Abstract
We investigated the effects of caffeine mouth rinse on endurance performance, muscle recruitment (i.e., electromyographic activity of the vastus lateralis and rectus femoris), rating of perceived effort and heart rate. Twelve physically-active healthy men cycled at 80% of their respiratory compensation point until task failure. The participants rinsed their mouths for 10 seconds with placebo (PLA, 25 mL of a solution composed of non-caloric mint essence) or caffeine (CAF, 25 mL of 1.2% of anhydrous caffeine concentration with non-caloric mint essence) every 15 minutes of exercise. Time until exhaustion increased 17% (effect size = 0.70) in CAF compared to PLA (p = 0.04). The wavebands of low-frequency electromyographic activity (EMG) of the vastus lateralis and rectus femoris was lower in CAF group than PLA at 50% of the time until exhaustion (p = 0.04). The global EMG signal was lower in CAF group than PLA at 100% of the time until exhaustion (p = 0.001). The rating of perceived effort pooled was higher in CAF mouth rinse (p = 0.001) than PLA group. No effect was found on the heart rate between the groups (p > 0.05). Caffeine mouth rinse increases endurance performance, rating of perceived effort and decreases muscle activity during a moderate-intensity exercise.
Keywords: Endurance Capacity, Muscle Skeletal, Nutrition, Exercise
INTRODUCTION
The ergogenic effects of caffeine (CAF) ingestion have been evidenced in several endurance exercises (i.e., time to exhaustion or time-trials) [1–3]. However, CAF ingestion might lead to some side effects during and/or after exercises, such as gastrointestinal discomfort, muscle pain, insomnia, anxiety and headache [4]. To avoid some of these negatives side effects, CAF mouth rinse has been tested as an alternative ergogenic strategy since it does not involve digestion and metabolization of caffeine [5, 6]. The ergogenicity of CAF mouth rinse is, however, controversial and deserves further investigation [7].
Studies investigating the ergogenic effect of CAF mouth rinse between 5–10 seconds have indicated either an improved on high-intensity exercise performance [8, 9], or no effect on endurance task [10] and variables of the Wingate test [11]. In addition to the mouth rinse time, a recent review concluded that heterogeneity in the other methods (i.e., CAF concentration, mouth rinse time, exercise intensity, habitual intake, genetic, bitter or no bitter taste solution) can influence the efficacy of CAF mouth rinsing on physical performance [7, 12]. Due to the few studies, the most efficient set of methods for using this resource is not yet known. Thus, the ergogenic effect of CAF mouth rinse on exercise performance, mainly in relation to the endurance-based task has not been well established.
The mechanism by which CAF mouth rinse would increase exercise performance is not fully known, but it has been suggested that 20 seconds of CAF mouth rinse stimulates a group of sensory receptors in the oral cavity, which actives some brain areas associated with reward and motor control [13], a mechanism similar to reported for CHO mouth rinse [14, 15]. Previous studies provided evidence that CHO mouth rinse attenuates the exercise-induced reduction in electromyography activity (EMG) of the vastus lateralis during moderate-intensity cycling, indicating maintenance of skeletal muscle recruitment during the last phase of a prolonged exercise [16, 17]. However, skeletal muscle activation and recruitment pattern (i.e., recruitment of type I or II muscle fibers) in endurance exercise, mainly the EMG low-frequency analyzes that are associated with the recruitment of slow motor units, have not yet been investigated by CAF mouth rinse.
It could be expected that CAF mouth rinse activates the prefrontal cortex (i.e., orbitofrontal and dorsolateral), regions associated with reward, attention and cognition [13], which could exert a central role in the motor control process and Ratings of Perceived Exertion (RPE). Some studies have reported that CAF mouth rinse cannot influence the RPE [8, 10], but no study has assessed fatigue tolerance during prolonged exercise. The investigation of the relationship between CAF mouth rinse and RPE seems to be plausible since studies using CAF intake reported negative a correlation between CAF metabolization and RPE [18, 19], as well as fatigue tolerance [20, 21].
In the present study, we investigated the effects of 10 seconds of CAF mouth rinse on performance, muscle recruitment pattern, rating of perceived exertionand heart rate throughout the endurance test in cycle ergometer. We hypothesized that CAF mouth rinse would increase endurance performance and fatigue tolerance by changing muscle recruitment, heart rate and rating of perceived exertion.
MATERIALS AND METHODS
Participants
Twelve physically-active healthy men, who were accustomed to cycling recreationally were included in this study (VO2MAX 38.5 ± 8.1 mL⋅kg-1⋅min⋅-1; Intensity equivalent to VO2MAX = 217 ± 37 Watts; BMI 19.5 ± 2.9 kg/m²; height 174.0 ± 8.9 cm; body mass 68.2 ± 12.2 Kg; body fat 11.2 ± 6.2%; Age 22.0 ± 2.8 years). The sample size was calculated post hoc using the time until exhaustion (average ± SD) for the groups, following input parameters for the t-test (matched pairs): A) number (= 12); B) α error probability (= 0.05); C) effect size (= 0.78). The power sample (1-β error probability) was = 0.70. Participants were free of injuries or diseases in the six months prior to the study. Participants were informed about the risks and benefits associated with the study andsigned a consent form before starting the experiments. The study was conducted in accordance with the Declaration of Helsinki (2008) and approved by the Local Ethics Committee (protocol number: 40062214.1.0000.5013).
Experimental Protocol
The study was conducted using a single-blind, randomized, counterbalanced, placebo-controlled crossover design. In the first visit, anthropometric measurements (body mass, height, and body fat) were taken, and a maximal incremental exercise test to determine respiratory compensation point (RCP), VO2max and peak power output was performed. In the second and third visits, participants cycled at 80% of RCP until task failure with either CAF orplacebo (PLA) mouth rinse. All tests were performed on a magnetically-braked cycle ergometer (Ergo Fit 167, Ergo-FitGmbH e Co., Pirmasens, Germany®). The tests were carried out during the summer months, same time of the day, laboratory temperature maintained at 22 ± 1 ºC and after two hours after the last meal. The position of the cycle ergometer seat was individually adjusted (vertically and horizontally) and replicated in the subsequent trials. To avoid any bias from single-blind design, verbal encouragement was standardized in all experimental trials. The endurance performance was not revealed to the participants until all tests had been completed. The experimental trials were performed with a minimum of 72 h and a maximum of 96 h intervals. RPE was collected immediately before the beginning of the tests to control to ensure that the participants were rested. No participant performed the protocol declaring to have the RPE above 7 points. The participants were instructed to refrain from vigorous physical activities and caffeinated substances or alcoholic beverages 48 hours before each test. Participants also filled out a 24-h dietary recall before the incremental test; the dietary recall was photocopied and handed back to the participants, whowere asked to repeat this diet before subsequent trials.
Anthropometric Measurements
Bodyweight and height were measured using an electronic scale and stadiometer, respectively. The skinfold thickness (chest, abdomen and thigh) was measured with a Lange caliper (Cambridge Scientific Industries, Inc. Cambridge, Maryland, USA®). The body density and body fat were estimated using the generalized equations of Jackson and Pollock (1985) and Siri (1961), respectively.
Maximal Incremental Exercise Test
After a 5-min warm-up at 30 W, power output was increased 30 W⋅min-1 until participants were unable to maintain the pedal cadence between 60–70 revolutions per minute (rpm).
Throughout the test, oxygen consumption (VO2), carbon dioxide (VCO2) and ventilation (VE) were recorded breath by breath using an automatic metabolic cart (Quark CPET, Cosmed, Roma, Italia®). The gas analyzer was calibrated before to each test using known concentrations of O2 and CO2 (16% and 5%, respectively). The volume of expired air was measured by a turbine, calibrated prior each test with a 3-L syringe. Heart rate was monitored during the entire trial using a heart rate monitor (Polar FT4 – Polar, Kempele, Finnland®). The RPE was recorded after the exhaustion using a 15-point Borg scale [33].
The trial was considered maximal when at least three of the following criteria was noted: plateau in VO2 (increase ≤ 150 ml min-1 or 2 ml kg-1⋅min-1), respiratory exchange ratio ≥ 1.15, final heart rate ≥ 90% predicted by age (220 – age) and RPE ≥ 18 [22, 23]. (Howleyand Bassett, 1995; Taylor, Buskirk and Henschel, 1955). Peak power output was considered as the maximum power achieved during the test. The respiratory compensation point was visually identifiedby threeindependent evaluators, using the second break in the ventilation curve, an increase in VE/VCO2 ratio, and the first drop point of the CO2 fractionas criteria [24].
Experimental Trials
Participants cycled at an exercise intensity corresponding to 80% of the RCP (174 ± 30 Watts), maintaining a pedal cadence between 60 and 70 rpm. The test was interrupted when the participant was unable to maintain a pedal cadence above 60 rpm after three consecutive warnings from the evaluator. The task failure was considered as the time elapsed from the start until the interruption of the trial measured the nearest seconds. Participants were blinded to the elapsed time. The RPE using a 15-point Borg scale was recorded immediately before and every 5 min through the test performed [33].
Mouth Rinse
The CAF and PLA solutions were tested several times in a pilot study until reach identical fluid characteristics. The participants of the current study were not able to identify any differences between solutions after the trials. Participants rinsed their mouths with PLA (25 mL of a solution composed of non-caloric mint essence) or CAF (25 mL of 1.2% of anhydrous caffeine concentration) for 10 s and then expelled in an appropriate bottle. Mouth rinse for 10 s did not increase plasma CAF [10]. The solutions were administered immediately before the beginning of the trial and every 15 minutes during the trial.
Electromyographic Signal Acquisition and Analysis
The EMG acquisition was captured during 2 min, starting immediately after each mouth rinse period. The EMG signal of the vastus lateralis (VL) and rectus femoris (RF) muscles of the right thigh were continually monitored using an electromyography system (EMG system Brazil, model 410c, São Paulo, Brazil) with a rejection rate in common mode > 100 dB, 20 x gain, and sampling frequency of 2000 Hz per channel. Before the trials, a tricotomy was performed, followed by asepsis with alcohol swabs to reduce the impedance of the skin. Ag/AgCl bipolar surface electrodes (AGCL –Hal®) were placed on the VL and RF muscles. The ground electrode was positioned in a neutral location (tibial tuberosity). The electrodes were fixed to the skin using adhesive tape (Micropore ™ 3M ®). The placement and location of the electrodes followed the recommendations of Hermens et al. [25]. The sampling frequency for the acquisition of electromyographic signals was 2000 Hz per channel and signal acquisition was performed for 2-min just after participants rinsed each solution. Signals were filtered using a second-order Butterworth band pass filter (cutoff frequency between 20–450 Hz). The average rectified value was then used as a measure for global EMG activity [26].
The unfiltered signals were used in a series of band-pass filters in order to assess the magnitude of low and high-frequency components [27, 28, 29]. Nine bands were determined using a fifth order Butterworth digital filter in order to separate the full signal in high (146.95–300.80 Hz) and low (26.95–75.75 Hz), each band was converted in their Average Rectified Value (global EMG activity). The sum of the global EMG activity signals of the nine averaged frequency bands was computed as a measure of total activation for each muscle. The fifth, sixth, and seventh bands were averaged to compute the global EMG activity high-frequency components of the signals, which would potentially represent the response of larger motor units (Wakeling et al. 2002). The first and the second bands were averaged to compute the global EMG activity from low-frequency components of the signals, which would represent the response of smaller motor units [28]. The data was then separated in the beginning (0%); mid (~50%) and until task failure (immediately prior to 100%) based on the duration of each test. The global EMG activity at the beginning (0%) was used to normalize global EMG activity and wave bands at 50 and 100% time points.
Statistical analysis
The Kolgomorov-Smirnov test was used to verify the normality of data distribution. The data were tested for homogeneity using the Levene’s test. Both normality and homogeneity were confirmed; therefore, a paired samples t-test was used to compare endurance capacity (until task failure) between PLA vs. CAF mouth rinse. Two-way ANOVAs having time and supplement as factors, followed by LSD post hoc test when necessary, was used for analyzing EMG signals (wavebands and global EMG activity) of the RF and VL muscles, HR and RPE. All values of RPE during each test were pooled for each group and compared by T-test for independent samples. The number of observations of RPE for each scale (range 6–20) was distributed for the groups. Effect size (ES) was also calculated for differences in endurance performance and EMG signals where thresholds for small, moderate and large effects were set at 0.20, 0.50 and 0.80, respectively [30]. Statistical tests were calculated using SPSS (version 13.0, Chicago, USA) and Statistica (Statistica® version 10.0, StataSoft, Tulsa, OK), adopting a significance level of p ≤ 0.05. Data are presented as mean ± SD and confidence intervals.
RESULTS
Time until task failure was 17% longer CAF mouth rinse condition (91 ± 22 min, CI95% = 79.8–105) when compared to PLA mouth rinse condition (76 ± 19 min, CI95% = 65.1–86.9; p = 0.04; ES = 0.70, moderate).
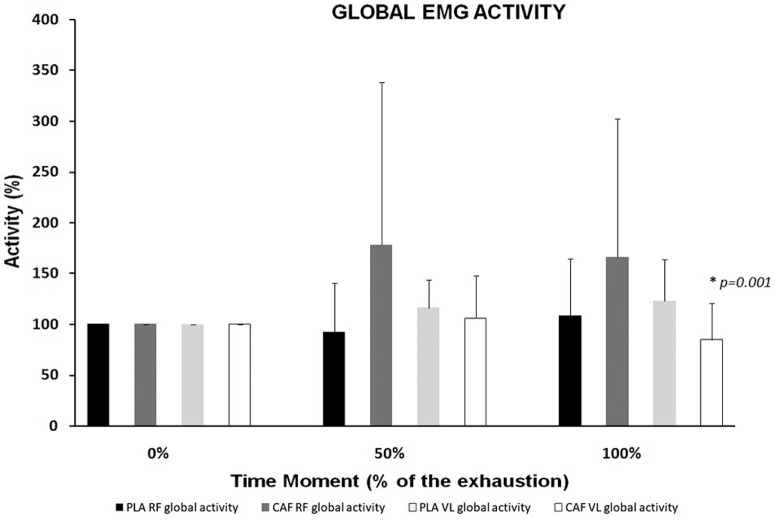
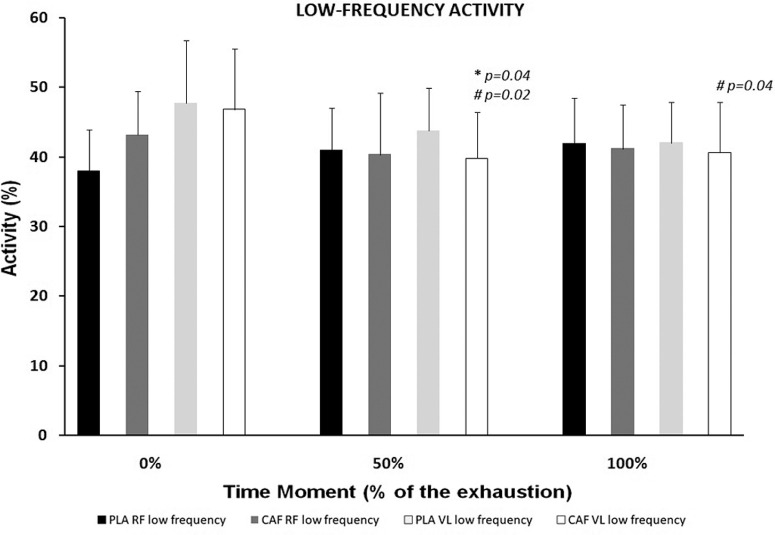
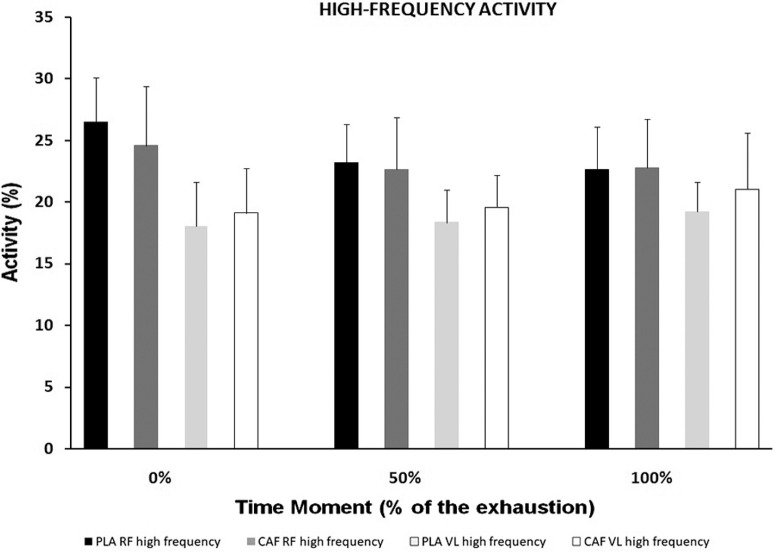
Analyzes of variance indicated differences in the: Global Electromyographic Signal Analysis for the RF (inter-group = F = 1.63; p = 0.21; intra-group through time = F = 5.86; p = 0.02) and VL (inter-group = F = 3.12; p = 0.05; intra-group through time = F = 6.26; p = 0.01); low-frequency wavebands for the RF (inter-group = F = 1.27; p = 0.29; intra-group through time = F = 0.530; p = 0.47) and VL (inter-group = F = 0.766; p = 0.47; intra-group through time = F = 3.68; p = 0.06); high-frequency wavebands for the RF (inter-group = F = 0.402; p = 0.67; intra-group through time = F = 0.651; p = 0.42) and VL (intergroup = F = 0.100; p = 0.90; intra-group through time = F = 3.97; p = 0.06).
Specifically, the post hoc test indicated that CAF mouth rinse reduced the Global EMG activity for VL muscle (p = 0.001; ES = 2.03) at moment equivalent to 100% of the time until task failure (Figure 1). Similarly, at a moment equivalent to 50% of the time until task failure, in low-frequency wavebands, there was a decrease in EMG activity in CAF group in relation to PLA for VL (p = 0.04; ES = 6.24) muscle (Figure 2). The CAF intra-group for VL reduced the EMG activity at 50% (p = 0.02; ES = 4.28) and 100% (p = 0.04; ES = 4.35) moments in comparison to 0% (Figure 2). No difference in the low-frequency group was found in RF muscle through time.
FIG. 1.
Muscle activation for the vastus lateralis (VL) and rectus femoris (RF) in global EMG activity.
Note: * Significant differencebetween CAF and PLA.
FIG. 2.
Muscle activation for the vastus lateralis (VL) and rectus femoris (RF) in low frequencies (wavebands).
Note: * Significant difference between CAF and PLA.
No differences (intra-group and inter-group) were found in high-frequency wavebands (Figure 3).
FIG. 3.
CAF vs. PLA. Muscle activation for the vastus lateralis (VL) and rectus femoris (RF) in high frequencies (wavebands). No significant differences were observed.
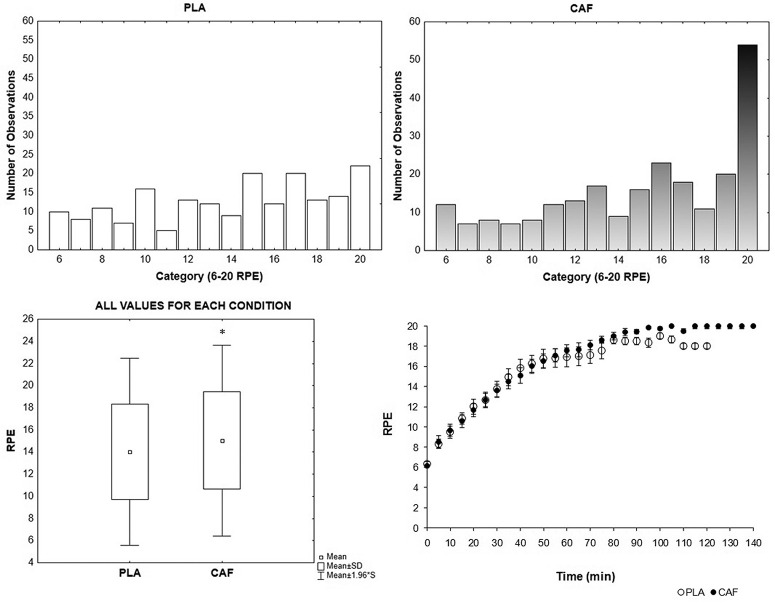
No differences were found between conditions (F = 0.951; p = 0.39) for RPE at equivalent specific times of the test (0%, 50% and 100%) (Table 1; Figure 4D), but there was intra-group difference through time (F = 476.488; p < 0.01) (Table 1). However, RPE in the sum of all the values assigned throughout the test (Figure 4C) was higher in CAF than PLA group. The numbers of observations at maximal scale point (i.e., 20) were reported 54 (equivalent to 22% of the total 235 observations) and 22 fold (equivalent to 11% of the total 192 observations) for CAF and PLA groups respectively (Figure 4 A and B).
TABLE 1.
Values are mean ± standard deviation. Heart rate (beats per minute) and rating of perceived effort (RPE) at the beginning (0%), middle (50%) and end (100%) of the constant-load exercise.
| Variables | Conditions | 0% | 50% | 100 % |
|---|---|---|---|---|
| HR | CAF | 105 ± 12 (CI95% = 98–112) |
145 ± 17 * (p = 0.01) (CI95% = 135–155) |
152 ± 16 * (p = 0.01) (CI95% = 143–161) |
| PLA | 96 ± 24 (CI95% = 82–110) ES = 2.23 |
145 ± 23 * (p = 0.01) (CI95% = 132–158) ES < 0.01 |
153 ± 19 * (p = 0.01) (CI95% = 142–164) ES = 0.47 |
|
|
| ||||
| RPE | CAF | 10 ± 2 (CI95% = 9–11) | 16 ± 2 * (p = 0.01) (CI95% = 15–17) | 19 ± 1 * (p = 0.01)#(p = 0.01) (CI95% = 18–20) |
| PLA | 9 ± 1 (CI95% = 8–10) ES = 1.41 |
15 ± 2 * (p = 0.01) (CI95% = 14–16) ES < 0.01 |
18 ± 2 * (p = 0.01)#(p = 0.01) (CI95% = 17–19) ES = 1.41 |
|
Note: * different from moment 0% intra-group.
different from moment 50% intra-group.
ES- Effect size between CAF vs PLA at same moment.
FIG. 4.
CAF vs. PLA. (A) Number of observations for RPE scale values in PLA group; (B) Number of observations for RPE scale values in CAF group; (C) All values of RPE for each test pooled in group. Difference between CAF and PLA (p = 0.01); (D) Time and RPE throughout test at CAF and PLA conditions.
No difference was found inter-group (F = 0.001; p = 0.99) for HR (Table 1). However, there was intra-group difference through time (F = 430.895; p < 0.01) (Table 1).
DISCUSSION
The results of the present study corroborated with the hypothesis that CAF mouth rinse increases endurance performance until task failure when compared to PLA. CAF mouth rinse increased the fatigue tolerance reported by the increased RPE and decreased EMG Activity and Wavebands throughout the exercise in the CAF mouth rinse condition.
Our finding indicates that 10 s of CAF mouth rinse is effective to improve endurance during exercise lasting more than 60 minutes (17% longer until task failure, moderate effect size). This result corroborates with previous studies in shorter duration exercises (30 minutes) [6, 8] but is contrary to the no-effect reported during a 60-min cycling time-trial [10]. Differences in data analysis/interpretation, exercise protocols (i.e. time trial vs. until task failure) and/or CAF concentration (present study = 1.2% concentration, like Beaven et al. [5]; and Doering et al. [10] = 0.14% concentration) may explain these contradictions since the time of rinse was the same. In addition, participants from Doering et al. [10] received 4.5 ml⋅kg-1 of water and were allowed to swallow, which may have affected the perception of gastric emptying.
Regarding RPE, no differences were found between conditions analyzing specific and equivalent moments of the test (0%, 50% and 100%) (Table 1, Figure 4D) and these results, at least in part, corroborate with the findings related to CAF intake, which point out that in exercises until exhaustion, RPE tends to be similar between CAF and PLA [19]. Nevertheless, our data indicated that CAF condition promoted fatigue tolerance and higher values of RPE compared to PLA (p = 0.01) (Figure 4C). Analyzing the RPE values from a “cumulative” perspective, we calculated the distributions of observations for each scale point (i.e., 6–20), it is clear that participants in the CAF group are more resistant to fatigue, supporting higher RPE scores compared to the PLA condition (Figure 4A and B). This result is similar to a study carried out with CAF intake [20] showing that CAF mouth rinse can increase fatigue tolerance for endurance exercise. In this line, we are tempted to speculate two mechanisms: (1) CAF mouth rinse results in high activation of brain areas and (2) bitter taste of CAF solution may induce a “driven by expectancy” [12], which may be linked to attention, reward and as a consequence with RPE.
Regarding EMG Global and Wavebands, it would be reasonable to expect EMG activity to be altered at times close to fatigue, at least in the condition with the best performance (maybe reducing its signal due to greater physiological demands)[16, 17]. We initially expected that, in the CAF condition there would be a decrease in the Global EMG Activity or at least in the low-frequency bands (Wavebands) representing type 1 fibers [26]. These patterns were observed in the present study, which leads us to believe that in recreationally trained populations, VL muscle recruitment pattern, tend to be reduced throughout the effort with CAF mouth rinse. Thus, greater fatigue tolerance and longer time to exhaustion in CAF group consequently decreased the EMG activity and motor pattern for low-frequency waveband in VL muscle. On the other hand, the RF EMG activity was not changed in any frequency analyzes, corroborating with Bastos-Silva et al. [16] that found in similar with CHO mouth rinse protocol changes in the VL, but not in the RF. Probably, the CAF mouth rinse does not activate the motor cortex regions associated to increase the muscle electrical activity [31]. CAF-induced did not increase or sustain the EMG during endurance task. The main change in EMG activity occurred in the VL, the most important muscle in relation to the RF, to tolerate the endurance effort in physically active individuals.
Regarding HR, no differences were found between conditions analyzing specific moments of the test (0%, 50% and 100%) (Table 1). These data are in contrast to the difference observed in the RPE and may seem confusing at first, considering that heart rate may have a high correlation with RPE [32]. However, the use of CAF as an ergogenic resource (ingestion or rinse) can compromise this correlation, since our results contradict this relationship between RPE and HR, as well as studies with the CAF intake [33, 34].
The present study presents some limitations, such as the reduced number of muscles evaluated during the tests (only two), the exercise protocol that partially distances itself from the currently practiced cycling modalities (mostly competitions against the clock time), besides not evaluating aspects such as motivation or attention focus. However, these limitations do not affect the internal validity of the present study and provide an initial framework for using CAF mouthwash as an ergogenic aid during exercise in physically-active healthy men.
CONCLUSIONS
In conclusion, caffeine mouth rinse increases endurance performance at moderate-intensity exercise, muscle activity (i.e., global and low-frequency waveband signal), and fatigue tolerance in physically-active healthy men. Therefore, the ergogenic effect of the CAF mouth rinse has a relevant practical application since it minimizes the side effects of ingestion.
REFERENCES
- 1.Costill DL, Dalsky GP, Fink WJ. Effects of caffeine ingestion on metabolism and exercise performance. Med Sci Sports. 1978;10(3):155–8. [PubMed] [Google Scholar]
- 2.Lane SC, Areta JL, Bird SR, Coffey VG, Burke LM, Desbrow B, Karagounis LG, Hawley JA. Caffeine ingestion and cycling power output in a low or normal muscle glycogen state. Med Sci Sports Exerc. 2013;45(8):1577–84. doi: 10.1249/MSS.0b013e31828af183. [DOI] [PubMed] [Google Scholar]
- 3.Mielgo-Ayuso J, Marques-Jiménez D, Refoyo I, Del Coso J, León-Guereño P, Calleja-González J. Effect of Caffeine Supplementation on Sports Performance Based on Differences Between Sexes: A Systematic Review. Nutrients. 2019;11(10):2313. doi: 10.3390/nu11102313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mora-Rodriguez R, Pallarés JG. Performance outcomes and unwanted side effects associated with energy drinks. Nutr Rev. 2014;72:108–20. doi: 10.1111/nure.12132. [DOI] [PubMed] [Google Scholar]
- 5.Beaven CM, Maulder P, Pooley A, Kilduff L, Cook C. Effects of caffeine and carbohydrate mouth rinses on repeated sprint performance. Appl Physiol Nutr Metab. 2012;38(6):633–7. doi: 10.1139/apnm-2012-0333. [DOI] [PubMed] [Google Scholar]
- 6.Sinclair J, Bottoms L. The effects of carbohydrate and caffeine mouth rinsing on arm crank time-trial performance. J Sport Res. 2014;1(2):34–44. [Google Scholar]
- 7.Ehlert AM, Twiddy HM, Wilson PB. The Effects of Caffeine Mouth Rinsing on Exercise Performance: A Systematic Review. Int J Sport Nutr Exerc Metab. 2020;30(5):362–373. doi: 10.1123/ijsnem.2020-0083. [DOI] [PubMed] [Google Scholar]
- 8.Bottoms L, Hurst H, Scriven A, Lynch F, Bolton J, Vercoe L, Shone Z, Barry G, Sinclair J. The effect of caffeine mouth rinse on self-paced cycling performance. Comp Exerc Physiol. 2014;10(4):239–45. [Google Scholar]
- 9.Kizzi J, Sum A, Houston FE, Hayes LD. Influence of a caffeine mouth rinse on sprint cycling following glycogen depletion. Eur J Sport Sci. 2016;1391:1–8. doi: 10.1080/17461391.2016.1165739. [DOI] [PubMed] [Google Scholar]
- 10.Doering TM, Fell JW, Leveritt MD, Desbrow B, Shing CM. The effect of a caffeinated mouth-rinse on endurance cycling time-trial performance. Int J Sport Nutr Exerc Metab. 2014;24(1):90–7. doi: 10.1123/ijsnem.2013-0103. [DOI] [PubMed] [Google Scholar]
- 11.Marinho AH, Mendes EV, Vilela RA, Bastos-Silva VJ, Araujo GG, Balikian P. Caffeine mouth rinse has no effects on anaerobic energy yield during a Wingate Test. J Sports Med Phys Fitness. 2020;60(1):69–74. doi: 10.23736/S0022-4707.19.09928-6. [DOI] [PubMed] [Google Scholar]
- 12.Pickering C. Are caffeine’s performance-enhancing effects partially driven by its bitter taste? Med Hypotheses. 2019;131:109301. doi: 10.1016/j.mehy.2019.109301. [DOI] [PubMed] [Google Scholar]
- 13.De Pauw K, Roelands B, Knaepen K, Polfliet M, Stiens J, Meeusen R. Effects of caffeine and maltodextrin mouth rinsing on P300, brain imaging and cognitive performance. J Appl Physiol. 2015;118(6):776–82. doi: 10.1152/japplphysiol.01050.2014. [DOI] [PubMed] [Google Scholar]
- 14.Turner CE, Byblow WD, Stinear CM, Gant N. Carbohydrate in the mouth enhances activation of brain circuitry involved in motor performance and sensory perception. Appetite. 2014;80:212–9. doi: 10.1016/j.appet.2014.05.020. [DOI] [PubMed] [Google Scholar]
- 15.Jeffers R, Shave R, Ross E, Stevenson EJ, Goodall S. The effect of a carbohydrate mouth-rinse on neuromuscular fatigue following cycling exercise. Appl Physiol Nutr Metab. 2014;40(6):557–64. doi: 10.1139/apnm-2014-0393. [DOI] [PubMed] [Google Scholar]
- 16.Chambers ES, Bridge MW, Jones D. Carbohydrate sensing in the human mouth: effects on exercise performance and brain activity. J Physiol. 2008;587(8):1779–94. doi: 10.1113/jphysiol.2008.164285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ataide-Silva T, Ghiarone T, Bertuzzi R, Stathis CG, Leandro CG, Lima-Silva AE. CHO Mouth Rinse Ameliorates Neuromuscular Response with Lower Endogenous CHO Stores. Med Sci Sports Exerc. 2016;48(9):1810–1820. doi: 10.1249/MSS.0000000000000973. [DOI] [PubMed] [Google Scholar]
- 18.Bastos-Silva VJ, de A. Melo A, Lima-Silva AE, Moura FA, Bertuzzi R, de Araujo GG. Carbohydrate mouth rinse maintains muscle electromyographic activity and increases time to exhaustion during moderate but not high-intensity cycling exercise. Nutrients. 2016;8(3):49. doi: 10.3390/nu8030049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Whalley P, Paton C, Dearing CG. Caffeine metabolites are associated with different forms of caffeine supplementation and with perceived exertion during endurance exercise. Biol Sport. 2021;38(2):261–7. doi: 10.5114/biolsport.2020.98455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Doherty M, Smith PM. Effects of caffeine ingestion on rating of perceived exertion during and after exercise: A meta-analysis. Scand J Med Sci Sport. 2005;15(2):69–78. doi: 10.1111/j.1600-0838.2005.00445.x. [DOI] [PubMed] [Google Scholar]
- 21.Kumar N, Warren GL, Snow TK, Millard-Stafford M. Caffeine ingestion with or without low-dose carbohydrate improves exercise tolerance in sedentary adults. Front Nutr. 2019;6:1–9. doi: 10.3389/fnut.2019.00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Howley ET, D R Bassett DR, Jr, Welch HG. Criteria for maximal oxygen uptake: review and commentary. Med Sci Sports Exerc. 1995;27(9):1292–1301. [PubMed] [Google Scholar]
- 23.Taylor E, Buskirk E, Henschel A. Maximal oxygen intake as an objective measure of cardio-respiratory performance. J Appl Physiol. 1955;8(1):73–80. doi: 10.1152/jappl.1955.8.1.73. [DOI] [PubMed] [Google Scholar]
- 24.Beaver WL, Wasserman K, Whipp BJ. A new method for detecting anaerobic threshold by gas exchange. J Appl Physiol. 1986;60(6):2020–7. doi: 10.1152/jappl.1986.60.6.2020. [DOI] [PubMed] [Google Scholar]
- 25.Hermens HJ, Freriks B, Disselhorst-Klug C, Rau G. Development of recommendations for SEMG sensors and sensor placement procedures. J Electromyogr Kinesiol. 2000;10(5):361–74. doi: 10.1016/s1050-6411(00)00027-4. [DOI] [PubMed] [Google Scholar]
- 26.Chapman R, Vicenzino B, Blanch P, Dowlan S, Hodges PW. Does cycling effect motor coordination of the leg during running in elite triathletes ? J Sci Med Sport. 2008;11(4):371–380. doi: 10.1016/j.jsams.2007.02.008. [DOI] [PubMed] [Google Scholar]
- 27.Piucco T, Bini R, Sakaguchi M, Diefenthaeler F, Stefanyshyn D. Motor unit firing frequency of lower limb muscles during an incremental slide board skating test. Sport Biomech. 2017;3141:1–12. doi: 10.1080/14763141.2016.1246600. [DOI] [PubMed] [Google Scholar]
- 28.Quesada JIP, Sampaio LT, Bini R, Rossato M, Cavalcanti V. Multifactorial cycling performance of Cyclists and Non-Cyclists and their effect on skin temperature. J Therm Anal Calorim. 2016;127(2):1479–1489. [Google Scholar]
- 29.Wakeling JM, Kaya M, Temple GK, Johnston IA, Herzog W. Determining patterns of motor recruitment during locomotion. J Exp Biol. 2002;205(3):359–369. doi: 10.1242/jeb.205.3.359. [DOI] [PubMed] [Google Scholar]
- 30.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2° ed. Erlbaum: Lawrence; 1988. [Google Scholar]
- 31.Ataide-Silva T, Di Cavalcanti Alves de Souza ME, De Amorim JF, Stathis CG, Leandro CG, Lima-Silva AE. Can carbohydrate mouth rinse improve performance during exercise? A systematic review. Nutrients. 2013;6(1):1–10. doi: 10.3390/nu6010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fares EJM, Kayser B. Carbohydrate mouth rinse effects on exercise capacity in pre- and postprandial states. J Nutr Metab. 2011;2011:385962. doi: 10.1155/2011/385962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Borg GAV. Psychophysical bases of perceived exertion. Med Sci Sport Sport Exerc. 1982;14(5):377–381. [PubMed] [Google Scholar]
- 34.Glaister M, Gissane C. Caffeine and Physiological Responses to Submaximal Exercise: A Meta-Analysis. Int J Sports Physiol Perform. 2018;13(4):402–11. doi: 10.1123/ijspp.2017-0312. [DOI] [PubMed] [Google Scholar]