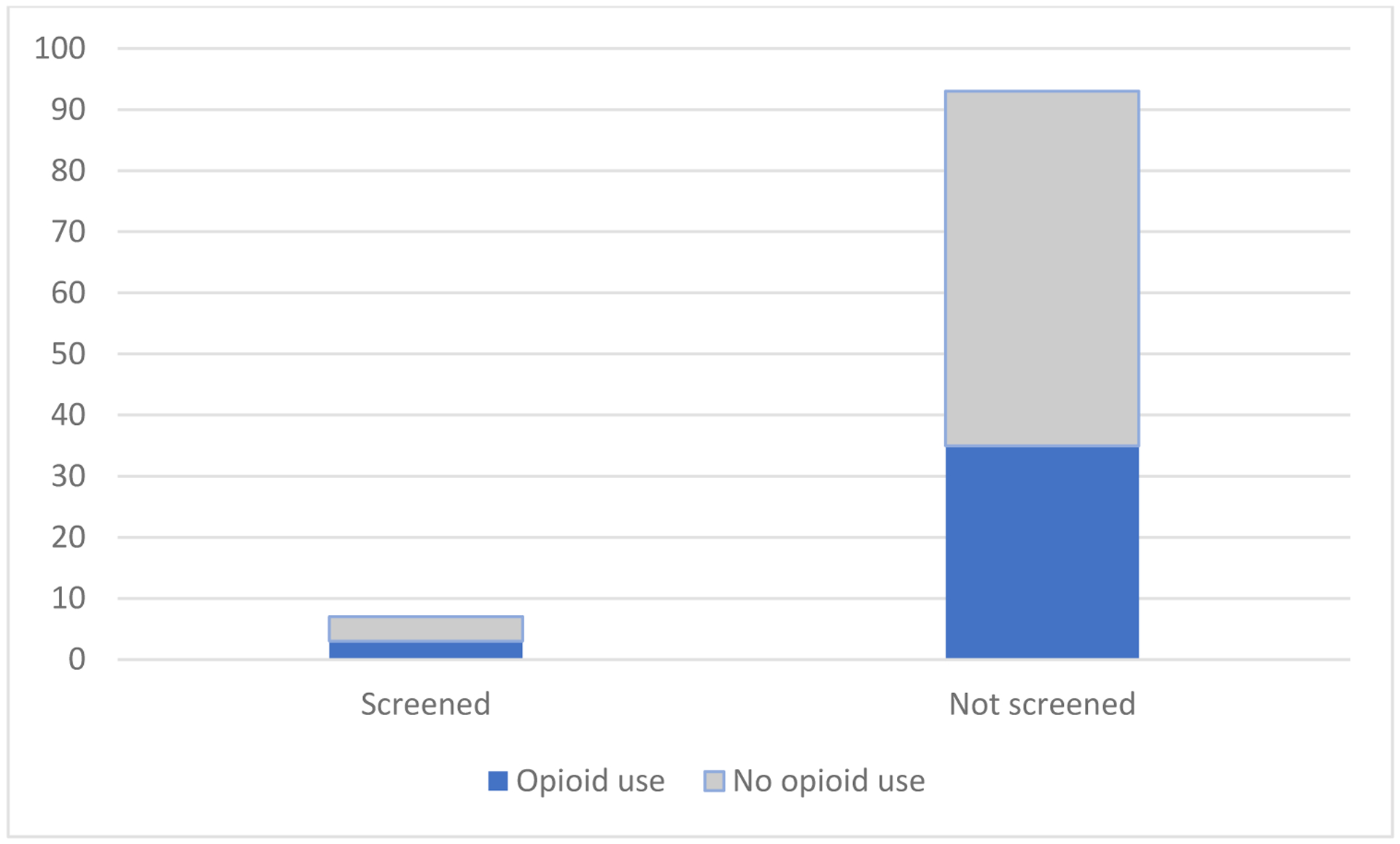
Pre-operative screening for opioid use
Pre-operative screening for opioid use
Ninety-three percent of patient’s charts lacked documentation of pre-operative screening. No patient had an ICD-10 code related to opioid abuse/misuse/dependence in their charts. Of the seven patients who were pre-operatively screened for opioids, 3 (43%) reported opioid use in the past year. Of the 93 patients who were not screened, 35 (37%) reported opioid use in the past year (Figure 1).
The 100 patients were seen by 39 unique providers. A slight majority of providers were female (56%). No provider consistently documented screening for opioid misuse in all of their patients. Provider sex was also not associated with screening (males, 41%, females, 52%). Trainees were the largest group (43%) of providers followed by APCs (30%) and surgeons (27%). Provider role was not associated with likelihood of opioid screening (surgeon versus trainee, PR =1.2, 95% CI 0.2–8.5) (surgeons versus APCs, PR=1.05, 95% CI 0.17–8.53).
Concordance/Agreement between patient-reported substance use and EMRs.
Again, 38% of patients self-reported opioid use in the past year while no patients had opioid misuse documented in the EMR.A total of 25% of those who self-reported no alcohol had EMR documentation to the contrary. Only two patient’s EMR charts did not have alcohol use documented even though the patients self-reported alcohol use in the survey. Likewise, 40% of patients self-reported that they did not use tobacco; however, there was disagreement between the survey and chart since their EMR included tobacco use. No patients acknowledged tobacco use in the survey that wasn’t also confirmed in the EMR, though the EMR reported that 16% more patients had tobacco use (Figure 2).
Figure 2:
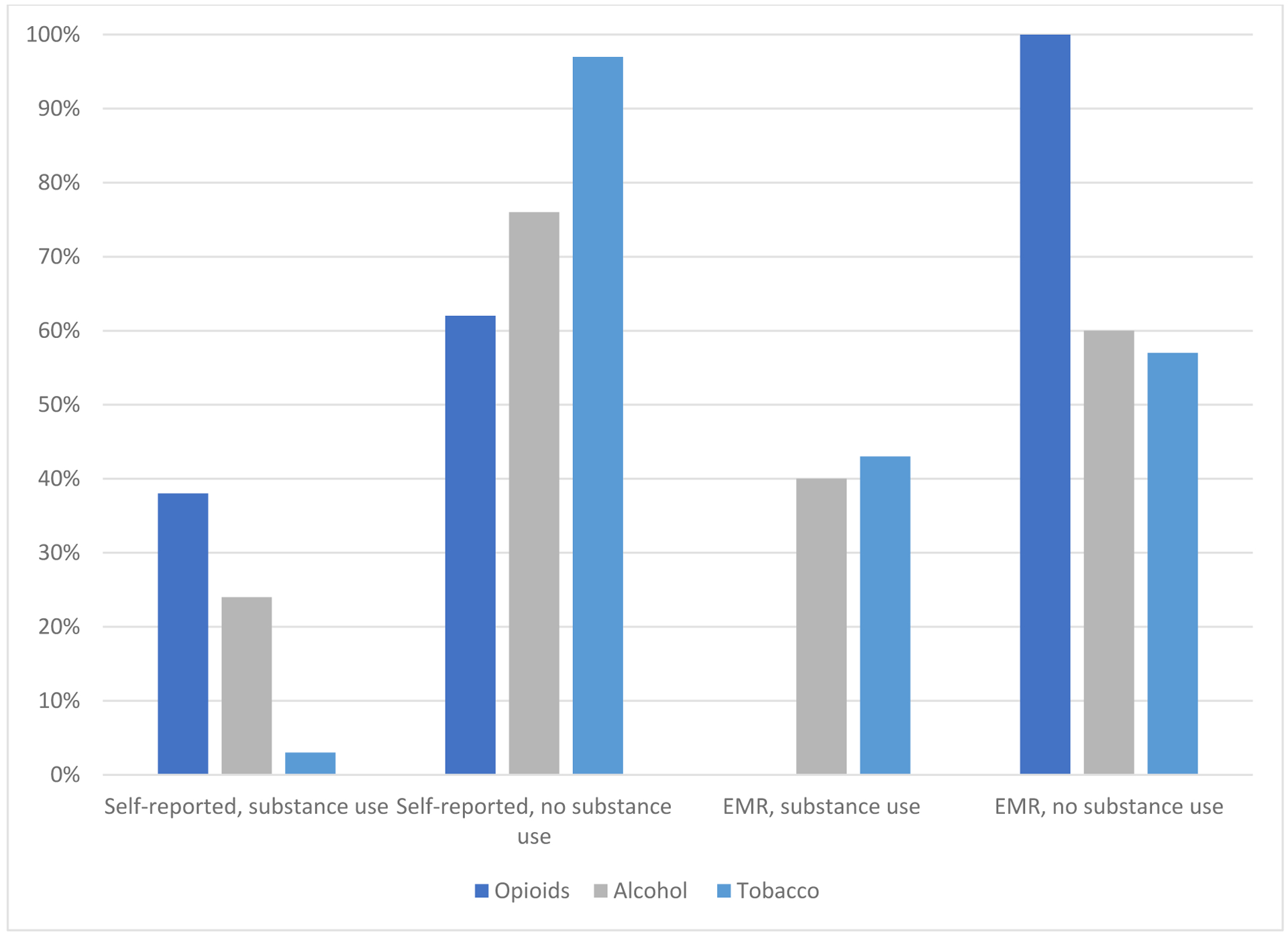
Comparison of patient self-reporting versus EMR documentation of opioid, alcohol, and tobacco use
In qualitative interviews with surgical providers, the most common perceived barriers to routine pre-operative screening were not having sufficient time; lack of clarity about who is responsible for screening; screening not being part of their clinical workflow; and lack of pre-defined prompts or consistent location to document in charting templates (Table 2). Providers acknowledged that they screen only when they suspect opioid misuse in their patients and they did not have a systematic screening process built into their workflow. One APC reported that the stigma surrounding opioids prevents providers from documenting misuse in the patient’s chart. They felt that if OUD were perceived as any other chronic condition such as hypertension or diabetes mellitus, then providers could have more upfront and open conversations with their patients. Overall, providers acknowledged that while they felt comfortable prescribing opioids, they were uncomfortable screening or providing a diagnosis of OUD and felt the responsibility should be with other providers. Surgeons reported that screening and documentation of opioid misuse was not within their scope of practice. Nor did they feel that they had the clinical expertise to make such a diagnosis.
Table 2.
Surgical provider perspectives on pre-operative screening for opioids use
| Theme | Quote |
|---|---|
| Barriers | Provider: “Time, cost, logistics are all barriers to screening for opioid misuse.” Provider: “Barriers are: that nothing is documented, patients are not up front about their opioid use, our Utah controlled substance database doesn’t follow out of state folks who may have misuse issues.” Provider: “I think if all providers felt this was like any other condition such as DM, HTN… it would get mentioned in all documentation where it is relevant to discuss.” |
| Unclear who should screen | Provider: “Unsure where to document, not an expert in the area, sensitive to putting this in the chart without out proper workup and expertise.” Provider: “I screen based on a history of abuse concern for additional abuse.” Provider: “I don’t have a system for [screening].” |
| Not within surgical scope of practice/lack of expertise | Provider: “Typically I have those with more expertise manage the pain.” Provider: “I think we sometimes are not sure where or how to respectfully document [opioid misuse].” Provider: “Most physicians do not want to place that label [opioid misuse] on a patient without being 100% sure.” |
Discussion
In our current study, we found that patients are rarely screened pre-operatively for opioids patient self-reported use of opioids, as well as substance abuse controls of alcohol, and tobacco does not match with the EMR; and surgical providers report significant barriers to routine pre-operative screening for opioids. Only 7% of patients had documented screening for pre-operative opioid use. There were significant discrepancies between patient reported opioid, alcohol, and tobacco use with what was recorded in the EMR. Providers identified time, cost, logistics, unsure who and how to screen and document, and expertise in pain management specialization as key reasons for not documenting screening in a patient’s chart before surgery.
Our study found that nearly a third of patients used opioids in the year prior to surgery, but screening by providers was rare. Failure to identify patients with prior opioid use can lead to the higher than expected inpatient dosing of opioids which is associated with increased rates of mortality, respiratory depression and failure, and myriad other surgical complications17, 18. A lack of screening can also have the unintended result of putting a patient back into a dependence situation after having previously overcome OUD. There has been improved effort to identify chronic opioid use and misuse in patients in general19; however, the surgical environment is a key area where patients are receiving exposure to opioids and there is a lack of data on screening for opioid use and dependence.
In the patient sample, patients that were screened were on average older (61 years) and not a younger group as is typically seen in the opioid epidemic mortality population6, 20, 21. During qualitative interviews, providers acknowledged that they screened patients for opioid misuse based on clinical suspicion or review of concurrent medications instead of just targeting a particular age group. When we looked at substance abuse controls that were deemed to be more socially acceptable than opioids, there was a discrepancy in acknowledgement for alcohol (16%) or tobacco use (40%) in a self-reported survey by patients even though it was documented by providers in the EMR. This could represent an error in the medical record or a change in behavior over time, but could also represent a lack of willingness for patients to acknowledge these habits. However, the fact that patients were more willing to acknowledge social habits with providers when asked directly, as seen in this study, could indicate a need for providers to screen for opioid misuse in their patients and not rely on patients to offer up that information prior to surgery or to depend on the EMR for accurate or up to date documentation of the condition22–25. Furthermore, Goodyear et al., 2018 described how social stigma surrounding opioid misuse can have an effect on the delivery of patient care11. Patients may not be willing to offer up this information and receive proper pain management unless providers carefully assess patients for opioid misuse and dependence. Green et al. showed a positive predictive value of ICD9/10 codes at 81% in classifying opioid overdoses and encouraged the use of the EMR to monitor opioid overdoses24, but there seems to be a disconnect between screening for and giving patients a diagnosis of opioid misuse.
In exploratory qualitative interviews, surgical providers identified a number of barriers to pre-operative screening for opioids. Providers were comfortable prescribing opioids but hesitant to label patients as chronic opioid users or with OUD. They felt these diagnoses were outside of their clinical expertise. However, when asked if they refer to a pain management team before surgery, providers responded that time, costs, and logistics usually prevented them from doing so. This may represent a system-level opportunity to integrate routine screening with referrals to pain management services pre-operatively. Surgical providers felt that other providers should perform screening and assist in the management of patients using opioids chronically or with OUD. This is similar to a diagnosis of hypertension or diabetes, where surgical providers may provide management during an acute period of time after surgery, but transition ongoing management to primary care providers.
There are limitations to this study. This research was conducted at a single academic tertiary center and our findings may not be generalizable to other surgical settings or populations. Anecdotal evidence from discussions with many surgeons suggests though that lack of routine opioid screening is common. Also, since the rates of screening were so low, we could not examine the factors associated with screening. Providers reported that they screen patients they consider high-risk as well as whether there are predictors associated.
Conclusions
Many patients either have a past medical history of opioid misuse or are currently using opioids prior to surgery. This puts them at risk for either peri-operative complications or inadequate pain management. However, screening for pre-operative opioid misuse is rarely done. In addition, EMRs may not accurately reflect ongoing opioid, alcohol and tobacco use and need to be routinely updated. Significant barriers to routine pre-operative screening exist, notwithstanding the risks associated with not screening patients. Additional research is needed to understand barriers and generate buy-in from surgical providers and health systems, before effective implementation of opioid misuse screening and documentation in surgical patients can occur.
Funding:
The research reported in this publication was supported (in part or in full) by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR002538. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Disclosure: All authors have nothing to disclose in regards to this research.
References:
- 1.Hah JM, Bateman BT, Ratliff J, Curtin C, Sun E. Chronic Opioid Use After Surgery: Implications for Perioperative Management in the Face of the Opioid Epidemic. Anesthesia and analgesia. 2017;125(5):1733–1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hall M, Schwartzman A, Zhang J, Liu X. Ambulatory Surgery Data From Hospitals and Ambulatory Surgery Centers: United States, 2010. Natl Health Stat Report. February 2017;102:1–15. [PubMed] [Google Scholar]
- 3.Han B, Compton WM, Blanco C, Crane E, Lee J, Jones CM. Prescription Opioid Use, Misuse, and Use Disorders in U.S. Adults: 2015 National Survey on Drug Use and Health. (1539–3704 (Electronic)). [DOI] [PubMed] [Google Scholar]
- 4.Kessler E, Shah M, Gruschkus S, Raju A. Cost and quality implications of opioid-based postsurgical pain control using administrative claims data from a large health system: opioid-related adverse events and their impact on clinical and economic outcomes. Pharmacotherapy. 2013;33(4):383–389. [DOI] [PubMed] [Google Scholar]
- 5.Jiang X, Orton M, Feng R, Hossain E, Malhotra N, Zager E, et al. Chronic Opioid Usage in Surgical Patients in a Large Academic Center. Annals of Surgery. April 2017;265(4):722–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Katz J Opioid Epidemic Drug Overdose Deaths Are Rising Faster Than Ever. . New York Times, 2017. [Google Scholar]
- 7.Holman J, Stoddard G, Horwitz D, Higgins T. The effect of preoperative counseling on duration of postoperative opiate use in orthopaedic trauma surgery: a surgeon-based comparative cohort study. Journal of Orthopedic Trauma. 2014;28(9):502–506. [DOI] [PubMed] [Google Scholar]
- 8.Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain--United States, 2016. JAMA. 2016;315(15):1624–1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pulley D Preoperative Evaluation of the Patient with Substance Use Disorder and Perioperative Considerations. Anesthesiol Clin.34(1):201–211. [DOI] [PubMed] [Google Scholar]
- 10.West R, Raw M, McNeill A, Stead L, Aveyard P, Bitton J, et al. Health-care interventions to promote and assist tobacco cessation: a review of efficacy, effectiveness and affordability for use in national guideline development. Natl Health Stat Report. February 2017;102:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goodyear K, Haass-Koffler C, Chavanne D. Opioid use and stigma: The role of gender, language and precipitating events. Drug Alcohol Dependence. April 1 2018;185:339–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Loheswaran G, Soklaridis S, Selby P, Le Foll B. Screening and Treatment for Alcohol, Tobacco and Opioid Use Disorders: A Survey of Family Physicians across Ontario. (1932–6203 (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Angelini K, Sutherland M, Fantasia H. Reported Alcohol and Tobacco Use and Screening Among College Women. J Obstet Gynecol Neonatal Nurs. May-Jun 2017;46(3):e75–e82. [DOI] [PubMed] [Google Scholar]
- 14.Cooper S, Campbell G, Larance B, Murnion B, Nielsen S. Perceived stigma and social support in treatment for pharmaceutical opioid dependence. Drug Alcohol Rev. 2018;37(2):262–272. [DOI] [PubMed] [Google Scholar]
- 15.Kennedy-Hendricks A, Barry CL, Gollust SE, Ensminger ME, Chisolm MS, McGinty EE. Social Stigma Toward Persons With Prescription Opioid Use Disorder: Associations With Public Support for Punitive and Public Health-Oriented Policies. (1557–9700 (Electronic)). [DOI] [PubMed] [Google Scholar]
- 16.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical informatics. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cozowicz C, Olson A, Poeran J, Mörwald E, Zubizarreta N, Girardi F, et al. Opioid prescription levels and postoperative outcomes in orthopedic surgery. Pain. 2017;158(12):2422–2430. [DOI] [PubMed] [Google Scholar]
- 18.Lee JS, Hu HM, Edelman AL, Brummett CM, Englesbe MJ, Waljee JF, et al. New Persistent Opioid Use Among Patients With Cancer After Curative-Intent Surgery. (1527–7755 (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brummett CM, Waljee JF, Goesling J, Moser S, Lin P, Englesbe MJ, et al. New Persistent Opioid Use After Minor and Major Surgical Procedures in US Adults. (2168–6262 (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Institute on Drug Abuse N. Overdose death rates. Available at: https://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates. Accessed January 19, 2019.
- 21.Prevention. CfDCa. Opioid Drug Overdose Death Data. Available at: https://www.cdc.gov/drugoverdose/data/statedeaths.html. Accessed 2/27/19.
- 22.Yadav S, Kazanji N, K CN, Paudel S, Falatko J, Shoichet S, et al. Comparison of accuracy of physical examination findings in initial progress notes between paper charts and a newly implemented electronic health record. (1527–974X (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.March C, Scholl G, Dversdal R, Richards M, Wilson L, Mohan V, et al. Use of Electronic Health Record Simulation to Understand the Accuracy of Intern Progress Notes. J Grad Med Educ. May 2016;8(2):237–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Green C, Perrin N, Janoff S, Campbell C, Chilcoat H, Coplan P. Assessing the accuracy of opioid overdose and poisoning codes in diagnostic information from electronic health records, claims data, and death records. Pharmacoepidemiol Drug Safety. May 2017;26(5):509–517. [DOI] [PubMed] [Google Scholar]
- 25.Lingren T, Sadhasivam S, Zhang X, Marsolo K. Electronic medical records as a replacement for prospective research data collection in postoperative pain and opioid response studies. (1872–8243 (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]


