Abstract
Methyl p-hydroxycinnamate (MH), an esterified derivative of p-Coumaric acid exerts anti-inflammatory effects on lipopolysaccharide (LPS)-stimulated RAW264.7 macrophages. Based on these effects, the present study investigated the protective role of MH in a mouse model of LPS-induced acute respiratory distress syndrome (ARDS). The results demonstrated that administration of LPS (5 mg/kg intranasally) markedly increased the neutrophil/macrophage numbers and levels of inflammatory molecules (TNF-α, IL-6, IL-1β and reactive oxygen species) in the bronchoalveolar lavage fluid (BALF) of mice. On histological examination, the presence of inflammatory cells was observed in the lungs of mice administered LPS. LPS also notably upregulated the secretion of monocyte chemoattractant protein-1 and protein content in BALF as well as expression of inducible nitric oxide synthase in the lungs of mice; it also caused activation of p38 mitogen-activated protein kinase (MAPK) and NF-κB signaling. However, MH treatment significantly suppressed LPS-induced upregulation of inflammatory cell recruitment, inflammatory molecule levels and p38MAPK/NF-κB activation, and also led to upregulation of heme oxygenase-1 (HO-1) expression in the lungs of mice. In addition, the ability of MH to induce HO-1 expression was confirmed in RAW264.7 macrophages. Taken together, the findings of the present study indicated that MH may exert protective effects against airway inflammation in ARDS mice by inhibiting inflammatory cell recruitment and the production of inflammatory molecules.
Keywords: acute respiratory distress syndrome, methyl p-hydroxycinnamate, inflammatory cell, NF-κB, heme oxygenase-1
Introduction
Acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) are characterized by rapid pulmonary inflammation and ARDS is considered the most severe form of ALI (1). Pro-inflammatory cytokines (TNF-α, IL-6 and IL-1β) have been identified as biomarkers of ALI/ARDS (2,3). Neutrophil-derived reactive oxygen species (ROS) promote lung injury in the pathogenesis of ALI/ARDS (4) and increased ROS levels indicate neutrophil activation. Furthermore, macrophage-derived monocyte chemoattractant protein-1 (MCP-1) accelerates pulmonary inflammation by inducing neutrophil/macrophage recruitment (5). Lipopolysaccharide (LPS) is used to induce ALI/ARDS in mouse models (6–8), which show significant upregulation of inflammatory cytokines and chemokines (TNF-α, IL-6, IL-1β and MCP-1). In addition, an increase in inducible nitric oxide synthase (iNOS) protein levels in the lung has been reported in clinical and pre-clinical studies of ALI/ARDS (9–11).
In ALI/ARDS pathogenesis, inflammatory cytokines, chemokines and mediators are expressed following NF-κB activation (5,12). Mitogen-activated protein kinase (MAPK) activation serves an important role in LPS-stimulated inflammatory response (13,14). Cumulative evidence suggests that an increase in the expression of heme oxygenase-1 (HO-1) relieves inflammatory response in ALI and ARDS (15,16).
Methyl p-hydroxycinnamate (MH) is an esterified derivative of p-Coumaric acid that has been shown to possess anti-lipid peroxidation activity (17). Previously, the anti-inflammatory properties of MH were confirmed in LPS-stimulated RAW264.7 macrophages (18); MH strongly inhibited the production of TNF-α and IL-1β, which serve as clinical predictors in ALI/ARDS (1,5). Based on these previous results, MH may exert ameliorative effects on ARDS. Therefore, the present study aimed to investigate the potential protective role of MH against pulmonary inflammation in a mouse model of LPS-induced ARDS.
Materials and methods
Cell culture
RAW264.7 cells were purchased from American Type Culture Collection and maintained in DMEM supplemented with 10% FBS and 1% antibiotic/antimycotic solution (all Invitrogen; Thermo Fisher Scientific, Inc.) in 5% CO2 (37°C). To detect HO-1 expression, cells were seeded into 6-well plates (5×105 cells/well) and incubated at 37°C with 5, 10 and 20 µM MH (SynQuest Laboratories, Inc.) for 16 h.
Mouse model of LPS-induced ALI
Male C57BL/6 mice (n=24; age, 6 weeks; weight, 18–20 g) were purchased from Koatech Co., Ltd. and were housed in specific-pathogen-free cages (22–23°C; 55–60% humidity; 12 h light/dark cycle) with free access to food and water. The animal experimental procedures were approved by the Institutional Animal Care and Use Committee of the Korea Research Institute of Bioscience and Biotechnology (Ochang, Korea). To induce ARDS in mice, the dosage of LPS was selected based on previous studies (5,8). In brief, mice were intranasally exposed to LPS (5 mg/kg, 40 µl) on day 0. At 1 h after LPS administration, MH and dexamethasone (DEX; positive control) were intraperitoneally administered on days 0–2. The mice were randomly divided into four groups (n=6/group) as follows: i) Normal control (NC; treated with normal saline, i.p.); ii) ARDS (LPS); iii) DEX (LPS + 1 mg/kg DEX, i.p.) and iv) MH 15 (LPS + 15 mg/kg MH, i.p.). DEX and MH were dissolved with 1% DMSO and 1% Tween-20 in PBS.
Inflammatory cell count and ELISA
To evaluate the number of inflammatory cells and levels of inflammatory molecules in bronchoalveolar lavage fluid (BALF), BALF was collected as previously described (19). The mice were anesthetized with Zoletil 50 (30–50 mg/kg i.p.; Virbac) and xylazine (5–10 mg/kg i.p.; Bayer-Korea, Ltd.) on day 3, as previously described (19). Tracheal PBS perfusion was performed 24 h after the final intraperitoneal treatment of MH and DEX, and BALF was collected from all groups. Then, BALF cells were mounted on glass slides, stained with Diff-Quik® solution at room temperature for 30 sec (Sysmex Co., Ltd.) to distinguish the cells according to morphology and then manually counted under a light microscope (magnification, ×400). The levels of TNF-α, IL-6 and IL-1β in BALF were determined using ELISA kits according to the manufacturer's instructions (cat. nos. 558534, 555240 and 559603, respectively; all BD Biosciences, Inc.). To evaluate the level of intracellular ROS activity, BALF cells were maintained with 20 µM 2′,7′-dichloroflurorescein diacetate (Sigma-Aldrich; Merck KGaA) for 10 min at 37°C as previously described (20). Then, fluorescence was detected using a plate reader (wavelength, 488 nm excitation and 525 nm emission). The levels of total protein content in BALF were determined using a BCA assay kit (Thermo Fisher Scientific, Inc.) according to the manufacturer's protocol.
Lung wet/dry (W/D) ratio
The degree of edema was determined as the ratio of lung W/D weight. Briefly, lungs were collected from the mice, washed with PBS to remove blood and weighed with electronic balance (wet weight). Then, the lungs were dried at 60°C for 48 h in an incubator before measuring dry weight. The calculation of W/D ratio was determined to evaluate the lung edema as previously described (13).
Western blotting
Following the collection of BALF, the mice were sacrificed by cervical dislocation as previously described (21). Lysate of mouse lung and RAW264.7 whole cells were prepared using CelLytic™ MT Cell lysis buffer (cat. no. c3228; SigmaAldrich; Merck KGaA) in the presence of protease and phosphatase inhibitor cocktail as previously described (19) and protein quantification was performed using BCA assay. Then, the protein (50 µg/lane) was separated with 10–12% SDS-PAGE and transferred to PVDF membranes. Each membrane was blocked at room temperature with 5% skimmed milk in 0.3% (TBST for 1 h and incubated at 4°C for 16 h with primary anti-phosphorylated (p)-p38 (cat. no. 9211; 1:1,000; Cell Signaling Technology, Inc.), anti-p-IκBα (cat. no. 2859; 1:1,000; Cell Signaling Technology, Inc.), anti-p-p65 (cat. no. 3033; 1:1,000; Cell Signaling Technology, Inc.), anti-p65 (cat. no. 8242; 1:1,000; Cell Signaling Technology, Inc.), anti-β-actin (cat. no. sc-69879; 1:2,000; Santa Cruz Biotechnology, Inc.), anti-p38 (cat. no. sc-7149; 1:1,000; Santa Cruz Biotechnology, Inc.), anti-CD68 (cat. no. sc-20060; 1:1,000; Santa Cruz Biotechnology, Inc.), anti-p-HO-1 (cat. no. 27338; 1:1,000; Invitrogen; Thermo Fisher Scientific, Inc.) and anti-IκBα (cat. no. 15132; 1:1,000; Invitrogen; Thermo Fisher Scientific, Inc.), Then, membranes were washed at room temperature with TBST and incubated with horseradish peroxidase-conjugated secondary antibodies (goat antimouse & anti-rabbit; both 1:2,000; cat. nos. 115-035-003 and 111-035-003, respectively; both Jackson ImmunoResearch Laboratories, Inc.) at room temperature for 1 h. Finally, each membrane was developed with Clarity™ Western ECL Substrate (cat. no. 170–5061; Bio-Rad Laboratories Inc.). Protein bands were visualized using an ImageQuant LAS 4000 mini luminescent Image Analyzer (GE Healthcare, Inc) and the levels of protein expression were quantified using ImageJ software (version 1.50e; National Institutes of Health). β-actin was used as the loading control.
Histological examination
To confirm histological changes, lung tissue was isolated from mice and fixed at room temperature for 48 h with 10% formalin. Then, the lungs were embedded in paraffin, cut into 4-µm sections using a microtome and stained with hematoxylin and eosin (H&E) at room temperature for 5 and 1 min, respectively. The levels of inflammatory cells in the airway were quantitatively measured using ImageJ software (version 1.50e; National Institutes of Health).
Statistical analysis
Data are presented as the mean ± standard deviation of ≥3 independent experiments. One-way ANOVA followed by Tukey's multiple comparison test was performed to analyze differences using SPSS 20.0 software (IBM Corp.). P<0.05 was considered to indicate a statistically significant difference.
Results
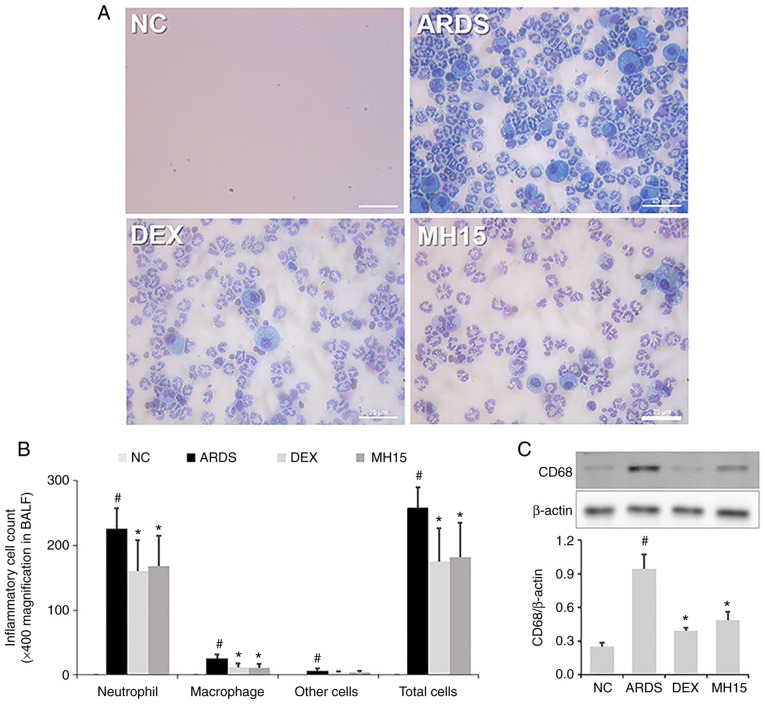
Effects of MH on neutrophil/macrophage recruitment in LPS-induced ARDS mice
According to the procedure in Fig. 1, the protective effect of MH on LPS-induced ARDS in mice was assessed. The inhibitory effect of MH on neutrophil recruitment was investigated; a significant increase in neutrophil numbers was confirmed in the BALF of LPS-induced ARDS mice (Fig. 2A and B). This increase was lower in BALF of the MH15 group compared with the ARDS group. Similar to its effects on neutrophils, MH treatment also suppressed the increase in numbers of macrophages in the BALF of ARDS mice. In addition, western blotting indicated that the expression of CD68, which is a marker of pro-inflammatory M1 macrophages, was significantly increased in lungs of LPS-induced ARDS mice (Fig. 2C). However, MH treatment decreased this increase in lungs of ARDS mice. The inhibitory effects of 15 mg/kg MH were similar to those of 1 mg/kg DEX, which was used as a positive control.
Figure 1.
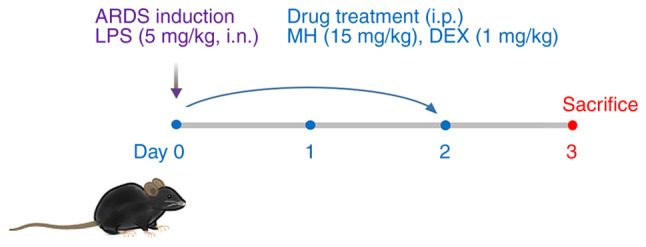
Induction of LPS-induced ARDS and treatment with MH or DEX in a mouse model. C57BL/6 mice were randomly divided into four groups (n=6/group) and administered 5 mg/kg LPS i.n. on day 0. At 1 h after LPS administration, i.p. administration of MH (15 mg/kg) or DEX (1 mg/kg) was performed on days 0–2. On day 3, mice were sacrificed and the collection of bronchoalveolar lavage fluid and lung tissue was performed for analysis. ARDS, acute respiratory distress syndrome; LPS, lipopolysaccharide; MH, methyl p-hydroxycinnamate; DEX, dexamethasone; i.p., intraperitoneal; i.n., intranasal.
Figure 2.
MH decreases the numbers of neutrophils and macrophages and expression of CD68 in lipopolysaccharide-induced ARDS mice. (A) Neutrophil and macrophage counts in BALF of mice were determined using Diff-Quik® staining and (B) cell counting (magnification, ×400; scale bar, 25 µM). (C) Expression level of CD68 in the lungs of mice was determined using western blotting. Quantitative analysis of CD68 was performed using ImageJ. Data are expressed as the mean ± SD. #P<0.05 vs. NC; *P<0.05 vs. ARDS. NC, normal control; ARDS, acute respiratory distress syndrome; DEX, dexamethasone; MH, methyl p-hydroxycinnamate; BALF, bronchoalveolar lavage fluid.
Effects of MH on inflammatory molecule levels in LPS-induced ARDS mice
Next, it was investigated whether MH exerted inhibitory effects on the levels of inflammatory molecules. A significant increase in TNF-α, IL-6 and IL-1β levels was observed in the BALF of LPS-induced ARDS mice (Fig. 3A-C). MH treatment significantly inhibited this increase. The increased levels of ROS in the BALF of ARDS mice was also decreased by MH treatment (Fig. 3D). The inhibitory ability of 15 mg/kg MH on the levels of these molecules was similar to that of 1 mg/kg DEX, which was used as a positive control.
Figure 3.
MH decreases inflammatory molecule levels in lipopolysaccharide-induced ARDS mice. The levels of (A) TNF-α, (B) IL-6 and (C) IL-1β in the bronchoalveolar lavage fluid of mice were determined using ELISA. (D) ROS production in the bronchoalveolar lavage fluid of mice was determined as 2′,7′-dichloroflurorescein diacetate fluorescence measurement. Data are expressed as the mean ± SD. #P<0.05 vs. NC; *P<0.05 vs. ARDS. ROS, reactive oxygen species; NC, normal control; ARDS, acute respiratory distress syndrome; DEX, dexamethasone; MH, methyl p-hydroxycinnamate.
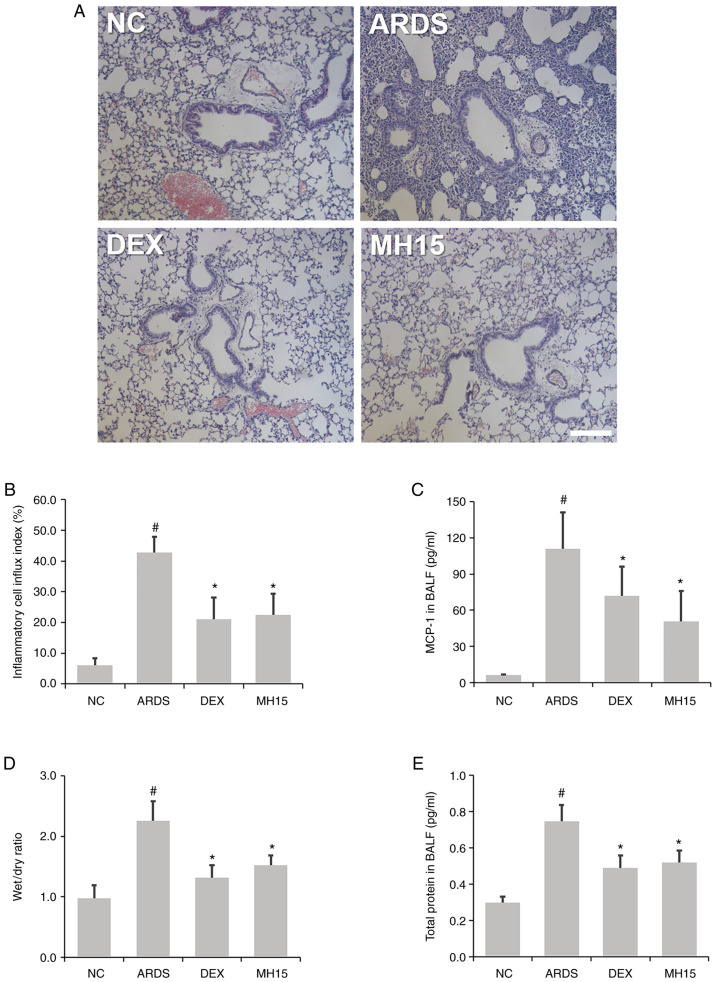
Effects of MH on inflammatory cell infiltration and lung edema in LPS-induced ARDS mice
H&E staining showed that the influx of inflammatory cells around the airway was higher in the lungs of LPS-induced ARDS mice compared with the NC group, whereas this trend was decreased in ARDS mice receiving MH treatment (Fig. 4A and B). In addition, the results of ELISA demonstrated that MH treatment attenuated the LPS-induced MCP-1 secretion in the BALF of mice (Fig. 4C). MH exerted an inhibitory effect on LPS-induced increase of ratio of lung W/D weight (Fig. 4D). Furthermore, MH decreased LPS-induced upregulation of total protein content in BALF of mice (Fig. 4E), showing that MH exerted a regulatory effect in LPS-induced inflammatory cell influx and lung edema. The inhibitory effects of 15 mg/kg MH on the level of inflammatory cell infiltration and lung edema were similar to that of 1 mg/kg DEX, which was used as a positive control.
Figure 4.
MH suppresses inflammatory cell influx and MCP-1 secretion in lipopolysaccharide-induced ARDS mice. (A) Hematoxylin and eosin staining was used to detect inflammatory cells around the airways in the lungs of mice (magnification, ×100; scale bar, 100 µM). (B) Quantitative analysis of airway inflammation. (C) ELISA was used to determine the secretion level of MCP-1 in BALF of mice. (D) Lung wet/dry ratio and (E) BALF protein were evaluated to determine lung edema. Data are expressed as the mean ± SD. #P<0.05 vs. NC; *P<0.05 vs. ARDS. MCP-1, monocyte chemoattractant proein-1; NC, normal control; ARDS, acute respiratory distress syndrome; DEX, dexamethasone; MH, methyl p-hydroxycinnamate; BALF, bronchoalveolar lavage fluid.
Effects of MH on iNOS expression in LPS-induced ARDS mice
Western blotting results demonstrated that the expression of iNOS protein was significantly upregulated in lungs of LPS-induced ARDS mice (Fig. 5). However, MH treatment decreased this upregulation in the lungs of ARDS mice. The inhibitory effects of 15 mg/kg MH on the expression of iNOS were similar to that of 1 mg/kg DEX, which was used as a positive control.
Figure 5.
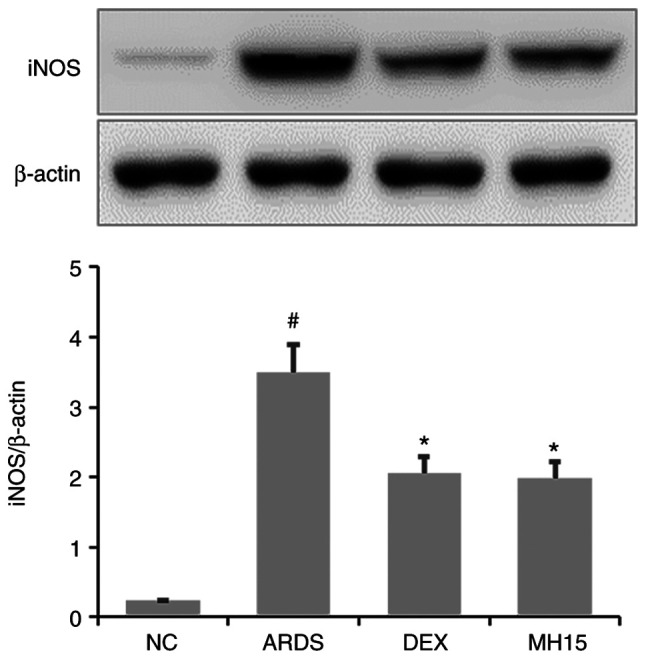
MH downregulates the expression of iNOS in lipopolysaccharide-induced ARDS mice. The expression level of iNOS in the lungs of mice was determined using western blotting. Quantitative analysis of iNOS was performed using ImageJ software. Data are expressed as the mean ± SD. #P<0.05 vs. NC; *P<0.05 vs. ARDS. iNOS, inducible nitric oxide synthase; NC, normal control; ARDS, acute respiratory distress syndrome; DEX, dexamethasone; MH, methyl p-hydroxycinnamate.
Effects of MH on p38MAPK/NF-κB activation in LPS-induced ARDS mice
Increased p38 phosphorylation was confirmed in the lungs of LPS-induced ARDS mice, whereas this was significantly reversed by MH treatment (Fig. 6A and B). Similar to these results, MH exerted inhibitory effects on LPS-induced upregulation of IκB and NF-κB phosphorylation (Fig. 6C and D). In total, the inhibitory ability of 15 mg/kg MH on the activation of p38MAPK and NF-κB was similar to that of 1 mg/kg DEX, which was used as a positive control.
Figure 6.
MH inhibits activation of p38 MAPK and NF-κB in lipopolysaccharide-induced ARDS mice. The phosphorylation levels of (A and B) p38 MAPK and (C and D) NF-κB in the lungs of mice were determined using western blotting. Quantitative analysis of p-p38, p-IκB and p-p65 was performed using ImageJ. Data are expressed as the mean ± SD. #P<0.05 vs. NC; *P<0.05 vs. ARDS. p-, phosphorylated; NC, normal control; ARDS, acute respiratory distress syndrome; DEX, dexamethasone; MH, methyl p-hydroxycinnamate.
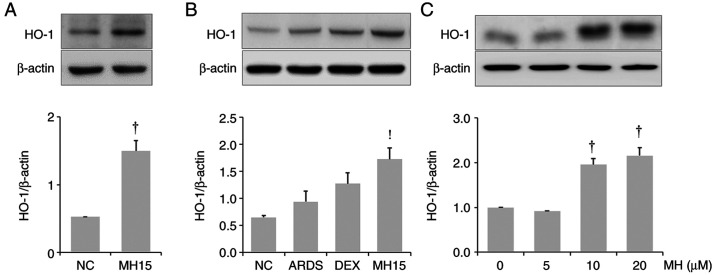
Effects of MH on HO-1 induction in lungs of mice and RAW264.7 macrophages
It was investigated whether MH affects HO-1 expression in the lungs of control or ARDS mice. MH treatment resulted in upregulation of HO-1 expression in the lungs of control mice or ARDS mice (Fig. 7A and B). The results also demonstrated that MH treatment at 10 and 20 µM led to an increase in HO-1 expression in RAW264.7 macrophages (Fig. 7C).
Figure 7.
MH upregulates HO-1 expression in the lungs of ARDS mice and in RAW264.7 macrophages. (A) Western blotting was used to detect the expression of HO-1 in lungs of (A) control and (B) ARDS mice and (C) RAW264.7 macrophages. Quantitative analysis of HO-1 was performed using ImageJ software. Data are expressed as the mean ± SD. †P<0.05 vs. NC; !P<0.05 vs. LPS. HO-1, heme oxygenase-1; NC, normal control; MH, methyl p-hydroxycinnamate; ARDS, acute respiratory distress syndrome; DEX, dexamethasone.
Discussion
Accumulating evidence has shown that endotoxins cause pulmonary inflammation by inducing excessive production of TNF-α, IL-6, IL-1β, ROS and MCP-1, thereby leading to organ dysfunction and lung edema during the pathogenesis of ALI/ARDS (5,22–24). Macrophages and neutrophils accelerate pulmonary inflammation by participating in the production of these molecules (5). Thus, regulation of these cell-derived inflammatory molecules may ameliorate the development of ALI/ARDS. The aim of the present study was to confirm the inhibitory effect of MH on neutrophil/macrophage recruitment and the production of TNF-α, IL-6, IL-1β, ROS and MCP-1 in mice with LPS-induced ARDS. The present study demonstrated that MH exerted an ameliorative effect on the recruitment of inflammatory cells (neutrophils and macrophages), production of cytokines and chemokines and lung edema. In addition, the inhibitory effect of MH on inflammatory cell infiltration of lung tissue was also confirmed by histological examination. These results indicated that MH may exert protective effects by suppressing pulmonary inflammation in ALI/ARDS mice by controlling inflammatory cell recruitment and inflammatory molecule secretion.
Increased iNOS-induced NO generation contributes to the formation of peroxynitrite, which leads to vascular leakage and organ injury in ALI/ARDS (25). Researchers have reported that iNOS inhibitors effectively relieve inflammatory response in in vivo studies of ALI/ARDS (26,27). In a previous study, MH was shown to exert inhibitory effects on both iNOS and NO production in LPS-induced RAW264.7 macrophages (18). In the present study, the inhibitory effect of MH on iNOS expression was confirmed in ARDS mice. These results collectively suggest that MH may serve as an iNOS inhibitor in ALI/ARDS.
Activation of p38 MAPK is associated with ROS generation (28,29). Inhibition of p38 relieves pulmonary inflammation in mice with ALI/ARDS (30,31). Accumulating evidence has shown that suppression of NF-κB activation ameliorates airway inflammation by downregulating inflammatory cytokines, chemokines and mediators (6,32–34) in in vivo studies on ALI/ARDS. Therefore, therapeutic approaches to inflammatory diseases, including ALI/ARDS, have focused on the regulation of these signaling pathways. Based on these studies, the role of MH in the regulation of p38 MAPK and NF-κB activation was examined. In the present study, MH was shown to exert suppressive effect on LPS-induced p38 MAPK/NF-κB activation, indicating that the protective effects of MH were mediated not only by regulating inflammatory molecule production, but also by p38 MAPK/NF-κB activation.
LPS-induced ROS generation leads to excessive inflammation and oxidative damage (35,36) and the induction of the antioxidant protein HO-1 exerts protective effects against LPS-induced pulmonary inflammation and oxidative stress in mice (6,19,37,38). Inhibition of expression of cytokines (TNF-α, IL-6 and IL-1β), chemokines (MCP-1) and inflammatory mediators (iNOS) and of activation of p38MAPK/NF-κB is accompanied by HO-1 upregulation. The present study confirmed that MH inhibited the production of TNF-α, IL-6, IL-1β, MCP-1 and ROS, expression of iNOS and p38 MAPK/NF-κB activation. Based on these results, the present study investigated whether MH leads to HO-1 induction. The results revealed the ability of MH to induce HO-1 expression both in vivo and in vitro, suggesting that MH has antioxidant properties that may be associated with its anti-inflammatory activity.
In conclusion, the present study demonstrated that MH effectively ameliorated pulmonary inflammation in LPS-induced ARDS mice. This effect was accompanied by suppression of p38MAPK/NF-κB activation. In addition, MH led to an increase in HO-1 expression. Thus, MH may be of value as an adjuvant for the treatment of ALI/ARDS.
Acknowledgements
Not applicable.
Funding Statement
The present study was supported by Korea Research Institute of Bioscience and Biotechnology Research Initiative Program (grant nos. KGM5522113 and KGS1402113).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
SMK, JHM, JHK, JC, JMP, JL, SHG, JHO, SHK, WC and KSA performed the experiments and analyzed data. SK and JWL designed and conceived the study and revised the manuscript. All authors have read and approved the final manuscript. All authors drafted and revised the manuscript. All authors have read and approved the final manuscript. SMK, JHM, JHK, SK and JWL confirm the authenticity of all the raw data.
Ethics approval and consent to participate
The experimental procedures were approved by the Institutional Animal Care and Use Committee of the Korea Research Institute of Bioscience and Biotechnology (Ochang, Korea; approval no. KRIBB-AEC-21111).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Spadaro S, Park M, Turrini C, Tunstall T, Thwaites R, Mauri T, Ragazzi R, Ruggeri P, Hansel TT, Caramori G, Volta CA. Biomarkers for Acute Respiratory Distress syndrome and prospects for personalised medicine. J Inflamm (Lond) 2019;16:1. doi: 10.1186/s12950-018-0202-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhargava M, Wendt CH. Biomarkers in acute lung injury. Transl Res. 2012;159:205–217. doi: 10.1016/j.trsl.2012.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barnett N, Ware LB. Biomarkers in acute lung injury-marking forward progress. Crit Care Clin. 2011;27:661–683. doi: 10.1016/j.ccc.2011.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kellner M, Noonepalle S, Lu Q, Srivastava A, Zemskov E, Black SM. ROS signaling in the pathogenesis of acute lung Injury (ALI) and acute respiratory distress syndrome (ARDS) Adv Exp Med Biol. 2017;967:105–137. doi: 10.1007/978-3-319-63245-2_8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee JW, Chun W, Lee HJ, Min JH, Kim SM, Seo JY, Ahn KS, Oh SR. The role of macrophages in the development of acute and chronic inflammatory lung diseases. Cells. 2021;10:897. doi: 10.3390/cells10040897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee JW, Chun W, Kwon OK, Park HA, Lim Y, Lee JH, Kim DY, Kim JH, Lee HK, Ryu HW, et al. 3,4,5-Trihydroxycinnamic acid attenuates lipopolysaccharide (LPS)-induced acute lung injury via downregulating inflammatory molecules and upregulating HO-1/AMPK activation. Int Immunopharmacol. 2018;64:123–130. doi: 10.1016/j.intimp.2018.08.015. [DOI] [PubMed] [Google Scholar]
- 7.Lee JW, Park HA, Kwon OK, Park JW, Lee G, Lee HJ, Lee SJ, Oh SR, Ahn KS. NPS 2143, a selective calcium-sensing receptor antagonist inhibits lipopolysaccharide-induced pulmonary inflammation. Mol Immunol. 2017;90:150–157. doi: 10.1016/j.molimm.2017.07.012. [DOI] [PubMed] [Google Scholar]
- 8.Liu B, Cheng Y, Wu Y, Zheng X, Li X, Yang G, He T, Li S, Shen F. Emodin improves alveolar hypercoagulation and inhibits pulmonary inflammation in LPS-provoked ARDS in mice via NF-κB inactivation. Int Immunopharmacol. 2020;88:107020. doi: 10.1016/j.intimp.2020.107020. [DOI] [PubMed] [Google Scholar]
- 9.Frank JA, Pittet JF, Lee H, Godzich M, Matthay MA. High tidal volume ventilation induces NOS2 and impairs cAMP- dependent air space fluid clearance. Am J Physiol Lung Cell Mol Physiol. 2003;284:L791–L798. doi: 10.1152/ajplung.00331.2002. [DOI] [PubMed] [Google Scholar]
- 10.Xiao Q, Cui Y, Zhao Y, Liu L, Wang H, Yang L. Orientin relieves lipopolysaccharide-induced acute lung injury in mice: The involvement of its anti-inflammatory and anti-oxidant properties. Int Immunopharmacol. 2021;90:107189. doi: 10.1016/j.intimp.2020.107189. [DOI] [PubMed] [Google Scholar]
- 11.Lee SA, Lee SH, Kim JY, Lee WS. Effects of glycyrrhizin on lipopolysaccharide-induced acute lung injury in a mouse model. J Thorac Dis. 2019;11:1287–1302. doi: 10.21037/jtd.2019.04.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moine P, McIntyre R, Schwartz MD, Kaneko D, Shenkar R, Le Tulzo Y, Moore EE, Abraham E. NF-kappaB regulatory mechanisms in alveolar macrophages from patients with acute respiratory distress syndrome. Shock. 2000;13:85–91. doi: 10.1097/00024382-200013020-00001. [DOI] [PubMed] [Google Scholar]
- 13.Zhong WT, Wu YC, Xie XX, Zhou X, Wei MM, Soromou LW, Ci XX, Wang DC. Phillyrin attenuates LPS-induced pulmonary inflammation via suppression of MAPK and NF-κB activation in acute lung injury mice. Fitoterapia. 2013;90:132–139. doi: 10.1016/j.fitote.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 14.Guo S, Jiang K, Wu H, Yang C, Yang Y, Yang J, Zhao G, Deng G. Magnoflorine ameliorates lipopolysaccharide-induced acute lung injury via suppressing NF-κB and MAPK activation. Front Pharmacol. 2018;9:982. doi: 10.3389/fphar.2018.00982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lei J, Wei Y, Song P, Li Y, Zhang T, Feng Q, Xu G. Cordycepin inhibits LPS-induced acute lung injury by inhibiting inflammation and oxidative stress. Eur J Pharmacol. 2018;818:110–114. doi: 10.1016/j.ejphar.2017.10.029. [DOI] [PubMed] [Google Scholar]
- 16.Pooladanda V, Thatikonda S, Bale S, Pattnaik B, Sigalapalli DK, Bathini NB, Singh SB, Godugu C. Nimbolide protects against endotoxin-induced acute respiratory distress syndrome by inhibiting TNF-α mediated NF-κB and HDAC-3 nuclear translocation. Cell Death Dis. 2019;10:81. doi: 10.1038/s41419-018-1247-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kwon YS, Kim CM. Antioxidant constituents from the stem of Sorghum bicolor. Arch Pharm Res. 2003;26:535–539. doi: 10.1007/BF02976877. [DOI] [PubMed] [Google Scholar]
- 18.Vo VA, Lee JW, Shin SY, Kwon JH, Lee HJ, Kim SS, Kwon YS, Chun W. Methyl p-Hydroxycinnamate suppresses lipopolysaccharide-induced inflammatory responses through akt phosphorylation in RAW264.7 cells. Biomol Ther (Seoul) 2014;22:10–16. doi: 10.4062/biomolther.2013.095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Park JW, Ryu HW, Ahn HI, Min JH, Kim SM, Kim MG, Kwon OK, Hwang D, Kim SY, Choi S, et al. The anti-inflammatory effect of trichilia martiana C. DC. in the lipopolysaccharide-stimulated inflammatory response in macrophages and airway epithelial cells and in LPS-challenged mice. J Microbiol Biotechnol. 2020;30:1614–1625. doi: 10.4014/jmb.2006.06042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee JW, Ryu HW, Lee SU, Kim MG, Kwon OK, Kim MO, Oh TK, Lee JK, Kim TY, Lee SW, et al. Pistacia weinmannifolia ameliorates cigarette smoke and lipopolysaccharide-induced pulmonary inflammation by inhibiting interleukin8 production and NF-κB activation. Int J Mol Med. 2019;44:949–959. doi: 10.3892/ijmm.2019.4247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tian M, Peng S, Wang S, Li X, Li H, Shen L. Pristimerin reduces dextran sulfate sodium-induced colitis in mice by inhibiting microRNA-155. Int Immunopharmacol. 2021;94:107491. doi: 10.1016/j.intimp.2021.107491. [DOI] [PubMed] [Google Scholar]
- 22.Bhatia M, Moochhala S. Role of inflammatory mediators in the pathophysiology of acute respiratory distress syndrome. J Pathol. 2004;202:145–156. doi: 10.1002/path.1491. [DOI] [PubMed] [Google Scholar]
- 23.Parsons PE, Eisner MD, Thompson BT, Matthay MA, Ancukiewicz M, Bernard GR, Wheeler AP, NHLBI Acute Respiratory Distress Syndrome Clinical Trials Network Lower tidal volume ventilation and plasma cytokine markers of inflammation in patients with acute lung injury. Crit Care Med. 2005;33:1–6. doi: 10.1097/01.CCM.0000149854.61192.DC. discussion 230-2. [DOI] [PubMed] [Google Scholar]
- 24.Dong Z, Yuan Y. Accelerated inflammation and oxidative stress induced by LPS in acute lung injury: Inhibition by ST1926. Int J Mol Med. 2018;41:3405–3421. doi: 10.3892/ijmm.2018.3574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guimarães LMF, Rossini CVT, Lameu C. Implications of SARS-Cov-2 infection on eNOS and iNOS activity: Consequences for the respiratory and vascular systems. Nitric Oxide. 2021;111-112:64–71. doi: 10.1016/j.niox.2021.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen JR, Tang Y, Wang YL, Cui Q, Inam M, Kong LC, Ma HX. Serine protease inhibitor MDSPI16 ameliorates LPS-induced acute lung injury through its anti-inflammatory activity. Int Immunopharmacol. 2020;88:107015. doi: 10.1016/j.intimp.2020.107015. [DOI] [PubMed] [Google Scholar]
- 27.Wu YX, Zeng S, Wan BB, Wang YY, Sun HX, Liu G, Gao ZQ, Chen D, Chen YQ, Lu MD, Pang QF. Sophoricoside attenuates lipopolysaccharide-induced acute lung injury by activating the AMPK/Nrf2 signaling axis. Int Immunopharmacol. 2021;90:107187. doi: 10.1016/j.intimp.2020.107187. [DOI] [PubMed] [Google Scholar]
- 28.Sun WH, Liu F, Chen Y, Zhu YC. Hydrogen sulfide decreases the levels of ROS by inhibiting mitochondrial complex IV and increasing SOD activities in cardiomyocytes under ischemia/reperfusion. Biochem Biophys Res Commun. 2012;421:164–169. doi: 10.1016/j.bbrc.2012.03.121. [DOI] [PubMed] [Google Scholar]
- 29.Lan A, Liao X, Mo L, Yang C, Yang Z, Wang X, Hu F, Chen P, Feng J, Zheng D, Xiao L. Hydrogen sulfide protects against chemical hypoxia-induced injury by inhibiting ROS-activated ERK1/2 and p38MAPK signaling pathways in PC12 cells. PLoS One. 2011;6:e25921. doi: 10.1371/journal.pone.0025921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fang W, Cai SX, Wang CL, Sun XX, Li K, Yan XW, Sun YB, Sun XZ, Gu CK, Dai MY, et al. Modulation of mitogen-activated protein kinase attenuates sepsis-induced acute lung injury in acute respiratory distress syndrome rats. Mol Med Rep. 2017;16:9652–9658. doi: 10.3892/mmr.2017.7811. [DOI] [PubMed] [Google Scholar]
- 31.Wu H, Zhao G, Jiang K, Chen X, Zhu Z, Qiu C, Li C, Deng G. Plantamajoside ameliorates lipopolysaccharide-induced acute lung injury via suppressing NF-κB and MAPK activation. Int Immunopharmacol. 2016;35:315–322. doi: 10.1016/j.intimp.2016.04.013. [DOI] [PubMed] [Google Scholar]
- 32.Jha P, Das H. KLF2 in Regulation of NF-κB-Mediated immune cell function and inflammation. Int J Mol Sci. 2017;18:2383. doi: 10.3390/ijms18112383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Meng L, Li L, Lu S, Li K, Su Z, Wang Y, Fan X, Li X, Zhao G. The protective effect of dexmedetomidine on LPS-induced acute lung injury through the HMGB1-mediated TLR4/NF-κB and PI3K/Akt/mTOR pathways. Mol Immunol. 2018;94:7–17. doi: 10.1016/j.molimm.2017.12.008. [DOI] [PubMed] [Google Scholar]
- 34.Tang J, Xu L, Zeng Y, Gong F. Effect of gut microbiota on LPS-induced acute lung injury by regulating the TLR4/NF-kB signaling pathway. Int Immunopharmacol. 2021;91:107272. doi: 10.1016/j.intimp.2020.107272. [DOI] [PubMed] [Google Scholar]
- 35.Zhang WB, Yang F, Wang Y, Jiao FZ, Zhang HY, Wang LW, Gong ZJ. Inhibition of HDAC6 attenuates LPS-induced inflammation in macrophages by regulating oxidative stress and suppressing the TLR4-MAPK/NF-κB pathways. Biomed Pharmacother. 2019;117:109166. doi: 10.1016/j.biopha.2019.109166. [DOI] [PubMed] [Google Scholar]
- 36.Dong Q, Li Y, Chen J, Wang N. Azilsartan Suppressed LPS-Induced Inflammation in U937 Macrophages through Suppressing Oxidative Stress and Inhibiting the TLR2/MyD88 Signal Pathway. ACS Omega. 2020;6:113–118. doi: 10.1021/acsomega.0c03655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu Q, Ci X, Wen Z, Peng L. Diosmetin Alleviates Lipopolysaccharide-Induced acute lung injury through activating the Nrf2 Pathway and inhibiting the NLRP3 Inflammasome. Biomol Ther (Seoul) 2018;26:157–166. doi: 10.4062/biomolther.2016.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liu Y, Song M, Zhu G, Xi X, Li K, Wu C, Huang L. Corynoline attenuates LPS-induced acute lung injury in mice by activating Nrf2. Int Immunopharmacol. 2017;48:96–101. doi: 10.1016/j.intimp.2017.04.029. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.