Abstract
OBJECTIVE
To examine short-term mortality and cause of death among youth and young adults (YYAs) with youth-onset diabetes.
RESEARCH DESIGN AND METHODS
We included 19,717 YYAs newly diagnosed with diabetes before 20 years of age from 1 January 2002 to 31 December 2015 enrolled in the SEARCH for Diabetes in Youth Study. Of these, 14,721 had type 1; 4,141 type 2; and 551 secondary and 304 other/unknown diabetes type. Cases were linked with the National Death Index through 31 December 2017. We calculated standardized mortality ratios (SMRs) and 95% CIs based on age, sex, and race/ethnicity for state and county population areas and examined underlying causes of death.
RESULTS
During 170,148 person-years (PY) (median follow-up 8.5 years), 283 individuals died: 133 with type 1 (103.0/100,000 PY), 55 with type 2 (161.5/100,000 PY), 87 with secondary (1,952/100,000 PY), and 8 with other/unknown diabetes type (312.3/100,000 PY). SMRs (95% CI) for the first three groups were 1.5 (1.2–1.8), 2.3 (1.7–3.0), and 28.0 (22.4–34.6), respectively. Diabetes was the underlying cause of death for 42.1%, 9.1%, and 4.6% of deaths, respectively. The SMR was greater for type 2 than for type 1 diabetes (P < 0.001). SMRs were significantly higher for individuals with type 1 diabetes who were <20 years of age, non-Hispanic White and Hispanic, and female and for individuals with type 2 diabetes who were <25 years of age, from all race/ethnic minority groups, and from both sexes.
CONCLUSIONS
Excess mortality was observed among YYAs for each type of diabetes with differences in risk associated with diabetes type, age, race/ethnicity, and sex. The root causes of excess mortality among YYAs with diabetes merit further study.
Introduction
Diabetes is one of the most common chronic diseases diagnosed in childhood. The SEARCH for Diabetes in Youth Study (SEARCH) reported a 1.9% increase per year in the incidence of type 1 diabetes and 4.8% per year increase for type 2 diabetes from 2002 to 2015 among U.S. youth (1) with significant increases in prevalence from 2001 to 2017 also reported (2). A continued upward trend in diabetes incidence will result in a substantial increase in the number of youth with type 1 and type 2 diabetes, especially youth from minority race/ethnic groups (3). As the incidence and prevalence of youth-onset diabetes increases in the United States, diabetes-related morbidity and mortality among these youth and young adults (YYAs) as they age requires further attention.
While excess mortality risk has been reported for individuals with youth-onset type 1 diabetes with differences in risk varying by country (4–11), there are fewer reports of mortality among individuals with youth-onset type 2 diabetes, a relatively recent condition, compared with the general population. In an earlier SEARCH analysis, YYAs with type 2 diabetes experienced over twice the excess mortality at an average diabetes duration of just over 5 years compared with populations of similar age, sex, and race/ethnicity (12).
To provide a contemporary assessment of mortality among YYAs with youth-onset diabetes, we assembled a large diverse cohort of individuals with youth-onset type 1, type 2, and secondary diabetes diagnosed from 2002 through 2015 with a median follow-up period of ∼8 years. We evaluated the impact of diabetes type and demographic characteristics (age, sex, and race/ethnicity) on mortality risk and explored the cause of death by diabetes type and sex.
Research Design and Methods
Study Population
SEARCH is a prospective multicenter population-based observational study of youth with diabetes diagnosed prior to 20 years of age. A detailed description of study methods has been published previously (13). In brief, incident physician-diagnosed diabetes cases among individuals aged <20 years diagnosed from 2002–2018 were identified. Cases were ascertained from geographically bounded populations in Ohio and adjacent counties, Colorado, South Carolina, and Washington, among health plan enrollees in California (Kaiser Permanente Southern California), and among Indian Health Service beneficiaries from American Indian populations in Arizona and New Mexico. Cases were identified through networks of pediatricians, endocrinologists, and other health care providers, hospitals, health centers, and health plans. Diabetes type was based on physician report ∼6 months after diabetes diagnosis and categorized as type 1 diabetes (including type 1, type 1a, and type 1b), type 2 diabetes, secondary diabetes (any cause), other types (such as monogenic forms of diabetes), and unknown diabetes type (type was missing or not known). Cases were registered anonymously with the Coordinating Center (Wake Forest School of Medicine). Case ascertainment has been >90% for incident cases of type 1 and type 2 diabetes during the study (2,13). Case ascertainment and registration were performed under a Health Insurance Portability and Accountability Act of 1996 waiver of written informed consent granted by local institutional review boards with jurisdiction over the study populations.
Ascertainment of Vital Status
All individuals in the SEARCH registry with incident diabetes diagnosed between 1 January 2002 and 31 December 2015 (n = 20,148) were eligible for inclusion in the mortality surveillance study. The end date for incident cases (31 December 2015) was chosen to allow for a minimum of 2 years of follow-up after diabetes diagnosis through 31 December 2017 with the latter date chosen in consideration of the ∼18-month lag in mortality data availability. From the 20,148 cases registered, 433 cases (2.1%) were excluded due to insufficient individual-level data for linkage with the National Death Index (NDI) (14) and unknown vital status from other sources at the end of the study period. Compared with the cases who were included, those excluded were older at diagnosis and more likely to have type 2 than type 1 diabetes, to be non-Hispanic Black or unknown race/ethnicity than other race/ethnicities, and to be from the earlier incidence years of the study (Supplementary Table 1).
Vital status (living, deceased, and unknown) and underlying and contributing causes of death were determined by linking the remaining 19,717 diabetes cases with NDI Plus database from the date of diabetes diagnosis through 31 December 2017 after excluding cases known to be alive on or after 31 December 2017 from local clinical or research records. Records in which individuals were known to be deceased were submitted to the NDI to obtain cause of death. Death certificates and reports of deaths by immediate family members or healthcare providers were also considered definitive evidence of death. NDI records were searched for all years for which vital status could not be confirmed. Deaths were verified by matching name, social security number (when available), date of birth, and sex.
Cause of Death
Cause of death was derived from the NDI Plus database where it had been classified per ICD-10. “Underlying cause of death” was used for cause-specific mortality. “Contributing cause of death” was used to identify deaths in which diabetes was a significant condition contributing to death but not the underlying cause. For Diabetes (ICD-10 codes E00–E14), Metabolic Diseases (E15–E99), and External causes of morbidity and mortality (V00–Y89), specific conditions listed within the series of codes are reported for the underlying cause of death. For other conditions with fewer decedents in our study, only the broader categories are reported.
Statistical Analysis
Person-years (PY) of follow-up were calculated from date of diabetes diagnosis to 31 December 2017 or date of death, whichever occurred first. Crude mortality rates by diabetes type and additionally stratified by age, sex, and race/ethnicity were calculated per 100,000 PY. Standardized mortality ratios (SMRs) were calculated as observed numbers of deaths in the SEARCH study cohort divided by expected numbers of deaths based on age, sex, and race/ethnicity distributions for U.S. state and county populations from which diabetes cases were identified. These areas included corresponding state (South Carolina and Colorado) and county populations (California, seven counties; Washington, five counties; Ohio, four counties; Kentucky, three counties; Indiana, one county; Arizona, three counties; and New Mexico, seven counties). The Kentucky and Indiana counties were part of the Ohio surveillance area. The county populations in Arizona and New Mexico were restricted to the Native American YYAs, as only Indian Health Service beneficiaries were enrolled from these counties.
For each year, population sizes and deaths in the corresponding state and county populations were obtained from the Centers for Disease Control and Prevention Wide-ranging Online Data for Epidemiologic Research (CDC WONDER) online tool, which contains mortality and population counts for all U.S. counties. The 95% CIs for the SMRs are calculated using Byars approximation of the exact Poisson distribution (15). A two-sided skew-corrected inverted score test assuming a binomial distribution was used to determine if the SMRs were significantly different for type 1 and type 2 diabetes. While the main focus of these analyses was individuals with type 1 and type 2 diabetes, the largest contributors to youth-onset diabetes incidence, we included limited analyses for the secondary and other/unknown diabetes type groups both for cohort completeness and due to the potential for high mortality rate among the secondary diabetes cases. Cause-specific mortality rates were not calculated because the numbers of deaths were too small for reliable estimates. However, we described the underlying causes of death and contributing cause of death when it was diabetes stratified by diabetes type and for YYA with type 1 and type 2 diabetes, additionally stratified by sex as an exploratory analysis.
Results
These analyses included 19,717 individuals with youth-onset diabetes with a median follow-up period was 8.5 years (range 0–16 years) (Table 1). During 170,148 PY of observation, there were 283 deaths: 133 decedents with type 1 diabetes, 55 with type 2 diabetes, 87 with secondary diabetes, and 8 with other/unknown diabetes type (Supplementary Table 2). The corresponding duration of diabetes at death (mean [SD]) was 7.4 (4.5) years, 6.6 (4.2) years, 4.4 (3.7) years, and 3.9 (4.6) years, respectively (Table 1). Time from diagnosis to death by diabetes type is shown in Supplementary Fig. 1.
Table 1.
Demographic and clinical characteristics of the 19,717 youth-onset diabetes cases in the SEARCH for Diabetes in Youth mortality surveillance study, overall and by diabetes type, incident years 2002–2015
| Diabetes type | |||||
|---|---|---|---|---|---|
| Total | Type 1 | Type 2 | Secondary | Other/unknown‡ | |
| N | 19,717 | 14,721 | 4,141 | 551 | 304 |
| Age at diabetes dx, years, mean (SD) | 11.1 (4.6) | 10.0 (4.5) | 14.8 (2.8) | 13.4 (4.1) | 13.3 (4.2) |
| Age at diabetes dx, years, n (%) | |||||
| 0–4 | 2,521 (12.8) | 2,472 (16.8) | 7 (0.2) | 29 (5.3) | 13 (4.3) |
| 5–9 | 4,925 (25.0) | 4,635 (31.5) | 186 (4.5) | 53 (9.6) | 51 (16.9) |
| 10–14 | 7,725 (39.2) | 5,449 (37.0) | 1,905 (46.0) | 255 (46.3) | 116 (38.4) |
| 15–19 | 4,543 (23.0) | 2,164 (14.7) | 2,043 (49.3) | 214 (38.8) | 122 (40.4) |
| Sex, n (%) | |||||
| Female | 9,935 (50.4) | 6,918 (47.0) | 2,536 (61.2) | 310 (56.3) | 171 (56.6) |
| Male | 9,780 (49.6) | 7,803 (53.0) | 1,605 (38.8) | 241 (43.7) | 131 (43.4) |
| Race/Ethnicity, n (%) | |||||
| Non-Hispanic White | 11,177 (56.7) | 9,995 (67.9) | 752 (18.2) | 312 (56.6) | 118 (38.8) |
| Non-Hispanic Black | 3,576 (18.1) | 1,841 (12.5) | 1,556 (37.6) | 110 (20.0) | 69 (22.7) |
| Hispanic | 3,498 (17.7) | 2,137 (14.5) | 1,181 (28.5) | 99 (18.0) | 81 (26.6) |
| Other/unknown* | 1,466 (7.4) | 748 (5.1) | 652 (15.7) | 30 (5.4) | 36 (11.8) |
| Year of diagnosis, n (%) | |||||
| 2002–2005 | 4,961 (25.2) | 3,842 (26.1) | 905 (21.9) | 147 (26.7) | 67 (22.0) |
| 2006–2010 | 7,105 (36.0) | 5,299 (36.0) | 1,464 (35.4) | 225 (40.8) | 117 (38.5) |
| 2011–2015 | 7,651 (38.8) | 5,580 (37.9) | 1,772 (42.8) | 179 (32.5) | 120 (39.5) |
| Follow-up time from dx, years,† median (minimum–maximum) | 8.5 (0–16) | 8.7 (0–16) | 7.8 (0–16) | 7.9 (0–16) | 8.2 (0–15.9) |
| Age at death/censor, years, mean (SD) | 19.7 (5.9) | 18.7 (5.9) | 23.0 (4.7) | 21.5 (5.7) | 21.8 (5.8) |
| Age group at death/censor, years, n (%) | |||||
| <15 | 4,222 (21.4) | 3,971 (27.0) | 152 (3.7) | 63 (11.4) | 36 (11.9) |
| 15–19 | 5,939 (30.1) | 4,693 (31.9) | 1,018 (24.6) | 149 (27.0) | 79 (26.2) |
| 20–24 | 5,607 (28.4) | 3,748 (25.5) | 1,575 (38.0) | 182 (33.0) | 102 (33.8) |
| 25–29 | 3,183 (16.1) | 1,942 (13.2) | 1,060 (25.6) | 122 (22.1) | 59 (19.5) |
| 30–34 | 762 (3.9) | 366 (2.5) | 335 (8.1) | 35 (6.4) | 26 (8.6) |
| PY of follow-up | 170,148 | 129,083 | 34,046 | 4,457 | 2,562 |
dx, diagnosis.
Other/unknown race/ethnicity (n = 1,466) is comprised of Asian/Pacific Islanders (n = 618), Native Americans (n = 353), non-Hispanic/other races (n = 226), and unknown race/ethnicity (n = 269).
Follow-up time is from diabetes diagnosis to death or censoring on 31 December 2017 (the end date for the NDI search).
Among the other/unknown diabetes type group, 76 (25.0%) had monogenic diabetes, 4 (1.3%) had hybrid diabetes type, and 224 (73.7%) had unknown diabetes type or their type was missing from the medical record.
SMRs
Among individuals with type 1 diabetes, the crude mortality rate was 103.0/100,000 PY, and the overall SMR was 1.5 (95% CI 1.2, 1.8) (Table 2). The SMR was significantly higher than the underlying population for individuals <20 years of age (<15 and 15–19 years), for non-Hispanic White and Hispanic individuals and for females but not males (Fig. 1A). Among individuals with type 2 diabetes, the overall crude morality rate was 161.5/100,000 PY, and the SMR was 2.3 (95% CI 1.7, 3.0) (Table 2 and Fig. 1B). The SMR was significantly higher for individuals <25 years of age (<15, 15–19, and 20–24 years), among YYAs from all race/ethnic groups except non-Hispanic White, and among both males and females (Fig. 1B). The crude mortality rate for YYAs with type 2 was significantly higher than for YYAs with type 1 diabetes (P < 0.001) (Table 2). For secondary and unknown diabetes type, the crude mortality rates were 1,952.0 and 312.3, respectively, and the SMRs were 28.0 (95% CI 22.4, 34.6) and 4.5 (95% CI 1.9, 8.8), respectively (data not shown).
Table 2.
Mortality rates per 100,000 PY through 31 December 2017 among 18,862 YYAs with type 1 and type 2 diabetes by diabetes type for incident years 2002–2015, and for comparable state/county populations: the SEARCH for Diabetes in Youth Study
| Type 1 diabetes, N = 14,721 incident cases | Type 2 diabetes, N = 4,141 incident cases | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| PY | N of deaths | Crude mortality rate/100,000 PY | PY | N of deaths | Crude mortality rate/100,000 PY | |||||
| Observed | Expected | SEARCH | Population* | Observed | Expected | SEARCH | Population* | |||
| All cases | 129,083 | 133 | 89 | 103.0 | 69.7 | 34,046 | 55 | 23 | 161.5 | 69.7 |
| Sex | ||||||||||
| Female | 61,241 | 58 | 28 | 94.7 | 46.4 | 20,889 | 21 | 10 | 100.5 | 46.4 |
| Male | 67,842 | 75 | 61 | 110.6 | 91.8 | 13,157 | 34 | 12 | 258.4 | 91.8 |
| Race/ethnicity | ||||||||||
| NH White | 88,962 | 88 | 61 | 98.9 | 69.1 | 6,569 | 7 | 5 | 106.6 | 69.1 |
| NH Black | 15,691 | 22 | 19 | 140.2 | 122.4 | 12,561 | 27 | 15 | 215.0 | 122.4 |
| Hispanic | 17,790 | 19 | 11 | 106.8 | 60.0 | 9,460 | 11 | 6 | 116.3 | 60.0 |
| Other/unknown | 6,640 | 4 | 3 | 60.2 | 52.3 | 5,456 | 10 | 2 | 183.3 | 52.3 |
| Age at death or end of follow-up, years | ||||||||||
| <15 | 22,253 | 20 | 12 | 89.9 | 52.7 | 553 | 2 | 0 | 361.6 | 52.7 |
| 15–19 | 38,624 | 50 | 20 | 129.5 | 51.3 | 4,923 | 15 | 2 | 304.7 | 51.3 |
| 20–24 | 38,340 | 40 | 32 | 104.3 | 84.3 | 11,559 | 23 | 10 | 199.0 | 84.3 |
| 25–29 | 24,596 | 20 | 21 | 81.3 | 88.3 | 12,239 | 11 | 11 | 89.9 | 88.3 |
| 30–34 | 5,271 | 2 | 5 | 37.9 | 102.9 | 4,772 | 3 | 5 | 62.9 | 102.9 |
NH, non-Hispanic.
Population: the U.S. state and county populations from which the cases were drawn.
Figure 1.
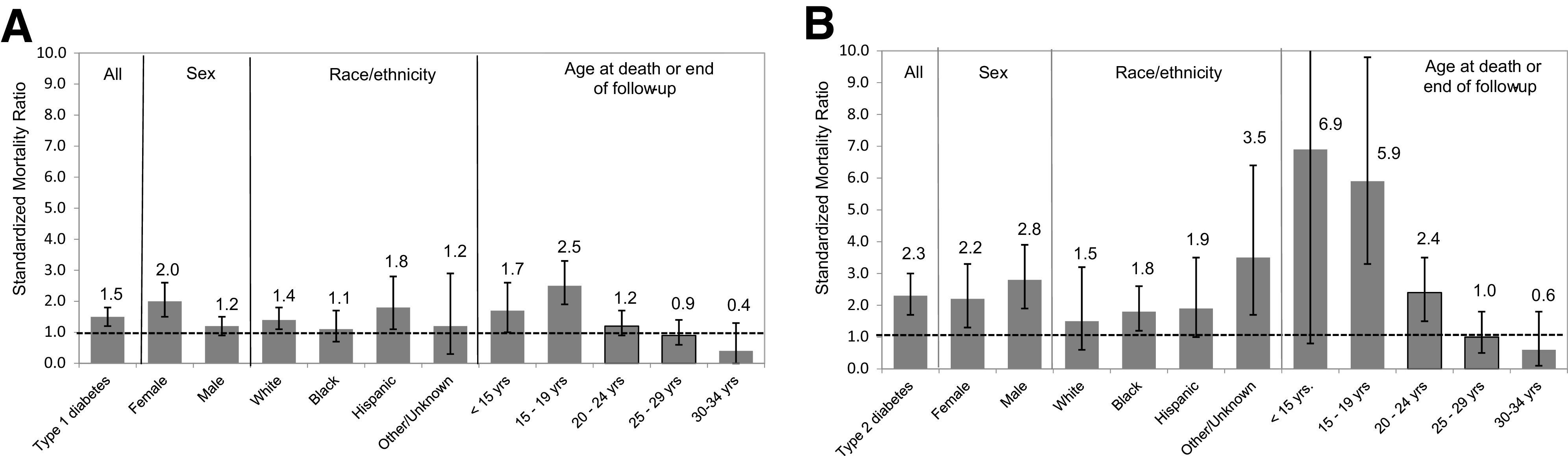
SMRs and 95% CIs for type 1 (A) and type 2 (B) diabetes overall and by sex, race/ethnicity, and age at death or end of follow-up. The number on the top of or beside the bar is the SMR. The error bars show the range of the 95% CI. The top of the error bar for <15 years in B is 24.9.
Cause of Death
Among decedents with type 1 diabetes, the most frequent underlying cause of death was diabetes (42.1%) of which two-thirds were coded as having ketoacidosis (E10.1 or E14.1) or coma (E14.0) (Table 3). This did not differ significantly by sex; 39.7% of females and 44.0% of males had diabetes reported as the underlying cause of death (P = 0.25) (Supplementary Table 3). The other most frequent underlying causes of death were external causes of morbidity and mortality (36.8%) comprised predominantly of accidental injury (12.8%), transport/motor vehicle accidents (12.0%), and intentional self-harm (9.8%). There was not a significant difference for females and males (29.3% vs. 42.7%; P = 0.11), respectively (Supplementary Table 3). Diabetes was a contributing cause of death for 10.5% of individuals with type 1 diabetes. For deaths in which diabetes was the contributing cause (n = 14), the underlying cause was external causes (V00–Y89, 64.3%), diseases of the central nervous system (G04.9, 21.4%), the circulatory system (I26.9, 7.1%), and the musculoskeletal system (M32.1, 7.1%) (data not shown).
Table 3.
Underlying cause of death for 283 decedents for 2002–2015 incident diabetes cases through 31 December 2017 by diabetes type: the SEARCH for Diabetes in Youth Study
| Diabetes type | |||||
|---|---|---|---|---|---|
| ICD-10 codes | Type 1, N (%) | Type 2, N (%) | Secondary, N (%) | Other/unknown,* N (%) | |
| Deaths from all causes, N | — | 133 | 55 | 87 | 8 |
| Underlying cause of death | |||||
| Certain infectious and parasitic disease | A00–B99 | 1 (0.8) | 2 (3.6) | 5 (5.7) | 0 |
| Cancer/neoplasms | C00–D48 | 1 (0.8) | 6 (10.9) | 10 (11.5) | 2 (25.0) |
| Diseases of the blood and blood-forming organs | D50–D89 | 1 (0.8) | 2 (3.6) | 2 (2.3) | 0 |
| Diabetes | E00–E14 | 56 (42.1) | 5 (9.1) | 4 (4.6) | 1 (12.5) |
| Type 1 diabetes with ketoacidosis | E10.1 | 12 (9.0) | 0 | 0 | 0 |
| Type 1 diabetes with renal complications | E10.2 | 0 | 0 | 0 | 1 (12.5) |
| Type 1 diabetes with without complications | E10.9 | 6 (4.5) | 0 | 0 | 0 |
| Unspecified diabetes, with coma | E14.0 | 1 (0.8) | 1(1.8) | 0 | 0 |
| Unspecified diabetes, with ketoacidosis | E14.1 | 25 (18.8) | 2 (3.6) | 0 | 0 |
| Unspecified diabetes with renal complications | E14.2 | 0 | 1 (1.8) | 1 (1.1) | 0 |
| Unspecified diabetes with multiple complications | E14.7 | 1 (0.8) | 0 | 0 | 0 |
| Unspecified diabetes, without complications | E14.9 | 11 (8.3) | 1 (1.8) | 3 (3.4) | 0 |
| Metabolic disorders | E70–E90 | 0 | 1 (1.8) | 36 (41.4) | 1 (12.5) |
| Neuronal ceroid lipofuscinosis | E75.4 | 0 | 1 (1.8) | 0 | 0 |
| Disorders of iron metabolism | E83.1 | 0 | 0 | 1 (1.1) | 0 |
| CF | E84.x | 0 | 0 | 35 (40.2) | 1 (12.5) |
| Mental and behavioral disorders | F01–F99 | 0 | 1 (1.8) | 1 (1.1) | 1 (12.5) |
| Diseases of the nervous system | G00–G98 | 8 (6.0) | 4 (7.3) | 4 (4.6) | 0 |
| Diseases of the circulatory system | I00–I99 | 6 (4.5) | 5 (9.1) | 6 (6.9) | 0 |
| Diseases of the respiratory system | J00–J98 | 2 (1.5) | 2 (3.6) | 2 (2.3) | 0 |
| Diseases of the digestive system | K00–K92 | 0 | 1 (1.8) | 2 (2.3) | 1 (12.5) |
| Diseases of the musculoskeletal system and connective tissue | M00–M99 | 1 (0.8) | 0 | 4 (4.6) | 0 |
| Diseases of the genitourinary system | N00–N98 | 1 (0.8) | 1 (1.8) | 1 (1.1) | 0 |
| Pregnancy, childbirth, and the puerperium | O00–O99 | 0 | 0 | 2 (2.3) | 0 |
| Certain conditions originating in perinatal period | P00–P96 | 1 (0.8) | 0 | 0 | 0 |
| Congenital malformations, deformations, and chromosomal abnormalities | Q00–Q99 | 1 (0.8) | 4 (7.3) | 2 (2.3) | 1 (12.5) |
| Symptoms, signs, and abnormal clinical and laboratory findings, not elsewhere classified | R00–R99 | 2 (1.5) | 0 | 0 | 0 |
| External causes of morbidity and mortality | V00–Y89 | 49 (36.8) | 19 (34.5) | 6 (6.9) | 0 |
| Transport/motor vehicle accident | V00–V99 | 16 (12.0) | 4 (7.3) | 3 (3.4) | 0 |
| Other external causes of accidental injury | W00–X59 | 17 (12.8) | 6 (10.9) | 2 (2.3) | 0 |
| Intentional self-harm | X60–X74 | 13 (9.8) | 2 (3.6) | 1 (1.1) | 0 |
| Assault | X85–Y09 | 1 (0.8) | 5 (9.1) | 0 | 0 |
| Event of undetermined intent | Y10–Y34 | 2 (1.5) | 0 | 0 | 0 |
| Complications of medical/surgical care | Y40–Y84 | 0 | 1 (1.8) | 0 | 0 |
| Sequelae of external causes of morbidity and mortality | Y85–Y89 | 0 | 1 (1.8) | 0 | 0 |
| Unknown cause of death reported to study† | Unknown | 3 (2.3) | 2 (3.6) | 0 | 1 (12.5) |
| Contributing cause of death | |||||
| Diabetes | E00–E14 | 14 (10.5) | 7 (12.7) | 10 (11.5) | 2 (25.0) |
All eight of these decedents had their type classified as unknown. None were classified as having monogenic or hybrid diabetes type.
Reported as deceased by the family or medical care providers but were not matched in the NDI search due to nonlinkage with the NDI.
Among decedents with type 2 diabetes, diabetes was the underlying cause of death for 9.1%; the most frequent causes of death were external causes of morbidity and mortality (34.5%), including predominantly other external causes of injury (10.9%), assault (9.1%), and transport/motor vehicle accident (7.3%) as well as cancer (10.9%) and diseases of the circulatory system (9.1%). Diabetes was a contributing cause of death for 12.7% of decedents. For deaths with diabetes as a contributing cause (n = 7), one was attributed to an external cause (X31) and the other six to a variety of medical conditions (data not shown).
Among decedents with secondary diabetes, diabetes was the underlying cause of death for 4.6% and a contributing cause of death for 11.5%. The most frequent underlying cause of death was cystic fibrosis (CF) (E84.x, 40.2%), and the next most frequent cause was cancer (11.5%). Only 6.9% of deaths were from external causes.
Conclusions
YYAs with youth-onset diabetes experience mortality at significantly higher rates than the general population with varying degrees of excess mortality by diabetes type after a median follow-up of just over 8 years after diabetes diagnosis. Compared with mortality for YYAs in comparable regions of the United States, mortality was ∼1.5 times greater for YYAs with type 1 diabetes, 2.3 times greater for type 2 diabetes, and 28 times greater for secondary diabetes, which is often caused by conditions with significant morbidity and mortality, such as CF, pancreatitis, medications such as glucocorticoids, and genetic syndromes (16).
Type 1 Diabetes
Excess mortality in earlier studies of individuals with type 1 diabetes was greater than in the more contemporary studies, including the current study, and has varied significantly by country (4). As examples, in the Allegheny County (Pennsylvania) registry (diagnosed at <18 years old from 1965–1979), there was seven times greater mortality than the comparison population after a mean of 30 years of diabetes duration (7). In the Chicago Diabetes Registry diagnosed with presumptive type 1 diabetes <18 years between 1985–2000 and followed over 7.8 years, the death rate was 237/100,000 PY (6), which was twice that reported in the current study (103/100,000 PY) during a median of 8.7 years of follow-up. In the Western Australia Children’s Diabetes Database (aged <18 years at diagnosis from 1987–2011), there were 74.5 deaths/100,000 PY during 7.6 years of follow-up, which is less than identified in the SEARCH study (11). In the SWEDIABKIDS register (diagnosed <18 years of age, 2006–2014), the SMR was 2.7 compared with the general Swedish population (17). In a study in Yorkshire, U.K. (diagnosed <15 years of age from 1978 to 2013) followed for a median of 17.7 years, there were 188 deaths/100,000 PY (5). Mortality in the last diagnosis period (2006–2013) of the U.K. study was significantly lower (hazard ratio 0.13) than the earliest periods. The lower mortality rates and SMRs seen in the Western Australia and SEARCH registries could be due to a shorter duration of diabetes and the focus on more contemporary cohorts, which may have benefited from advances in diabetes treatment.
Mortality was significantly higher (SMR 2.0) for females with type 1 diabetes but not for males. Other studies have reported excess deaths for females compared with males with type 1 diabetes. The Western Australian Children’s Diabetes Database found that all-cause mortality for females with type 1 diabetes was 10 times that of the general population in early adulthood, but there was no increased mortality risk for males (11), and in Sweden, there was also significant excess mortality for females with type 1 diabetes (SMR 8.7) but not males (SMR 1.8) (17). In Northern Ireland (18), both males and females had excess mortality compared with the general population, but the excess was much greater for females (SMR 534) than for males (SMR 202). In the current study, we observed that the crude mortality rates for males and females with type 1 diabetes were similar—94.7/100,000 and 110.6/100,000, respectively—and the hazard ratios were not significantly different by sex. However, the SMR is higher for females because the mortality rate for the female comparison population was lower than for our cohort with type 1 diabetes. The proportion of the underlying causes of death attributed to diabetes and external causes were similar for males and females.
Among all decedents with type 1 diabetes, approximately two-thirds of the deaths with diabetes as the underlying cause were attributed to diabetes with diabetic ketoacidosis (DKA) or coma. Hospitalizations for DKA among individuals <45 years of age decreased slightly from 2000 to 2009 and then increased steadily from 2009 until 2014, although the case fatality rates from DKA have declined over time (19).
Type 2 Diabetes
Both males and females with type 2 diabetes had excess mortality as did Black and Hispanic YYAs. For White YYAs, the difference in mortality between youth with type 2 diabetes and the comparable population was not statistically significant. There are few studies of mortality among individuals with youth-onset type 2 diabetes, a relatively recent condition. In a population-based study of Pima Indians in Arizona conducted between 1965 and 2002, the death rate was 3.0 times as high in individuals with youth-onset type 2 diabetes and 1.4 times as high in individuals with older-onset diabetes (aged 20–54 years) compared with nondiabetic controls (20). In an Australian study that included 588 individuals diagnosed with type 2 diabetes between 15 and 29 years of age from 1986 onward, including deaths through 2011, the SMR was 3.4. While the crude mortality rate was lowest for individuals in this age group, the SMR declined linearly with each 10-year increment (2.5 for 30–39 years and 1.8 for 40–49 years) (21). Similarly, a recent meta-analysis reported that each 1-year increase in age at type 2 diabetes diagnosis was associated with a 4% decreased risk of all-cause mortality when adjusted for current age (22). Thus, while preventing type 2 diabetes would provide the maximum reduction in mortality, delaying the onset of type 2 diabetes until later in life may also result in a reduction in mortality.
Among YYAs with type 2 diabetes, only 9.1% were attributed to diabetes, while about a third were attributed to external causes (e.g., motor vehicle accidents, other accidental injuries, and assault) and the remainder to other health conditions. The proportion of deaths attributable to external causes (34.5%) was consistent with the U.S. population in general. The leading cause of death for individuals in the United States aged 1–44 years is unintentional injuries (31.8% of 1–9 years, 40.6% of 10–24 years, and 34.6% of 25–44 years) (23). However, there remains an excess in mortality among YYAs with type 2 diabetes beyond that experienced by the comparison population, perhaps due in part to socioeconomic disadvantage, as evidenced by lower household income, lower parental education, and greater reliance on Medicaid (24). Mortality in childhood and early adulthood has been shown to be associated with parental socioeconomic status (25). Lower levels of educational attainment and financial wealth have been shown to be strong predictors of mortality risk among adults with diabetes (26).
Secondary Diabetes
The mortality rate from secondary diabetes, which includes diseases of the exocrine pancreas (such as CF and pancreatitis), and drug- or chemical-induced diabetes (such as chemotherapy and glucocorticoids) was much higher than for youth with type 1 or type 2 diabetes and the general population. The largest number of deaths in our secondary diabetes cohort was attributed to CF. CF-related diabetes (CFRD) is the most common comorbidity in individuals with CF. CFRD occurs in <5% of children with CF aged ≤10 years and 15–20% of adolescents (27). The risk of CFRD is increased using glucocorticoids and immunosuppressive drugs that are associated with worsening pulmonary disease and transplantation (28,29). We found that only 7% of deaths among YYAs with secondary diabetes were attributed to external causes; most of these deaths were attributed to medical conditions.
Limitations and Strengths
There are several limitations to our study. We did not conduct cause-specific mortality analyses or calculate SMRs by specific causes of death due to the relatively small number of deaths. Our outcomes, vital status, and cause of death were based on linkage with the NDI. Studies have demonstrated that the NDI is an accurate source for ascertaining vital status even when social security numbers are not available. Sensitivity of the NDI ranges from 87% to 98%, and use of different combinations of personal identifiers can correctly identify 83% to 92% of decedents and 92% to 99% of living individuals (30). While our analyses covered 14 years of incident diabetes cases in the SEARCH registry, we did not have a large enough sample size to undertake a trend analysis because of the larger number of cases in later years (with shorter duration of diabetes) compared with the earlier years of the study due to increasing incidence (1). A small number of cases were excluded due to missing information required for linkage. The direction of potential bias caused by excluding these cases is unknown, although excluding such a small proportion likely had only a minor effect on the overall results.
The strengths of our study include the large contemporary population-based cohort of individuals with youth-onset diabetes diagnosed in the past two decades, including perhaps the largest population-based sample of individuals with youth-onset type 2 diabetes. Mortality data for individuals with youth-onset type 2 diabetes is particularly limited, and studies have reported higher mortality with younger ages of type 2 diabetes diagnosis (21,22). Consistent methods were used for ascertainment of incident diabetes cases with high levels of completeness (1,31) and for the determination of diabetes type since the beginning of the SEARCH study, making the comparison of mortality rates for type 1, type 2, and secondary diabetes robust. While the number of Asian/Pacific Islander and Native American YYAs was small relative to the other three race/ethnic groups, there is significant racial/ethnic diversity among the YYAs in the overall SEARCH registry, and the large sample sizes for non-Hispanic White, Black, and Hispanic YYAs allowed for important comparisons of SMRs for these three race/ethnic groups.
Conclusion
Among individuals with youth-onset diabetes, there is excess short-term mortality, with this excess mortality being greater for type 2 and secondary diabetes than for type 1 diabetes after a median of 8 years of diabetes duration. With the rising number of YYAs with youth-onset diabetes (1–3), the number of excess deaths among persons with diabetes is also likely to rise unless the etiology of the excess mortality associated with having diabetes can be identified and prevented. Detailed cause-specific mortality analyses would be needed to determine whether specific sociodemographic characteristics are associated with cause of death.
Article Information
Acknowledgments. The SEARCH for Diabetes in Youth Study is indebted to the many youths, families, and health care providers, whose participation made this study possible.
Funding. SEARCH 4: The SEARCH for Diabetes in Youth Cohort Study is funded by the National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases (1R01DK127208-01 and 1UC4DK108173) and supported by the CDC. The Population Based Registry of Diabetes in Youth Study is funded by the CDC (DP-15-002) National Center for Chronic Disease Prevention and Health Promotion (1U18DP0 06131, U18DP006133, U18DP006134, U18DP006 136, U18DP006138, and U18DP006139) and supported by the National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. SEARCH 1–3: SEARCH for Diabetes in Youth is funded by the CDC (Program Announcement numbers 00097, DP-05-069, and DP-10-001) and supported by the National Institute of Diabetes and Digestive and Kidney Diseases. Funding was also provided by Kaiser Permanente Southern California (U48/CCU919219, U01 DP000246, and U18DP002714), University of Colorado Denver (U48/CCU819241-3, U01 DP000247, and U18DP000247-06A1), Cincinnati Children’s Hospital Medical Center (U48/CCU519239, U01 DP000248, and 1U18DP002709), University of North Carolina at Chapel Hill (U48/CCU419249, U01 DP000254, and U18DP002708), Seattle Children’s Hospital (U58/CCU019235-4, U01 DP000244, and U18DP002710-01), and Wake Forest University School of Medicine (U48/CCU919219, U01 DP000250, and 200-2010-35171).
The authors acknowledge the involvement of the Kaiser Permanente Southern California’s Marilyn Owsley Clinical Research Center (funded by Kaiser Foundation Health Plan and supported in part by the Southern California Permanente Medical Group), the South Carolina Clinical & Translational Research Institute at the Medical University of South Carolina, National Institutes of Health (NIH)/National Center for Advancing Translational Sciences (NCATS) (grants UL1 TR000062 and UL1 TR001450), Seattle Children’s Hospital and the University of Washington (NIH/NCATS grant number UL1 TR00423), University of Colorado Pediatric Clinical and Translational Research Center (NIH/NCATS grant UL1 TR000154), the Barbara Davis Center at the University of Colorado at Denver (Diabetes Endocrinology Research Centers NIH grant P30 DK57516), the University of Cincinnati (NIH/NCATS grants UL1 TR000077 and UL1 TR001425), and the Children with Medical Handicaps program managed by the Ohio Department of Health.
This study includes data provided by the Ohio Department of Health, which should not be considered an endorsement of this study or its conclusions. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC or the National Institute of Diabetes and Digestive and Kidney Diseases.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. J.M.L., A.M., C.P., D.D., L.D., and L.H. researched or oversaw the collection of the data. J.M.L., K.R., S.I., and L.W. wrote the manuscript. S.H.S., A.M., C.P., D.D., L.D., L.H., A.D.L., and J.D. reviewed and edited the manuscript. All authors reviewed and approved the final version of the manuscript. S.I. is the guarantor of this work and, as such, had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article contains supplementary material online at https://doi.org/10.2337/figshare.16606313.
A complete list of the SEARCH for Diabetes in Youth Study Group can be found in the supplementary material online.
Contributor Information
Collaborators: SEARCH for Diabetes in Youth Study Group:, Jean M. Lawrence, Peggy Hung, Corinna Koebnick, Xia Li, Eva Lustigova, Kristi Reynolds, David J. Pettitt, Elizabeth J. Mayer-Davis, Amy Mottl, Joan Thomas, Malaka Jackson, Lisa Knight, Angela D. Liese, Christine Turley, Deborah Bowlby, James Amrhein, Elaine Apperson, Bryce Nelson, Dana Dabelea, Anna Bellatorre, Tessa Crume, Richard F. Hamman, Katherine A. Sauder, Allison Shapiro, Lisa Testaverde, Georgeanna J. Klingensmith, David Maahs, Marian J. Rewers, Paul Wadwa, Stephen Daniels, Michael G. Kahn, Greta Wilkening, Clifford A. Bloch, Jeffrey Powell, Kathy Love-Osborne, Diana C. Hu, Lawrence M. Dolan, Amy S. Shah, Debra A. Standiford, Elaine M. Urbina, Catherine Pihoker, Irl Hirsch, Grace Kim, Faisal Malik, Lina Merjaneh, Alissa Roberts, Craig Taplin, Joyce Yi-Frazier, Natalie Beauregard, Cordelia Franklin, Carlo Gangan, Sue Kearns, Mary Klingsheim, Beth Loots, Michael Pascual, Carla Greenbaum, Santica M. Marcovina, Alan Chait, Noemie Clouet-Foraison, Jessica Harting, Greg Strylewicz, Ralph D’Agostino, Jr., Elizabeth T. Jensen, Lynne E. Wagenknecht, Ramon Casanova, Jasmin Divers, Maureen T. Goldstein, Leora Henkin, Scott Isom, Kristin Lenoir, June Pierce, Beth Reboussin, Joseph Rigdon, Andrew Michael South, Jeanette Stafford, Cynthia Suerken, Brian Wells, Carrie Williams, Giuseppina Imperatore, Sharon H. Saydah, and Barbara Linder
References
- 1. Divers J, Mayer-Davis EJ, Lawrence JM, et al. Trends in incidence of type 1 and type 2 diabetes among youths - selected counties and Indian reservations, United States, 2002-2015. MMWR Morb Mortal Wkly Rep 2020;69:161–165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lawrence JM, Divers J, Isom S, et al.; SEARCH for Diabetes in Youth Study Group . Trends in prevalence of type 1 and type 2 diabetes in children and adolescents in the US, 2001-2017. JAMA 2021;326:717–727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Imperatore G, Boyle JP, Thompson TJ, et al.; SEARCH for Diabetes in Youth Study Group . Projections of type 1 and type 2 diabetes burden in the U.S. population aged <20 years through 2050: dynamic modeling of incidence, mortality, and population growth. Diabetes Care 2012;35:2515–2520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Morgan E, Cardwell CR, Black CJ, McCance DR, Patterson CC. Excess mortality in type 1 diabetes diagnosed in childhood and adolescence: a systematic review of population-based cohorts. Acta Diabetol 2015;52:801–807 [DOI] [PubMed] [Google Scholar]
- 5. Evans-Cheung TC, Bodansky HJ, Parslow RC, Feltbower RG. Mortality and acute complications in children and young adults diagnosed with type 1 diabetes in Yorkshire, UK: a cohort study. Diabet Med 2018;35:112–120 [DOI] [PubMed] [Google Scholar]
- 6. Burnet DL, Cooper AJ, Drum ML, Lipton RB. Risk factors for mortality in a diverse cohort of patients with childhood-onset diabetes in Chicago. Diabetes Care 2007;30:2559–2563 [DOI] [PubMed] [Google Scholar]
- 7. Secrest AM, Becker DJ, Kelsey SF, LaPorte RE, Orchard TJ. All-cause mortality trends in a large population-based cohort with long-standing childhood-onset type 1 diabetes: the Allegheny County type 1 diabetes registry. Diabetes Care 2010;33:2573–2579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Washington RE, Orchard TJ, Arena VC, LaPorte RE, Secrest AM, Tull ES. All-cause mortality in a population-based type 1 diabetes cohort in the U.S. Virgin Islands. Diabetes Res Clin Pract 2014;103:504–509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Asao K, Sarti C, Forsen T, et al.; Diabetes Epidemiology Research International Mortality Study Group . Long-term mortality in nationwide cohorts of childhood-onset type 1 diabetes in Japan and Finland. Diabetes Care 2003;26:2037–2042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bruno G, Cerutti F, Merletti F, et al.; Piedmont Study Group for Diabetes Epidemiology . Short-term mortality risk in children and young adults with type 1 diabetes: the population-based Registry of the Province of Turin, Italy. Nutr Metab Cardiovasc Dis 2009;19:340–344 [DOI] [PubMed] [Google Scholar]
- 11. Cooper MN, de Klerk NH, Jones TW, Davis EA. Clinical and demographic risk factors associated with mortality during early adulthood in a population-based cohort of childhood-onset type 1 diabetes. Diabet Med 2014;31:1550–1558 [DOI] [PubMed] [Google Scholar]
- 12. Reynolds K, Saydah SH, Isom S, et al. Mortality in youth-onset type 1 and type 2 diabetes: The SEARCH for Diabetes in Youth study. J Diabetes Complications 2018;32:545–549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hamman RF, Bell RA, Dabelea D, et al.; SEARCH for Diabetes in Youth Study Group . The SEARCH for Diabetes in Youth Study: rationale, findings, and future directions. Diabetes Care 2014;37:3336–3344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Centers for Disease Control and Prevention, National Center for Health Statistics . National Death Index Hyattsville, MD 20782. Accessed 1 February 2021. Available from https://www.cdc.gov/nchs/ndi/index.htm
- 15. Breslow NE, Day NE. Statistical methods in cancer research. Volume II--The design and analysis of cohort studies. IARC Sci Publ 1987;82: 1–406 [PubMed] [Google Scholar]
- 16. American Diabetes Association . 2. Classification and diagnosis of diabetes: Standards of Medical Care in Diabetes—2020. Diabetes Care 2020;43(Suppl. 1):S14–S31 [DOI] [PubMed] [Google Scholar]
- 17. Samuelsson J, Samuelsson U, Hanberger L, Bladh M, Åkesson K. Poor metabolic control in childhood strongly correlates to diabetes-related premature death in persons <30 years of age-A population-based cohort study. Pediatr Diabetes 2020;21:479–485 [DOI] [PubMed] [Google Scholar]
- 18. Morgan E, Black CR, Abid N, Cardwell CR, McCance DR, Patterson CC. Mortality in type 1 diabetes diagnosed in childhood in Northern Ireland during 1989-2012: a population-based cohort study. Pediatr Diabetes 2018;19:166–170 [DOI] [PubMed] [Google Scholar]
- 19. Benoit SR, Zhang Y, Geiss LS, Gregg EW, Albright A. Trends in diabetic ketoacidosis hospitalizations and in-hospital mortality - United States, 2000-2014. MMWR Morb Mortal Wkly Rep 2018;67:362–365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Pavkov ME, Bennett PH, Knowler WC, Krakoff J, Sievers ML, Nelson RG. Effect of youth-onset type 2 diabetes mellitus on incidence of end-stage renal disease and mortality in young and middle-aged Pima Indians. JAMA 2006;296:421–426 [DOI] [PubMed] [Google Scholar]
- 21. Al-Saeed AH, Constantino MI, Molyneaux L, et al. An inverse relationship between age of type 2 diabetes onset and complication risk and mortality: the impact of youth-onset type 2 diabetes. Diabetes Care 2016;39:823–829 [DOI] [PubMed] [Google Scholar]
- 22. Nanayakkara N, Curtis AJ, Heritier S, et al. Impact of age at type 2 diabetes mellitus diagnosis on mortality and vascular complications: systematic review and meta-analyses. Diabetologia 2021;64:275–287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Heron M. Deaths: leading causes for 2017. Natl Vital Stat Rep 2019;68:1–77 [PubMed] [Google Scholar]
- 24. Dabelea D, Stafford JM, Mayer-Davis EJ, et al.; SEARCH for Diabetes in Youth Research Group . Association of type 1 diabetes vs type 2 diabetes diagnosed during childhood and adolescence with complications during teenage years and young adulthood. JAMA 2017;317:825–835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Braudt DB, Lawrence EM, Tilstra AM, Rogers RG, Hummer RA. Family socioeconomic status and early life mortality risk in the United States. Matern Child Health J 2019;23:1382–1391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Saydah SH, Imperatore G, Beckles GL. Socioeconomic status and mortality: contribution of health care access and psychological distress among U.S. adults with diagnosed diabetes. Diabetes Care 2013;36:49–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Moran A, Dunitz J, Nathan B, Saeed A, Holme B, Thomas W. Cystic fibrosis-related diabetes: current trends in prevalence, incidence, and mortality. Diabetes Care 2009;32:1626–1631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hadjiliadis D, Madill J, Chaparro C, et al. Incidence and prevalence of diabetes mellitus in patients with cystic fibrosis undergoing lung transplantation before and after lung transplantation. Clin Transplant 2005;19:773–778 [DOI] [PubMed] [Google Scholar]
- 29. Marshall BC, Butler SM, Stoddard M, Moran AM, Liou TG, Morgan WJ. Epidemiology of cystic fibrosis-related diabetes. J Pediatr 2005;146:681–687 [DOI] [PubMed] [Google Scholar]
- 30. Williams BC, Demitrack LB, Fries BE. The accuracy of the National Death Index when personal identifiers other than Social Security number are used. Am J Public Health 1992;82:1145–1147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Mayer-Davis EJ, Lawrence JM, Dabelea D, et al.; SEARCH for Diabetes in Youth Study . Incidence trends of type 1 and type 2 diabetes among youths, 2002-2012. N Engl J Med 2017;376:1419–1429 [DOI] [PMC free article] [PubMed] [Google Scholar]


