Abstract
Background
Complex and high-risk coronary intervention (CHIP-PCI) and PCI in cardiogenic shock complicating acute coronary syndrome (ACS) are increasingly performed under mechanical circulatory support—so-called protected PCI. Among the available options, Impella Cardiac Power (CP) heart pump (Abiomed) is percutaneously inserted over the femoral artery and typically requires a second arterial access to perform PCI, which further enhances the risk of vascular and bleeding complications. The single-access technique allows Impella CP placement and PCI performance through the same vascular access. When a 7 Fr system is desirable, only a long and entirely hydrophilic coated sheath has been previously used, which is not available in Europe.
Case summary
A 85-year-old patient admitted with non ST-elevation - acute coronary syndrome (NSTE-ACS), severely reduced left ventricular function and three-vessel coronary artery disease underwent single-access CHIP-PCI under Impella CP support. After a failed attempt to insert a standard 7 Fr long femoral sheath alongside the Impella catheter, we successfully introduced a 7.5 Fr sheathless guiding catheter and delivered the planned percutaneous treatment with the benefits conferred by a 7 Fr—rather than 6—lumen catheter, without the need for an additional arterial access.
Discussion
This is, to the best of our knowledge, the first case of CHIP-PCI performed under Impella support utilizing the single-access technique with a 7.5 Fr sheathless guiding catheter. Beyond advantages of the single-access technique in sparing time and avoiding vascular complications associated with gaining a second arterial access, the lower outer diameter of the sheathless catheter compared with standard 7 Fr sheaths may allow improved limb perfusion and lower chance of interference with the Impella CP catheter.
Keywords: Mechanical circulatory support, Impella CP, CHIP-PCI, Single-access technique, Protected PCI, Case report
Learning points
An increasing number of complex and high-risk coronary intervention (CHIP-PCI) and PCI in cardiogenic shock complicating acute coronary syndrome are performed under mechanical circulatory support—so-called protected PCI.
Impella placement and PCI performance can be achieved through the same vascular access, avoiding vascular complications associated with gaining a second arterial access.
When a 7 Fr system is desirable to perform CHIP-PCI and the long specific hydrophilic coated sheath is not available, a sheathless guiding catheter can be directly inserted within the Impella sheath alongside the Impella catheter to perform PCI.
Introduction
The use of mechanical circulatory support (MCS) devices during PCI continues to grow in either cardiogenic shock (CS) complicating acute coronary syndromes (ACS) or complex and high-risk coronary intervention (CHIP-PCI). The European Society of Cardiology guidelines1,2 recommend short-term MCS in selected patients with ACS and CS depending on patient age, comorbidities, neurological function and prospects for long-term survival and predicted quality of life (Class IIb; Level of evidence C). The evidence for the use of MCS in CHIP-PCI is also scant. The Impella CP (Abiomed, Danvers, MA) is one of the short-term MCS currently available. Percutaneous Impella CP placement requires femoral access and insertion of a 14 Fr peel-away sheath (Figure 1). A second arterial access is typically obtained to perform PCI. In trials comparing Impella with IABP in either CS3 or CHIP-PCI,4 where a second arterial access was obtained for PCI, the use of Impella was associated with higher rates of bleeding from the vascular access sites and higher rate of limb ischaemia without significant outcome advantages. A single-access technique has been described for both Impella placement and PCI performance,5,6 avoiding the risks of multiple access site complications, especially in patients with peripheral artery disease, and preventing delays in obtaining a second arterial access in urgent settings such as CS.
Figure 1.

Fourteen French Impella CP femoral peel-away sheath.
As previously described,5 the standard single-access technique requires puncturing the superior portion of the haemostatic valve of the Impella sheath (Figures 2 and 3) and inserting a 6 or 7 Fr sheath over a 0.035″ guidewire (Figure 4). The placement of a 7 Fr sheath is only possible with a 45 cm sheath with long (35 cm) hydrophilic coating because of the friction between the sheath itself and the shaft of the Impella CP catheter. However, this hydrophilic coating sheath is not available in Europe. We therefore describe the first case of successful CHIP-PCI with single-access technique utilizing a 7.5 Fr sheathless guiding catheter directly inserted through the haemostatic valve of the Impella CP sheath over a standard 0.035″ guidewire (Figure 5).
Figure 2.
The haemostatic valve of the Impella sheath needs to be pierced in the superior part (as indicated by *) in order to avoid puncturing the Impella catheter.
Figure 3.

Haemostatic valve punctured at 11 o’clock position; puncture at 2 o’clock position is also possible.
Figure 4.

After puncture, a standard J-tipped 0.035″ guidewire is advanced through the needle and needle removed.
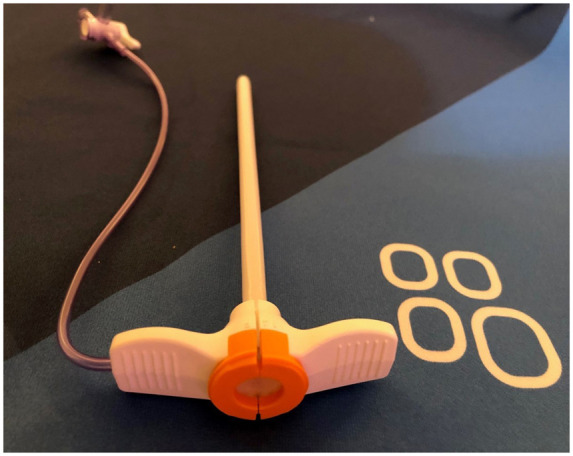
Figure 5.

The sheathless Power Backup 3.5 7.5 Fr is directly inserted over the 0.035″ guide wire parallel to the Impella catheter.
Timeline
| Time | Event |
|---|---|
| Day 1 | The patient was admitted to a peripheral hospital with NSTE-acute coronary syndrome presenting with sustained ventricular tachycardia (VT), which was initially treated with a single DC shock. Echocardiogram showed severely reduced systolic ventricular function |
| Day 2 | He was transferred to our tertiary centre where coronary angiography showed a three-vessel coronary artery disease with chronic total occlusion of right coronary and left circumflex and diseased left anterior descending artery (LAD). The VT episode was linked to ischaemia of the last remaining vessel and revascularization deemed necessary. The case was discussed within the heart team and the patient was considered too high risk for surgery. A decision was made to perform PCI of last remaining vessel under Impella support |
| Day 3 | Impella CP was inserted over the 14 Fr sheath in the right femoral artery after pre-closure with two Perclose. A single-access technique was attempted and a sheathless Power Backup 3.5 7.5 Fr guiding catheter was directly inserted over the 0.035″ guidewire, without friction and mechanical interference with the Impella catheter. Complex PCI to LAD was performed. The Impella device was removed and the arterial access closed percutaneously without complications |
| Day 4 | The patient remained asymptomatic and was transferred to referring hospital |
Case presentation
We present the case of an 85-year-old patient with medical history notable for hypertension, dyslipidaemia, and glucose intolerance, without previous cardiac events, who was admitted overnight to a local hospital complaining of chest pain and palpitation. Initial electrocardiogram (ECG) showed sustained ventricular tachycardia (VT) with haemodynamic instability requiring electrical cardioversion with a single DC shock. Baseline ECG after cardioversion (Supplementary material online, Figure 1) revealed T waves inversion in inferolateral leads and hs-TnT level was elevated with a peak value of 2245 ng/L. A diagnosis of non ST elevation - acute coronary syndrome (NSTE-ACS) was made and the patient was transferred to our tertiary centre for urgent coronary angiography. At arrival the patient was chest pain free, blood pressure was 95/55 mmHg without signs of congestion or hypoperfusion. Trans-radial coronary angiography showed severe three-vessel coronary artery disease with chronic total occlusion of the right coronary and left circumflex arteries and a severely diseased and calcified mid to proximal left anterior descending artery (LAD; last remaining vessel) with proximal stenosis involving the origin of the first diagonal (Video 1). Aorto-bifemoral angiography was also performed showing good patency of the right common but not of the left femoral arteries for potential Impella placement. Echocardiogram showed severely reduced left ventricular function [ejection fraction (EF) 30–35%] with inferior and inferolateral akinesia and anterolateral hypokinesia. After heart team discussion, also considering the good functional status of the patient prior to the event, PCI of the last remaining vessel under Impella support was deemed appropriate.
After pre-closure with 2 Perclose, the 14 Fr sheath was inserted and Impella Cardiac Power (CP) was correctly placed over the aortic valve and set at automatic mode. The superior portion of the haemostatic valve was then punctured at 11 o’clock position as previously described (Figures 2 and 3). A standard 0.035″ J-tipped guidewire was advanced (Figure 4) and an attempt was made to advance a 7 Fr 45 cm long sheath with short hydrophilic coating (Destination, Terumo), which proved unsuccessful due to high degree of friction and initial Impella device displacement. A sheathless Power Backup 3.5 7.5 Fr (ASAHI INTECC) was then directly inserted over the 0.035″ guide and advanced up to the ascending aorta (Figure 5). The advancement of the guiding catheter progressed smoothly, without any interference with the Impella catheter while controlling the position of the pump in the left ventricle under fluoroscopy. The LAD calcified lesions were initially treated with rotational atherectomy using a 1.5 mm burr and pre-dilation with high-pressure non-compliant balloons. Two stents were successfully deployed in mid-proximal LAD and kissing balloon LAD/diagonal and POT (proximal optimization technique) were performed with an acceptable angiographic result (Video 2–3 and Video 1–2 in supplementary material online). The guiding catheter was removed over the guidewire without any back-bleeding from the haemostatic valve. The Impella device was withdrawn, the 14 Fr sheath removed and femoral access closed with closure devices previously positioned. Patient did well after the revascularization without access site complication or new arrhythmic events and remained chest pain free and haemodynamically stable. Only slight haemoglobin drop (Hb at presentation 145 g/L, 124 g/L at discharge) and creatinine rise was observed (103 μmol/L at admission, 104 at discharge). He was transferred to referring hospital the day after the procedure and discharged home 3 days later, after titration of optimal medical therapy. At 2-month follow-up visit, patient was chest pain free and returned to his functional status prior to the event. Furthermore, echocardiogram showed significant improvement of left ventricular function with ejection fraction of 45%.
Discussion
The single-access technique for both Impella placement and PCI allows performing PCI in contexts where obtaining a second arterial access is undesirable such as in emergencies and in patients with obstructive peripheral artery disease. Peripheral angiography performed in our patient showed significant arterial disease involving the left iliac-femoral system, so obtaining a second access to perform CHIP-PCI with a 7 Fr guiding through the left femoral or the radial arteries would have been still possible, but undesirable because of higher risk of vascular complications. The single-access technique has been described using the 14 Fr Impella CP system. The use of the 6 Fr sheath is possible, inserted alongside the Impella catheter. In this particular case, the use of a 7 Fr guiding catheter was preferable because of lesion calcification and the need to have more support from the guiding catheter, potential need of rotational atherectomy with burr larger than 1.5 mm and because of the presence of a bifurcation lesion with potential for double stent PCI. When a 7 Fr guiding catheter is required for CHIP-PCI, only a 45 cm long sheath with a long hydrophilic coating has been successfully used, which remains unavailable in Europe. We attempted in this and previous cases the insertion of a long 7 Fr sheath alongside the Impella catheter but we had to abort the attempt due to high friction and initial displacement of the device in the left ventricle. To the best of our knowledge, this is the first case of a single-access technique utilizing a 7.5 Fr sheathless guiding catheter directly inserted through the haemostatic valve of the Impella sheath during CHIP-PCI. The 7.5 Fr guiding catheter was easily advanced through the Impella sheath without interfering with the Impella catheter, allowing the use of a large-bore guiding catheter and obviating to the unavailability of 7 Fr long hydrophilic sheaths in EU. A potential advantage of using the single-access technique with a sheathless catheter is the lower outer diameter of the guiding catheter comparing with 7 Fr sheaths. The sheathless Power Backup 3.5 7.5 Fr has an outer diameter of 2.49 mm whereas the corresponding figure of 7 Fr hydrophilic sheath 3.1 mm. This carries potential for improved blood perfusion to lower limb especially in patients with peripheral artery disease and during lengthy coronary procedures.
Lead author biography

Marco Araco is an Italian physician who currently works as attending interventional cardiologist at Fondazione Cardiocentro Ticino in Lugano, Switzerland. After general medical training in Italy, USA, and UK, he completed the general cardiology training in Italy and UK and the interventional curriculum in Lugano, where he works as attending physician from 3 years. Dr Araco’s main interest is on coronary and structural interventions; he is actively involved in complex PCI procedures, TAVI planning and performance, and teaching residents and medical students in the catheterization laboratory.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The authors confirm that written consent for submission and publication of this case report including images and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: M.V. reports personal fees from AstraZeneca, Alvimedica/ CID, Abbott Vascular, Daiichi Sankyo, Bayer, CoreFlow, Idorsia Pharmaceuticals Ltd, Universität Basel/Dept. Klinische Forschung, Vifor, Bristol Myers Squibb SA, Biotronik, Boston Scientific, Medtronic, Vesalio, Novartis, Chiesi, and PhaseBio, and grants and personal fees from Terumo, outside the submitted work. The other authors have no conflicts of interest to declare.
Funding: None declared.
Supplementary Material
References
- 1.Collet JP, Thiele H, Barbato E, Barthélémy O, Bauersachs J, Bhatt DL. et al. ; ESC Scientific Document Group. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J 2021;42:1289–1367. [DOI] [PubMed] [Google Scholar]
- 2.Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U. et al. ; ESC Scientific Document Group. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J 2019;40:87–165.30165437 [Google Scholar]
- 3.Wernly B, Seelmaier C, Leistner D, Stähli BE, Pretsch I, Lichtenauer M. et al. Mechanical circulatory support with Impella versus intra-aortic balloon pump or medical treatment in cardiogenic shock—a critical appraisal of current data. Clin Res Cardiol 2019;108:1249–1257. [DOI] [PubMed] [Google Scholar]
- 4.O'Neill WW, Kleiman NS, Moses J, Henriques JP, Dixon S, Massaro J. et al. A prospective, randomized clinical trial of hemodynamic support with Impella 2.5 versus intra-aortic balloon pump in patients undergoing high-risk percutaneous coronary intervention: the PROTECT II study. Circulation 2012;126:1717–1727. [DOI] [PubMed] [Google Scholar]
- 5.Wollmuth J, Korngold E, Croce K, Pinto DS.. The single-access for Hi-risk PCI (SHiP) technique. Catheter Cardiovasc Interv 2020;96:114–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kumar K, Reddy S, Acharya D, Lotun K.. Novel technique of performing multivessel PCI through an Impella sheath. Catheter Cardiovasc Interv 2020;96:117–120. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


