Many scholars and practitioners have drawn on the theory of syndemics to make sense of the pandemic of coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Horton (2020) suggested in The Lancet that COVID-19 is syndemic rather than pandemic, as did Irons (2020), and others have used vocabulary from the lexicon of syndemics to describe the complex ways in which symptomatic infection with the virus clusters with pre-existing conditions, interacts with other biological processes to amplify disease burden, and moves along established fault lines of society (Gravlee, 2020; Poteat et al., 2020). In some cases, these fault lines have been rooted in social inequalities, such as the circumstances of essential workers who have had to choose between viral or financial risk. This risk was especially poignant for those working in factories, where many outbreaks occurred in the first year of the pandemic and where, in many regions of the world, outbreaks still do occur (Herstein et al., 2021; Taylor et al., 2020). In other cases, the fault lines were steeped in politics, as was acutely apparent in the U.S. and Brazil, where those who believed they were protected from infection—by their race, class, health, or politics—rejected masks, social distancing guidelines, or vaccines (Adolph et al., 2021). In these ways, COVID-19 has become syndemic in different high- and low-income settings.
The syndemic dimensions of COVID-19 differ across contexts. These differences were stark from the beginning of the pandemic when countries like New Zealand and Taiwan shut their borders and focused their resources and communication in line with the carefully defined pandemic preparedness plans at their disposal (Baker et al., 2020; Summers et al., 2020). Other countries, like Rwanda, fostered trust and clarity in quarantine and social behaviors to prevent spread (BMJ, 2020). But as months marched forward, these pandemics changed. At this moment, access to (and belief in the efficacy of) a vaccine plays a powerful role in determining how and where SARS-CoV-2 continues to spread and in determining which populations are at greatest risk in terms of morbidity and mortality. In this way, syndemics differ by region, country, and community—as diseases move in and between people in different ways and for different reasons.
The theory of syndemics is relevant for understanding the pandemic because COVID-19 demonstrates affliction due to both disease concentration and disease interaction driven by harmful social conditions—the central tenets of Singer's (1996) original theory. In his initial proposal, syndemics are stitched together by three rules: two or more diseases cluster together in time or space; these diseases interact in meaningful ways, whether social, psychological, or biological; and harmful social conditions drive these interactions. We designed this Special Issue specifically to address the need for innovative scholarship around how syndemics are measured and therefore understood as locally driven.
Transdisciplinary approaches to studying syndemics have failed to achieve methodological clarity about how diseases “interact”. In a pair of companion papers that leveled the first broadside against methodological incoherence in the empirical literature on syndemics, Tsai and Burns (2015) and Tsai and Venkataramani (2016) demonstrated that researchers in this literature have not successfully accomplished what they set out to achieve (see also the helpful reply by Stall et al., 2015; as well as subsequent refinements by Tsai, 2018; Tsai et al., 2017). This critique has brought the theoretical work of syndemics from anthropology into social epidemiology and public health. To date, engagement across fields has pushed scholars to begin developing novel research approaches for characterizing syndemics and their impacts on wellbeing, making abstract theory actionable and introducing it to concrete practice.
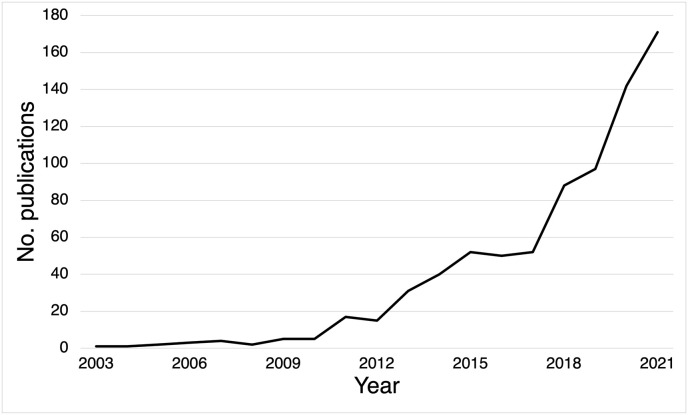
The critical medical anthropologist Merrill Singer first coined the term “syndemic” in the early 1990s while investigating a cluster of substance misuse, violence, and HIV in Hartford, Connecticut (Singer, 1992, 1994, 1996). The earliest publications were, appropriately, limited exclusively to social science journals. In the first decade of scholarship, theory was devoted to understanding what syndemics are in relation to social and medical conditions concurrent with HIV, e.g., Singer (1996, 1994), Singer and Clair (2003), Singer et al. (1992), and Rhodes et al. (2005). Nearly a decade after Singer's initial exposition, behavioral scientist Ron Stall (who was also trained in medical anthropology) and colleagues published what would quickly become a classic in the field of HIV prevention and the most highly cited application of syndemic theory to date (Stall et al., 2003). Nevertheless, the concept of a syndemic was little noticed in the medical literature until the past decade, when interest in this theory increased substantially (Fig. 1 ).
Fig. 1.
Total number of articles related to syndemics in Web of Science through December 10, 2021. The figure represents the yearly count of publications (N = 779) returned from the following Web of Science search: AB=(syndemic or syndemics) or KP = syndemic or AK=(syndemic or syndemics). A similarly expansive PubMed search reveals qualitatively similar trends (N = 883): syndemic [MeSH Terms] OR syndemic [All Fields] OR syndemics [All Fields].
Singer later expanded and historicized scholarship on syndemics in a textbook, Introduction to Syndemics, and in doing so clearly emphasized ecological syndemic models, which he called eco-syndemics (Singer, 2009). Soon after, two book-length analyses were published that attempted to historicize the politics and embodiment of syndemics of metabolic conditions (Marshall, 2013; Mendenhall, 2012). While this move from a primary focus on HIV was significant, the uptick of scholarship on syndemics in disciplines other than anthropology has now come to expand the ways in which the theory of syndemics is used and applied in significant ways. The Lancet Series on syndemics raised the profile of the concept to a broader audience of global health and clinical medicine (Mendenhall, 2017; Mendenhall et al., 2017; Singer et al., 2017; Tsai et al., 2017; Willen et al., 2017). At the same time, there appeared increasingly influential critiques of the empirical approaches to characterizing syndemics that had thus far dominated the field (Chakrapani et al., 2020; Stall et al., 2015; Tomori et al., 2018; Tsai and Burns, 2015; Tsai and Venkataramani, 2016).
This Special Issue provides papers that inform a rigorous rethink about what data and analyses are needed for assessing syndemics, what these data need to capture, and how these data can be described clearly and effectively. The need for this focus on “how” syndemics are characterized is imperative as more scholars draw from the theory of syndemics to inform new interventions, policies, and clinical practice. These papers engage varied epistemological and methodological approaches, with some thinking about the impact, for example, of development interventions on syndemics (Tallman et al., 2020), others focused on innovative uses of network modeling (Brewis et al., 2020), and others located syndemics in historical contexts (Proctor, 2020).
The dialogue with history is in many ways new. That micro- and macro-socioeconomic factors, ecological change, and politics have long shaped past disease burden is not a concept lost on historians of medicine or historical epidemiologists. However, historians have yet to grapple with syndemic theory in a sustained way. Everyone concerned with past health would gain considerably by viewing epidemic clusters through the lens of syndemic theory, where applicable. Histories of disease have long suffered from narrow approaches that consider epidemic and endemic illnesses in isolation. This “disease biography” approach, to which Grmek (1969) offered a partial remedy with his concept of pathocenosis, tends to cast historical populations as suffering diseases discretely or in sequence, as opposed to interconnectedly or concurrently. In identifying the rise and decline of syndemics through time, and establishing contexts and driving forces underlying them, historians stand to gain greatly, as do those already thinking about syndemics, like anthropologists, social epidemiologists, and public health professionals. Naturally, pursuing syndemics in history, both recent and nonrecent, can prove instructive and have ramifications for the present. The Special Issue pushes the syndemic framework into new territory in part by engaging with history, which further underscores the concept's value and hopefully compels more historians to reassess past morbidity and mortality, the assumptions typically made when disease histories are written, and the benefits a syndemic framework provides when conceptualizing health history.
Many papers in this Special Issue have attempted to think innovatively about syndemics, where they sit in the historical record, within families and communities, and how they straddle contexts. Slagboom, Crone, and Reis's (2020) work on syndemic vulnerability in a small fishing village in the Netherlands exposes how syndemics emerge and progress within families and across generations. Tallman et al. (2020) investigate how large development projects, such as dams and roads, produce syndemic effects in the Amazon by causing vector-borne diseases to converge with sex work (and related infections) and the psychological distress of socio-ecological displacement. Kohrt and Carruth (2020) describe how political violence amidst humanitarian emergencies becomes embedded in the body and coexists within interacting multi-morbidities. Sawchuk, Tripp, and Samakaroon (2020), in an example of the needed historical scholarship to which we referred earlier, revisit a mid-nineteenth-century cholera and smallpox syndemic in Gibraltar, identifying how quarantine, overcrowding, and poor sanitation drove morbidity and death. Similarly, Proctor (2020) describes how hazardous labor conditions and environmental constraints caused gastrointestinal diseases to cluster in early-twentieth-century Gabon. A third article in this field illuminates an early-twentieth-century syndemic of hookworm and malaria among plantation workers in British Malaya, revealing colonialism as a driving force of this syndemic in the past (Webb, 2020).
Measuring where and how syndemics emerge was central to our aims for the Special Issue. Doing so requires that scholars translate what “drivers” exist within certain contexts and how they interact with co-occurring medical conditions. Tsai et al. (2017) argued that “the field can achieve more efficient population-level prevention of the disease burden wrought by syndemics if attention is shifted towards elimination of the large-scale forces that condition the distributions of individual-risk factors” but these “analyses have largely gone unmodeled” (p. 981). Modeling such vast upstream factors in relation to disease concentration and disease interaction, however, can be a complex undertaking. Notably, one paper shows that some synergistic relationships are not syndemic, revealing how economic measures may coexist with pathogenic and nutritional risk yet not interact (Hoke and McCabe, 2021); this work emphasizes how disease interactions, within disease concentrations, are critical for understanding syndemics.
A second gap in the literature is occasioned by a major critique of the field—that summing up the associations across variables being used as proxies for syndemics tends to overlook the central tenet of syndemic theory: interaction (Tsai and Burns, 2015; Tsai and Venkataramani, 2016). While this approach “can help to demonstrate that being subjected to multiple psychosocial and structural problems is associated with adverse health outcomes,” as Tsai and Venkataramani (2016) argue, it fails to demonstrate also that “they interact with each other to worsen health outcomes” (p.425, emphasis added). In one response to this argument, Tomori et al. (2018) argue that “the third defining criterion of syndemic theory might be broadened to include cumulative (additive) adversity, rather than solely focusing on synergistic, mutually reinforcing interactions” (p.115). Tomori et al. (2018) further concluded that “closer attention to the cumulative development, underlying causal pathways, and possible synergistic interaction of co-occurring epidemics through combined qualitative and quantitative methodologies may yield more effective interventions for vulnerable, marginalized populations” (p.110). The problem with broadening the concept of a syndemic beyond Singer's original theorization, however, is that while doing so might expand the umbrella of what is considered “syndemic” and, therefore, superficially expand the influence of syndemic theory, it may also rob the nomenclature of its explanatory power. As Tsai and Venkataramani (2016) showed mathematically, the “cumulative adversity” conceptualization adds very little to the simple multivariable regression model.
Tsai (2018) distilled current scholarship on syndemics into a simple typology. First, synergistically interacting epidemics, in which there is a departure from additivity in the adverse effects of two or more epidemics. This is the classic “syndemic” described, with numerous examples, by Singer and Clair (2003). Second, mutually causal epidemics, in which two or more epidemics feed each other. Singer (1996) also described this arrangement as a “syndemic.” Third, serially causal epidemics, in which one epidemic leads to a second (potentially with cumulative adverse effects), and then to a third. While Singer's original expositions did not describe this arrangement as a “syndemic,” many subsequent applications of his theory have done so. And fourth, the “cumulative adversity” model described above, which Singer and Clair (2003) explicitly described as not providing insight into syndemic interaction. While Tsai (2018) is sometimes misinterpreted as elaborating a typology of syndemics (Hayran and Ataç, 2019), he does no such thing; he simply describes various arrangements of co-occurring epidemics—some thought to be syndemic and others not—even while some have, as described above, argued for expanding the notion of what constitutes a syndemic.
Others have suggested a primary focus on social and structural drivers, with less of an emphasis on what constitutes syndemic interaction. In such a world, the need for syndemic theory is unclear. We already have more established theoretical frameworks of social and structural determinants (Berkman et al., 2014; Link and Phelan, 1995) and intersectionality (Collins, 2019; Mullings, 2002; Schulz and Mullings, 2006); without disease interaction, then any of these more parsimonious frameworks would be sufficient to explain disease co-occurrence and clustering. This critique was emphasized in a commentary in the Special Issue (Sangaramoorthy and Benton, 2021). Sangaramoorthy and Benton (2021) critique two papers in the Special Issue that emphasize how crucial understanding intersectional drivers of clustered health conditions is for identifying syndemics and potentially mitigating upstream factors that produce them (Kline, 2020, Quinn, 2019). The original authors responded in agreement that one should not equate syndemics with intersectionality, but rather learn from, engage with, and use intersectional framing in biosocial context (Kline, 2021, Quinn, 2021). Yet, none of these papers address the contours of biological interaction and population dynamics, which are two of the three central tenets of syndemic theory. Relatedly, a second fundamental confusion for the field is that labeling all these configurations of co-occurring epidemics as “syndemic” would render the construct, and its attendant implications for intervention, unintelligible.
In this Special Issue, we aimed to highlight the diversity of methods for characterizing syndemics. Special Issue authors take different approaches for characterizing syndemics in history (Proctor, 2020; Sawchuk et al., 2020; Slagboom et al., 2020; Newfield, 2021), syndemic interactions (Boateng et al., 2020; Hatcher et al., 2019; Himmelgreen et al., 2020; Saxena and Mendenhall, 2020; Snodgrass et al., 2019), syndemics in different communities (Brewis et al., 2020; Weaver and Kaiser, 2020), syndemics resulting from development or humanitarian interventions (Kohrt and Carruth, 2020; Tallman et al., 2020), and clinical interventions (Chakrapani et al., 2020). Additional contributions leverage spatial methods to understand the relations between environmental context and disease clustering and disease co-occurrence (Brazil, 2021, Shrestha et al., 2020).
In a study of the substance use, HIV, and violence (SAVA) syndemic among men residing in a peri-urban settlement near Johannesburg, South Africa, Hatcher et al. (2019) found that alcohol misuse, gender inequitable views, intimate partner violence perpetration, and HIV transmission risk behaviors were pervasive. They assessed the co-occurrence of these variables and found evidence to suggest that these variables interacted synergistically in their impacts on HIV transmission risk behavior. Further, building on the example of Chakrapani et al. (2019), they tested a structural equation model specifying gender inequity as the structural driving force behind alcohol misuse and violence against women, both of which then led in the final pathway to HIV transmission risk behavior.
Others have innovatively used mixed methods to interrogate complex distinctions in synergistic interactions between otherwise similar communities, using qualitative methods to explain population-level differences. This is exemplified by the Brewis et al. (2020) application of the “risk environments” concept by Rhodes et al. (2005), in which social and physical factors localize through syndemic processes, or what they call “syndemic localization”, to evaluate how certain synergistic features influence mental and physical health outcomes differently across contexts. To achieve this, they draw from two different datasets and epistemologies to create a novel analysis of how the consequences of chronic social inequality (crime, hunger, and discrimination) drive health disparities across three very low-resource—but quite different—communities in Haiti. They used quantitative data (surveys) to understand differences in “exposure” across communities and text data analysis to “show the nuance, context, and local embeddedness of core themes as they emerged from respondents’ own words” (p. 3). They then used a semantic network analysis to understand how people spoke about, and therefore experienced, these driving features of distress, thereby revealing how small communities within a relatively limited geographic area can experience syndemic localization very differently. How people think through and make evident what these interactions look like, and what they do, have the potential to make a big impact on how understanding the drivers of syndemics can influence upstream policy and interventions to mitigate the downstream effects.
Community interventions are critical. For instance, community support groups, mental health interventions, investment in community projects, and elevating the cultural, political, and social priorities of people and communities can play a role in mitigating the effects of syndemics on people's health. For example, Kohrt and Carruth (2020) describe how they shifted an exclusively trauma-based treatment for returning child soldiers to one that targeted discrimination and social exclusion, through “activities such as reducing discrimination by teachers in schools directed toward former girl soldiers” (p.5) and creating opportunities for these girls to pursue myriad activities to plan for their futures, from scholarly to technical (e.g., seamstress) and livelihood programs (e.g., raising livestock) (Kohrt et al., 2015; Kohrt and Carruth, 2020). Similarly, Reed and Miller (2016) recommend that effective mitigation of the SAVA syndemic requires addressing both structural drivers of oppression as well as fostering family acceptance, community involvement, and social activism.
This Special Issue puts some innovative epistemologies and methodologies on the table. The methodological and theoretical responses to the critiques that have been raised will be imperative to moving our understanding of syndemics (and hence the utility of the concept) forward. This agenda will require transdisciplinary teams of scholars working together to understand where, when, how, and why conditions move together within one population, region, or area more virulently than another. This phenomenon was exemplified by COVID-19 and will only intensify with changes in climate and emerging infectious diseases.
The papers in this Special Issue share a common theme in their empirical research: the importance of understanding how diseases emerge, interact, and change through time. While each paper makes a contribution to its own discipline, perhaps more importantly, this collection of articles represents the most diverse set of methodologically and analytically varied thinking about how syndemics produce disparate health problems in some populations and not others. Taken together, these studies provide a comprehensive view of how syndemics emerge, converge, and change, and what are the best methods to measure these interactions.
References
- Adolph C., Amano K., Bang-Jensen B., Fullman N., Wilderson J. Pandemic politics: timing state-level social distancing responses to COVID-19. J. Health Polit. Pol. Law. 2021;46(2):211–233. doi: 10.1215/03616878-8802162. [DOI] [PubMed] [Google Scholar]
- Baker M., Wilson N., Anglemyer A. Successful elimination of covid-19 transmission in New Zealand. N. Engl. J. Med. 2020;383(e56) doi: 10.1056/NEJMc2025203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkman L.F., Kawachi I., Glymour M.M. Social Epidemiology. second ed. Oxford University Press; New York: 2014. [Google Scholar]
- BMJ Rwanda's secret weapon against COVID-19: Trust. BMJ. 2020;371 doi: 10.1136/bmj.m4720. [DOI] [PubMed] [Google Scholar]
- Boateng G.O., Workman C.L., Miller J.D., Onono M., Neilands T.B., Young S.L. The syndemic effects of food insecurity, water insecurity, and HIV on depressive symptomatology among Kenyan women. Soc. Sci. Med. 2020:113043. doi: 10.1016/j.socscimed.2020.113043. In this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brazil N. The multidimensional clustering of health and its ecological risk factors. Soc. Sci. Med. 2021:113772. doi: 10.1016/j.socscimed.2021.113772. In this issue. [DOI] [PubMed] [Google Scholar]
- Brewis A., Wutich A., Galvin M., Lachaud J. Localizing syndemics: a comparative study of hunger, stigma, suffering, and crime exposure in three Haitian communities. Soc. Sci. Med. 2020:113031. doi: 10.1016/j.socscimed.2020.113031. In this issue. [DOI] [PubMed] [Google Scholar]
- Chakrapani V., Kaur M., Tsai A.C., Newman P.A., Kumar R. The impact of a syndemic theory-based intervention on HIV transmission risk behaviour among men who have sex with men in India: pretest-posttest non-equivalent comparison group trial. Soc. Sci. Med. 2020:112817. doi: 10.1016/j.socscimed.2020.112817. In this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakrapani V., Lakshmi P.V.M., Tsai A.C., Vijin P.P., Kumar P., Srinivas V. The syndemic of violence victimisation, drug use, frequent alcohol use, and HIV transmission risk behaviour among men who have sex with men: cross-sectional, population-based study in India. SSM Popul. Health. 2019;7(April):100348. doi: 10.1016/j.ssmph.2018.100348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins P.H. Intersectionality as Critical Social Theory. Duke University Press; Durham: 2019. [Google Scholar]
- Gravlee C.C. Systemic racism, chronic health inequities, and COVID-19: a syndemic in the making? Am. J. Hum. Biol. 2020;32(5):e23482. doi: 10.1002/ajhb.23482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grmek M. Préliminaires d’une étude historique des maladies. Ann. Hist. Sci. Soc. 1969;24(6):1473–1483. [Google Scholar]
- Hatcher A.M., Gibbs A., McBride R.S., Rebombo D., Khumalo M., Christofides N.J. Gendered syndemic of intimate partner violence, alcohol misuse, and HIV risk among peri-urban, heterosexual men in South Africa. Soc. Sci. Med. 2019:112637. doi: 10.1016/j.socscimed.2019.112637. In this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayran O., Ataç Ö. Syndemics or synergistic epidemics. J. Health Syst. Policies. 2019;1(3):174–188. https://dergipark.org.tr/en/pub/jhesp/issue/50952/642042 [Google Scholar]
- Herstein J., Degarege A., Stover D., Austin C., Schwedhelm M., Lawler J., Lowe J., Ramos A., Donahue M. Characteristics of SARS-CoV-2 transmission among meat processing workers in Nebraska, USA, and effectiveness of risk mitigation measures. Emerg. Infect. Dis. 2021;27(4):1032–1039. doi: 10.3201/eid2704.204800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himmelgreen D., Romero-Daza N., Heuer J., Lucas W., Salinas-Miranda A.A., Stoddard T. Using syndemic theory to understand food insecurity and diet-related chronic diseases. Soc. Sci. Med. 2020:113124. doi: 10.1016/j.socscimed.2020.113124. In this issue. [DOI] [PubMed] [Google Scholar]
- Hoke M., McCabe K.A. Malnutrition, illness, poverty, and infant growth: a test of a syndemic hypothesis in Nuñoa, Peru. Soc. Sci. Med. 2021:113720. doi: 10.1016/j.socscimed.2021.113720. In this issue. [DOI] [PubMed] [Google Scholar]
- Horton R. Offline: COVID-19 is not a pandemic. Lancet. 2020;396(10255):874. doi: 10.1016/S0140-6736(20)32000-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irons R. Pandemic ... or syndemic? Re-framing COVID-19 disease burden and ‘underlying health conditions’. Soc. Anthropol. 2020 doi: 10.1111/1469-8676.12886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohrt B.A., Carruth L. Syndemic effects in complex humanitarian emergencies: a framework for understanding political violence and improving multi-morbidity health outcomes. Soc. Sci. Med. 2020:113378. doi: 10.1016/j.socscimed.2020.113378. In this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline N. Syndemic statuses: Intersectionality and mobilizing for LGBTQ+ Latinx health equity after the Pulse shooting. Soc. Sci. Med. 2020:113260. doi: 10.1016/j.socscimed.2020.113260. In this issue. [DOI] [PubMed] [Google Scholar]
- Kline N. Response to commentary by Sangaramoorthy and Benton. Soc. Sci. Med. 2021:113786. doi: 10.1016/j.socscimed.2021.113786. In this issue. [DOI] [PubMed] [Google Scholar]
- Kohrt B.A., Burkey M., Stuart E.A., Koirala S. Alternative approaches for studying humanitarian interventions: propensity score methods to evaluate reintergration packages impact on depression, PTSD, and function impairment among child soldiers in Nepal. Glob. Ment. Health (Camb) 2015;2:e16. doi: 10.1017/gmh.2015.1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link B., Phelan J. Social conditions as fundamental causes of disease. J. Health Soc. Behav. 1995;35(Extra Issue):80–94. [PubMed] [Google Scholar]
- Marshall M. Drinking Smoke: the Tobacco Syndemic in Oceania. University of Hawai’i Press; Honolulu: 2013. [Google Scholar]
- Mendenhall E. Syndemic Suffering: Social Distress, Depression, and Diabetes among Mexican Immigrant Women. Left Coast Press; Walnut Creek: 2012. [Google Scholar]
- Mendenhall E. Syndemics: a new path for global health research. Lancet. 2017;389:889–891. doi: 10.1016/S0140-6736(17)30602-5. [DOI] [PubMed] [Google Scholar]
- Mendenhall E., Kohrt B., Norris S., Ndetei D., Prabhakaran D. Non-communicable disease syndemics: poverty, depression, and diabetes among the urban poor. Lancet. 2017;389:951–963. doi: 10.1016/S0140-6736(17)30402-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullings L. The sojourner syndrome: race, class, and gender in health and illness. Voices. 2002;6(1):32–36. [Google Scholar]
- Newfield T. Syndemics and the history of disease: towards a new engagement. Soc. Sci. Med. 2021:114454. doi: 10.1016/j.socscimed.2021.114454. In this issue. [DOI] [PubMed] [Google Scholar]
- Poteat T., Millett G., Nelson L., Beyrer C. Understanding COVID-19 risks and vulnerabilities among black communities in America: the lethal force of syndemics. Ann. Epidemiol. 2020;47(July):1–3. doi: 10.1016/j.annepidem.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proctor D.A. Testing the waters: syndemic gastrointestinal distress in Lambaréné, Gabon, 1926–1932. Soc. Sci. Med. 2020:113405. doi: 10.1016/j.socscimed.2020.113405. In this issue. [DOI] [PubMed] [Google Scholar]
- Quinn K.G. Applying an intersectional framework to understand syndemic conditions among young Black gay, bisexual, and other men who have sex with men. Soc. Sci. Med. 2019:112779. doi: 10.1016/j.socscimed.2019.112779. In this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn K.G. The relationship between syndemics and intersectionality: A response to the commentary by Sangaramoorthy and Benton. Soc. Sci. Med. 2021:113784. doi: 10.1016/j.socscimed.2021.113784. In this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed S.J., Miller R.L. Thriving and adapting: resilience, sense of community, and syndemics among young black gay and bisexual men. Am. J. Community Psychol. 2016;57(1–2):129–143. doi: 10.1002/ajcp.12028. [DOI] [PubMed] [Google Scholar]
- Rhodes T., Singer M., Bourgois P., Friedman S.R., Strathdee S.A. The social structural production of HIV risk among injecting drug users. Soc. Sci. Med. 2005;61(5):1026–1044. doi: 10.1016/j.socscimed.2004.12.024. [DOI] [PubMed] [Google Scholar]
- Sangaramoorthy T., Benton A. Intersectionality and syndemics: A commentary. Soc. Sci. Med. 2021:113783. doi: 10.1016/j.socscimed.2021.113783. In this issue. [DOI] [PubMed] [Google Scholar]
- Sawchuk L.A., Tripp L., Samakaroon M. Assessing a syndemic: Gibraltar in the time of cholera. Soc. Sci. Med. 2020:112956. doi: 10.1016/j.socscimed.2020.112956. In this issue. [DOI] [PubMed] [Google Scholar]
- Saxena A., Mendenhall E. Syndemic thinking in large-scale studies: case studies of disability, hypertension, and diabetes across income groups in India and China. Soc. Sci. Med. 2020:113503. doi: 10.1016/j.socscimed.2020.113503. In this issue. [DOI] [PubMed] [Google Scholar]
- Schulz A.J., Mullings L. Gender, Race, Class & Health: Intersectional Approaches. Jossey-Bass; San Francisco: 2006. [Google Scholar]
- Singer M. A dose of drugs, a touch of violence, a case of AIDS: conceptualizing the SAVA syndemic. Free Inq. Creativ. Sociol. 1996;24(2):99–110. [Google Scholar]
- Singer M., Bulled N., Ostrach B., Mendenhall E. Syndemics and the biosocial conception of health. Lancet. 2017;389:941–950. doi: 10.1016/S0140-6736(17)30003-X. [DOI] [PubMed] [Google Scholar]
- Shrestha S., Bauer C.X.C., Hendricks B., Stopka T.J. Spatial epidemiology: An empirical framework for syndemics research. Soc. Sci. Med. 2020:113352. doi: 10.1016/j.socscimed.2020.113352. In this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer M.C. AIDS and the health crisis of the U.S. urban poor: the perspective of critical medical anthropology. Soc. Sci. Med. 1994;39(7):931–948. doi: 10.1016/0277-9536(94)90205-4. [DOI] [PubMed] [Google Scholar]
- Singer M.C. Introduction to Syndemics: A Systems Approach to Public and Community Health. Jossey-Bass; San Francisco: 2009. [Google Scholar]
- Singer M.C., Clair S. Syndemics and public health: reconceptualizing disease in bio-social context. Med. Anthropol. Q. 2003;17(4):423–441. doi: 10.1525/maq.2003.17.4.423. [DOI] [PubMed] [Google Scholar]
- Singer M., Valentín F., Baer H., Jia Z. Why does Juan García have a drinking problem? The perspective of critical medical anthropology. Med. Anthropol. 1992;14(1):77–108. doi: 10.1080/01459740.1992.9966067. [DOI] [PubMed] [Google Scholar]
- Slagboom M.N., Crone M.R., Reis R. Exploring syndemic vulnerability across generations: a case study of a former fishing village in The Netherlands. Soc. Sci. Med. 2020:113122. doi: 10.1016/j.socscimed.2020.113122. In this issue. [DOI] [PubMed] [Google Scholar]
- Snodgrass J.G., Lacy M.G., Cole S.W. Internet gaming, embodied distress, and psychosocial well-being: a syndemic-syndaimonic continuum. Soc. Sci. Med. 2019:112728. doi: 10.1016/j.socscimed.2019.112728. In this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stall R., Mills T.C., Williamson J., Hart T., Greenwood G., Paul J., Pollack L., Binson D., Osmond D., Catania J.A. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am. J. Public Health. 2003;93(6):939–942. doi: 10.2105/AJPH.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stall R., Coulter R.W.S., Friedman M.R., Plankey M.W. Commentary on “Syndemics of psychosocial problems and HIV risk: a systematic review of empirical tests of the disease interaction concept” by A. Tsai and B. Burns. Soc. Sci. Med. 2015;145:129–131. doi: 10.1016/j.socscimed.2015.07.016. [DOI] [PubMed] [Google Scholar]
- Summers J., Cheng H., Lin H., Barnard L., Kvalsvig A., Wilson N., Baker M. Potential lessons from the Taiwan and New Zealand health responses to the COVID-19 pandemic. Lanc. Reg. Health West. Pac. 2020;4:100044. doi: 10.1016/j.lanwpc.2020.100044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tallman P.S., Riley-Powell A.R., Schwarz L., Salmón-Mulanovich G., Southgate T., Pace C., Valdés-Velásquez A., Hartinger S.M., Paz-Soldán V.A., Lee G.O. Ecosyndemics: the potential synergistic health impacts of highways and dams in the Amazon. Soc. Sci. Med. 2020:113037. doi: 10.1016/j.socscimed.2020.113037. In this issue. [DOI] [PubMed] [Google Scholar]
- Taylor C., Boulos C., Almond D. Livestock plants and COVID-19 transmission. Proc. Natl. Acad. Sci. Unit. States Am. 2020;117(50):31706–31715. doi: 10.1073/pnas.2010115117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomori C., McFall A.M., Solomon S.S., Srikrishnan A.K., Anand S., Balakrishnan P., Mehta S.H., Celentano D.D. Is there synergy in syndemics? Psychosocial conditions and sexual risk among men who have sex with men in India. Soc. Sci. Med. 2018;206:110–116. doi: 10.1016/j.socscimed.2018.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai A.C. Syndemics: a theory in search of data or data in search of a theory? Soc. Sci. Med. 2018;206:117–122. doi: 10.1016/j.socscimed.2018.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai A.C., Burns B.F.O. Syndemics of psychosocial problems and HIV risk: a systematic review of empirical tests of the disease interaction concept. Soc. Sci. Med. 2015;139(Aug):26–35. doi: 10.1016/j.socscimed.2015.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai A.C., Mendenhall E., Trostle J.A., Kawachi I. Co-occurring epidemics, syndemics, and population health. Lancet. 2017;389(10072):978–982. doi: 10.1016/S0140-6736(17)30403-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai A.C., Venkataramani A.S. Syndemics and health disparities: a methodological note. AIDS Behav. 2016;20(2):423–430. doi: 10.1007/s10461-015-1260-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver L.J., Kaiser B.N. Syndemics theory must take local context seriously: an example of measures for poverty, mental health, and food insecurity. Soc. Sci. Med. 2020:113304. doi: 10.1016/j.socscimed.2020.113304. In this issue. [DOI] [PubMed] [Google Scholar]
- Webb J.L.A., Jr. Syndemic anemia in British Malaya: An early global health encounter with hookworm and malaria co-infections in plantation workers. Soc. Sci. Med. 2020:113555. doi: 10.1016/j.socscimed.2020.113555. In this issue. [DOI] [PubMed] [Google Scholar]
- Willen S.S., Knipper M., Abadia-Barrero C., Davidovitch N. Syndemic vulnerability and the right to health. Lancet. 2017;389:964–977. doi: 10.1016/S0140-6736(17)30261-1. [DOI] [PubMed] [Google Scholar]