Abstract
Background
Patients who undergo coronary artery bypass graft (CABG) surgery rarely develop global pericardial tamponade due to pericardial adhesions. There are no reports of multiple coronary artery perforations following global pericardial tamponade during percutaneous coronary intervention (PCI) in these patients.
Case summary
A 52-year-old male who underwent CABG surgery developed effort angina pectoris. Coronary angiography demonstrated chronic total occlusion (CTO) of the first diagonal branch with severe stenosis of the second diagonal branch. Because his chest pain did not improve with medical therapy and ischaemia of the left ventricular anterolateral wall was confirmed by myocardial scintigraphy, PCI was performed. The second diagonal branch stenosis was passed anterogradely by a 0.014-inch coronary angioplasty guidewire, while the first diagonal branch CTO was recanalized by side-branch intravascular ultrasonography-guided parallel wiring. After stent deployment, coronary artery perforation at the distal end of the second diagonal branch was detected via contrast injection. We immediately performed intravascular haemostasis, leading to the disappearance of contrast. However, multiple bleeding sites were visualized by angiography at different sites of coronary arteries, including the circumflex artery. Although intravascular haemostasis is a standard procedure, we could not control rebleeding. Despite intensive care, the patient died.
Discussion
Increased tissue pressure due to bleeding possibly led to global pericardial tamponade with multiple coronary artery perforations. We report a rare case of a patient with multiple coronary artery perforations during coronary intervention.
Keywords: Coronary artery disease, Percutaneous coronary intervention, Chronic total occlusion, Complication, Pericardial tamponade, case report
Learning points
This is the first report of multiple coronary artery perforations following global pericardial tamponade during percutaneous coronary intervention in patients with a history of coronary artery bypass graft (CABG).
Coronary perforation sometimes leads to global pericardial tamponade, whereas it is a rare complication in patients with a history of CABG.
Patients with a history of CABG might develop multiple coronary perforations that cause global pericardial tamponade and a lethal outcome.
Introduction
Coronary artery perforation is a serious complication of percutaneous coronary intervention (PCI), requiring urgent care. The rate of coronary artery perforation during PCI is reportedly 0.15–0.3%. Further, 16–20% of patients with coronary artery perforation develop cardiac tamponade and 7–17% of them result in death.1,2 In general, patients who undergo coronary artery bypass graft (CABG) surgery rarely develop global pericardial tamponade due to pericardial adhesions.3,4 Therefore, there are only a few reports on global pericardial tamponade during PCI in patients with a history of CABG surgery.5,6
To the best of our knowledge, this is the first report of a patient with a history of CABG surgery who experienced multiple coronary artery perforations, which led to an extensive pericardial tamponade.
Timeline
| Time | Events |
|---|---|
| Two years before | The patient underwent coronary artery bypass graft surgery. |
| Two months before | The patient developed effort angina pectoris and visited our hospital. |
| One month before | Coronary angiography demonstrated chronic total occlusion of the first diagonal branch (Segment #9) and severe stenosis of the second diagonal branch (Segment #10). |
| Day 1 | |
| 13:40 | Started percutaneous coronary intervention (PCI). |
| 15:00 | Segments #9 and #10 were anterogradely passed. |
| 15:40 | Stent deployment. |
| 16:05 | Detected coronary artery perforation at the distal end of Segment #10. |
| 16:10 | Fat tissue embolization for Segment #10. |
| 16:45 | Detected coronary artery perforation at the distal end of Segment #9. |
| 16:55 | Fat tissue embolization for Segment #9. |
| 17:15 | Multiple coronary perforation were confirmed from Segment #9, Segment #10 and circumflex artery (Cx). |
| 17:30 | Pericardial drainage. |
| 19:20 | Coil embolization for the Cx. |
| 21:00 | Additional bleeding occurred from the Cx graft. |
| 21:10 | Coil embolization for the Cx and Cx graft. |
| 22:20 | Confirmed haemostasis and completed PCI. |
| 22:30 | Admitted into the intensive care unit. |
| Day 2 | |
| 5:30 | Patient died. |
Case presentation
A 52-year-old male who had undergone CABG due to effort angina pectoris (left internal-thoracic artery to S7, free right internal-thoracic artery to S12, and free right radial artery to S4PD) 2 years prior visited our hospital for a recurrence of effort angina pectoris. A pre-PCI echocardiographic movie is shown in Supplementary material online, Video S1. Pertinent laboratory information upon admission was unremarkable. Coronary angiography demonstrated chronic total occlusion (CTO) of the first diagonal branch (S9, Figure 1A, dotted line) and severe stenosis of the second diagonal branch (S10, Figure 1A, arrow). Significant stenoses were not detected in other coronary arteries, including prior bypass grafts (Figure 1B). Ischaemia of the left ventricular anterolateral wall was confirmed by myocardial scintigraphy. His chest pain at effort did not improve with the administration of bisoprolol 5 mg/day, nitroglycerine 25 mg/day, and aspirin 100 mg/day. Percutaneous coronary intervention was performed for Segments #9 and #10 after adding clopidogrel 75 mg/day to his medications. Segment #10 stenosis was anterogradely passed by a 0.014-inch coronary angioplasty guidewire (SION Black, Asahi Intec, Nagoya, Japan), and Segment #9 CTO was recanalized by side-branch intravascular ultrasonography-guided parallel wiring (Conquest Pro 12, Asahi Intec, Nagoya, Japan). After the stent deployment for each lesion, coronary artery perforation was detected by contrast injection; this was a complication from the wire manipulation at the distal end of Segment #10 (Figure 2A, arrows and Video 1). We immediately performed intravascular embolization using fat tissue, and contrast oozing disappeared at once (Figure 2B, arrows). Eventually, another wire perforation was found at the tip of Segment #9 (Figure 3A, arrow and Video 2). This was treated using the same method. However, rebleeding occurred at Segments #9 and #10, and in the left circumflex artery (Cx; Figure 3B, arrows and Video 3). Because the patient instantly experienced cardiac shock caused by the global pericardial tamponade, pericardial drainage was immediately performed. After drainage, bleeding was also observed around the Cx graft (pointed by the arrows in Figure 3C, and Supplementary material online, Video S2). Haemostasis of the whole Cx and its graft was achieved by coil embolization using a microcatheter (C-STOPPER, Piolax Medical Devices, Yokohama, Japan, Figure 4, pointed by a dotted line). In contrast, haemostasis of Segments #9 and #10 occurred spontaneously. This was confirmed by the final angiography (Figure 4 and Supplementary material online, Videos S3 and S4). After PCI, rebleeding occurred. The amount of bleeding gradually increased to 400 mL/min. Unfortunately, the patient died due to cardiac and hypovolemic shock despite 7 h of intensive care and blood transfusions.
Figure 1.
Initial angiogram demonstrating chronic total occlusion of Segment #9 (A, dotted line) and stenosis of Segment #10 (A, arrow). There are no significant stenoses in other native coronary arteries and bypass grafts (B).
Figure 2.
After the stent deployment for each lesion, coronary artery perforation at the distal end of Segment #10 can be seen (A, arrows). Contrast oozing disappeared at once after microcatheter embolization using fat tissue (B, arrows).
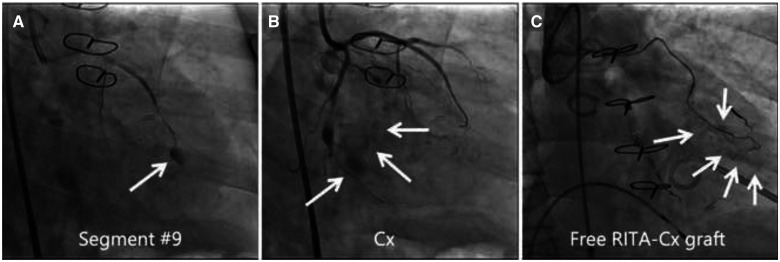
Figure 3.
Another extravasation occurred at the tip of Segment #9 (A, arrow), and in the left circumflex artery (B, arrow). After pericardial drainage, bleeding is also observed around the left circumflex artery graft (C, arrows).
Figure 4.
Haemostasis of the whole left circumflex artery and left circumflex artery graft was achieved by coil embolization (dotted line), whereas haemostasis of Segments #9 and #10 occurred spontaneously, which was confirmed by the final angiography.
Discussion
The rate of coronary artery perforation during PCI is reportedly 0.15–3.0%.1,2 Its severity has been classified into four grades: Ellis Grade I, a crater extending outside of the lumen only and the absence of linear staining angiographically suggestive of a dissection; Ellis Grade II, pericardial or myocardial blush without a ≥ 1-mm exit hole; Ellis Grade III, frank streaming of contrast through a >1-mm exit hole; and Ellis Grade III cavity spilling, contrast jet extravasation into an anatomic cavity (e.g. cardiac chamber or coronary sinus).7 Of the patients with an Ellis Grade III perforation but without cavity spilling, 59% developed cardiac tamponade, 59% underwent covered stent implantation and 11% died during hospitalization.8 However, global pericardial tamponade is a rare complication in patients with a history of CABG surgery.3 Intramural and localized pericardial haematomas have been reported as severe and major complications.5,9,10 Haematomas are sometimes difficult to drain due to the location of the effusion. In addition, there is no percutaneous management option in cases of chamber obstruction. To the best of our knowledge, there are no reports of multiple coronary artery perforations following global pericardial tamponade during PCI in patients with a history of CABG surgery.3–6
Balloon tamponade, fat embolization, coil embolization, and covered stents are the common methods for haemostasis. In general, smaller calibre and distal vessel injury can be locally treated with fat embolization or coil embolization delivered via a microcatheter, whereas larger calibre vessel injury may require implantation of a covered stent.11 Balloon tamponade may be effective in both smaller and larger vessels, and after the bleeding is controlled, appropriate treatment can be given. In the present case, because the distal wire perforations at Segments #9 and #10 were clearly confirmed, local haemostasis using a microcatheter was important. Regarding Cx, the bleeding area was extensive; thus, treatment was required for both the smaller and larger vessels. Covered stent implantation was inadequate due to unclear bleeding points, requiring the use of long-segment coil embolization to achieve haemostasis.
In general, in coronary artery perforation during PCI, outward perforation causes bleeding into the pericardial cavity and inward perforation causes an intramural haematoma. Bleeding into the pericardial cavity is more likely to lead to a cardiac tamponade than an intramural haematoma due to differences in the compression by surrounding tissues. However, there is less free space in the pericardial cavity in patients with a history of CABG surgery because the visceral pericardium adheres to the mediastinum during postoperative healing. Therefore, most cases of pericardial bleeding in patients with a history of CABG surgery are small and resolves spontaneously. There are few case reports on global pericardial tamponade following blood accumulation in the pericardial cavity in patients with a history of CABG surgery.3–6
Next, we speculated the aetiology of multiple coronary artery perforations that were not directly treated in this intervention. Perforation from the vessel lumen was not directly caused by instrumentation in the vessel because no devices were inserted into the Cx or its graft during PCI. Therefore, multiple coronary artery perforations were most likely due to traction injury on the outside of the vessel.
Combining the above considerations, we propose two scenarios for the perforation mechanism in this case. The first mechanism is illustrated in Figure 5A. When the guidewire passed through Segment #10, an outward coronary artery perforation occurred, and a localized pericardial haematoma was formed. Although bleeding reduced due to intravascular haemostasis and adhesion, an increase in intracavity pressure caused a gradual detachment of adhesion. The micro-perforator branch that adhered to the visceral pericardium and mediastinum was disconnected by the detachment of adhesion, which caused additional perforation from non-treated coronary arteries. Finally, it resulted in global pericardial tamponade.
Figure 5.
Hypothesis 1 (A): Outward coronary artery perforation occurred, and a localized pericardial haematoma was formed. An increase in intracavity pressure caused a gradual detachment of adhesion. The micro-perforator branch that adhered to the visceral pericardium and mediastinum was disconnected by the detachment of adhesion, which caused additional perforation from non-treated coronary arteries. Finally, it resulted in global pericardial tamponade. Hypothesis 2 (B): Inward coronary artery perforation occurred, and an intramural haematoma was formed. Myocardial dissection occurred due to an increase in intramyocardial pressure, injuring the perforator branch of non-treated coronary arteries and thereby resulting in an additional coronary artery perforation. Finally, the accumulated blood ruptured from the myocardium toward the adhered pericardial cavity, resulting in global pericardial tamponade.
The second mechanism is illustrated in Figure 5B. When the guidewire passed through Segment #10, an inward coronary artery perforation occurred that formed an intramural haematoma. Although intravascular haemostasis reduced bleeding, slight bleeding persisted. Then, the dissection of myocardial tissue occurred due to an increase in intramyocardial pressure, which injured the perforator branch of non-treated coronary arteries, resulting in an additional coronary artery perforation. Finally, the accumulated blood ruptured from the myocardium toward the adhered pericardial cavity, resulting in global pericardial tamponade.
We recognize that the above mechanisms are hypothetical, and although we discussed with CTO-PCI experts, the exact mechanism of the complications, in this case, could not be identified. If complete haemostasis by coil embolization was performed in the early phase of bleeding, severe global pericardial tamponade might have been avoided.
Coronary artery perforation is a serious complication of PCI that often requires emergent treatment. When coronary artery perforation occurs, it is necessary to manage bleeding appropriately and immediately, even in patients with a history of CABG surgery. This is the first report of a patient with multiple coronary artery perforations and a history of CABG.
Lead author biography

Takehiro Yamada graduated from Gifu University in Japan and has majored in cardiology. Currently, he is working at Cardiovascular Center of Kizawa Memorial Hospital. He is interested in coronary artery disease, peripheral artery disease, heart failure, and arrhythmia. Recently, he has been particularly keen on treatment of peripheral artery disease.
Supplementary material
Supplementary material is available at European Heart Journal—Case Reports online.
Supplementary Material
Acknowledgements
Support from institutional sources only.
Slide sets: A fully edited slide set detailing these cases and suitable for local presentation is available online as Supplementary data.
Consent: The patient died following the procedure and was unable to provide consent for the publication of this manuscript. The authors confirm that written consent for submission and publication of this case report, including images and associated text, has been obtained from the patient's family in line with COPE guidance.
Conflict of interest: None declared.
Funding: None declared.
References
- 1.Shimony A, Zahger D, Van Straten M, Shalev A, Gilutz H, Ilia R. et al. Incidence, risk factors, management and outcomes of coronary artery perforation during percutaneous coronary intervention. Am J Cardiol 2009;104:1674–1677. [DOI] [PubMed] [Google Scholar]
- 2.Javaid A, Buch AN, Satler LF, Kent KM, Suddath WO, Lindsay J Jr. et al. Management and outcomes of coronary artery perforation during percutaneous coronary intervention. Am J Cardiol 2006;98:911–914. [DOI] [PubMed] [Google Scholar]
- 3.Goel PK, Moorthy N.. Successful conservative management of coronary artery rupture: role of post pericardiotomy adhesions as a protective barrier. Cardiovasc Interv Ther 2013;28:131–134. [DOI] [PubMed] [Google Scholar]
- 4.Tajti P, Karmpaliotis D, Alaswad K, Jaffer FA, Yeh RW, Patel M. et al. In-hospital outcomes of chronic total occlusion percutaneous coronary interventions in patients with prior coronary artery bypass graft surgery. Circ Cardiovasc Interv 2019;12:e007338. [DOI] [PubMed] [Google Scholar]
- 5.Karatasakis A, Akhtar YN, Brilakis ES.. Distal coronary perforation in patients with prior coronary artery bypass graft surgery: the importance of early treatment. Cardiovasc Revasc Med 2016;17:412–417. [DOI] [PubMed] [Google Scholar]
- 6.Lowe R, Hammond C, Perry RA.. Prior CABG does not prevent pericardial tamponade following saphenous vein graft perforation associated with angioplasty. Heart 2005;91:1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ellis SG, Ajluni S, Arnold AZ, Popma JJ, Bittl JA, Eigler NL. et al. Increased coronary perforation in the new device era. Incidence, classification, management, and outcome. Circulation 1994;90:2725–2730. [DOI] [PubMed] [Google Scholar]
- 8.Azzalini L, Poletti E, Ayoub M, Ojeda S, Zivelonghi C, La Manna A. et al. Coronary artery perforation during chronic total occlusion percutaneous coronary intervention: epidemiology, mechanisms, management, and outcomes. EuroIntervention 2019;15:e804–e811. [DOI] [PubMed] [Google Scholar]
- 9.Jothidasan A, Attaran S, Hunter D, de Souza AC.. Management of a left atrial intramural hematoma after percutaneous intervention. Ann Thorac Surg 2014;97:2196–2197. [DOI] [PubMed] [Google Scholar]
- 10.Vondran M, Ghazy T, Andrási TB, Graff J, Rastan AJ.. Giant intramural right ventricular hematoma after PCI in a patient with condition after CABG. Thorac Cardiovasc Surg Rep 2020;9:e11–e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.May A, Bhagwandeen R, Collins N.. Contemporary management of coronary artery perforation. Heart Lung Circ 2019;28:e121–e125. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.