Abstract
Introduction
By the end of 2021, Ethiopia plans to vaccinate 20% of the population. The prioritized group includes people older than 65 years, health care workers, teachers, soldiers, and people living with comorbid diseases, including HIV/AIDS. However, due to a lack of intention and other reasons, only less than one percent of the population has taken COVID-19 vaccine. Therefore, this study aimed to assess the determinant factors of intention to receive the COVID-19 vaccine among HIV-positive patients attending ART clinics in southern Ethiopia.
Methods
A facility-based cross-sectional study was conducted among 398 HIV-positive patients from March 1 to April 28, 2021. Data were collected using a structured questionnaire by three midwives. We entered the data into Epi InfoTM 3.5.1. Binary logistic regression was used to identify independently associated variables in bivariate and multivariate analyses using SPSS version 20.
Results
Currently, the intention to take COVID-19 vaccine among HIV-positive patients was 33.7%. The probability of PLWHA to take COVID-19 vaccine was two (AOR = 2 (1.08–3.44)) times higher among those who have been diagnosed with chronic diseases (exclude HIV) with those with not been diagnosed. PLWHA who were male in sex were five (AOR = 5 (2.96–8.68)) times more likely to take COVID-19 vaccine than female. The study also indicated that the odds of intention to take the COVID-19 vaccine were 4.1 times (AOR = 4.1 (2.33–7.31)) times higher among those participants who had good knowledge of COVID-19 practice compared with those who had poor knowledge.
Conclusion
The overall intention to receive the COVID-19 vaccine among PLWHA is low. Therefore, there is a need to improve the intention to receive the COVID-19 vaccine among HIV-positive patients to achieve the 2021 goal of Ethiopia for 20% of the population vaccination. Patients with chronic illness, knowledge of the COVID-19 vaccine, and sex were factors associated with the intention to receive COVID-19 vaccine.
Keywords: COVID-19, HIV positive, vaccine intention
Introduction
COVID-19 is caused by a single-stranded novel coronavirus that severely affects the respiratory system.1 Fever, cough, fatigue, and dyspepsia are some of the signs and symptoms of COVID-19.2 In December 2019, the first human case of COVID-19 was reported in Wuhan, China, which affected more than 200 million people in the world until August 2021.3 According to a World Health Organization (WHO) report, there were over 1.8 million cases and 38,000 deaths from December to August 30, 2020.4 About 371,448 cases and 9480 deaths were from Africa.5
Different countries in the world develop and vaccinate various kinds of COVID-19 vaccines to tackle this pandemic. The WHO reported that 5.9 billion vaccine doses were administered even if it lacks equitable access to safe and effective vaccines in developing countries.6,7
Ethiopia launched the COVID-19 vaccine introduction on March 31, 2021, targeting a prioritized group of people to address 20% of the population by the end of 2021.8 People over the age of 65 years, health care workers, teachers, soldiers, and people living with comorbid diseases, including HIV-positive patients, were among those prioritized.8
The clinical course of people living with HIV/AIDS (PLWHA) with COVID-19 is not well studied, but the World Health Organization has reported high occurrences of severe disease and mortality.9–11 Many vaccine preparations for this group of people are on trial.12 The WHO recommended only COVID-19 vaccines (AstraZeneca/Oxford, Johnson & Johnson, Moderna, Pfizer, Sinopharm, and Sinovac) are safe for people living with HIV.13
Ethiopia’s ministry of health put PLWHA as the top priority group to take the COVID-19 vaccine. However, a small number of the population received COVID-19 vaccine due to a lack of intention to vaccinate and vaccine.14 Besides this, people’s myths and misconceptions about the vaccine, lack of trust in vaccines, unavailability of vaccine, poor knowledge about vaccine, and vaccine hesitancy are some factors that affect the low uptake of COVID-19 vaccine.15,16
Currently, in Ethiopia, not only new cases but also death rates are rapidly increasing. Therefore, understanding HIV-positive patients’ intention to receive COVID-19 vaccine is one of the pillars to lowering the transmission of this pandemic. Besides their intention, it needs to develop and implement appropriate measures to increase COVID-19 vaccine uptake.
As there was no study conducted among HIV-positive patients in Ethiopia, this study aimed to assess the magnitude and determinant factors of intention to receive the COVID-19 vaccine among HIV-positive patients in southern Ethiopia.
Patients and Methods
Study Setting and Period
A facility-based cross-sectional study was conducted at Butajira General Hospital from March 1 to April 28, 2021. Butajira hospital is located in the Gurage Zone, 135 km from Addis Ababa, Ethiopia. The hospital has 110 beds that provide service to Butajira town and the surrounding area. It also offers free ART services to 1021 registered HIV-positive patients.
Study Population
All HIV-positive patients who visited the ART clinic were the source population, while patients who visited the ART clinic during the data collection period were the study population. Participants who were 18 years of age or older were included in the study. However, patients whose medical records were incomplete and seriously ill were excluded.
Sample Size Determination and Procedure
The sample size was estimated using a single proportion formula with the assumption of a prevalence of 50%, which was used due to no study done in Ethiopia, marginal error (d) 0.05, with a 95% confidence interval. After accounting for a 10% non-response rate, the total sample size was 424.
First, the total number of HIV-positive patients who registered in the Butajira Hospital ART clinic was 1021. An average of 15 patients visits the ART clinic daily for 450 HIV-positive patients a month. Then, systematic random sampling was used to select study participants. The first participant was selected randomly; then, the subsequent participants were selected by a systematic sampling technique every two intervals.
Data Collection Tools and Procedure
The data were collected by using a pre-tested structured questionnaire. The tool was first designed in English, translated into Amharic, and then back to English for language consistency. The main components of the questionnaire are socio-demographic characteristics, health and perception of the COVID-19 vaccine, and the knowledge of the COVID-19 vaccine questionnaires. The Cronbach's Alpha of variable knowledge of COVID-19 vaccine items was 86.2%. The comprehensive understanding of the COVID-19 vaccine of the respondent was collected using five questions.
Three midwives collected data, and one MSc Midwife supervisored the procedure. The data collector is given a one-day training before the actual data collection on interviewing approach and data recording. An interviewer-administered questionnaire via face-to-face interview was used to collect the data. An interviewer-administered questionnaire via face-to-face interview was used to collect the data.
Data Processing and Analysis
After a manual check of completeness, we entered data in Epi info TM version 3.5.1. Statistical Package of Social Science (SPSS) version 25 was used for analysis. We used descriptive statistics such as percentages, frequencies, and mean/median to characterize the study population as appropriate. A bivariate analysis was computed to identify potential variables for the multivariable logistic regression model. We considered variables with p-value of ≤0.25 in the bivariate analysis for multivariable analysis. The model goodness of fitness has been checked using the Hosmer–Lemeshow statistic. Finally, p-value <0.05 was considered as a cut-off point to declare a significant statistical association.
Result
Socio-Demographic Characteristics of the Respondent
A total of three hundred and ninety-eight HIV-positive patients participated, with a response rate of 93.8%. The respondent’s age range was 18–67 years, with a mean age of 32.15 (SD ± 5.1) years. Out of these 398 PLWHA, 72.5% and 72.6% were Orthodox-Christians, and married, respectively. Regarding the educational and occupational status, 135 (34%) and 94 (31.2%) of the respondents were attended higher education and were employed, respectively. The majority of the respondent, 236 (59.3%) of ART users, had an annual income of ≥£300 (Table 1).
Table 1.
Socio-Demographic Characteristics Intention to Take COVID-19 Among PLWHA in Southwest Ethiopia (N = 398)
| Variable | Number | Percent (%) |
|---|---|---|
| Sex | ||
| Male | 236 | 59 |
| Female | 162 | 41 |
| Age | ||
| 18–26 | 107 | 26.9 |
| 27–36 | 159 | 39.9 |
| 37–47 | 81 | 20.4 |
| >47 | 51 | 12.8 |
| Education | ||
| No education | 96 | 24.1 |
| Primary | 113 | 28.4 |
| Secondary | 152 | 38.2 |
| Higher education and above | 37 | 9.3 |
| Occupation | ||
| Unemployed | 107 | 26.9 |
| Employed | 124 | 31.2 |
| Housewife | 118 | 29.6 |
| Others | 49 | 12.3 |
| Religion | ||
| Orthodox | 288 | 72.5 |
| Muslim | 99 | 24.9 |
| Other | 11 | 2.6 |
| Income | ||
| <£180 | 76 | 19.1 |
| £180–£300 | 86 | 21.6 |
| >£300 | 236 | 59.3 |
| Marital status | ||
| Currently Married | 233 | 49.5 |
| Currently unmarried | 165 | 41.5 |
Health Status and COVID-19 Experience
Of the 398 ART users, 341 (85.6%) respondents had received medical care after the COVID-19 restriction. Three hundred eighty-three (96.2%) and three hundred forty-four (86.4%) of respondents responded that they had no personal history of COVID-19 infection and had taken the ART drug for less than ten years, respectively. Regarding the perception of susceptibility to COVID-19 infection, which causes severe illness and death, 170 (42.3%), 251 (63.6%), and 86 (21.6%) of respondents agree with it, respectively (Table 2).
Table 2.
Health Status and COVID-19 Experience in Southwest Ethiopia (N = 398)
| Variable | Frequency (n) | Percent (%) |
|---|---|---|
| Receive medical care after COVID-19 restriction | ||
| Yes | 341 | 85.6 |
| No | 57 | 14.4 |
| Duration on ART | ||
| <10 years | 344 | 86.4 |
| >10 years | 54 | 15.6 |
| Personal history of COVID-19 infection | ||
| No | 383 | 96.2 |
| Yes | 15 | 3.8 |
| Perceived susceptible to COVID-19 | ||
| No | 228 | 57.3 |
| Yes | 170 | 42.3 |
| Know someone infected by COVID-19 | ||
| No | 286 | 71.8 |
| Yes | 112 | 28.2 |
| Know someone died of COVID-19 | ||
| No | 329 | 82.6 |
| Yes | 69 | 17.4 |
| Perceive COVID-19 causes severe illness | ||
| Yes | 253 | 63.6 |
| No | 145 | 36.4 |
| Belief about the likelihood of dying COVID-19 | ||
| No | 312 | 78.4 |
| Yes | 86 | 21.6 |
| Previous diagnosis with chronic disease | ||
| No | 254 | 70.3 |
| Yes | 134 | 29.7 |
Knowledge and Preventive Practice of COVID-19
Only 20.1% of respondents have good knowledge about COVID-19 prevention practice. Only 10.9%, 8.6%, and 4.3% use facemask, wash their hands, and keep social distance based on the recommendation.
The Proportion of Intention to Take COVID-19 Vaccine
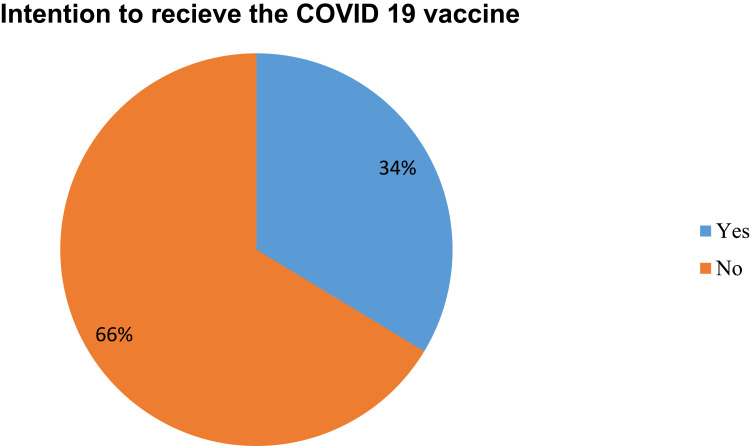
Around 134 (33.7% (95% CI, 0.29–0.38)) of respondents have the intention to take the COVID-19 vaccine (Figure 1).
Figure 1.
Magnitude HIV positive patient to intention to take COVID-19 vaccine in southwest Ethiopia (N = 398).
Factors Associated with intention to receive COVID 19 vaccine
Variables that were significantly associated with the dependent variable at bivariate analysis and with P-value <0.25 were further analyzed in the multivariate analysis to identify their associated effects to take COVID-19 vaccine.
The probability of PLWHA to take COVID-19 vaccine was two (AOR=2.0 (1.08–3.44)) times higher among those who have been diagnosed with chronic diseases (exclude HIV) than those who have not been diagnosed.
PLWHA were male sex who had five (AOR= 5 (2.96–8.68)) time more likely to take COVID-19 vaccine compared with those who were female.
The study also indicated that the odds of intention to take the COVID-19 vaccine were 4.1 times (AOR= 4.1 (2.33–7.31)) times higher among those participants who had good knowledge of COVID-19 practice compared with those who had poor knowledge (Table 3).
Table 3.
Factors Associated with Intention to Receive COVID-19 Vaccine Among HIV Patients in Southwest Ethiopia
| Variable | Intention to Receive COVID-19 Vaccine | OR (95% CI) | AOR (95% CI) | P-value | |
|---|---|---|---|---|---|
| Yes (%) | No (%) | ||||
| Age | |||||
| 18–26 | 21 (5.3) | 86 (21.6) | 1.00 | 1.00 | |
| 27–36 | 37 (9.3) | 122 (30.6) | 1.2 (0.68–2.27) | 0.78 (0.23–1.71) | 0.68 |
| 37–47 | 46 (11.6) | 35 (8.8) | 5.4 (3.52–10.29) | 2.2 (0.47–7.41) | 0.63 |
| >47 | 30 (7.5) | 21 (5.3) | 5.8 (2.82–12.21) | 2.7 (0.57–9.01) | 0.24 |
| Previous diagnosis with chronic disease | |||||
| Yes | 78 (19.6) | 53 (13.3) | 5.4 (3.48–9.07) | 2.0 (1.08–3.44) | 0.027 |
| No | 56 (14.1) | 211 (53.0) | 1.00 | 1.00 | |
| Educational status | |||||
| No education | 24 (6.0) | 72 (18.1) | 1.00 | 1.00 | |
| Primarily | 38 (9.5) | 75 (18.8) | 1.52 (0.83–2.78) | 1.1 (0.62–2.12) | 0.66 |
| Secondary | 52 (13.1) | 100 (25.1) | 1.56 (0.88–2.76) | 1.2 (0.69–2.2) | 0.49 |
| Higher | 20 (5.0) | 17 (4.2) | 3.52 (1.59–7.81) | 2.6 (0.93–6.2) | 0.054 |
| Occupation | |||||
| Unemployed | 23 ((5.8) | 84 (21.1) | 1.00 | 1.00 | |
| Employed | 64 (16.1) | 60 (15.1) | 3.8 (2.18–6.96) | 2.4 (0.68–5.16) | 0.12 |
| Student | 24 (6.0) | 94 (23.6) | 0.9 (0.49–1.77) | 0.6 (0.34–1.32) | 0.45 |
| Others | 23 (5.8) | 26 (6.5) | 3.2 (1.56–6.67) | 2.1 (0.5–4.71) | 0.29 |
| Income | |||||
| <£180 | 19 (4.8) | 57 (14.3) | 1.00 | 1.00 | |
| £180–£300 | 28 (7.0) | 58 (14.6) | 1.4 (0.71–2.88) | 0.5 (0.21–1.21) | 0.62 |
| >£300 | 87 (21.9) | 149 (37.4) | 1.8 (0.92–3.14) | 0.78 (0.28–2.2) | 0.68 |
| Sex | |||||
| Male | 116 (29.1) | 120 (30.2) | 7.8 (1.84–14.63) | 5.0 (2.96–8.68) | 0.001 |
| Female | 18 (4.4) | 145 (36.3) | 1.00 | 1.00 | |
| Marital status | |||||
| Married | 80 (20.1) | 153 (38.4) | 5 (2.31–10.60) | 2.6 (0.95–5.3) | 0.058 |
| Unmarried | 54 (13.6) | 111 (27.9) | 1.00 | 1.00 | |
| Knowledge to COVID-19 preventive practice | |||||
| Good | 62 (15.6) | 28 (7.1) | 7.2 (2.21–12.65) | 4.1 (2.32–7.31) | 0.001 |
| Poor | 72 (18.1) | 236 (59.2) | 1.00 | 1.00 | |
| Duration on ART | |||||
| <10 years | 114 (28.6) | 230 (57.8) | 1.2 (0.67–2.18) | 1.1 (0.71–2.01) | 0.45 |
| >10 years | 20 (5.1) | 34 (8.5) | 1.00 | 1.00 | |
Discussion
This study has assessed the magnitude and factors associated with the intention to receive COVID-19 vaccine among PLWHA. As a result, the magnitude of intention to take COVID-19 vaccine among PLWHA was 33.7% (95% CI, 0.29–0.38), and the independently associated factors with intention to take COVID-19 vaccine were being male, having good knowledge about the COVID-19 vaccine and diagnosis with chronic illness additional to HIV/AIDS.
Even though there was no analogous study conducted on this specific research question within the area, the magnitude of intention to receive the COVID-19 vaccine reported by this study is in line with studies conducted among school teachers in southern Ethiopia (34.2%), Jordan (36.4%), and Hong Kong (37.2%).17–19
The finding of this study is lower than findings documented in studies; in British Columbia, Canada (70.7%), and Foch Hospital, Suresnes, France (71.3%).20,21 A possible explanation could be that these studies vary such that the observed discrepancy could be due to geographical variation of the region selected, the methodology adopted, and the characteristics of the study populations. This implies the vaccine hesitancy and highlights the strong need necessary to promote COVID-19 vaccine among PLWHA.
This finding showed that the respondents who had good knowledge about COVID-19 vaccine were A 4.1 times compared with those who had poor knowledge. This finding agrees with a study done in southern Ethiopia, Pakistan, and U.S.A.22–24 It might be due to having good knowledge about a COVID-19 vaccine being a prerequisite for using it. Therefore, from this study, we can clearly understand that we are still backward towards COVID-19 vaccine awareness creation since less than two-thirds of the participants had good knowledge of the vaccine.
In the present study, the male sex was five times more likely to have the intention to take COVID-19 vaccine compared to females. Similar findings have been evidenced in Wolaita Sodo, southern Ethiopia, Northern Ghana, New York, and Israel.14,25–27 This difference may be due to males having better health-seeking behavior than females in the current study context, which helps males to have more knowledge about COVID-19 vaccine. Therefore, addressing female PLWHA is important to enhance COVID-19 vaccine acceptance.
Furthermore, respondents whoever had a diagnosis with a chronic illness additional to HIV were more likely to have the intention to take COVID-19 vaccine than those not diagnosed with a chronic illness. This finding is supported by the study in southwestern Ethiopia.28 This may be due to the reason people know that patients diagnosed with chronic disease were at high risk for severe infection and death by COVID-19 infection.
Finally, this study has some limitations and strengths to be noted. The study tried to address the determinant factor of intention to take COVID-19 vaccine among PLWHA, which more affects with severe illness and death if affected by COVID-19. The limitation of this study is the design. The cross-sectional study made it impossible to draw a causal relationship. The other end of this study does not include the political and other community factors.
Conclusion and Recommendation
The overall intention to take COVID-19 vaccine among PLWHA is low. Therefore, in light of this finding, there is a need to improve intention to receive COVID-19 vaccine by strengthening and scale-up intervention geared towards a focus on PLWHA without chronic illness and increasing knowledge on COVID-19 vaccine and given to community education about COVID-19 vaccine through the involvement of female PLWHA to achieve the 2021 goal of Ethiopian for 20% of population vaccination.
Acknowledgments
The authors would like to thank Butajira hospital administration for their cooperation in providing information and support letters. The authors would like to provide our gratitude to Wolkite University for its ethical approval. Finally, we are grateful to all data collectors and study participants for their valuable contributions.
Funding Statement
This study did not receive any specific grants from funding agencies, governmental or other organizations.
Abbreviations
PLWHA, people living with HIV/AIDS; WHO, World Health Organization; AOR, adjusted odds ratio; ART, antiretroviral therapy; CI, confidence interval; COR, crude odds ratio.
Data Sharing Statement
The corresponding author could obtain a full data set and other materials relating to this study upon reasonable request.
Ethical Approval and Consent to Participate
Helsinki’s declaration was followed to undertake this study. We obtained a letter of ethical clearance from Wolkite University College of Medical and Health Science Research, Community Services, and Industry Linkage with reference no. 010/13. We also took a supportive letter from Butajira Hospital. After the data collector informed the purpose and objective of the study, they obtained written consent from each study participant. All information gained during data collection was kept confidential, and we did not record any personal identification on the questionnaire. Participants were informed about their right to withdraw from the study at any time if they were not comfortable with the questionnaire.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Kumar D, Malviya R, Sharma PK. Corona virus: a review of COVID-19. EJMO. 2020;4(1):8–25. [Google Scholar]
- 2.Malik YS, Sircar S, Bhat S, et al. How artificial intelligence may help the Covid‐19 pandemic: pitfalls and lessons for the future. Rev Med Virol. 2020;31:e2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sohrabi C, Alsafi Z, O’neill N, et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zomahoun DJ, Burman AL, Snider CJ. Impact of COVID-19 pandemic on global poliovirus surveillance. MMWR Morb Mortal Wkly Rep. 2021;69(5152):1648–1652. doi: 10.15585/mmwr.mm695152a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Africa C. Latest updates on the COVID-19 crisis from Africa CDC; 2019.
- 6.World Health Organization. COVID-19 vaccines: safety surveillance manual; 2021.
- 7.Singh B, Chattu VK. Prioritizing ‘equity in COVID-19 vaccine distribution through global health diplomacy. Health Promot Perspect. 2021;11(3):281–287. doi: 10.34172/hpp.2021.36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tesfaye LM. Ethiopia introduces the COVID-19 vaccine in a national launching ceremony; 2021.
- 9.Arora NK, Das MK. COVID-19 vaccine development and the way forward. Indian J Public Health. 2020;64(6):108. doi: 10.4103/ijph.IJPH_520_20 [DOI] [PubMed] [Google Scholar]
- 10.Bogart LM, Ojikutu BO, Tyagi K, et al. COVID-19 related medical mistrust, health impacts, and potential vaccine hesitancy among Black Americans living with HIV. J Acquir Immune Defic Syndr. 2021;86(2):200. doi: 10.1097/QAI.0000000000002570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gong C, Song X, Li X, Lu L, Li T. Immunological changes after COVID-19 vaccination in an HIV-positive patient. Int J Infect Dis. 2021. doi: 10.1016/j.ijid.2021.08.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Singh JA. COVID-19 vaccine trials: duty of care and standard of prevention considerations. Vaccine. 2020;38(48):7578. doi: 10.1016/j.vaccine.2020.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alter G, Bingham K, Corey L, et al. Whither COVID-19 vaccines. Nat Biotechnol. 2020;38:1132–1145. doi: 10.1038/s41587-020-0697-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mesele M. COVID-19 vaccination acceptance and its associated factors in Sodo Town, Wolaita Zone, Southern Ethiopia: cross-sectional study. Infect Drug Resist. 2021;14:2361–2367. doi: 10.2147/IDR.S320771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alle YF, Oumer KE. Attitude and associated factors of COVID-19 vaccine acceptance among health professionals in Debre Tabor Comprehensive Specialized Hospital, North Central Ethiopia; 2021: a cross-sectional study. Virus Dis. 2021;32(2):272–278. doi: 10.1007/s13337-021-00708-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Handebo S, Wolde M, Shitu K, Kassie A. Determinant of intention to receive COVID-19 vaccine among school teachers in Gondar City, Northwest Ethiopia. PLoS One. 2021;16(6):e0253499. doi: 10.1371/journal.pone.0253499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Al-Qerem WA, Jarab AS. COVID-19 vaccination acceptance and its associated factors among a Middle Eastern population. Front Public Health. 2021;9:34. doi: 10.3389/fpubh.2021.632914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wong MC, Wong EL, Huang J, et al. Acceptance of the COVID-19 vaccine based on the health belief model: a population-based survey in Hong Kong. Vaccine. 2021;39(7):1148–1156. doi: 10.1016/j.vaccine.2020.12.083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shitu K, Wolde M, Handebo S, Kassie A. Acceptance and willingness to pay for COVID-19 vaccine among school teachers in Gondar City, Northwest Ethiopia. Trop Med Health. 2021;49(1):63. doi: 10.1186/s41182-021-00337-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vallée A, Fourn E, Majerholc C, Touche P, Zucman D. COVID-19 vaccine hesitancy among French people living with HIV. Vaccines (Basel). 2021;9(4):302. doi: 10.3390/vaccines9040302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaida A, Brotto LA, Murray MC, et al. Intention to receive a COVID-19 vaccine by HIV status among a population-based sample of women and gender diverse individuals in British Columbia, Canada. medRxiv. 2021. doi: 10.1101/2021.08.19.21262249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Berihun G, Walle Z, Berhanu L, Teshome D. Acceptance of COVID-19 vaccine and determinant factors among patients with chronic disease visiting Dessie comprehensive specialized hospital, Northeastern Ethiopia. Patient Prefer Adherence. 2021;15:1795. doi: 10.2147/PPA.S324564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guidry JP, Laestadius LI, Vraga EK, et al. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am J Infect Control. 2021;49(2):137–142. doi: 10.1016/j.ajic.2020.11.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Belingheri M, Roncalli M, Riva MA, Paladino ME, Teruzzi CM. COVID-19 vaccine hesitancy and reasons for or against adherence among dentists. J Am Dent Assoc. 2021;152(9):740–746. doi: 10.1016/j.adaj.2021.04.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Agyekum MW, Afrifa-Anane GF, Kyei-Arthur F, Addo B. Acceptability of COVID-19 vaccination among health care workers in Ghana. Adv Public Health. 2021;2021:1–8. doi: 10.1155/2021/9998176 [DOI] [Google Scholar]
- 26.Dror AA, Eisenbach N, Taiber S, et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35(8):775–779. doi: 10.1007/s10654-020-00671-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shaw J, Stewart T, Anderson KB, et al. Assessment of US health care personnel (HCP) attitudes towards COVID-19 vaccination in a large university health care system. Clin Infect Dis. 2021. doi: 10.1093/cid/ciab054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Angelo AT, Alemayehu DS, Dachew AM. Health care workers’ intention to accept COVID-19 vaccine and associated factors in southwestern Ethiopia, 2021. PLoS One. 2021;16(9):e0257109. doi: 10.1371/journal.pone.0257109 [DOI] [PMC free article] [PubMed] [Google Scholar]