Abstract
Benign ganglioneuroma contains mature autonomous ganglion cells, including satellite cells and long axonal processes, as well as Schwann cells, which come from neural crest-derived cells that form the adrenal medulla and sympathetic nervous system during embryonic development and is a rare benign tumor which occurs spontaneously and can also occur during radiotherapy or chemotherapy, accounting for 0.72% -1.6% of primary retroperitoneal tumors, commonly found in the posterior mediastinum and retroperitoneum, and affected patients usually have no symptoms due to of its non-functional feature, although several complications can arise if the tumor is large enough to press against adjacent organs.
Keywords: Ganglioneuroma, Computed Tomography, US, RM
Background
Ganglioneuroma is a rare benign neuroblastic tumor that includes Schwann cells and ganglion cells [1,2], the differential diagnosis between adrenal ganglioneuroma and other adrenal solid tumors is difficult, with an average age in children and in young adults at diagnosis of approximately 7 years [3] and a higher frequency is reported in patients with type II multiple endocrine neoplasms and type 1 neurofibromatosis. Due to their slow growth, most ganglioneuromas are found randomly and most patients experience long-term disease-free survival even after incomplete resection, [4], with rare malignant transformation [1], paucity of distinct clinical symptoms as only a minority of GNs are functional [5] such as to produce hormones, such as catecholamines, vasointestinal peptides and androgens.
Case presentation
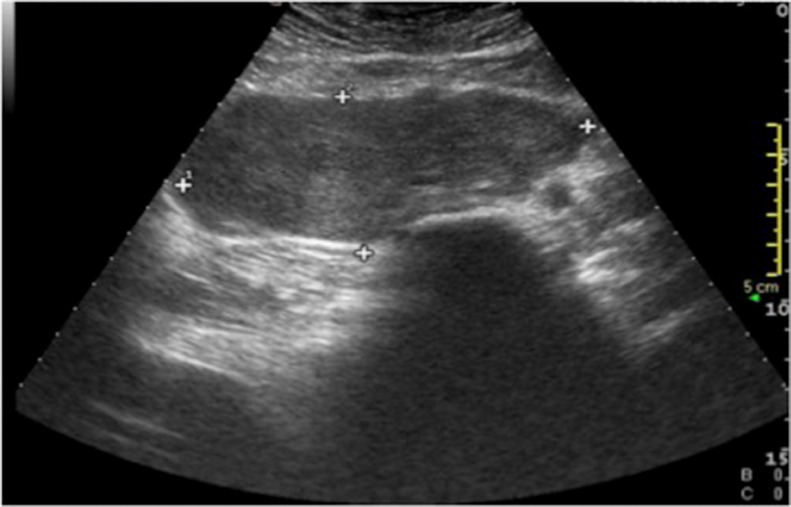
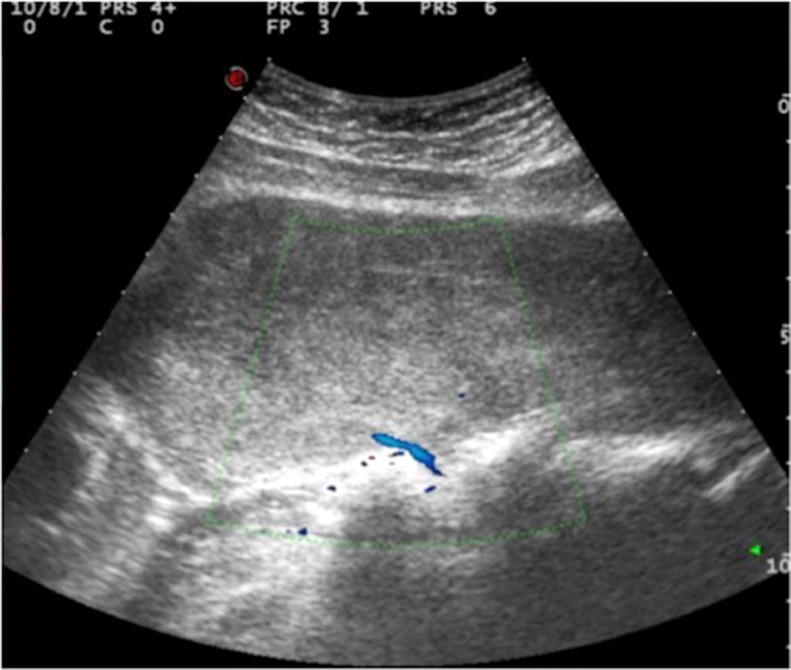
In January 2021, a 15-year-old boy, with no known disease, came to our observation for suspected orchitis, performing a testicular ultrasound showing a finding of acute left orchi-epididymitis, also performing an ultrasound examination of the abdomen for mild and diffuse pain, which showed a "voluminous hypoechoic retroperitoneal mass, with clear margins and regular contours, maximum dimensions of 15 × 7.5 cm, placed in front of the right psoas muscle and the rachis'' (Fig. 1), with close contiguity with the adjacent vertebral soma and with evidence of a vascular peduncle of probable afferent vertebral origin (Fig. 2).
Fig. 1.
Ultrasound examination of the abdomen revealed "voluminous hypoechoic retroperitoneal mass, with clear margins and regular contours, with maximum dimensions of 15 x 7.5 cm, which is arranged in front of the right psoas muscle and the rachis".
Fig. 2.
The aforesaid mass has close contiguity relationships with the adjacent vertebral soma with evidence of a vascular peduncle of probable afferent vertebral origin.
On physical examination the patient appeared alert, with no signs of respiratory distress, without pallor or cyanosis, laboratory tests were normal, and the abdomen was treatable, with no pathological palpatory findings.
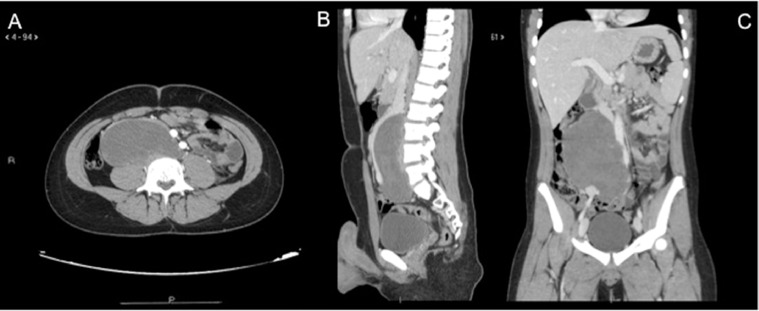
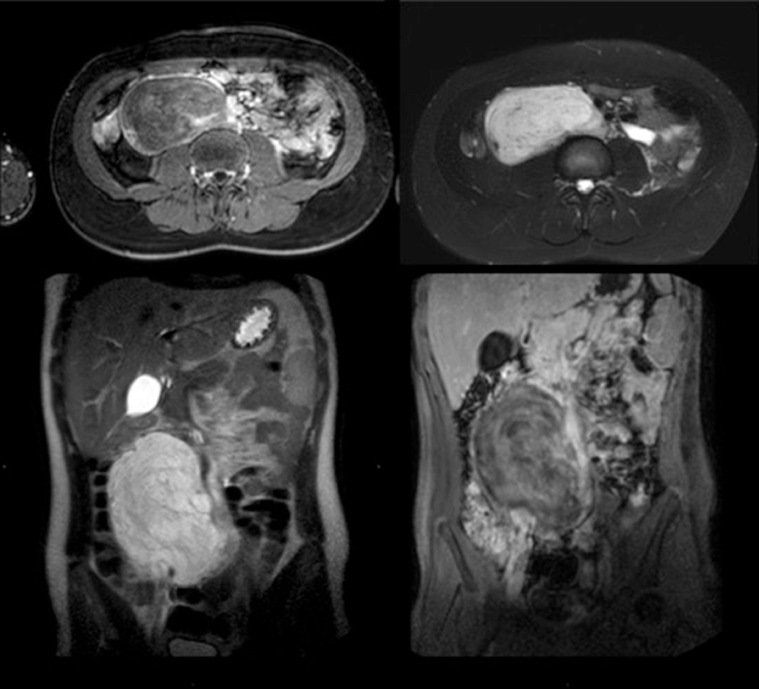
The patient also performed the CT examination (Fig. 3) with contrast medium of the abdomen and the MRI examination (Fig. 4) with contrast medium which allowed to complete the diagnostic procedure, addressing the diagnosis which was subsequently confirmed by the histological examination after surgical exeresis of the massive retroperitoneal ganglioneuromatous mass.
Fig. 3.
CT examination performed with contrast medium, axial acquisition (A) with reconstruction along the sagittal plane (B) and reconstruction in coronal (C), which confirms the presence of "bulky expansive retroperitoneal mass, with right median-paramedian site, which it does not have septa or calcifications or solid and / or adipose components.
Fig. 4.
Through magnetic resonance examination, a solid tissue peduncle, richly vascularized, indissociable from the right antero-lateral paravertebral space, was seen at the level of the L4 soma.
Discussion
The clinical manifestations of GN are diverse and in most cases the symptoms result from compression of the neoplasm which can cause vascular compression and pain in the lower abdomen, as happened to our young 15-year-old male patient who presented to ours observation with orchiepididymitis and pain in the lower abdomen, as ganglioneuromas are usually asymptomatic tumors, discovered randomly or characterized by non-specific symptoms, due to the mass effect and compression of nearby organs (vomiting and abdominal pain due to compression of the stomach or intestine; dyspnea due to compression on the diaphragm).
Ganglioneuroma usually represents a non-secreting tumor and can occasionally release hormones that can cause sweating and diarrhea, high blood pressure due to the secretion of catecholamines and intestinal vasoactive peptide [6], and can also cause tenesmus and weight loss. In our case, the patient presented no such complaints, but only orchiepididymitis and abdominal pain from venous compression and complete removal of the ganglioneuroma is described as adequate therapy with excellent prognosis [7].
Conclusion
Ganglioneuroma is a benign and bulky tumor that can lead to various complications and at the moment the post exeresis histological examination is the only approach to formulate an exact diagnosis, even if through a multimodal radiological diagnostic approach, such as the one we have provided to the patient. that came to our observation, it is possible to provide adequate information to direct the clinician towards a correct diagnosis.
Patient consent
The patient confirmed the consense for publication of our case report.
Footnotes
Competing Interests: The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
References
- 1.Shimada H, Ambros IM, Dehner LP, Hata J, Joshi VV, Roald B. Terminology and morphologic criteria of neuroblastic tumors: recommendations by the International Neuroblastoma Pathology Committee. Cancer. 1999;86:349–363. [PubMed] [Google Scholar]
- 2.Ambros IM, Hata J, Joshi VV, Roald B, Dehner LP, Tüchler H, et al. Morphologic features of neuroblastoma (Schwannian stromapoor tumors) in clinically favorable and unfavorable groups. Cancer. 2002;94:1574–1583. doi: 10.1002/cncr.10359. [DOI] [PubMed] [Google Scholar]
- 3.De Bernardi B, Gambini C, Haupt R, Granata C, Rizzo A, Conte M, et al. Retrospective study of childhood ganglioneuroma. J Clin Oncol. 2008;26:1710–1716. doi: 10.1200/JCO.2006.08.8799. [DOI] [PubMed] [Google Scholar]
- 4.Lonergan GJ, Schwab CM, Suarez ES, Carlson CL. Neuroblastoma, ganglioneuroblastoma, and ganglioneuroma: radiologic-pathologic correlation. Radiographics. 2002;22(4):911–934. doi: 10.1148/radiographics.22.4.g02jl15911. [DOI] [PubMed] [Google Scholar]
- 5.Hay ID, Wass JAH. Clinical endocrine oncology. 2008;67:p. 437-504.
- 6.Anila KR, Somanathan T, Hews AM, Jayasree K. Incidentally detected Ganglioneuroma of adrenal gland. J Case Rep Pract. 2014;2(2):45–47. [Google Scholar]
- 7.Sapalidis K, Mandalovas S., Kesisoglou I. Laparoscopic excision of an adrenal ganglioneuroma presented as an incindentaloma of the retro peritoneum. Curr Health Sci J. 2018;44(1):71–75. doi: 10.12865/CHSJ.44.01.12. Published online 2018 Feb 11. doi: 10.12865/CHSJ.44.01.12. [DOI] [PMC free article] [PubMed] [Google Scholar]