Abstract
Introduction and importance
With the widespread use of laparoscopic inguinal hernia repair, it is known that some clinically evident inguinal hernias lack a peritoneal sac and are referred to as “sacless hernias”.
Presentation of case
A 61-year-old man presented with a left inguinal bulge. On physical examination, the diagnosis of bilateral inguinal hernias was made, and laparoscopic transabdominal repair was performed. Intraoperatively, the left peritoneal hernia orifice was not identified from the peritoneal cavity and there was only a lipoma. Pressing the lipoma with forceps from inside the peritoneum confirmed the presence of a hernia. The preperitoneal space was opened and the hernia orifice revealed.
Discussion
The terminology and definition of sacless hernias are poorly defined, even though this is not a rare condition. Consistent with Russell's dogma, there are arguments that any prolapse can only be called a hernia if there is an accompanying peritoneal sac. The proportion of patients with sacless hernias and pure cord lipomas are very similar and these conditions are often confused. Detailed and repeated physical examination may distinguish a sacless hernia from a pure lipoma. A watchful waiting strategy is useful and ensures safety.
Conclusion
Once the diagnosis of inguinal hernia is made on physical examination, open the preperitoneal cavity if a peritoneal hernia orifice was not identified during laparoscopy.
Keywords: Sacless hernia, Inguinal hernia, TAPP, Lipoma, Preperitoneal fat
Highlights
-
•
The exact terminology and definition of a “sacless hernia” is still unclear and there were very few literatures, despite this situation has been commonly known.
-
•
Attention should be paid not to confuse a sacless hernia with a spermatic cord lipoma. Preoperative physical examination and diagnosis is a key to distinguish them.
-
•
Once a robust diagnosis of inguinal hernia is made by physical examination, open the preperitoneal cavity if the peritoneal hernia orifice was not identified during laparoscopy.
1. Introduction
With the widespread use of transabdominal preperitoneal (TAPP) repair for inguinal hernias, it is known that some clinically diagnosed inguinal hernias lack a peritoneal sac at laparoscopy and are referred to as “sacless hernias”. Though the definition of a sacless hernia is not precisely stated, causes of this condition have been reported to be a lipoma of the spermatic cord or round ligament, preperitoneal fatty tissue, and a femoral hernia [1]. We present a patient with a sacless hernia with an orifice obscured by a preperitoneal lipoma.
2. Case presentation
A 61-year-old man presented with several weeks history of a left inguinal bulge. His medical history was remarkable for hypertension, type 2 diabetes mellitus and he is status-post bilateral inguinal hernia repairs at age 2. On physical examination, the diagnosis of bilateral inguinal hernias was made, and bilateral laparoscopic transabdominal repair was planned. Intraoperatively, the peritoneal hernia orifice was not identified on the left side. There was only a lipoma near the left internal inguinal ring. By pressing on the lipoma with forceps from the intra-peritoneal side, herniation was confirmed externally. The preperitoneal space was opened and the hernia orifice was revealed as a defect in the abdominal wall. Bilateral direct inguinal hernias were repaired with mesh. His symptoms resolved and there is no recurrence at more than two years postoperatively (Fig. 1).
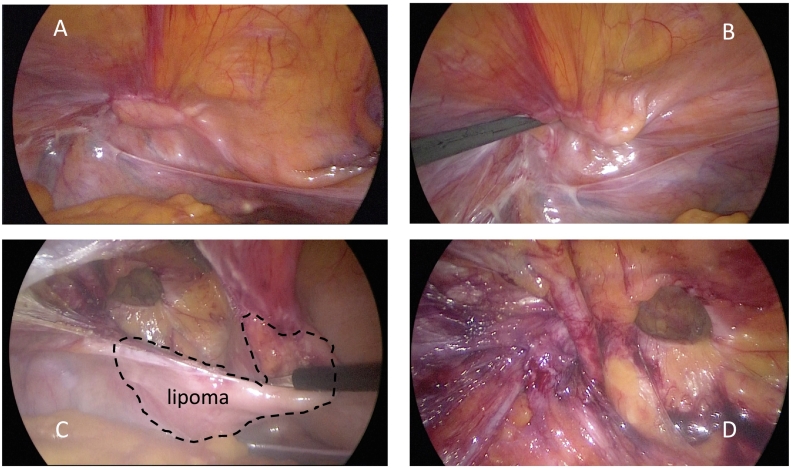
Fig. 1.
A peritoneal hernia orifice was not seen on the left side. There was only a lipoma near the left internal inguinal ring. (A) Pressing the lipoma with forceps from the intra-peritoneal side demonstrated a protruding inguinal mass externally. (B) The preperitoneal space was opened and the hernia orifice revealed as a defect in the abdominal wall. The preperitoneal lipoma was not connected to the spermatic cord. (C) Preperitoneal dissection was completed. (D).
3. Discussion
The importance of preperitoneal pathology for the diagnosis and treatment of inguinal hernias might not have been strongly considered in the open herniorrhaphy era because it does not affect the surgical procedure used. During laparoscopic hernia repairs, the absence of a peritoneal defect has been reported and some surgeons refer to this condition as a “sacless hernia”. The terminology and definition of a sacless hernia are still poorly defined, even though this situation is commonly known. An extensive search was conducted on PubMed of articles with the search term “sacless hernia” and only two references were found.
One of the articles identified reported that 6.2% of 2190 TAPP hernia repairs were for sacless hernias. Of these hernia repairs, femoral hernias, sacless sliding hernias with a lipoma of the cord and round ligament, and sliding hernias of preperitoneal fatty tissue represented 30.1%, 33.8%, and 22.8%, respectively [1]. The authors recommend preperitoneal dissection for patients with clinically diagnosed groin hernias because pathology in the preperitoneal space cannot be identified through the peritoneum and in particular, a sliding hernia may be overlooked.
The terminology and mechanism of abdominal and pelvic herniation, where the entity of sacless hernia was described were reviewed [2]. Sliding hernias are the protrusion of an extraperitoneal viscus, kidney, ureter, and bladder unaccompanied by peritoneum, into the scrotum. However, consistent with Russell's dogma, there are arguments that any prolapse could only be called a hernia if an accompanying peritoneal sac is present.
The incidence of pure lipomas of the cord and round ligament was reported to be 6.4 to 8% [3], [4]. They are not true hernias, but hernia repair is indicated because of inguinal symptoms. Interestingly, the proportion of patients with sacless hernias and pure cord lipomas are very similar. It is difficult to know if they are describing the same condition as different diagnoses or not. Some call these entities a sliding hernia while others say they are a symptomatic lipoma without a true hernia. A typical operative procedure would suggest that once the preperitoneal space was opened and there was no hernia orifice identified, mesh would be placed. In such a case, the true diagnosis could be unclear. Some surgeons recommend exploration of the preperitoneal space even in the case of a symptomatic pure cord lipoma which lacks a true hernia [5]. The sacless hernia is widely known but clinical reports of it are limited, and it is often confused with spermatic cord lipomas, which this report emphasizes.
In the present patient, a tissue complex including an elastic lipoma and the peritoneum obscured the orifice of the hernia. It was a true hernia, and the sac did not protrude with normal intraperitoneal pressure during the TAPP procedure but appeared after application of direct intraoperative pressure using a forceps. If a hernia repair using an anterior open approach was performed on this patient, the hernia sac would be extracted and identified as a simple direct hernia.
To avoid confusion during laparoscopic surgery, we recommend a simple approach. Surgery should be performed when inguinal symptoms are obvious and typical. Any mass should be not only protruding but also reducible. If the groin mass or pain was induced by a pure lipoma, the mass cannot be reduced. Detailed and repeated physical examinations may distinguish a sacless hernia from a pure lipoma. A watchful waiting strategy is very useful and ensures safety [6]. When the diagnosis of an inguinal hernia is made with confidence preoperatively, the preperitoneal space can be entered without hesitation. Pressing the internal inguinal ring with a forceps is a non-invasive and useful technique to confirm the diagnosis.
4. Conclusion
The exact terminology and definition of a “sacless hernia” is still unclear and there are few existing reports, despite this being a common situation. Attention should be paid not to confuse a sacless hernia with a spermatic cord lipoma. Preoperative physical examination and diagnosis is the key to distinguish these two entities. Once a robust diagnosis of inguinal hernia is made by physical examination, open the preperitoneal cavity if the peritoneal hernia orifice was not identified during laparoscopy.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Ethical approval
This case report is exempt from ethical approval in our institution.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Guarantor
Kazuhiro Nishida, MD.
Research registration number
Not applicable.
CRediT authorship contribution statement
KN gathered patient's date, designed the case report and drafted manuscript. SO and AKL have made substantial contribution to the conception and design of the case study. All authors read and approved the final manuscript.
Declaration of competing interest
The authors declare they have no competing interests.
Contributor Information
Kazuhiro Nishida, Email: pandadebanda4@gmail.com.
Alan Kawarai Lefor, Email: alefor@jichi.ac.jp.
References
- 1.Hollinsky C., Hollinsky Sandberg S. Clinically diagnosed groin hernias without a peritoneal sac at laparoscopy–what to do? Am. J. Surg. 2010;199:730–735. doi: 10.1016/j.amjsurg.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 2.Read R.C. Archaic terms and dogmas impeding care of abdominal and pelvic herniation. Hernia. 2007;11:299–302. doi: 10.1007/s10029-007-0230-7. [DOI] [PubMed] [Google Scholar]
- 3.Lilly M.C., Arregui M.E. Lipomas of the cord and round ligament. Ann. Surg. 2002;235:586–590. doi: 10.1097/00000658-200204000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nasr A.O., Tormey S., Walsh T.N. Lipoma of the cord and round ligament: an overlooked diagnosis? Hernia. 2005;9(3):245–247. doi: 10.1007/s10029-005-0335-9. [DOI] [PubMed] [Google Scholar]
- 5.Gersin K.S., Heniford B.T., Garcia-Ruiz A., Ponsly J.L. Missed lipoma of the spermatic cord. A pitfall of transabdominal preperitoneal laparoscopic hernia repair. Surg. Endosc. 1999;13:585–587. doi: 10.1007/s004649901046. [DOI] [PubMed] [Google Scholar]
- 6.Fitzgibbons R.J., Jr., Giobbie-Hurder A., Gibbs J.O., Dunlop D.D., Reda D.J., McCrthy M., Jr., et al. Watchful waiting vs repair of inguinal hernia in minimally symptomatic men: a randomized clinical trial. JAMA. 2006;295:285–292. doi: 10.1001/jama.295.3.285. [DOI] [PubMed] [Google Scholar]