Introduction
MPNs are a group of clonal hematologic malignancies morphologically characterized by expansion of terminally differentiated myeloid cells (white blood cells erythrocytes and platelets).1 There are three “classical” Philadelphia negative MPNs (hereafter referred to as MPNs): polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (PMF). In addition, a prefibrotic form of myelofibrosis (pre-PMF) is increasingly recognized as a distinct member of the MPNs. Moreover, there are a group of patients that share many features of an MPN that do not meet diagnostic criteria for PMF, ET and PV and they fall into a grab bag group termed MPNs-unclassifiable (MPN-U). MPNs are often discussed together as they share similar pathobiologic and clinical features. In addition, patients with ET and PV can progress to myelofibrosis (MF), termed post-ET MF and post-PV MF, respectively.2 Other rarer diseases classified as MPNs by the World Health Organization (WHO) include chronic neutrophilic leukemia (CNL), mastocytosis, and chronic eosinophilic leukemia but will not be discussed here.3
Initially CML was included as a classical MPN, in addition to paroxysmal nocturnal hemoglobinuria. However, CML was found to be associated with a specific cytogenetic abnormality - a translocation between chromosome 9 and 22 resulting in the generation of the BCR/ABL fusion gene which possessed tyrosine kinase activity.4 CML patients each inevitably progressed to a universally fatal form of acute leukemia termed CML-blast crisis which was refractory to chemotherapy. This progression of CML to CML blast phase was associated with the progressive acquisition of new cytogenetic abnormalities which provided evidence of the multistep pathogenesis of a hematological malignancy.5 During the 1970’s, 1980’s and 1990’s CML patients could only be cured in the chronic phase of their disease by allogeneic stem cell transplantation, confirming that CML was a stem cell disease.6 In fact, during this period CML was the most frequent indication for allogeneic stem cell transplantation.7 However, this picture dramatically changed in the 1990’s with the discovery of specific tyrosine kinase inhibitors which inhibited the BCR/ABL fusion protein and led to the depletion of CML progenitor and stem cells.8 This first-in-class tyrosine kinase inhibitor, imatinib, was approved by the Federal Drug Administration in 2001 and changed the outcomes of virtually all CML patients.9 The discovery of imatinib was a result of synergistic interactions between academic scientists and clinicians with the pharmaceutical industry focusing on discovery science and translating these findings into the development of strategies to improve the lives of cancer patients. The other Philadelphia chromosome negative MPNs, including ET, PV and PMF, share many clinical characteristics with CML. Although their clinical courses are frequently more indolent than CML, their origins have proven to be more complex which has hampered success in developing therapeutic agents which share the clinical efficacy of imatinib.
Clinical manifestations across MPNs include panmyelosis (marrow hypercellularity with multilineage involvement), splenomegaly, constitutional symptoms, and a propensity towards thrombosis or bleeding. An overactive JAK-STAT pathway is a unifying pathobiologic feature of all the MPNs.10 Thrombotic complications and disease progression are the most serious complications of MPNs and often the most common causes of death in patients with MPNs.11 Current treatment approaches involves cytoreductive therapy, aspirin, and JAK1/2 inhibitors, such as ruxolitinib and fedratinib. While these agents have demonstrated success in terms of symptom control and reduction in spleen volume, they do not necessarily halt disease progression.12–14 At present, the only curative therapy for patients with MPNs is allogeneic stem cell transplantation which is offered to a limited proportion of MF patients with advanced risk disease and without prohibitive comorbidities.15 Thus, there is considerable interest in the development of novel agents for patients with MPNs, particularly MF.16, 17 These new therapeutic strategies will be detailed in this series by Dr. John Mascarenhas in his article entitled “Current clinical investigations in myelofibrosis.”
Epidemiologically, the MPNs are considered to be a rare disease. The incidence of PV and ET is around 1–2 per 100,000 in the United States, while the incidence of PMF is 0.3 per 100,000.18 Although typically thought of as a disease of older adults, with a median age of around 60 years old, MPNs can also arise in young adults and children.19, 20 MPNs are generally more common in males as compared to females, with the notable exception of ET which is more prevalent among females.21 Drs. Amer Zeiden and Nikolai Podoltsev will delve into more specifics of the epidemiology of MPNs in their article “Epidemiology of myeloproliferative neoplasms.”
In this introductory article on the series, we will first detail the history of MPNs including original observations and relevant scientific and clinical figures in the early conceptual development. To set the stage for the remainder of this series, we will detail diagnostic criteria as defined by the WHO. We will then briefly describe the pathophysiology, concentrating on unifying themes that run across each of the MPNs. Finally, we will describe complications of MPNs including thrombosis and progression.
History
The dawn of hematology occurred in the mid 1650s. The refinement of the light microscope in the 1600s allowed Dutch biologist Jan Swammerdam to visualize the red blood cells (RBCs) of a frog in 1658.22 Unaware of his work, Antonie van Leeuwenhoek also visualized the RBCs (from blood pricked from his thumb) and estimated their size as “25,000 times smaller than a fine grain of sand.”23 White blood cells (WBCs) were first described in 1749 by Joseph Lieutaud, calling them globuli albicantes.24 Platelets were the last blood cell lineage to be identified by Alfred François Donné in 1842.25 The first MPN to be described was CML, which was detailed in a 1845 case report by the English pathologist John Hughes Bennett.26 It wasn’t until 1879 that cases of myelofibrosis were reported by Gustav Heuck, a German surgeon, who detailed two young patients with massive splenomegaly, leukoerythroblastosis, and bone marrow fibrosis, differentiating it from CML.27 The first description of PV came in 1882, when the French physician Louis Henri Vaquez described a 40-year old man with chronic vascular congestion with marked erythrocytosis. On autopsy, no cardiac abnormalities were noted but he did observe splenomegaly and hepatomegaly. Vaquez concluded that this disease was caused by hematopoietic hyperactivity, a remarkable conclusion considering the time.28 This description was further defined by William Osler 1903 when he described four cases of “chronic cyanosis, with polycythemia and enlarged spleen: a new clinical entity.”29 ET was the last MPN to be formally described. Two Austrian pathologists Emil Epstein and Alfred Goedel, described a patient with extreme thrombocytosis (“more than three times normal values”) associated with megakaryocytic hyperplasia. This patient had recurrent mucocontaenous bleeding.30
One of the most important figures responsible for developing the concept that the MPNs are an interrelated group of disorders was William Dameshek. In 1951, he hypothesized that trilineage myeloproliferation unified CML PMF, PV, and ET and coined this group of diseases as “myeloproliferative disorders.” He considered these disease to be clinically and biologically related and “perhaps due to a hitherto undiscovered stimulus.”31 A major step in understanding the underlying etiology of MPNs was made by Philip Fialkow, who studied polymorphisms in the X-linked glucose-6-phosphate dehydrogenase locus to confirm the clonal nature of PV,32 ET,33 and PMF.34 Although many hematologists had debated whether these myeloproliferative disorders represented blood cancers, the seminal investigations of Fialkow and his talented group of collaborators indicated that these disorders were clonal in origin and involved all types of myeloid cells, supplying the first indications that they represented hematological malignancies that originated at the level of the hematopoietic stem cell. While our pathobiologic understanding of MPNs progressed, methodologic rigor was not applied to therapeutic efforts. Louis Wasserman, an American hematologist from Mount Sinai Hospital formed the Polycythemia Vera Study Group (PSVG) in 1967. This group formalized clinical investigation of PV and included seminal multi-institutional, international studies establishing the leukemogenicity of chlorambucil and intravenous P-32,35 providing early evidence of hydroxyurea efficacy in reducing thrombosis,36 and describing the dangers of high dose antiplatelet therapy.37 The next paradigm shift in the MPN field occurred in 2005 when four independent laboratories identified the gain-of-function JAK2V617F mutation that is possessed by virtually all patients with PV and 50% of patients with ET and MF.38–41 There have been numerous other important discoveries over the last 15 years. Subsequently driver mutations in the thrombopoietin receptor (MPL) and chaperone protein calreticulin (CALR) were reported in ET and MF patients and a mutation in exon 12 of JAK2 rather than exon 14 as occurs in JAK2V617F was shown to be associated with a form of PV characterized by isolated erythrocytosis. As this series will outline, our understanding of MPNs has deepened dramatically since the days of Dameshek. However, observations made by these pioneers in the field (Figure 1) are still fundamental to our current understanding of the pathogenesis and treatment of MPNs.
Figure 1.
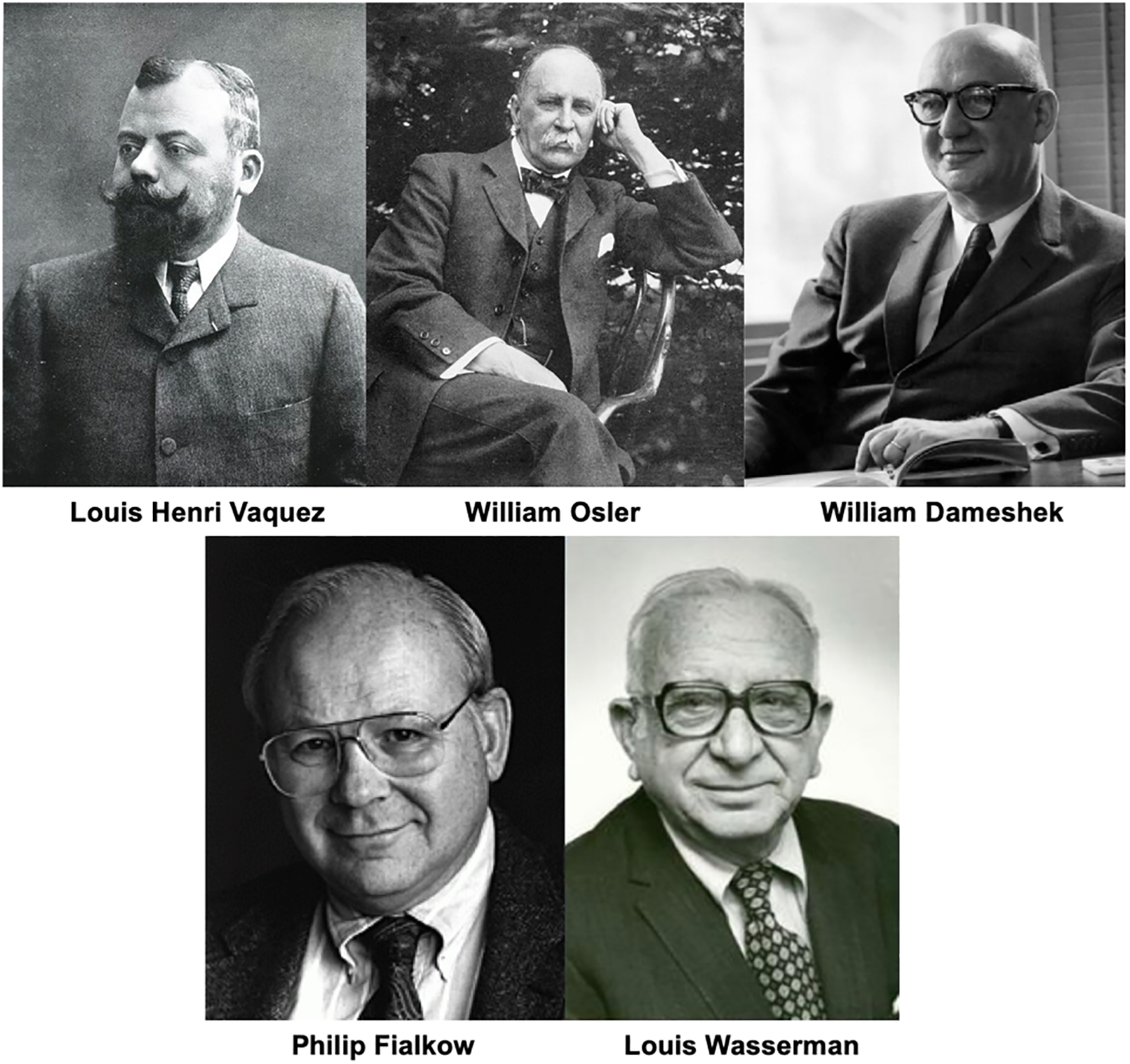
Major clinical investigators responsible for early diagnostic and therapeutic advances in myeloproliferative neoplasms. Louis Henri Vaquez was the first to describe polycythemia vera, which was later expanded by William Osler. William Dameshek described pathologic links and coined the term “myeloproliferative disorders.” Philip Fialkow identified myeloproliferative neoplasms as a stem cell disease and Louis Wasserman formed the Polycythemia Vera Study Group, the first dedicated organization to study therapies in myeloproliferative neoplasms.
Diagnostic criteria
The WHO has proposed the most widely used diagnostic criteria for MPNs. The 2016 revision of these criteria for PV, ET and PMF are listed in Table 1, 2, and 3, respectively.3 Megakaryocytic hyperplasia and atypia is one of the cardinal histopathological features of each of the MPNs. The cause and consequences of this megakaryocytic hyperplasia In the MPNs will be discussed in the paper by Dr. John Crispino, Dr. Anna Rita Franco Migliaccio and Dr. Johanna Melo-Cardenas. The WHO criteria are far from perfect and numerous investigators debate their value. They have, however, proven useful in identifying patients with a particular MPN for entry in clinical trials but in everyday practice they should be used as guides to diagnosis rather than rigid criteria.
Table 1.
Diagnostic Criteria for Polycythemia Vera3
| Major criteria |
| 1. Hemoglobin >16.5 g/dL in men, Hemoglobin >16.0 g/dL in women |
| or, |
| Hematocrit >49% in men, Hematocrit >48% in women |
| or, |
| increased red cell mass (RCM), more than 25% above mean normal predicted value. |
| 2. BM biopsy showing hypercellularity for age with trilineage growth (panmyelosis) including prominent erythroid, granulocytic, and megakaryocytic proliferation with pleomorphic, mature megakaryocytes (differences in size) |
| 3. Presence of JAK2V617F or JAK2 exon 12 mutation |
| Minor criterion |
| Subnormal serum erythropoietin level |
| Diagnosis of PV requires meeting either all 3 major criteria, or the first 2 major criteria and the minor criterion† |
Criterion number 2 (BM biopsy) may not be required in cases with sustained absolute erythrocytosis: hemoglobin levels >18.5 g/dL in men (hematocrit, 55.5%) or >16.5 g/dL in women (hematocrit, 49.5%) if major criterion 3 and the minor criterion are present. However, initial myelofibrosis (present in up to 20% of patients) can only be detected by performing a BM biopsy; this finding may predict a more rapid progression to overt myelofibrosis (post-PV MF).
Table 2.
Diagnostic Criteria for Essential Thrombocythemia3
| Major criteria |
| 1. Platelet count ≥450 × 109/L |
| 2. BM biopsy showing proliferation mainly of the megakaryocyte lineage with increased numbers of enlarged, mature megakaryocytes with hyperlobulated nuclei. No significant increase or left shift in neutrophil granulopoiesis or erythropoiesis and very rarely minor (grade 1) increase in reticulin fibers |
| 3. Not meeting WHO criteria for BCR-ABL1+ CML, PV, PMF, myelodysplastic syndromes, or other myeloid neoplasms |
| 4. Presence of JAK2, CALR, or MPL mutation |
| Minor criterion |
| Presence of a clonal marker or absence of evidence for reactive thrombocytosis |
| Diagnosis of ET requires meeting all 4 major criteria or the first 3 major criteria and the minor criterion |
Table 3.
Diagnostic Criteria for Primary Myelofibrosis3
| Major criteria |
| 1. Presence of megakaryocytic proliferation and atypia, accompanied by either reticulin and/or collagen fibrosis grades 2 or 3* |
| 2. Not meeting WHO criteria for ET, PV, BCR-ABL1+ CML, myelodysplastic syndromes, or other myeloid neoplasms |
| 3. Presence of JAK2, CALR, or MPL mutation or in the absence of these mutations, presence of another clonal marker,† or absence of reactive myelofibrosis‡ |
| Minor criteria |
| Presence of at least 1 of the following, confirmed in 2 consecutive determinations: |
| a. Anemia not attributed to a comorbid condition |
| b. Leukocytosis ≥11 × 109/L |
| c. Palpable splenomegaly |
| d. LDH increased to above upper normal limit of institutional reference range |
| e. Leukoerythroblastosis |
| Diagnosis of overt PMF requires meeting all 3 major criteria, and at least 1 minor criterion |
In the absence of any of the 3 major clonal mutations, the search for the most frequent accompanying mutations (eg, ASXL1, EZH2, TET2, IDH1/IDH2, SRSF2, SF3B1) are of help in determining the clonal nature of the disease.
BM fibrosis secondary to infection, autoimmune disorder, or other chronic inflammatory conditions, hairy cell leukemia or other lymphoid neoplasm, metastatic malignancy, or toxic (chronic) myelopathies.
PV is suspected in a patient with an elevated hematocrit, however a full evaluation is required. Polycythemia must be classified as relative or absolute. Relative polycythemia occurs in the setting of an absolute increase in hematocrit without an increase in red cell mass. This is typically a spurious finding caused by a contraction in plasma volume in the setting of protracted vomiting or diarrhea, plasma loss from an external burn, insensible fluid loss in the setting of fever, or Gaisböck syndrome, a benign condition classically found in middle-age, obese men who smoke.42, 43 Absolute polycythemia is characterized by an increase in red cell mass and can be due to primary or secondary causes. Causes of secondary erythrocytosis include hypoxemia as a result of pulmonary or cardiac disease, erythropoietin-secreting tumors (e.g. renal cell carcinoma), and drug-induced such as erythropoiesis stimulating agents, androgens and corticosteroids.44 There are congenital polycythemias that result from the mutations in the hemoglobin genes that lead to an increased in oxygen affinity with resultant compensatory erythrocytosis.45 Other causes of congenital polycythemias include 2,3-BPG deficiency, methemoglobinemia or genetic disorders of oxygen sensing including Chuvash polycythemia (caused by a mutation in the Van Hippel Landau VHL gene), gain of function mutations in the HIF-2 gene and prolyl hydroxylases (PHDs) mutations.46–49 These mutations in the oxygen sensing pathway each ultimately result in increased production of erythropoietin which results in lifelong erythrocytosis. Chuvash polycythemia has been reported more frequently in Asia, Chuvashia and the island of Ischia in Italy and is associated with an abbreviated life span.50, 51
PV encompasses the vast majority of primary polycythemias, however there are familial causes of erythrocytosis that result from activating gene mutations of the erythropoietin receptor.45 The JAK2V617F mutation is the genetic sine qua non of the diagnosis of PV, being present in about 98% of patients.52 In a patient with a subnormal EPO and absence of JAK2V617F, evaluation for the exon 12 mutation JAK2 identifies another variant of PV.53 A bone marrow biopsy may not be necessary to make a diagnosis of PV in cases of extreme erythrocytosis (>18.5 g/dL in men or >16.5 g/dL in women) when a JAK2 mutation is identified (Table 1).3 Many investigators, however, argue that red cell mass studies are necessary and hematocrit/hemoglobin values are at best imperfect parameters for documenting the presence of erythrocytosis.54 Unfortunately, red cell mass measurements are rarely available at most institutions throughout the world.
Thrombocytosis is often secondary to an acute inflammatory condition and termed reactive thrombocytosis, which is often transient and resolves after resolution of the precipitating process. Common causes of reactive thrombocytosis include infection, surgery, inflammatory conditions, and malignancy.55 Even with high platelet counts, thrombosis is rare in patients with reactive forms of thrombocytosis.56 There are also rare familial forms of thrombocytosis. Different mutant TPO alleles have been described in families with an autosomal dominant form of thombocytosis.57 Each of these mutations act by augmenting the efficiency of translation of the TPO mRNA.57, 58 The rate of thrombotic and hemorrhagic complications in family members from two different kindreds has been reported to be comparable with that of patients with sporadic ET.59 Most commonly, persistent thrombocytosis absent a prolonged underlying condition identified above raises the concern for an underlying MPN. CML must always be ruled out in patients with isolated thrombocytosis since this presentation is not unusual. Diagnostic evaluation of suspected ET includes evaluation of a driver mutation, specifically JAK2, CALR, and MPL, as well as a polymerase chain reaction (PCR) testing for BCR/ABL (Table 2). However, 10–15% of ET patients may be negative for these three driver mutations and are classified as so called “triple negative” ET.60 A minority of these patients may have a non-canonical mutations in JAK2 or MPL detected with whole exome sequencing.61 A bone marrow biopsy is essential for establishing a diagnosis of ET as it can distinguish ET from pre-PMF.3
The diagnosis of PMF requires exclusion of other MPNs, secondary forms of marrow fibrosis (such as metastatic cancer to the marrow, tuberculosis and fungal diseases, hairy cell leukemia, autoimmune etiologies) myelodysplastic syndrome (MDS), and CML (Table 3). A bone marrow biopsy is essential as grade 2–3 fibrosis is a requisite for the diagnosis, which is accompanied by megakaryocytic atypia and proliferation. Similar to ET, mutational assessment for a driver mutation is also important, however 8–10% of patients will have “triple negative” PMF which is associated with a poor prognosis.60 In addition, other somatic mutations are frequently present in patients with PMF including ASXL1, TET2, SRSF2, EZH2, and IDH1/IDH2, among others.62 Dr. Sara Christina Meyer will explore these topics further in her article entitled “Genetics of myeloproliferative neoplasms.”
In 2016, the WHO defined a new entity called pre-PMF pathologically characterized by megakaryocytic atypia without reticulin fibrosis greater than grade 1 and a hypercelluar marrow (Table 4). Although this diagnostic entity was only recently incorporated into WHO diagnostic criteria, pre-PMF was first described as a distinct clinical entity in 1976 and was formally introduced in the previous 2001 and 2008 WHO diagnostic criteria.63–65 Clinically, pre-PMF is often associated with isolated thrombocytosis and is often misdiagnosed as ET. In fact, a review of over 1000 cases of 2008 WHO diagnosed ET demonstrated that nearly one in five meets criteria for pre-PMF instead of ET.66 The pathologic considerations of MF will be discussed in this series by Dr. Mohamed Salama, including the diagnosis of pre-PMF. Although both disorders are characterized by an increased risk of developing thrombotic events. The distinction between ET and pre-PMF is key as pre-PMF carries a significantly elevated risk of transformation to leukemia and death.66
Table 4.
Diagnostic criteria for prePMF3
| Major criteria |
| 1. Megakaryocytic proliferation and atypia, without reticulin fibrosis >grade 1*, accompanied by increased age-adjusted BM cellularity, granulocytic proliferation, and often decreased erythropoiesis |
| 2. Not meeting the WHO criteria for BCR-ABL1+ CML, PV, ET, myelodysplastic syndromes, or other myeloid neoplasms |
| 3. Presence of JAK2, CALR, or MPL mutation or in the absence of these mutations, presence of another clonal marker,† or absence of minor reactive BM reticulin fibrosis‡ |
| Minor criteria |
| Presence of at least 1 of the following, confirmed in 2 consecutive determinations: |
| a. Anemia not attributed to a comorbid condition |
| b. Leukocytosis ≥11 × 109/L |
| c. Palpable splenomegaly |
| d. LDH increased to above upper normal limit of institutional reference range |
| Diagnosis of prePMF requires meeting all 3 major criteria, and at least 1 minor criterion |
In the absence of any of the 3 major clonal mutations, the search for the most frequent accompanying mutations (eg, ASXL1, EZH2, TET2, IDH1/IDH2, SRSF2, SF3B1) are of help in determining the clonal nature of the disease.
Minor (grade 1) reticulin fibrosis secondary to infection, autoimmune disorder or other chronic inflammatory conditions, hairy cell leukemia or other lymphoid neoplasm, metastatic malignancy, or toxic (chronic) myelopathies
Survival among is longest with ET patients among the MPNs, with an estimated median survival of around 20 years.60 Patients with PV have a shorter estimated survival as compared with ET, with one study reporting a median overall survival 14.1 years after diagnosis.52 Patients with pre-PMF have a median survival of approximately 14.7 years based on a large European series, however survival is significant shorter in patients with adverse karyotypic or mutational profiles.67 Overt MF portends the worse prognosis among the MPNs, with a median survival of 3.1 to 5.8 years.67, 68 However the survival of all MPNs are highly dependent on many patient and disease specific factors.
Other WHO recognized MPNs, including CNL, mastocytosis, and chronic eosinophilic leukemia and MPNs not otherwise specified will not be discussed in this series. However, a group of disorders which have characteristics of both myelodysplastic syndrome (MDS) and MPNs, called MDS/MPN overlap syndrome will be detailed by Dr. Andrew Kuykendall, Dr. Rami Komrokji, and Dr. Franco Castillo Tokumori in their article “MDS/MPN overlap syndromes.” These disorders include chronic myelomonocytic leukemia (CMML), juvenile myelomonocytic leukemia (JMML) and atypical chronic myeloid leukemia (aCML).
Pathogenesis
The pathogenesis of MPNs are multifactorial and incompletely understood. However, substantial progress has been made over the last several decades towards understanding the biologic underpinnings of MPNs. It is important to recognize that all MPNs originate at the level of a pluripotent hematopoietic stem cell (HSC).69, 70 In murine models, even a single cell carrying the JAK2V617F mutation can initiate the MPN phenotype.71 However there is considerable complexities in MPN pathogenies as it relates to the stem cell microenvironment. Interactions between HSCs and nonhematopoietic marrow cells in MF are responsible for marrow fibrosis, increased microvascular density and production of inflammatory cytokines.72 In particular, transforming growth factor beta (TGF-β) is a potent stimulator of fibroblast growth, which are not part of the malignant clone.73 However monocytes that belong to the malignant clone can acquire the properties that allow resemble fibroblasts and are termed fibrocytes. These fibrocytes along with fibroblast contribute to marrow fibrosis in MF.74 Dr. Angela Fleischman will expand upon this topic in her article entitled “The microenvironment in myeloproliferative neoplasms.”
A key pathogenetic event in all MPNs is constitutive activation of the JAK/STAT pathway. Seminal to this understanding was the identification of mutations JAK2 in 98% of patients with PV, and 50–60% of patients with ET and PMF.38–41 Additional somatic mutations, such as the thrombopoietin receptor MPL in JAK2V617F-negative MPN patients suggest common genetic mutations resulting in overactivation of the JAK-STAT pathway.75 In addition, a small subset of JAK2V617F negative polycythemic patients harbor a mutation in LNK, which inhibits JAK2 phosphorylation and serves as a negative regulator of MPL signaling.76, 77 The CALR mutation, which is generally exclusive to JAK2 and MPL mutations, creates a mutant protein that directly binds the thrombopoietin receptor (MPL) leading to constitutive activation of downstream signaling molecules in the JAK/STAT pathway.78, 79 The central role of the JAK-STAT pathway in the pathogenesis of MPNs was confirmed by a seminal study by Rampal et al using gene expression profiling. JAK/STAT target genes were upregulated, independent of JAK2 mutational status or clinical phenotype. Even “triple negative” MPN cases were characterized by upregulation of this pathway affirming the central role of hyperactive JAK/STAT pathway.10 This dependency on upregulated JAK/STAT signaling accounts for the success of JAK2 inhibitors as a cornerstone therapy in patients with MF regardless of driver mutation status.
Additional somatic mutations appear frequently occur in patients with MPNs, especially those involved in epigenetic regulation. In a study of 197 MPN patients, after JAK2 and CALR, the most commonly mutated genes were TET2, ASXL1, DNMT3A, and EZH2.80 These mutations are likely involved in disease initiation as well as evolution.80, 81 Further details of epigenetic mechanisms of MF are including in the article by Dr. Ross Levine entitled “Epigenetics of myelofibrosis.”
It has long been recognized that inflammation is an important contributor to neoplastic development, sometimes referred to as “oncoinflammation.”82 In MPNs, there is biochemical, molecular, clinical, and epidemiologic evidence that links overactive inflammation and MPN development. Patients with MPNs have persistently elevated C-reactive protein, an acute phase reactant, and the degree of elevation is predictive of leukemic transforomation.83, 84 Several genes involved in immune regulation and inflammation are upregulated, particularly interferon-related genes such as interferon-inducible (IFI) gene IFI27.85 Upregulation of IFI27 is step wise, with higher levels observed in MF as compared to ET or PV, suggesting a role of inflammation in disease progression.86 Fischer and colleagues showed that the increased production of cytokines in MF patients, including tumor necrosis factor, were driven partly by each of the NFκB, MAP kinase, and JAK-STAT pathways.87 Their observations indicated that an intact NFκB pathway is necessary for maximal production of these cytokines in MF. Interestingly, epidemiologic evidence also supports a link between inflammation and development of an MPN. Patients with an autoimmune disorder, including Crohn’s disease, polyarthritis rheumatica, giant cell arthritis, carry an increased risk for subsequent development of an MPN.88 Tobacco smoking has also been consistently associated with an increased risk of MPN development.89
Inflammatory cytokines are responsible for many of the clinical features of myelofibrosis. TGF-β has been implicated in angiogenesis, tumor growth, collagen fibrosis in a number of tumor types. In MF, TGF-β is more abundantly produced as compared with other fibrogenic cytokines, such as platelet-derived growth factor (PDGF), and fibroblast growth factor-basic (FGF-b).90 Cytokine overexpression is also thought to be related to constitutive mobilization of CD34+ cells into the peripheral blood of MF patients.91 In addition, splenomegaly and constitutional symptoms have been correlated with and hepatocyte growth factor (HGF) and interleukin (IL)-6, respectively. In addition, IL-8, IL-2R, IL-12, and IL-15 have been shown to be independently prognostic in patients with MF.92 Dr. Adam Mead will expand on these topics in his article “Novel technologies for understanding myeloproliferative neoplasm biology.”
Complications
The major complications experienced by patients with MPNs include thrombosis, bleeding, and disease progression of disease to overt phases of MF or MPN-BP. In PV and ET, the primary contributor of morbidity and mortality is thrombosis, which can be either arterial or venous. In a large population based Swedish study, the hazard ratio (HR) for arterial thrombosis 3 months, 1 year, and 5 years after diagnosis was 3.0, 2.0, and 1.5, respectively, as compared with the general population. The corresponding HRs for venous thrombosis was 9.7, 4.7, and 3.2, suggesting a significantly increased rate of thrombosis compared to patients without MPNs, particularly in the few months following diagnosis.93 Another hallmark of MPN-related thrombosis is the development of clots in atypical locations, particularly the splanchnic bed.94, 95 Thrombosis of the hepatic vein (Budd Chiari syndrome) and the portal vein are particularly prevalent and may be related to endothelial cells harboring the endothelial cells and increase P-selectin expression.96, 97 Erythromelalgia is another microvascular disorder caused by platelet microthrombi and activation which is ameliorated by aspirin.98
Bleeding is also a concern for MPN patients, especially those with ET and PMF. In a meta-analysis, bleeding complications occurred in 8.9% of patients with MF, 7.3% in ET, and 6.9% in PV, with gastrointestinal and mucocutaneous locations being the most common sites.99 Thrombocytosis is among the most important risk factors for bleeding, as demonstrated in a post-hoc analysis of the PT1 trial.100 In particular, significant elevations in platelets can lead to acquired von Willebrand syndrome.101 Dr. Andrew I. Schafer will describe these complications further in his article entitled “Thrombotic and hemorrhagic complications of myeloproliferative neoplasms.”
Progression from a proliferative disease (i.e. ET or PV) to a fibrotic disease (i.e. PET-MF or PPV-MF) and MPN-BP is a primary concern for clinicians and patients alike.11 The risk of progression varies depending on series and risk factors, such as age, mutational status, and other clinical factors. In one series, progression rate from ET and PV to PET-MF and PPV-MF was 9.2–10.3% and 12.5–21%, respectively.60 Transformation to MPN-BP is highest with PMF, with a 10-year risk of 10–20%, followed by PV (2–4%) and ET (1–2%).102 Many clinical, laboratory, cytogenetic, and molecular risk factors have been identified. These factors have been incorporated into multiple risk scores.103–105 Unlike de novo AML, MPN-BP is rarely associated with mutations in NPM1 or FLT3, highlighting its unique biology as compared to other forms of secondary leukemia.106 Dr. Raajit Rampal will delve further into leukemic transformation in his article entitled “Accelerated and blast phase myeloproliferative neoplasms.”
Infections are more common in MPN patients as compared with the general population and remains one of the primary contributors towards mortality in patients with MPNs.107 Although the risk is highest in patients with PMF, there is still a significant increase in the risk of infection with ET and PV.108 There is also growing evidence, albeit controversial, that ruxolitinib may increase the risk of infection in patients with MPNs.109, 110 In addition, patients with MPNs are at an increased risk of developing second primary malignancies, in particular skin cancer.111 The reason for this observation is not known, but has been hypothesized to be related to the chronic inflammatory milieu in patients with MPNs.112 A recent provocative study suggested that ruxolitinib was associated with the development of B-cell lymphomas.113 However this association has not been confirmed in subsequent studies.114, 115
Summary
MPNs represent a biologically related group of hematologic disorders with significant clinical consequences. Early work from pioneering hematologists established the relationships between this group of disorders and led to early understanding of its pathogenesis. Importantly, the 2005 identification of the JAK2V617F, which is present in the majority of patients with MPNs), has established the central role of the JAK-STAT pathway in MPN biology. Inflammation is also a major contributor to disease initiation and progression. Further studies are needed to identify additional pathogenic mechanisms, including the role of epigenetics, additional signaling pathways, and megakaryocyte abnormalities.
Despite the progress in our pathobiologic understanding of MPNs, significant advancements in therapeutically impacting the natural history of disease remains elusive. For patients with proliferative disease (ET and PV), cytoreduction is the mainstay of therapy. However, it is not clear if this intervention significantly impacts the thrombotic burden in ET and PV. In addition, the impact on progression of disease to MF or MPN-BP is lacking. Given the chronic nature of MPNs and the relatively low event rate of disease transformation and thrombosis, which are key clinical outcomes, the performance of clinical trials in MPNs are extremely challenging as Dr. Amylou Dueck will outline in her article “Advancing effective clinical trial designs for MF.” Despite significant improvement in symptom burden and spleen size with JAK inhibitor treatment for MF, these therapies are unlikely to significantly alter disease progression to MPN-BP. Additional therapies are urgently needed that can deplete the MPN stem cell and significantly impact the course of disease, with the ultimate goal of improving the quality and quantity of life of MPN patients.
Key points:
Myeloproliferative neoplasms (MPNs) are clinically and biologically related but clinically and histopathologically distinct chronic hematopoietic disorders.
Diagnostic criteria for each MPN have been established by the World Health Organization and often include a bone marrow biopsy.
Pathobiologically, MPNs are progressive clonal diseases originating at the level of the hematopoietic stem cell which are associated with three specific driver mutations resulting in constitutive activation of the JAK-STAT pathway, systemic inflammation, constitutional symptoms and splenomegaly.
Major complications include thrombosis and progression of disease, either to a fibrotic stage or blast phase.
Synopsis.
William Dameshek coined the term myeloproliferative disorders in 1951 to describe a group of diseases morphologically linked by terminal myeloid cell expansion that frequently evolve from one clinical phenotype to another and which each eventually progress to acute myeloid leukemia. Diagnostic criteria for the Philadelphia chromosome-negative MPNs have been established by the World Health Organization and they are considered to be blood cancers. MPNs have a complex and incompletely understood pathogenesis that includes systemic inflammation, clonal hematopoiesis, and constitutive activation of the JAK-STAT pathway. Complications, such as thrombosis and progression to overt forms of myelofibrosis and acute leukemia, contribute significantly to the morbidity and mortality of MPN patients.
Disclosure Statement:
Dr. Hoffman is a consultant for Protagonist and serves on Data Safety Monitoring Boards for Novartis and AbbVie. He also receives research support from Novartis, Dompe, Kartos, AbbVie, Scholar Rock and Turning Point Therapeutics. Dr. Yacoub is a consultant for Incyte and Novartis. He has stocks and ownership in Hylapharm.
References
- 1.Dickstein JI, Vardiman JW. Hematopathologic findings in the myeloproliferative disorders. Semin Oncol 1995;22(4):355–373. [PubMed] [Google Scholar]
- 2.Barosi G, Mesa RA, Thiele J, et al. Proposed criteria for the diagnosis of post-polycythemia vera and post-essential thrombocythemia myelofibrosis: a consensus statement from the International Working Group for Myelofibrosis Research and Treatment. Leukemia 2008;22(2):437–438. [DOI] [PubMed] [Google Scholar]
- 3.Arber DA, Orazi A, Hasserjian R, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood 2016;127(20):2391–2405. [DOI] [PubMed] [Google Scholar]
- 4.Rowley JD. Letter: A new consistent chromosomal abnormality in chronic myelogenous leukaemia identified by quinacrine fluorescence and Giemsa staining. Nature 1973;243(5405):290–293. [DOI] [PubMed] [Google Scholar]
- 5.Cortes JE, Talpaz M, Giles F, et al. Prognostic significance of cytogenetic clonal evolution in patients with chronic myelogenous leukemia on imatinib mesylate therapy. Blood 2003;101(10):3794–3800. [DOI] [PubMed] [Google Scholar]
- 6.Goldman JM, Apperley JF, Jones L, et al. Bone marrow transplantation for patients with chronic myeloid leukemia. The New England journal of medicine 1986;314(4):202–207. [DOI] [PubMed] [Google Scholar]
- 7.Gratwohl A, Baldomero H, Horisberger B, et al. Current trends in hematopoietic stem cell transplantation in Europe. Blood 2002;100(7):2374–2386. [DOI] [PubMed] [Google Scholar]
- 8.Druker BJ, Sawyers CL, Kantarjian H, et al. Activity of a specific inhibitor of the BCR-ABL tyrosine kinase in the blast crisis of chronic myeloid leukemia and acute lymphoblastic leukemia with the Philadelphia chromosome. The New England journal of medicine 2001;344(14):1038–1042. [DOI] [PubMed] [Google Scholar]
- 9.Cohen MH, Williams G, Johnson JR, et al. Approval summary for imatinib mesylate capsules in the treatment of chronic myelogenous leukemia. Clinical cancer research : an official journal of the American Association for Cancer Research 2002;8(5):935–942. [PubMed] [Google Scholar]
- 10.Rampal R, Al-Shahrour F, Abdel-Wahab O, et al. Integrated genomic analysis illustrates the central role of JAK-STAT pathway activation in myeloproliferative neoplasm pathogenesis. Blood 2014;123(22):e123–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mesa RA, Miller CB, Thyne M, et al. Differences in treatment goals and perception of symptom burden between patients with myeloproliferative neoplasms (MPNs) and hematologists/oncologists in the United States: Findings from the MPN Landmark survey. Cancer 2017;123(3):449–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mylonas E, Yoshida K, Frick M, et al. Single-cell analysis based dissection of clonality in myelofibrosis. Nat Commun 2020;11(1):73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Verstovsek S, Mesa RA, Gotlib J, et al. Long-term treatment with ruxolitinib for patients with myelofibrosis: 5-year update from the randomized, double-blind, placebo-controlled, phase 3 COMFORT-I trial. Journal of hematology & oncology 2017;10(1):55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harrison CN, Vannucchi AM, Kiladjian JJ, et al. Long-term findings from COMFORT-II, a phase 3 study of ruxolitinib vs best available therapy for myelofibrosis. Leukemia 2016;30(8):1701–1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Deeg HJ, Bredeson C, Farnia S, et al. Hematopoietic Cell Transplantation as Curative Therapy for Patients with Myelofibrosis: Long-Term Success in all Age Groups. Biology of blood and marrow transplantation : journal of the American Society for Blood and Marrow Transplantation 2015;21(11):1883–1887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tremblay D, Marcellino B, Mascarenhas J. Pharmacotherapy of Myelofibrosis. Drugs 2017;77(14):1549–1563. [DOI] [PubMed] [Google Scholar]
- 17.Asher S, McLornan DP, Harrison CN. Current and future therapies for myelofibrosis. Blood Rev 2020;42:100715. [DOI] [PubMed] [Google Scholar]
- 18.Shallis RM, Wang R, Davidoff A, et al. Epidemiology of the classical myeloproliferative neoplasms: The four corners of an expansive and complex map. Blood Rev 2020;42:100706. [DOI] [PubMed] [Google Scholar]
- 19.Passamonti F, Malabarba L, Orlandi E, et al. Polycythemia vera in young patients: a study on the long-term risk of thrombosis, myelofibrosis and leukemia. Haematologica 2003;88(1):13–18. [PubMed] [Google Scholar]
- 20.Cario H, Schwarz K, Herter JM, et al. Clinical and molecular characterisation of a prospectively collected cohort of children and adolescents with polycythemia vera. British journal of haematology 2008;142(4):622–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Srour SA, Devesa SS, Morton LM, et al. Incidence and patient survival of myeloproliferative neoplasms and myelodysplastic/myeloproliferative neoplasms in the United States, 2001–12. British journal of haematology 2016;174(3):382–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cobb M. Reading and writing The Book of Nature: Jan Swammerdam (1637–1680). Endeavour 2000;24(3):122–128. [Google Scholar]
- 23.Hamarneh S. Measuring the Invisible World. The life and works of Antoni van Leeuwenhoek. Science 1960;132(3422):289–290. [Google Scholar]
- 24.Piller G. Leukaemia - a brief historical review from ancient times to 1950. British journal of haematology 2001;112(2):282–292. [DOI] [PubMed] [Google Scholar]
- 25.Donne AF. De l’origine des globules du sang, de leur mode de formatton et de leur fin 1842.
- 26.Bennett JH. Case of hypertrophy of the spleen and liver, in which death took place from suppuration of the blood. Edinburgh Med Sug J 1845;64:413–423. [Google Scholar]
- 27.Heuck G. Zwei fälle von Leukämie mit eigenthümlichem Blut-resp. Knochenmarksbefund. Archiv für pathologische Anatomie und Physiologie und für klinische Medicin 1879;78(3):475–496. [Google Scholar]
- 28.Vaquez H. Sur une forme spéciale de cyanose s’ accompagnant d’hyperglobulie excessive et persistante. CR Soc Biol (Paris) 1892;44:384–388. [Google Scholar]
- 29.Osler W. Chronic cyanosis, with polycythæmia and enlarged spleen: a new clinical entity. The American Journal of the Medical Sciences (1827–1924) 1903;126(2):187. [DOI] [PubMed] [Google Scholar]
- 30.Epstein E, Goedel A. Hemorrhagic thrombocythemia with a cascular, sclerotic spleen. Virchows Arch 1934;293:233–248. [Google Scholar]
- 31.Dameshek W. Some speculations on the myeloproliferative syndromes. Blood 1951;6(4):372–375. [PubMed] [Google Scholar]
- 32.Adamson JW, Fialkow PJ, Murphy S, et al. Polycythemia vera: stem-cell and probable clonal origin of the disease. New England Journal of Medicine 1976;295(17):913–916. [DOI] [PubMed] [Google Scholar]
- 33.Fialkow PJ, Faguet GB, Jacobson RJ, et al. Evidence that essential thrombocythemia is a clonal disorder with origin in a multipotent stem cell. 1981. [PubMed]
- 34.Jacobson RJ, Salo A, Fialkow PJ. Agnogenic myeloid metaplasia: a clonal proliferation of hematopoietic stem cells with secondary myelofibrosis. 1978. [PubMed]
- 35.Wasserman LR, Berk PD, Berlin NI. Polycythemia vera and the myeloproliferative disorders: WB Saunders Company; 1995. [Google Scholar]
- 36.Fruchtman SM, Mack K, Kaplan ME, et al. From efficacy to safety: a Polycythemia Vera Study group report on hydroxyurea in patients with polycythemia vera. Semin Hematol 1997;34(1):17–23. [PubMed] [Google Scholar]
- 37.Tartaglia AP, Goldberg JD, Berk PD, et al. Adverse effects of antiaggregating platelet therapy in the treatment of polycythemia vera. Semin Hematol 1986;23(3):172–176. [PubMed] [Google Scholar]
- 38.Levine RL, Loriaux M, Huntly BJ, et al. The JAK2V617F activating mutation occurs in chronic myelomonocytic leukemia and acute myeloid leukemia, but not in acute lymphoblastic leukemia or chronic lymphocytic leukemia. Blood 2005;106(10):3377–3379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.James C, Ugo V, Le Couedic JP, et al. A unique clonal JAK2 mutation leading to constitutive signalling causes polycythaemia vera. Nature 2005;434(7037):1144–1148. [DOI] [PubMed] [Google Scholar]
- 40.Kralovics R, Passamonti F, Buser AS, et al. A gain-of-function mutation of JAK2 in myeloproliferative disorders. The New England journal of medicine 2005;352(17):1779–1790. [DOI] [PubMed] [Google Scholar]
- 41.Baxter EJ, Scott LM, Campbell PJ, et al. Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders. Lancet 2005;365(9464):1054–1061. [DOI] [PubMed] [Google Scholar]
- 42.Biswas M, Prakash PK, Cossburn M, et al. Life-threatening thrombotic complications of relative polycythaemia. J Intern Med 2003;253(4):481–483. [DOI] [PubMed] [Google Scholar]
- 43.Weinreb NJ, Shih CF. Spurious polycythemia. Semin Hematol 1975;12(4):397–407. [PubMed] [Google Scholar]
- 44.Kremyanskaya M, Mascarenhas J, Hoffman R. Why does my patient have erythrocytosis? Hematol Oncol Clin North Am 2012;26(2):267–283, vii–viii. [DOI] [PubMed] [Google Scholar]
- 45.Huang LJ, Shen YM, Bulut GB. Advances in understanding the pathogenesis of primary familial and congenital polycythaemia. British journal of haematology 2010;148(6):844–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sergeyeva A, Gordeuk VR, Tokarev YN, et al. Congenital polycythemia in Chuvashia. Blood 1997;89(6):2148–2154. [PubMed] [Google Scholar]
- 47.Hoyer JD, Allen SL, Beutler E, et al. Erythrocytosis due to bisphosphoglycerate mutase deficiency with concurrent glucose-6-phosphate dehydrogenase (G-6-PD) deficiency. American journal of hematology 2004;75(4):205–208. [DOI] [PubMed] [Google Scholar]
- 48.Formenti F, Beer PA, Croft QP, et al. Cardiopulmonary function in two human disorders of the hypoxia-inducible factor (HIF) pathway: von Hippel-Lindau disease and HIF-2alpha gain-of-function mutation. FASEB journal : official publication of the Federation of American Societies for Experimental Biology 2011;25(6):2001–2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Albiero E, Ruggeri M, Fortuna S, et al. Isolated erythrocytosis: study of 67 patients and identification of three novel germ-line mutations in the prolyl hydroxylase domain protein 2 (PHD2) gene. Haematologica 2012;97(1):123–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gordeuk VR, Sergueeva AI, Miasnikova GY, et al. Congenital disorder of oxygen sensing: association of the homozygous Chuvash polycythemia VHL mutation with thrombosis and vascular abnormalities but not tumors. Blood 2004;103(10):3924–3932. [DOI] [PubMed] [Google Scholar]
- 51.Percy MJ, McMullin MF, Jowitt SN, et al. Chuvash-type congenital polycythemia in 4 families of Asian and Western European ancestry. Blood 2003;102(3):1097–1099. [DOI] [PubMed] [Google Scholar]
- 52.Tefferi A, Rumi E, Finazzi G, et al. Survival and prognosis among 1545 patients with contemporary polycythemia vera: an international study. Leukemia 2013;27(9):1874–1881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pardanani A, Lasho TL, Finke C, et al. Prevalence and clinicopathologic correlates of JAK2 exon 12 mutations in JAK2V617F-negative polycythemia vera. Leukemia 2007;21(9):1960–1963. [DOI] [PubMed] [Google Scholar]
- 54.Silver RT, Krichevsky S. Distinguishing essential thrombocythemia JAK2V617F from polycythemia vera: limitations of erythrocyte values. Haematologica 2019;104(11):2200–2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Santhosh-Kumar CR, Yohannan MD, Higgy KE, et al. Thrombocytosis in adults: analysis of 777 patients. J Intern Med 1991;229(6):493–495. [DOI] [PubMed] [Google Scholar]
- 56.Vannucchi AM, Barbui T. Thrombocytosis and thrombosis. Hematology American Society of Hematology Education Program 2007:363–370. [DOI] [PubMed] [Google Scholar]
- 57.Wiestner A, Schlemper RJ, van der Maas AP, et al. An activating splice donor mutation in the thrombopoietin gene causes hereditary thrombocythaemia. Nature genetics 1998;18(1):49–52. [DOI] [PubMed] [Google Scholar]
- 58.Ghilardi N, Wiestner A, Kikuchi M, et al. Hereditary thrombocythaemia in a Japanese family is caused by a novel point mutation in the thrombopoietin gene. British journal of haematology 1999;107(2):310–316. [DOI] [PubMed] [Google Scholar]
- 59.Teofili L, Larocca LM. Advances in understanding the pathogenesis of familial thrombocythaemia. British journal of haematology 2011;152(6):701–712. [DOI] [PubMed] [Google Scholar]
- 60.Tefferi A, Guglielmelli P, Larson DR, et al. Long-term survival and blast transformation in molecularly annotated essential thrombocythemia, polycythemia vera, and myelofibrosis. Blood 2014;124(16):2507–2513; quiz 2615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Milosevic Feenstra JD, Nivarthi H, Gisslinger H, et al. Whole-exome sequencing identifies novel MPL and JAK2 mutations in triple-negative myeloproliferative neoplasms. Blood 2016;127(3):325–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tefferi A, Lasho TL, Finke CM, et al. Targeted deep sequencing in primary myelofibrosis. Blood Adv 2016;1(2):105–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Thiele J, Georgii A, Vykoupil KF. Ultrastructure of chronic megakaryocytic-granulocytic myelosis. Blut 1976;32(6):433–438. [DOI] [PubMed] [Google Scholar]
- 64.Vardiman JW, Harris NL, Brunning RD. The World Health Organization (WHO) classification of the myeloid neoplasms. Blood 2002;100(7):2292–2302. [DOI] [PubMed] [Google Scholar]
- 65.Vardiman JW, Thiele J, Arber DA, et al. The 2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important changes. Blood 2009;114(5):937–951. [DOI] [PubMed] [Google Scholar]
- 66.Barbui T, Thiele J, Passamonti F, et al. Survival and disease progression in essential thrombocythemia are significantly influenced by accurate morphologic diagnosis: an international study. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 2011;29(23):3179–3184. [DOI] [PubMed] [Google Scholar]
- 67.Guglielmelli P, Pacilli A, Rotunno G, et al. Presentation and outcome of patients with 2016 WHO diagnosis of prefibrotic and overt primary myelofibrosis. Blood 2017;129(24):3227–3236. [DOI] [PubMed] [Google Scholar]
- 68.Cervantes F, Dupriez B, Pereira A, et al. New prognostic scoring system for primary myelofibrosis based on a study of the International Working Group for Myelofibrosis Research and Treatment. Blood 2009;113(13):2895–2901. [DOI] [PubMed] [Google Scholar]
- 69.Skoda RC, Duek A, Grisouard J. Pathogenesis of myeloproliferative neoplasms. Experimental hematology 2015;43(8):599–608. [DOI] [PubMed] [Google Scholar]
- 70.Kralovics R, Skoda RC. Molecular pathogenesis of Philadelphia chromosome negative myeloproliferative disorders. Blood Rev 2005;19(1):1–13. [DOI] [PubMed] [Google Scholar]
- 71.Lundberg P, Takizawa H, Kubovcakova L, et al. Myeloproliferative neoplasms can be initiated from a single hematopoietic stem cell expressing JAK2-V617F. The Journal of experimental medicine 2014;211(11):2213–2230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zahr AA, Salama ME, Carreau N, et al. Bone marrow fibrosis in myelofibrosis: pathogenesis, prognosis and targeted strategies. Haematologica 2016;101(6):660–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kimura A, Katoh O, Hyodo H, et al. Transforming growth factor-beta regulates growth as well as collagen and fibronectin synthesis of human marrow fibroblasts. British journal of haematology 1989;72(4):486–491. [DOI] [PubMed] [Google Scholar]
- 74.Ozono Y, Shide K, Kameda T, et al. Neoplastic fibrocytes play an essential role in bone marrow fibrosis in Jak2V617F-induced primary myelofibrosis mice. Leukemia 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Pardanani AD, Levine RL, Lasho T, et al. MPL515 mutations in myeloproliferative and other myeloid disorders: a study of 1182 patients. Blood 2006;108(10):3472–3476. [DOI] [PubMed] [Google Scholar]
- 76.Lasho TL, Pardanani A, Tefferi A. LNK mutations in JAK2 mutation-negative erythrocytosis. The New England journal of medicine 2010;363(12):1189–1190. [DOI] [PubMed] [Google Scholar]
- 77.Tong W, Lodish HF. Lnk inhibits Tpo-mpl signaling and Tpo-mediated megakaryocytopoiesis. The Journal of experimental medicine 2004;200(5):569–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Marty C, Pecquet C, Nivarthi H, et al. Calreticulin mutants in mice induce an MPL-dependent thrombocytosis with frequent progression to myelofibrosis. Blood 2016;127(10):1317–1324. [DOI] [PubMed] [Google Scholar]
- 79.Klampfl T, Gisslinger H, Harutyunyan AS, et al. Somatic mutations of calreticulin in myeloproliferative neoplasms. The New England journal of medicine 2013;369(25):2379–2390. [DOI] [PubMed] [Google Scholar]
- 80.Lundberg P, Karow A, Nienhold R, et al. Clonal evolution and clinical correlates of somatic mutations in myeloproliferative neoplasms. Blood 2014;123(14):2220–2228. [DOI] [PubMed] [Google Scholar]
- 81.Vannucchi AM, Lasho TL, Guglielmelli P, et al. Mutations and prognosis in primary myelofibrosis. Leukemia 2013;27(9):1861–1869. [DOI] [PubMed] [Google Scholar]
- 82.Colotta F, Allavena P, Sica A, et al. Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability. Carcinogenesis 2009;30(7):1073–1081. [DOI] [PubMed] [Google Scholar]
- 83.Barbui T, Carobbio A, Finazzi G, et al. Inflammation and thrombosis in essential thrombocythemia and polycythemia vera: different role of C-reactive protein and pentraxin 3. Haematologica 2011;96(2):315–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Barbui T, Carobbio A, Finazzi G, et al. Elevated C-reactive protein is associated with shortened leukemia-free survival in patients with myelofibrosis. Leukemia 2013;27(10):2084–2086. [DOI] [PubMed] [Google Scholar]
- 85.Skov V, Larsen TS, Thomassen M, et al. Molecular profiling of peripheral blood cells from patients with polycythemia vera and related neoplasms: identification of deregulated genes of significance for inflammation and immune surveillance. Leukemia research 2012;36(11):1387–1392. [DOI] [PubMed] [Google Scholar]
- 86.Skov V, Larsen TS, Thomassen M, et al. Whole-blood transcriptional profiling of interferon-inducible genes identifies highly upregulated IFI27 in primary myelofibrosis. European journal of haematology 2011;87(1):54–60. [DOI] [PubMed] [Google Scholar]
- 87.Fisher DAC, Miner CA, Engle EK, et al. Cytokine production in myelofibrosis exhibits differential responsiveness to JAK-STAT, MAP kinase, and NFkappaB signaling. Leukemia 2019;33(8):1978–1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kristinsson SY, Landgren O, Samuelsson J, et al. Autoimmunity and the risk of myeloproliferative neoplasms. Haematologica 2010;95(7):1216–1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Pedersen KM, Bak M, Sorensen AL, et al. Smoking is associated with increased risk of myeloproliferative neoplasms: A general population-based cohort study. Cancer Med 2018;7(11):5796–5802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wang JC, Chang TH, Goldberg A, et al. Quantitative analysis of growth factor production in the mechanism of fibrosis in agnogenic myeloid metaplasia. Experimental hematology 2006;34(12):1617–1623. [DOI] [PubMed] [Google Scholar]
- 91.Cho SY, Xu M, Roboz J, et al. The effect of CXCL12 processing on CD34+ cell migration in myeloproliferative neoplasms. Cancer research 2010;70(8):3402–3410. [DOI] [PubMed] [Google Scholar]
- 92.Tefferi A, Vaidya R, Caramazza D, et al. Circulating interleukin (IL)-8, IL-2R, IL-12, and IL-15 levels are independently prognostic in primary myelofibrosis: a comprehensive cytokine profiling study. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 2011;29(10):1356–1363. [DOI] [PubMed] [Google Scholar]
- 93.Hultcrantz M, Bjorkholm M, Dickman PW, et al. Risk for Arterial and Venous Thrombosis in Patients With Myeloproliferative Neoplasms: A Population-Based Cohort Study. Annals of internal medicine 2018;168(5):317–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sekhar M, McVinnie K, Burroughs AK. Splanchnic vein thrombosis in myeloproliferative neoplasms. British journal of haematology 2013;162(6):730–747. [DOI] [PubMed] [Google Scholar]
- 95.Tremblay D, Vogel AS, Moshier E, et al. Outcomes of Splanchnic Vein Thrombosis in Patients with Myeloproliferative Neoplasms in a Single Center Experience. European journal of haematology 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sozer S, Fiel MI, Schiano T, et al. The presence of JAK2V617F mutation in the liver endothelial cells of patients with Budd-Chiari syndrome. Blood 2009;113(21):5246–5249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Guy A, Gourdou-Latyszenok V, Le Lay N, et al. Vascular endothelial cell expression of JAK2(V617F) is sufficient to promote a pro-thrombotic state due to increased P-selectin expression. Haematologica 2019;104(1):70–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.van Genderen PJ, Lucas IS, van Strik R, et al. Erythromelalgia in essential thrombocythemia is characterized by platelet activation and endothelial cell damage but not by thrombin generation. Thromb Haemost 1996;76(3):333–338. [PubMed] [Google Scholar]
- 99.Rungjirajittranon T, Owattanapanich W, Ungprasert P, et al. A systematic review and meta-analysis of the prevalence of thrombosis and bleeding at diagnosis of Philadelphia-negative myeloproliferative neoplasms. BMC cancer 2019;19(1):184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Campbell PJ, MacLean C, Beer PA, et al. Correlation of blood counts with vascular complications in essential thrombocythemia: analysis of the prospective PT1 cohort. Blood 2012;120(7):1409–1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Mital A, Prejzner W, Bieniaszewska M, et al. Prevalence of acquired von Willebrand syndrome during essential thrombocythemia: a retrospective analysis of 170 consecutive patients. Pol Arch Med Wewn 2015;125(12):914–920. [DOI] [PubMed] [Google Scholar]
- 102.Dunbar AJ, Rampal RK, Levine R. Leukemia secondary to myeloproliferative neoplasms. Blood 2020;136(1):61–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Vallapureddy RR, Mudireddy M, Penna D, et al. Leukemic transformation among 1306 patients with primary myelofibrosis: risk factors and development of a predictive model. Blood cancer journal 2019;9(2):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Vannucchi AM, Guglielmelli P, Rotunno G, et al. Mutation-Enhanced International Prognostic Scoring System (MIPSS) for Primary Myelofibrosis: An AGIMM & IWG-MRT Project. Blood 2014;124(21):405–405. [Google Scholar]
- 105.Tefferi A, Guglielmelli P, Nicolosi M, et al. GIPSS: genetically inspired prognostic scoring system for primary myelofibrosis. Leukemia 2018;32(7):1631–1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Tefferi A, Lasho TL, Guglielmelli P, et al. Targeted deep sequencing in polycythemia vera and essential thrombocythemia. Blood Adv 2016;1(1):21–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Hultcrantz M, Wilkes SR, Kristinsson SY, et al. Risk and Cause of Death in Patients Diagnosed With Myeloproliferative Neoplasms in Sweden Between 1973 and 2005: A Population-Based Study. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 2015;33(20):2288–2295. [DOI] [PubMed] [Google Scholar]
- 108.Landtblom AR, Andersson TM, Dickman PW, et al. Risk of infections in patients with myeloproliferative neoplasms-a population-based cohort study of 8363 patients. Leukemia 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Lussana F, Cattaneo M, Rambaldi A, et al. Ruxolitinib-associated infections: A systematic review and meta-analysis. American journal of hematology 2018;93(3):339–347. [DOI] [PubMed] [Google Scholar]
- 110.Tremblay D, King A, Li L, et al. Risk factors for infections and secondary malignancies in patients with a myeloproliferative neoplasm treated with ruxolitinib: a dual-center, propensity score-matched analysis. Leukemia & lymphoma 2019:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Frederiksen H, Farkas DK, Christiansen CF, et al. Chronic myeloproliferative neoplasms and subsequent cancer risk: a Danish population-based cohort study. Blood 2011;118(25):6515–6520. [DOI] [PubMed] [Google Scholar]
- 112.Hasselbalch HC. Chronic inflammation as a promotor of mutagenesis in essential thrombocythemia, polycythemia vera and myelofibrosis. A human inflammation model for cancer development? Leukemia research 2013;37(2):214–220. [DOI] [PubMed] [Google Scholar]
- 113.Dickinson M, Kamdar M, Huntly BJP, et al. A Phase I Study of Molibresib (GSK525762), a Selective Bromodomain (BRD) and Extra Terminal Protein (BET) Inhibitor: Results from Part 1 of a Phase I/II Open Label Single Agent Study in Subjects with Non-Hodgkin’s Lymphoma (NHL). Paper presented at: ASH Annual Meeting2018. [Google Scholar]
- 114.Pemmaraju N, Kantarjian H, Nastoupil L, et al. Characteristics of patients with myeloproliferative neoplasms with lymphoma, with or without JAK inhibitor therapy. Blood 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Hong J, Lee JH, Byun JM, et al. Risk of disease transformation and second primary solid tumors in patients with myeloproliferative neoplasms. Blood Adv 2019;3(22):3700–3708. [DOI] [PMC free article] [PubMed] [Google Scholar]


