Abstract
Background:
Although previous literature suggested that several factors may be associated with higher risk of adverse health outcomes related to heat, research is limited for birth outcomes.
Objectives:
We investigated associations between exposure to heat/heat waves during the last week of gestation and preterm birth (PTB) in North Carolina (NC) and evaluated effect modification by residential greenness, urbanicity, and socioeconomic status (SES).
Methods:
We obtained individual-level NC birth certificate data for May-September 2003–2014. We estimated daily mean temperature at each maternal residential address using Parameter-elevation Regressions on Independent Slopes Model (PRISM) data. We created 3 definitions of heat waves (daily temperature ≥ 95th, 97th, 99th percentile for NC warm season temperature, for ≥ 2 consecutive days). Normalized Difference Vegetation Index (NDVI) was used to assess residential greenness. Community-level modifiers (e.g., income, urbanicity) were considered. We applied Cox proportional hazard models to estimate the association between exposure to heat/heat waves and PTB, controlling for covariates. Stratified analyses were conducted to evaluate whether the association between heat and PTB varied by several individual and community characteristics.
Results:
Of the 546,441 births, 8% were preterm. Heat exposure during the last week before delivery was significantly associated with risk of PTB. The hazard ration for a 1°C increase in temperature during the last week before delivery was 1.01 (95% CI: 1.00, 1.02). Higher heat-PTB risk was associated with some characteristics (e.g., areas that were urbanized, low SES, or in the Coastal Plain). We also found significant PTB-heat risk in areas with low greenness for urbanized area. For heat waves, we did not find significantly positive associations with PTB.
Discussion:
Findings provide evidence that exposure to heat during pregnancy increases risk of PTB and suggest disparities in these risks. Our results have implications for future studies of disparity in heat and birth outcomes associations.
Keywords: Heat, Heat waves, Greenness, Preterm birth, Urbanicity, Vulnerable population
1. Introduction
Preterm birth (PTB), defined as the birth before 37 weeks of gestation, is one of the leading causes of infant mortality and morbidity worldwide, and can impact adverse health outcomes in later life (Chehade et al. 2018; Harding and Maritz 2012; Shapiro-Mendoza 2016). The incidence of PTB is increasing worldwide (WHO 2018). An estimated 15 million infants are born prematurely every year, and approximately 1 million children died from PTB complications in 2015 (Liu et al. 2016). Given that the PTB can cause substantial public health burden, understanding the risk factors of PTB is critical. Although the determinants of PTB are not fully known, several risk factors such as genetics, maternal factors, environmental stressors (e.g., air pollution, extreme heat) may contribute to PTB. Recently, an increasing number of studies suggested that exposure to heat or extreme heat event (i.e., heat waves) during pregnancy was associated with risk of PTB (Ilango et al. 2020; Sun et al. 2019; Wang et al. 2020). Recent reviews on the associations between heat during pregnancy and risk of adverse birth outcomes reported evidence that exposure to heat is associated with an increase in adverse birth outcomes, especially PTB (Bekkar et al. 2020; Chersich et al. 2020). Some studies on temperature and health estimated health risks of a single day of heat (i.e., one day of high temperature) and others investigated associations between health outcomes and consecutive days of extreme heat (i.e., heat waves) as health response may differ for prolonged periods of consecutive days of extreme heat. There is no standard definition of a heat wave, however most studies have used a combination of intensity and duration to define a heat wave. In this study, we estimated effects of both heat and heat waves on preterm birth. Considering that climate change is anticipated to result in overall global warming with increased frequency and severity of temperature extremes, more research on various regions and climates are needed with respect to how heat impacts adverse birth outcomes.
Globally, the urban population is growing rapidly and about 68% of the population is expected to live in urban areas by 2050 (United Nations, 2018). Rapid urbanization results in extensive environmental changes including reduced vegetation and the urban heat island effect (Seto et al. 2012). Although previous literature suggested beneficial impacts of residential greenness on the association between heat exposure and several health outcomes such as mortality (Gronlund et al. 2015; Son et al. 2016; Xu et al. 2013; Zanobetti et al. 2013), research is very limited for birth outcomes. Moreover, those findings are inconsistent (Kloog 2019). A recent study reported positive interactions between heat waves and low greenness for preterm birth (Sun et al. 2020), while others observed opposite findings or no effect modification by residential greenness (Asta et al. 2019; Son et al. 2019). Various social and contextual factors may affect the vulnerability and adaptation to heat and thus influence the impacts of heat on health, such as through differences in baseline health or access to health care. Community-level socioeconomic status (SES) can also play an important role in this association. Several studies demonstrated that area-level low SES is associated with higher estimated effects of heat on preterm birth (Asta et al. 2019; Son et al. 2019). A recent review suggested that exacerbation of heat exposure related to climate change may be significantly associated with risk of birth outcomes in the US (Bekkar et al. 2020). They noted that some subpopulations such as pregnant women, residents in urban area may be particularly vulnerable to adverse birth outcomes and several social determinants of health may contribute to disproportionate health burden. Understanding the impacts of heat/heat waves and identifying community-level modifiers such as green space among vulnerable subpopulations such as pregnant women is important, especially given that rapid urbanization is occurring simultaneously with climate change.
North Carolina (NC) is a relatively large and diverse state with a range of geographies (e.g., agricultural regions, forests, coastal areas, and multiple medium-large urban centers) and distinct spatial patterns of socio-demographics (e.g., racial distribution, poverty patterns). This study area allows us to evaluate diverse populations and factors regarding environmental health disparities. In this study, we investigated the association between exposure to heat and heat waves during the last week of pregnancy and PTB in NC from 2003 to 2014. We also evaluated effect modification by several characteristics such as residential greenness, urbanicity, and SES in this association.
2. Methods
Data
We obtained birth certificate data from the NC Vital Statistics Reporting System, Department of Health and Human Services, Center for Health Statistics. Data included mother’s residential address, infant’s sex, birth weight, gestational age, parity, and mother’s age, race/ethnicity, and marital status. Clinical estimates of gestational age based on ultrasound and obstetric measures were used. Maternal residential addresses on birth certificates were geocoded. We restricted the study period to the warm season (May-September) to focus on the exposure of heat and heat waves. Of the 570,530 births, we restricted study participants to 546,593 singleton births delivered at 28–44 completed weeks of gestation and excluded births less than 400g of birth weight (0.03 %). Preterm birth was defined as a live birth before 37 weeks of gestation. We excluded extremely preterm birth with gestational age < 28 weeks or >44 weeks based on previous studies as these births may have different etiologies or due to implausible gestational age (Wang et al. 2020; Honein et al. 2009). In total, 546,441 births were included in the analysis. We considered several infant and maternal characteristics including sex of infant (male, female), mother’s age (<20, 20–34, and ≥35 years), mother’s race/ethnicity (Non-Hispanic White, Non-Hispanic Black, Other), mother’s marital status (married, unmarried), and parity (1, 2, 3, 4 or more).
We estimated individual-level daily mean temperature at the maternal residential address (latitude/longitude) using Parameter-elevation Regressions on Independent Slopes Model (PRISM) data. PRISM Climate Group provides gridded daily weather data for the continental US at high spatial resolution (4×4 km grid). Detailed descriptions and algorithms have been described elsewhere (Daly et al. 2008; PRISM Climate Group 2019). For each birth, we assigned individual-level average temperature during the last week of gestation. We considered exposure windows for heat and heat waves for each study participant for 1 week before delivery.
To estimate the exposure to heat waves during the last week of gestation, we created 3 definitions of heat waves as ≥ 2 consecutive days with daily individual-level mean temperature at or above the 95th, 97th, or 99th percentile warm season mean temperature for that county. Similar heat wave definitions were used in previous studies (Lee et al. 2018; Xu et al. 2019). For each heat wave definition, maternal heat wave exposure was assigned as binary variable (yes/no) and was considered exposed if the mother experienced a heatwave during the last week before delivery (i.e., date of birth or any of the 6 preceding days).
We used the Normalized Difference Vegetation Index (NDVI) derived from the Moderate Resolution Imaging Spectroradiometer (MODIS) sensor aboard the Terra satellite image from NASA’s Earth Observing System to assess residential greenness. We used the global MODIS product MOD13Q1 version 5, which is a 16-day composite at a spatial resolution of 250 m (Huete et al. 2002; Weier and Herring 2000). We calculated average NDVI at the county-level over the study period and area for the main analysis. We categorized greenness groups of low, medium, and high as tertiles.
Many previous studies observed that air pollution levels such as PM2.5 and O3 may confound the association between weather and health outcomes (O’Neill et al. 2005; Rainham and Smoyer-Tomic 2003). For adjustment of air pollution exposure, we obtained modelled estimates of daily ambient particulate matter with aerodynamic diameter ≤2.5 μm (PM2.5) and ozone (O3) for NC from the US Environmental Protection Agency (EPA). We used Fused Air Quality Surface using Downscaling (FAQSD) data that integrates monitoring data and gridded output from the atmospheric models at the Census tract level. We calculated county-level daily PM2.5 (24-hr average) and O3 (8-hr max) and assigned average exposure during the last week of gestation for each study participant.
We used 2010 Census data at the Census-tract level to examine community-level effect modification. We considered median household income and percentage less than high school as surrogates for SES, and the Census Bureau’s urban-rural classification, which classified urbanicity as Urbanized Areas (UAs of ≥50,000 people), Urban Clusters (UCs of >2,500 and <50,000 people), and rural areas (defined as those not included within an UA or UC). We categorized median household income as tertiles. We also included an indicator variable for region (i.e., Mountains, Piedmont, and Coastal Plain) to consider NC’s physical, social, and economic regional characteristics.
Statistical analysis
We applied Cox proportional hazard models to estimate the association between exposure to heat/heat waves during the last week of gestation and PTB. The primary outcome was time to event (i.e., PTB) with gestational week as the time scale. This approach accounts for the impacts of time-varying exposure to heat and differences in exposure length among births. The effects of heat at time t depend on the value of heat at the same time t and were examined relative to other participants for the same follow-up interval. This individual-level approach allows us to use the entire population of births (fetuses-at-risk) and to account for potential bias that may affect both seasonal patterns of conception and risk of preterm birth (Auger et al. 2014; Wang et al. 2020). For heat effect, we estimated the hazard ratios (HRs) and 95% confidence intervals (CIs) for a 1°C increment in average temperature during the last week before delivery. We tested the linearity assumption for heat exposure and preterm birth using a spline approach. The p-value of chi-square statistic was not significant indicating the presence of linearity (p=0.2045). Models controlled for individual-level variables of infant sex, maternal age, maternal race/ethnicity, parity, year of birth, and maternal marital status; and community-level variables of median household income, percentage with less than a high school education, region indicator, average dew point temperature, and air pollution (PM2.5 or O3) based on previous literature review. We evaluated whether the association between heat and risk of PTB varied by several individual- and community-level characteristics (i.e., maternal age, race/ethnicity, residential greenness, urbanicity, region, and median household income). For heat wave effect, stratified analyses by each of the three heat wave definitions were conducted to estimate the HRs and 95% CIs for preterm birth and exposure to heat wave during the last week before delivery. Maternal heat wave exposure was assigned as binary variable (yes/no) based on each heat wave definition. and was considered exposed if the mother experienced a heatwave during the last week before delivery (i.e., date of birth or any of the 6 preceding days). We repeated main model by each of the three heat wave definitions.
We evaluated combined disparities of greenness and SES (e.g., low SES neighborhood with low greenness), and greenness and urbanicity (e.g., urban green vs. rural green). For analysis of combined disparities, greenness was categorized as above or below the median. We used the cutoffs as the median of county-level average NDVI for (1) all urbanicity categories (i.e., use same cutoff across all urbanicity groups) and (2) each urbanicity category (i.e., use different cutoffs by each UA, UC, and rural areas) to categorize greenness groups. We conducted stratified analyses by disparity factor (e.g., level of greenness), and combinations of factors (e.g., low greenness and low urbanicity, low greenness and high urbanicity). We used SAS software, version 9.4 (SAS Institute Inc., Cary, NC, USA).
3. Results
Supplemental Table 1 provides summary statistics of the study population. Our analysis included 546,441 singleton births, with 8% preterm birth. The mean gestational age was 34.5 weeks for preterm births and 39.1 weeks for full-term birth. The average birth weight was 3.4 kg for full-term birth and 2.4 kg for preterm births. Compared to full-term births, PTB was more frequent among mothers who were younger (<20 years) or older (≥35 years), Non-Hispanic Black, unmarried, had parity of 4 or more, or lived in rural areas.
Supplemental Figure 1 shows the spatial distribution of county-level temperature used to determine heat waves. The temperature levels for all percentiles (i.e., 95th, 97th, 99th) showed similar trends, with distinct spatial distribution across the three regions. The overall temperature level was higher in the Coastal Plain than Mountain region, with generally increasing trend from the Mountain region to the Coastal Plain.
Supplemental Table 2 shows the comparison of the proportion of births that were preterm by heat wave exposure status during the last week of gestation and heat wave definitions. The proportions of births that were preterm were similar in heat wave exposure and non-heat wave exposure populations for all heat wave definitions (range: 7.9 to 8.2%).
Distribution of meteorological factors and air pollutants are provided in Supplemental Table 3. The daily mean temperature across all study participants ranged from 7.6 to 31.5°C. The mean concentrations of air pollutants were 13.0 μg/m3 for PM2.5 and 48.5 ppb for O3.
Supplemental Table 4 provided the number of heat waves and heat wave days across counties. The number of heat waves for our heat wave definition based on warm season mean temperatures ≥ 95th percentile and ≥ 2 days duration ranged from 0 to 12 per year. The median of number of days per heat wave was 3 days.
Overall, we found positive associations between heat wave exposure during the last week of gestation and PTB for all heat wave definitions, however the results were not statistically significant (Table 1).
Table 1.
Associations between heat wave exposure during last week before delivery and preterm birth in NC, 2003–2014 warm season
| HR (95% CI) | |||
|---|---|---|---|
| Air pollution adjustment | HWD1 | HWD2 | HWD3 |
| Without adjustment for air pollution | 1.007 (0.971, 1.043) | 1.013 (0.971, 1.056) | 1.033 (0.969, 1.101) |
| Adjusted for PM2.5 | 1.001 (0.965, 1.038) | 1.007 (0.964, 1.051) | 1.026 (0.962, 1.095) |
| Adjusted for O3 | 0.997 (0.961, 1.034) | 1.002 (0.959, 1.047) | 1.022 (0.958, 1.091) |
Note: Heat waves were defined as ≥ 2 consecutive days with individual-level daily mean temperature at or above the 95th (HWD1), 97th (HWD2), 99th (HWD3) percentile for the warm season temperature for that county.
Models adjusted for maternal age, race/ethnicity, median annual household income, parity, infant sex, year of birth, maternal marital status, average dew point temp, average PM2.5 or O3 during last week of pregnancy, region, and percentage of population with less than high school education.
Table 2 shows the associations between heat exposure during the last week of gestation and risk of PTB. Higher heat exposure during the last week of gestation was significantly associated with higher risk of PTB, and results were robust to adjustment by air pollution. HR for PTB for a 1°C increase in average temperature during the last week of gestation was 1.01 (95% CI 1.00, 1.02) for results without adjustment for air pollution. We performed sensitivity analysis for the main findings to adjust for air pollution levels during whole pregnancy rather than the last week of gestation. The results were similar with original findings (Supplemental Table 5).
Table 2.
Associations between heat exposure (1°C increment) during last week before delivery and preterm birth in NC, 2003–2014 warm season
| Air pollution adjustment | HR (95% CI) |
|---|---|
| Without adjustment for air pollution | 1.010 (1.003, 1.017) |
| Adjusted for PM2.5 | 1.010 (1.002, 1.018) |
| Adjusted for O3 | 1.010 (1.000, 1.020) |
Note: HR for 1°C increase in average temperature during the last week before delivery
Models adjusted for maternal age, race/ethnicity, median annual household income, parity, infant sex, year of birth, maternal marital status, average dew point temp, average PM2.5 or O3 during last week of pregnancy, region, and percentage of population with less than high school education
Figure 1 shows the risk of PTB from exposure to heat during last week of pregnancy by individual- and community-level characteristics. This association was slightly higher among mothers who were older (≥35 years), living in areas with medium greenness, in Urbanized Areas, in communities with low SES, and in the Coastal Plain. We observed a higher heat-PTB association with lower community-level SES, with the highest risk for the low SES communities and the lowest risk for the high SES communities. However, we did not find any statistically significant differences among groups for these factors, except for region for which the heat-PTB association for the Coastal Plain was higher than that of the Mountain or Piedmont regions.
Figure 1.
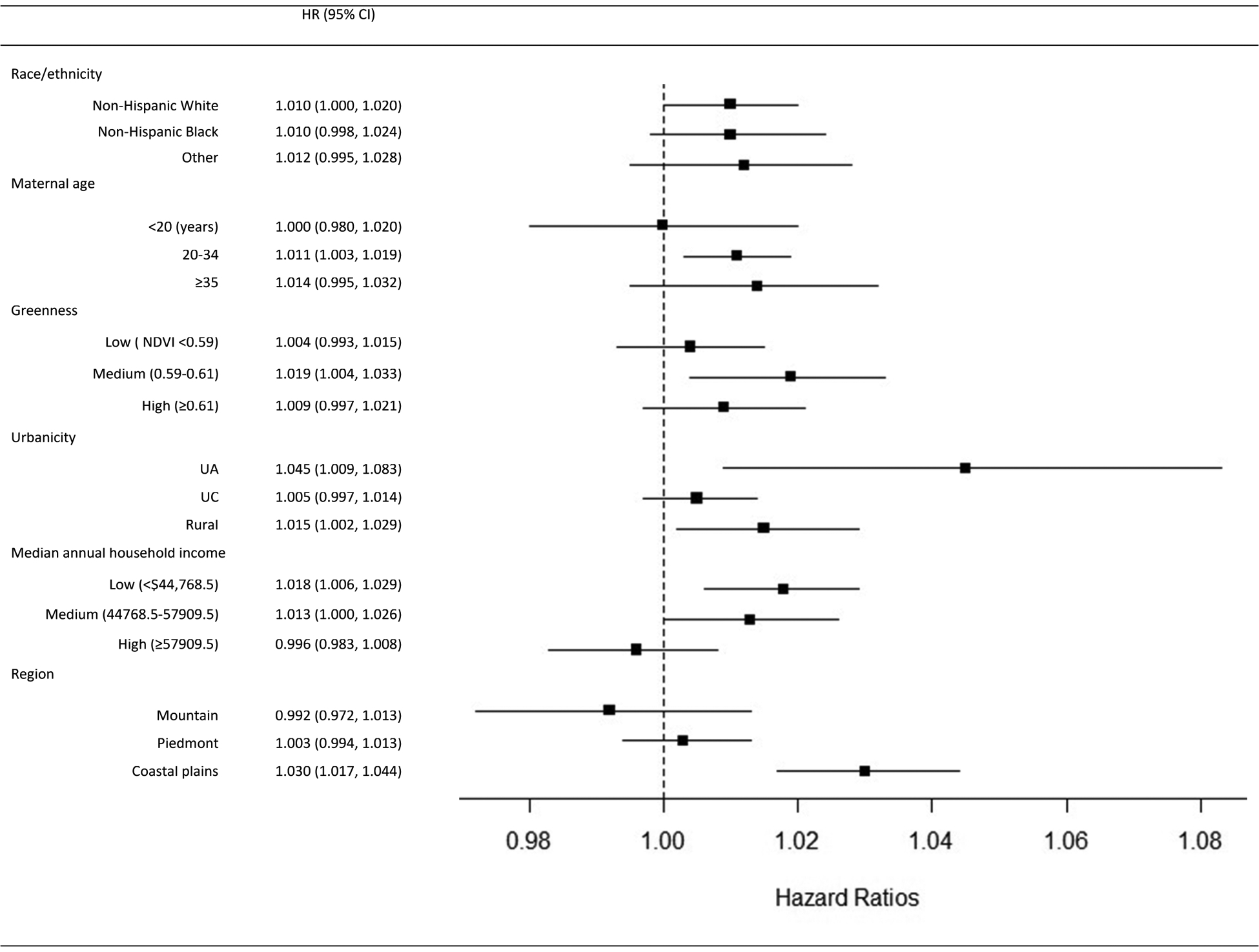
Associations between heat exposure (1°C increment) during last week before delivery and preterm birth by maternal and community characteristics
Note: Squares represent central estimates. Horizontal lines reflect 95% confidence intervals.
We evaluated multiple disparities by combinations of greenness with urbanicity and SES (Tables 3 and 4). Significant risks of PTB from heat were found in some areas. We observed higher risk of preterm birth from heat in areas with low greenness for Urbanized Areas. In rural areas, we found higher risk of PTB associated with heat in areas with high greenness. Additional analysis using the different categorizations for greenness (i.e., based on separate median values for each urbanicity group) provided generally similar results (Supplemental Table 6). For combinations of greenness and SES, we observed higher risk of PTB associated with heat exposure in low SES areas, regardless of greenness level. The highest association between heat exposure during the last week of gestation and the risk of PTB was found in mothers living in areas with both low greenness and low SES.
Table 3.
Associations between heat exposure (1°C increment) during last week of gestation and preterm birth stratified by urbanicity and greenness
| HR (95% CI) | Urbanicity | ||
|---|---|---|---|
| Urbanized Areas (UA) | Urban Cluster (UC) | Rural | |
| Greenness | |||
| Low (<0.6) | 1.061 (1.014, 1.110) | 1.004 (0.994, 1.015) | 1.014 (0.983, 1.046) |
| High (≥0.6) | 1.016 (0.959, 1.077) | 1.002 (0.988, 1.016) | 1.018 (1.003, 1.033) |
Note: Threshold for designating greenness as high or low based on the median of county-level average NDVI for all urbanicity categories.
Number of births by greenness category and urbanicity: UA and low greenness 15729, UA and high greenness 6535; UC and low greenness 247512, UC and high greenness 142114; Rural and low greenness 31063, Rural and high greenness 103488.
Models adjusted for maternal age, race/ethnicity, median annual household income, parity, infant sex, year of birth, maternal marital status, average dew point temp, region, and percentage of population with less than high school education.
Table 4.
Associations between heat exposure (1°C increment) during last week of gestation and preterm birth stratified by greenness and SES
| HR (95% CI) | SES (median annual household income) | ||
|---|---|---|---|
| Low (<44768.5) | Medium (44768.557909.5) | High (≥57909.5) | |
| Greenness | |||
| Low (<0.6) | 1.025 (1.007, 1.043) | 1.005 (0.981, 1.029) | 1.000 (0.986, 1.014) |
| High (≥0.6) | 1.015 (1.000, 1.030) | 1.018 (1.002, 1.034) | 0.979 (0.951, 1.009) |
Note: Threshold for designating greenness as high or low based on the median of county-level average NDVI for all urbanicity categories.
Number of births by greenness category and SES: low SES and low greenness 87123, low SES and high greenness 91577; medium SES and low greenness 53883, medium SES and high greenness 126381; high SES and low greenness 153298, high SES and high greenness 34179.
4. Discussion
Previous literature reported evidence of the impacts of heat or heat waves exposure during pregnancy on PTB (Gronlund et al. 2020; Smith and Hardeman 2020; Vicedo-Cabrera et al. 2015; Wang et al. 2019; Wang et al. 2020), consistent with our findings. A study in China found that exposure to high temperature (23°C, 95th percentile) during the entire pregnancy was significantly associated with increased risk of PTB compared to pregnancies with average temperature below a threshold (12°C) (Wang et al. 2020). Another study in NC examined the impact of high heat over 5-years (2011–2015) during the warm season using a case-crossover design and observing significant impacts on PTB with modest regional variations (Ward et al. 2019). Although they investigated heat and PTB in same study area as our study, they focused on determining thresholds considering regional variations at which risk of PTB significantly increases using various meteorological variables for heat exposure. Also, they did not examine different effects by individual- and community-level characteristics, as in our study.
Our study found generally positive associations between heat wave exposure during the last week of gestation and PTB, however results were not statistically significant. Several factors may influence this finding such as heat waves warning systems, behavior, and adaptation measures such as air conditioning. Similar with our finding, a previous study found higher risk of preterm birth for exposure to moderate heat but not for extreme heat (Vicedo-Cabrera et al. 2015). Another possible reason for our finding is that pregnant women might take more protective measures (e.g., stay inside) during heat waves than times of moderate temperature. A study in California found consistent associations across twelve heat wave definitions that mothers who experienced heat waves during the last week of gestation had increased risk of PTB compared to mothers who did not (Ilango et al. 2020). However, some studies reported no association between heat exposure and PTB (Auger et al. 2014; Wolf and Armstrong 2012). Heterogeneity in findings across studies relate to differences in several characteristics such as population (e.g., race/ethnicity, socioeconomic composition, age distribution), methodology (e.g., exposure windows, heat wave definitions), and other environmental characteristics.
The association between heat exposure during pregnancy and risk of PTB can be explained through several biological mechanisms. Possible biological pathways include increased secretion of hormones (e.g., oxytocin, prostaglandin, antidiuretic hormone) under heat stress, decreased uterine activity, and heat-related dehydration, which could reduce maternal fluid level, uterine blood flow and induce preterm birth. In addition, placental vascular development, placental dysfunction, oxidative stress leading to placental inflammation may influence labor onset (Dreiling et al. 1991; Fukushima et al. 2005; Khamis et al. 1983).
Our analysis of disparities in the heat-preterm birth association as modified by individual- and community-level characteristics considered several variables such as residential greenness. Overall, we found higher associations of heat for PTB in infants living in areas with medium greenness. In our investigation of how PTB risk from heat is influenced by multiple disparities by combinations of greenness and urbanicity, we observed significant risk of PTB in areas with low greenness for Urbanized Areas. However, in rural areas, we found significant risk of PTB in areas with high greenness. There are few studies evaluating residential greenness as an effect modifier in the association between heat exposure and health outcomes, especially for birth outcomes. Although some studies suggested that residential greenness may contribute to lower associations between heat or heat waves and other health outcomes such as mortality (Gronlund et al. 2015; Xu et al. 2013), only a few studies investigated the role of residential greenness on associations between gestational exposure to heat or heat waves and PTB. Moreover, previous findings of residential greenness as an effect modifier in associations between heat and PTB are inconsistent. In the US, Sun et al. (2020) found positive interactions between heat waves and low NDVI-based green space for PTB. However, a study in Rome used maternal residential proximity to green spaces and average NDVI within a 100m buffer around mother’s residential address as greenness indicators. They found higher risk of PTB from heat exposure in women living within 100m from green spaces compared to women living beyond 500m, and no effect modification was observed for NDVI as tertiles (Asta et al. 2019). A study in South Korea did not find significant difference of heat effect for PTB by residential greenness (Son et al. 2019). Possible pathways through which greenness could reduce temperature’s health impacts are different exposure patterns; increased overall health such as physical activity, mental health and wellbeing; and other factors. Greenness can influence ambient temperature through cooling effects by transpiration, shading, and convection (Kloog 2019). Increased urban green can mitigate the urban heat island. However, several other factors may affect inconsistent findings across studies such as differences in regional characteristics, mitigation measures such as use of air conditioning, greenness metrics, behaviors (e.g., actual use of green space), and complex interactions among factors (e.g., green space may relate with higher maternal outdoor activities resulting in increased exposure to heat).
Although risks of heat for PTB were not statistically different across levels of urbanicity, risk was highest for infants living in Urbanized Areas. We also observed increased risk of heat for PTB in rural areas, although the magnitude of effect estimate was smaller than that of Urbanized Areas. Some studies reported higher associations between heat and health outcomes in urban areas than in rural areas (Gabriel and Endlicher 2011). Other studies reported higher effect of heat in rural areas compared to urban areas (Henderson et al. 2013). The effect of heat on health outcomes in urban and rural areas may be differ by characteristics such as population, baseline health status, access to health care, and other environmental conditions may differ across urban versus rural areas and their interactions are complex. A study in NC reported several area-level risk factors for heat-related illness in urban and rural areas (Kovach et al. 2015). They suggested that the number of mobile homes, non-citizens, and the labor-intensity of agriculture were associated with higher risk of heat-related morbidity in rural areas. In urban areas, decreased vegetation, poverty, and low education were associated with heat-related illness. Further studies considering several factors that may affect urban and rural differences are needed.
Our findings showed regional differences across NC for risk of heat on PTB. We found significantly higher effect of heat for PTB in the Coastal Plain compared to other regions. NC three distinct geographic regions (i.e., Mountains, Piedmont, and Coastal Plain)have diverse climate conditions and social and economic distributions. A previous study reported significant heat and PTB associations across NC regions, finding higher associations in the Mountain and Coastal Plain regions (Ward et al. 2019). In contrast to our study using individual-level heat exposure, they used county-level values for meteorological indicators of heat exposure. Another study reported higher risk for heat-related illness in the NC Coastal Plain region (Kovach et al. 2015). They identified that rural areas of the Coastal Plain region had particularly high vulnerability to heat in relation to poverty and a high percentage of mobile homes. Several factors may contribute to regional differences in heat-related risk in NC such as variation in socioeconomics (e.g., limited insurance coverage, energy costs for use of air conditioning), urbanicity, housing with inefficient cooling systems across regions, and population characteristics.
We found consistent evidence of increased risk of PTB from heat for infants living in areas with low SES. For combinations of greenness and SES, we also observed higher risk of preterm birth associated with heat exposure during the last week of gestation in low SES areas, regardless of greenness level, with the highest association in infants living in areas with both low greenness and low SES. Previous studies reported differences in the association between heat exposure and PTB by several individual- and community-level socioeconomic factors such as maternal education, income, occupation, local taxes (including income tax, automobile tax, and property tax), and other measures of area-level SES index (based on education, occupation, home ownership, family composition, crowding, and immigration) (Asta et al. 2019; Schifano et al. 2013; Son et al. 2019; Wang et al. 2020).
Our findings on multiple disparities by combinations of disparity factors can contribute to understanding that intersectionality of disparity factors may affect health disparities from heat exposures. We found that infants living in areas with low SES and high greenness had lower risk of PTB from heat exposure than those living in areas with low SES and low greenness. This indicates that vulnerable populations such as those in low SES areas may benefit more from greenness with respect to the health burden from heat exposure. This study suggests that some disparity factors such as greenness may contribute to reduced disproportionate health burden from heat exposure.
Our study has some limitations. We used satellite-derived NDVI as an indicator of maternal residential greenness. NDVI is a widely used effective metric of greenness, however it does not reflect different aspects of greenness such as vegetation types, green space species, quality of greenness, and accessibility. Moreover, mothers’ actual exposure to greenness (e.g., frequency of visiting or using green space) may play an important role in how greenness may influence the heat-PTB association. Future studies should consider these relevant factors and more detailed assessments of greenness to evaluate the modifying effect of residential greenness on heat and birth outcomes associations. Although we adjusted for many covariates that may affect the association between heat exposure and PTB, other confounding factors may remain. Maternal risk factors (e.g., previous medical conditions, prenatal care, smoking), individual time-activity patterns and behaviors (e.g., use of air conditioning), and residential mobility during pregnancy may affect the association. Future studies could consider further information on potential confounding factors. While our study is very representative of North Carolina as we used birth certificate registry data, we do not have the detailed data that would be available from a cohort study. It is important to evaluate the critical exposure window for the association between heat exposure and birth outcomes. Several previous studies have investigated this issue however, no consistent exposure time frames were identified for this association and the underlying biological mechanisms are not fully understood. Our exposure window of interest is the last week of gestation as we aim to investigate whether the acute exposure to heat and heat wave may trigger an earlier delivery. Future research may also investigate other exposure windows including in relation to other adverse birth outcomes. Studies investigating the effect of time-varying exposures on health outcomes have used several epidemiologic designs including time-series, case-crossover, and cohort. A strength of our study is that we applied an alternative study design, a time to event approach, which has methodological benefits of accounting for potential bias. Another strength of our study is use of individual-level health data and individual-level heat exposure using high-resolution meteorological data. Our analysis estimated individual-level daily mean temperature at high spatial resolution using the maternal residential address (latitude/longitude). Although some studies on heat exposure and health outcomes have been conducted for NC (Kovach et al. 2015; Ward et al. 2019), those studies used county-level values to assign heat exposure for each participant or ZIP code level heat-related ED visits data from the NC public health surveillance system rather than an individual-level heat exposure, thus our study avoids potential exposure misclassification. Also, these previous works did not investigate health disparities by several individual- and community-level factors for birth outcomes, as done in this study. Although we could assign temperature at a high spatial resolution for each participant, other datasets (e.g., air pollution, NDVI) were aggregated at the county-level. Further research using higher resolution of data for other variables is needed to confirm our findings in this study.
5. Conclusion
Our findings provide scientific evidence that heat exposure during the last week of gestation was associated with increased risk of PTB. The risk of PTB from heat was associated with some factors such as urbanicity, residential greenness, and SES. These findings have implications for environmental health disparities regarding protection of subpopulations who suffer more from exposure to heat and policies to protect their health. Understanding underlying mechanisms that link high temperature to PTB and identifying determinants in this association are critical given the adverse health impacts of PTB and the anticipated overall increases in temperature due to a rapidly changing climate. More research is needed to identify the modifying factors for the risk of PTB due to heat exposure among pregnant women.
Supplementary Material
Funding Sources
This publication was developed under Assistance Agreement No. RD835871 awarded by the U.S. Environmental Protection Agency to Yale University. It has not been formally reviewed by EPA. The views expressed in this document are solely those of the authors and do not necessarily reflect those of the Agency
Research reported in this publication was supported by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under Award Number R01MD012769. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Abbreviations
- CI
confidence interval
- HR
hazard ratio
- NDVI
Normalized Difference Vegetation Index
- PRISM
Parameter-elevation Regressions on Independent Slopes Model
- PTB
preterm birth
- SES
socioeconomic status
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Ji-Young Son: Conceptualization, Methodology, Formal analysis, Writing- Original Draft, Writing- Review & Editing. Hyon Michelle Choi: Data Curation, Writing- Review & Editing. Marie Lynn Miranda: Resources, Writing- Review & Editing. Michelle L. Bell: Writing- Review & Editing, Supervision.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Asta F, Michelozzi P, Cesaroni G, De Sario M, Badaloni C, Davoli M et al. 2019. The modifying role of socioeconomic position and greenness on the short-term effect of heat and air pollution on preterm births in Rome, 2001–2013. Int J Environ Res Public Health. 16:2497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auger N, Naimi AI, Smargiassi A, Lo E, Kosatsky T. 2014. Extreme heat and risk of early delivery among preterm and term pregnancies. Epidemiology 25:344–350. [DOI] [PubMed] [Google Scholar]
- Bekkar B, Pacheco S, Basu R, DeNicola N. 2020. Associations of air pollution and heat exposure with preterm birth, low birth weight, and stillbirth in the US A systematic review. JAMA Network Open 3(6):e208243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chehade H, Simeoni U, Guignard JP, Boubred F. 2018. Preterm birth: Long term cardiovascular and renal consequences. Curr Pediatr Rev. 14(4):219–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chersich MF, Pham MD, Area A, Haghighi MM, Manyuchi A, Swift CP et al. 2020. Associations between high temperatures in pregnancy and risk of preterm birth, low birth weight, and stillbirths: systematic review and meta-analysis. BMJ 371:m3811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly C, Halbleib M, Smith JI, Gibson WP, Doggett MK, Taylor GH et al. 2008. Physiographcally sensitive mapping of climatological temperature and precipitation across the conterminous United States. Int J Climatol. 28:2031–2064. [Google Scholar]
- Dreiling CE, Carman III FS, Brown DE. 1991. Maternal endocrine and fetal metabolic responses to heat stress. J Dairy Sci. 74(1):312–327. [DOI] [PubMed] [Google Scholar]
- Fukushima A, Kawahara H, Isurugi C et al. 2005. Changes in serum levels of heat shock protein 70 in preterm delivery and pre-eclampsia. J Obstet Gynaecol Res. 31:72–77. [DOI] [PubMed] [Google Scholar]
- Gabriel K, Endlicher R. 2011. Urban and rural mortality rates during heat waves in Berlin and Brandenburg, Germany. Environmental Pollution 159(8):2044–2050. [DOI] [PubMed] [Google Scholar]
- Gronlund CJ, Berrocal VJ, White-Newsome JL, Conlon KC, O’Neill MS. 2015. Vulnerability to extreme heat by socio-demographic characteristics and area green space among the elderly in Michigan, 1990–2007. Environ Res. 136:449–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gronlund CJ, Yang AJ, Conlon KC, Bergmans RS, Le HQ, Batterman SA et al. 2020. Time series analysis of total and direct associations between high temperatures and preterm births in Detroit, Michigan. BMJ Open 10:e032476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harding R, Maritz G. 2012. Maternal and fetal origins of lung disease in adulthood. Semin. Fetal Neonatal Med 17:67–72. [DOI] [PubMed] [Google Scholar]
- Henderson SB, Wan V, Kosatsky T. 2013. Differences in heat-related mortality across four ecological regions with diverse urban, rural, and remote populations in British Columbia, Canada. Health & Place 23:48–53. [DOI] [PubMed] [Google Scholar]
- Honein MA, Kirby RS, Meyer RE, Xing J, Skerrette NI, Yuskiv N et al. 2009. The association between major birth defects and preterm birth. Matern Child Health J 13:164–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huete AR, Didan K, Miura T, Rodriguez EP, Gao X, Ferreira LG. 2002. Overview of the radiometric and biophysical performance of the MODIS vegetation indices. Remote Sens Environ. 83:195–213. [Google Scholar]
- Ilango SD, Weaver M, Sheridan P, Schwarz L, Clemesha RES, Bruckner T et al. 2020. Extreme heat episodes and risk of preterm birth in California, 2005–2013. Environ Int. 137:105541. [DOI] [PubMed] [Google Scholar]
- Khamis Y, Shaala S, Damarawy H, Romia A, Toppozada M. 1983. Effect of heat on uterine contractions during normal labor. Int J Gynaecol Obstet. 21(6):491–493. [DOI] [PubMed] [Google Scholar]
- Kloog I 2019. Air pollution, ambient temperature, green space and preterm birth. Curr Opin Pediatr. 31:237–243. [DOI] [PubMed] [Google Scholar]
- Kovach MM, Konrad II CE, Fuhrmann CM. 2015. Area-level risk factors for heat-related illness in rural and urban locations across North Carolina, USA. Applied Geography 60:175–183. [Google Scholar]
- Lee W, Choi HM, Lee JY, Kim DH, Honda Y, Kim H. 2018. Temporal changes in mortality impacts of heat wave and cold spell in Korea and Japan. Environ Int. 116:136–146. [DOI] [PubMed] [Google Scholar]
- Liu L, Oza S, Hogan D, Chu Y, Perin J, Zhu J et al. 2016. Global, regional, and national causes of under-5 mortality in 2000–15; an updated systematic analysis with implications for the sustainable development goals. Lancet 388(10063):3027–3035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Neill MS, Hajat S, Zanobetti A, Ramirez-Aguilar M, Schwartz J. 2005. Impact of control for air pollution and respiratory epidemics on the estimated associations of temperature and daily mortality. Int J Biometeorology 50:121–129. [DOI] [PubMed] [Google Scholar]
- PRISM Climate Group. 2019. Oregon State University. https://prism.oregonstate.edu/documents/PRISM_datasets.pdf Accessed on March 16, 2021.
- Rainham DG, Smoyer-Tomic KE. 2003. The role of air pollution in the relationship between a heat stress index and human mortality in Toronto. Environ Res. 93(1):9–19. [DOI] [PubMed] [Google Scholar]
- Schifano P, Lallo A, Asta F, De Sario M, Davoli M, Michelozzi P. 2013. Effect of ambient temperatura and air pollutants on the risk of preterm birth, Rome 2001–2010. Environ Int 61:77–87. [DOI] [PubMed] [Google Scholar]
- Seto KC, Güneralp B, Hutyra LR. 2012. Global forecasts of urban expansion to 2030 and direct impacts on biodiversity and carbon pools. Proc Natl Acad Sci. 109:16083–16088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro-Mendoza CK. 2016. CDC grand rounds: public health strategies to prevent preterm birth. MMWR Morb. Mortal. Wkly Rep 65. [DOI] [PubMed] [Google Scholar]
- Son JY, Lane KJ, Lee JT, Bell ML. 2016. Urban vegetation and heat-related mortality in Seoul, Korea. Environ Res. 151:728–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Son JY, Lee JT, Lane KJ, Bell ML. 2019. Impacts of high temperature on adverse birth outcomes in Seoul, Korea: Disparities by individual- and community-level characteristics. Environ res. 168:460–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun S, Weinberger KR, Spangler KR, Eliot MN, Braun JM, Wellenius GA. 2019. Ambient temperature and preterm birth: A retrospective study of 32 million US singleton births. Environ Int. 126:7–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Y, Ilango SD, Schwarz L, Wang Q, Chen JC, Lawrence JM et al. 2020. Examining the joint effects of heatwaves, air pollution, and green space on the risk of preterm birth in California. Environ Res Lett. 15:104099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uejio CK, Wilhelmi OV, Golden JS, Mills DM, Gulino SP, Samenow JP. 2011. Intra-urban societal vulnerability to extreme heat: The role of heat exposure and the built environment, socioeconomics, and neighborhood stability. Health & Place 17:498–507. [DOI] [PubMed] [Google Scholar]
- United Nations. 2018. Department of Economic and Social Affairs, Population Division. World Urbanization Prospects: The 2018 Revision, 2018. [Google Scholar]
- Vicedo-Cabrera AM, Olsson D, Forsberg B. 2015. Exposure to seasonal temperaturas during the last month of gestation and the risk of preterm birth in Stockholm. Int J Environ Res Public Health. 12:3962–3978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J, Tong S, Williams G, Pan X. 2019. Exposure to heat wave during pregnancy and adverse birth outcomes An exploration of susceptible windows. Epidemiology. 30:S115–S121. [DOI] [PubMed] [Google Scholar]
- Wang Q, Li B, Benmarhnia T, Hajat S, Ren M, Liu T et al. 2020. Independent and combined effects of heatwaves and PM2.5 on preterm birth in Guangzhou, China: A survival analysis. Environ Health Perspect. 128(1):017006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Bobb JF, Papi B, Wang Y, Kosheleva A, Di Q, Schwartz JD, Dominici F. 2016. Heat stroke admissions during heat waves in 1916 US counties for the period from 1999 to 2010 and their effect modifiers. Environmental Health. 15:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang YY, Li Q, Guo Y, Zhou H, Wang QM, Shen HP, Zhang YP et al. 2020. Ambient temperature and the risk of preterm birth: A national birth cohort study in the mainland China. Environ Int. 142:105851. [DOI] [PubMed] [Google Scholar]
- Ward A, Clark J, McLeod J, Woodul R, Moser H, Konrad C. 2019. The impact of heat exposure on reduced gestational age in pregnant women in North Carolina, 2011–2015. Int J Biometeorol 63:1611–1620. [DOI] [PubMed] [Google Scholar]
- Weier J, Herring D. 2000. Measuring vegetation (NDVI & EVI). Available: https://earthobservatory.nasa.gov/features/MeasuringVegetation (accessed 21.08.07)
- Wolf J, Armstrong B. 2012. The association of season and temperature with adverse pregnancy outcome in two German states, a time-series analysis. PLoS ONE 7:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Preterm birth: Fact sheet 2018. https://www.who.int/news-https://www.who.int/news-room/fact-sheets/detail/preterm-birthroom/fact-sheets/detail/preterm-birth Accessed on March 10, 2021.
- Xu Y, Dadvand P, Barrera-Gómez J, Sartini C, Marí-Dell’Olmo M, Borrell C et al. 2013. Differences on the effect of heat waves on mortality by sociodemographic and urban landscape characteristics. J Epidemiol Community Health. 67:519–525. [DOI] [PubMed] [Google Scholar]
- Xu Z, Tong S, Cheng J, Crooks JL, Xiang H, Li X et al. 2019. Heatwaves and diabetes in Brisbane, Australia: a population-based retrospective cohort study. Int J Epidemiol. 48(4):1091–1100. [DOI] [PubMed] [Google Scholar]
- Zanobetti A, O’Neill MS, Gronlund CJ, Schwartz JD. 2013. Susceptibility to mortality in weather extremes: Effect modification by personal and small-area characteristics. Epidemiology. 24:809–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


