Abstract
Objectives
To evaluate patient factors associated with post-ureteroscopy opioid prescriptions, provider-level variation in opioid prescribing, and the relationship between opioid-free discharges and ED visits.
Methods
This is a retrospective analysis of a prospective cohort study of adults age 18 years and older who underwent primary ureteroscopy for urinary stones from June 2016 to September 2019 within the Michigan Urological Surgery Improvement Collaborative (MUSIC) Reducing Operative Complications from Kidney Stones (ROCKS) quality improvement initiative. Postoperative opioid prescription trends and variation among practices and surgeons were examined. Multivariable logistic regression models defined risk factors for receipt of opioid prescriptions. The association among opioid prescriptions and postoperative ED visits within 30 days of surgery was assessed among complete case and propensity matched cohorts, matched on all measured characteristics other than opioid receipt.
Results
13,143 patients underwent ureteroscopy with 157 urologists across 28 practices. Post-ureteroscopy opioid prescriptions and ED visits declined (86% to 39%, p<0.001; 10% to 6%, p<0.001, respectively). Practice and surgeon-level opioid prescribing varied from 8% to 98%, and 0% to 98%, respectively. Patient-related factors associated with opioid receipt included male, younger age, and history of chronic pain. Procedure-related factors associated with opioid receipt included pre-and post-ureteroscopy ureteral stenting and access sheath use. An opioid-free discharge was not associated with increased odds of an ED visit (OR 0.77, 95% CI 0.62-0.95, p=0.014).
Conclusions
There was no increase in ED utilization among those not prescribed an opioid after ureteroscopy, suggesting their routine use may not be necessary in this setting.
Keywords: Quality improvement, Ureteroscopy, Lithotripsy, Kidney Calculi, Analgesics, Opioid
Introduction
Kidney stones are highly prevalent, affecting an estimated 1 in 11 Americans, and are increasingly being treated with ureteroscopy.1,2 Opioid pain medications are overprescribed after surgery, which has contributed to the ongoing opioid abuse epidemic.3,4 Following ureteroscopy as many as 1 in 16 opioid-naïve patients will become new-persistent opioid users, defined as those continuing to fill an opioid prescription more than 90 days after surgery.5–7 These data and others have informed the creation of perioperative pain control guidelines, such as those by the American Pain Society, which recommend limiting opioids while encouraging multimodal pain control regimens.8 Urologists too have recognized this growing public health issue and recently published a consensus statement on opioid prescribing after urological surgery, which recommends judicious use of opioids after ureteroscopy.8
Though concerns about post-ureteroscopy opioid prescribing are gaining widespread attention, it is important to note that unplanned healthcare encounters, namely emergency department (ED) visits following ureteroscopy, are common and most often due to pain.9–11 Therefore, it is possible that patients not prescribed an opioid in the postoperative period could have increased ED visits due to poorly controlled pain and efforts to reduce postoperative opioid use could exacerbate this problem. These visits have a negative impact on patients in the form of diminished quality of life and productivity as well as on the healthcare system as a whole in the form of increased cost.9
Therefore, we used data from the Michigan Urological Surgery Improvement Collaborative’s Reducing Operative Complications from Kidney Stones (MUSIC ROCKS) clinical registry to understand the implications of an opioid-free pathway after ureteroscopy. In particular, we assessed patient factors associated with opioid receipt following ureteroscopy as well as provider level variation in opioid prescribing. After accounting for observed patient and clinical factors, and adjusting for correlation within provider and practice, we examined the relationship between opioid-free discharges and ED visits following ureteroscopy. We hypothesized that patients not prescribed opioids would have similar rates of emergency department visits as those that received a prescription. It is our intention that findings presented herein further support efforts to decrease opioid prescribing after ureteroscopy.
Materials and Methods
Data source
MUSIC is a collaborative quality improvement initiative comprised of a diverse group of community and academic urology practices across the state of Michigan. This initiative is funded by Blue Cross Blue Shield of Michigan (BCBSM) and includes more than 90% of practicing urologists in the state. MUSIC maintains a prospective clinical registry with data entered by trained abstractors at each participating practice. Data validity is confirmed through semi-annual site visits and chart audits. In 2016, MUSIC ROCKS was formed with the goal to improve the quality of care for patients with urinary stone disease. The ROCKS registry includes detailed demographic, clinical, and operative data for patients undergoing either ureteroscopy or shockwave lithotripsy for kidney stones.12 Patient data entry begins at the time of initial surgery (either ureteroscopy or shockwave lithotripsy) and outcomes such as unplanned ED visits or hospitalizations are tracked out to 60 days from the index procedure. Over the course of the study period the collaborative has developed and disseminated patient and physician educational resources, but no specific interventions, e.g. planned post-operative calls, etc. were implemented during the study period.
Study population and outcome measures
Using data from the ROCKS registry, we identified patients 18 years of age and older who underwent ureteroscopy for urinary stones from June 2016 to September 2019. Patients were excluded if they had an ipsilateral nephrostomy tube, underwent ureteroscopy as a second-stage lithotripsy procedure, had synchronous bilateral procedures, or had concomitant non-stone related surgery at the time of ureteroscopy. We chose these exclusion criteria in an attempt to create a more homogenous study population and limit confounding. Patients with an indwelling ureteral stent, but did not have first stage lithotripsy, were included. First we examined the rates of opioid and NSAID prescribing following ureteroscopy and factors associated with opioid prescriptions. We then assessed whether opioid-free discharges following ureteroscopy were associated with unplanned ED visits.
Statistical analysis
The proportion of patients over the study period who were prescribed opioid pain medication within 60 days after ureteroscopy are presented. The number of opioid pills dispensed when a prescription was given are reported by year and tested with ANOVA; year 2016 was excluded from the ANOVA as the number of pills dispensed was not routinely collected at that time. The frequency of NSAID prescriptions was similarly evaluated starting in 2018. The proportion of patients who presented to the ED within 30 days after ureteroscopy as well as the clinical diagnoses for the ED visit are reported.
We made bivariate comparisons of postoperative opioid prescription status with a variety of patient demographics, clinical characteristics, surgical characteristics, and patient outcomes, including: age, insurance type, comorbidity (as measured by the Charlson index),13 body mass index (BMI), sex, concomitant diagnosis of chronic pain, presence of a preoperative ureteral stent, urine culture (negative, positive, not performed), surgical acuity, stone size and location (ureteral, renal, both), placement of a ureteral stent, ureteral access sheath use, presence of an intraoperative complication, unplanned ED visit within 30 days, and readmission. Continuous variables were compared with t-tests and categorical variables with chi-square tests. Understanding that physician-level differences also dictate opioid prescribing patterns, we assessed practice-level and physician-level variation in opioid prescribing. For reliability purposes, when assessing practice-level data we only included those who had performed at least 10 ureteroscopy during the study period and used similar methods for the physician-level data.
Our goal was to determine both factors associated with receipt of a post-ureteroscopy opioid prescription, as well as whether receipt of an opioid prescription impacted ED utilization. To this end, we performed two distinct multivariable logistic regression mixed models. The first evaluated patient demographic, clinical, and surgical variables as fixed effects, with random effects of provider and practice, to understand factors independently associated with opioid receipt following ureteroscopy. The second was performed to assess whether post-ureteroscopy opioid prescriptions impacted unplanned ED visits, again using demographic, clinical, and surgical variables as fixed effects and provider and practice as random effects. Results from the first model indicated that there were significant differences among patients that did and did not receive opioids. Due to concerns that these differences may confound the relationship between opioid receipt and ED utilization, we performed propensity score matching with the goal of comparing ED utilization among groups that were similar in all measured aspects other than receipt of an opioid prescription. We calculated the probability of opioid receipt from our first model and used this as a propensity score (Supplemental Figure 1). The propensity scores showed a lack of overlap by opioid receipt group; therefore, a propensity score matched model was used to assess the association of opioid receipt with unplanned ED visits within 30 days. Patients were matched between opioid groups using a propensity score difference < 0.0015 with greedy matching without replacement.
All previously presented analyses were performed with a complete case model. However, opioid data was missing in 16.7% of patients. We thus performed a sensitivity analysis using multiple imputation of the missing data and repeating our previously described multivariable logistic regression models to test whether our findings persisted. The multiple imputation methods and results of the sensitivity analyses can be found in the supplement (Supplement methods and Supplement Table 2).
All statistical analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC) with a 2-sided type I error rate of 5%. Each MUSIC practice obtained an exemption or approval for collaborative participation from a local institutional review board. The University of Michigan institutional review board deemed this project exempt from review as it represents a quality improvement initiative.
Results
We identified 13,143 patients who underwent ureteroscopy during the study period (2016-2019) with 157 urologists across 28 practices. Of the 10,948 with data on opioid prescriptions, 6,383 (58%) were prescribed an opioid and 4,565 (42%) did not receive a prescription. Rates of opioid prescribing declined significantly over the course of the study (86% to 39%, p<0.001, Figure 1). Among cases where opioids were prescribed, the overall mean number of pills dispensed was 15.5 (SD 8.35). The mean number of pills dispensed decreased over time from 16.4 (SD 8.6) in 2018 to 13.3 (SD 6.6) in 2019 (p<0.001, Supplemental Table 1). Utilization of NSAIDs increased over time, from 34% of patients receiving a prescription in 2018 to 64% in 2019.
Figure 1.
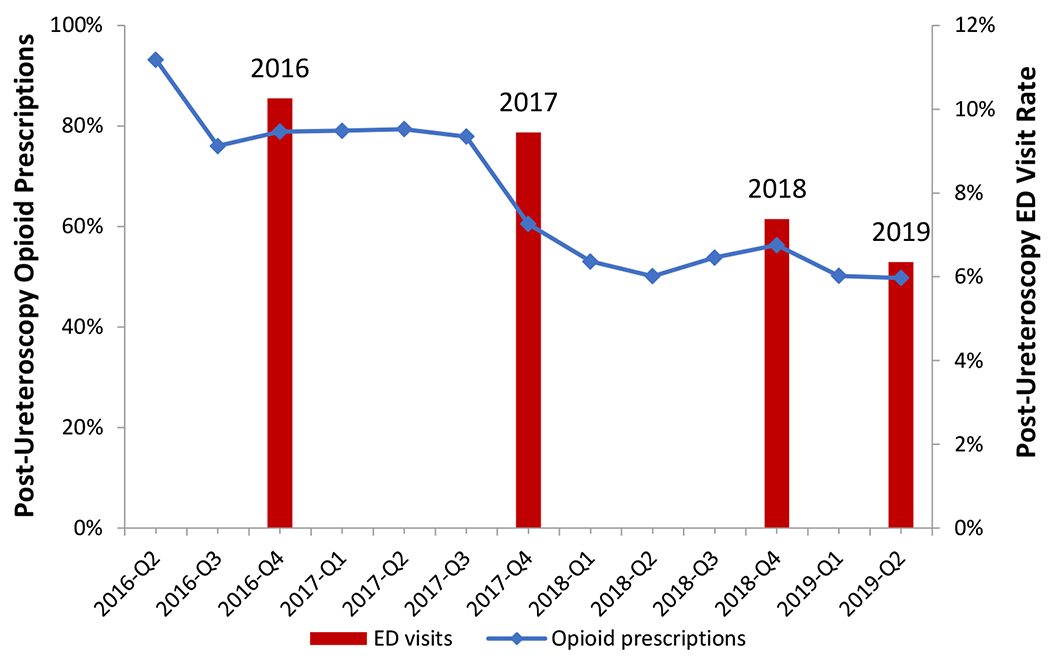
Trends in post-ureteroscopy opioid pain medication prescriptions within 60 days plotted by quarter and unplanned emergency department (ED) visits within 30 days plotted by year. Both the percentage of post-ureteroscopy patients prescribed opioid pain medication and the percentage that had an unplanned ED visit within 30 days decreased significantly over time (p < 0.001 for each trend).
Rates of ED utilization also decreased significantly over the study period (10% to 6%, p<0.001, Figure 1). The most common reasons for an unplanned ED visit — where patients could be included in more than one category — were flank pain (54%), hematuria (17%), fever (13%), nausea (13%), and abdominal pain (8%).
There was wide variation in post-ureteroscopy opioid prescribing across ROCKS practices. The percentage of post-operative patients prescribed opioid pain medications over the study period ranged 8% to 98% (p<0.001) (Figure 2a). At a surgeon-level, opioid prescriptions also varied, ranging from 0% to 98% of patients (p<0.001) (Figure 2b).
Figure 2a.
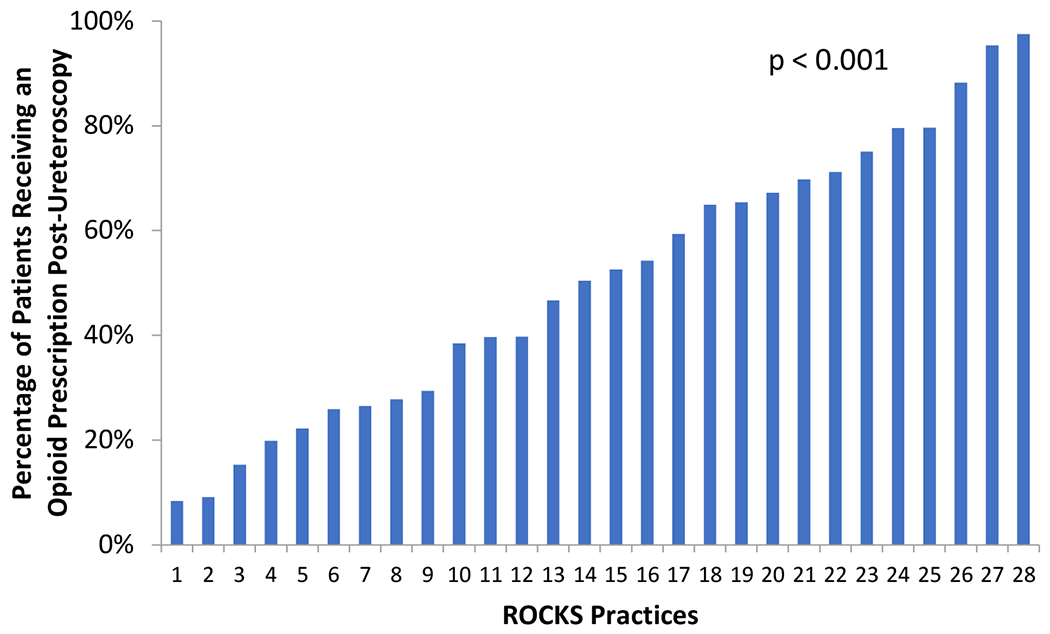
Variation in post-ureteroscopy opioid prescriptions across MUSIC urology practices among practices with at least 10 cases in the MUSIC ROCKS registry.
Figure 2b.
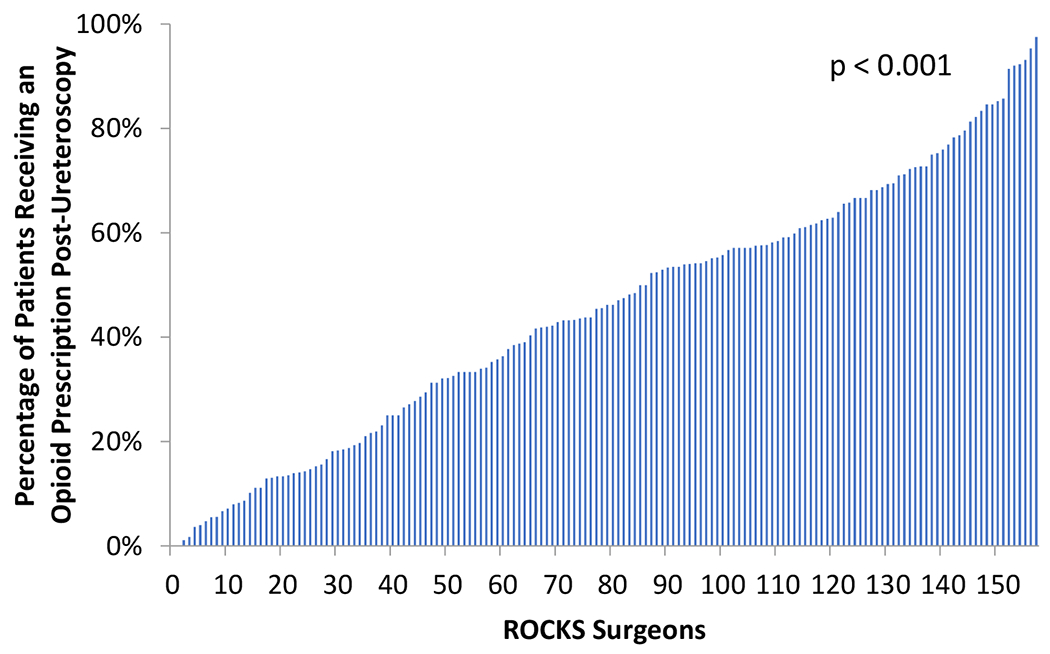
Variation in post-ureteroscopy opioid prescriptions across MUSIC urologists among urologists with at least 10 cases in the MUSIC ROCKS registry
Table 1 displays the differences in patient demographic, clinical and surgical variables among those who did and did not receive post-ureteroscopy opioid prescriptions. Additionally, it displays the balance of these covariates in the propensity-matched cohort demonstrated by small standardized differences. On multivariable logistic regression, factors independently associated with receipt of an opioid prescription included year (association with opioid prescriptions decreased over time), younger age, male sex, higher BMI, absence of a pre-operative ureteral stent, stent placed during surgery, and use of a ureteral access sheath (Table 2).
Table 1.
Demographics
| Entire Cohort | Matched Cohort | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Variable | No Opioids (N=4565) | Opioids (N=6383) | Total (n=13143) | p-value | No Opioids (N=2222) | Opioids (N=2222) | Standardized Difference | |
| Demographics | ||||||||
| Age, years | Mean (sd) | 57.7 (16.2) | 54.3 (15.7) | <0.001 | 56.5 (16.3) | 56.3 (15.7) | −0.01 | |
| Insurance | None | 102 (2.2%) | 157 (2.5%) | 305 | 0.01 | 50 (2.3%) | 43 (1.9%) | 0 |
| Private | 2578 (56.5%) | 3772 (59.1%) | 7724 | 1305 (58.6%) | 1316 (59.2%) | |||
| Public | 1854 (40.6%) | 2422 (37.9%) | 5045 | 871 (39.2%) | 863 (38.8%) | |||
| Charlson comorbidity index | 0 | 3106 (68.0%) | 4562 (71.5%) | 9318 | <0.001 | 1519 (68.4%) | 1537 (69.2%) | 0.06 |
| 1 | 751 (16.5%) | 1017 (15.9%) | 2092 | 389 (17.5%) | 362 (16.3%) | |||
| ≥2 | 707 (15.5%) | 801 (12.6%) | 1729 | 314 (14.1%) | 323 (14.5%) | |||
| unknown | 1 (0.0%) | 3 (0.1%) | 4 | |||||
| BMI | <25 | 941 (20.6%) | 1238 (19.4%) | 2558 | 0.004 | 476 (21.4%) | 490 (22.1%) | 0.03 |
| 25-30 | 1321 (28.9%) | 1932 (30.3%) | 3850 | 680 (30.6%) | 671 (30.2%) | |||
| 30-35 | 977 (21.4%) | 1448 (22.7%) | 2832 | 527 (23.7%) | 528 (23.8%) | |||
| >35 | 977 (21.4%) | 1541 (24.1%) | 2930 | 539 (24.3%) | 533 (24.0%) | |||
| unknown | 349 (7.7%) | 224 (3.5%) | 973 | |||||
| Sex | Male | 2092 (45.8%) | 3236 (50.7%) | 6437 | <0.001 | 1064 (47.9%) | 1070 (48.2%) | 0.01 |
| Female | 2473 (54.2%) | 3147 (49.3%) | 6706 | 1158 (52.1%) | 1152 (51.9%) | |||
| Chronic pain | no | 4486 (98.3%) | 6187 (96.9%) | 12830 | <0.001 | 2184 (98.3%) | 2188 (98.5%) | −0.01 |
| yes | 67 (1.5%) | 161 (2.5%) | 251 | 38 (1.7%) | 34 (1.5%) | |||
| unknown | 12 (0.3%) | 35 (0.6%) | 62 | |||||
| Clinical characteristics | ||||||||
| Prior ureteral stent | no | 2558 (56.0%) | 4125 (64.6%) | 7874 | <0.001 | 1308 (58.9%) | 1288 (58.0%) | 0.02 |
| yes | 1995 (43.7%) | 2251 (35.3%) | 5229 | 914 (41.1%) | 934 (42.0%) | |||
| unknown | 12 (0.3%) | 7 (0.1%) | 40 | |||||
| Urine culture | Positive | 600 (13.1%) | 814 (12.8%) | 1606 | <0.001 | 273 (12.3%) | 284 (12.8%) | 0.04 |
| Negative | 3077 (67.4%) | 4606 (72.2%) | 8997 | 1596 (71.8%) | 1593 (71.7%) | |||
| Not performed | 888 (19.5%) | 963 (15.1%) | 2540 | 353 (15.9%) | 345 (15.5%) | |||
| Surgical acuity | Elective | 3712 (81.3%) | 5157 (80.8%) | 10775 | 0.04 | 1836 (82.6%) | 1827 (82.2%) | −0.01 |
| Urgent/Emergent | 696 (15.3%) | 1077 (16.9%) | 1982 | 386 (17.4%) | 395 (17.8%) | |||
| unknown | 157 (3.4%) | 149 (2.3%) | 386 | |||||
| Stone location | Renal and ureteral | 769 (16.9%) | 1049 (16.4%) | 2111 | 0.008 | 389 (17.5%) | 372 (16.7%) | 0.06 |
| Renal | 980 (21.5%) | 1536 (24.1%) | 2981 | 506 (22.8%) | 469 (21.1%) | |||
| Ureter | 2637 (57.8%) | 3568 (55.9%) | 7530 | 1327 (59.7%) | 1381 (62.2%) | |||
| unknown | 179 (3.9%) | 230 (3.6%) | 521 | |||||
| Maximum Stone Diameter, mm | mean (std) | 7.4 (3.9) | 7.4 (3.7) | 0.9 | ||||
| Stone size | ≤0.5 cm | 1506 (33.0%) | 2101 (32.9%) | 4282 | 0.9 | 728 (32.8%) | 746 (33.6%) | 0.03 |
| >0.5-1cm | 2212 (48.5%) | 3103 (48.6%) | 6367 | 1134 (51.0%) | 1133 (51.0%) | |||
| >1cm | 671 (14.7%) | 965 (15.1%) | 1959 | 360 (16.2%) | 343 (15.4%) | |||
| unknown | 176 (3.9%) | 214 (3.4%) | 535 | |||||
| Surgical characteristics | ||||||||
| Stent during surgery | no | 1431 (31.4%) | 1430 (22.4%) | 3514 | <0.001 | 593 (26.%) | 593 (26.7%) | 0 |
| yes | 3131 (68.6%) | 4945 (77.5%) | 9606 | 1629 (73.3%) | 1629 (73.3%) | |||
| unknown | 3 (0.1%) | 8 (0.1%) | 23 | |||||
| Ureteral access sheath | no | 2995 (65.6%) | 3685 (57.7%) | 8137 | <0.001 | 1392 (62.7%) | 1430 (64.4%) | −0.04 |
| yes | 1521 (33.3%) | 2611 (40.9%) | 4812 | 830 (37.4%) | 792 (35.6%) | |||
| unknown | 49 (1.1%) | 87 (1.4%) | 294 | |||||
| Intra-operative complications | no | 4503 (98.6%) | 6287 (98.5%) | 12949 | 0.6 | 2191 (98.6%) | 2190 (98.6%) | 0 |
| yes | 56 (1.2%) | 90 (1.4%) | 168 | 31 (1.4%) | 32 (1.4%) | |||
| unknown | 6 (0.1%) | 6 (0.1%) | 26 | |||||
| Outcomes | p-value | |||||||
| Unplanned ED visit within 30 days | no | 4231 (92.7%) | 5736 (89.9%) | 12032 | <0.001 | 2047 (92.1%) | 2001 (90.1%) | 0.015 |
| yes | 297 (6.5%) | 605 (9.5%) | 991 | 175 (7.9%) | 221 (10.0%) | |||
| unknown | 37 (0.8%) | 42 (0.7%) | 120 | |||||
| 0.103 | ||||||||
| Readmission | no | 4391 (96.2% | 6100 (95.6%) | 12613 | 0.003 | 2137 (96.6%) | 2119 (95.7%) | |
| yes | 131 (2.9%) | 253 (4.0%) | 419 | 75 (3.4%) | 96 (4.3%) | |||
| missing | 43 (0.9%) | 30 (0.5%) | 111 | |||||
Table 2.
Multivariable logistic regression model assessing factors independently associated with Opioid prescription after ureteroscopy (N=9499)
| Variable | Adjusted OR | 95% CI | p-value | |
|---|---|---|---|---|
| Year | ||||
| 2016 | 15.73 | 12.18 | 20.30 | <0.0001 |
| 2017 | 9.36 | 7.91 | 11.07 | <0.0001 |
| 2018 | 2.75 | 2.44 | 3.10 | <0.0001 |
| 2019 | Ref | _ | _ | _ |
| Age, years | 0.99 | 0.98 | 0.99 | <0.0001 |
| Insurance | ||||
| Public | Ref | _ | _ | _ |
| None | 1.04 | 0.741 | 1.46 | 0.82 |
| Private | 1.07 | 0.96 | 1.19 | 0.22 |
| Charlson comorbidity index | ||||
| 0 | Ref | _ | _ | _ |
| 1 | 0.98 | 0.854 | 1.127 | 0.79 |
| ≥ 2 | 0.87 | 0.746 | 1.009 | 0.07 |
| Gender | ||||
| Female | Ref | _ | _ | _ |
| Male | 1.29 | 1.168 | 1.431 | <0.0001 |
| BMI category | ||||
| ≤ 25 | Ref | _ | _ | _ |
| >25 - 30 | 1.21 | 1.05 | 1.383 | 0.008 |
| >30 - 35 | 1.22 | 1.049 | 1.408 | 0.009 |
| >35 | 1.22 | 1.056 | 1.415 | 0.007 |
| Urine culture | ||||
| Negative | Ref | _ | _ | _ |
| Positive | 0.88 | 0.758 | 1.03 | 0.1 |
| Not performed | 0.86 | 0.743 | 0.991 | 0.03 |
| Stone location | ||||
| Ureter | Ref | _ | _ | _ |
| Both | 1.04 | 0.904 | 1.186 | 0.6 |
| Renal | 1.13 | 0.993 | 1.291 | 0.06 |
| Prior stent | ||||
| No | Ref | _ | _ | _ |
| Yes | 0.88 | 0.783 | 0.987 | 0.03 |
| Procedure acuity | ||||
| Urgent | Ref | _ | _ | _ |
| Elective | 0.95 | 0.813 | 1.099 | 0.46 |
| Intraoperative complications | ||||
| No | Ref | _ | _ | _ |
| Yes | 0.80 | 0.523 | 1.213 | 0.29 |
| Stent during surgery | ||||
| No | Ref | _ | _ | _ |
| Yes | 1.49 | 1.315 | 1.698 | <0.0001 |
| Stone diameter, mm | ||||
| ≤ 5 | Ref | _ | _ | _ |
| >5 - 10 | 1.02 | 0.915 | 1.145 | 0.69 |
| >10 | 1.09 | 0.923 | 1.278 | 0.32 |
| Chronic pain | ||||
| No | Ref | _ | _ | _ |
| Yes | 1.42 | 0.983 | 2.044 | 0.062 |
| Ureteral access sheath | ||||
| No | Ref | _ | _ | _ |
| Yes | 1.30 | 1.153 | 1.47 | <0.0001 |
Emergency department (ED)
Michigan Urological Surgery Improvement Collaborative (MUSIC)
Reducing Operative Complications from Kidney Stones (ROCKS)
Blue Cross Blue Shield of Michigan (BCBSM)
An opioid-free discharge was independently associated with decreased odds of an unplanned ED visit (OR 0.77, 95% CI 0.62-0.95, p = 0.014) in our propensity-matched logistic regression model (Supplemental Table 2). This finding persisted in our sensitivity analyses using multiple imputation to address the missingness in opioid prescription data (Supplemental Table 3).
Discussion
We examined data from the diverse urology practices of the MUSIC ROCKS registry and found a dramatic decline in post-ureteroscopy opioid prescriptions over time, with an absolute decrease in prescriptions of 47% over the 3-year time period of our study. Still, there was wide variation in opioid prescribing across practices and providers. Factors independently associated with receipt of an opioid prescription included year (association with opioid prescriptions decreased over time), younger age, male sex, higher BMI, absence of a pre-operative ureteral stent, stent placed during surgery, and use of a ureteral access sheath (Table 2). After adjusting for patient demographics, clinical and surgical characteristics, surgeon, and practice, an opioid-free discharge following ureteroscopy was not associated with an increase in ED visits within 30 days of surgery. In fact, our model suggested an opioid-free discharge was associated with lower odds of an ED visit. Utilization of NSAIDs was low overall but increased over time.
The decline in post-ureteroscopy opioid prescriptions observed in our study is consistent with a national trend toward decreasing opioid prescribing over time amongst surgical subspecialists.14 Additionally, the wide variation in post-ureteroscopy opioid prescribing we observed is not entirely surprising, as prior work has also demonstrated variation in post-operative opioid prescriptions.15–18 Within urology, others have seen decreased opioid prescribing over time, such as in the management of acute renal colic and after major prostate and renal surgery.19,20 Still, this is the first study, to our knowledge, to specifically examine the trends in opioid prescribing patterns over time amongst patients undergoing ureteroscopy and assess the association of opioid prescriptions with unplanned healthcare encounters. These trends are likely multifactorial, and may be due in part to legislative changes, increased physician and patient awareness of the risks of opioids, guideline statements on perioperative pain control, and increasing evidence in the literature on the feasibility of opioid-free ureteroscopy. Although not specifically evaluated in our study, the demographic, clinical, and surgical factors that were independently associated with receipt of an opioid prescription may relate to case complexity, intraoperative ureteral manipulation, and perceived patient pain tolerance.
The association between an opioid-free discharge and decreased ED utilization was an unexpected finding, as we hypothesized that there would be no difference among those who did and did not receive opioids. This association persisted in our sensitivity analyses, although we suspect that this finding is likely due to unmeasured confounding in our observational study, potentially related to disease severity. Several previously published small, retrospective single institution or surgeon studies did not find a significant difference in post-ureteroscopy ED utilization among patients in whom opioids were or were not prescribed.21–23 Similarly, a recent single institution prospective study of an opioid sparing enhanced recovery pathway did not find a difference in unplanned healthcare encounters among patients managed with and without post-ureteroscopy opioid prescriptions.24
Our study does have several potential limitations. First, the rate of post-ureteroscopy opioid prescriptions may be higher than the immediate post-operative prescription rate reported herein if patients are obtaining an opioid prescription at pre-operative health care encounters, such as for renal colic, and have unused pills or subsequent health care encounters after surgery. That said, data abstractors are trained to enter any prescription within 60 days following ureteroscopy regardless of prescribing clinician, although they did not have access to the Michigan prescription monitoring program used to track controlled substances. Second, the reasons for the declining rate of post-ureteroscopy opioid prescriptions over time, as well as the variation amongst practices and surgeons, are likely multifactorial, and incompletely measured in this study. On the other hand, a detailed investigation of the drivers of opioid prescribing is beyond the scope of the study. Third, likely due in part to large sample size, there were numerous statistically significant differences in the comparisons among groups; however, the clinical significance of these differences is admittedly questionable. Fourth, we did not track postoperative phone calls or office visits, which may have been associated with opioid prescription utilization. Still, these healthcare encounters are typically less burdensome and costly to the patients, providers, and the health system compared with ED visits. Lastly, although we found that an opioid-free discharge was associated with decreased ED utilization, our study was observational in nature and not designed to specifically evaluate this outcome. Nevertheless, our findings do suggest that an opioid omitting pain control strategy is safe and does not increase unplanned ED visits.
Despite these limitations, our findings have implications for patients, surgeons, and policymakers. For patients, omitting a post-ureteroscopy opioid prescription avoids the risks associated with their use, and does not increase the likelihood of an unplanned ED visit — an often burdensome and costly encounter with the healthcare system. For surgeons, wide variation in opioid prescribing suggests potential to further drive down opioid prescription rates and opportunities to increase NSAID use for post-ureteroscopy pain management. Although the drivers of this variation are incompletely measured here, we can hypothesize that there may be differences in prescribers’ perceptions of opioid and NSAID safety and effectiveness in this setting. For policymakers, opioid sparing pain management strategies appear feasible and do not increase ED utilization, potentially making ureteroscopy an attractive target for incentive-based payment modifications for procedures performed without opioid prescriptions. This was implemented in the State of Michigan by one of the payors in July of 2019, at the conclusion of our study period.25
Conclusions
We observed a substantial decline in post-ureteroscopy opioid prescribing in the state of Michigan between 2016 and 2019. Wide variation in post-ureteroscopy opioid prescriptions across MUSIC ROCKS practices and surgeons suggests opportunities for quality improvement to drive continued reduction in opioid prescribing. Patients not prescribed an opioid pain medication following ureteroscopy did not have increased ED utilization compared with those who received opioids, although further study is needed to elucidate the impact of opioid-free discharges on patient reported outcomes. These results provide reassurance to urologists that routine use of opioids following ureteroscopy may not be necessary.
Supplementary Material
References:
- 1.Scales CD, Smith AC, Hanley JM, Saigal CS. Prevalence of kidney stones in the United States. Eur Urol. 2012;62(1):160–165. doi: 10.1016/j.eururo.2012.03.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chung KJ, Kim JH, Min GE, et al. Changing Trends in the Treatment of Nephrolithiasis in the Real World. J Endourol. 2019;33(3):248–253. doi: 10.1089/end.2018.0667 [DOI] [PubMed] [Google Scholar]
- 3.Vu JV, Gunaseelan V, Brummett CM, Waljee JF, En. Statewide Implementation of Postoperative Opioid Prescribing Guidelines. N Engl J Med. 2019;381(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Theisen KM, Myrga JM, Hale N, et al. Excessive Opioid Prescribing After Major Urologic Procedures. Urology. 2019;123:101–107. doi: 10.1016/j.urology.2018.06.057 [DOI] [PubMed] [Google Scholar]
- 5.Tam CA, Dauw CA, Ghani KR, et al. New Persistent Opioid Use After Outpatient Ureteroscopy for Upper Tract Stone Treatment. Urology. 2019:103–108. doi: 10.1016/j.urology.2019.08.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kang C, Shu X, Herrell SD, Miller NL, Hsi RS. Opiate Exposure and Predictors of Increased Opiate Use after Ureteroscopy. J Endourol. 2019;33(6):480–485. doi: 10.1089/end.2018.0796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hosier GW, McGregor T, Beiko D, et al. Persistent Opioid Use Among Patients with Urolithiasis: A Population based Study. Eur Urol Focus. 2019:1–7. doi: 10.1016/j.euf.2019.08.011 [DOI] [PubMed] [Google Scholar]
- 8.Koo K, Faisal F, Gupta N, et al. Recommendations for Opioid Prescribing after Endourological and Minimally Invasive Urological Surgery: An Expert Panel Consensus. J Urol. 2019;203(January):151–158. doi: 10.1097/ju.0000000000000514 [DOI] [PubMed] [Google Scholar]
- 9.Scales CD, Saigal CS, Hanley JM, Dick AW, Setodji CM, Litwin MS. The impact of unplanned postprocedure visits in the management of patients with urinary stones. Surg (United States). 2014;155(5):769–775. doi: 10.1016/j.surg.2013.12.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Du K, Wang RS, Vetter J, et al. Unplanned 30-Day Encounters after Ureterorenoscopy for Urolithiasis. J Endourol. 2018;32(12):1100–1107. doi: 10.1089/end.2018.0177 [DOI] [PubMed] [Google Scholar]
- 11.Tan HJ, Strope SA, He C, Roberts WW, Faerber GJ, Wolf JS. Immediate unplanned hospital admission after outpatient ureteroscopy for stone disease. J Urol. 2011;185(6):2181–2185. doi: 10.1016/j.juro.2011.01.081 [DOI] [PubMed] [Google Scholar]
- 12.Dauw CA, Swarna K, Qi J, et al. Shockwave Lithotripsy Use in the State of Michigan: American Urological Association Guideline Adherence and Clinical Implications. Urology. 2020;137:38–44. doi: 10.1016/j.urology.2019.11.037 [DOI] [PubMed] [Google Scholar]
- 13.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A New Method of Classifying Prognostic in Longitudinal Studies : Development. J Chronic Dis. 1987;40(5):373–383. http://www.sciencedirect.com/science/article/pii/0021968187901718. [DOI] [PubMed] [Google Scholar]
- 14.Romman AN, Hsu CM, Chou L, Kuo Y. Opioid Prescribing to Medicare Part D Enrollees , 2013 – 2017 : Shifting Responsibility to Pain Management Providers. 2020;0(0):1–9. doi: 10.1093/pm/pnz344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fujii MH, Hodges AC, Russell RL, et al. Post-Discharge Opioid Prescribing and Use after Common Surgical Procedure. J Am Coll Surg. 2018;226(6):1004–1012. doi: 10.1016/j.jamcollsurg.2018.01.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ziegelmann MJ, Joseph JP, Glasgow AE, et al. Wide Variation in Opioid Prescribing After Urological Surgery in Tertiary Care Centers. Mayo Clin Proc. 2019;94(2):262–274. doi: 10.1016/j.mayocp.2018.08.035 [DOI] [PubMed] [Google Scholar]
- 17.Berger I, Strother M, Talwar R, et al. National Variation in Opioid Prescription Fills and Long-Term Use in Opioid Naïve Patients after Urological Surgery. J Urol. 2019;202(5):1036–1043. doi: 10.1097/ju.0000000000000343 [DOI] [PubMed] [Google Scholar]
- 18.Thiels CA, Anderson SS, Ubl DS, et al. Wide Variation and Overprescription of Opioids after Elective Surgery. Ann Surg. 2017;266(4):564–573. doi: 10.1097/SLA.0000000000002365 [DOI] [PubMed] [Google Scholar]
- 19.Myrga JM, Macleod LC, Bandari J, Jacobs BL, Davies BJ. Decrease in Urologic Discharge Opioid. Urology. 2020;139:84–89. doi: 10.1016/j.urology.2020.02.002 [DOI] [PubMed] [Google Scholar]
- 20.Kominsky H, Rose J, Lehman A, et al. Trends in acute pain management for renal colic in the emergency department at a tertiary care academic medical center. J Endourol. 2020;(614):1–31. doi: 10.1089/end.2020.0402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Milburn PA, Thai KH, El Mekresh A, Lowry PS, El Tayeb MM. Relation of postoperative pain medication to return for unplanned care after ureteroscopy. Baylor Univ Med Cent Proc. 2019;32(2):199–201. doi: 10.1080/08998280.2019.1573715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Large T, Heiman J, Ross A, Anderson B, Krambeck A. Initial Experience with Narcotic-Free Ureteroscopy: A Feasibility Analysis. J Endourol. 2018;32(10):907–911. doi: 10.1089/end.2018.0459 [DOI] [PubMed] [Google Scholar]
- 23.Sobel DW, Cisu T, Barclay T, Pham A, Callas P, Sternberg K. A Retrospective Review Demonstrating the Feasibility of Discharging Patients Without Opioids After Ureteroscopy and Ureteral Stent Placement. J Endourol. 2018;32(11):1044–1049. doi: 10.1089/end.2018.0539 [DOI] [PubMed] [Google Scholar]
- 24.Gridley C, Robles J, Calvert J, et al. Enhanced Recovery After Surgery Protocol for Patients Undergoing Ureteroscopy: Prospective Evaluation of An Opioid-Free Protocol. J Endourol. 2020:1–21. doi: 10.1089/end.2019.0552 [DOI] [PubMed] [Google Scholar]
- 25.Blue Cross Blue Shield of Michigan. BCBSM promotes effective pain control through limiting post-operative opioid dispensing in Pain Control Optimization Pathways (POP). Record. June 2019. Available at: https://michigan-open.org/wp-content/uploads/2019/10/BCBSM.Modifier-22.FAQ_.7.23.19.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


