Abstract
Background
Hospital acquired infections are preventable cause for morbidity and mortality worldwide. In the current pandemic era proper implementation of infection control measures can prevent the spread of such infections including SARS-CoV 2. The study was done to identified the source and reason for spread of COVID-19 infection and devise recommendations to halt the progress of infection in a non-COVID area.
Methods
An outbreak in a non-COVID area of a tertiary care hospital was investigated by the infection control team along with the epidemiologist when they were notified about the rising cases of COVID-19 from Advanced Trauma Center’s (ATC) disaster ward. The time, place and person distribution of the cases were studied. Recommendations based on gaps identified were developed onsite and implemented to control the outbreak.
Results
The outbreak lasted from 19th December 2020 to 12th January 2021, affecting 34 people (25 patients and 9 health care workers). The attack rate was 9.2%. We identified the causes of current outbreak as compromises in infection prevention measures, high bed patient ratio, irregularities in the ventilation system, overcrowding by patient attendants and communication gaps between nursing officers and doctors. Measures required to control the outbreak were implemented and no cases were reported for 2 weeks following the last positive case.
Conclusion
Non-COVID areas of hospitals are also at risk of nosocomial outbreaks of SARS-CoV 2 and therefore strict infection prevention measures those designated to COVID areas should be followed in non-COVID zones also to prevent such outbreaks.
Keywords: COVID-19, outbreak, hospital acquired infection, infection prevention control measures, tertiary care institute, India
Introduction
A large proportion of hospital acquired infections (HAIs) can be prevented by following proper infection prevention control (IPC) measures.1-3 Specific measures to prevent spread of SARS-CoV 2 infection in hospitals include snuggly fitted mask around the face covering nose and mouth securing the chin with no pockets for air entry around the mouth and nasal region, washing hands with soap and water for at least 20 s or with gentle amount of 60% to 90% alcohol for minimum of 20 s following the 6 steps between patients, maintaining a minimum distance of at least 6 ft between 2 people, practicing cough etiquette such as covering mouth while coughing or using tissues and hand hygiene. 4 Non-compliance to any of these steps can be a source of exposure for contracting infection.
Hospital are the places where health care workers (HCWs) deal directly with the patients and are at maximum risk of contracting the infection. Similarly, the patients and their family members visiting hospitals are also at greater risk of contracting infection. In non-COVID areas of hospitals if people are little lax and IPC measures are not followed strictly, there is a risk of nosocomial transmission of COVID 19.
The present study reports the results of an outbreak investigation conducted after a surge in number of COVID 19 cases in the non-COVID emergency ward of our tertiary care institute. Outbreak investigation was carried out to identify the source of infection, reasons for spread of infection, following which the control measures were undertaken to prevent further spread.
Outbreak Investigation (Methods)
Our hospital has designated areas for COVID and non-COVID patients. Initially all patients admitted to our hospital are screened for SARS-CoV-2 infection and tested for COVID-19 using Reverse Transcriptase Polymerase Chain Reaction (RTPCR)/Gene Xpert. The patients who test positive are either admitted in the designated COVID area or are sent for home isolation depending upon severity of COVID 19 infection. Patients with a negative COVID report are admitted to various non-COVID wards for further management. All HCWs in the institute have undergone training in infection prevention control measures including how to wear Personal Protective Equipment (PPE) correctly. In the COVID areas, HCWs work in recommended PPE and the donning and doffing of PPE are strictly supervised in these areas. 5 Also the hand hygiene of staff is monitored and a strict loop of audit and feedback is maintained. Patient attendants are not allowed inside these wards. Ventilation of COVID hospital was modified to make it suitable for housing these patients. 6
In the non-COVID areas, patients’ attendants are allowed to accompany the patient and perform many healthcare related activities due to manpower resource constraint. The ventilation system had not been altered. Donning and doffing is not strictly supervised although a “buddy system” is generally recommended to be followed by the infection control team (ICT). HCWs working in the non-COVID areas have access to recommended PPE and are instructed to wear face shields or goggles while performing any aerosol generating procedures however supervision is not there in these areas.
The current outbreak occurred in the Disaster ward of our Advanced Trauma Centre. The ATC area is used as transit point for patients of orthopedic and neurosurgery departments. ATC Disaster ward is divided into 2 areas, a ward area comprising of 30 beds and a waiting hall which has a capacity to house up to 12 trolleys. It is a very busy ward and at the time of this outbreak there was a foot fall of the 80 patients daily. The patient bed ratio was 1:2.6, which is more than 100% capacity of the area.
Normally, in 1 week, there are 1 or 2 patients who are reported positive for COVID-19 from this ward. On 4th January 2021, 6 patients were reported as positive within a span of 24 h. This sudden increase was communicated by the nursing staff of ATC area to the infection control team (ICT) who along with the epidemiologist visited the site and confirmed the outbreak after reviewing the records. A detailed outbreak investigation was then carried out by this team. The time, place and person distribution of the cases was studied. The outbreak investigation team observed the PPE being worn by HCWs and patients’ attendants and audited hand hygiene practices. The distance between the adjacent beds and trolleys was noted. The heating ventilation and air conditioning (HVAC) system of the area was also looked at with the help of the Engineering staff.
Surveillance was carried out to identify the source the indirect transmission apart from direct transmission (person to person). Sampling was done from various environmental surfaces in the ward area and waiting hall (bed railings, medicine trolleys, bed sheets, nursing stations, intravenous sets).
The guidelines of Ministry of Health and Family Welfare (MoHFW) for control of COVID-19 outbreak in a non-COVID area were implemented for controlling the outbreak. 7 Recommendations were made on the basis of the gaps identified to prevent further outbreaks.
Results of Investigation and Outbreak Control Measures Implemented
The team found that the index patient, had been reported positive on 19th December 2021 but the doctor on duty had misplaced this report. Three days passed before a repeat sample was sent. which was positive and then this patient was shifted to our COVID hospital. The team interviewed the nursing staff and doctors regarding this delay in testing but it was noted that although temperature was recorded in the nursing charts, it was not communicated to the doctors. Sometimes doctors missed suspecting COVID-19 cases due to a similarity with symptoms due to injury/trauma with that of the COVID-19 symptoms. Maintaining a log book/alert book was advised by the ICT which had to be seen/ checked by the nursing officer and resident doctors in change over shifts.
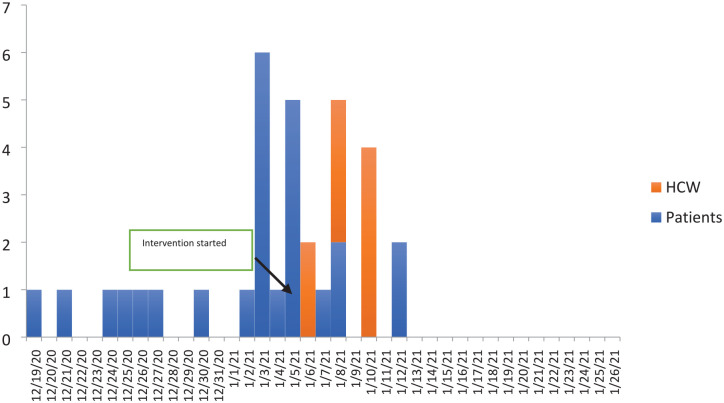
During the outbreak 34 people were found COVID-19 positive including 25 patients and 9 healthcare workers. During the outbreak period, that is, from 19th December 2020 to 12 January 2021, 328 patients were admitted to this ward and 47 health care workers were posted in ATC disaster ward. The attack rate among HCWs was (47) 19.1% while that among patients was (328) 7.6%. The overall attack rate was 9.2% at the institutional level (ATC ward). There was no mortality among the patients or HCWs affected in the outbreak. The date of onset of COVID-19 cases are presented in the epidemic curve (Figure 1). The outbreak control measures were implemented from 4th January 2021. Maximum number of cases were reported on 3rd January 2021. The last case was reported on 12th January 2021.
Figure 1.
Epidemic curve of COVID-19 cases in disaster ward of advance trauma center from 19th December 2020 to 12th January 2021.
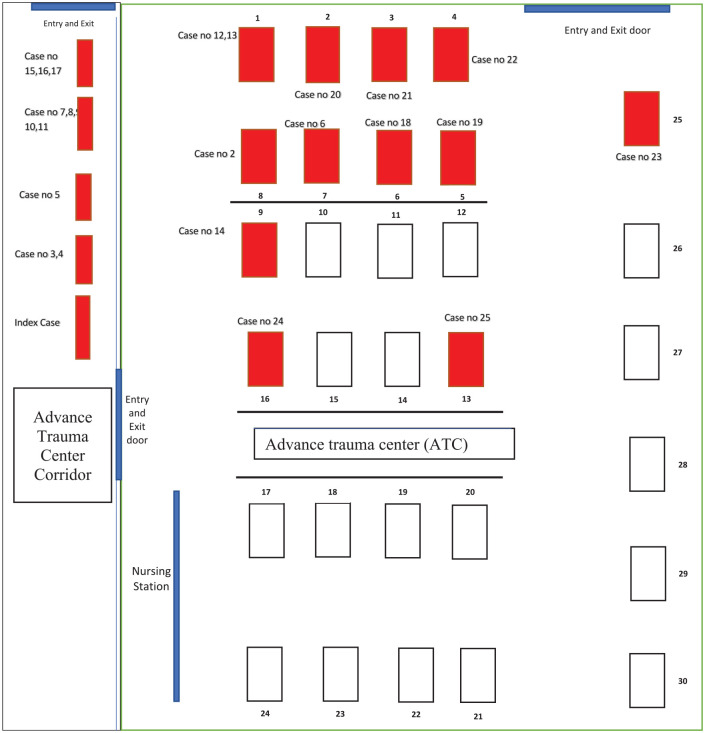
The location of beds of the COVID 19 positive cases is shown in Figure 2. Most of the cases were reported from the corridor where patient trolleys had been placed in corridor in close proximity to each other and also on the beds near the entry and exit gates. This suggests that COVID-19 infection was found mostly in the area of maximum human movement. The line list of admitted patients and the staff posted in ATC disaster ward is presented in Tables 1 and 2 respectively. The study found that the median duration between admission and becoming COVID-19 positive was 19 days (IQR: 9.5-23 days). There was delay of approximately 3 days in appearance of symptoms and sending sample for testing of the patients and the health care workers.
Figure 2.
Spot map of COVID-19 cases in disaster ward of advance trauma center from 19th December 2020 to 12th January 2021.
Table 1.
Line List of the COVID-19 Positive Patients Admitted in ATC Ward from December 19th 2020 to January 12th 2021.
| Case no. | Date of admission | Date of start of symptoms | Date of COVID 19 positive report | Time between symptoms and sending sample (days) | Duration of stay in ATC ward | Symptoms | Discharged/shifted to COVID hospital |
|---|---|---|---|---|---|---|---|
| 1 | 30/11/2020 | 15/12/20 | 19/12/2020 and 23/12/2020 | 4 | 19 | No | Shifted to COVID hospital |
| 2 | 05/12/2020 | 19/12/ 2020 | 21/12/2020 | 2 | 16 | Fever | Home isolation |
| 3 | 25/11/2020 | 21/12/2020 | 24/12/2020 | 3 | 29 | Fever | Home isolation |
| 4 | 3/12/2020 | NA | 25/12/2020 | NA | 22 | No | Home isolation |
| 5 | 8/12/2020 | NA | 26/12/2020 | NA | 18 | No | Home isolation |
| 6 | 8/12/2020 | 24/12/20 | 27/12/2020 | 3 | 19 | Fever | Shifted to COVID hospital |
| 7 | 10/12/2020 | NA | 30/12/2020 | NA | 20 | No | Home isolation |
| 8 | 25/12/2020 | NA | 02/01/2021 | NA | 8 | No | Home isolation |
| 9 | 29/12/2020 | NA | 03/01/2021 | NA | 5 | No | Shifted to COVID hospital |
| 10 | 12/12/2020 | NA | 03/01/2021 | NA | 22 | No | Home isolation |
| 11 | 01/01/2021 | NA | 03/01/2021 | NA | 2 | No | Home isolation |
| 12 | 22/12/2020 | NA | 03/01/2021 | NA | 12 | No | Home isolation |
| 13 | 13/12/2020 | NA | 03/01/2021 | NA | 21 | No | Shifted to COVID hospital_ |
| 14 | 16/12/2020 | NA | 04/01/2021 | NA | 19 | No | Home isolation |
| 15 | 23/12/2020 | 1/1/21 | 03/01/2021 | 2 | 11 | Fever | Shifted to COVID hospital |
| 16 | 18/12/2020 | 2/1/21 | 05/01/2021 | 3 | 18 | Fever | Home isolation |
| 17 | 27/12/2020 | NA | 05/01/2021 | NA | 9 | No | Home isolation |
| 18 | 17/12/2020 | NA | 05/01/2021 | NA | 19 | No | Home isolation |
| 19 | 6/12/2020 | NA | 05/01/2021 | NA | 30 | No | Shifted to COVID hospital |
| 20 | 17/12/2020 | NA | 05/01/2021 | NA | 19 | No | Home isolation |
| 21 | 04/01/2021 | NA | 07/01/2021 | NA | 3 | No | Home isolation |
| 22 | 01/01/2021 | 5/1/21 | 08/01/2021 | 3 | 7 | Fever | Home isolation |
| 23 | 29/12/2020 | NA | 05/01/2021 | NA | 7 | No | Home isolation |
| 24 | 28/12/2020 | NA | 12/01/2021 | NA | 15 | No | Home isolation |
| 25 | 1/1/2021 | 10/1/21 | 12/01/2021 | 2 | 11 | Fever | Home isolation |
Table 2.
Characteristics of the Health Care Staff Found COVID 19 Positive in ATC Ward from December 19th 2020 to January 12th 2021.
| S. No | Date of posting in ATC ward | Symptoms | Date of symptoms | Date of testing COVID- 19 positive |
|---|---|---|---|---|
| 1 | Permanently posted | Fever | 4/1/2021 | 6/1/2021 |
| 2 | Permanently posted | Fever | 4/1/2021 | 6/1/2021 |
| 3 | Permanently posted | Fever | 7/1/2021 | 8/1/2021 |
| 4 | Permanently posted | Fever | 7/1/2021 | 8/1/2021 |
| 5 | Permanently posted | Fever | 7/1/2021 | 8/1/2021 |
| 6 | Permanently posted | Fever, Malaise | 8/1/2021 | 10/1/2021 |
| 7 | 28/12/2020 to 6/1/2021 | Fever | 9/1/2021 | 10/1/2021 |
| 8 | 28/12/2020 to 6/1/2021 | Fever | 9/1/2021 | 10/1/2021 |
| 9 | 28/12/2020 to 6/1/2021 | Fever | 8/1/2021 | 10/1/2021 |
The outbreak investigation team determined that the HVAC system in the ATC disaster was not working at the time of visit. The Engineering department dealing with the HVAC system of ATC was immediately contacted. It came to light that the HVAC system is operated as a single system for the whole building. If one has to shut down the system for 1 floor the whole system gets shut down and the ventilation of the other floors also gets compromised. The HVAC system had been working intermittently or as per demand of the users. The team concluded that there had been poor ventilation with inadequate air exchanges during the month prior to the outbreak period. Orders were given to immediately start the HVAC system following the Indian Society of Heating, Refrigeration and Air Conditioning Engineers (ISHARE) guidelines. The engineering department was also advised to maintain adequate ventilation in ATC disaster ward in the future.
Compliance to hand hygiene practice was found to be suboptimal among the staff members as well as the attendants of the patients. The investigation team noticed that staff wore poorly fitting masks leading to breach in PPE. Many attendants of the patients were either wearing cloth masks or ill-fitting surgical masks. The team strictly implemented both proper masks wearing and adequate hand hygiene between patients in ATC disaster ward. One security guard was designated at the entrance of ATC ward and was advised to distribute surgical mask to everyone who was wearing a cloth mask or poor-quality mask (torn or old looking mask).
The distance between the beds in the ATC area was found to be less than 2 m on either side. We also found that the ward was overcrowded, the patient to bed ratio was of 1:2.6 times and each patient was accompanied by 2 to 3 attendants which was making the place very congested. The patients with symptoms suggestive of COVID 19 were isolated. It was decided that 1 patient will be accompanied by 1 attendant at a time and attendants can stay with the patients in shifts after following IPC measures.
A meeting was conducted under the chairmanship of Head of the Institute, in-charge of the ward area, faculty of the concerned departments and outbreak control team. During the meeting it was decided to stop new admissions. It was also decided to stop shifting patients from ATC disaster ward to other wards immediately. It was also decided that new patients will be admitted only after all the existing admitted patients gets tested and were found negative.
All staff members and the patients in the wards were tested as per the GOI guidelines for testing of persons with high-risk exposure. All symptomatic patients in the ATC ward were tested for COVID-19 infection. Those who were positive and had mild symptoms were discharged for home isolation. The patients who were positive and had moderate to severe symptoms were shifted to designated COVID hospital in the institute. The asymptomatic patients who had high risk exposure were also discharged and were advised home quarantine and to get tested on day 7 of discharge or before, if symptomatic. The family members of home discharged patients were also advised to get tested. The current study telephonically followed up the patients who were home discharged as well as their family contacts and found that none of the patients as well as their family member became COVID19 positive.
All environmental surfaces sampled were negative for SARS-CoV 2 by RT-PCR. Nevertheless, the frequency of surface cleaning and disinfection was increased to once per shift (6-8 h) in the ward.
All patients had been discharged out of hospital or found negative by the 12th January 2021. The negative patients were shifted out to other wards for further management of their clinical conditions. The Disaster ward was disinfected on 13th January 2021 using 0.1% hypochlorite solution for surfaces and 0.5% for sanitary areas. The ward resumed services from 15th January 2021.
Discussion
The current study describes a nosocomial outbreak of COVID-19 infection in the non-COVID area of the tertiary care institute. A total of 34 persons tested positive which included 9 health care workers and 25 patients during this outbreak. The outbreak investigation team visited the site and assessed the risk factors for the outbreak and implemented the interventions with immediate effect to break the chain of transmission.
Both staff as well as attendants were found to be wearing ill-fitting masks along with poor compliance to hand hygiene. As demonstrated in previous studies, implementation of strict protocols for masks and hand hygiene in the current outbreak and supervision of the same stemmed the spread of infection.8-12
The current study found long median duration of stay in hospitals among the patients who came COVID-19 positive. Various studies have found longer duration of stay in hospital and nosocomial infections among patients.13,14 The COVID-19 positivity among the patients admitted in the hospital for some non-COVID related etiology indicate nosocomial/hospital acquired infection as found in our current study. This is similar to the reports of acquiring COVID-19 infection among non-COVID patients from other hospitals settings where nosocomial infections have been reported.15-17 The index case in our study had a long duration of stay in hospital who underwent multiple surgeries before becoming febrile and being detected as COVID-19 RT-PCR positive. Many studies have reported unknown or unidentified infectious persons/staff members as a source of transmission in nosocomial infection.17,18
Overcrowding in hospitals has been seen as a serious issue with respect to transmission of infection. The current study found a bed patient ratio of 1:2.6 ratio which suggested high bed occupancy in ATC ward and waiting area (bay). More patients in wards also meant more number of attendants along with them. The attendants are themselves a potential source or amplifier of spreading infection in such situations. Overcrowded wards have been associated with a higher prevalence of nosocomial infection than non-crowded wards. 19 Managing more patients in limited space leads to frequent transfer of the patients in and out of the area. Heavy patient load coupled with frequent transfer of patients made it difficult for the staff in supervising the implementation of infection prevention control measures properly by the patients and their attendants. This might have led to the transmission of infection among the patients admitted in the ATC area. We implemented 1 patient 1 attendant policy to control the outbreak.
Ventilation involves in fluxing clean air and removing stale air from a place in order to improve or maintain air quality. 20 The COVID 19 spreads more often when an infected person is kept in closed spaces. Ventilation is done either by the natural means such as opening a window or by mechanical systems such as installing HVAC systems. It is critical to bring in the air from outside and avoid pockets of stagnant air which are formed indoors. We found poor ventilation and air exchange in the disaster ward of ATC area during the outbreak period. This might have been a major factor along with others to the spread of this outbreak. Mechanical ventilation systems and air conditioning systems limits the risk of COVID-19 infection by improving the quality of outdoor air with filtration. 21 A study by Myaat et al 22 demonstrated the spread of rhinovirus associated with poor ventilation. A study by Kaushal et al 23 recommended a ventilation system that resulted in 9 minimum total air exchanges per hour with relative humidity of 30% to 60% and environmental temperature of 24°C to 27°C. Ventilation is not a single measure to control the spread of COVID 19 infection and should be implemented as part of comprehensive package of measures such as physical distancing, wearing a mask, frequent hand washing, and coughing and sneezing into a bent elbow. 20
Coordination is important for the successful running of an organization (nursing staff and doctors). A good clinical record is helpful in aiding coordination and continuity of care, informed decision making for patient management and targeting diagnostics and treatment plans. 24 Record keeping of patient data in the form of a logbook by staff in each shift helped to establish a continuum of information between subsequent shifts. This also improved communication between nursing staff and doctors in this otherwise busy unit.
Breaking the chain of transmission is an important intervention to stop the surge of cases in any setting. Various interventions implemented in our study helped in controlling the infection to a large extent. Studies have reported strict hygiene bundle, avoiding unnecessary endoscopic examination and aerosol generating procedures, wearing surgical mask properly while performing aerosol generating procedures such as pulmonary function test, intubation and mechanical ventilation, weaning, and extubation has helped in controlling the nosocomial spread of COVID-19 infection.25-27
Other studies have also reported similar causes of nosocomial outbreak.28,29 Isolation of COVID-19 symptomatic patients from others can help in breaking the chain of transmission of infection but the current study had asymptomatic patients also who were RTPCR positive, which made isolation of patients challenging. More than half of the asymptomatic or pre-symptomatic patients are found to transmit COVID-19 infection and thus pose a challenge in containing the infection. 30
Further, the infection from the health care workers to the patients cannot also be ruled out if infection control practices are breached. 31 There was delay in testing of HCWs which could have contributed to transmission. In a way the HCWs can be an amplifier of the infection and can exaggerate the outbreaks as they are the common link between patients. Owing to the community transmission of COVID-19 infection, it is difficult to exclude community acquisition of infection by the health care providers and transmitting it to the patients. 32
The study has some limitations also. The COVID-19 positivity among the asymptomatic patients can be a source of bias resulting in underestimation of total number of positive cases as they are less likely to get tested. Therefore, the attack rate calculated in our study could be an underestimation. The exact role of each factor (droplet transmission, shared equipment, hands of HCWs, overcrowding, poor ventilation) could not be determined. Possibly it was multifactorial. However, the findings for this study can be helpful in formulating internal policy in similar hospitals to prevent the spread of nosocomial outbreaks of COVID 19.
Conclusion
COVID 19 infection is a highly transmissible infection in overcrowded and poorly ventilated units of in hospitals. Overcrowding should be kept at minimum and ventilation of the area should be adequate so as to prevent pooling of droplets. Immediate testing of the symptomatic and isolating them from the non-infected individuals should be done at the earliest. An alert book/logbook should be maintained and complied so that nursing officers and resident doctors can read and follow the instructions and chances of missing COVID diagnosis should be minimum. Even during low community transmission periods, the index of suspicion should be high as closed areas can rapidly become hotspots of transmission of this disease. Most importantly, proper hand hygiene and snuggly fitting masks should be strictly implemented. There should be strict supervision of infection control practices in designated non-COVID areas in hospitals also as both staff as well as patient attendants tend to be lax here. Follow up of asymptomatic patients after discharge should be carried out to understand the burden of COVID-19 infection and to curtail transmission in the community.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: The manuscript has been approved by the Institutional Ethics Committee (INT/IEC/2021SPL-1357).
ORCID iDs: Kirtan Rana  https://orcid.org/0000-0001-9862-5700
https://orcid.org/0000-0001-9862-5700
P. V. M. Lakshmi  https://orcid.org/0000-0002-6921-9794
https://orcid.org/0000-0002-6921-9794
References
- 1. Shekelle PG, Pronovost PJ, Wachter RM, et al. The top patient safety strategies that can be encouraged for adoption now. Ann Intern Med. 2013;158:365-368. [DOI] [PubMed] [Google Scholar]
- 2. Shirol SS, Nimbaragi G, Prabhu M, et al. Health care associated infection fact sheet. 2019. Epub ahead of print. doi: 10.1007/s00238-013-0923-3 [DOI] [Google Scholar]
- 3. Allegranzi B, Bagheri Nejad S, Combescure C, et al. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet. 2011;377:228-241. [DOI] [PubMed] [Google Scholar]
- 4. National Centre for Disease Control; Directorate General of Health Services. National guidelines for infection prevention in health and control in healthcare facilities. 2020. [Google Scholar]
- 5. Dhandapani M, Kaur S, Das K, et al. Enhancing the safety of frontline healthcare workers during coronavirus disease: a novel real-time remote audiovisual aided doffing approach. Infect Dis. 2021;53:145-147. [DOI] [PubMed] [Google Scholar]
- 6. Pandey N, Kaushal V, Puri GD, et al. Transforming a General hospital to an infectious disease hospital for COVID-19 over 2 weeks. Front Public Health. 2020;8:382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. MoHFW. COVID -19 outbreak guidelines for setting up isolation facility/ward. Directorate General of Health Services. Ministry of Health & Family Welfare; 2020. [Google Scholar]
- 8. Lai AC, Poon CK, Cheung AC. Effectiveness of facemasks to reduce exposure hazards for airborne infections among general populations. J R Soc Interface. 2012;9:938-948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ueki H, Furusawa Y, Iwatsuki-Horimoto K, et al. Effectiveness of face masks in preventing airborne transmission of SARS-CoV-2. mSphere. Epub ahead of print 21 October 2020. doi: 10.1128/msphere.00637-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Stone SP, Fuller C, Savage J, et al. Evaluation of the national cleanyourhands campaign to reduce Staphylococcus aureus bacteraemia and Clostridium difficile infection in hospitals in England and Wales by improved hand hygiene: four year, prospective, ecological, interrupted time series study. BMJ. 2012;344:e3005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ho ML, Seto WH, Wong LC, Wong TY. Effectiveness of multifaceted hand hygiene interventions in long-term care facilities in Hong Kong: a cluster-randomized controlled trial. Infect Control Hosp Epidemiol. 2012;33:761-767. [DOI] [PubMed] [Google Scholar]
- 12. Pittet D, Hugonnet S, Harbarth S, et al. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Infection control programme. Lancet. 2000;356:1307-1312. [DOI] [PubMed] [Google Scholar]
- 13. Sulzgruber P, Schnaubelt S, Koller L, et al. An extended duration of the pre-operative hospitalization is associated with an increased risk of healthcare-associated infections after cardiac surgery. Sci Rep. 2020;10(1):8006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Jia H, Li L, Li W, et al. Impact of healthcare-associated infections on length of stay: a study in 68 hospitals in China. Biomed Res Int. 2019;2019:2590563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. J Am Med Assoc. 2020;323:1061-1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Meredith LW, Hamilton WL, Warne B, et al. Rapid implementation of SARS-CoV-2 sequencing to investigate cases of health-care associated COVID-19: a prospective genomic surveillance study. Lancet Infect Dis. 2020;20:1263-1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rickman HM, Rampling T, Shaw K, et al. Nosocomial transmission of COVID-19: a retrospective study of 66 hospital-acquired cases in a London teaching hospital. Clin Infect Dis. 2020;72:ciaa816-2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kabesch M, Roth S, Brandstetter S, et al. Successful containment of Covid-19 outbreak in a large maternity and perinatal center while continuing clinical service. Pediatr Allergy Immunol. 2020;31:560-564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Humphreys H. Overcrowding, understaffing and infection in hospitals. Ir Med J. 2006;99:102. [PubMed] [Google Scholar]
- 20. Coronavirus Disease (COVID-19): ventilation and air conditioning. Accessed September 1, 2021. https://www.who.int/news-room/q-a-detail/coronavirus-disease-covid-19-ventilation-and-air-conditioning
- 21. Kapur V, Agarwal B, Baliga G, et al. ISHRAE COVID-19 guidance document for air conditioning and ventilation. 2020. [Google Scholar]
- 22. Myatt TA, Johnston SL, Zuo Z, et al. Detection of airborne rhinovirus and its relation to outdoor air supply in office environments. Am J Respir Crit Care Med. 2004;169:1187-1190. [DOI] [PubMed] [Google Scholar]
- 23. Kaushal V, Saini PS, Gupta AK. Environmental control including ventilation in hospitals. J Sci. 2004;6:229-232. [Google Scholar]
- 24. Keehner J, Horton LE, Pfeffer MA, et al. SARS-CoV-2 infection after vaccination in health care workers in California. New Engl J Med. 2021;384:1774-1775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ambrosch A, Rockmann F, Klawonn F, Lampl B. Effect of a strict hygiene bundle for the prevention of nosocomial transmission of SARS-CoV-2 in the hospital: a practical approach from the field. J Infect Public Health. 2020;13:1862-1867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kaur R, Weiss TT, Perez A, et al. Practical strategies to reduce nosocomial transmission to healthcare professionals providing respiratory care to patients with COVID-19. Crit Care. 2020;24(1):571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ren J, Yang X, Xu Z, et al. Prevention of nosocomial COVID-19 infections in otorhinolaryngology-head and neck surgery. World J Otorhinolaryngol Head Neck Surg. 2020;6:S6-S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ong SWX, Tan YK, Chia PY, et al. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020;323:1610-1612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Klompas M, Baker MA, Rhee C. Airborne transmission of SARS-CoV-2: theoretical considerations and available evidence. JAMA. 2020;324:441-442. [DOI] [PubMed] [Google Scholar]
- 30. Oran DP, Topol EJ. Prevalence of asymptomatic SARS-CoV-2 infection: a narrative review. Ann Intern Med. 2020;173:362-367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Abbas M, Robalo Nunes T, Martischang R, et al. Nosocomial transmission and outbreaks of coronavirus disease 2019: the need to protect both patients and healthcare workers. Antimicrob Resist Infect Control. 2021;10:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kluytmans-van den Bergh MFQ, Buiting AGM, Pas SD, et al. SARS-CoV-2 infection in 86 healthcare workers in two Dutch hospitals in march 2020. medRxiv. 2020. 2020.03.23.20041913. [Google Scholar]