Patients with chronic rheumatic diseases are a particularly susceptible population affected by the COVID-19 pandemic,1, 2 and their protection through vaccination was prioritised accordingly. Nevertheless, many patients were reluctant to receive the vaccine due to fear of side-effects, disease flare, and lack of information regarding the novel vaccines.3, 4, 5 The objectives of this study were to assess the acceptability of the COVID-19 vaccine in patients with chronic rheumatic diseases and health-care professionals in Arab countries and to identify the factors associated with acceptability.
The Arab League of Associations for Rheumatology (ArLAR) COVID Vaccination (ARCOVAX) cross-sectional study used an anonymous web-based survey adapted from the VAXICOV study,3, 6 translated to Arabic by the authors and validated by the ArLAR scientific committee. A pilot test done in three languages (Arabic, English, and French) found the survey to be well understood and easy to complete.
The survey was disseminated online in the three languages between April 13 and May 11, 2021, through multiple social media platforms of ArLAR, the Arab Adult Arthritis Awareness (AAAA) group (an ArLAR Special Interest Group), rheumatologist and patient association accounts, emails from the ArLAR and AAAA groups, WhatsApp messages, and direct invitation to patients using a QR code on display in physician waiting rooms. Health-care professionals were considered as a convenience control group, expected to serve as a landmark for optimal vaccine acceptability at the time of the study.
Demographic and disease data, perceptions about COVID-19, and perceptions about vaccine hesitancy were presented descriptively. They were compared between patients and health-care professionals using χ2 or t tests, as appropriate. Health-care professionals who also identified themselves as patients with chronic rheumatic diseases were counted twice, once in each group.
Vaccine acceptability was defined as participants who were already vaccinated or willing to be vaccinated. Non-acceptability was defined as participants who were undecided or refused to be vaccinated, as per the WHO definition of vaccine hesitancy as a delay in acceptance or refusal of vaccines despite availability of vaccine services.7 Acceptability was compared between patients and health-care professionals, first in the whole study population, then in non-vaccinated participants.
Perceptions about vaccination were evaluated on a 0–10 scale, where 10 is the highest agreement, and stratified according to the vaccine acceptability. Factors associated with acceptability were evaluated using two separate logistic regression models for patients and health-care professionals, with vaccine acceptability as the dependent variable. All statistical analyses were done with SPSS (version 18.0) software.
Accessing the Google form and then clicking on “Agree” after reading the survey description was considered as consent to participate. The study was approved by the institutional review boards of the Saint-Joseph University (Beirut, Lebanon) and Specialized Medical Center (Riyadh, Saudi Arabia).
3176 participants from 19 Arab countries completed the survey (1595 patients, 1517 health-care professionals [including 48 health-care professionals who were also patients], and 64 with missing categories). The participants were recruited from the following countries: Algeria, Bahrain, Comoros, Egypt, Iraq, Jordan, Kuwait, Lebanon, Libya, Morocco, Oman, Palestine, Qatar, Saudi Arabia, Sudan, Syria, Tunisia, United Arab Emirates, and Yemen. The mean age of the patients was 39 years (SD 13), 1159 (73%) of 1595 patients were females, 422 (26%) were males, and the remaining 14 (1%) patients either had missing data or preferred not to state their gender (appendix p 1). The mean age of health-care professionals was 40 years [12], 900 (59%) of 1517 health-care professionals were females, 610 (40%) were males, and the remaining seven (<1%) had missing data or preferred not to state their gender. In the past 3 years, 481 (30%) of 1595 patients and 632 (42%) of 1517 health-care professionals had received the influenza vaccine. The fear of COVID-19 was estimated as a median of 7 (IQR 5–10) on the 10-point perception scale in both groups (appendix p 1).
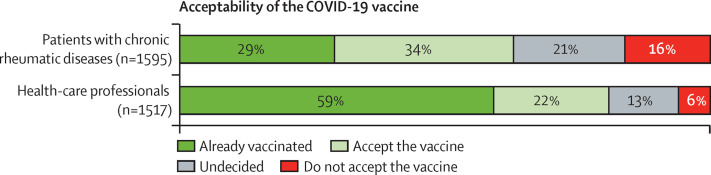
469 (29%) of 1595 patients, compared with 899 (59%) of 1517 health-care professionals, were already vaccinated against COVID-19. Vaccine acceptability was significantly lower in patients than in health-care professionals (1008 [63%] vs 1237 [82%]; p<0·001; figure ), and remained significantly lower when considering the non-vaccinated participants exclusively (539 [48%] of 1126 non-vaccinated patients vs 338 [55%] of 618 non-vaccinated health-care professionals; p=0·006). There was no difference in acceptability between all physicians and other health-care professional categories (p=0·96).
Figure.
COVID-19 vaccine acceptability in patients with chronic rheumatic diseases and health-care professionals in 19 Arab countries
Acceptability is defined as having already been vaccinated or expressing the will to be vaccinated.
Among the non-vaccinated participants, 191 (56%) of the 339 undecided patients and 99 (40%) of the 248 patients who refused the vaccine would be willing to get vaccinated if their physician recommended it, compared to 72 (37%) of 195 undecided health-care professionals and 13 (15%) of 85 health-care professionals who refused the vaccine. In addition, 142 (43%) of the 332 undecided patients and 68 (28%) of 247 patients who refused the vaccine would be willing to be vaccinated if it were mandatory by law, compared to 101 (53%) of 191 undecided health-care professionals and 21 (25%) of 85 health-care professionals who refused the vaccine (appendix p 4).
981 (62%) of 1595 patients trusted their rheumatologist as the most reliable source of information about the vaccine. The most important concerns among patients about the vaccine were concerns about side-effects and the scarcity of experience with and background information about new COVID-19 vaccines, followed by concerns about the health crisis management and concerns about vaccination in general; whereas it was the scarcity of experience with and background information about the vaccines and concerns about the health crisis management by governments, followed by concerns about side-effects among health-care professionals (appendix p 5). The concerns were greater in participants who refused the vaccine than in those who accepted it (p<0·001; appendix p 2).
In the multivariable analysis, vaccine acceptability was associated with a higher gross domestic product (GDP), the feeling that it is important to be personally vaccinated, fewer concerns regarding the vaccine side-effects, fewer concerns about vaccination in general, previous influenza vaccination, fear of COVID-19, and fewer concerns about the risk of autoimmune flare (appendix p 3). Although the association with age and gender was not confirmed in the multivariable analysis, older age in patients and male gender in health-care professionals were associated with acceptability. Comorbidities were not associated with vaccine acceptability in both groups.
This is the first large-scale study to assess the acceptability of the COVID-19 vaccine in patients with chronic rheumatic diseases and health-care professionals across Arab countries. Vaccine acceptability was 63% in patients, within the same range as other international studies of patients with chronic rheumatic diseases, including the VAXICOV study (54–93%),3, 4, 5, 8 but higher than in the general population in Arab countries (37–53%),9, 10 suggesting the lack of hesitancy specifically related to chronic rheumatic diseases. Notably, more health-care professionals received the vaccine than patients (59% vs 29%), which could be related to vaccine accessibility and national vaccination strategies targeting health-care professionals as a priority at the time of data collection. In April and May, 2021, the vaccine was not compulsory in any of the population categories, and it was offered free of charge by the governments. Nonetheless, acceptability remained lower in patients (48% vs 55%) even after considering the non-vaccinated participants exclusively.
Notably, the results confirmed the influence of the rheumatologist in convincing the patients to get vaccinated.3, 8, 9 However, different strategies should be used to motivate the health-care professionals to get vaccinated, as their acceptability increased significantly if the vaccine was mandatory by law.
The greatest concerns regarding the vaccine were the fear of side-effects (although the type of side-effect was not specified in this study) and the scarcity of experience with and background information about the vaccines among patients, and the scarcity of experience with and background information about the vaccines and the concerns about the health crisis management by governments among health-care professionals. In the VAXICOV study, Felten and colleagues noted that the highly rated concerns among patients and health-care professionals were similar to the current study—ie, the scarcity of experience with and background information regarding the vaccines, the use of new technology, and side-effects of the vaccine. Nevertheless, the concern about the health crisis management by the health authorities was more frequently reported in our study than in the VAXICOV study. This finding highlights the need for better transparency and communication about safety data to build much-needed trust in vaccines.
One of the possible concerns that could not be identified by the study questionnaire might be the use of vaccines that were not approved by European or American agencies, such as vaccines from China or Russia, at the time of data collection.
The current study also identified a clear association between the GDP level and the vaccine acceptability, indicating that people in countries with higher GDPs were more acceptive, which could be related, in some part, to vaccine access, but most probably to cultural and health-care system differences and higher trust in health authorities.
The strength of this study lies in the large number of participants, including both patients with chronic rheumatic diseases and health-care professionals from 19 Arab countries. The limitations include the possibility of a selection bias and the lack of comparison among the individual countries.
Acceptability of the COVID-19 vaccine was not optimal (63% in patients, 81% in health-care professionals) but could be substantially improved if doctors recommended the vaccine to patients. Moreover, addressing the main determinants of acceptability and providing accurate and updated data to physicians can help them to relay more timely and transparent information to their patients, thus facilitating the vaccine uptake in both groups.
LA reports consulting fees and honoraria from Pfizer and AstraZeneca, outside this work. All other authors declare no competing interests. NZ, LEK, IH, and MM designed the study and were part of the steering committee that wrote the study protocol, included participants from their respective countries, and supervised the recruitment of participants in all the countries. LA and RF provided the original questionnaire from the VAXICOV study and participated in the questionnaire adaptation and in the finalisation of the protocol. NZ, LEK, MM, and IH drafted the manuscript and handled the comments of the authors. NA, HH, ME, MER, BM, FA, WH, AA, and AAN participated in the study design and protocol, included participants from their respective countries, and helped in addressing logistical issues during recruitment. NZ and IH analysed the results of the survey and designed the tables and figures. All authors made substantial contributions to work and participated in the discussion of the study results, the draft of the manuscript, and revised the final submitted document for intellectual content. All the authors approved the version to be published and agreed to be accountable for all aspects of the work. RF and LA contributed equally.
Supplementary Material
References
- 1.Furer V, Rondaan C, Agmon-Levin N, et al. Point of view on the vaccination against COVID-19 in patients with autoimmune inflammatory rheumatic diseases. RMD Open. 2021;7 doi: 10.1136/rmdopen-2021-001594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Strangfeld A, Schäfer M, Gianfrancesco MA, et al. Factors associated with COVID-19-related death in people with rheumatic diseases: results from the COVID-19 Global Rheumatology Alliance physician-reported registry. Ann Rheum Dis. 2021;80:930–942. doi: 10.1136/annrheumdis-2020-219498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Felten R, Dubois M, Ugarte-Gil MF, et al. Vaccination against COVID-19: expectations and concerns of patients with autoimmune and rheumatic diseases. Lancet Rheumatol. 2021;3:e243–e245. doi: 10.1016/S2665-9913(21)00039-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boekel L, Hooijberg F, van Kempen ZLE, et al. Perspective of patients with autoimmune diseases on COVID-19 vaccination. Lancet Rheumatol. 2021;3:e241–e243. doi: 10.1016/S2665-9913(21)00037-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ammitzbøll C, Thomsen MK, Erikstrup C, Hauge EM, Troldborg A. National differences in vaccine hesitancy: a concern for the external validity of vaccine studies. Lancet Rheumatol. 2021;3:e324. doi: 10.1016/S2665-9913(21)00083-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Felten R, Dubois M, Ugarte-Gil MF, et al. Cluster analysis reveals three main patterns of beliefs and intention with respect to SARS-CoV-2 vaccination in patients with autoimmune and inflammatory diseases. Rheumatology. 2021;60:SI68–SI76. doi: 10.1093/rheumatology/keab432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO Report of the Sage Working Group on Vaccine Hesitancy. 2014. https://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdf (Oct 15, 2021).
- 8.Gaur P, Agrawat H, Shukla A. COVID-19 vaccine hesitancy in patients with systemic autoimmune rheumatic disease: an interview-based survey. Rheumatol Int. 2021;41:1601–1605. doi: 10.1007/s00296-021-04938-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.El-Elimat T, AbuAlSamen MM, Almomani BA, Al-Sawalha NA, Alali FQ. Acceptance and attitudes toward COVID-19 vaccines: a cross-sectional study from Jordan. PLoS One. 2021;16 doi: 10.1371/journal.pone.0250555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alqudeimat Y, Alenezi D, AlHajri B, et al. Acceptance of a COVID-19 vaccine and its related determinants among the general adult population in Kuwait. Med Princ Pract. 2021;30:262–271. doi: 10.1159/000514636. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.