Abstract
Acetabular fractures are complex injuries with an annual incidence of approximately 4 per 100,000 (Laird and Keating, 2005 [1]. Although the open reduction is currently advocated for treating acetabular fractures, some acetabular fractures can be treated by minimally invasive surgery, with the advantages of minor trauma, less bleeding, reduced infection, and shorter operation time. Therefore, we report a case of a patient with a transverse fracture involving the acetabulum treated with a new method of cannulated screw fixation combined with a personalized 3D printed guide to achieving minimally invasive and precise treatment of acetabular fractures while we review the relevant papers.
Keywords: Acetabular fracture, Posterior column screw, Minimally invasive, 3D printing
Highlights
-
•
Some acetabular fractures can be treated by minimally invasive surgery, with the advantages of minor trauma, less bleeding, reduced infection, and shorter operation time.
-
•
We report a case of a patient with a transverse fracture involving the acetabulum treated with a new method of cannulated screw fixation combined with a personalized 3D printed guide to achieving minimally invasive and precise treatment of acetabular fractures.
-
•
Through the new channel of posterior column screw, minimally invasive antegrade screw placement, guided plate assistance, we can complete the operation faster and more conveniently for the benefit of patients.
Case report
A 45-year-old man was brought to the hospital emergency room with left hip pain and limited mobility due to a car accident trauma. On admission, pelvic CT showed a transverse acetabular fracture (Fig. 1A, B, C, and D) with a displacement of the fracture end > 3 mm without associated hip dislocation. The patient had pain and immobility in the right hip, while he was unbearable to stay in bed for a long time, and not strictly bedridden was prone to the displacement of the fracture end. Therefore, surgery was performed on day 5. The patient and family were informed of the condition and treatment plan, consent for surgery was obtained, and informed consent was given for publication of this study and use of their photographs.
Fig. 1.
Three-dimensional CT of the pelvis showing transverse acetabular fractures involving the anterior and posterior columns.
Preoperative design
-
(1)
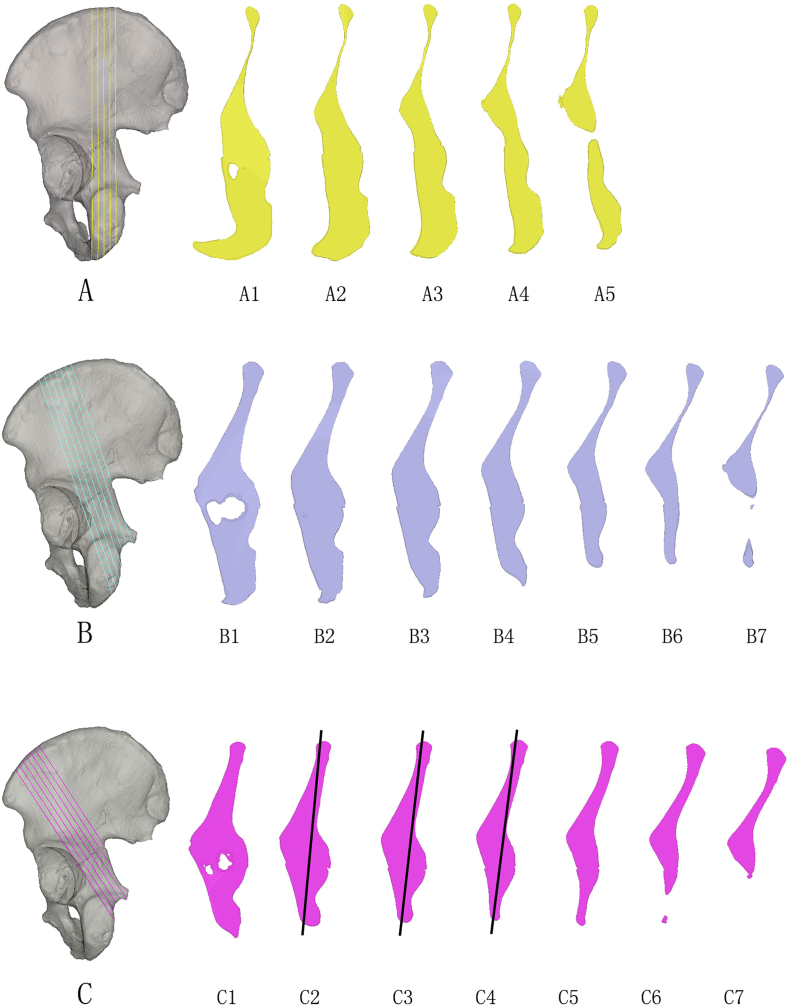
Import the preoperative scanned CT images into E-3Dsoftware in Dicom format (Fig. http://www.e3d-med.com; E3D Digital Medical and Virtual Reality Research Center, Central South University, Hunan Province, China) for digital three-dimensional reconstruction to segment each acetabular fracture fragment. Since we can easily palpate the iliac crest, if there is a screw entry point here, we can easily find the entry point position and place the screw into the bone, but it is also safer. Therefore, we set up three paths from the anteromedial part of the iliac crest to the posterior column of the acetabulum, perpendicular to the iliac crest along each of the three paths, and performed virtual sections equally spaced distances (5 mm) to observe the condition of the sections (Fig. 2A, B, C).
-
(2)
Select the narrowest part of the ilium (i.e., iliac fossa, superior acetabulum, acetabular center, sub-acetabulum) to make a contour line, respectively, and observe whether there is an intersection of these four contour lines by axial fluoroscopy and the intersection area means the presence of the channel (Fig. 3A, B);
-
(3)
By the above method, only the third path (Fig. 2C) has a channel; that is, between the anterior superior iliac crest and the iliac tuberosity, and in the direction to the ischial spine, there is a suitable channel to allow screws to be placed in the fixed posterior column of the acetabulum. Among them, the channel was measured to be 158 mm long and 17.5 mm wide, with a maximum accommodation of 7.91 mm diameter screws, and the optimal entry point (redpoint) was measured to be 32.3 mm away from the anterior superior iliac spine (green point) and 41.3 mm away from the midpoint of the iliac tubercle (yellow point) (Fig. 3A-E).
-
(4)
Set the anterior and posterior column screws in the model, continuously adjust the direction and length of the screws so that they are in the optimal position. Posterior column screws run in the direction of the ischial spine using the insertion point between the iliac tuberosity and the anterior superior iliac crest. According to the method of Wang [2], the anterior column screw is used as the entry point in the posterosuperior acetabulum and runs in the direction of the pubic symphysis. Screws are designed so that the cortex is not penetrated (Fig. 4A, B, C).
-
(5)
to increase the accuracy of screw placement, save surgical time, and reduce intraoperative fluoroscopic radiation injuries, we designed a personalized navigation template to assist screw placement. The bone surface between the iliac tubercle and the anterior superior iliac crest was used as a template for the guide base, which wrapped the bone surface in a“C” pattern. Due to the bone enlargement at the iliac tuberosity, it can block the movement of the guide and ensure the accurate position of the guide. At the same time, a K-wire is placed in the hole on this template to increase the stability of the guide. Finally, the guide plate is designed by fusing the guide column of the posterior and anterior column screws on the template so that a guide plate can assist in the placement of two screws in the anterior and posterior columns (Fig. 4A, B, C). 3D printed guides were obtained using rapid prototyping technology and disinfected for future use.
Fig. 2.
Three paths were set from the anteromedial part of the iliac crest to the posterior column of the acetabulum, which was perpendicular to the iliac crest along three paths, A, B, and C, respectively, and virtual sections were performed at equal spacing (5 mm) to observe the condition of the sections.
Fig. 3.
A: Respectively make a contour line at the local narrowest part of the ilium (namely, iliac fossa, supraacetabular region, acetabular center, and sub-acetabular region); B: transparent the model, observe the intersection of these four contour lines by the method of axial fluoroscopy, and the intersection area is posterior column screw channel; C: measure that the maximum diameter of a channel can accommodate 7.91 mm screw; D: measure that the channel length is 158 mm and the width is 17.5 mm; E: a measure that the optimal entry point (red point) is 32.3 mm away from the anterior superior iliac spine (green point) and 41.3 mm away from the midpoint of iliac tubercle (yellow point). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Fig. 4.
Orient the anterior and posterior column screws. ABC for three different perspectives. ① Position and direction of posterior column screw placement ② Position and direction of anterior column screw placement ③ Position and direction of the anti-Kirschner wire. ④ 3D printing combined with a guide template.
Intraoperative operation:
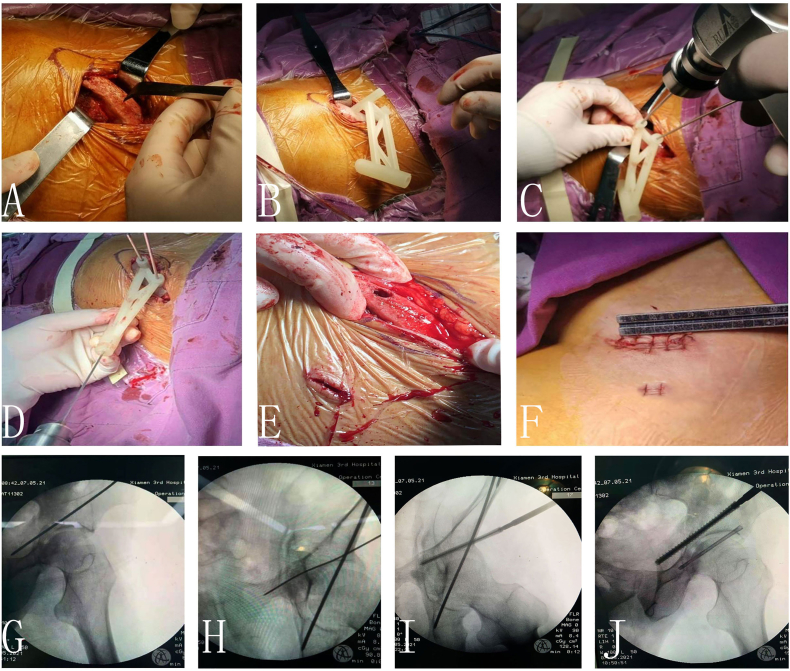
The patient was placed supine, the surgical field was disinfected and draped, and an assistant performed appropriate traction. At about 2 cm from the anterior superior iliac spine, the skin was incised about 3 cm in length along the direction of the iliac crest, and the soft tissue attached to the iliac crest was dissected clean using electrocautery and bone stripping. The 3D printed guide was precisely sleeved into the iliac crest bone surface and temporarily fixed with Kirschner wires. A 2.5 mm diameter hollow screw guidewire was placed from the posterior column guide hole of the guide plate, and then a 1.5 mm diameter hollow screw guidewire was placed under the guidance of the anterior column guide cannula, and the excellent position of each guidewire was confirmed under multi-angle fluoroscopy. Therefore, a fully threaded hollow lag screw with a diameter of 7.0 mm and a length of 120 mm for the posterior column and a fully threaded hollow lag screw with a diameter of 5.0 mm and a length of 80 mm for the anterior column were placed for depth measurement and reaming, respectively. For simple fractures with slight fracture displacement, hollow lag screws can be used to compress the fracture ends to achieve the effect of fracture reduction. C-arm digital X-ray machine confirmed good alignment and alignment of the fracture under multi-directional and multi-angle fluoroscopy, good screw position, and adequate stability of the fracture end (Fig. 5, A-J).
Fig. 5.
A. Minimally invasive exposure of the iliac crest bone surface. B. 3D printed guides were placed on the iliac crest. C. The guide plate was temporarily fixed with an anti-rotation Kirschner wire, and a 2.5 mm posterior column screw guide pin was placed. D. Insertion of 1.5 mm anterior column screw guide pin. E. Entry point of posterior column screw channel on iliac crest. F. Surgical incision G-J. Intraoperative C-arm iliac oblique film and closed oblique film showed that the anterior and posterior column screws were suitable and did not enter the hip joint.
Postoperative treatment:
Pelvic CT was routinely taken postoperatively. Outpatient follow-up was performed every month after surgery until the fracture healed, and the patients were instructed to perform functional exercises, and full weight-bearing was prohibited before fracture healing. At 1-year follow-up, the patient was ambulatory, had hip flexion and extension range of motion from 0 to 130 degrees, and had 40 degrees of abduction without subjective perception of hip pain or osteoporosis (Fig. 6A-D).
Fig. 6.
A-B. Postoperative pelvic CT showed that the position and direction of acetabular posterior column screws were good, and the gap at the fracture end was reduced. C-D. The patient had good function one year after surgery.
Discussion:
Acetabular fractures are complex injuries with an annual incidence of approximately 4 per 100,000 [1]. Judet [3] and Letournel [4] were the first to report the classification method and surgical skills of acetabular fractures, of which open anatomical reduction and rigid fixation are the keys to treatment. However, open reduction and internal fixation with plates may lead to complications such as a wide range of surgical exposure, long operation time, excessive intraoperative blood loss, iatrogenic injury of nerves and blood vessels, and infection, and acetabular fractures have received increasing attention through minimally invasive surgery. The acetabular posterior column lag screw technique was first proposed by Judet [3], and Tile [5] has reported the fixation of acetabular T-fractures by applying the posterior column lag screw technique. However, he believes that this is not an easy technique and that although the incision is small, the risk is significant. Reinerl [6] proposed the treatment of transverse fractures by fixing the anterior and posterior columns with two long cancellous threaded screws, respectively, which has the advantages of minor trauma and reliable internal fixation. With the development of technology, the acetabular lag screw has been widely used, with the advantages of minor trauma, shorter time, and faster recovery. Moreover, studies have shown that there is no significant difference in the stability of acetabular fractures using lag screw internal fixation versus internal plate fixation and combined plate and screw fixation [7].
Indications of a minimally invasive technique of antegrade lag screw technique for the posterior column of the acetabulum: 1. transverse or T-type acetabular fracture without displacement or mild displacement; 2. posterior column fracture of the acetabulum with apparent displacement can be fixed with antegrade lag screw for the posterior column of acetabulum if closed reduction traction, simple anterior approaches such as ilioinguinal approach or extended iliofemoral approach are used to reduce anterior column fracture, complete or most of the reduction of posterior column fracture is also obtained.
However, the entry point of traditional antegrade posterior column screws is in the iliac fossa (1 cm at the anterior margin of the sacroiliac joint and 2.5 cm at the side opening), and the exit point is at the midpoint of the ischial tuberosity [8]. Generally, it is necessary to expose the bone surface of the iliac fossa to place the traditional posterior column screw anterogradely. Because of the extensive incision injury, more vital nerves and blood vessels, more bleeding, long operation time, the slight angle between screw and bone surface, easy slippage of screw and misplacement into acetabulum or pelvic cavity, high risk, postoperative pain, and functional rehabilitation time of patients. Some scholars have also used retrograde posterior column screws to fix the posterior column of the acetabulum. However, this technique is suitable for the treatment of fractures without significant displacement and with a lower fracture line, which is difficult to position and fluoroscopy, the placement of screws may not be long enough, may damage the sub hip nerve, and may have pain at the entry point after surgery, Hence, development of this technique is limited [9]. Therefore, for acetabular fractures involving the posterior column with slight displacement, an attempt should be made to find a posterior column screw channel that can be placed, minimally invasive, and anterogradely.
By observing path slices of a three-dimensional iliac bone model, we found a channel on the iliac crest suitable for screw placement and fixation to the posterior column of the acetabulum. The primary entry point is between the anterior superior iliac crest and the iliac tuberosity, and the direction of screw placement is towards the ischial spine. Because the iliac crest is easily palpable subcutaneously, the entry point is more superficial and suitable for percutaneous screw placement, and the direction of screw placement is almost perpendicular to the bone surface and not easy to slip. The screw insertion channel, in this case, was measured to accommodate a maximum of 7.91 mm diameter screw, while the 7 mm diameter screw we used was large enough to provide sufficient stability to the fracture end. This channel was measured to be 158 mm long, and in fact, the 7 mm diameter screw was not so long, so we made a bone tunnel between the medial and lateral iliac plates and directly screwed the 100 mm long screw through the bone tunnel through the fracture ends to produce compression at the fracture end.
Furthermore, screws are more stable when clamped down on the medial and lateral iliac plates. Due to the unique anatomy of the posterior column of the acetabulum, in the direction of the posterior column lag screw is inaccurate. It penetrates the hip joint or penetrates the posterior column bone cortex in the pelvic cavity, resulting in neurological and vascular injury. Therefore, we use 3D printed guide plate in combination, complete the safe placement of two screws in anterior and posterior columns simultaneously under the guidance of one guide plate, increase the accuracy of screws, and reduce the operation time and X-ray radiation injury simple. It is a suitable screw placement method.
Of course, the angle of screw placement, anatomical parameters, individual differences, gender differences, fluoroscopy methods, indications, etc., of this channel are still understudied, and we will strengthen further studies later.
In conclusion, this case used preoperative CT data to reconstruct the pelvic model in three dimensions and plan the anterior and posterior column screw channel to minimally invasive, adequate fixation, and reduce surgical risks. At the same time, to increase the accuracy of screw placement and save the operation time, a personalized navigation template was used to assist the placement of anterior and posterior column screws during the operation, which was easy to operate and worthy of promotion.
Acknowledgments
The financial support from the Management Research Project of Fujian University of Traditional Chinese Medicine to the research project XB2021097 on “Digital Feasibility Analysis of Minimally Invasive Interlamellar Channel Screw Fixation of Acetabular Posterior Column Fractures” is greatly acknowledged.
References
- 1.Laird A., Keating J.F. Acetabular fractures: a 16-year prospective epidemiological study. The Journal of Bone and Joint Surgery. 2005;87(7):969–973. doi: 10.1302/0301-620X.87B7.16017. British Volume. [DOI] [PubMed] [Google Scholar]
- 2.Wang X., Ran G., Chen X. Obturator oblique and pubic ramus inlet views can better guide the insertion of an anterior column acetabular Screw. Orthop. Surg. 2021;13(3):1086–1093. doi: 10.1111/os.12943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Judet R., Judet J., Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction. Preliminary report. The Journal of Bone and Joint Surgery. 1964;46:1615–1646. American Volume. [PubMed] [Google Scholar]
- 4.Letournel E., Judet R. Springer-Verlag; R.A. Elson. Berlin Heidelberg: 1981. Fractures of the Acetabulum[M] [Google Scholar]
- 5.2021-10-04. Fractures of the Pelvis and Acetabulum (AO)[EB/OL].https://www.thieme.com/books-main/orthopaedic-surgery/product/2126-fractures-of-the-pelvis-and-acetabulum [Google Scholar]
- 6.Reinert C.M., Bosse M.J., Poka A. A modified extensile exposure for the treatment of complex or malunited acetabular fractures. The Journal of Bone and Joint Surgery. 1988;70(3):329–337. American Volume. [PubMed] [Google Scholar]
- 7.Le Quang H., Schmoelz W., Lindtner R.A. Biomechanical comparison of fixation techniques for transverse acetabular fractures - single-leg stance vs. Sit-to-stand loading. Injury. 2020;51(10):2158–2164. doi: 10.1016/j.injury.2020.07.008. [DOI] [PubMed] [Google Scholar]
- 8.Mu W.-D., Wang X.-Q., Jia T.-H. Quantitative anatomic basis of antegrade lag screw placement in posterior column of acetabulum. Arch. Orthop. Trauma Surg. 2009;129(11):1531–1537. doi: 10.1007/s00402-009-0836-6. [DOI] [PubMed] [Google Scholar]
- 9.Zhang P., Tang J., Dong Y. A new navigational apparatus for fixation of acetabular posterior column fractures with percutaneous retrograde lagscrew: design and application. Medicine. 2018;97(36) doi: 10.1097/MD.0000000000012134. [DOI] [PMC free article] [PubMed] [Google Scholar]