Abstract
Introduction
Preoperative computed tomography (CT)-guided localization is commonly employed to facilitate video-assisted thoracoscopic surgery (VATS)-guided diagnostic wedge resection of pulmonary nodules (PNs).
Aim
The present meta-analysis was conducted with the goal of better evaluating the feasibility, safety, and clinical efficacy of preoperative CT-guided localization for multiple PNs (MPNs).
Material and methods
PubMed, Embase, and the Cochrane Library databases were reviewed in order to identify all relevant studies published as of June 2020. Random effects modeling was then used to evaluate the pooled data. The meta-analysis was conducted using Stata v12.0 software.
Results
Eight relevant studies were identified for inclusion in the present meta-analysis. In total, 345 patients with 799 PNs were treated with preoperative CT-guided localization and subsequent wedge resection. The overall pooled technical success rate based on the nodules and patients was calculated to be 97% (95% confidence interval (CI): 0.94–0.99) and 92% (95% CI: 0.86–0.97), respectively. The overall pooled incidence rate of complications was calculated to be 40% (95% CI: 0.16–0.63). Significant heterogeneity was observed among the studies for all the parameters described above (I2 = 74.5%, 77.7%, and 96.3%, respectively). No significant differences were detected in the technical success of localization and incidence of complications between coil and hook-wire groups. The risk of publication bias in the reporting of technical success rate of localization based on both nodules and patients was found to be high (p < 0.001 and < 0.001, respectively).
Conclusions
Preoperative CT-guided localization may be effective in guiding VATS-guided wedge resection in patients with MPNs.
Keywords: computed tomography, lung nodule, multiple, localization
Introduction
Preoperative computed tomography (CT)-guided localization is commonly employed to facilitate video-assisted thoracoscopic surgery (VATS)-guided diagnostic wedge resection of pulmonary nodules (PNs), achieving high rates of successful localization (89.6–100%) and wedge resection (97–100%), with an acceptable rate of complications (8.8–12.6%) [1–3]. Localization methods usually involve methylene-blue, hook-wire, coils, and radio-labeling agents [1–7]. Relative to cases without localization, preoperative localization can significantly decrease the need for thoracotomy or VATS anatomical resection when diagnosing PNs [4].
Preoperative CT-guided localization of PNs has a number of advantages over other methods and is widely used for patients with multiple PNs (MPNs) [8–15]. Several groups have reported their experiences of one-stage localization for MPNs [12, 14, 15]. However, variability in the technical success of such localization has been reported, with studies employing different localization methods (methylene blue, hook-wire, or coils) reporting success rates of anywhere between 88% and 100% [8–15]. There is a similar degree of variability in the reported complication rates (13–90%) [8–15]. As such, there is a clear need for other large-scale studies with large datasets to more accurately evaluate the feasibility and safety of preoperative CT-guided localization for MPNs.
Aim
The present meta-analysis was conducted with the goal of better evaluating the feasibility, safety, and clinical efficacy of preoperative CT-guided localization for MPNs.
Material and methods
Study selection
PubMed, Embase, and the Cochrane Library databases were searched for all relevant articles published up to June 2020, using the following search strategy: ((localization[Title/Abstract]) AND (nodule[Title/Abstract])) AND (multiple[Title/Abstract]).
Only studies that satisfied the following criteria were included in the review: (a) studies specifically focused on preoperative CT-guided localization (including staining materials, hook-wire, coil, and radio-label localization) for PNs; (b) patients with MPNs; (c) the diameter of each PN ≤ 30 mm; and (d) studies should report the technical success of CT-guided localization.
Studies were excluded if they were: (a) case reports (only 1–3 cases); (b) conference abstracts; (c) non-human studies; or (d) reviews.
Data extraction
Two investigators independently extracted data from all studies; the corresponding author asked to resolve any discrepancies that arose. Baseline data, demographic information, and treatment-related data were extracted from all studies.
Quality assessment
All studies identified for inclusion in the present meta-analysis had a non-randomized design. Their quality was evaluated using the Newcastle–Ottawa scale [16]. Any study with a score ≥ 5 was deemed to be of high quality [16].
Endpoints
The endpoints of this meta-analysis included the technical success of localization, technical success of wedge resection, and localization-related complications.
MPNs were defined as the number of PNs > 1. Technical failure of localization was defined as the surgeon being unable to visualize the localized materials [9]. When the localization device was dislodged it was also considered a technical failure. Wedge resection was considered to be successful if the target nodule was identified in the wedge-shaped lung tissue [15].
Meta-analysis
Stata v12.0 software was used to conduct the present meta-analysis. Owing to presumed heterogeneity, a random-effects model was used to calculate the pooled results, with weighting applied according to the inverse variance of the included studies, where heterogeneity was assumed. Heterogeneity of the studies was evaluated using the Q test and measured using the I2 statistic, with I2 > 50% indicative of substantial heterogeneity. Subgroup analysis was used to investigate sources of heterogeneity. P-value < 0.05 was the threshold of significance. Egger’s regression asymmetry test was used to evaluate the risk of publication bias.
Results
Study characteristics
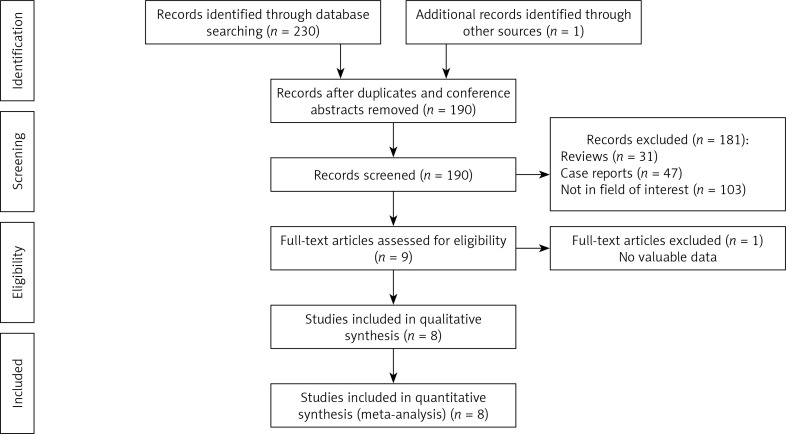
In the initial literature search, 231 studies that were potentially relevant to the present analysis were identified. Of these, 8 were ultimately included in the final meta-analysis. Full details of the study selection process are presented in Figure 1.
Figure 1.
Flowchart of the meta-analysis
The overall characteristics of the studies included in the present meta-analysis are shown in Table I. All studies included in the review were retrospective, with scores on the Newcastle-Ottawa scale in the range 6–8. In total, 345 patients with 799 PNs were treated with preoperative CT-guided localization and subsequent wedge resection. In four studies, coil localization was used [11, 12, 14, 15], hook-wire localization was used in 3 [8, 10, 13], and one used methylene-blue localization [9]. The characteristics of the procedures are presented in Table II.
Table I.
Characteristics of studies included in the meta-analysis
| Study | Year | Country | Number of patients | Number of nodules | Mean age [years] | Newcastle–Ottawa score |
|---|---|---|---|---|---|---|
| Iguchi [8] | 2015 | Japan | 35 | 80 | 59.9 | 8 |
| Tseng [9] | 2016 | Taiwan | 100 | 217 | 59.9 | 6 |
| Kadeer [10] | 2018 | China | 76 | 194 | 55 | 8 |
| Li [11] | 2018 | China | 51 | 126 | 58.9 | 8 |
| Fu [12] | 2019 | China | 19 | 43 | 56.3 | 6 |
| Sun [13] | 2019 | China | 16 | 34 | 47 | 6 |
| Teng [14] | 2020 | China | 31 | 68 | 55 | 8 |
| Yang [15] | 2020 | China | 17 | 37 | Not given | 6 |
Table II.
Characteristics of procedures
| Study | Mean lesion size | Localized materials | TS of localization (per nodule) | TS of localization (per patient) | TS of wedge resection (per nodule) | TS of wedge resection (per patient) | Complication rate |
|---|---|---|---|---|---|---|---|
| Iguchi [8] | 0.8 cm | Hook-wire | 96% | 91% | Not given | Not given | 90% |
| Tseng [9] | 0.8 cm | Methylene blue | 99% | 98% | 100% | 100% | 55% |
| Kadeer [10] | 0.7 cm | Hook-wire | 88% | 72% | 96% | 85% | 64% |
| Li [11] | 0.8 cm | Coil | 96% | 90% | Not given | Not given | 24% |
| Fu [12] | 0.7 cm | Coil | 98% | 95% | 100% | 100% | 16% |
| Sun [13] | 0.7 cm | Hook-wire | 100% | 100% | 100% | 100% | 13% |
| Teng [14] | 0.7 cm | Coil | 99% | 97% | 100% | 100% | 13% |
| Yang [15] | 0.9 cm | Coil | 97% | 94% | 100% | 100% | Not given |
TS – technical success.
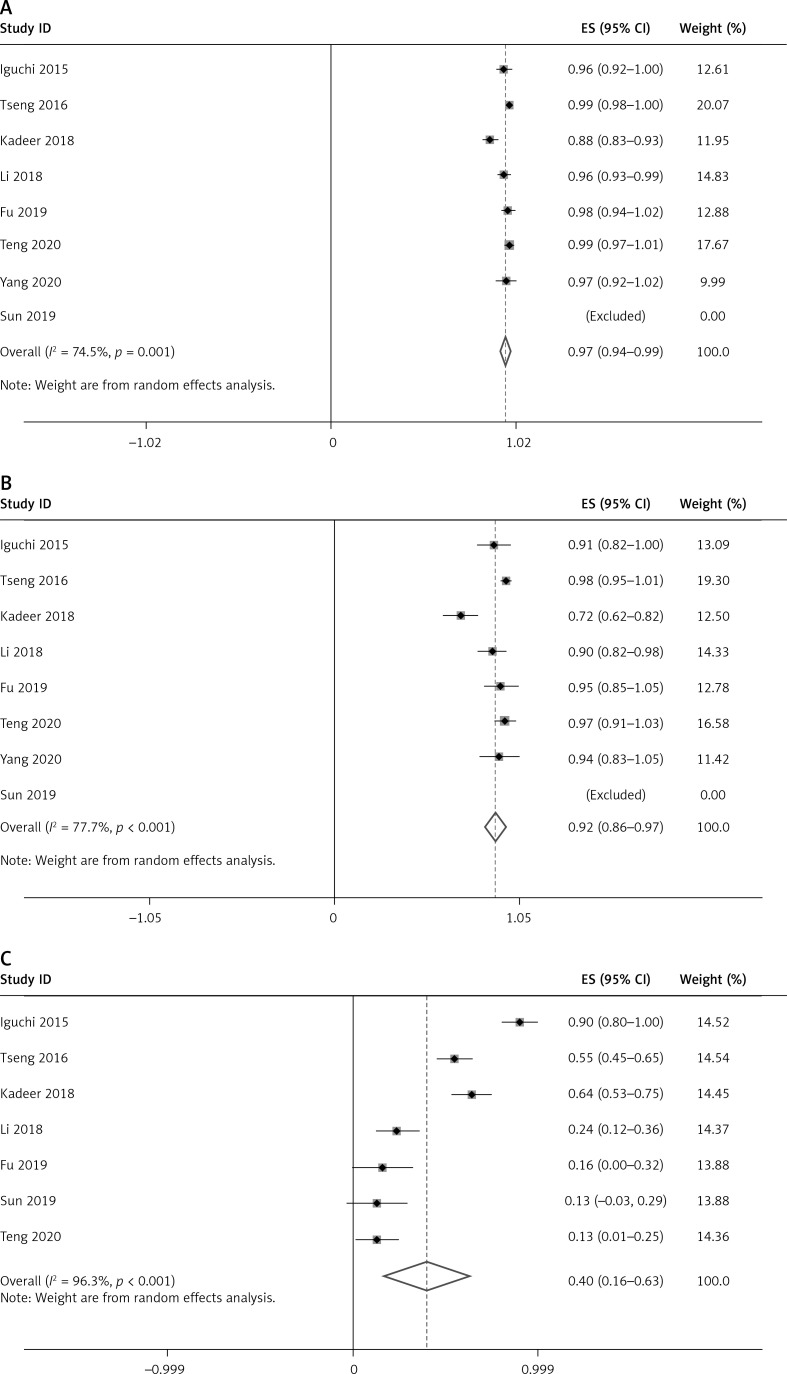
Technical success of localization
Data pertaining to the technical success of localization were reported in all studies, and calculated in relation to both nodules and patients. The overall pooled technical success rate based on nodules was calculated to be 97% (95% confidence interval (CI): 0.94–0.99, Figure 2 A). Significant heterogeneity was detected among these studies (I2 = 74.5%, p = 0.001). The overall pooled technical success rate based on patients was calculated to be 92% (95% CI: 0.86–0.97, Figure 2 B), also with significant heterogeneity among the studies (I2 = 77.7%, p = 0.000).
Figure 2.
Forest plots of the technical success rate of localization (based on PNs) (A) Technical success rate of localization (based on patients) (B) and complication rate (C)
Technical success of wedge resection
The technical success of wedge resection was reported in 6 studies [9, 10, 12–15]. However, because 5 of those studies reported a technical success rate for wedge resection of 100% [9, 12–15], it was not possible to pool the results.
Complications
The complication rate was reported in 7 studies [8–14]. The overall pooled complication rate was calculated to be 40% (95% CI: 0.16–0.63, Figure 2 C). Significant heterogeneity was detected among the studies (I2 = 96.3%, p < 0.001).
Subgroup analysis
Subgroup analysis was then conducted for each endpoint variable for the different localization techniques (Table III). Only one study used methylene blue localization [9] and so it was excluded from the subgroup analysis. No significant differences were found in the technical success of localization and the incidence of complications between coil and hook-wire groups.
Table III.
Subgroup analyses
| Variable | TS of localization (per nodule) | TS of localization (per patient) | Complication rate |
|---|---|---|---|
| Total | 97% | 92% | 40% |
| Localized materials: | |||
| Coil | 98% | 95% | 18% |
| Hook-wire | 92% | 82% | 56% |
| P-value | 0.104 | 0.117 | 0.163 |
TS – technical success.
Publication bias
Publication bias analysis suggested that the risk of such bias relating to the reported complication rate was low (p = 0.351). In contrast, the risk of publication bias pertaining to the reported technical success rate of localization based on both nodules and patients was found to be high (p < 0.001 and 0.001, respectively).
Discussion
In the present meta-analysis, the feasibility, safety, and clinical efficacy of preoperative CT-guided localization for MPNs were evaluated. The overall results of our analysis were relatively positive, with a pooled technical success rate of 97% and 92%, respectively, for localization in PN- and patient-based analyses. These results may indicate that it is feasible to simultaneously localize MPNs in a single-stage procedure. However, significant heterogeneity was also detected and it might decrease the reliability of the conclusion. The source of heterogeneity may come from the following factors: (a) all included studies are retrospective in nature; and (b) the included studies used different localized materials. Subgroup analysis demonstrated that the technical success rate for localization was not significantly different for coil and hook-wire groups. These results possibly indicate that the preoperative technical success of localization was not influenced by localization method. Although the study of Tseng et al. [9] was not included in the subgroup analysis due to the use of methylene blue, the technical success rates of localization in PN- and patient-based analyses were 99% and 98%, respectively. Nevertheless, further meta-analysis which focuses on one unique localized material is still required.
The reasons for technical failure using the different localization methods differ. The failure of methylene blue localization was due principally to its diffusive nature [2, 9]. The failure of hook-wire localization was due to it becoming dislodged while coils were occasionally inserted into the lung parenchyma causing the loss of intra-operative localization function [1]. Recently, Zhang et al. [17] reported their clinical experience of computed tomography in combination with intraoperative noninvasive percutaneous ultrasonic localization of PNs with a high technical success rate of 95.6%. Intraoperative ultrasound can provide real-time localization. However, this technique may not localize the MPNs simultaneously.
Although the pooled localization technical success rate was more than 90%, the raw data of the studies included in the review indicated that the majority of studies had a 100% technical success for wedge resection [9, 12–15]. VATS-guided wedge resection was usually initially performed following preoperative localization [18]. If localization failed, wedge resection could be performed on tissue identified by palpation of the nodule or coil [1, 9, 12, 14, 15]. Therefore, wedge resection was possible even if preoperative localization failed, although this resulted in wasted surgical time. Fu et al. [12] and Teng et al. [14] found that preoperative CT-guided multiple coil localization could be used to guide single-stage VATS diagnostic wedge resection in patients with MPNs.
Some researchers also performed simultaneous VATS for PNs and synchronous mediastinal/esophageal lesions [1, 19]. Under this condition, if the PNs were metastatic lesions or presented with ground-glass PNs, only wedge resection was enough [1, 18]. Therefore, preoperative CT-guided localization should be performed for such patients to increase the technical success rate of wedge resection.
In the meta-analysis, the pooled complication rate was 40%. This rate is higher than that reported in previous studies (24–29%) regarding preoperative localization for a single PN [11, 20]. It seems reasonable that localization-related complications occurred more frequently in patients with MPNs. However, the significant heterogeneity still requires further trials to confirm this conclusion. Subgroup analysis revealed that the complication rate in the coil group was lower than in the hook-wire group, although not significantly so (18% vs. 56%, p = 0.163). This may be as a result of the limited number of studies. A previous study of coil vs. hook-wire localization for PNs indicated that the total complication rate was lower in the coil group (25% vs. 54%, p = 0.04) [21]. Further meta-analysis which compares the clinical effectiveness between different localized materials is required. Although the pooled complication rate was high in this meta-analysis, the majority of studies reported that most localization-related complications did not influence the subsequent VATS-guided resection procedure [1, 9, 12, 14, 15].
There are a number of limitations to the present meta-analysis. Firstly, all studies included in the analysis were retrospective. In addition, we detected significant heterogeneity in the pooled results. Some variability may be attributable to the many potential confounding variables or covariates not reported in the manuscripts, such as operator experience, the direction of approach, or needle tract depth. Furthermore, the meta-analysis included a variety of different localization methods, thus potentially biasing the results of technical success and complication rate analysis.
Conclusions
The results of the present meta-analysis suggest that preoperative CT-guided localization may be used effectively to guide VATS wedge resection in patients with MPNs. The use of a coil may decrease localization-related complications. Further meta-analysis which focuses on one unique localized material is still required.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Fu YF, Zhang M, Wu WB, et al. Coil localization-guided video-assisted thoracoscopic surgery for lung nodules. J Laparoendosc Adv Surg Tech A. 2018;28:292–7. doi: 10.1089/lap.2017.0484. [DOI] [PubMed] [Google Scholar]
- 2.Gruber-Rouh T, Naguib NNN, Beeres M, et al. CT-guided hook-wire localisation prior to video-assisted thoracoscopic surgery of pulmonary lesions. Clin Radiol. 2017;72:898.e7–8.e11. doi: 10.1016/j.crad.2017.05.015. [DOI] [PubMed] [Google Scholar]
- 3.Zhang ZD, Wang HL, Liu XY, et al. Methylene blue versus coil-based computed tomography-guided localization of lung nodules. Thorac Cardiovasc Surg. 2020;68:540–4. doi: 10.1055/s-0040-1708836. [DOI] [PubMed] [Google Scholar]
- 4.Finley RJ, Mayo JR, Grant K, et al. Preoperative computed tomography-guided microcoil localization of small peripheral pulmonary nodules: a prospective randomized controlled trial. J Thorac Cardiovasc Surg. 2015;149:26–31. doi: 10.1016/j.jtcvs.2014.08.055. [DOI] [PubMed] [Google Scholar]
- 5.Iguchi T, Hiraki T, Gobara H, et al. Transfissural route used for preoperative localization of small pulmonary lesions with a short hook wire and suture system. Cardiovasc Intervent Radiol. 2015;38:222–6. doi: 10.1007/s00270-014-0862-9. [DOI] [PubMed] [Google Scholar]
- 6.Xia FF, Shi YB, Wang T, et al. Computed tomography-guided transfissural coil localization of lung nodules. Thorac Cardiovasc Surg. 2020;68:545–8. doi: 10.1055/s-0039-1695759. [DOI] [PubMed] [Google Scholar]
- 7.Lin MW, Tseng YH, Lee YF, et al. Computed tomography-guided patent blue vital dye localization of pulmonary nodules in uniportal thoracoscopy. J Thorac Cardiovasc Surg. 2016;152:535–44.e2. doi: 10.1016/j.jtcvs.2016.04.052. [DOI] [PubMed] [Google Scholar]
- 8.Iguchi T, Hiraki T, Gobara H, et al. Simultaneous multiple preoperative localizations of small pulmonary lesions using a short hook wire and suture system. Cardiovasc Intervent Radiol. 2015;38:971–6. doi: 10.1007/s00270-014-1028-5. [DOI] [PubMed] [Google Scholar]
- 9.Tseng YH, Lee YF, Hsieh MS, et al. Preoperative computed tomography-guided dye injection to localize multiple lung nodules for video-assisted thoracoscopic surgery. J Thorac Dis. 2016;8(Suppl 9):S666–71. doi: 10.21037/jtd.2016.09.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kadeer X, Wang L, Zhang L, et al. Modified hook-wire placement technique for localizing multiple pulmonary nodules. J Surg Oncol. 2018;118:1188–93. doi: 10.1002/jso.25261. [DOI] [PubMed] [Google Scholar]
- 11.Li F, Chen Y, Bian J, et al. Preoperative computed tomography-guided microcoil localization for multiple small lung nodules before video-assisted thoracoscopic surgery. Zhongguo Fei Ai Za Zhi. 2018;21:857–63. doi: 10.3779/j.issn.1009-3419.2018.11.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fu YF, Gao YG, Zhang M, et al. Computed tomography-guided simultaneous coil localization as a bridge to one-stage surgery for multiple lung nodules: a retrospective study. J Cardiothorac Surg. 2019;14:43. doi: 10.1186/s13019-019-0870-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sun W, Zhang L, Wang L, et al. Three-dimensionally printed template for percutaneous localization of multiple lung nodules. Ann Thorac Surg. 2019;108:883–8. doi: 10.1016/j.athoracsur.2019.03.060. [DOI] [PubMed] [Google Scholar]
- 14.Teng F, Wu AL, Yang S, et al. Preoperative computed tomography-guided coil localization for multiple lung nodules. Ther Adv Respir Dis. 2020;14:1753466620909762. doi: 10.1177/1753466620909762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang ZJ, Liang YH, Li M, et al. Preoperative computed tomography-guided coil localization of lung nodules. Minim Invasive Ther Allied Technol. 2020;29:28–34. doi: 10.1080/13645706.2019.1576053. [DOI] [PubMed] [Google Scholar]
- 16.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 17.Zhang Q, Wang Z, Jiang Y, et al. The application value of computed tomography in combination with intraoperative noninvasive percutaneous ultrasonic localisation of subpleural pulmonary nodules/ground-glass opacity in uniportal video-assisted thoracoscopy. Videosurgery Miniinv. 2020 doi: 10.5114/wiitm.2020.101238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhong L, Hu W, Li S, et al. Clinical study of video-assisted thoracoscopic surgery wedge resection in early-stage lung cancer by tumor mapping with indocyanine green. Videosurgery Miniinv. 2019;14:545–50. doi: 10.5114/wiitm.2019.89986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zeng L, Zhuang R, Tu Z. Simultaneous uniportal video-assisted thoracic surgery for pulmonary nodules and synchronous mediastinal lesions. Videosurgery Miniinv. 2020 doi: 10.5114/wiitm.2020.101240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen S, Zhou J, Zhang J, et al. Video-assisted thoracoscopic solitary pulmonary nodule resection after CT-guided hookwire localization: 43 cases report and literature review. Surg Endosc. 2011;25:1723–9. doi: 10.1007/s00464-010-1502-3. [DOI] [PubMed] [Google Scholar]
- 21.Rostambeigi N, Scanlon P, Flanagan S, et al. CT fluoroscopic-guided coil localisation of lung nodules prior to video-assisted thoracoscopic surgical resection reduces complications compared to hook wire localization. J Vasc Interv Radiol. 2019;30:453–9. doi: 10.1016/j.jvir.2018.10.013. [DOI] [PubMed] [Google Scholar]