Summary
Background
Encouraging and assisting smokers to quit remains a key public health goal. Government and commercial initiatives have nudged smokers towards supported cessation. We tracked long-term trends in Australian smokers’ quit attempt methods across 20 years.
Methods
Data from 11,917 smokers were collected from an annual, cross-sectional, face-to-face, random and representative population survey. The survey measured demographic characteristics, tobacco use, recent quit attempts, nicotine dependence, quit intentions, and recent methods used when attempting to quit. Quit attempt preferences were analysed over time and by smoker characteristics.
Findings
Each year, more smokers attempted to quit than remained quit, with a stable trend over time. Socioeconomic disadvantage and mental health conditions are more likely among smokers, but there was no difference in quit attempts by these characteristics. Quit attempts have risen among those aged 60 years and over whereas other age groups have remained stable. Although trending downwards, unassisted quitting remained the most common method: 1998: 61% and 2017: 40%. Asking a doctor for help/advice (34%) was the most common assisted method in 2017, increasing from 18% in 1998. Methods of quitting varied by smoker characteristics, with supported methods used more often by older, more dependent, socio-economically disadvantaged smokers and those with a mental health condition.
Interpretation
The relative stability of recent quit attempts, persistence in unassisted quitting, and fluctuating preferences for supported cessation methods indicate that it is important for clinicians and policy makers to continue to support quit attempts through a variety of options, tailored to smoker's needs.
Keywords: Quit attempt methods, Trends, Population survey, Smokers
Research in context.
Evidence before this study
Medline (Ovid), Embase and PsychINFO were searched for articles published prior to 10 June 2021 that examined trends in methods of attempting to quit smoking. The following search terms were used: (cig$ OR cigar$ OR nicotine OR tobacco OR smoking OR smoker) AND ‘smoking cessation’ AND 'quit attempt' AND (support OR assist) AND (survey) AND (time OR trend OR wave). The search returned 91 unique articles with all but three articles outside of the scope (e.g. intervention studies, single year or sub-population group studies, or not measuring multiple smoking cessation methods). Of the three relevant studies, the first tracked trends in methods of quitting from 2002 to 2009 among Australian smokers with a recent quit attempt. The second study tracked trends in methods of quitting from 2001 to 2010 among Australian smokers regardless of recent quit attempt. Unassisted quitting was not tracked in either study. There was evidence that medication use increased in line with policy interventions (i.e. reduced cost due to Government subsidy), but whether this trend was temporary or sustained cannot be ascertained from the current literature. The third study compared results from two European surveys (comprised of 27 European Union member states with varying levels of tobacco control policy) conducted five years apart (2012 and 2017). This study reported a decrease in the use of pharmacotherapy and smoking cessation services among current smokers who had ever tried to quit. None of these papers include mental health condition as a co-variate. From these articles, it is not clear whether long-term changes in quit attempt methods have occurred following the increased availability of low-cost smoking cessation supports.
Added value of this study
Our study is the first to use cross-sectional data collected annually over twenty years to track changes in prevalence of common methods used by tobacco smokers to attempt to quit (i.e. nicotine replacement therapy (NRT), prescription medication, asking doctor for help or advice, using telephone counselling services (i.e. Quitline), using app or text messaging services, or quitting unassisted). We demonstrated that critical changes in how smokers approach quitting have occurred in this time. Unassisted quitting, while still the most prevalent method in 2017 (40%), has gradually declined since 1998 (61%). Conversely, asking a doctor for help or advice has increased, initially corresponding with the availability of subsidised prescription medicine in 2008, but maintaining a rate of approximately one third of smokers ever since. In contrast, use of prescribed medication has plateaued at around one fifth of smokers since 2012.
Implications of all the available evidence
Our findings advance the existing literature by identifying important long-term trends in smokers’ use of cessation support. This can guide resource allocation and the development of guidelines and interventions to best support smokers in their attempts to quit. One key implication is the growing importance of tailored approaches to suit the varied needs of smokers. Doctors are recognised as an important source of practical and emotional support and are in a unique position to provide evidence-based support matched to the needs of the smoker. There is great opportunity to increase the utilization of these services through brief interventions, such as the ‘Ask, Advise, Help’ model which has evidence of effectiveness. Another key implication is that unassisted quitting remains a dominant and legitimate method for many.
Alt-text: Unlabelled box
Introduction
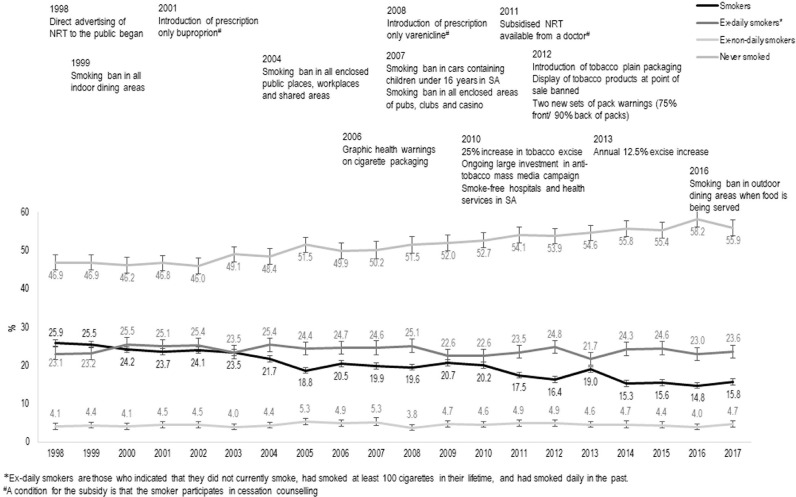
Quitting smoking is profoundly important for health and reducing the burden on the health system, so supporting smokers to quit is a high priority for many Governments. Multi-country data shows that most smokers have tried to quit at least once, approximately one-third of smokers have tried without success in the past 12 months, and multiple attempts are often required before quitting for good, indicating that unsuccessful quit attempts are normal and expected.1 Offering help to quit tobacco use is a core global strategy in reducing smoking prevalence.2 Numerous strategies to address this need have commenced in the past 20 years, including Government policy and the commercialization of cessation products. In Australia, this has included behavioural support (e.g. telephone counselling), as well as increased availability of reduced-cost pharmacotherapy from a physician through the introduction of prescription-only buproprion (2001) and varenicline (2008), and prescribed nicotine patches (2011), to the Australian Pharmaceutical Benefits Scheme (PBS).3 This has occurred against a broader background of population-level strategies to disincentivise smoking (e.g. significant annual tax increases),3 facilitating quitting without external assistance, which is common.4 The commencement of these key tobacco control strategies are summarised in Figure 1 along with the change in smoking status of the population during the same period, showing that smoking prevalence among those aged 15 years and over significantly decreased from 25·9% (95%CI=24·2%−27·7%) in 1998 to 15·8% (95%CI=14·3%−17·4%) in 2017. There are currently no published data available that examines the long-term trends in quit attempt methods by demographic sub-groups (i.e. age, gender, socioeconomic disadvantage, location, mental illness) around this critical period. Identifying trends in smokers’ quit attempt methods is critical for resource allocation and the development of guidelines and interventions that best support smokers in their attempts to quit.
Figure 1.
Trend in smoking prevalence along with commencement of key tobacco control initiatives, 1998–2017.
Early cohort multi-wave data (2002–2009)5 showed that nicotine replacement therapy (NRT) was used by 31% of Australian smokers who had made a quit attempt between baseline and follow-up survey approximately one year later. Behavioural support was less common (11%), and prescription medication increased dramatically from 4·9% in 2007–08 to 23·9% in 2008–09. A cross-sectional multi-wave study (2001–2010)6 of Australian's who had smoked in the past year and reported their use of quit smoking support services during that time found that asking a doctor for help to quit and using medication had increased over time. The study also showed that the most socio-economically disadvantaged smokers were more likely to seek help from a doctor and use prescription medication than the least disadvantaged, but the results were mixed for NRT. Other studies investigating quit attempt methods among smokers who had attempted to quit in the past year have reported a relationship between indicators of socioeconomic advantage and preference for assisted support7,8 but others have found mixed6 or null results.5 A preference among smokers with a recent (past year) quit attempt for assisted cessation methods has been associated with more nicotine-dependent smokers, older age and females.5,7, 8, 9 Furthermore, although data are scarce, people with complex needs such as mental health conditions, indicated that they preferred supported methods when discussing methods of support associated with past and future quit attempts.10
In 2019, while using NRT (17%) and asking a doctor for help to quit (10%) were the most common assisted methods of attempting to quit by Australian smokers in the previous 12 months, 23% had tried to quit by ‘going cold turkey’.11 A 2015 report on current smokers with at least one quit attempt indicated that 38% had never used a supported method, whereas 54% had used NRT and 18% had used the Quitline at least once.12 Interestingly, ex-smokers were more likely to have never used supports (62%) and less likely to have ever used NRT (27%) or the Quitline (4%). European data from 2017 shows that 66% of current smokers who had ever tried to quit had not used assistance when trying to quit in the past.13 Furthermore, rates of using pharmacotherapy (17%) and smoking cessation services (6%) were low and had declined from 2012 (23% and 9%, respectively). These data suggest that evidence-based methods of achieving long-term abstinence, such as a combined behavioural and pharmacological approach,14 are under-utilised. A recent US study showed that only 4% of former smokers who had quit in the previous three years used a combined approach, whereas 22% used only pharmacological methods, and 2% used only behavioural methods to quit smoking.15 Notably, the majority (72%) of former smokers had quit unassisted. Similar results were observed in a review study of the prevalence of unassisted quit attempts among smokers and former smokers,4 although the trend in unassisted quit attempts appeared to decline between 1986 and 2010.4 Unassisted quitting has a long-term success rate of about 3–5% but is a major contributor to reducing smoking prevalence because of the large numbers of smokers who use this method.16
This study aimed to examine preferences in smoking cessation methods by current smokers in an Australian state (South Australia (SA)), by a range of demographic and smoking characteristics, from 1998 to 2017. The results will help to inform tobacco control policy and the promotion of smoking cessation in response to current trends and preferences.
Methods
Procedure
Data were collected from 1998 to 2017 via the SA Health Omnibus Survey (HOS); an annual, cross-sectional, face-to-face, random and representative population survey conducted in spring (September-December). Each survey sampled households in locations with at least 1000 people using a clustered, multi-staged and self-weighted area design. Within each household one person aged 15 years or over was selected for a face-to-face structured interview with a trained interviewer. The HOS methodology has remained consistent over time, enabling direct comparison of year-by-year data. A total of 59,129 interviews were conducted, 11,917 of which were with current smokers. The sample size ranged from a low of 2398 in 2007 to a high of 3055 in 2012. Participation rates ranged from 64.3% in 2009 to 82.0% in 1998. Ethics approval was granted by the South Australian Department of Human Services/Department of Health and Ageing Human Research Ethics Committee and the University of Adelaide Human Research Ethics Committee.
Measurements
Demographic characteristics included age, gender, and postcode of home address. Postcode was matched to Australia's Census of Population and Housing, which has a classification tool for region and a ranking tool for area-level socioeconomic disadvantage and region.17 The Index of Relative Disadvantage is a ranking scale that is derived from multiple indicators (e.g. income, employment, qualifications) to classify the socioeconomic disadvantage score for each area. This score was converted into a dichotomous variable of most (scored in the bottom 40%) versus least socioeconomic disadvantage. Presence of a mental health condition was ascertained if a person indicated “yes” to either receiving treatment for anxiety, depression or any other mental health problem or receiving a disability pension for a psychological or psychiatric illness. Smoking characteristics included current smoking status, prior quit attempts, heaviness of smoking and quit intentions. Participants were asked “Do you currently smoke cigarettes, cigars, pipes or any other tobacco products: daily; at least weekly (but not daily); less often than weekly; or not at all”, with any response other than “not at all” resulting in a “current smoker” classification. Of current smokers, those with a recent quit attempt were identified if they responded with 1 or more to the question: “How many serious attempts have you made to quit smoking in the last year?”. To determine heaviness of smoking, participants were asked “on average how many cigarettes do you smoke per day (daily smokers)/each week (weekly smokers)?” with responses coded as “10 or less”, “more than 10″, or not stated. Interest in quitting was determined by asking participants to indicate (yes, no, can't say) if they were “seriously considering quitting within the next 6 months”.
With the exception of 2009 and 2015, participants who indicated that they were a smoker with a recent (past 12 months) serious quit attempt were asked by a trained interviewer: “During the past year, have you done any of the following…”, with the interviewer prompting “anything else” after each response given. A core set of response options were presented each year: “Used Nicotine Replacement Therapy”, “Asked your doctor for advice or help to quit”, and “Called the Quitline”. Additional response options were added in subsequent surveys as new supports became available. “Bupropion (Zyban)” [2002–2012] and “Varenicline (Champix)” [2010–2012] were initially presented separately, then as a combined option from 2013 onwards (“Used quit smoking medication (e.g. Zyban, Bupropion or Champix)”). Response options regarding a specific or general app or text service were added in 2011 (e.g. “Used Quit app”) and “Been referred to the Quitline by your doctor” was added in 2012. The interviewer could record “None of these” if none of the options were selected. Participants who had not used any of these supports were classified as having a quit attempt with no support (i.e. “unassisted quit attempt/s”).
Analysis
Data were analysed using Stata version 1518 using the “svy” function to control for the complex sample design and allow for the calculation of 95% confidence intervals (CIs). There was minimal missing data as the interviewer was permitted to record a “Can't say/not stated” response, which has been included as a subgroup for smoking characteristic variables. Participants were excluded from an analysis when data were missing, which occurred for only 30 (total N = 59,127) participants where socioeconomic status and region was unavailable, and for 13 participants where smoking status was unavailable. The “subpop” command, which uses all cases to calculate standard errors, was used when selecting only those participants from the full sample who answered questions relating to their smoking behaviours and quit attempts. A series of logistic regression models were constructed to examine whether demographic (age, gender, socioeconomic disadvantage, region) and smoking characteristics (quit intentions, heaviness of smoking) changed over time as predictors of recent (past 12 months) quit attempts, and the following quit attempt methods: no support, using NRT, using quit smoking medication, asking a doctor for advice or help to quit, referral to the Quitline by a doctor, Called the Quitline, and used a Quit app or text messaging service. A quadratic (squared) term for survey year was included to detect any non-linearity. Interactions between predictor variables and survey year and the quadratic term for survey year were tested for improvement to model fit for each outcome variable and retained if the likelihood ratio-test was <0·10. The margins command was used to estimate the probabilities and Average Marginal Effects (AME) for each of the predictors based on the results of the corresponding logistic regression model. Interaction effects were graphed and tested for marginal effects at representative values of the following survey years: 1998, 2007 and 2017 (see Supplementary File). The same procedure was used to produce a logistic regression model of demographic predictors of smoking status (smoker versus non-smoker) over time to provide context on the changing demographic profile of smokers. The models were re-run using data from 2005 to 2017 to allow for the inclusion of mental health condition as a predictor of each of the outcome variables. Statistical significance was set at p<0·05. Data were first weighted by chance of selection, and then by age, gender and area of residence to be representative of the South Australian population.
Role of funding source
The funder had no involvement in any aspect of the study.
Results
There are differences in the demographic characteristics of smokers, some of which have changed over time (see Supplementary File: Table 1, Fig. 1). The largest change occurred across age groups. Those aged 15–29 years and 30–44 years had the highest likelihood of smoking in 1998, but both declined over time, with a steeper decline among 15–29 year olds. Conversely, the likelihood of smoking among those aged 45 years and over has remained stable over time. By 2017, those aged 30–59 years had the highest likelihood of smoking. The probability of smoking decreased at a more rapid rate among those living in metropolitan compared to country areas. The probability of smoking was consistently higher among males than females, among the most compared to the least disadvantaged people, and among those with, compared to without a mental health condition.
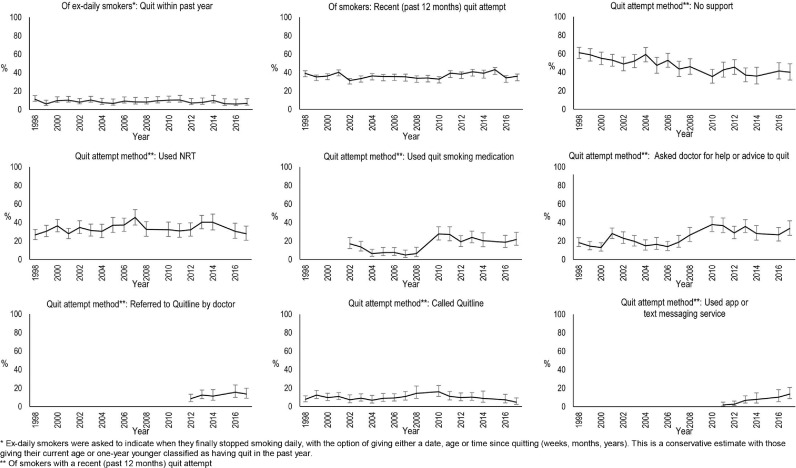
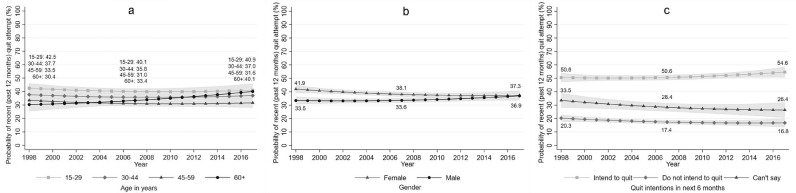
Figure 2 displays the proportion of smokers who had made a quit attempt in the past year, with the results ranging from 31·3% (95%CI =27·5%−35·3%) in 2002 to 43·1% (95%CI=37·8%−48·5%) in 2015. Figure 2 also shows that in any given year, the proportion of ex-smokers who quit in the past year is between 6% and 11%. The predictive margins, derived from the logistic regression model (Table 1) for recent (past year) quit attempt indicated that the average adjusted probability of having a recent quit attempt was 36·3% (95%CI=35·3%−37·3%), which did not vary significantly over time (1998=37·2% [95%CI=34·8%−39·6%], 2007=35·6% [34·1%−37·0%], 2017=37·1% 95%CI=34·2%−40·1%]) or by socioeconomic status, region or mental health condition. Survey year did moderate the relationship between quit attempt and age, gender and quit intentions, although the effects over time were small and mostly non-significant. As shown in Figure 3a, there was an age gradient from youngest to oldest age groups in probability of having a recent quit attempt in 1998, which persisted through to 2017 for 15–59 year olds. However, as shown in Table 1, the difference in probability between those aged 15–29 years and 60 years and over had become non-significant by 2017 (p = 0.812) due to the rise in probability of having a quit attempt among those aged 60 and over (9.7 percentage point (pp) change, p = 0.011). Figure 3b shows that the probability of a recent quit attempt was initially higher for females than males but over time the difference narrowed to become non-significant. Figure 3c shows that having a recent quit attempt was more likely for those with than those without quit intentions, and the difference between the two groups widened over time. Survey year did not moderate the probability of having a recent quit attempt according to heaviness of smoking, but there was a gradient with lighter smokers having a higher probability than heavier smokers and those not quantifying cigarettes per day.
Figure 2.
trends over time in the proportion of smokers with a recent quit attempt, proportion of ex-daily smokers who quit within the past year, and the proportion of smokers with a recent quit attempt using the following quit attempt methods: no support, used NRT, used quit smoking medication, asked doctor for help or advice to quit, referred to the Quitline by a doctor, called the Quitline, and/or used an app or text messaging service.
Table 1.
Likelihood of having a recent (past 12 months) quit attempt by demographic and smoking characteristics (n = 11,830): logistic regression with predictive margins (%) and average marginal effects (AME).
| Logistic Regression |
Predictive margins |
AME^ | ||||
|---|---|---|---|---|---|---|
| aOR | 95%CI | p-value | % | 95%CI | p-value | |
| Year | 0·98 | 0·94,1·01 | 0·199 | |||
| Year by Year | 1·00 | 1·00,1·00 | 0·303 | |||
| Age group (years) | ||||||
| 15–29 | Ref | See Fig. 3a | ||||
| 30–44 | 0·80 | 0·64,1·00 | 0·048 | |||
| 45–59 | 0·65 | 0·50,0·84 | 0·001 | |||
| 60+ | 0·54 | 0·39,0·74 | <0·0001 | |||
| 30–44 years by Year | 1·00 | 0·98,1·02 | 0·876 | |||
| 45–59 years by Year | 1·00 | 0·97,1·02 | 0·856 | |||
| 60+ years by Year | 1·03 | 1·00,1·06 | 0·033 | |||
| Gender | ||||||
| Female | Ref | See Fig. 3b | ||||
| Male | 0·65 | 0·55,0·78 | <0·0001 | |||
| Male by year | 1·02 | 1·00,1·04 | 0·013 | |||
| Socioeconomic disadvantage | ||||||
| Most | 1·09 | 0·98,1·20 | 0·099 | 37·1 | 35·7,38·4 | 0·098 |
| Least | Ref | 35·4 | 33·9,36·9 | |||
| Region | ||||||
| Metropolitan | Ref | 36·4 | 35·2,37·5 | |||
| Country | 0·99 | 0·89,1·10 | 0·852 | 36·2 | 34·3,38·0 | 0·852 |
| Heaviness of smoking | ||||||
| 10 or fewer cigarettes per day | Ref | 39·6 | 38·0,41·2 | |||
| More than 10 per day | 0·84 | 0·76,0·93 | 0·001 | 36·1 | 34·7,37·4 | 0·001 |
| Quantity not provided | 0·43 | 0·35,0·52 | <0·0001 | 23·5 | 20·6,26·4 | <0·0001 |
| Quit intentions in next 6 months | ||||||
| Intend to quit | Ref | See Fig. 3c | ||||
| Do not intend to quit | 0·24 | 0·20,0·30 | <0·0001 | |||
| Can't say | 0·50 | 0·37,0·66 | <0·0001 | |||
| Do not intend to quit by Year | 0·98 | 0·96,1·00 | 0·036 | |||
| Can't say by Year | 0·97 | 0·95,1·00 | 0·039 | |||
| Mental health condition | 2005 to 2017 (n = 6785) | |||||
| No | Ref | 36·1 | 34·6,37·5 | |||
| Yes | 1·15 | 0·98,1·35 | 0·083 | 38·9 | 35·9,41·8 | 0·085 |
Comparing percentage point difference in predictive margins compared to reference group for average values when no interaction is present (AME). Representative values for the years of 1998, 2007 and 2017 are available in the Supplementary data file. Notes: aOR=adjusted Odds Ratio, 95%CI=95% Confidence Interval Lower and Upper.
Figure 3.
Estimated probability of having a recent (past year) quit attempt (%) from 1998 to 2017 by (a) age, (b) gender, and (c) intentions to quit.
Figure 2 displays the unadjusted proportions of the types of cessation support used by smokers with a recent quit attempt over time. Unassisted quit attempts were the most used method in both 1998 (61·1%; 95%CI=54·9%−67·0%) and 2017 (40·0%; 95%CI=31·6%−49·2%), although the proportion had generally declined over time. In 1998, using NRT (26·6%; 95%CI=21·5%−32·4%) was more common than asking a doctor for help or advice (18·3%; 95%CI=14·0%−23·5%), whereas in 2017, asking a doctor for help or advice (33·5%; 95%CI=26·1%−41·9%) was more common than using NRT (27·8%; 95%CI=20·8%−36·1%), with the change over time driven by an increase in speaking with a doctor while NRT use plateaued. The use of each method has fluctuated over time with the peak (relative to 2017) for unassisted quitting, NRT and calling the Quitline occurring in 1998, 2007, and 2010, respectively. Conversely, the use of quit smoking medication and asking a doctor for help or advice became more common in recent years (2010–17) compared to previous years (1998–2008) and using app and text messaging services have gradually increased since 2011.
Results for having a quit attempt with no support, using prescription medication, and asking a doctor for advice or help to quit are displayed in Table 2 and Supplementary Tables 3 to 5, using NRT is displayed in Table 3 and Supplementary Table 6, and doctor referral to the Quitline, calling the Quitline and using a Quit app or text messaging service are displayed in Table 4 and Supplementary Tables 7 to 9.
Table 2.
Likelihood of having a quit attempt with no support (n = 3848), using prescription medication (n = 2732), and asking a doctor for advice or help to quit (n = 3843) by demographic and smoking characteristics: logistic regressions with predictive margins (%) and average marginal effects (AME).
| No Support |
Used Prescription medication (2002–2017) |
Asked doctor for advice or help to quit |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Logistic Regression |
Predictive margins |
AME^ |
Logistic Regression |
Predictive margins |
AME^ |
Logistic Regression |
Predictive margins |
AME^ |
||||
| aOR (95%CI) | p-value | % (95%CI) | p-value | aOR (95%CI) | p-value | % (95%CI) | p-value | aOR (95%CI) | p-value | % (95%CI) | p-value | |
| Year | 0·97 (0·95–0·99) | 0·001 | 1·06 (1·02,1·10) | 0·001 | 1·07 (1·04,1·10) | <0·0001 | ||||||
| Age group (years) | ||||||||||||
| 15–29 | Ref | 57·0 (53·7,60·4) | Ref | 8·6 (6·2,11·0) | Ref | 17·0 (14·5,19·6) | ||||||
| 30–44 | 0·55 (0·45,0·67) | <0·0001 | 43·7 (40·8,46·5) | <0·0001 | 2·36 (1·63,3·42) | <0·0001 | 17·5 (14·7,20·4) | <0·0001 | 1·74 (1·37,2·20) | <0·0001 | 25·7 (23·1,28·3) | <0·0001 |
| 45–59 | 0·59 (0·48,0·74) | <0·0001 | 45·3 (41·6,48·9) | <0·0001 | 2·75 (1·87,4·02) | <0·0001 | 19·7 (16·4,22·9) | <0·0001 | 1·83 (1·42,2·35) | <0·0001 | 26·6 (23·5,29·7) | <0·0001 |
| 60+ | 0·67 (0·52,0·87) | 0·003 | 48·2 (43·4,52·9) | 0·003 | 2·41 (1·57,3·69) | 0·0001 | 17·8 (13·9,21·7) | 0·0001 | 1·86 (1·39,2·48) | <0·0001 | 26·9 (22·8,30·9) | 0·0001 |
| Gender | ||||||||||||
| Female | Ref | 45·2 (42·8,47·5) | Ref | 16·0 (13·9,18·0) | Ref | 27·0 (24·9,29·1) | ||||||
| Male | 1·37 (1·17,1·59) | 0·0001 | 52·0 (49·4,54·6) | 0·0001 | 0·72 (0·35,1·49) | 0·378 | 15·4 (13·2,17·7) | 0·741 | 0·67 (0·56,0·80) | <0·0001 | 20·4 (18·3,22·5) | <0·0001 |
| Male by year | – | – | 1.02 (0.97, 1.08) | 0.408 | – | – | – | – | ||||
| Socioeconomic disadvantage | ||||||||||||
| Most | 1·31 (0·98,1·76) | 0·072 | 50·1 (47·6,52·5) | 0·117 | 1·05 (0·81,1·36) | 0·692 | 16·0 (14·0,18·0) | 0·691 | 1·27 (1·06,1·53) | 0·011 | 25·2 (23·2,27·3) | 0·010 |
| Least | Ref | 47·2 (44·5,49·9) | Ref | 15·3 (12·9,17·8) | Ref | 21·3 (19·0,23·5) | ||||||
| Most by Year | 0·98 (0·96,1·01) | 0·278 | NS | – | – | – | – | |||||
| Region | ||||||||||||
| Metropolitan | Ref | See Fig. 4a & Supp Table 3 | Ref | 14·7 (12·9,16·5) | Ref | 23·9 (22·1,25·7) | ||||||
| Country | 1·47 (1·05,2·06) | 0·024 | 1·25 (0·95,1·63) | 0·107 | 17·5 (14·5,20·5) | 0·118 | 0·93 (0·76,1·14) | 0·473 | 22·7 (19·9,25·5) | 0·469 | ||
| Country by Year | 0·97 (0·94,1·00) | 0·064 | – | – | – | – | ||||||
| Heaviness of smoking (Cigarettes per day) | ||||||||||||
| 10 or fewer | Ref | 59·0 (56·3,61·7) | Ref | 9·5 (7·7,11·3) | Ref | |||||||
| More than 10 | 0·39 (0·33,0·46) | <0·0001 | 37·5 (35·1,39·9) | <0·0001 | 2·73 (2·08,3·58) | <0·0001 | 21·6 (19·1,24·1) | <0·0001 | 2·82 (1·96,4·06) | <0·0001 | See Fig. 4b & Supp Table 5 | |
| Quantity not provided | 2·20 (1·49,3·24) | 0·0001 | 75·1 (68·4,81·7) | <0·0001 | 0·69 (0·30,1·63) | 0·401 | 6·9 (1·7,12·0) | 0·340 | 0·57 (0·20,1·61) | 0·288 | ||
| More than 10 by Year | – | – | – | – | 0·98 (0·95,1·01) | 0·146 | ||||||
| Qty not provided by Year | – | – | – | – | 1·00 (0·93,1·08) | 0·950 | ||||||
| Quit intentions in next 6 months | ||||||||||||
| Intend to quit | Ref | 44·4 (42·3,46·5) | Ref | 16·6 (14·8,18·5) | Ref | 26·2 (24·4,28·1) | ||||||
| Do not intend to quit | 2·21 (1·81,2·71) | <0·0001 | 62.0 (58·1,65·8) | <0·0001 | 0.72 (0.51,1.01) | 0.060 | 12·8 (9·5,16·1) | 0·045 | 0·47 (0·36,0·61) | <0·0001 | 15.0 (12·1,17·9) | <0·0001 |
| Can't say | 1·65 (1·26,2·17) | 0·0003 | 55·6 (49·8,61·3) | 0·0003 | 0·78 (0·49,1·24) | 0·300 | 13·7 (8·8,18·6) | 0·271 | 0·66 (0·49,0·90) | 0·008 | 19·5 (15·2,23·8) | 0·004 |
| Mental health condition | ||||||||||||
| No | Ref | 43·8 (41·0,46·5) | Ref | 16·8 (14·7,18·9) | Ref | 25·4 (23·0,27·8) | ||||||
| Yes | 0·74 (0·56,0·97) | 0·032 | 37·2 (31·9,42·6) | 0·029 | 1·05 (0·76–1·48) | 0·767 | 17·4 (13·6,21·3) | 0·769 | 1·82 (1·39,2·38) | <0·0001 | 37·2 (32·1,42·3) | <0·0001 |
Comparing percentage point difference in predictive margins compared to reference group for average values when no interaction is present (AME). Representative values for the years of 1998, 2007 and 2017 are available in the Supplementary data file. Notes: aOR=adjusted Odds Ratio, 95%CI=95% Confidence Interval Lower and Upper.
Table 3.
Likelihood of having a quit attempt using Nicotine Replacement Therapy (NRT) by demographic and smoking characteristics (n = 3843): logistic regression with predictive margins (%) and average marginal effects (AME).
| Logistic Regression |
Predictive margins |
AME^ | ||||
|---|---|---|---|---|---|---|
| aOR | 95%CI | p-value | % | 95%CI | p-value | |
| Year | 1·13 | 1·06,1·20 | 0·0001 | |||
| Year by Year | 0·99 | 0·99,1·00 | 0·0002 | |||
| Age group | ||||||
| 15–29 years | Ref | 25·8 | 22·8,28·8 | |||
| 30–44 years | 1·77 | 1·44,2·18 | <0·0001 | 37·4 | 34·6,40·2 | <0·0001 |
| 45–59 years | 1·61 | 1·28,2·03 | <0·0001 | 35·4 | 31·9,38·8 | <0·0001 |
| 60+ years | 1·62 | 1·23,2·12 | 0·001 | 35·4 | 30·8–40·0 | 0·001 |
| Gender | ||||||
| Female | Ref | 34·3 | 32·1,36·5 | |||
| Male | 0·90 | 0·77,1·05 | 0·194 | 32·1 | 29·7,34·6 | 0·193 |
| Socioeconomic disadvantage | ||||||
| Most | 0·53 | 0·39,0·72 | <0·0001 | See Fig. 4d | ||
| Least | Ref | |||||
| Most by Year | 1·04 | 1·01,1·07 | 0·004 | |||
| Region | ||||||
| Metropolitan | Ref | 34·5 | 32·5,36·5 | |||
| Country | 0·83 | 0·69,0·99 | 0·042 | 30·5 | 27·4,33·7 | 0·039 |
| Heaviness of smoking | ||||||
| 10 or fewer cigarettes per day | Ref | See Fig. 4e | ||||
| More than 10 per day | 2·67 | 1·94,3·68 | <0·0001 | |||
| Quantity not provided | 0·95 | 0·44,2·08 | 0·901 | |||
| More than 10 per day by Year | 0·97 | 0·94,1·00 | 0·027 | |||
| Quantity not provided by Year | 0·94 | 0·87,1·01 | 0·099 | |||
| Quit intentions in next 6 months | ||||||
| Intend to quit | Ref | See Fig. 4f | ||||
| Do not intend to quit | 0·76 | 0·52,1·13 | 0·176 | |||
| Can't say | 0·65 | 0·39,1·10 | 0·109 | |||
| Do not intend to quit by Year | 0·95 | 0·91,0·99 | 0·013 | |||
| Can't say by Year | 1·01 | 0·96,1·06 | 0·680 | |||
| Mental health condition | 2005 to 2017 (n = 2041) | |||||
| No | Ref | 35·4 | 32·8,38·1 | |||
| Yes | 0·92 | 0·71,1·20 | 0·536 | 33·7 | 28·7,38·7 | 0·533 |
Comparing percentage point difference in predictive margins compared to reference group for average values when no interaction is present (AME). Representative values for the years of 1998, 2007 and 2017 are available in the Supplementary data file. Notes: aOR=adjusted Odds Ratio, 95%CI=95% Confidence Interval Lower and Upper.
Table 4.
Likelihood of having a quit attempt with a referral to the Quitline by a doctor (n = 897), calling the Quitline (n = 3843), and using a Quit app or text messaging service (n = 1042) by demographic and smoking characteristics: logistic regressions with predictive margins (%) and average marginal effects (AME).
| Referral to Quitline by doctor (2012–2017) |
Called Quitline |
Used Quit app or text messaging service (2011–2017) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Logistic Regression |
Predictive margins |
AME^ |
Logistic Regression |
Predictive margins |
AME^ |
Logistic Regression |
Predictive margins |
AME^ |
||||
| aOR(95%CI) | p-value | %(95%CI) | p-value | aOR(95%CI) | p-value | %(95%CI) | p-value | aOR(95%CI) | p-value | %(95%CI) | p-value | |
| Year | 1·10 (0·97,1·24) | 0·132 | 1·09 (1·00,1·19) | 0·041 | 1·34 (1·15,1·56) | <0·0001 | ||||||
| Year by Year | – | – | 1·00 (0·99,1·00) | 0·031 | – | – | ||||||
| Age group (years) | ||||||||||||
| 15–29 | Ref | 8·1 (3·9,12·3) | Ref | 8·9 (7·0,10·8) | Ref | 9·4 (4·7,14·1) | ||||||
| 30–44 | 2·22 (1·14,4·33) | 0·019 | 15·9 (11·5,20·3) | 0·010 | 1·30 (0·96,1·77) | 0·090 | 11·2 (9·4,13·1) | 0·085 | 1·28 (0·64,2·57) | 0·489 | 11·5 (7·8,15·2) | 0·478 |
| 45–59 | 1·67 (0·81,3·47) | 0·168 | 12·6 (8·2,17·1) | 0·155 | 1·06 (0·75,1·49) | 0·745 | 9·4 (7·4,11·3) | 0·745 | 0·25 (0·10,0·61) | 0·002 | 2·7 (1·1,4·3) | 0·008 |
| 60+ | 1·08 (0·47,2·46) | 0·858 | 8·7 (4·2,13·1) | 0·858 | 0·71 (0·44,1·13) | 0·151 | 6·5 (4·2,8·9) | 0·130 | – | – | ||
| Gender | ||||||||||||
| Female | Ref | 13·8 (10·2,17·5) | Ref | 11·7 (10·3, 13·2) | Ref | 8·2 (5·6,10·9) | ||||||
| Male | 0·76 (0·49,1·18) | 0·224 | 11·0 (8·1,14·0) | 0·229 | 0·63 (0·50,0·81) | 0·0003 | 7·9 (6·5,9·3) | 0·0002 | 0·75 (0·42,1·34) | 0·326 | 6·4 (3·9,9·0) | 0·322 |
| Socioeconomic disadvantage | ||||||||||||
| Most | 0·73 (0·45,1·18) | 0·199 | 10·9 (8·2,13·7) | 0·209 | 1·28 (1·00,1·63) | 0·047 | 10·6 (9·1,12·1) | 0·046 | 0·45 (0·26,0·78) | 0·004 | 5·1 (3·2,6·9) | |
| Least | Ref | 14·2 (10·0,18·4) | Ref | 8·6 (7·2,10·0) | Ref | 10·1 (6·8,13·3) | 0·006 | |||||
| Region | ||||||||||||
| Metropolitan | Ref | 9·6 (7·2,12·1) | Ref | 10·9 (9·6,12·2) | Ref | See Fig. 4c & Supp Table 9 | ||||||
| Country | 1·96 (1·20,3·18) | 0·007 | 16·8 (11·9,21·7) | 0·012 | 0·66 (0·49,0·88) | 0·005 | 7·5 (5·7,9·2) | 0·002 | 0·01 (0·00,1·69) | 0·080 | ||
| Country by Year | – | – | 1·26 (0·96,1·65) | 0·094 | ||||||||
| Heaviness of smoking (Cigarettes per day) | ||||||||||||
| 10 or fewer | Ref | 8·9 (5·9,11·9) | Ref | 7·0 (5·7,8·3) | Ref | 7·8 (5·1,10·5) | ||||||
| More than 10 | 2·01 (1·26,3·21) | 0·004 | 16·0 (12·4,19·7) | 0·003 | 1·98 (1·52,2·57) | <0·0001 | 12·7 (11·0,14·4) | <0·0001 | 0·81 (0·45,1·47) | 0·496 | 6·5 (4·1,9·0) | 0·498 |
| Quantity not provided | 0·43 (0·09,2·05) | 0·292 | 4·1 (−1·8,10·1) | 0·155 | 0·62 (0·29,1·33) | 0·219 | 4·5 (1·4,7·6) | 0·145 | – | – | ||
| Quit intentions in next 6 months | ||||||||||||
| Intend to quit | Ref | 13·8 (11.0,16·5) | Ref | 11·5 (10·2,12·8) | Ref | 7·3 (5·2,9·4) | ||||||
| Do not intend to quit | 0·31 (0·14,0·67) | 0·003 | 4·9 (1·5,8·2) | 0·0001 | 0·46 (0·32,0·66) | <0·0001 | 5·7 (3·9,7·6) | <0·0001 | 1·14 (0·54,2·38) | 0·731 | 8·2 (3·5,12·8) | 0·738 |
| Can't say | 0·67 (0·30,1·50) | 0·328 | 9·8 (3·1,16·4) | 0·272 | 0·26 (0·14,0·47) | <0·0001 | 3·4 (1·5,5·2) | <0·0001 | 0·47 (0·13,1·72) | 0·253 | 3·8 (−0·6,8·1) | 0·141 |
| Mental health condition | 2012 to 2017 (n = 896) | 2005 to 2017 (n = 2041) | 2011 to 2017 (n = 1042) | |||||||||
| No | Ref | 11·8 (9·2,14·5) | Ref | 8·9 (7·4,10·4) | Ref | 7·4 (5·3,9·5) | ||||||
| Yes | 1·19 (0·71,2·00) | 0·501 | 13·7 (8·8,18·6) | 0·514 | 1·92 (1·36,2·70) | 0·0002 | 15·5 (11·8,19·3) | 0·001 | 0·86 (0·45,1·62) | 0·632 | 6·5 (3·3,9·7) | 0·621 |
Comparing percentage point difference in predictive margins compared to reference group for average values when no interaction is present (AME). Representative values for the years of 1998, 2007 and 2017 are available in the Supplementary data file. Notes: aOR=adjusted Odds Ratio, 95%CI=95% Confidence Interval Lower and Upper.
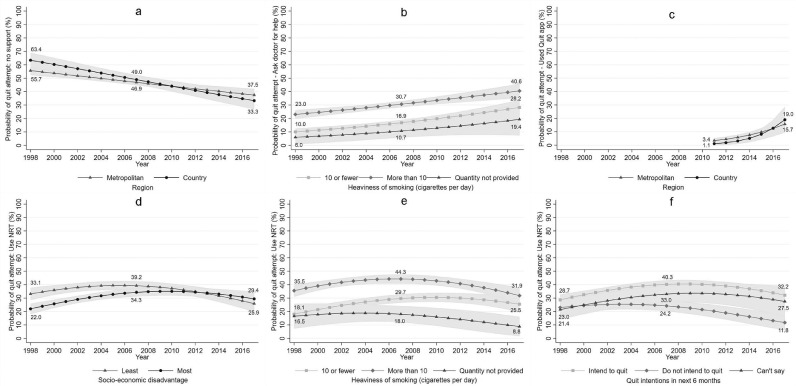
No support
The average adjusted probability for a recent quit attempt without any formal support decreased over time (1998=58·3% [95%CI=55·3%−61·2%], 2007=47.6% [95%CU=45·7%−49·5%], 2017=36·1% [95%CI=32·4%−39·9%). The trends over time were mostly consistent across demographic and smoking characteristic subgroups, except for region. As shown in Figure 4a, those living in country areas compared to metropolitan areas had a steeper decline in having a quit attempt without support, but a statistically significant difference between the two groups was only observed in 1998 (7·75pp, p = 0·022). On average across all years (see Table 2), the probability of having a quit attempt without support was higher among smokers aged 15–29 years, males, lighter smokers, those without serious quit intentions and those without a mental health condition, compared to their demographic counterparts.
Figure 4.
Estimated probability (%) of using various methods of support during a quit attempt from 1998 to 2017, including (a) no support, (b) Asking a doctor for help or advice to quit by heaviness of smoking, (c) using a quit app or text messaging service by region, (d) NRT by socioeconomic disadvantage, (e) NRT by heaviness of smoking, (f) NRT by quit intentions,.
Used prescription medication
The average adjusted probability for using medication as a quit attempt method increased over time (1998=8·0% [95%CI=5·6%−10·4%], 2007=13·7% [95%CI=12·0%−15·4%], 2017=23·6% [95%CI=19·8% −27·4%). Survey year did not moderate the effect of any other variables on using prescription medication. On average across all years (see Table 2), the probability of using quit medication was higher among adults aged 30 years and over compared to 15–29 year olds, and heavier compared to lighter smokers.
Asked doctor for advice or help to quit
The average adjusted probability for asking a doctor for advice or help to quit increased over time (1998=16·6% [95%CI=14·5%−18·7%], 2007=23·8% [95%CI=22·2% −25·3%], 2017=34·2% [95%CI=30·4%−37·9%). Only heaviness of smoking was modified by survey year (see Figure 4b). There was a greater increase in probability of asking a doctor for help observed in those not quantifying the number of cigarettes per day compared to the other groups, whereas heavier smokers were consistently more likely than lighter smokers to ask a doctor for help over time. On average across all years (see Table 2), the probability of asking a doctor for help to quit was higher among adults aged 30 years and over, females, those with the most socioeconomic disadvantage, with serious quit intentions and with a mental health condition, compared to their demographic counterparts.
Used NRT
The average adjusted probability for a recent quit attempt using NRT exhibited a curvilinear trend over time, lower in 1998 (27·0%, 95%CI=23·5%−30·4%) and 2017 (27·8%; 95%CI=23·0%−32·6%) compared to 2007 (36·5%; 95%CI=33·9%−39·2%). Survey year moderated the relationship between using NRT and socioeconomic disadvantage, quit intentions and heaviness of smoking. Figure 4d shows that the likelihood of NRT use was higher among the least compared to the most socio-economically disadvantaged smokers until around the peak of the curve in 2007, after which the two groups converged due to a more rapid decline among the least disadvantaged (13.3pp, p<0.0001). Figure 4e shows that heavier smokers were initially more likely to use NRT than lighter smokers (17·47pp, p<0·0001). However, the likelihood of using NRT among lighter smokers relative to heavier smokers has increased over time such that the difference between the two groups in 2017 was not statistically significant (6·39pp, p = 0·066). Figure 4f shows that there were minimal differences in the likelihood of using NRT according to quit intentions, but the difference between those with and those without quit intentions widened to 20·4pp by 2017 (p<0·0001). Using NRT was more likely among smokers aged 30 years and over compared to 15–29 year olds, and among those living in metropolitan compared to country areas (see Table 3).
Doctor referral to the quitline
The average adjusted probability of a doctor referral to the Quitline was 12·2% (95%CI=9·9%−14·5%), which did not vary over time (2012 to 2017). As shown in Table 4, the probability of having a doctor referral to the Quitline was higher for those aged 30–44 years compared to 15–29 years, heavier compared to lighter smokers, those with compared to without serious quit intentions and those living in country compared to metropolitan areas.
Called the quitline
The average adjusted probability for calling the Quitline exhibited a curvilinear trend over time, lower in 1998 (8·0%; 95%CI=5·9%−10·2%) and 2017 (7·3%; 95%CI=4·8%−9·8%) compared to 2007 (11·0%; 95%CI=9·3%−12·7%). Survey year did not moderate the effect of any other variables on calling the Quitline. On average across all years (see Table 4), the probability of calling the Quitline was higher for females, the most socio-economically disadvantaged, those living in metropolitan areas, those with quit intentions, heavier smokers and those with a mental health condition compared to their demographic counterparts.
Using a quit app or text messaging service
The average adjusted probability for using a Quit app or text messaging service has increased over time (2011=2·8% [95%CI=1·4%−4·2%, 2017=16·7%; 95%CI=11·2%−22·3%). Only region was modified by survey year (see Figure 4c) and the size of the effect was small (Supplement Table 6). Those living in metropolitan compared to country areas initially had a higher probability, but the rate of change over time was greater for those living in country areas. The probability of using an app or text messaging service was higher for those aged 15–29 compared to those aged 45 years and over and for the least compared to the most disadvantaged smokers.
Discussion
Overall, the results indicate that smokers who are thinking about quitting should continue to be supported through a variety of cessation method options. Furthermore, it is important for clinicians and policy makers to recognize that preferences and perceptions of the various quit attempt methods may fluctuate in response to tobacco control activity which promotes cessation from many angles, including subsidizing therapies and increases in tax on cigarettes. It is noteworthy that in any given year there are many more smokers who have attempted to quit than who have successfully quit. Therefore, it is vitally important to understand how smokers approach quitting as it informs decision making surrounding resource allocation and acknowledges the need for a multi-factorial approach. Nevertheless, an important caveat of the results is that they do not reflect the rate at which each cessation method was used, or the success rate of each method, because former smokers were not asked how they achieved their long-term abstinence from smoking.
Our results show that the demographic profile of smokers has changed over time, mirroring the change in demographic profile of Australian smokers more broadly.11 Among this demographically skewed population, socioeconomic status and mental health were not predictors of quit attempts, and the gap has only slightly widened between those with and without quit intentions. These results, along with the finding that there has been no change over time in probability of a quit attempt for heavier smokers, suggest that the remaining smokers, who disproportionally fall into these demographic categories, are not becoming increasingly ‘hardcore’ smokers with no interest in quitting. The ‘hardening hypothesis’ (i.e. the remaining smokers are less interested in or capable of quitting compared to previous generations of smokers) has been proposed by those advocating harm reduction strategies, such as e-cigarettes and heated tobacco products.19 However, evidence does not support the hardening hypothesis in Australia20 or elsewhere.21 As this study explores, changes in cessation method preferences may be driven by the needs of the individual and the support options available. As is increasingly understood, sustained abstinence is a dynamic process of multiple quit attempts, with past quitting experiences influencing future intentions.22 Further research is needed on how to tailor strategies to support ongoing quit attempts.
Unassisted cessation
Unassisted quit attempts have gradually decreased over time but are still the most common method of quitting smoking. Like other studies conducted elsewhere,15 our study showed that an unassisted quit attempt was most likely among young, male, light smokers who did not have serious intentions to quit in the future. Self-perception of not being dependent on cigarettes and belief in having the willpower to succeed contribute to high confidence in quitting ability and limited need for formal cessation support.23 As reflected in our data and elsewhere,24 these self-perceptions are more prevalent among younger smokers and tend to diminish with age.
Unassisted quitting is the most common method of quitting reported by ex-smokers across various countries.4,13,15 Yet research is scarce on what drives success with this mode of quitting, why it only works some of the time, and why smokers prefer to quit unassisted when multiple support options are readily available.24 The limited evidence suggests that internal drive to succeed may be critical, with social and structural factors determining the ease in which an appropriate mindset can be achieved.25 Unassisted quitting may also be preferred because of beliefs about the poor efficacy of other methods and concerns about side effects from prescription medications.23 Importantly, over the course of multiple quit attempts, smokers may cycle through a range of both assisted and unassisted techniques as they learn what works for them.24
Viewing quitting as a process helps to contextualize unassisted quitting within a broader framework of support. Smokers with strong ‘mind over matter’ beliefs may be resistant to support that undermines their sense of control, but they may be open to self-directed tools and regular check-ins, which may explain the rise in smoking cessation apps.26 However, as shown in this study, they may appeal to younger and socio-economically advantaged audiences. Population-level evidence-based strategies may assist in building confidence to make further attempts to quit after a setback. For example, anti-tobacco campaigns like “Every try counts”27 normalises the learning experience that comes from multiple quit attempts.
Assisted cessation
The trend over time in proportion of smokers with a recent quit attempt using quit smoking medication and asking a doctor for advice or help to quit followed a similar trajectory, with a noticeable rise coinciding with a large increase in the use of prescribed cessation medication that occurred after varenicline became subsidised through the Australian Pharmaceutical Benefits Scheme (PBS) in 2008. NRT use was curvilinear, peaking in 2007 at 46%. The decline in NRT use post-2007 coincided with the increased availability of varenicline (Champix), suggesting that some smokers may have replaced one form of pharmacotherapy with another. NRT was the only supported quit attempt method where there was evidence of a long-term decrease in use, and it was specific to smokers without serious quit intentions when surveyed. During the same period, NRT use rose among lighter smokers, so there are multiple factors at play that would require further investigation to determine what effect NRT use has on future quit intentions when the quit attempt is unsuccessful.
NRT has had a relatively consistent rate of between 30 and 40% use over the last 20 years, making it the most popular form of assisted cessation support. Subsidised nicotine patches became available to all smokers with a prescription in 2011, but NRT products have been available without a prescription since 1988, leading to increased advertising spend and widespread availability as over-the-counter items in supermarkets and pharmacies.28 However, the high use of NRT does not mean that it is being used optimally. Until recently, only nicotine patches were subsidised through the PBS.28 The evidence indicates the efficacy of NRT increases when fast and slow acting products are used in conjunction, and when it is combined with behavioural support.28 The results of this study are consistent with others13,15 showing that accessing behavioural support via services such as the Quitline is relatively uncommon. This study also shows that Quitline referrals by doctors was relatively low (13·6%) compared to the proportion of smokers who sought help from a doctor (33·5%).
Recent data showed that 83% of Australians aged 15 years and over visited a General Practitioner (GP) in the previous 12 months, although the rate was below 70% for males under 34 years.29 Consequently, GPs are in a unique position to provide cessation advice, but they may underutilise opportunities due to time, skills and knowledge barriers.30 A brief intervention model (Ask, Advise, Help) is designed to reduce barriers and is included in clinical guidelines for GPs.31 In practice, this involves identifying all people who smoke, offering brief advice to quit as routine practice, and helping by arranging referrals to external services (e.g. Quitline), encouraging use of behavioural support and evidence-based pharmacotherapy. We were unable to ascertain what assistance was provided by GPs, but the results suggest that improvements to Quitline referrals are needed. This may be facilitated by exploring whether this type of support is offered and refused by smokers who would prefer to quit without behavioural support.
Reported use of assisted methods (i.e. NRT, medication, asking doctor for help, calling the Quitline, referral to Quitline by a doctor) tended to be greater among older participants, dependent smokers and those with serious quit intentions. This is consistent with other studies showing that more nicotine-dependent smokers are more likely to seek out support.5,15 This study adds new insight into socioeconomic differences in preferred methods, with the most compared to the least disadvantaged smokers more likely to seek help from a doctor and call the Quitline, were initially less likely to use NRT but the gap has narrowed, and less likely to use apps/text messaging services. Tailored support accounting for individual circumstances may be needed for the most disadvantaged smokers because the evidence is mixed on whether cost/access is a significant barrier.5, 6, 7 Multi-component interventions that address specific needs may have greater efficacy in populations that have complex needs and high relapse rates.32 For example, advice from GPs and social contacts are key drivers of smoking cessation among smokers with a mental health condition.33 GPs are seen as important because they can provide practical and emotional support,10 but some smokers with mental health conditions have indicated that they are not getting adequate support from these services.34
This study has some limitations. The ‘method of quit attempt’ question with pre-specified response options was designed to capture broad trends in preferences among smokers rather than detailed insights into individual smoking cessation strategies over time or the likelihood of success from each of the methods that were trialed. Research shows that quitting histories are complex and may involve assisted methods before eventually quitting unassisted.24 The question was also not asked of former smokers, so it is not possible to determine which method, if any, led to greater success in quitting smoking. The response options evolved over time to incorporate novel approaches within the constraints of the broader questionnaire design. Promoting e-cigarettes as a cessation aid is not permitted in Australia, so e-cigarettes were not included in the pre-coded quit attempt response options. Generalisability is limited to the broad SA population. Furthermore, the HOS is not designed to capture data from small population sub-groups (e.g. Aboriginal and Torres Strait Islander people, incarcerated people, residents in mental health facilities, and homeless people) who, based on national data, have high rates of smoking.11
Despite some changing preferences over time, it is clear that there is a substantial proportion of smokers who prefer to quit unassisted. However, the increasing trend towards seeking help from a doctor, and the high likelihood of interaction with a GP at least once per year, is an opportunity for further development. Particularly, communicating to health professionals the importance smokers may place on these interactions. We also note that the most disadvantaged smokers were more likely to seek help from a doctor and call the Quitline, so further promotion of these services may increase uptake among key high prevalence groups. More broadly, there is also opportunity to clearly communicate to smokers and those providing cessation support how various methods may be utilised for smoking cessation and that unsuccessful quit attempts are common and expected during the process of quitting for good.
Contributors
CM and JB conceptualised and designed the study. JD and KM analysed the data. JD, KM, JB and CM provided input on data, results, and interpretation. JD and KM drafted the manuscript with editorial input from CM and JB. All authors have read and approved the final version of the manuscript. All authors have verified the underlying data and have had full access to the data throughout the study. All authors had final responsibility for the decision to submit for publication.
Declaration of interests
All support for the present manuscript is described in the funding statement. The authors have no other relationships/activities/interests to declare.
Acknowledgments
Acknowledgments
The authors wish to acknowledge the research assistants and participants in the Health Omnibus Survey years 1998–2017 who made this research possible.
Data sharing
Non-identifiable participant data will be available from the corresponding author on reasonable request (including a study outline) and with an appropriate data sharing agreement.
Funding
This study was supported by Drug and Alcohol Services SA (Government of South Australia), via funding of the Tobacco Control Research and Evaluation Program within Cancer Council SA (1998–2013) and the Health Policy center, SAHMRI (2013–2021). The funder had no involvement in any aspect of the study.
Ethics
Ethics approval was granted by the South Australian Department of Human Services/Department of Health and Ageing Human Research Ethics Committee and the University of Adelaide Human Research Ethics Committee.
Footnotes
Funding: South Australian Government.
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lanwpc.2021.100342.
Supplementary materials
References
- 1.Partos T.R., Borland R., Yong H.-.H., Hyland A., Cummings K.M. The quitting rollercoaster: how recent quitting history affects future cessation outcomes (data from the International Tobacco Control 4-country cohort study) Nicotine & Tobacco Research. 2013;15(9):1578–1587. doi: 10.1093/ntr/ntt025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . Geneva; 2019. WHO report on the global tobacco epidemic 2019: offer help to quit tobacco use. [Google Scholar]
- 3.Department of Health. Tobacco control – key facts and figures. 2018. https://www.health.gov.au/resources/publications/tobacco-control-key-facts-and-figures (accessed 7 Dec 2020).
- 4.Edwards S.A., Bondy S.J., Callaghan R.C., Mann R.E. Prevalence of unassisted quit attempts in population-based studies: a systematic review of the literature. Addict Behav. 2014;39(3):512–519. doi: 10.1016/j.addbeh.2013.10.036. [DOI] [PubMed] [Google Scholar]
- 5.Cooper J., Borland R., Yong H.H. Australian smokers increasingly use help to quit, but number of attempts remains stable: findings from the International Tobacco Control Study 2002–09. Aust N Z J Public Health. 2011;35(4):368–376. doi: 10.1111/j.1753-6405.2011.00733.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clare P., Slade T., Courtney R.J., Martire K.A., Mattick R.P. Use of Smoking Cessation and Quit Support Services by Socioeconomic Status Over 10 Years of the National Drug Strategy Household Survey. Nicotine & Tobacco Research. 2014;16(12):1647–1655. doi: 10.1093/ntr/ntu119. [DOI] [PubMed] [Google Scholar]
- 7.Shiffman S., Brockwell S.E., Pillitteri J.L., Gitchell J.G. Individual differences in adoption of treatment for smoking cessation: demographic and smoking history characteristics. Drug Alcohol Depend. 2008;93(1–2):121–131. doi: 10.1016/j.drugalcdep.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 8.Kotz D., Batra A., Kastaun S. Smoking Cessation Attempts and Common Strategies Employed. Dtsch Arztebl Int. 2020;117(1–2):7–13. doi: 10.3238/arztebl.2020.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Soulakova J.N., Crockett L.J. Level of Cigarette Consumption and Duration of Smoking Abstinence During Failed Quit Attempts Among Long-Term Daily Smokers: the Role of Race/Ethnicity and Cessation Aids. J Racial Ethn Health Disparities. 2018;5(2):293–303. doi: 10.1007/s40615-017-0370-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parnell A., Box E., Bonevski B., et al. Potential sources of cessation support for high smoking prevalence groups: a qualitative study. Aust N Z J Public Health. 2019;43(2):108–113. doi: 10.1111/1753-6405.12869. [DOI] [PubMed] [Google Scholar]
- 11.Australian Institute of Health and Welfare . AIHW; Canberra: 2020. National drug strategy household survey 2019. cat. no. phe 270. [Google Scholar]
- 12.Cancer Institute NSW. NSW Smoking and Health Survey 2015. 2017. https://www.cancer.nsw.gov.au/about-cancer/document-library/nsw-smoking-and-health-survey-2015 . (accessed 15 October 2021)
- 13.Filippidis F.T., Laverty A.A., Mons U., Jimenez-Ruiz C., Vardavas C.I. Changes in smoking cessation assistance in the European Union between 2012 and 2017: pharmacotherapy versus counselling versus e-cigarettes. Tob Control. 2019;28(1):95–100. doi: 10.1136/tobaccocontrol-2017-054117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hartmann-Boyce J., Hong B., Livingstone-Banks J., Wheat H., Fanshawe T.R. Additional behavioural support as an adjunct to pharmacotherapy for smoking cessation. Cochrane Database of Systematic Reviews. 2019;(6) doi: 10.1002/14651858.CD009670.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Soulakova J.N., Crockett L.J. Unassisted Quitting and Smoking Cessation Methods Used in the United States: analyses of 2010-2011 Tobacco Use Supplement to the Current Population Survey Data. Nicotine & Tobacco Research. 2017;20(1):30–39. doi: 10.1093/ntr/ntw273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hughes J.R., Keely J., Naud S. Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction. 2004;99(1):29–38. doi: 10.1111/j.1360-0443.2004.00540.x. [DOI] [PubMed] [Google Scholar]
- 17.Australian Bureau of Statistics. Census. 2021. https://www.abs.gov.au/census/find-census-data/more-products (accessed 10 Jun 2021).
- 18.StataCorp . StataCorp LLC; College Station, TX: 2017. Stata statistical software: release 15. [Google Scholar]
- 19.Polosa R., Rodu B., Caponnetto P., Maglia M., Raciti C. A fresh look at tobacco harm reduction: the case for the electronic cigarette. Harm Reduct J. 2013;10(1):19. doi: 10.1186/1477-7517-10-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brennan E., Greenhalgh E.M., Durkin S.J., Scollo M.M., Hayes L., Wakefield M.A. Hardening or softening? An observational study of changes to the prevalence of hardening indicators in Victoria, Australia, 2001–2016. Tob Control. 2020;29(3):252–257. doi: 10.1136/tobaccocontrol-2019-054937. [DOI] [PubMed] [Google Scholar]
- 21.Buchanan T., Magee C.A., See V.H., Kelly P.J. Tobacco harm reduction: are smokers becoming more hardcore? J Public Health Policy. 2020;41(3):1–17. doi: 10.1057/s41271-020-00226-1. [DOI] [PubMed] [Google Scholar]
- 22.Hughes J.R., Solomon L.J., Naud S., Fingar J.R., Helzer J.E., Callas P.W. Natural History of Attempts to Stop Smoking. Nicotine & Tobacco Research. 2014;16(9):1190–1198. doi: 10.1093/ntr/ntu052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morphett K., Partridge B., Gartner C., Carter A., Hall W. Why Don't Smokers Want Help to Quit? A Qualitative Study of Smokers' Attitudes towards Assisted vs. Unassisted Quitting. Int J Environ Res Public Health. 2015;12(6):6591–6607. doi: 10.3390/ijerph120606591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smith A.L., Carter S.M., Dunlop S.M., Freeman B., Chapman S. Revealing the complexity of quitting smoking: a qualitative grounded theory study of the natural history of quitting in Australian ex-smokers. Tob Control. 2018;27(5):568–576. doi: 10.1136/tobaccocontrol-2017-053919. [DOI] [PubMed] [Google Scholar]
- 25.Smith A.L. Being serious about quitting: a qualitative analysis of Australian ex-smokers’ explanations of their quitting success. International Journal of Drug Policy. 2020;86 doi: 10.1016/j.drugpo.2020.102942. [DOI] [PubMed] [Google Scholar]
- 26.Thornton L., Quinn C., Birrell L., et al. Free smoking cessation mobile apps available in Australia: a quality review and content analysis. Aust N Z J Public Health. 2017;41(6):625–630. doi: 10.1111/1753-6405.12688. [DOI] [PubMed] [Google Scholar]
- 27.FDA. Every Try Counts Campaign. 2020. https://www.fda.gov/tobacco-products/every-try-counts-campaign#Reference (accessed 4 Dec 2020).
- 28.Greenhalgh E., Stillman S. In: Tobacco in australia: facts and issues melbourne. Greenhalgh E, Scollo M, Winstanley M, editors. Cancer Council Victoria; 2020. Ford C. 7.16 Pharmacotherapies. [Google Scholar]
- 29.Australian Bureau of Statistics. Patient Experiences in Australia: Summary of Findings. 2020. https://www.abs.gov.au/statistics/health/health-services/patient-experiences-australia-summary-findings/2019-20 (accessed 7 Dec 2020).
- 30.Holtrop J.S., Malouin R., Weismantel D., Wadland W.C. Clinician perceptions of factors influencing referrals to a smoking cessation program. BMC Fam Pract. 2008;9(1):18. doi: 10.1186/1471-2296-9-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.The Royal Australian College of General Practitioners. Supporting smoking cessation: a guide for health professionals. 2019. https://www.racgp.org.au/clinical-resources/clinical-guidelines/key-racgp-guidelines/view-all-racgp-guidelines/supporting-smoking-cessation (accessed 10 Jun 2021).
- 32.Wilson A., Guillaumier A., George J., Denham A., Bonevski B. A systematic narrative review of the effectiveness of behavioural smoking cessation interventions in selected disadvantaged groups (2010-2017) Expert Rev Respir Med. 2017;11(8):617–630. doi: 10.1080/17476348.2017.1340836. [DOI] [PubMed] [Google Scholar]
- 33.Dickerson F., Bennett M., Dixon L., et al. Smoking cessation in persons with serious mental illnesses: the experience of successful quitters. Psychiatr Rehabil J. 2011;34(4):311–316. doi: 10.2975/34.4.2011.311.316. [DOI] [PubMed] [Google Scholar]
- 34.Sharma-Kumar R., Meurk C., Ford P., Beere D., Gartner C. Are Australian smokers with mental illness receiving adequate smoking cessation and harm reduction information? Int J Ment Health Nurs. 2018;27(6):1673–1678. doi: 10.1111/inm.12465. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.