Abstract
Screen time has been associated with overweight and obesity, as well as with poorer dietary quality. However, the reasons explaining these associations are not well understood. The objectives of this cross-sectional study were (1) to determine the extent of overall TV viewing as well as using screens while eating (e.g., watching TV or using a tablet), (2) to compare food and nutrient consumption of on- versus off-screen eating occasions, and (3) to determine whether TV viewing and using screens while eating is associated with overall dietary intake. Participants were from the Food Environment Chilean Cohort (n=938, 4–6 y) and the Growth and Obesity Cohort Study (n=752, 12–14 y). Dietary data was collected via one 24-h food recall. For each eating occasion, activity performed during consumption (e.g., watching TV, playing sports) was reported. Weekly TV viewing time was collected via an additional survey instrument. Analyses included multivariable linear and logistic regression. Post-hoc pairwise comparisons examined differences in outcomes by tertiles. Our sample reported a median of 9 to 13.5 weekly hours of TV viewing and 87.5% reported consuming at least one meal or snack per day while using screens. The median kilocalories contributed by eating during screen use was 387 kcal/d in children and 848 kcal/day in adolescents, which represents 34.7% and 42.3 % of daily energy intake, respectively. There were no consistent differences when comparing eating occasions consumed on-screen versus off-screen. Higher weekly TV viewing was associated with elements of a less healthy diet including more sweets and desserts in children, and more sugar sweetened beverages in adolescents. A large percentage of Chilean children and adolescents’ daily energy is consumed while using screens. In depth, longitudinal work is needed to understand how screen time eating affects diet quality and nutritional status.
Keywords: Screen time, television viewing, diet, children, adolescents
1. INTRODUCTION1
Screen time is a broad term commonly used to refer to a collection of sedentary behaviors, including television (TV) viewing, playing video games, computer use and use of other electronic devices, such as smartphones and tablets (1). Screen time has been linked to a wide range of physical, social and emotional outcomes in childhood (2) and in particular, the association between screen time and obesity has been widely studied (3, 4) in a number of cross-sectional (5–7) and longitudinal studies (8–10). At least three mechanisms have been proposed to explain these associations (11): reduced physical activity attributable to increased time spent engaging in a sedentary behavior (3), the effect of unhealthy food marketing on eating behaviors (12) and thirdly, distracted eating due to screen use during meals which might lead to overeating (4).
Until recently, TV viewing remained the most common form of screen time among children and adolescents (3). Therefore, most of the literature examining these associations to date has focused on overall TV viewing (4, 13). For the purposes of this study, however, other screens in addition to TV which might be used while eating are also of interest, such as tablets and smartphones. Among children, TV viewing while eating has been related to lower consumption of fruits and vegetables and higher consumption of sugar-sweetened beverages and high-fat/high-sugar foods (13). Likewise, among adolescents, TV viewing during meals has been associated with lower intakes of vegetables, calcium-rich food, and grains and higher intakes of soft drinks (14) and lower overall dietary quality (15). Furthermore, the presence of a TV during family meals has also been found to be negatively associated with the healthfulness and the emotional atmosphere of the meal (16).
A key question that remains unanswered is whether children who spend more hours in front of a screen are also more likely to eat a greater proportion of their calories during screen use. A second question of interest is whether TV viewing and using screens while eating are associated with overall dietary intake. Progress in this area has been difficult because most studies lack information on actual food intake during screen time. Instead, many studies have assessed the association between screen time and dietary intake, regardless of whether the dietary intake actually occurred while using screens (10, 17–19). For example, they might assess whether TV viewing is associated with consumption of specific food groups; but assess the consumption of these food groups using a food frequency instrument that does not capture whether the food was consumed while using screens. In addition, the few studies that do have a detailed measure of intake during screen use (20–22) lack information regarding total time spent during the week using screens. We seek to add to the body of literature regarding screen time behaviors and diet by combining dietary data from a 24-hour food recall questionnaire with data from a media exposure questionnaire in a sample of children and adolescents. The 24-hour food recall captures screen time eating behaviors, while the media exposure questionnaire allows for the assessment of screen time, in this case, TV viewing.
To address these gaps, this paper has three objectives utilizing two cohort studies. Firstly, we determine the extent of overall TV viewing as well as using screens while eating (e.g. watching TV or using a phone or tablet), in our samples, in addition to the correlation between these two different, but likely related exposures. Then, we compare food and nutrient consumption of on- versus off-screen eating occasions. Finally, we determine whether TV viewing and using screens while eating is associated with overall dietary intake.
2. METHODS
2.1. Participants and setting
In this cross-sectional study, participants were preschool children and adolescents from two Chilean cohorts: the Food Environment Chilean Cohort (FECHIC) and the Growth and Obesity Cohort Study (GOCS). Both study cohorts were recruited from low- and middle-income neighborhoods in the southeastern area of Santiago, Chile. Recruitment strategies and inclusion and exclusion criteria of both cohorts have been described elsewhere (23–25). FECHIC included children who were singleton births (as opposed to twins or multiple births), whose mothers were in charge of food purchases at home and primary caregivers of children, and who had no mental health condition or gastrointestinal diseases that would affect food consumption. These children were recruited in 2016. GOCS participants were recruited in 2006 when they were 3–5 years old, and included children who were a single birth with a birthweight > 2,500 grams, who were enrolled the previous year in the National Nursery Schools Council Program (JUNJI, acronym for the name in Spanish) and who did not have physical or psychological conditions that could severely affect growth. In 2016 these children were 12–14 years old and constituted our adolescent group.
Data collection for this study included completion of a media use questionnaire and one 24-hour dietary recall, which are explained in more detail in section 2.2 (Measures). Because of missing data on total weekly TV viewing time (n=34), dietary variables (n=46), and self-reported caloric intakes outside the plausible range (<400 kilocalories (kcal), n=2), the final analytic sample consisted of 1690 participants (preschool children, n=938; adolescents, n=752). For both cohorts, we obtained written informed consent from parents or legal guardians of participants; in the case of adolescents, we also obtained an assent prior to data collection. The ethics committee of the Institute of Nutrition and Food Technology approved the study protocol.
2.2. Measures
2.2.1. Weekly TV viewing time
This included mother-reported (for preschoolers) and self-reported (adolescents) TV viewing. We assessed the number of TV viewing hours within a typical week with an adaptation of the Global Weekly Estimate of TV viewing (26). The adapted instrument asked participants to estimate hours of TV viewing during six different periods: weekdays before school, after school until 10pm, and from 10pm until sleep time and weekends before noon, from noon until 10pm, and from 10pm until sleep. For each period, the response categories were “no hours” (=0), “less than an hour” (=0.5 to represent midpoint of range), “between one and two hours” (=1.5, to represent midpoint of range), and more than two hours (=3, as a conservative estimate, although participants might have viewed more than 3 hours, particularly during afternoons). Additionally, participants reported the number of days the TV was on in a typical week in the household. To create an estimate of weekly TV viewing hours, we combined the sum of the reported hours of TV viewing within each of the six periods, with the typical number of days per week of television use, an approach that has been previously used (27, 28) and that we describe in more detail in Supplementary File 1.
2.2.2. Dietary intake
This study includes dietary data collected between April and July of 2016. Trained nutritionists conducted 24-hour dietary recalls, using a multiple-pass method assisted by a computer software (SER-24). In the GOCS cohort, adolescents reported their own intake. For the FECHIC cohort, the mother (primary caregiver) completed the recall, with input from child. A food atlas (29) was used to assess serving sizes of common Chilean food and beverages, with use of images such as bowls, plates, mugs and glasses. Participants’ responses were entered to SER-24; and the information was later reviewed by a second nutritionist to check for inconsistencies and ensure data quality in reporting. One 24-hour dietary recall was used for each participant.
Respondents identified name and time of eating occasions during the interviews. Participants reported items as either breakfast, colación (smaller meal or snack), lunch, once (sit-down meal typically consisting of bread and an assortment of fixings -such as jam, butter, avocado and cheese- and done in late afternoon), dinner, and picoteo (snack or small appetizer). In most cases, once might replace dinner.
Additionally, for each eating occasion participants were asked what activity they engaged in during food consumption: watching TV or on a phone, sitting, standing, studying, playing sports, walking or riding in a bus, car or other (transportation). Day of week of the dietary recall and place of consumption were also reported. Nutrient values were calculated with the use of the United States Department of Agriculture (USDA) Food and Nutrient Database (30–32) for non-packaged products. For packaged products, we obtained nutrient values from the nutrition facts panel of the product’s package, which was collected using a standardized protocol (33). For cases in which participants did not mention product brand for the packaged product consumed, we used the most similar product in our database in terms of name, flavor and description. We linked all eating occasions, foods, and their corresponding nutrients to activity performed during consumption.
For this analyses, grams and energy contribution (in kilocalories) of ready-to-eat (RTE) breakfast cereals, salty snacks, sweets and desserts, sugar-sweetened beverages, milks and yogurt, and fruits were assessed for each participant, by eating occasion and at the daily level. Sugar-sweetened beverages included industrial flavored waters, sports and energy drinks, sodas (non-diet), and fruit and vegetable drinks (with added sugar). The first four groups are energy-dense products commonly marketed on television to children and adolescents globally (34), whereas the consumption yogurt, milk and fruits is an indicator of improved diet quality and thus promoted in dietary guidelines (35). Supplementary File 2 includes a list of common foods and beverages included in each one of these groups.
2.2.3. Using screens while eating
We derived this variable from the dietary intake data, which was reported by participants in the case of adolescents, or their mothers, in the case of preschoolers. We dichotomized activity performed concurrently during food and beverage consumption into “screen time”, which included consumption while watching TV or on phone, and “non-screen time”, which included all other activities mentioned (e.g. sitting, standing, playing sports, walking, or riding the bus or car). We then calculated the number of eating occasions and the percent of total energy intake (in kilocalories) consumed while using screens for each study participant.
2.2.4. Socio demographics
In the children cohort, mothers reported sex and birthdate of child during interviews. For adolescents, the information was self-reported. This study did not collect data on household income. However, education is a commonly used proxy for socio-economic status (36, 37) and thus, maternal education level is our main socio-economic variable, which we categorized in three groups: less than high school, high school complete and above high school.
2.3. Data Analyses
All analyses were conducted using Stata Version 14 (38). We used descriptive statistics to present sociodemographic characteristics, as well as the extent of weekly TV viewing and using screens while eating among study participants. We then determined per capita and per consumer energy intake of key food/beverage groups consumed on-screen versus off-screen. Per capita refers to the mean consumption using our total sample as a denominator (stratified by age group), and per consumer refers to the mean consumption of a food/beverage group among those who reported consuming it.
Because many studies report only screen time (such as TV viewing) rather than using screens while eating, it is important to determine how well weekly TV viewing might or might not capture using screens while eating. We examined the correlation of TV viewing and using screen while eating with the Spearman’s Rank correlation coefficient (39) (continuous variables: hours/week and % kcal during screen time).
2.3.1. Eating occasion analyses
The eating occasion level of analyses allows us to differentiate screen vs non-screen time consumption, since each eating occasion could have been performed (and thus, reported) doing a different activity. Using multivariable linear regression models, we compared energy (kcal), percent energy from total sugars, percent energy from saturated fats, and sodium per 1000 kcal of eating occasion performed during on-screen time with those consumed off-screen time, while accounting for correlated errors due to repeated measures of eating occasions within individuals during a single day.
In our models, the primary outcome was the continuous variable for nutrients and the main independent predictor was a dichotomous variable for whether or not the eating occasion was done during screen time. Because the screen time – nutrient association might vary by type of eating occasion (meal versus snack), we additionally included an interaction term (screen*meal) in our models. These models additionally controlled for day of the food recall (week vs. weekend/holiday), location of consumption (school vs. not at school), sex, age and mother’s education level. Location of consumption was included as a covariate to account for the possibility of it confounding the relationship between screens and dietary intake. Pairwise comparisons were computed at an α level of 0.05 to examine differences in nutrient densities between screen- and off-screen eating occasions, within each type of eating occasion.
To estimate the probability of consumption of our key food and beverage groups, we created dichotomous variables for each group. Logistic regression models were used to estimate the association between on- and off-screen time consumption of food and beverage groups at a particular eating occasion. Similar to our nutrient density analysis, the model included an interaction term (screen*meal) and controlled for key covariates.
2.3.2. Daily consumption analyses
Our second analysis focused on examining the association between (1) weekly TV viewing and (2) using screens while eating with daily total intake. Thus, the unit of analysis was each study participant. To assess these associations, we created tertiles based on (1) energy intake consumed while using screens and (2) weekly TV viewing hours, both stratified by age group. The approach of categorizing the exposure via tertiles (or other quantiles) is common in the screen time literature (40–42), and was considered more appropriate given the distribution of the exposures of interest, as well as to ensure similar sample size within each comparison group. Additionally, there might have been measurement error when assessing TV viewing, and therefore we considered it more appropriate to group the sample into levels of viewing as opposed to considering hours as an exact amount. Finally, by categorizing into tertiles, we reduce the effect of extreme values of our exposures in the estimated associations. We conducted crude (simple regression with one predictor – either TV viewing or using screens while eating) and multivariable regression models (to examine the associations of interest using the aforementioned control variables and used post-hoc pairwise comparisons to examine differences in our main outcomes by tertiles, compared to our reference tertile (lowest category).
3. RESULTS
The mean age was 4.8±0.5 y for preschool children and 13.7±0.4 y for adolescents. 51.2% of children and 49.9% of adolescents were female. Maternal education level was lower in the adolescent cohort, as reflected by the greater percent who had not completed high school (29.1% in adolescents vs 17.7% in children) (Table 1).
Table 1.
Socio demographic characteristics, television viewing and using screens while eating in study sample stratified by sex
| Characteristics | Children | Adolescents | ||||||
|---|---|---|---|---|---|---|---|---|
| Girls (n=480) | Boys (n=458) | Girls (n=375) | Boys (n=377) | |||||
|
| ||||||||
| Socio demographics | ||||||||
| Age (y; mean, sd) | 4.8 | 4.8±0.5 | 4.8 | 4.8±0.5 | 13.7 | 13.7±0.4 | 13.6 | 13.6±0.4 |
| Mother’s education level1 (%) | ||||||||
| Less than high school | 94 | 19.6 | 72 | 15.7 | 96 | 26.1 | 119 | 32.2 |
| High school complete | 194 | 40.4 | 195 | 42.6 | 188 | 51.1 | 162 | 43.8 |
| More than high school | 192 | 40.0 | 191 | 41.7 | 84 | 22.8 | 89 | 24.1 |
| TV viewing 2 | ||||||||
| Number of TVs in home (mean, sd) | 3.1±1.1 | 3.1±1.2 | 3.3±1.2 | 3.3±1.1 | ||||
| Weekly hours reported (median, range) | 9 h, 0–45 | 10.5 h, 0–49.5 | 13.5 h, 0–50.5 | 11.5 h, 0–44.5 | ||||
| Total weekly use (%) | ||||||||
| None | 45 | 9.4 | 53 | 11.6 | 20 | 5.3 | 31 | 8.2 |
| Less than 14 hours | 284 | 59.2 | 241 | 52.6 | 176 | 46.9 | 189 | 50.1 |
| 14 hours or more | 151 | 31.5 | 164 | 35.8 | 179 | 47.7 | 157 | 41.6 |
| Using screens while eating 3 | ||||||||
| Per capita energy intake (kcal; median, iqr) | 375, 425 | 407, 487 | 580, 727 | 748, 971 | ||||
| Per capita energy intake (% of total) | 34.8, 36.7 | 34.4, 38.9 | 38.7, 46.7 | 43.8, 47.6 | ||||
| Percentage consuming | 86.2 | 87.3 | 84.6 | 84.9 | ||||
| Per consumer4 intake (kcal; median, iqr) | 422, 382 | 461, 457 | 680, 648 | 893, 842 | ||||
| Per consumer intake (%; median, iqr) | 38.7, 34.9 | 39.1, 34.6 | 44.5, 37.1 | 48.2, 42.7 | ||||
| Eating occasion frequency during screen time (%)5 | ||||||||
| Breakfast | 49.3 | 51.6 | 33.6 | 37.5 | ||||
| Lunch | 36.6 | 32.7 | 34.3 | 37.6 | ||||
| Once | 49.7 | 54.5 | 59.7 | 64.4 | ||||
| Dinner | 46.4 | 40.2 | 68.8 | 67.2 | ||||
| Any meal | 80.2 | 79.5 | 74.3 | 75.7 | ||||
| Any snack (picoteo or colación) | 48.3 | 51.1 | 56.3 | 57.6 | ||||
| .. Number of eating occasions during screen time (%) | ||||||||
| . None | 58 | 12.1 | 53 | 11.6 | 51 | 13.6 | 52 | 13.8 |
| .. One to two | 258 | 53.8 | 241 | 52.6 | 197 | 52.5 | 179 | 47.5 |
| .. Three to four | 136 | 28.3 | 149 | 32.5 | 114 | 30.4 | 124 | 32.9 |
| .. Five or more | 28 | 5.8 | 15 | 3.3 | 13 | 3.5 | 22 | 5.8 |
Missing data for 14 adolescents.
Calculated with data from media exposure questionnaire.
Calculated from 24-hour recalls.
Those consuming at least one eating occasion during screen time.
Percent calculated with number of participants consuming each type of eating occasion as the denominator.
3.1. TV viewing and using screens while eating
Children reported a median of 9 to 10.5 hours of weekly TV viewing, whereas in adolescents it was 11.5 to 13.5 hours. Using screens while eating was common in both age groups, with over 85% of participants reporting at least one eating occasion a day during screen use, and about a third of participants (30.4% children and 31.6% adolescents) reporting 3–4 eating occasions using screens. The median kilocalories contributed by using screens while eating was 387 kcal/d in children and 848 kcal/day in adolescents, which represents 34.7% and 42.3 % of daily energy intake, respectively.
Among children, breakfast and once were the meals most frequently consumed while using screens, while among adolescents, dinner and once were the meals most frequently consumed while using screens. More than half of our sample (49.7% children and 57.0% adolescents) reported at least one snack per day while using a screen.
Associations between using screens while eating and weekly TV viewing use variables are reported in Table 2. Overall, the Spearman correlations were weak for both children and adolescents, for the whole week as well as only on weekend and weekdays separately (range 0.07 to 0.16).
Table 2.
Spearman correlations of participant’s weekly television viewing (hours/week) with using screens while eating (% total kcal)
| Using screens while eating1 | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| Weekdays | Weekend days | Overall | |||||||
|
|
|||||||||
| Rho | 95%CI | p-value | Rho | 95%CI | p-value | Rho | 95%CI | p-value | |
|
| |||||||||
| Children | 0.14 (n2=802) | [0.07, 0.21] | <.05 | 0.07 (n=136) | [−0.10, 0.23] | 0.43 | 0.13 (n=938) | [0.06, 0.20] | <.05 |
| Adolescents | 0.16 (n=612) | [0.08, 0.24] | <.05 | 0.16 (n=140) | [−0.01, 0.33] | 0.06 | 0.16 (n=752) | [0.09, 0.23] | <.05 |
Variable operationalized from 24-hour recalls.
Sample size refers to number of participants (each participant contributed one food recall in the analysis)
3.2. Foods consumed during screen time and off screen time
As shown in the Figure 1, most food groups contributed to a greater percent of energy off-screen when compared to on-screen, which can be explained because at the daily level, overall more calories were consumed off-screen. Supplementary File 4 provides further details in the per capita and per consumer mean energy intakes of these key food groups.
Figure 1.
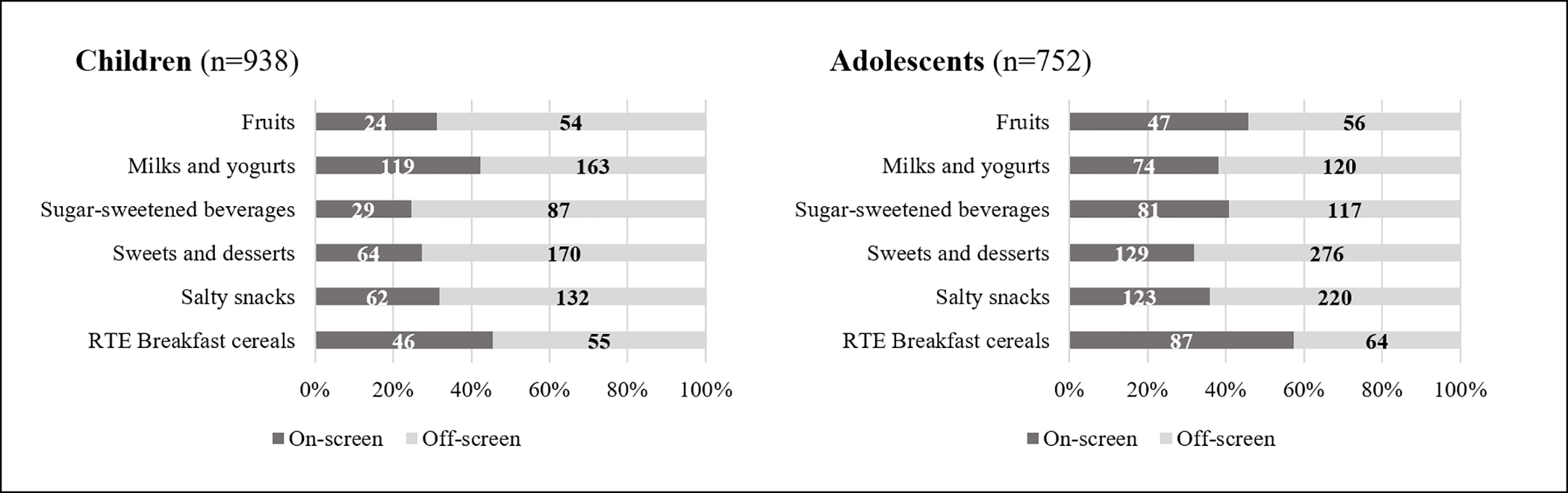
Proportion of energy intake from key food groups consumed on- versus off-screen, in children and adolescents (numbers in figure are in kilocalories).
3.3. Eating occasion analyses with and without concurrent screen use
Table 3 shows nutrient density and predicted probability of food group consumption during eating occasions with and without concurrent screen use. Among children, screen use meals were higher in total sugars (as a percent of energy intake) but lower in overall energy, than non-screen use meals. In contrast, screen use snacks were lower in total sugars compared to non-screen time snacks (p<0.05). During screen use meals, RTE breakfast cereals, sweets and desserts, and milk and yogurts were more likely to be consumed, whereas fruits were less likely to be consumed. For snacks, sugar-sweetened beverages were less likely to be consumed during screen use snacks, whereas milks and yogurts were more likely to be consumed during screen use (p<.05)
Table 3.
Comparison of nutrient densities and food group consumption during eating occasions with and without concurrent screen time1
| Children | Meals Screen (n=1,383) | Non-screen (n=1,826) | Snacks Screen (n=613) | Non screen (n=1,545) | ||||||||||
|
| ||||||||||||||
| Nutrients | mean | se | mean | se | Dif | p-value | mean | se | mean | se | Dif | p-value | ||
| Energy (kcal) | 249 | 4 | 265 | 4 | −17 | 5 | 0.00 | 150 | 5 | 152 | 4 | −1 | 6 | 0.80 |
| Total sugars (% kcal) | 28 | 1 | 25 | 0 | 3 | 1 | 0.00 | 46 | 1 | 50 | 1 | −4 | 1 | 0.01 |
| Total saturated fats (% kcal) | 10 | 0 | 10 | 0 | 0 | 0 | 0.37 | 9 | 0 | 8 | 0 | 0 | 0 | 0.35 |
| Total sodium (mg/100 kcal) | 131 | 3 | 138 | 3 | −7 | 4 | 0.08 | 80 | 5 | 85 | 6 | −5 | 9 | 0.55 |
| Food Groups | % | se | % | se | Dif | % | Se | % | se | Dif | ||||
| RTE Breakfast cereals | 6.1 | 0.7 | 3.0 | 0.4 | 3.1 | 0.8 | 0.00 | 7.3 | 1.1 | 6.2 | 0.6 | 1.1 | 1.3 | 0.38 |
| Salty snacks | 0.5 | 0.2 | 0.4 | 0.2 | 0.1 | 0.3 | 0.78 | 5.8 | 1.1 | 4.3 | 0.5 | 1.5 | 1.3 | 0.23 |
| Sweets and desserts | 11.9 | 1.0 | 9.0 | 0.7 | 2.8 | 1.2 | 0.02 | 29.8 | 1.9 | 31.7 | 1.3 | −1.9 | 2.4 | 0.42 |
| SSBs | 18.5 | 1.1 | 18.2 | 0.9 | 0.3 | 1.5 | 0.86 | 12.7 | 1.5 | 19.8 | 1.0 | −7.1 | 1.9 | 0.00 |
| Milk and yogurts | 45.4 | 1.4 | 39.8 | 1.0 | 5.6 | 1.9 | 0.00 | 34.5 | 2.0 | 28.8 | 1.2 | 5.7 | 2.5 | 0.02 |
| Fruits | 10.2 | 0.9 | 12.8 | 0.8 | −2.6 | 1.1 | 0.02 | 19.7 | 1.7 | 19.5 | 1.1 | 0.2 | 2.1 | 0.92 |
|
| ||||||||||||||
| Adolescents | Meals Screen (n=985) | Non-screen (n=1,265) | Snacks Screen (n=562) | Non-screen (n=1,192) | ||||||||||
|
| ||||||||||||||
| Nutrients | mean | se | mean | se | Dif | p-value | mean | se | mean | se | Dif | p-value | ||
| Energy (kcal) | 445 | 9 | 428 | 8 | 17 | 13 | 0.19 | 223 | 10 | 244 | 8 | −21 | 14 | 0.14 |
| Total sugars (% kcal) | 19.2 | 1 | 21.0 | 1 | −2 | 1 | 0.04 | 42 | 1 | 39 | 1 | 3 | 2 | 0.12 |
| Total saturated fats (% kcal) | 9.2 | 0 | 9.1 | 0 | 0 | 0 | 0.74 | 9 | 0 | 10 | 0 | −1 | 0 | 0.03 |
| Total sodium (mg/100 kcal) | 149.0 | 5 | 139.0 | 3 | 10 | 6 | 0.10 | 88 | 21 | 108 | 13 | −20 | 26 | 0.45 |
| Food Groups | % | se | % | se | Dif | % | se | % | se | Dif | ||||
| RTE Breakfast cereals | 3.2 | 0.6 | 2.7 | 0.5 | 0.6 | 0.7 | 0.43 | 5.2 | 1.0 | 3.5 | 0.6 | 1.8 | 1.2 | 0.13 |
| Salty snacks | 0.6 | 0.3 | 0.8 | 0.3 | −0.2 | 0.4 | 0.54 | 10.6 | 1.6 | 7.9 | 1.0 | 2.7 | 2.1 | 0.20 |
| Sweets and desserts | 11.4 | 1.2 | 12.1 | 0.9 | −0.7 | 1.5 | 0.67 | 37.8 | 2.3 | 39.6 | 1.6 | −1.8 | 3.0 | 0.55 |
| SSBs | 27.1 | 1.6 | 24.5 | 1.2 | 2.6 | 2.1 | 0.21 | 20.4 | 1.8 | 18.4 | 1.2 | 2.0 | 2.3 | 0.37 |
| Milk and yogurts | 17.2 | 1.3 | 25.0 | 1.2 | −7.8 | 1.8 | 0.00 | 14.6 | 1.5 | 12.5 | 1.1 | 2.0 | 1.9 | 0.29 |
| Fruits | 11.4 | 1.2 | 11.3 | 0.9 | 0.1 | 1.5 | 0.95 | 17.3 | 1.8 | 10.7 | 1.1 | 6.6 | 2.2 | 0.00 |
Model adjusted for sex, age in months, maternal education level, day of interview (weekday vs weekday/holiday), and location of consumption (school vs. not at school).
Standard errors adjusted for 938 clusters (in children) and 738 clusters (in adolescents).
Among adolescents, there were no major differences when comparing the nutrient profile of screen use to non-screen use meals and snacks. Compared to non-screen use eating occasions, screen use meals were slightly lower in percent of total sugar (p<0.05) and screen time snacks were slightly lower in saturated fats, compared to non-screen use snacks (p<0.05). During screen time meals, milks and yogurts were less likely to be consumed than during non-screen time, whereas for snacks, fruits were more likely to be consumed during screen use compared to off-screen.
3.4. Daily consumption analyses
As displayed in Table 4, children who consumed a greater proportion of their energy while using screens consumed more total daily sugars (% energy) and less fruits (g) than children who consumed the least energy while using screens (p<0.05). Among adolescents, higher eating during screen use was associated with lower total daily intake of energy, saturated fat, sweets and desserts and fruit consumption.
Table 4a.
Predicted daily nutrient intake by consumption during screen time (% kcal) and tertiles of TV viewing (weekly hours), among children.
|
Using screens while eating
|
||||||||
|
Tertile 1 (n=313)
Range: 0–21.7% kcal |
Tertile 2 (n=313)
Range: 21.8–46.9% |
Tertile 3 (n=312)
Range: 47.0–100% |
p-value | |||||
| mean | se | mean | se | mean | se | 2 vs 1 | 3 vs 1 | |
|
| ||||||||
| Nutrients | ||||||||
| Energy (kcal) | 1,260 | 22 | 1,243 | 22 | 1,210 | 22 | 0.59 | 0.10 |
| Total sugars (% energy) | 27.7 | 0.5 | 29.1 | 0.5 | 29.2 | 0.5 | 0.03 | 0.02 |
| Saturated fat (% energy) | 9.7 | 0.2 | 9.9 | 0.2 | 9.9 | 0.2 | 0.30 | 0.36 |
| Sodium (mg/1000 kcal) | 1208 | 25 | 1217 | 25 | 1220 | 25 | 0.80 | 0.74 |
| Food Groups | ||||||||
| RTE Breakfast cereals (g) | 6.9 | 0.8 | 6.9 | 0.8 | 7.0 | 0.8 | 0.97 | 0.90 |
| Salty snacks (g) | 3.8 | 0.9 | 5.5 | 0.9 | 4.2 | 0.9 | 0.19 | 0.77 |
| Sweets and desserts (g) | 54.4 | 3.5 | 51.2 | 3.5 | 45.9 | 3.5 | 0.51 | 0.09 |
| SSBs (g) | 155.4 | 10.8 | 163.9 | 10.8 | 155.2 | 10.8 | 0.58 | 0.99 |
| Milks and yogurts (g) | 282.4 | 12.5 | 260.4 | 12.5 | 294.6 | 12.5 | 0.21 | 0.49 |
| Fruits (g) | 80.6 | 5.2 | 66.5 | 5.2 | 61.1 | 5.2 | 0.06 | 0.01 |
|
| ||||||||
|
Weekly hours of television viewing
|
||||||||
|
Tertile 1 (n=324)
Range: 0 – 5.5 h |
Tertile 2 (n=304)
Range: 5.6 – 14 h |
Tertile 3 (n=310)
Range: 14.5 – 49.5 h |
p-value | |||||
| mean | se | mean | se | mean | se | 2 vs 1 | 3 vs 1 | |
|
| ||||||||
| Nutrients | ||||||||
| Energy (kcal) | 1,222 | 21 | 1,243 | 22 | 1,249 | 22 | 0.50 | 0.38 |
| Total sugars (% energy) | 28.7 | 0.5 | 28.8 | 0.5 | 28.5 | 0.5 | 0.91 | 0.83 |
| Saturated fat (% energy) | 9.6 | 0.2 | 9.9 | 0.2 | 10.0 | 0.2 | 0.29 | 0.19 |
| Sodium (mg/1000 kcal) | 1186 | 24 | 1210 | 25 | 1251 | 25 | 0.49 | 0.06 |
| Food Groups | ||||||||
| RTE Breakfast cereals (g) | 7.7 | 0.8 | 6.9 | 0.8 | 6.1 | 0.8 | 0.46 | 0.14 |
| Salty snacks (g) | 4.4 | 0.9 | 3.8 | 0.9 | 5.1 | 0.9 | 0.65 | 0.57 |
| Sweets and desserts (g) | 42.9 | 3.5 | 54.8 | 3.6 | 54.2 | 3.5 | 0.02 | 0.02 |
| SSBs (g) | 163.9 | 10.6 | 142.2 | 10.9 | 167.8 | 10.8 | 0.16 | 0.80 |
| Milks and yogurts (g) | 280.6 | 12.3 | 280.4 | 12.7 | 276.3 | 12.6 | 0.99 | 0.81 |
| Fruits (g) | 73.2 | 5.1 | 69.0 | 5.3 | 65.8 | 5.3 | 0.57 | 0.32 |
Model adjusted for sex, age in months, mother’s education level, and day of interview (weekday versus non-weekday).
Children reporting more weekly TV viewing consumed more sweets and desserts (in grams). Adolescents reporting more weekly TV viewing consumed on average more energy and sugar-sweetened beverages (SSBs) (in grams), and less milk and yogurt (in grams) (Table 4). While there was also a tendency in both children and adolescents, towards lesser consumption of fruits with higher reported TV viewing, the differences were not statistically significant.
4. DISCUSSION
We found that among Chilean children and adolescents, using screens while eating was very common (more than 85% of sample reporting screen time consumption), and that children consumed a notable proportion of their daily calories while using a screen (34.7% and 42.3 % of daily energy intake for children and adolescents, respectively). When comparing eating occasions consumed on-screen versus off-screen, there were no consistent differences in the nutrient profile or food groups consumed for either age group. However, our daily consumption analyses revealed that higher weekly hours of TV viewing was associated with elements of a less healthy diet including more sweets and desserts in children, and more sugar sweetened beverages in adolescents.
Overall TV viewing was lower than in other Latin American countries such as Brazil (43) and Mexico (44) and much lower than the US. In the US, for example, the average TV viewing time was close to 2.5 hours/day, but when other forms of media use were taken into account, the total amount of screen time was between 5 and 12 hours/day depending on age group (45). Nevertheless, screen time in Chile (~ 2h and 2.5 h, for children and adolescents, just in TV viewing) surpasses recommendations to limit screen time use to 1 hour/day (46) in children 2–5 years and <2 hours/day (47) for children and teens 5 to 17 years.
Despite lower TV viewing time, using screens while eating was more common and contributed to a higher proportion of total daily calories in Chile compared to the United States. Specifically, one study conducted in a small US sample found that children consumed 17–26% of daily energy intake during TV viewing, compared to 36–43% in this study (20). These differences between both studies could be due to study setting (place and year) as well as in how screen time consumption was defined. Over 70% of our sample reported at least one main meal in front of a screen, which is similar to a recent UK study (22), but higher than in Brazil (~60%) (48) and Canada (~30%) (49). The eating occasions most frequently consumed while using a screen in our sample were breakfast and once, in children, and dinner and once for adolescents. Because once often replaces dinner, our results are similar to what was found in the US (20) and in Mexico (50) in which dinner and snacks were most frequently consumed while on a screen.
The high proportion of calories and eating occasions consumed while on a screen in our sample is of concern, given previous research linking poor diet quality to screen time consumption (13). However, in our study, we did not find a large, consistent association between using screens while eating and nutritional quality (as measured by % of calories from critical nutrients or by more- or less- healthy food groups) when we examined this relationship at the eating occasion level. For children, at the eating occasion level, on-screen meals were associated with a higher percent of energy from total sugar, but the opposite was found for snacks. At meals consumed on-screen, children were more likely to consume breakfast cereals, desserts/sweets, and milk and yogurt than off-screen, which could be a reflection of the fact that breakfast was the most commonly meal consumed on-screen. Surprisingly, sugary drinks were actually less likely to be consumed during snacks consumed while viewing a screen. Meanwhile, adolescents, there were only trivial differences in the nutritional profile for on- vs. off- screen snacks and meals, with similarly small differences found for food groups consumed.
These mixed results were further reflected when we analyzed the association between using screens while eating and total daily intake. Children who consumed the most calories on-screen consumed a higher percent of sugar and less fruit. However, adolescents who consumed the most calories on-screen consumed fewer total calories, a lower percentage of saturated fat, and less sweets and desserts, and fruit. Although somewhat surprising, previous studies have also reported mixed findings. For example, while one recent study found that children who watched TV during meals consumed on average 6% more energy from ultra-processed foods overall, compared to those who did not (22), another study (21) did not find significant associations between increased TV viewing at meals and overall diet quality.
When we examined the relationship between TV viewing (i.e. overall, not during the meal) and diet, we found more consistent associations between higher TV viewing and poorer dietary quality, although the differences remained relatively small. For example, we found that children watching more TV consumed more sweets and desserts, and adolescents with higher TV viewing consumed more SSBs, and milks and yogurts. While there was also a tendency towards lesser consumption of fruits with higher reported TV viewing, the differences were not statistically significant. One explanation for our observed associations is that there might be unmeasured characteristics that are related to screen time, such as parenting style, which also might drive or affect children’s dietary behaviors. For example, parental self-efficacy to limit screen time has been associated with children’s screen time (51), and it could also be related to self-efficacy of other family dietary behaviors. In that sense, it is plausible that parents who can effectively restrict their children’s weekly TV viewing, might also more effectively counteract child’s requests for sugary-beverages or unhealthy snacks or treats specially in younger children.
A second aspect to consider is TV food and beverage advertising. Children and adolescents are exposed to unhealthy food marketing around the globe (34). Across different countries, the products that are advertised tend to be high in energy, saturated fats, sugars, and sodium, and be of little nutritional value (34). Unhealthy food and beverage marketing affects children’s food preferences, choice and consumption (52, 53) of advertised products, and in Chile, products commonly advertised on TV during the same time period than when our data collection took place included sodas and sweet desserts (cookies, chocolate, candies, and bakery) (54). Our results suggest that the increase in consumption of advertised products might not necessarily be during screen time itself, but at other times of the day (at least for adolescents), since we did not observe a consistent increased likelihood of consumption of typically advertised products during screen time. For example, in adolescents, SSBs were as likely to be consumed at meals with or without screens and those with higher proportion of energy consumed while on screens did not consume more SSBs. However, those with higher weekly TV viewing had higher consumption of SSBs overall. Likewise, in preschoolers, higher weekly TV viewing (and not using screens while eating) was associated with consumption of sweets and desserts. If we believe that food marketing might be the major driver of these associations, then our results suggest that discouraging overall screen time as a behavior might be more important than discouraging consumption during screen time itself; indeed, the two were not well correlated and it was only weekly TV viewing that was linked with poor diet.
Further research will also be needed to understand the relationship between non-TV screen time, eating behaviors, and dietary intake. Most of the research conducted to date has focused on TV viewing as the main form of screen time. However, child-directed TV supply, as well as the consumption of TV media has dropped in Chile over the past 3 years (55), with 2018 representing an all-time low in the average time on TV among children and adolescents. Furthermore, adolescents are the age group that most frequently reports use of TV via internet or streaming. Because research has shown that unhealthy food ads predominate in content on digital platforms such as YouTube (56, 57) Facebook (57) and Instagram (58), an area for future research is understanding how other forms of screen time (not only TV viewing) are related to diet, given the potential effects of unhealthy food marketing on these platforms.
Our study has several limitations. Because of questionnaire design and data available for the study, we were unable to distinguish between the eating that might have occurred with use of different devices (tablets, smartphones, computers, TVs, for example) and with different types of activities (video gaming, video watching, social media). It is possible that the relationship between screen time and dietary intake also depends on the type of device and activity. Second, our study sample was recruited from Southeastern Santiago, potentially limiting generalizability. However, 92% of Chilean children and adolescents (1st-8th grade) attend public funded schools (59), as does our sample, and we therefore believe that our sample is to an extent characteristic of this age group in Chile. Thirdly, as with any dietary study, our results are subject to the possibility of misreporting. In particular, the parents/caregivers of our younger participants might not have been aware of all foods consumed by the child, in particular during the school day, and even though we attempted to complement our information with the use of school lunch menus, it is always possible that the information is incomplete. In addition, the dietary intake was from a one-day period, which might not be representative of children and adolescents’ usual food consumption, nor of their typical screen time eating behaviors. Finally, our analyses did not include all food groups that might be indicative of dietary quality (vegetables, whole grains, nuts and seeds, for example).
Despite these limitations, several strengths are important to mention. First, our data enabled us to assess not only the behavior of using screens while eating, but also, how overall TV viewing relates to dietary intake. This allowed us to gain insights on the relative associations of each behavior, and whether behavioral interventions and recommendations should focus on discouraging one behavior versus the other. Second, our eating occasions analysis included a substantial sample, allowing us to compare on- versus off-screen time consumption with more level of detail than other studies have done. Furthermore, unlike other studies that also focused on the eating occasion level (21, 22), we did not restrict our analyses to main meals, but also captured snacks, providing a more complete picture of the associations of interest.
In conclusion, a large percentage of children and adolescents’ daily energy intake is consumed during screen use. Overall TV viewing, as well as using screens while eating were associated with some aspects of an unhealthy diet. The low correlation between using screens while eating and overall TV viewing highlights their unique importance in understanding the pathways linking screen time to diet quality and overweight. Further research is needed to fully understand the role of TV viewing and using screens while eating in diet quality, and whether obesity prevention interventions and policies should prioritize discouragement of these behaviors.
Supplementary Material
Table 4b.
Predicted daily nutrient intake by consumption during screen time (% kcal) and tertiles of TV viewing (weekly hours), among adolescents.
|
Using screens while eating
|
||||||||
|
Tertile 1 (n=251)
Range: 0–26.7% |
Tertile 2 (n=251)
Range: 26.8–56.8 |
Tertile 3 (n=250)
Range: 56.9–100% |
p-value | |||||
| mean | se | mean | se | mean | se | 2 vs 1 | 3 vs 1 | |
|
| ||||||||
| Nutrients | ||||||||
| Energy (kcal) | 1,953 | 41 | 1,782 | 41 | 1,840 | 41 | 0.00 | 0.05 |
| Total sugars (% energy) | 21.6 | 0.6 | 21.9 | 0.6 | 21.5 | 0.6 | 0.64 | 0.98 |
| Saturated fat (% energy) | 10.2 | 0.2 | 9.6 | 0.2 | 9.5 | 0.2 | 0.02 | 0.01 |
| Sodium (mg/1000 kcal) | 1294 | 29 | 1316 | 29 | 1346 | 29 | 0.60 | 0.21 |
| Food Groups | ||||||||
| RTE Breakfast cereals (g) | 4.7 | 1.1 | 6.2 | 1.0 | 7.0 | 1.1 | 0.33 | 0.13 |
| Salty snacks (g) | 14.6 | 2.4 | 16.2 | 1.0 | 9.3 | 2.4 | 0.65 | 0.12 |
| Sweets and desserts (g) | 105.5 | 6.7 | 69.5 | 2.4 | 76.6 | 6.7 | 0.00 | 0.00 |
| SSBs (g) | 321.1 | 24.2 | 332.5 | 6.7 | 341.1 | 24.2 | 0.74 | 0.56 |
| Milks and yogurts (g) | 193.4 | 12.4 | 170.0 | 24.1 | 154.9 | 12.3 | 0.18 | 0.03 |
| Fruits (g) | 69.8 | 6.5 | 73.6 | 12.3 | 53.8 | 6.5 | 0.68 | 0.08 |
|
| ||||||||
|
Weekly hours of television viewing
|
||||||||
|
Tertile 1 (n=269)
Range: 0 – 8.5 h |
Tertile 2 (n=235)
Range: 8.6 – 18.5 h |
Tertile 3 (n=248)
Range: 19 – 50.5 h |
p-value | |||||
| mean | se | mean | se | mean | se | 2 vs 1 | 3 vs 1 | |
|
| ||||||||
| Nutrients | ||||||||
| Energy (kcal) | 1,791 | 39 | 1,827 | 42 | 1,958 | 41 | 0.52 | 0.00 |
| Total sugars (% energy) | 21.2 | 0.5 | 21.8 | 0.6 | 22.0 | 0.6 | 0.48 | 0.31 |
| Saturated fat (% energy) | 10.0 | 0.2 | 9.8 | 0.2 | 9.5 | 0.2 | 0.59 | 0.09 |
| Sodium (mg/1000 kcal) | 1356 | 28 | 1282 | 30 | 1314 | 29 | 0.08 | 0.31 |
| Food Groups | ||||||||
| RTE Breakfast cereals (g) | 6.8 | 1.0 | 6.2 | 1.1 | 4.9 | 1.0 | 0.66 | 0.19 |
| Salty snacks (g) | 12.7 | 2.3 | 10.7 | 2.5 | 16.5 | 2.4 | 0.56 | 0.26 |
| Sweets and desserts (g) | 84.6 | 6.6 | 81.9 | 7.0 | 84.6 | 6.8 | 0.79 | 0.99 |
| SSBs (g) | 286.6 | 23.3 | 318.6 | 24.8 | 391.7 | 24.0 | 0.35 | 0.00 |
| Milks and yogurts (g) | 196.7 | 11.9 | 160.8 | 12.7 | 158.2 | 12.3 | 0.04 | 0.03 |
| Fruits (g) | 67.2 | 6.3 | 64.7 | 6.7 | 65.1 | 6.5 | 0.79 | 0.82 |
Model adjusted for sex, age in months, mother’s education level, and day of interview (weekday versus non-weekday).
Acknowledgements
The authors thank Karen Ritter for her assistance with data management. They also thank Leonela Muñoz, Cindy Granados, Catalina Cornejo, and Natalia Rebolledo for support with food and beverage grouping and understanding key aspects related to the data collection process in Chile.
Funding
Funding for this study came from Bloomberg Philanthropies, IDRC Grant 108180-001 (INTA-UNC); the Comisión Nacional de Investigación Científica y Tecnológica (CONICYT; grant number FONDECYT #1161436), the NIH National Research Service Award (Global Cardiometabolic Disease Training Grant) #T32 HL129969-01A1, and the Population Research Infrastructure Program awarded to the Carolina Population Center (P2C HD050924) at The University of North Carolina at Chapel Hill. Funders had no role in the study design, data collection, analysis or interpretation of results.
1. List of abbreviations throughout manuscript
- FECHIC
Food Environment Chilean Cohort
- GOCS
Growth and Obesity Cohort Study
- Kcal
kilocalories
- RTE
ready to eat
- SSBs
sugar-sweetened beverages
- TV
television
- USDA
United States Department of Agriculture
Footnotes
Ethics Statement
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects/patients were approved by the Ethics Committee of the Institute of Nutrition and Food Technology (INTA) at the University of Chile, and by the Institutional Review Board of the University of North Carolina (UNC) at Chapel Hill. Written informed consent was obtained from all subjects or their legal guardian. In the case of adolescents, we also obtained an assent prior to data collection.
Availability of data and material
The datasets generated and/or analyzed during the current study are not publicly available, but are available under request to the corresponding author.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
5. REFERENCES
- 1.Stiglic N, Viner RM. Effects of screentime on the health and well-being of children and adolescents: a systematic review of reviews. BMJ open. 2019;9(1):e023191–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reid Chassiakos YL, Radesky J, Christakis D, Moreno MA, Cross C. Children and Adolescents and Digital Media. Pediatrics. 2016;138(5). [DOI] [PubMed] [Google Scholar]
- 3.Robinson TN, Banda JA, Hale L, Lu AS, Fleming-Milici F, Calvert SL, et al. Screen media exposure and obesity in children and adolescents. Pediatrics. 2017;140(Supplement 2):S97–S101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ghobadi S, Hassanzadeh-Rostami Z, Salehi-Marzijarani M, Bellissimo N, Brett NR, Totosy de Zepetnek JO, et al. Association of eating while television viewing and overweight/obesity among children and adolescents: a systematic review and meta-analysis of observational studies. Obes Rev. 2018;19(3):313–20. [DOI] [PubMed] [Google Scholar]
- 5.Carson V, Janssen I. The mediating effects of dietary habits on the relationship between television viewing and body mass index among youth. Pediatr Obes. 2012;7(5):391–8. [DOI] [PubMed] [Google Scholar]
- 6.Cleland VJ, Schmidt MD, Dwyer T, Venn AJ. Television viewing and abdominal obesity in young adults: is the association mediated by food and beverage consumption during viewing time or reduced leisure-time physical activity? Am J Clin Nutr. 2008;87(5):1148–55. [DOI] [PubMed] [Google Scholar]
- 7.Fletcher EA, McNaughton S, Lacy K, Dunstan D, Carson V, Salmon J. Mediating effects of dietary intake on associations of TV viewing, body mass index and metabolic syndrome in adolescents. Obesity science & practice. 2016;2(3):232–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Falbe J, Rosner B, Willett WC, Sonneville KR, Hu FB, Field AE. Adiposity and different types of screen time. Pediatrics. 2013;132(6):e1497–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cleland VJ, Patterson K, Breslin M, Schmidt MD, Dwyer T, Venn AJ. Longitudinal associations between TV viewing and BMI not explained by the ‘mindless eating’ or ‘physical activity displacement’ hypotheses among adults. BMC public health. 2018;18(1):797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gebremariam MK, Bergh IH, Andersen LF, Ommundsen Y, Totland TH, Bjelland M, et al. Are screen-based sedentary behaviors longitudinally associated with dietary behaviors and leisure-time physical activity in the transition into adolescence? Int J Behav Nutr Phys Act. 2013;10:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boulos R, Vikre EK, Oppenheimer S, Chang H, Kanarek RB. ObesiTV: how television is influencing the obesity epidemic. Physiology & behavior. 2012;107(1):146–53. [DOI] [PubMed] [Google Scholar]
- 12.Lobstein T, Dibb S. Evidence of a possible link between obesogenic food advertising and child overweight. Obes Rev. 2005;6(3):203–8. [DOI] [PubMed] [Google Scholar]
- 13.Avery A, Anderson C, McCullough F. Associations between children’s diet quality and watching television during meal or snack consumption: A systematic review. Maternal & child nutrition. 2017;13(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Feldman S, Eisenberg ME, Neumark-Sztainer D, Story M. Associations between watching TV during family meals and dietary intake among adolescents. J Nutr Educ Behav. 2007;39(5):257–63. [DOI] [PubMed] [Google Scholar]
- 15.Lipsky LM, Nansel TR, Haynie DL, Liu D, Li K, Pratt CA, et al. Diet quality of US adolescents during the transition to adulthood: changes and predictors. Am J Clin Nutr. 2017;105(6):1424–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Trofholz AC, Tate AD, Miner MH, Berge JM. Associations between TV viewing at family meals and the emotional atmosphere of the meal, meal healthfulness, child dietary intake, and child weight status. Appetite. 2017;108:361–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fletcher EA, McNaughton SA, Crawford D, Cleland V, Della Gatta J, Hatt J, et al. Associations between sedentary behaviours and dietary intakes among adolescents. Public Health Nutr. 2018;21(6):1115–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pearson N, Biddle SJ, Williams L, Worsley A, Crawford D, Ball K. Adolescent television viewing and unhealthy snack food consumption: the mediating role of home availability of unhealthy snack foods. Public Health Nutr. 2014;17(2):317–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Falbe J, Willett WC, Rosner B, Gortmaker SL, Sonneville KR, Field AE. Longitudinal relations of television, electronic games, and digital versatile discs with changes in diet in adolescents. Am J Clin Nutr. 2014;100(4):1173–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Matheson DM, Killen JD, Wang Y, Varady A, Robinson TN. Children’s food consumption during television viewing. Am J Clin Nutr. 2004;79(6):1088–94. [DOI] [PubMed] [Google Scholar]
- 21.Trofholz AC, Tate A, Loth K, Neumark-Sztainer D, Berge JM. Watching Television while Eating: Associations with Dietary Intake and Weight Status among a Diverse Sample of Young Children. J Acad Nutr Diet. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martines RM, Machado PP, Neri DA, Levy RB, Rauber F. Association between watching TV whilst eating and children’s consumption of ultraprocessed foods in United Kingdom. Maternal & child nutrition. 2019:e12819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kain J, Corvalan C, Lera L, Galvan M, Uauy R. Accelerated growth in early life and obesity in preschool Chilean children. Obesity (Silver Spring). 2009;17(8):1603–8. [DOI] [PubMed] [Google Scholar]
- 24.Gaskins AJ, Pereira A, Quintiliano D, Shepherd JA, Uauy R, Corvalán C, et al. Dairy intake in relation to breast and pubertal development in Chilean girls. Am J Clin Nutr. 2017;105(5):1166–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jensen ML, Corvalan C, Reyes M, Popkin BM, Taillie LS. Snacking patterns among Chilean children and adolescents: is there potential for improvement? Public Health Nutr. 2019;22(15):2803–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bryant M, Lucove J, Evenson K, Marshall S. Measurement of television viewing in children and adolescents: a systematic review. Obes Rev. 2007;8(3):197–209. [DOI] [PubMed] [Google Scholar]
- 27.Christakis DA, Zimmerman FJ, DiGiuseppe DL, McCarty CA. Early television exposure and subsequent attentional problems in children. Pediatrics. 2004;113(4):708–13. [DOI] [PubMed] [Google Scholar]
- 28.Dillman Carpentier F, Correa T, Reyes M, Taillie L. Children’s and adolescents’ exposure to total and child-directed television advertising of unhealthy foods in Chile, based on direct television viewing and television use in the household. Am J Clin Nutr. [in press]. [Google Scholar]
- 29.Cerda R, Barrera C, Arena M, Bascuñán K, Jiménez G. Atlas Fotográfico de Alimentos y Preparaciones Típicas Chilenas. Edición Primera ed. Santiago: Universidad de Chile; 2010. [Google Scholar]
- 30.US Department of Agriculture, Agricultural Research Service. USDA National Nutrient Database for Standard Reference, Release 28 2015. [Available from: https://data.nal.usda.gov/dataset/composition-foods-raw-processed-prepared-usda-national-nutrient-database-standard-reference-release-28-0.
- 31.USDA Agricultural Research Service. USDA National Nutrient Database for Standard Reference. Release 28. 2016;Nutrient Data Laboratory Home Page, http://www.ars.usda.gov/ba/bhnrc/ndl. [Google Scholar]
- 32.USDA Agricultural Research Service. Food and Nutrient Database for Dietary Studies, 2013–14. Beltsville, MD: Agricultural Research Service, Food Surveys Research Group.; 2016. [Google Scholar]
- 33.Kanter R, Reyes M, Corvalan C. Photographic Methods for Measuring Packaged Food and Beverage Products in Supermarkets. Current Developments in Nutrition. 2017;1(10):e001016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kelly B, Vandevijvere S, Ng S, Adams J, Allemandi L, Bahena-Espina L, et al. Global benchmarking of children’s exposure to television advertising of unhealthy foods and beverages across 22 countries. Obes Rev. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ministerio de Educación. Guías Alimentarias para la Población Chilena 2017. [Available from: http://www.integra.cl/wp-content/uploads/2017/01/GUIAS-ALIMENTARIAS.pdf.
- 36.Braveman PA, Cubbin C, Egerter S, Chideya S, Marchi KS, Metzler M, et al. Socioeconomic status in health research: one size does not fit all. Jama. 2005;294(22):2879–88. [DOI] [PubMed] [Google Scholar]
- 37.Card D The causal effect of education on earnings. Handbook of labor economics. 3: Elsevier; 1999. p. 1801–63. [Google Scholar]
- 38.StataCorp. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP; 2015. [Google Scholar]
- 39.Mukaka MM. Statistics corner: A guide to appropriate use of correlation coefficient in medical research. Malawi Med J. 2012;24(3):69–71. [PMC free article] [PubMed] [Google Scholar]
- 40.Takagi H, Hari Y, Nakashima K, Kuno T, Ando T. Meta-analysis of the Relation of Television-Viewing Time and Cardiovascular Disease. Am J Cardiol. 2019;124(11):1674–83. [DOI] [PubMed] [Google Scholar]
- 41.Wijndaele K, Brage S, Besson H, Khaw K-T, Sharp SJ, Luben R, et al. Television viewing and incident cardiovascular disease: prospective associations and mediation analysis in the EPIC Norfolk Study. PloS one. 2011;6(5):e20058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vizcaino M, Buman M, DesRoches T, Wharton C. From TVs to tablets: the relation between device-specific screen time and health-related behaviors and characteristics. BMC public health. 2020;20(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bueno NB, de Melo IS, de Oliveira SL, da Rocha Ataide T. Very-low-carbohydrate ketogenic diet v. low-fat diet for long-term weight loss: a meta-analysis of randomised controlled trials. The British journal of nutrition. 110. England2013. p. 1178–87. [DOI] [PubMed] [Google Scholar]
- 44.Janssen I, Medina C, Pedroza A, Barquera S. Screen time in Mexican children: findings from the 2012 National Health and Nutrition Survey (ENSANUT 2012). Salud Publica Mex. 2013;55(5):484–91. [DOI] [PubMed] [Google Scholar]
- 45.Rideout V The Common Sense Census: Media use by teens and tweens 2015. [Available from: https://www.commonsensemedia.org/sites/default/files/uploads/research/census_researchreport.pdf.
- 46.American Academy of Pediatrics. American Academy of Pediatrics Announces New Recommendations for Children’s Media Use 2016. [Available from: https://services.aap.org/en/news-room/news-releases/aap/2016/aap-announces-new-recommendations-for-media-use/.
- 47.Canadian Society for Exercise Physiology. Canadian 24-Hour Movement Guidelines for Children and Youth: An Integration of Physical Activity, Sedentary Behaviour, and Sleep 2016. [Available from: https://csepguidelines.ca/wp-content/themes/csep2017/pdf/Canadian24HourMovementGuidelines2016_2.pdf. [DOI] [PubMed]
- 48.Oliveira JS, Barufaldi LA, Abreu Gde A, Leal VS, Brunken GS, Vasconcelos SM, et al. ERICA: use of screens and consumption of meals and snacks by Brazilian adolescents. Rev Saude Publica. 2016;50 Suppl 1:7s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dubois L, Farmer A, Girard M, Peterson K. Social factors and television use during meals and snacks is associated with higher BMI among pre-school children. Public Health Nutr. 2008;11(12):1267–79. [DOI] [PubMed] [Google Scholar]
- 50.Batis C, Rodriguez-Ramirez S, Ariza AC, Rivera JA. Intakes of Energy and Discretionary Food in Mexico Are Associated with the Context of Eating: Mealtime, Activity, and Place. J Nutr. 2016;146(9):1907s–15s. [DOI] [PubMed] [Google Scholar]
- 51.Goncalves WSF, Byrne R, Viana MT, Trost SG. Parental influences on screen time and weight status among preschool children from Brazil: a cross-sectional study. Int J Behav Nutr Phys Act. 2019;16(1):27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sadeghirad B, Duhaney T, Motaghipisheh S, Campbell N, Johnston B. Influence of unhealthy food and beverage marketing on children’s dietary intake and preference: a systematic review and meta-analysis of randomized trials. Obes Rev. 2016;17(10):945–59. [DOI] [PubMed] [Google Scholar]
- 53.Boyland EJ, Halford JC. Television advertising and branding. Effects on eating behaviour and food preferences in children. Appetite. 2013;62:236–41. [DOI] [PubMed] [Google Scholar]
- 54.Correa T, Reyes M, Taillie LS, Dillman Carpentier F. The prevalence and audience reach of food and beverage advertising on Chilean television according to marketing tactics and nutritional quality of products. Public Health Nutr. 2018:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Consejo Nacional de Televisión. Anuario Estadístico: Oferta y Consumo de Televisión. 2018. [Available from: https://www.cntv.cl/cntv/site/artic/20190329/asocfile/20190329114753/anuario_estadistico_de_oferta_y_consumo_2018.pdf.
- 56.Tan L, Ng SH, Omar A, Karupaiah T. What’s on YouTube? A Case Study on Food and Beverage Advertising in Videos Targeted at Children on Social Media. Childhood obesity (Print). 2018;14(5):280–90. [DOI] [PubMed] [Google Scholar]
- 57.Vandevijvere S, Aitken C, Swinburn B. Volume, nature and potential impact of advertisements on Facebook and YouTube by food brands popular in New Zealand. The New Zealand medical journal. 2018;131(1473):14–24. [PubMed] [Google Scholar]
- 58.Vassallo AJ, Kelly B, Zhang L, Wang Z, Young S, Freeman B. Junk Food Marketing on Instagram: Content Analysis. JMIR public health and surveillance. 2018;4(2):e54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gobierno de Chile, Ministerio de Educación. Estadísticas de la Educación 2016 2017. [Available from: https://centroestudios.mineduc.cl/wp-content/uploads/sites/100/2017/07/Anuario_2016.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


