Abstract
Environmental health indicators are helpful for tracking and communicating complex health trends, informing science and policy decisions, and evaluating public health actions. When provided on a national scale, they can help inform the general public, policy makers, and public health professionals about important trends in exposures and how well public health systems are preventing those exposures from causing adverse health outcomes. There is a growing need to understand national trends in exposures and health outcomes associated with climate change and the effectiveness of climate adaptation strategies for health. To date, most indicators for health implications of climate change have been designed as independent, individual metrics. This approach fails to take into account how exposure-outcome pathways for climate-attributable health outcomes involve multiple, interconnected components. We propose reframing climate change and health indicators as a linked system of indicators, which can be described as follows: upstream climate drivers affect environmental states, which then determine human exposures, which ultimately lead to health outcomes; these climate-related risks are modified by population vulnerabilities and adaptation strategies. We apply this new conceptual framework to three illustrative climate-sensitive health outcomes and associated exposure-outcome pathways: pollen allergies and asthma, West Nile Virus infection, and vibriosis.
Keywords: Climate change, health, public health, indicators, indicator system, framework
1. BACKGROUND
Climate change poses one of the most significant challenges to human health around the world (Costello et al. 2009). Given this level of importance, as well as the inherent complexity of the interactions between climate change and health (Haines and Ebi 2019; Tong and Ebi 2019; Watts et al. 2018; Pachauri 2014), there is an urgent need to monitor trends in climate change related exposures and health outcomes. This in turn requires enhanced data collection for monitoring and surveillance (Watts et al. 2015) to build the evidence base for collective understanding of the causal links between climate change and health and to better support public health action and decision making.
Effective public health practice is built upon the collection and interpretation of data on health status, health hazards and their root causes, and community needs and assets (CDC 2020). Establishing baseline status, evaluating trends, and analyzing successes and failures of public health interventions requires the development of useful, robust public health indicators. Indicators are signals of phenomena that often cannot be directly measured or seen (Briggs 2003). Indicators are summary measures that describe complex systems and track and communicate the state of such systems (English et al. 2009). They provide valuable long-term data to: 1) guide prevention strategies, interventions, and health services; 2) evaluate public health policies; and 3) form the basis of health communications for disseminating information to stakeholders (English et al. 2009). The use of a consistent set of indicators allows for comparison of phenomena over time and across geographic scales.
Traditional environmental and health indicators have tended to be conceptualized and collected as independent metrics, uncoupled from other factors in the causal pathway and detached from risk modifiers (Ebi et al. 2018; McMichael 2013). For many environmental health effects, such as those related to asbestos or lead, the relationship between exposure and outcome is relatively direct and straightforward, so independent indicators are useful for understanding exposures and trends in outcomes. Climate change, in contrast, is a complex exposure, one of several determinants of downstream health effects, and thus a greater challenge in terms of assessing impacts on health outcomes (Xun et al. 2010; Ebi 2008; Wilkinson et al. 2003; Hess et al.). The 2016 Climate and Health Assessment published by the U.S. Global Change Research Program (GCRP) describes this complexity through multi-step exposure pathways that include contextual measures representing additional environmental, social, and behavioral determinants of health (Crimmins et al. 2016).
For a number of health outcomes, such as heat-related mortality, there is a high degree of attribution to a climate-related factor. Current surveillance systems capture most deaths for which heat exposure is identified as an underlying or contributing cause on the death certificate (Vaidyanathan et al. 2020), and there is a relatively robust evidence base for associations between climate change related factors like frequency of heat waves and health outcomes. For such health outcomes as heat, it should therefore be possible to create a more complete indicator system that includes causal factors, modifying factors, and trends in outcomes. For other health outcomes, such as asthma or many infectious diseases, the degree of attribution and even the precise climate-related causative factors may not be fully known, and the health outcomes may not be adequately captured by current surveillance systems. Collecting spatially and temporally relevant data along the causal chain, as well as modifiers, is critical to establish evidence of trends in climate and health outcomes, elucidate the climate-attributable portion of the association, and identify which demographic and societal factors modify the exposure-outcome pathway (Wilkinson et al. 2003). Nonetheless, it may be possible to identify some components in the causal pathway and begin to present indicators for these outcomes with more complex or uncertain causal pathways in a linked manner. While such a systematic approach to indicators may initially be incomplete or exploratory, it may then also help to identify knowledge and data gaps (Beard 2016; Luber and McGeehin 2008; Haines et al. 2006; Rogers and Randolph 2006).
1.1. Building on Prior Indicator Efforts
A number of federal agencies and national organizations independently produce collections of indicators relevant to climate change and health at the national level, including the Centers for Disease Control and Prevention (CDC), Environmental Protection Agency (EPA), National Oceanic and Atmospheric Administration (NOAA), and U.S. Global Change Research Program (GCRP) (Table 1). CDC maintains a database of climate change and health indicators, primarily at the county scale, on their Environmental Public Health Tracking platform. Beyond climate-sensitive health outcomes, the platform features indicators for climate and environmental exposures and underlying vulnerabilities. In addition to collecting primary climate and environmental data that are used to develop indicators by other agencies such as CDC, NOAA maintains a small set of health-relevant indicators. EPA uses data collected by its own agency as well as external organizations to produce an inventory of climate and environmental indicators and a handful of health outcome indicators. GCRP hosts and manages a selection of indicators related to climate. The Council of State and Territorial Epidemiologists (CSTE) and the U.S. Department of Agriculture (USDA) both have put forth recommendations for climate change indicators that are relevant for their discipline but have not created or collected indicators. In all cases, climate and health indicators are not presented as linked along causal pathways or combined with specific vulnerability factors or adaptation metrics.
Table 1.
Data repositories for climate or climate change and health indicators, which can include exposure, health, or adaptation indicators. Repositories may house indicators from other external agencies.
| Indicator Repository (agency and categorya) | Component in Frameworkb | |||||
|---|---|---|---|---|---|---|
| CD | ES | PE | HO | PV | AS | |
| CDC | ||||||
| Air quality | X | X | ||||
| Asthma | X | |||||
| Climate change (cross-cutting) | X | X | X | X | ||
| COPD | X | |||||
| Drought | X | |||||
| Heart disease | X | |||||
| Heat stress illness | X | |||||
| Populations and vulnerabilities/community characteristics | X | |||||
| EPA | ||||||
| Ecosystems | X | X | ||||
| Greenhouse gases | X | |||||
| Health and society | X | X | ||||
| Oceans | X | X | ||||
| Snow and ice | X | X | ||||
| Weather and climate | X | X | ||||
| NOAA | ||||||
| Temperature, precipitation, and drought | X | X | ||||
| Extremes | X | X | ||||
| Societal impacts | X | X | ||||
| Snow and ice | X | |||||
| Teleconnections | X | |||||
| USGCRP | X | X | ||||
CDC: Centers for Disease Control and Prevention;
EPA: Environmental Protection Agency;
NOAA: National Oceanic and Atmospheric Administration;
USGCRP: U.S. Global Change Research Program
CD: climate driver; ES: environmental state; PE: proximate exposure; HO: health outcome; PV: population vulnerability; AS: adaptation strategies.
Indicators are identified at the higher-level category and may include multiple sub-categories of measures.
At least one of the measures in the category of indicators has relevance to human health exposure pathways.
Prior conceptual frameworks used to guide environmental assessments and sustainable development have grouped indicators with underlying causal connections (Table 2). The Driving Force-Pressure-State-Impact-Response (DPSIR) model builds on the original Pressure-State-Response (Rapport and Friend 1979; OECD 1993), introducing upstream driving forces that impose pressures on the environment and consequently change the state of the environment. These effects can lead to impacts on human health or ecosystems and shape societal responses that can in turn influence each link within the causal chain (EEA 1999). This framework has provided a useful systems-based approach to informing environmental indicator selection, but because it does not explicitly consider human exposures and is primarily focused on environmental impacts (Hambling, Weinstein, and Slaney 2011; Niemeijer and de Groot 2008), it is not as applicable for climate change impacts on health.
Table 2.
Comparison of frameworks.
| Features of the Framework | Framework | ||||
|---|---|---|---|---|---|
| DPSIR | DPSEEA | MEME | NCIS | ICCHIS | |
| Adaptable for climate change impacts | X | X | X | X | |
| Based on a causal framework | X | X | X | X | |
| Describes upstream and downstream factors | X | X | X | X | |
| Provides route of exposure | X | X | X | ||
| Includes interventions or adaptations | X | X | X | X | X |
| Incorporates sociodemographic vulnerabilities along the causal chain | X | ||||
DPSIR: Driving force–Pressure–State–Impact–Response; DPSEEA: Drivers–Pressures–State–Exposure–Effect–Action; MEME: Multiple Exposures–Multiple Effects; NCIS: National Climate Indicator System; ICCHIS: Integrated Climate Change and Health Indicator System
Adapted from Hambling 2011
The World Health Organization (WHO) conceptualized the Drivers-Pressures-State-Exposure-Effect; Action (DPSEEA) model as a way to guide indicator development and environmental policies that impact human health outcomes (Corvalán, Kjellström, and Smith 1999; Kjellström and Corvalán 1995). Similar to previous models, the DPSEEA shares the same upstream driving forces, pressures, and states concepts. Differences appear subsequent to these steps that emphasize human exposures: changes in environmental state can generate exposures to environmental hazards that lead to health effects, and across the entire framework, actions can be implemented to influence each step.
In discussing frameworks for indicators of children’s environmental health, Briggs noted the DPSEEA framework posed a risk of simplifying causal chains into single linear pathways and proposed instead the Multiple Exposures-Multiple Effects (MEME) framework might be more suitable for complex systems (Briggs 2003). Notably, the MEME framework explicitly incorporates contexts that can include socioeconomic and demographic vulnerability factors as well as preventive and remedial actions, which map well to climate mitigation and adaptation. However, there is an overall lack of distinction between upstream and downstream elements.
Hambling et al. reviewed eleven frameworks that could be applied to climate change and health indicators, including the DPSIR, DPSEEA, and MEME frameworks (Hambling, Weinstein, and Slaney 2011). They considered the DPSEEA framework as providing the best starting point for an integrated system of indicators for climate change and health, noting that by explicitly acknowledging the linkages among ecological and environmental states and human health, it is possible to direct interventions early in the causal chain to not only protect human health, but also in some cases, to preserve ecological integrity. In fact, around 2001, the WHO put forth the idea of adapting the DPSEEA conceptual framework to climate change and human health (Füssel and Klein 2004). More recently, the DPSEEA framework has been adapted for climate change and health issues, such as in New South Wales, Australia, to guide appropriate public health actions (Boylan et al. 2018). Challenges with the DPSEEA framework include incorporating non-climate factors into the causal chain and characterizing causal pathways with multiple sequential ecological steps (Füssel and Klein 2004).
Although not explicitly framed around causal relationships, the concept of a National Climate Indicator System was introduced in 2016 with climate change as a focal point and represented as a “system of physical, natural, and societal indicators that communicate and inform decisions about key aspects of the physical climate, climate impacts, vulnerabilities, and preparedness” (Kenney, Janetos, and Lough 2016). Kenney et al. later proposed a framework and rationale for a system of national climate indicators to provide a mechanism for sustained climate assessment (Kenney, Janetos, and Gerst 2018). Within this framework, health is conceptualized as a central factor influenced by climate and ecosystem drivers as well as adaptation strategies. While the authors do not identify any specific indicators, they list categories of health indicators that align closely with the exposure pathways used in this paper, include population vulnerability indicators, and also recommend expanding existing indicator systems with indicators of responses. They, however, do not propose groups of linked indicators to represent each exposure-outcome pathway.
2. THE CONCEPTUAL FRAMEWORK
2.1. Introduction
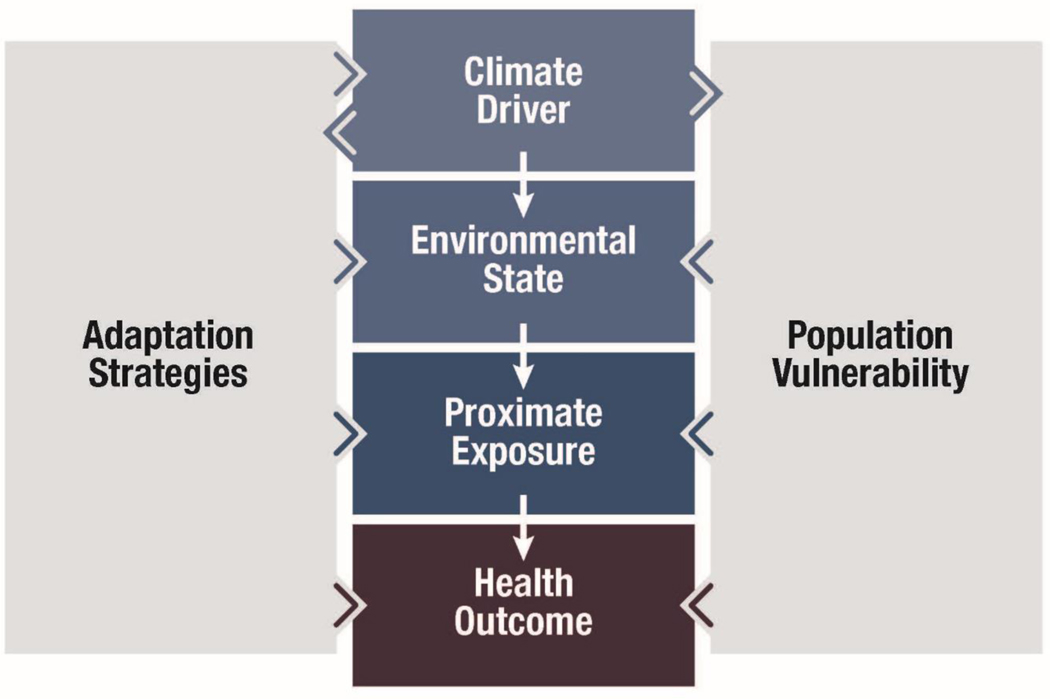
In order to create a comprehensive, integrated indicator system that captures not only the critical components of causal pathways but also quantifiable metrics of vulnerability and adaptation responses, we propose a new conceptual framework for a national Integrated Climate Change and Health Indicator System (Figure 1). This system of impact indicators combines elements of the DPSEEA and MEME frameworks, placing multi-step causal chains associated with climate change within a context of socioeconomic and demographic factors, societal actions, and other non-climate drivers. The components of our indicator system align closely with the exposure pathways concept of the 2016 GCRP Climate and Health Assessment (Crimmins et al. 2016) but add consideration of societal actions related to adaptation that were deliberately excluded from the framing of the report. While there are other important relationships between climate change and health, such as the health benefits of certain climate change mitigation actions, the framework presented in this paper focuses on capturing trends important to the health impacts of climate change and efforts to ameliorate those impacts.
Figure 1.
Conceptual diagram of the Integrated Climate Change and Health Indicator System Framework
For the purposes of our proposed indicator system, climate drivers include the climatological and meteorological conditions that cause downstream environmental and ecosystem changes. Environmental states refer to the status of the environment or ecosystem created influenced by upstream climatological and meteorological factors. Proximate exposures include environmental and biological factors that, when humans come in contact with them, affect human health by directly causing disease or injury. Health outcomes are illnesses or injuries resulting from such contact with biological, physical, or chemical substances in the environment. Population vulnerabilities encompass socioeconomic or demographic factors that render populations susceptible to health effects from climate change. Adaptation strategies are the actions developed or implemented to improve outcomes in response to the adverse effects of climate change and can reflect aspects of community resilience.
One goal of applying this systems approach to developing climate change and health indicators is to facilitate a “virtuous circle” of science whereby integration of exposure-outcome pathways, vulnerability factors, and societal responses leads to: 1) early identification of gaps in either scientific understanding of linkages or collection of data that are relevant to proposed linkages; 2) development of indicators of human health vulnerability that are most relevant to specific pathways; 3) association of societal responses with specific exposure pathways, and therefore specific environmental states and health outcomes, by which to measure the effectiveness of those societal responses; and 4) evaluation of gaps and trends that informs ongoing research in an iterative manner. We propose that integrating related factors in this way will lead to more relevant and accurate understanding of what is working well, what is not working, and the extent to which existing efforts to manage health risks are robust and effective. This systems approach will help to identify the most critical data for sustained observation and surveillance in order to track climate change impacts on human health in the US.
2.2. Selection of Exposure-Outcome Pathways
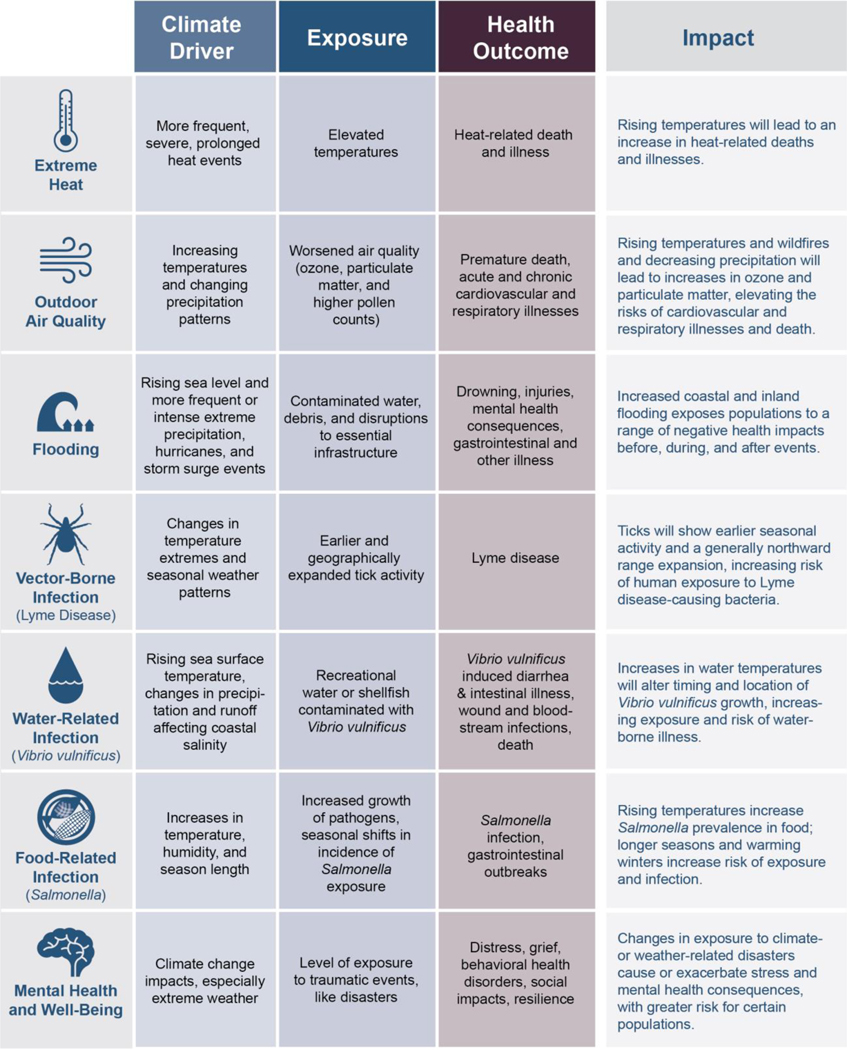
An initial question to consider is which exposure-outcome pathways should be included in a national set of climate and human health indicators. We propose as a starting point including exposure-outcome pathways for the major health outcomes mentioned in the 2016 GCRP Climate and Health Assessment and the Fourth National Climate Assessment (Crimmins et al. 2016; Reidmiller et al. 2018). Taken from the Climate and Health Assessment Executive Summary, Figure 2 provides a useful basis for identifying some of the potential indicators along the causal pathways for the seven different pathways listed. Some of the exposure-outcome pathways are categories, like water-borne and vector-borne diseases, that may have several important sub-pathways not included in the figure. For example, while Figure 2 identifies Lyme disease as an important vector-borne disease, it does not include other important vector-borne diseases in the United States such as West Nile virus (WNV) infection.
Figure 2.
Exposure pathways diagram illustrating examples of climate impacts on human health from the 2016 U.S. Global Change Research Program Climate and Health Assessment
2.3. Selection of Indicators
Previous authors have identified selection criteria for environmental health indicators (Hambling, Weinstein, and Slaney 2011; Briggs 2003). For our framework, we use as a starting point the selection criteria highlighted by Briggs, which fall into two categories: scientific validity and utility/practicability (Briggs 2003). In the absence of easy quantification of selection criteria, expert judgment is often used to score, rank, and weigh the various criteria. Initial sets of indicators for each exposure pathway can be adapted from the discussion of climate linkages in major assessments and reports, including those from the GCRP (Reidmiller et al. 2018; Crimmins et al. 2016) and Intergovernmental Panel on Climate Change (Pachauri 2014).
The complex exposure-outcome pathways involved in the health impacts of climate change complicate the process of selecting the most appropriate indicators. Specific climate drivers for a given exposure pathway may vary in time and space. For example, the literature suggests that for South Dakota, relative humidity and precipitation variations are key predictors of high-risk areas for WNV, while for coastal California, warmer temperatures are critical predictors of transmission risk (Skaff et al. 2020; Hess, Davis, and Wimberly 2018). Moreover, the factors most important for predicting variations in risk over finer time and space scales, for example, predicting high-risk counties in a state over a time period of weeks, may not be the most relevant for assessing longer term trends in infectious disease risk related to climate change (Hess, Davis, and Wimberly 2018). As a consequence, tradeoffs among selection criteria are necessary. Indicators most useful for understanding and communicating national-scale trends may not be the same factors that are useful for predicting disease risk on a time and spatial scale relevant to public health interventions. Similarly, given the many potential ways to process primary meteorological observations to develop critical climate driver measures, it is likely that ongoing research may identify similar but slightly different specific drivers for the various exposure pathways. In designing a national system of indicators for a comprehensive set of exposure pathways, there are likely to be tradeoffs between specificity and optimal scientific validity of upstream drivers and the criteria of practicality, understandability, and parsimony.
3. THE INDICATOR SYSTEM FRAMEWORK: THREE EXAMPLES
We present the application of the conceptual framework to three distinct climate-related health outcomes, allergies related to pollen, West Nile virus (WNV) infections, and Vibrio sp. infections as illustrative examples of how this conceptual framework may be used in practice. Primarily using indicators that are currently available from federal agencies, we identify indicators for these three exposure-outcome pathways that could comprise the elements of an Integrated Climate and Health Indicator System Framework. These examples are for descriptive purposes only; an actual initial set of pilot indicators would be selected through a more robust and inclusive process.
3.1. Allergies and Other Respiratory Conditions
Allergies and other respiratory conditions related to pollen have been associated with changes in climate (Barnes 2018). Warming temperatures, shifts in precipitation, and increasing concentrations of carbon dioxide affect plant growth and phenology (Ziska et al. 2019; Katelaris and Beggs 2018; Anenberg et al. 2017; Behrendt and Ring 2012). The pathway of data from exposure to outcome begins with the main (a) climate drivers of increasing surface temperatures, shifts in precipitation, and rising carbon dioxide levels, which shape various (b) environmental states, including earlier flowering and longer pollen seasons. These changing environmental states in turn affect the magnitude and frequency of (c) proximate exposures, such as the quantity and species of pollen grains in the air, which impact (d) human health through allergic disease or by exacerbating existing respiratory conditions like asthma (Katelaris and Beggs 2018); (e) population vulnerabilities such as age and existing morbidities and (f) adaptation strategies such as enhanced environmental monitoring (Katelaris and Beggs 2018) implemented at the local or more macro level play a role in modifying the linkage between exposure and outcome.
Potential initial indicator set
Climate drivers: CO2 concentration; national average surface temperature (wintertime)
Environmental state: first day of flowering in selected regions
Proximate exposures: peak oak pollen counts in selected regions; oak pollen season length
Health outcomes: asthma mortality; asthma and allergic disease-related hospitalizations; asthma and allergic disease-related emergency room visits
Vulnerability factor: pre-existing conditions
Adaptation strategy: early warning/pollen surveillance systems
3.2. West Nile Virus Infection
As a vector-borne disease, WNV infection is sensitive to climate and weather factors. Climate change affects both spatial and temporal patterns in human WNV cases because the transmission cycle involves stages of mosquito development and bird migration patterns that are vulnerable to climate and environment factors (Beard 2016). These factors also influence human behavior outdoors, which influences the likelihood of exposure and infection. A linked indicator system can help associate upstream climate factors and downstream health outcomes and capture at least some of the critical variables and mechanics involved in WNV disease transmission. Starting from the main (a) climate drivers of precipitation levels increasing surface temperatures, the pathway continues to the (b) environmental states, areas of standing water and birds infected with the virus, that are generated by these driving forces (Paull et al. 2017; Paz 2015; Paz and Semenza 2013). These environments create amenable habitats for downstream (c) proximate exposures like the vector index of infected mosquitoes, that in turn infect both bird populations and humans, causing the ultimate (d) health outcome, WNV infection, in individuals (Paz and Semenza 2013). In addition to climate and environmental factors, certain (e) population vulnerabilities, including age and outdoor occupation, and (f) adaptation strategies such as vector control programs and public health communication campaigns act within the system to modify WNV exposure and infection in the population.
Potential initial indicator set
Climate drivers: national average surface temperature (wintertime); soil moisture anomalies; precipitation anomalies
Environmental states: satellite derived images of standing water; anomalies from 30-year average
Proximate exposures: Culex mosquito counts; infected sentinel animals; date of first sentinel animal infection; annual prevalence of WNV disease in mosquitoes; annual prevalence of WNV disease in sentinel species
Health outcome: WNV neuroinvasive disease cases
Vulnerability factors: population over 65; percentage outdoor worker
Adaptation strategy: integrated pest management strategy
3.3. Vibriosis
Changes in climate have been shown to affect the distribution and proliferation of bacteria causing vibriosis (i.e., Vibrio and related groups) and cholera (Vibrio cholerae) in humans (Semenza et al. 2012; Vezzulli, Colwell, and Pruzzo 2013; Vezzulli et al. 2016). The main (a) climate drivers include rising sea surface temperatures for Vibrio exposures and infection and, in the case of cholera, heavy precipitation, which could include extreme weather events. These factors affect the (b) environmental state of the pathogen, leading to variations in concentrations of Vibrio bacteria, including potentially virulent subpopulations (Ebi et al. 2017; Semenza et al. 2012; Vezzulli, Colwell, and Pruzzo 2013). People are (c) exposed to these pathogens through ingestion when they consume raw or undercooked seafood containing high levels of these bacteria, via dermal contact through wounds or broken skin, or through eye and ear contact with contaminated water during recreational activities. This contact increases the risk of exposure and adverse (d) health outcomes such as vibriosis resulting in gastrointestinal illness, dermal infections, or eye and ear infections, conditions that may be modified by (e) population vulnerabilities including age and the presence of underlying chronic disease conditions in infected individuals; (f) an adaptation strategy such as monitoring of the seafood supply could also modulate risk (Tacket, Brenner, and Blake 1984).
Potential initial indicator set
Climate drivers: national average surface temperature; sea surface temperature; extreme precipitation
Environmental states: sea surface temperature anomalies; sea surface temperatures exceeding minimum thresholds (15oC); duration at temperatures above 15oC
Proximate exposure: Vibrio concentrations in selected sentinel estuaries
Health outcome: Vibrio illnesses
Vulnerability factors: age (over 50 and under 15); gender (male); immune status; liver conditions
Adaptation strategy: Vibrio early warning systems
4. DISCUSSION
This framework for a national Integrated Climate and Health Indicator System is intended to advance the understanding of trends in the human health impacts of climate change, inform data collection and surveillance strategies, and guide, as well as evaluate, public health actions. Over the long run, the development and refinement of indicator systems will benefit a number of audiences. First and foremost, the general public and policy makers will have greater understanding of the importance of health as an area of climate change impacts. Public health professionals will have a more robust foundation for data-driven guidelines and policies related to climate change and human health. Researchers will have a clearer sense of knowledge gaps. And data stewards will have greater support for maintenance and expansion of specific earth observation parameters and health surveillance data for public health purposes.
By establishing a linked system of indicators based on current understanding of exposure pathways and linkages, the framework provides a structured template within which to expand our collective understanding of climate change and its impacts on human health. While health outcome indicators may change over time from a wide variety of factors, consideration of linked indicators along causal pathways aids in the interpretation of health trends in the context of potential influences of climate change and secondary environmental changes. As additional data and research results are incorporated, the system can be refined and modified to reflect up-to-date knowledge. For example, the relationships between phenology and asthma exacerbations are just being explored in the United States (Sapkota et al. 2020). Whereas prior indicators focused on pollen season length, the finding that both late and early onset of phenologic spring are associated with increased asthma hospitalizations would suggest that an indicator of anomalies of phenology, and not just earlier onset, would be important to include. Moreover, while remotely sensed phenology provides a proxy of pollen concentrations in the absence of a national pollen monitoring network, advances in automated pollen sampling using drones may lead to the ability to incorporate more precise exposure measures over time. In this example, as in all cases, a balance will need to be struck between revisions in the face of scientific advances and the need for continuous, unchanging indicator definitions in order to delineate trends over time. For an area of science as critical and yet relatively immature as climate change and human health, identifying some sets of indicators as clearly developmental or as pilots, could help to strike this balance.
The complex nature of indicator systems necessitates the involvement of experts across multiple disciplines, from climate scientists and meteorological specialists, to biologists and infectious disease experts, to epidemiologists and public health practitioners. Because the Integrated Climate Change and Health Indicator System Framework attempts to capture the connections linking climate drivers to environmental states to proximate exposures and eventual health outcomes, as well as population vulnerabilities and adaptation strategies, relevant data sets are required for all these components. Consequently, coordination is key across earth observation systems and biological and health surveillance systems. Specialists in their respective fields are needed to provide their expertise to identify the most appropriate data sets, interpret the data and uncertainties, evaluate existing or create new indicators, and establish linkages throughout the exposure-outcome pathways. For some pathways, such as those for vector-borne diseases, ongoing research may reveal that the heterogeneity of ecosystems and primary drivers of disease risk around the country preclude national-scale linked indicators. In such cases, national scale modeling of vector range and niches may be the best proxy available. It may still be useful for local public health departments to track more localized, smaller-scale indicators of risk drivers of vector-borne diseases to guide their own efforts. Organizations that fund or provide services related to earth observing systems, biological monitoring system, and health surveillance systems should find that an integrated framework such as proposed in this paper provides enhanced guidance and justification for their missions.
Applying this framework will require a combination of vetting existing indicators, developing new indicators from existing datasets, and in some cases, awaiting or promoting the collection of new data. For example, CDC currently hosts datasets containing climate-sensitive disease incidence and prevalence at the county level (CDC 2021). It would be relatively straightforward to aggregate a national scale indicator from the county-level data for these diseases. Other types of indicators, such as trends in infectious disease vectors or various types of pollen concentrations, do not currently have robust sustained datasets to support them and would require more development of the monitoring data.
Building a national system of indictors presents an additional, particularly challenging scenario. Variation in the scope and scale of data (e.g., climate data on a kilometer grid at a daily timescale but health data available at the county level on a monthly timescale) may make it difficult to connect indicators. The current landscape of the health system is fragmented across the federal, state, local, and Tribal levels, which complicates data collection, validation of health outcomes of interest, and linkage of health data at the appropriate temporal and spatial levels to earth observation data. Identifying the appropriate temporal and geospatial scales for the indicator system will depend on the specific exposure-outcome pathway. In some cases, such as waterborne or vector-borne diseases that are more influenced by regional conditions, indicators may need to be presented as collections of localized data; in others, such as extreme heat-related illnesses, national summative measures may be suitable.
Taking a systems approach to climate change and human health indicators should facilitate more effective public health practice and more actionable public communications. By combining a comprehensive, multi-step model of exposure-outcome pathways with metrics of population vulnerability and societal interventions, a more complete picture of current risk levels and trends over time can emerge. This allows assessment of health status in a more robust risk context and helps identify the most salient driving forces and opportunities for refinements in public health protection. At the same time, organizing indicators as a holistic, multifactorial system instead of as individual indicators is a novel concept and may present challenges in communicating information. Thus, significant attention needs to be paid not only to the scientific evidence supporting linking indicators in this way, but also to the communication science and development of useful messages to describe the indicators from a systems perspective.
Transitioning from indicators as individual metrics to interconnected systems may present some unique logistical challenges. Initiating and sustaining partnerships may be difficult because there may be competing agency priorities across the institutions that are collecting data and generating indicators. Such discrepancies in priorities could hinder the process of merging data streams for an indicator system, providing data updates, or even coordinating collaborative activities. Tracking climate change indicators as a system can be a resource-intensive approach, and there might be limitations in terms of time, personnel, and money for sustained efforts. Privacy concerns related to health data and data security are not unique to an indicator systems framework. The issue, however, is further complicated within this context because of the multi-disciplinary nature inherent to a system of indicators. Data stewards of health-related indicators have established security protocols for safeguarding their data inventories, but the question of where and how to securely maintain a repository of indicators developed from health and non-health data is more complex.
5. CONCLUSION
Climate change has direct and indirect impacts on population health, and indicator systems are useful for capturing the complex relationships among upstream climate and downstream health effects while incorporating potential modifying vulnerabilities and adaptation strategies. This proposed Integrated Climate and Health Indicator System Framework provides a structure to try to capture the complex dynamics that define a climate-attributable health outcome. This paradigm shift in developing and tracking climate change and human health indicators as a linked system necessitates the collaboration of subject matter experts from multiple disciplines in collecting data, managing inventories of data sets, creating indicators, and monitoring trends. Tracking indicators as part of an integrated system for different climate-sensitive health outcomes has the potential to generate useful data to inform policymakers. The power comes from the comprehensive assessment across the indicator data streams which can then more usefully inform decision makers about trends, projections, and effectiveness of interventions. In addition, this proposed framework helps to identify the most essential earth observations and surveillance data for both continuous monitoring and ongoing research. Scientists working on these indicator systems also benefit from the iterative process of refining data inputs or adding or eliminating indicator components as research uncovers new information. Advancing the concept of indicators from individual, independent measures to an inter-connected system of upstream, downstream, and modifying indicators enhances the current state of thinking by bringing a holistic perspective to the approach of developing climate change and health indicators.
Acknowledgements
The authors thank Paul Schramm (CDC) for his invaluable comments and suggestions on the manuscript.
Declarations
This work was supported, in part, by the NIH, National Institute of Environmental Health Sciences.
Funding This work was conducted without external sources of funding.
Footnotes
Conflicts of interest/Competing interests Not applicable
Availability of data and material Not applicable
Code availability Not applicable
References
- Anenberg Susan C., Weinberger Kate R., Roman Henry, Neumann James E., Crimmins Allison, Fann Neal, Martinich Jeremy, and Kinney Patrick L.. 2017. ‘Impacts of oak pollen on allergic asthma in the United States and potential influence of future climate change’, GeoHealth, 1: 80–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes CS 2018. ‘Impact of Climate Change on Pollen and Respiratory Disease’, Curr Allergy Asthma Rep, 18: 59. [DOI] [PubMed] [Google Scholar]
- Beard CB, Eisen RJ, Barker CM, Garofalo JF, Hahn M, Hayden M, Monaghan AJ, Ogden NH, and Schramm PJ. 2016. “Ch. 5: Vectorborne Diseases. The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment.” In, edited by Global US Change Research Program, 129–56. Washington, DC. [Google Scholar]
- Behrendt H, and Ring J. 2012. ‘Climate change, environment and allergy’, Chem Immunol Allergy, 96: 7–14. [DOI] [PubMed] [Google Scholar]
- Boylan S, Beyer K, Schlosberg D, Mortimer A, Hime N, Scalley B, Alders R, Corvalan C, and Capon A. 2018. ‘A conceptual framework for climate change, health and wellbeing in NSW, Australia’, Public Health Res Pract, 28. [DOI] [PubMed] [Google Scholar]
- Briggs David. 2003. “Making a Difference: Indicators to Improve Children’s Environmental Health.” In France. [Google Scholar]
- CDC. 2020. ‘10 Essential Public Health Services’, CDC, Accessed November 3, 2020. https://www.cdc.gov/publichealthgateway/publichealthservices/essentialhealthservices.html.
- CDC. 2021. ‘National Environmental Public Health Tracking Network’. Accessed April 13, 2021. https://ephtracking.cdc.gov/DataExplorer/.
- Corvalán CF, Kjellström T, and Smith KR. 1999. ‘Health, environment and sustainable development: identifying links and indicators to promote action’, Epidemiology, 10: 656–60. [PubMed] [Google Scholar]
- Costello A, Abbas M, Allen A, Ball S, Bell S, Bellamy R, Friel S, Groce N, Johnson A, Kett M, Lee M, Levy C, Maslin M, McCoy D, McGuire B, Montgomery H, Napier D, Pagel C, Patel J, de Oliveira JA, Redclift N, Rees H, Rogger D, Scott J, Stephenson J, Twigg J, Wolff J, and Patterson C. 2009. ‘Managing the health effects of climate change: Lancet and University College London Institute for Global Health Commission’, Lancet, 373: 1693–733. [DOI] [PubMed] [Google Scholar]
- Crimmins A, Balbus J, Gamble L, Beard CB, Bell JE, Dodgen D, Eisen RJ, Fann N, Hawkins MD, Herring SC, Jantarasami L, Mills DM, Saha S, Sarofim MC, Trtanj J, and Ziska L. 2016. “The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment.” In, edited by USGCRP. Washington, D.C. [Google Scholar]
- Ebi Kristie L. 2008. ‘Healthy people 2100: modeling population health impacts of climate change’, Climatic Change, 88: 5–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebi Kristie L., Boyer Christopher, Bowen Kathryn J., Frumkin Howard, and Hess Jeremy. 2018. ‘Monitoring and Evaluation Indicators for Climate Change-Related Health Impacts, Risks, Adaptation, and Resilience’, International journal of environmental research and public health, 15: 1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebi Kristie L., Ogden Nicholas H., Semenza Jan C., and Woodward Alistair. 2017. ‘Detecting and Attributing Health Burdens to Climate Change’, Environmental health perspectives, 125: 085004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EEA. 1999. “Environmental Indicators: Typology and Overview.” In, edited by European Environment Agency. Copenhagen. [Google Scholar]
- English Paul B., Sinclair Amber H., Ross Zev, Anderson Henry, Boothe Vicki, Davis Christine, Ebi Kristie, Kagey Betsy, Malecki Kristen, Shultz Rebecca, and Simms Erin. 2009. ‘Environmental health indicators of climate change for the United States: findings from the State Environmental Health Indicator Collaborative’, Environmental health perspectives, 117: 1673–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Füssel Hans-Martin, and Klein Richard. 2004. Conceptual Frameworks of Adaptation to Climate Change and their Applicability to Human Health. [Google Scholar]
- Haines A, Kovats RS, Campbell-Lendrum D, and Corvalan C. 2006. ‘Climate change and human health: impacts, vulnerability, and mitigation’, The Lancet, 367: 2101–09. [DOI] [PubMed] [Google Scholar]
- Haines Andy, and Ebi Kristie. 2019. ‘The Imperative for Climate Action to Protect Health’, New England Journal of Medicine, 380: 263–73. [DOI] [PubMed] [Google Scholar]
- Hambling Tammy, Weinstein Philip, and Slaney David. 2011. ‘A review of frameworks for developing environmental health indicators for climate change and health’, International journal of environmental research and public health, 8: 2854–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hess A, Davis JK, and Wimberly MC. 2018. ‘Identifying Environmental Risk Factors and Mapping the Distribution of West Nile Virus in an Endemic Region of North America’, GeoHealth, 2: 395–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hess Jeremy J., Saha Shubhayu, Schramm Paul J., Conlon Kathryn C., Uejio Christopher K., and George Luber Luber. “Projecting Climate-Related Disease Burden: A Guide for Health Departments.” In, edited by Centers for Disease Control and Prevention. Atlanta, GA. [Google Scholar]
- Katelaris CH, and Beggs PJ. 2018. ‘Climate change: allergens and allergic diseases’, Intern Med J, 48: 129–34. [DOI] [PubMed] [Google Scholar]
- Kenney Melissa A., Janetos Anthony C., and Gerst Michael D.. 2018. ‘A framework for national climate indicators’, Climatic Change. [Google Scholar]
- Kenney Melissa A., Janetos Anthony C., and Lough Glynis C.. 2016. ‘Building an integrated U.S. National Climate Indicators System’, Climatic Change, 135: 85–96. [Google Scholar]
- Kjellström T, and Corvalán C. 1995. ‘Framework for the development of environmental health indicators’, World Health Stat Q, 48: 144–54. [PubMed] [Google Scholar]
- Luber George, and McGeehin Michael. 2008. ‘Climate Change and Extreme Heat Events’, American Journal of Preventive Medicine, 35: 429–35. [DOI] [PubMed] [Google Scholar]
- McMichael AJ 2013. ‘Globalization, climate change, and human health’, New England Journal of Medicine, 368: 1335–43. [DOI] [PubMed] [Google Scholar]
- Niemeijer David, and de Groot Rudolf S.. 2008. ‘A conceptual framework for selecting environmental indicator sets’, Ecological Indicators, 8: 14–25. [Google Scholar]
- OECD. 1993. “OECD Core Set of Indicators for Environmental Performance Review.” In. Paris, France: OECD. [Google Scholar]
- Pachauri Rajendra K. and Meyer Leo. 2014. “Climate Change 2014: Synthesis Report. Contribution of Working Groups I, II and III to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change.” In, 151. Geneva, Switzerland: IPCC. [Google Scholar]
- Paull SH, Horton DE, Ashfaq M, Rastogi D, Kramer LD, Diffenbaugh NS, and Kilpatrick AM. 2017. ‘Drought and immunity determine the intensity of West Nile virus epidemics and climate change impacts’, Proc Biol Sci, 284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paz S, and Semenza JC. 2013. ‘Environmental drivers of West Nile fever epidemiology in Europe and Western Asia--a review’, Int J Environ Res Public Health, 10: 3543–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paz Shlomit. 2015. ‘Climate change impacts on West Nile virus transmission in a global context’, Philosophical Transactions of the Royal Society B: Biological Sciences, 370: 20130561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapport David, and Friend Anthony. 1979. “Towards a comprehensive framework for environmental statistics: A stress-response approach.” In, edited by Office of the Senior Adviser on Integration Statistics Canada. Ottowa, Canada. [Google Scholar]
- Reidmiller DR, Avery CW, Easterling DR, Kunkel KE, Lewis KLM, Maycock TK, and Stewart BC 2018. “Impacts, Risks, and Adaptation in the United States: Fourth National Climate Assessment, Volume II.” In, edited by USGCRP. Washington, D.C. [Google Scholar]
- Rogers DJ, and Randolph SE. 2006. ‘Climate Change and Vector-Borne Diseases.’ in Hay Simon I., Graham Alastair and Rogers David J. (eds.), Advances in Parasitology (Academic Press; ). [DOI] [PubMed] [Google Scholar]
- Sapkota Amir, Dong Yan, Li Linze, Asrar Ghassem, Zhou Yuyu, Li Xuecao, Coates Frances, Spanier Adam J., Matz Jonathan, Bielory Leonard, Breitenother Allison G., Mitchell Clifford, and Jiang Chengsheng. 2020. ‘Association Between Changes in Timing of Spring Onset and Asthma Hospitalization in Maryland’, JAMA Network Open, 3: e207551–e51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semenza Jan C., Herbst Susanne, Rechenburg Andrea, Suk Jonathan E., Christoph Höser Christiane Schreiber, and Kistemann Thomas. 2012. ‘Climate Change Impact Assessment of Food- and Waterborne Diseases’, Critical reviews in environmental science and technology, 42: 857–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skaff NK, Cheng Q, Clemesha RES, Collender PA, Gershunov A, Head JR, Hoover CM, Lettenmaier DP, Rohr JR, Snyder RE, and Remais JV. 2020. ‘Thermal thresholds heighten sensitivity of West Nile virus transmission to changing temperatures in coastal California’, Proc Biol Sci, 287: 20201065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tacket Carol O., Brenner Frances, and Blake Paul A.. 1984. ‘Clinical Features and an Epidemiological Study of Vibrio vulnificus Infections’, The Journal of Infectious Diseases, 149: 558–61. [DOI] [PubMed] [Google Scholar]
- Tong S, and Ebi K. 2019. ‘Preventing and mitigating health risks of climate change’, Environmental Research, 174: 9–13. [DOI] [PubMed] [Google Scholar]
- Vaidyanathan Ambarish, Malilay Josephine, Schramm Paul, and Saha Shubhayu. 2020. ‘Heat-Related Deaths - United States, 2004–2018’, MMWR. Morbidity and mortality weekly report, 69: 729–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vezzulli L, Colwell RR, and Pruzzo C. 2013. ‘Ocean warming and spread of pathogenic vibrios in the aquatic environment’, Microb Ecol, 65: 817–25. [DOI] [PubMed] [Google Scholar]
- Vezzulli L, Grande C, Reid PC, Hélaouët P, Edwards M, Höfle MG, Brettar I, Colwell RR, and Pruzzo C. 2016. ‘Climate influence on Vibrio and associated human diseases during the past half-century in the coastal North Atlantic’, Proc Natl Acad Sci U S A, 113: E5062–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watts Nick, Adger W. Neil, Agnolucc Paolo, Blackstock Jason, Byass Peter, Cai Wenjia, Chaytor Sarah, Colbourn Tim, Collins Mat, Cooper Adam, Cox Peter M., Depledge Joanna, Drummond Paul, Ekins Paul, Galaz Victor, Grace Delia, Graham Hilary, Grubb Michael, Haines Andy, Hamilton Ian, Hunter Alasdair, Jiang Xujia, Li Moxuan, Kelman Ilan, Liang Lu, Lott Melissa, Lowe Robert, Luo Yong, Mace Georgina, Maslin Mark, Nilsson Maria, Oreszczyn Tadj, Pye Steve, Quinn Tara, Svensdotter My, Venevsky Sergey, Warner Koko, Xu Bing, Yang Jun, Yin Yongyuan, Yu Chaoqing, Zhang Qiang, Gong Peng, Montgomery Hugh, and Costello Anthony. 2015. ‘Health and climate change: policy responses to protect public health’, The Lancet, 386: 1861–914. [DOI] [PubMed] [Google Scholar]
- Watts Nick, Amann Markus, Sonja Ayeb-Karlsson Kristine Belesova, Bouley Timothy, Boykoff Maxwell, Byass Peter, Cai Wenjia, Diarmid Campbell-Lendrum Jonathan Chambers, Cox Peter M., Daly Meaghan, Dasandi Niheer, Davies Michael, Depledge Michael, Depoux Anneliese, Paula Dominguez-Salas Paul Drummond, Ekins Paul, Flahault Antoine, Frumkin Howard, Georgeson Lucien, Ghanei Mostafa, Grace Delia, Graham Hilary, Grojsman Rébecca, Haines Andy, Hamilton Ian, Hartinger Stella, Johnson Anne, Kelman Ilan, Kiesewetter Gregor, Kniveton Dominic, Liang Lu, Lott Melissa, Lowe Robert, Mace Georgina, Maquins Odhiambo Sewe Mark Maslin, Mikhaylov Slava, Milner James, Ali Mohammad Latifi Maziar Moradi-Lakeh, Morrissey Karyn, Murray Kris, Neville Tara, Nilsson Maria, Oreszczyn Tadj, Owfi Fereidoon, Pencheon David, Pye Steve, Rabbaniha Mahnaz, Robinson Elizabeth, Joacim Rocklöv Stefanie Schütte, Joy Shumake-Guillemot Rebecca Steinbach, Tabatabaei Meisam, Wheeler Nicola, Wilkinson Paul, Gong Peng, Montgomery Hugh, and Costello Anthony. 2018. ‘The Lancet Countdown on health and climate change: from 25 years of inaction to a global transformation for public health’, The Lancet, 391: 581–630. [DOI] [PubMed] [Google Scholar]
- Wilkinson P, Campbell-Lendrum D, Bartlett C, Corvalán C, Githeko AK, Woodward A, and Scheraga J. 2003. “Monitoring the health effects of climate change.” In. [Google Scholar]
- Xun Wei W., Khan Aneire E., Michael Edwin, and Vineis Paolo. 2010. ‘Climate change epidemiology: methodological challenges’, International Journal of Public Health, 55: 85–96. [DOI] [PubMed] [Google Scholar]
- Ziska Lewis H., Makra László, Harry Susan K., Bruffaerts Nicolas, Hendrickx Marijke, Coates Frances, Saarto Annika, Thibaudon Michel, Oliver Gilles, Damialis Athanasios, Charalampopoulos Athanasios, Vokou Despoina, Starri Heiđmarsson Ellý Guđjohnsen, Bonini Maira, Oh Jae-Won, Sullivan Krista, Ford Linda, G. Daniel Brooks, Dorota Myszkowska, Elena Severova, Regula Gehrig, Germán Darío Ramón, Paul J. Beggs, Kim Knowlton, and Allison R. Crimmins. 2019. ‘Temperature-related changes in airborne allergenic pollen abundance and seasonality across the northern hemisphere: a retrospective data analysis’, The Lancet Planetary Health, 3: e124–e31. [DOI] [PubMed] [Google Scholar]