Abstract
Although both long and short cephalomedullary devices (CMDs) are used in the treatment of extracapsular hip fractures, the advantages of either option are subject to debate. This study aims to evaluate the differences in clinical outcomes with long versus short CMDs for extracapsular hip fractures. Studies included must have included subjects with at least 1 year of follow-up and reported on at least one of the following outcomes: rate of reoperation; rate of peri-implant fracture; operating time; blood loss; complication rate; length of hospital stay; 1-year mortality. Only articles written in the English language were included in this study. A search was conducted across the databases of Medline, Embase, CENTRAL (Cochrane Central Register of Controlled Trials), CINAHL and Scopus for articles published from the inception of the database to 1 November 2020. Included studies were assessed for their risk of bias using the Risk of Bias Tool (RoB2) and the risk-of-bias in non-randomized studies – of interventions (ROBINS-I) tool. A total of 8460 fractures from 16 studies were included in the analysis, with 3690 fixed with short, and 4770 fixed with long CMDs. A meta-analysis of the results revealed that short CMDs offer peri-operative advantages, while long CMDs could offer longer-term advantages. Limitations of this study include a lack of randomized control trials included in the analysis. In conclusion, when planning for the treatment of extracapsular hip fractures, a patient specific approach may be necessary to make a decision according to the individual risk profile of the patient.
Subject terms: Outcomes research, Trauma
Introduction
Hip fractures are known to be increasing in frequency globally due to an ageing and active global population, with annual incidences set to rise to 6.26 million by 20501. Furthermore, with a 1-year mortality rate of about 20%, being able to choose the optimal treatment of a hip fracture is of increasing importance and relevance2,3. Of the different types of hip fractures, extracapsular fractures such as basicervical neck of femur fractures and intertrochanteric (IT) fractures are thought to be the most associated with falls from a standing height in elderly patients who have osteoporosis4.
Currently there is an increasing trend towards the using a cephalomedullary device (CMD) to manage both stable and unstable extracapsular hip fractures (EHFs) as these nails act as an intramedullary buttress to prevent excessive shaft medialization5–7. When compared with previous surgical options for management, CMDs have shown more favourable long term outcomes and a lower rate of complications8. CMDs which are < 250 mm in length are generally considered to be short, while those longer than 250 mm are classified as long CMDs, the difference being short CMDs do not cross the isthmus of the femur9.
Previous studies have compared the biomechanical properties of long and short CMDs and their effectiveness in fixation of EHFs. While it has been found that axial stiffness is greater in the use of short CMDs, the overall results show no significant differences between short or long CMDs and suggest that either option can be employed for fixation of unstable EHFs10,11.
Although both long and short CMDs are used in the treatment of EHFs, the theoretical advantages of either option are subject to debate12. In recent years, research into this topic has shown advantages of short CMDs over long CMDs, with better intra-operative outcomes, including a shorter operative time, less blood loss and lower rate of transfusion13,14. Conversely, there are also advantages for the use of long CMDs over short CMDs. The longer nail length theoretically provides increased stability in unstable patterns due to the possible distal subtrochanteric extension10,15. There have also been lower reported rates on the incidence of peri-implant fractures, possibly due to the full-length nail providing protection to the entire femoral shaft16,17. But these differences have not affected long term outcomes in patients, with both groups showing no significant difference in reoperation rates, complication rates or 1-year mortality rates18,19.
However, these findings have not been clearly shown in large scale review papers and meta-analyses. This systematic review and meta-analysis of current literature aims to evaluate the differences in clinical outcomes with long versus short cephalomedullary devices (CMDs) for extracapsular hip fractures with the primary outcome being operative time and secondary outcomes being complications such as blood loss and peri-implant fractures.
Methods
The systematic review was planned, conducted, and reported according to the PRISMA guidelines.
Eligibility criteria
To be included in this study, articles had to be either randomized controlled trials, retrospective or prospective cohort studies. These studies must have also reported on simple or multifragmentary EHFs (AO classification 31-A1, A2, and A3) and compared results from patients treated with long CMDs versus short CMDs. The studies must have also had subjects with at least 1 year of follow up, and reported on at least one of the following outcomes, operating time; estimated blood loss; length of hospital stay; overall rate of peri-implant fracture; overall rate of reoperation; overall complication rate; 1-year mortality. Only articles written in the English language were included in this study.
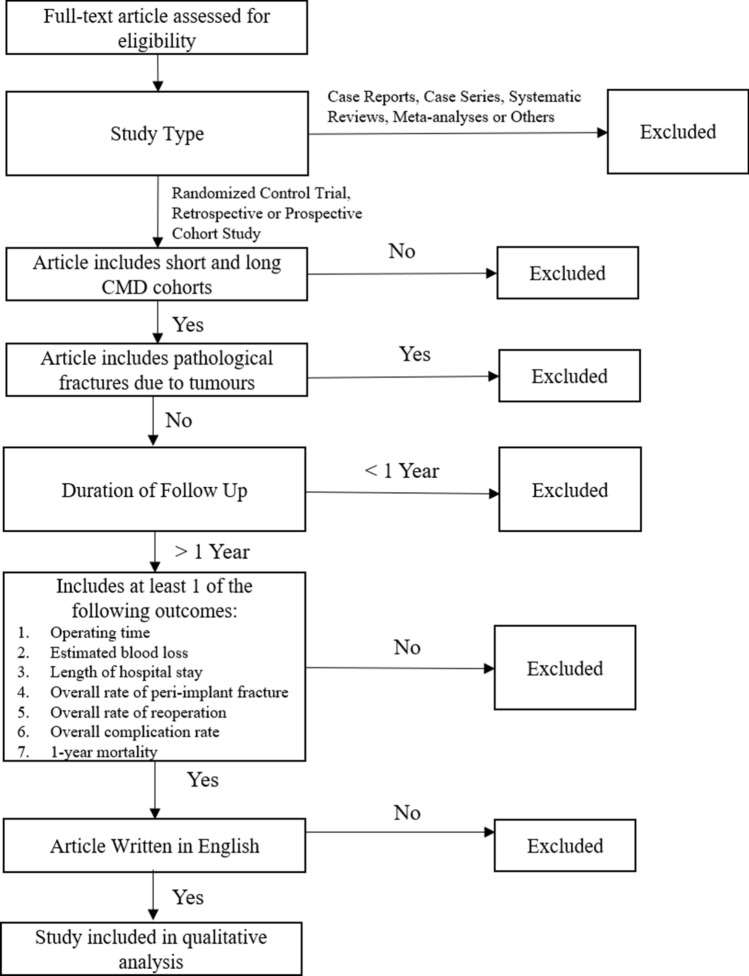
Case reports, case series, systematic reviews and meta-analyses were excluded from this study. Additionally, articles which did not include both short and long CMD cohorts for comparison, had less than 1 year follow up, or included pathological fractures due to tumours were also excluded (Fig. 1).
Figure 1.
Eligibility criteria.
Search strategy
A systematic search was conducted across the databases of Medline, Embase, CENTRAL (Cochrane Central Register of Controlled Trials), CINAHL and Scopus for articles published from the inception of the database to 1 November 2020. The search strategy used was based on: (Hip Fractures or Intertrochanteric Fractures or pertrochanteric fracture*) and (Fracture Fixation, Intramedullary or cephalomedullary nail* or cephalomedullary nail* or intermedullary nail*).
Study selection
Duplicate studies were identified and removed by Covidence, a systematic review tool which uses the Cochrane technology platform. Two independent reviewers then screened the identified studies for relevance. Full manuscripts of included studies were assessed according to the eligibility criteria and the data was extracted. Any inconsistency was resolved through discussion between the two reviewers.
Statistical analysis
All statistical analyses were performed using Cochrane Revman 5.3 Software (Cochrane Collaboration 2014). Risk ratios and 95% confidence intervals were calculated. A p value of < 0.05 was considered significant for this study.
Results
Systematic review
Study selection
A total of 4143 studies were identified through the database searches, with 16 meeting the inclusion criteria and being included in this study (Fig. 2). A total of 8460 fractures were included in the analysis, with 3690 fixed with short, and 4770 fixed with long CMDs. The study with the largest sample size was also the most recently published, by Sadeghi et al. with 5526 patients20. Detailed information on the studies included are included in Table 1.
Figure 2.
Flowchart of studies in review.
Table 1.
Eligible studies, study characteristics, population demographics.
| S/N | Study | Country | Inclusion period | Study design | Device model (short/long) | Number of fractures | Sample size (short/long) | Gender (M/F) | Mean age/years (SD) | Length of F/u (months) | ASA score (1/2/3/4) | OTA classification (31A1/2/3) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Hulet et al.21 | USA | 2000–2012 | Retrospective cohort | NI | 201 | 70 | 131 |
Short 23/47 Long 57/74 (p = 0.140) |
Short 70.6 (19.1) Long 70.1 (17.4) (p = 0.640) |
40.6 (range 6–158) | NI |
Short 23/28/19 Long 19/57/55 (p = 0.010*) |
| 2 | Krigbaum et al.22 | USA | 2001–2010 | Retrospective cohort | NI | 262 | 125 | 137 | Short 120/5 (p = 0.880) | (p = 0.340) |
Long 33.6 (SD 31.2) Short 24 (SD 26.4) |
NI | Short 0/125/0 |
| 3 | Kleweno et al.23 | USA | 2004–2010 | Retrospective cohort | Gamma 3, Synthes TFNA/Gamma 2, Gamma 3, Synthes TFNA | 559 | 219 | 340 | NI | NI | 30.1 (range 12–85) | NI | NI |
| 4 | Hou et al.18 | China | 2005–2009 | Retrospective cohort | TFNA (170 mm)/TFNA | 283 | 100 | 183 |
Short 16/84 Long 57/126 (p = 0.006*) |
Short 81.0 (range 53–102) Long 78.6 (range 47–98) (p = 0.064) |
37 (SD 2.3) |
Short 0/11/64/14 (NI = 11) Long 1/24/101/32 (NI = 25) |
Short 59/41/0 Long 67/116/0 (p = 0.000*) |
| 5 | Frisch et al.24 | USA | 2005–2010 | Retrospective cohort | InterTAN/InterTAN | 169 | 72 | 97 |
Short 18/54 Long 30/67 (p = 0.621) |
Short 76.2 (12.3) Long 76.3 (15.2) (p = 0.501) |
NC | NI | NI |
| 6 | Vaughn et al.12 | USA | 2006–2011 | Retrospective cohort | Gamma 3/Gamma 3 | 256 | 60 | 196 | NI | NI | > 12 | NI |
Short 37/23/0 Long 106/90/0 |
| 7 | Boone et al.25 | USA | 2008–2011 | Retrospective cohort | Gamma 3/Gamma 3 | 201 | 82 | 119 |
Short 25/57 Long 32/87 (p = 0.578) |
Short 83.3 (8.0) Long 79.6 (9.6) (p = 0.005*) |
NC | NI |
Short 31/51/0 Long 28/91/0 (p = 0.029) |
| 8 | Guo et al.26 | China | 2008–2013 | Retrospective cohort | Gamma 3 (180 mm)/Gamma 3 (320, 340, 360 mm) | 178 | 102 | 76 |
Short 42/60 Long 43/33 (p = 0.322) |
Short 82.7 (9.9) Long 78.9 (8.8) (p = 0.003*) |
23.1 (SD 6.8) | NI |
Short 47/55/0 Long 26/50/0 (p = 0.037) |
| 9 | Sellan et al.27 | Canada | 2008–2013 | RCT | InterTAN (180–200 mm)/InterTAN (260–460 mm) | 108 | 71 | 37 |
Short 20/51 Long 14/23 (p = 0.259) |
Short 80.6 (0.9) Long 78.0 (1.7) (p = 0.171) |
> 12 | NI | All A1/A2 |
| 10 | Okcu et al.28 | Turkey | 2009 | RCT | PFNA (240 mm)/PFNA (340–420 mm) | 33 | 15 | 18 |
Short 4/11 Long 4/14 (p = 0.767) |
Short 78 (range 67–95) Long 81 (range 73–89) (p = 0.255) |
Short 14.0 (range 12–19) Long 14.5 (range 12–21) |
NI |
Short 0/0/15 Long 0/0/18 |
| 11 | Hong et al.29 | Singapore | 2009–2012 | Retrospective cohort | PFNA (200 mm)/PFNA (320, 340, 380 mm) | 64 | 44 | 20 |
Short 13/31 Long 6/14 (p = 0.971) |
Short 80.0 (range 60–93) Long 79.8 (range 56–97) (p = 0.920) |
> 12 |
Short 1/22/21/0 Long 1/9/10/0 (p = 0.813) |
Short 11/33/0 Long 4/16/0 (p = 0.662) |
| 12 | Sadeghi et al.20 | USA | 2009–2014 | Retrospective cohort | Gamma 3 (170–180 mm), TFNA (170–180 mm)/Gamma 3, TFNA | 5526 | 2418 | 3108 |
Short 720/1698 Long 938/2170 |
Short 81.2 (10.8) Long 80.6 (11.0) |
NC |
Short (mean = 2.9) Long (mean = 2.8) (p = 0.600) |
NI |
| 13 | Li et al.30 | China | 2010–2012 | Retrospective cohort | PFNA/PFNA | 156 | 97 | 59 |
Short 46/51 Long 20/39 (p = 0.116) |
Short 76.81 (6.56) Long 74.85 (8.15) (p = 0.100) |
NC |
Short 49/31/18 Long 29/19/11 (p = 0.210) |
Short 17/27/15 Long 28/44/25 (p = 0.102) |
| 14 | Raval et al.31 | UK | 2011–2012 | Retrospective cohort | PFNA (240 mm) /PFNA (340–400 mm) | 80 | 40 | 40 |
Short 11/29 Long 13/27 (p = 0.625) |
Short 77.1 (9.2) Long 76.1 (8.7) (p = 0.806) |
> 12 | NI |
Short 12/24/4 Long 9/24/7 (p = 0.536) |
| 15 | Bovbjerg et al.32 | Denmark | 2012 | Retrospective cohort | Gamma 3/Gamma 3 | 216 | 95 | 121 |
Short 28/67 Long 43/78 (p = 0.346) |
Short 83.1 (8.35) Long 82.9 (7.69) (p = 0.884) |
> 12 | NI | NI |
| 16 | Shannon et al.33 | USA | 2014–2017 | RCT | Synthes TFNA, Gamma 3, Affixus/ Synthes TFNA, Gamma 3, Affixus | 168 | 80 | 88 |
Short 20/60 Long 25/63 (p = 0.720) |
Short 82 (range 79–84) Long 79 (range 76–82) (p = 0.110) |
Short 10.5 Long 10.2 |
NI |
Short 13/61/6 Long 12/67/9 (p = 0.230) |
RCT randomized controlled trial, NI no information, NC not possible to calculate.
*Indicates statistically significant difference reported.
All included studies were subject to an assessment of bias, with the revised Cochrane risk-of-bias tool (RoB 2) for the randomized controlled trials, and Risk-of-bias in Non-randomized Studies—of Interventions (ROBINS-I) tool for the retrospective cohort studies34,35. The detailed information on the assessment for bias is reported in Tables 2 and 3 respectively. None of the studies received external funding.
Study characteristics
Three studies, Sellan et al., Okcu et al. and Shannon et al., had a randomised controlled trail (RCT) design27,28,33. The remaining thirteen studies were retrospective cohort studies. Half of the studies were performed in the USA, with the remaining from Europe and Asia.
Device models
Data on the device models were collected from most studies, demonstrating a wide spectrum of device preferences across the board. Majority of the studies used a fixed device brand with nails of varying length for comparison, with the notable exception of Kleweno et al., which opted to include the Gamma 2 nail as a choice of long nail despite not including it under the short nail devices23.
Sample population characteristics
Most of the included studies had largely similar demographics of gender and age. However, Hou et al. noted a significant preponderance of females over males18. Boone et al. and Guo et al. also included significant differences in the ages of patients offered short and long nails, with older patients tending towards a short nail25,26. The included studies have a range of mean follow-up duration of 10.2–40.6 months post-operatively. Additionally, each study had at least one patient who was followed up for a minimum of 12 months post-operatively. ASA score was reported in four studies, ranging from 1 to 418,20,29,30.
Fracture pattern
Twelve studies reported on the fracture classification, with ten further subclassifying the fractures under the length of nail used. Many (n = 6) focused on 31A1/2 fractures, but some studies (n = 4) also elected to include patients from all 31A fractures. Of note, Okcu et al. only studied patients with 31A3 fractures28.
Operative time
Twelve studies included data on operative times for the surgical procedures. All but one study reporting a significantly longer operating time for long CMDs as compared to short CMDs, with Hong being the only dissenting study18,22–31,33.
Blood loss
Eight studies reported on the estimated blood loss from either procedure, with 7 studies reporting statistically significantly higher mean estimated blood loss in long CMD operations as opposed to short CMDs20,24–26,30,31,33. Five studies included information on the number of patients requiring blood transfusion, however only Boone et al. reported that there was a statistically significant difference in transfusion rates18,25–27,31.
Length of stay (LOS)
A total of 9 studies included the LOS of patients post-operatively, with 8 of the studies reporting no significant difference in LOS between the two groups18,20,22,25–29,31.
Information on intraoperative results have been reported in Table 2.
Table 2.
Intra-operative results.
| Study | Mean operating time/min (SD/range) | p value | Mean est. blood loss/mL (SD/range) | p value | No. of patients requiring transfusion (%) | p value | Length of stay/days (SD/range) | p value | |
|---|---|---|---|---|---|---|---|---|---|
| Hulet et al.21 | Short | NI | NI | NI | NI | NI | NI | NI | NI |
| Long | NI | NI | NI | NI | |||||
| Krigbaum et al.22 | Short | 66 (30.00) | < 0.001* | NI | NI | NI | NI | 6.9 (4.8) | 0.018* |
| Long | 90 (48.00) | NI | NI | 9.1 (8.9) | |||||
| Kleweno et al.23 | Short | 51 (22.00) | < 0.00* | NI | NI | NI | NI | NI | NI |
| Long | 70 (35.00) | NI | NI | NI | |||||
| Hou et al.18 | Short | 41 (range 19–106) | < 0.000* | 100 | 0.031* | 42 (42.0%) | 0.462 | 6.4 | 0.383 |
| Long | 61 (range 16–216) | 135 | 83 (45.4%) | 6.8 | |||||
| Frisch et al.24 | Short | 63.8 (20.00) | 0.001* | Long 161.4 (122.40) | 0.002* | NI | NI | NI | NI |
| Long | 82.6 (26.40) | Short 208.1 (116.90) | NI | NI | |||||
| Vaughn et al.12 | Short | NI | NI | NI | NI | NI | NI | NI | NI |
| Long | NI | NI | NI | NI | |||||
| Boone et al.25 | Short | 44.0 (10.70) | < 0.001* | 92.6 (47.20) | 0.002* | 33 (40.2%) | 0.002* | 7.7 (4.10) | 0.393 |
| Long | 56.8 (19.40) | 135.5 (91.90) | 68 (57.1%) | 8.0 (4.50) | |||||
| Guo et al.26 | Short | 43.5 (12.30) | 0.002* | 90.7 (50.60) | 0.004* | 42.3% | 0.041* | 12.9 (6.50) | 0.420 |
| Long | 58.5 (20.30) | 127.8 (85.90) | 56.7% | 12.7 (6.20) | |||||
| Sellan et al.27 | Short | 60 (range 30–120) | 0.021* | NI | NI | 33 (46.4%) | 0.364 | 20.2 (2.80) | 0.345 |
| Long | 73 (range 30–203) | NI | 16 (41.0%) | 15.7 (3.70) | |||||
| Okcu et al.28 | Short | 52.6 (range 34–65) | < 0.001* | NI | NI | NI | NI | 5.4 (range 2–11) | 0.510 |
| Long | 71.8 (range 57–94) | NI | NI | 4.9 (range 2–9) | |||||
| Hong et al.29 | Short | 73 (range 40–121) | 0.617 | NI | NI | NI | NI | 15.5 (range 4–53) | 0.793 |
| Long | 78.2 (range 29–315) | NI | NI | 14.0 (range 3–30) | |||||
| Sadeghi et al.20 | Short | 47.4 (22.80) | NI | 99.8 (105.50) | NI | NI | NI | 5.34 (4.24) | NI |
| Long | 62.7 (33.10) | 135.7 (151.70) | NI | 5.57 (4.43) | |||||
| Li et al.30 | Short | 53.08 (8.51) | 0.000* | 69.95 (21.55) | 0.063 | NI | NI | NI | NI |
| Long | 60.61 (11.43) | 77.97 (31.88) | NI | NI | |||||
| Raval et al.31 | Short | 58.6 (12.60) | 0.016* | Long 172.7 (156.90) | 0.042* | 4 (10.0%) | 0.210 | 11.1 (6.20) | 0.937 |
| Long | 87.7 (32.60) | Short 341.7 (191.80) | 8 (20.0%) | 10.9 (4.80) | |||||
| Bovbjerg et al.32 | Short | NI | NI | NI | NI | NI | NI | NI | NI |
| Long | NI | NI | NI | NI | |||||
| Shannon et al.33 | Short | 51 (range 48–55) | < 0.0001* | 70 (range 61–79) | < 0.001* | NI | NI | NI | NI |
| Long | 80 (range 74–87) | 207 (range 185–229) | NI | NI | |||||
NI no information.
*Indicates statistically significant difference reported.
Post-operative results and complications
Seven studies reported on the 1-year mortality rates of patients, with none of them finding any significant difference between the two groups18,21,22,27–29,31.
1-year complication rate was reported in 11 studies, with only Li et al. reporting statistically fewer incidences in the long CMD group12,18,21–23,26–28,30,32,33.
The 1-year reoperation rate was reported to be statistically similar in the 8 studies which included the information18,20,22,23,28,29,31,33.
Peri-implant fracture rates 1-year post-operatively were reported in 10 studies, with only Frisch et al. reporting a statistically higher rate of fractures on the short CMD group12,18,20,21,23,24,26,27,29,32,33.
Peri-implant infection rates 1-year post-operatively were also reported to be similar in the 6 studies which reported on them18,20,24,26,32,33.
Only three studies noted patient reported outcomes under the Harris Hip Score 1-year post-operatively. Of the studies, only Shannon et al. reported a significant difference between the groups, with the short CMD group reporting higher results28,30,33.
Detailed information on post-operative results and complications can be found in Table 3.
Table 3.
Post-operative results and complications.
| Study | 1-Year post-operative mortality (%) | p value | Overall complication rate (%) | p value | Overall rate of reoperation | p value | Overall rate of peri-prosthetic fractures | p value | Overall rate of peri-prosthetic infections | p value | 1 Year post-operative harris hip score (SD) | p value | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hulet et al.21 | Short | 33 (47.14%) | NI | 19 (27.14%) | NI | NI | NI | 0 (0.00%) | NI | NI | NI | NI | NI |
| Long | 41 (31.30%) | 34 (25.95%) | NI | 0 (0.00%) | NI | NI | |||||||
| Krigbaum et al.22 | Short | 35 (28%) | 0.33 | 21.0% | 0.710 | 5.00% | 0.120 | NI | NI | NI | NI | NI | NI |
| Long | 47 (34%) | 19.0% | 1.00% | NI | NI | NI | |||||||
| Kleweno et al.23 | Short | NI | NI | 80 (36.5%) | 0.930 | 7 (3.20%) | 0.810 | 6 (2.70%) | 0.35 | NI | NI | NI | NI |
| Long | NI | 122 (35.9%) | 12 (3.50%) | 5 (1.50%) | NI | NI | |||||||
| Hou et al.18 | Short | 22 (22.0%) | 0.785 | 10 (10.0%) | 0.518 | 5 (5.0%) | 0.809 | 0 (0.00%) | 0.178 | 1 (1.00%) | 0.942 | NI | NI |
| Long | 42 (23.0%) | 23 (12.6%) | 8 (4.4%) | 2 (1.10%) | 2 (1.10%) | NI | |||||||
| Frisch et al.24 | Short | NI | NI | NI | NI | NI | NI | 6 (8.30%) | 0.013* | 1 (1.40%) | 0.637 | NI | NI |
| Long | NI | NI | NI | 0 (0.00%) | 3 (3.10) | NI | |||||||
| Vaughn et al.12 | Short | NI | NI | 4 (6.63%) | NI | NI | NI | 2 (3.33%) | NI | NI | NI | NI | NI |
| Long | NI | 9 (4.60%) | NI | 0 (0.00%) | NI | NI | |||||||
| Boone et al.25 | Short | NI | NI | NI | NI | NI | NI | 1 (0.84%) | NI | NI | NI | NI | NI |
| Long | NI | NI | NI | 0 (0.00%) | NI | NI | |||||||
| Guo et al.26 | Short | NI | NI | 3 | > 0.05 | NI | NI | 1 (0.90%) | NI | 1 (0.90%) | > 0.05 | NI | NI |
| Long | NI | 4 | NI | 1 (1.30%) | 1 (1.30%) | NI | |||||||
| Sellan et al.27 | Short | 11 (15.5%) | 0.783 | 39 | NI | NI | NI | 5 (7.00%) | 0.35 | NI | NI | NI | NI |
| Long | 5 (12.8%) | 27 | NI | 1 (2.60%) | NI | NI | |||||||
| Okcu et al.28 | Short | 3 (16.6%) | 0.9 | 3 (20.0%) | 0.390 | 0 | 0.410 | NI | NI | NI | NI | 74 (8) | 0.11 |
| Long | 5 (18.1%) | 6 (33.3%) | 2 | NI | NI | 79 (10) | |||||||
| Hong et al.29 | Short | 2 (4.50%) | 0.625 | NI | NI | 4 (9.10%) | 0.689 | 3 (6.80%) | NI | NI | NI | NI | NI |
| Long | 0 (0.00%) | NI | 1 (5.00%) | 0 (0.00%) | NI | NI | |||||||
| Sadeghi et al.20 | Short | NI | NI | NI | NI | 46 (1.90%) | NI | 14 (0.60%) | NI | 1 (2.20%) | NI | NI | NI |
| Long | NI | NI | 50 (1.60%) | 13 (0.40%) | 0 (0.00%) | NI | |||||||
| Li et al.30 | Short | NI | NI | 3 (3.00%) | < 0.05* | NI | NI | NI | NI | NI | NI | 76.16 (10.84) | 0.28 |
| Long | NI | 0 (0.00%) | NI | NI | NI | 79.98 (8.9) | |||||||
| Raval et al.31 | Short | 3 (7.50%) | 0.456 | NI | NI | 1 (2.50%) | 0.556 | NI | NI | NI | NI | NI | NI |
| Long | 5 (12.50%) | NI | 2 (5.00%) | NI | NI | NI | |||||||
| Bovbjerg et al.32 | Short | NI | NI | 5 (5.25%) | NI | NI | NI | 1 (1.05%) | NI | 0 (0.00%) | NI | NI | NI |
| Long | NI | 7 (5.80%) | NI | 1 (0.83%) | 0 (0.00%) | NI | |||||||
| Shannon et al.33 | Short | NI | NI | 12 (15.5%) | 0.830 | 5 (6.25%) | 0.720 | 2 (2.49%) | 1 | 1 (1.25%) | 1 | 76 (3 months) (IQR 74–78) | 0.02* |
| Long | NI | 12 (13.60%) | 8 (9.09%) | 2 (2.27%) | 2 (2.27%) | 71 (3 months) (IQR 68,074) | |||||||
NI no information.
*Indicates statistically significant difference reported.
Meta-analysis
We performed a meta-analysis to compare several outcomes of interest between long and short CMD groups. The outcomes analysed were mean operating time, mean estimated blood loss, mean length of stay, peri-implant fracture rates, reoperation rates and 1-year mortality rates. All 16 included studies were included in the meta-analysis.
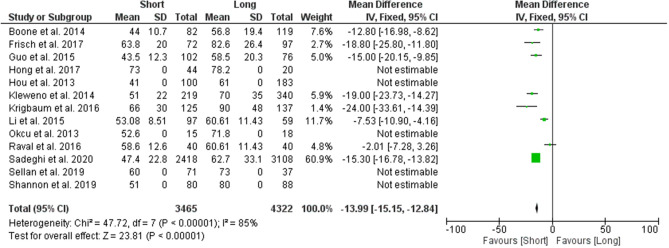
Mean operating time
A total of 8 studies were used to analyse the difference in mean operating time between the two groups. Results from the analysis favoured the group which used short CMDs, reporting a statistically significant lower mean operating time of 13.99 min (95% CI − 15.15 to − 12.84; p value < 0.00001) (Fig. 3).
Figure 3.
Forest plot of mean operating times between long and short CMD groups. Green boxes represent weighted mean values of each study. The black diamond represents the overall pooled weighted mean of all included studies.
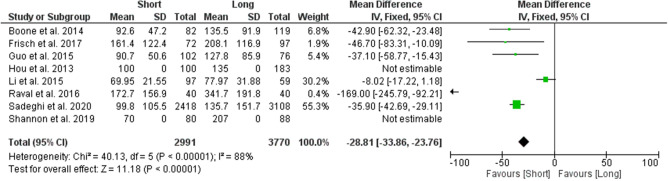
Mean estimated blood loss
A total of 6 studies were used to analyse the difference in mean estimated blood loss between the two groups. Results from the analysis favoured the group which used short CMDs, reporting a statistically significant lower estimated blood loss with a difference of 28.81 mL (95% CI − 33.86 to − 23.76; p value < 0.00001) (Fig. 4).
Figure 4.
Forest plot of mean estimated blood loss between long and short CMD groups. Green boxes represent weighted mean values of each study. The black diamond represents the overall pooled weighted mean of all included studies.
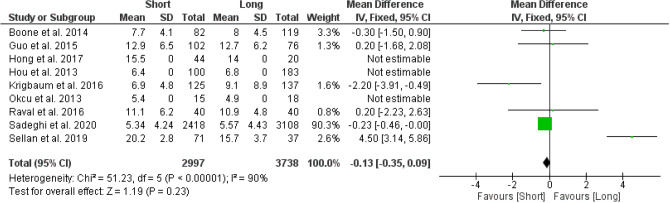
Mean length of stay
A total of 6 studies were used to analyse the difference in mean length of stay between the two groups. Results from the analysis favoured the group which used short CMDs, however this difference was found to not be statistically significant (95% CI − 0.35 to 0.09; p value = 0.23) (Fig. 5).
Figure 5.
Forest plot of mean length of stay between long and short CMD groups. Green boxes represent weighted mean values of each study. The black diamond represents the overall pooled weighted mean of all included studies.
Peri-implant fractures
A total of 10 studies were used to analyse the overall risk ratio for peri-implant fractures between the two groups, with results showing a statistically significant difference, favouring the group with long CMDs. The risk ratio of peri-implant fractures among patients with short CMDs was 1.85 (95% CI 1.14–2.98; p value = 0.01) times as likely as the risk among patients who had long CMDs (Fig. 6).
Figure 6.
Forest plot of risk ratio for peri-implant fractures between long and short CMD groups. Blue boxes represent weighted mean values of each study. The black diamond represents the overall pooled weighted mean of all included studies.
Reoperation rate
A total of 6 studies were used to analyse the risk ratio of reoperation rate among patients, with results showing no statistically significant differences between the groups. The risk ratio of peri-implant fractures among patients with short CMDs was 1.08 (95% CI 0.78–1.49; p value = 0.63) times as likely as the risk among patients who had long CMDs (Fig. 7).
Figure 7.
Forest plot of risk ratio for reoperation rates between long and short CMD groups. Blue boxes represent weighted mean values of each study. The black diamond represents the overall pooled weighted mean of all included studies.
1-Year Mortality Rate
A total of 7 studies were used to analyse the risk ratio for 1-year mortality rate between the two groups, with results showing no statistically significant differences between the groups. The risk ratio of 1-year mortality rate among patients with long CMDs was 1.03 (95% CI 0.83–1.27; p value = 0.78) times as likely as the risk among patients who had short CMDs (Fig. 8).
Figure 8.
Forest plot of risk ratio for 1-year mortality rate between long and short CMD groups. Blue boxes represent weighted mean values of each study. The black diamond represents the overall pooled weighted mean of all included studies.
Discussion
The aim of the study was to evaluate differences in clinical outcomes between using short and long CMDs in the treatment of extracapsular hip fractures. With the current lack of pooled analysis and comparison between these CMDs, it is difficult for surgeons to decide with conviction the optimal nail length for their patients. Through this systematic review and meta-analyses, we have found that long and short CMDs have different short-term and long-term outcomes. Short CMDs offered significant advantages in some of the peri-operative outcomes over the long CMDs. These were shorter operative times and less blood loss. However, long CMDs have shown advantages over short CMDs in their long-term benefits. With a significant reduction in risk of peri-implant fracture rate, the longer survivorship of the prosthesis could be a reflection of the theoretical increased stability provided by having a long CMD (Table 4).
Table 4.
Summary of findings.
| Long compared to short cephalomedullary devices for fixation of extracapsular hip fractures | |||||
|---|---|---|---|---|---|
| Outcomes | № of participants (studies) Follow-up |
Certainty of the evidence (GRADE) | Relative effect (95% CI) | Anticipated absolute effects | |
| Risk with Short cephalomedullary devices | Risk difference with long cephalomedullary devices | ||||
| Operating Time | 7619 (12 observational studies) |
⨁⨁⨁◯ Moderatea |
– | – | Mean 13.99 min more (12.84 more to 15.15 more) |
| Operating Time | 276 (2 RCTs) |
⨁⨁◯◯ Lowa,c,h |
– | – | – |
| Estimated Blood Loss | 6593 (8 observational studies) |
⨁⨁◯◯ Lowa,d |
– | – | Mean 28.81 ml higher (23.76 higher to 33.86 higher) |
| Estimated Blood Loss | 150 (1 RCT) |
⨁⨁◯◯ Low e,h |
– | The mean estimated Blood Loss was 70 ml | Mean 18 ml more |
| Length of Stay | 6594 (8 observational studies) |
⨁⨁◯◯ Lowa,f |
– | – | Mean 0.13 days more (0.09 fewer to 0.35 more) |
| Length of Stay | 141 (2 RCTs) |
⨁⨁◯◯ Lowa,g,h |
– | – | – |
| Peri-Implant Fractures | 7452 (9 observational studies) |
⨁⨁⨁◯ Moderatea |
RR 0.51 (0.30–0.86) | 11 per 1000 | 5 Fewer per 1000 (7 fewer to 1 fewer) |
| Peri-Implant Fractures | 276 (2 RCTs) |
⨁⨁◯◯ Lowa,h |
RR 0.53 (0.14–2.00) | 46 per 1000 | 22 Fewer per 1000 (40 fewer to 46 more) |
| Reoperation Rates | 6512 (6 observational studies) |
⨁⨁◯◯ Lowa,b,f |
RR 0.89 (0.78–1.49) | 22 per 1000 | 2 Fewer per 1000 (8 fewer to 5 more) |
| Reoperation Rates | 168 (1 RCT) |
⨁⨁◯◯ Lowh |
RR 1.45 (0.50–4.26) | 63 per 1000 | 28 More per 1000 (31 fewer to 204 more) |
| 1-Year Mortality | 890 (5 observational studies) |
⨁⨁◯◯ Lowa,f |
RR 1.13 (0.83–1.27) | 251 per 1000 | 33 More per 1000 (28 fewer to 108 more) |
| 1-Year Mortality | 141 (2 RCTs) |
⨁⨁◯◯ Lowa,h |
RR 1.12 (0.53–2.34) | 163 per 1000 | 20 More per 1000 (77 fewer to 218 more) |
|
*The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) CI: confidence interval; RR: risk ratio | |||||
|
GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect | |||||
aInformation used to generate the estimated effect obtained from studies with moderate risk of bias.
bInformation used to generate the estimated effect obtained from studies with severe risk of bias.
cMean operating time was reported without statistical analysis or standard deviation provided in the studies included.
dEstimated blood loss across studies had a large variations and standard deviation values.
eEstimated blood loss was reported without statistical analysis or standard deviation provided in the study included.
fLarge amount of heterogeneity within results with results approaching the line of no effect.
gLength of Stay was reported without statistical analysis or standard deviation provided in the studies included.
hSmall number of studies included for analysis.
Mean operating time between the two groups showed a significantly shorter operating time when using a short CMD as compared to a long CMD. This finding is in agreement with what has been reported in the existing literature where the number of steps and their complexity is lower when using a short CMD. This has been attributed to the additional time needed for reaming, as well the freehand placement of distal interlocking screws when inserting long CMDs36,37.
Estimated blood loss between the groups favoured the use of short CMDs over long CMDs, with the pooled data showing a statistically significant difference between the two groups. This has also been reported in the existing literature, with short CMDs showing a consistently lower blood loss over long CMDs36,38. The lower blood loss may also confer more advantages towards the use of a short nail, such as a reduction in the transfusion requirements, which had also been reported in 2 of the studies included25,26.
The short CMD group displayed a shorter LOS post-operatively as compared to the long CMD group. While this difference was not statistically significant, the difference in the length of stay could be due to a multitude of factors involving the condition and care of the patient. This may include the availability of community healthcare resources for the patient to be discharged to, rehabilitation services such as physiotherapy or other patient specific factors which may have altered their LOS. Another postulation is that patients who required long CMDs in the studies could have had a more complex or unstable fracture pattern which could have delayed their post-operative rehabilitation.
Rates of peri-implant fractures were significantly higher in the short CMD group, with a risk ratio of 1.85 times as compared to the long CMD group. The differences in these results may be due to the nail spanning the full length of the femur, and therefore providing additional stability and strength to the bone16,17. Peri-implant fractures were reported to be at the distal tip of the implant in several cases of long nails18,23,33. In some reports, the peri-implant fractures were due to identifiable incidents of trauma, such as falls from standing height12,23,25,32,33. Kleweno et al. reported no significant difference in the time to peri-implant fracture between the short and long nail cohorts23. In the studies included, the range of incidence for post-operative peri-implant fracture rates was reported to be from as early as 21 days post-operatively, up to 563 days post-operatively. It has been proposed that the timing of peri-implant fracture rates is not predictable as there is a large range of timings of reported incidence of this complication24.
Reoperation rates were similar in both groups, with no significant differences calculated. While the rate of peri-implant fractures 1-year post-operatively was higher in the short CMD group, rates of other complications was not well reported and thus a pooled analysis for the overall complication rate was not possible.
Finally, the 1-year mortality rate between the groups was found to be similar, with no significant difference between them. While the 1-year mortality rate has been reported to be as high as up to 58%, the current study has found significantly lower mortality rates across the groups39. The included studies have a 1-year mortality rate ranging from 0 (0/20) to 47% (33/70), with the vast majority reporting rates of under 30%. The decrease in 1-year mortality rate could reflect an improvement and development in operative technique, and post-operative care of hip fracture patients, thereby improving the prognosis.
Most studies included in this study have been deemed to have low levels of bias. However, those papers which have been identified to have potential issues with bias are commonly due to confounding variables, which most commonly are due to a significant difference between the ages of the short and long CMD groups. The studies which had these differences postulated that the difference could be attributed to shorter operative time which would be favourable in older age groups12,25,26.
In light of our analysis, we postulate that the use of short CMDs may be better suited for high-risk patients who may not be able to tolerate longer operating times. This includes those who have multiple medical comorbidities, and the elderly. The decrease in the amount of time under anaesthesia could be advantageous for these patients as it may decrease the risk of perioperative complications13,40. However, this should also be weighed against benefit in long-term outcomes that have been shown with the use of a long CMD.
While the study has presented several findings that could help guide the decision between the use of a short or long CMD, the strength of this study is in the volume of patients included in the analysis. This is the largest meta-analysis on the topic thus far, with the inclusion of large multi-centre data in the pooled analysis. Limitations of the paper would include the lack of RCTs included. While there were 3 included in the analysis, a larger pool of RCTs would be helpful in ascertaining the differences between short and long CMDs. Additionally, there was limited data available for some of the outcomes of interest, including 1-year post-operative HHS and transfusion rate, preventing a pooled analysis on these outcomes. Furthermore, the mean follow-up period of the included studies was varied (10.2–40.6 months), making a cross sectional study of the outcomes of interest difficult. While a key point of interest would be to investigate incidence and timeline of peri-implant fracture rates, few studies reported the time to the incidence of peri-implant fracture. This precluded further analysis on this subject, and the current study is only able to draw a conclusion to the overall rate of complications and peri-implant fractures. Other potentially interesting areas of further research on this topic would include a comparison between the peri-implant fracture rate in different periods post-operatively, including short- and long-term studies on the topic.
Conclusion
Short CMDs offer advantages of shorter operative time and lesser blood loss. However long CMDs could offer longer-term protection against peri-implant fractures. Therefore, in planning for the operation, a patient specific approach may be necessary to make a decision according to the individual risk profile of the patient.
Supplementary Information
Author contributions
H.R.B.A.R conceptualized and refined the research idea. He was also involved in the interpretation of the statistical analyses and drafting of the manuscript. G.K.Y.T and C.S.C were involved in the literature search, selecting and performing the statistical analysis and drafting of the manuscript. All authors reviewed the manuscript.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-03210-1.
References
- 1.Cooper C, Campion G, Melton LJ. Hip fractures in the elderly: A world-wide projection. Osteoporos. Int. 1992;2(6):285–289. doi: 10.1007/BF01623184. [DOI] [PubMed] [Google Scholar]
- 2.Cenzer IS, Tang V, Boscardin WJ, Smith AK, Ritchie C, Wallhagen MI, et al. One-year mortality after hip fracture: Development and validation of a prognostic index. J. Am. Geriatr. Soc. 2016;64(9):1863–1868. doi: 10.1111/jgs.14237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hu F, Jiang C, Shen J, Tang P, Wang Y. Preoperative predictors for mortality following hip fracture surgery: A systematic review and meta-analysis. Injury. 2012;43(6):676–685. doi: 10.1016/j.injury.2011.05.017. [DOI] [PubMed] [Google Scholar]
- 4.Ahn J, Bernstein J. Fractures in brief: Intertrochanteric hip fractures. Clin. Orthop. Relat. Res. 2010;468(5):1450–1452. doi: 10.1007/s11999-010-1263-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Page PRJ, Lord R, Jawad A, Dawe E, Stott P, Rogers B, et al. Changing trends in the management of intertrochanteric hip fractures—A single centre experience. Injury. 2016;47(7):1525–1529. doi: 10.1016/j.injury.2016.05.002. [DOI] [PubMed] [Google Scholar]
- 6.Seo J-S, Min H-J, Kim DM, Oh S-M, Kim S-M. Surgical results of the cephalomedullary nail for the femoral intertrochanteric fracture: Comparison between non-experienced surgeons and experienced surgeon. Hip Pelvis. 2016;28(4):225–231. doi: 10.5371/hp.2016.28.4.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fairag R, Abduljabbar FH, Page A, Dimentberg R. Are cephalomedullary nail guides accurate? A case report of an unexpected complication after nailing an intertrochanteric femoral fracture. Geriatr. Orthop. Surg. Rehabil. 2018;9:2151458518757797. doi: 10.1177/2151458518757797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yuan X, Yao Q, Ni J, Peng L, Yu D. Proximal femoral nail antirotation versus dynamic hip screw for intertrochanteric fracture in elders: A meta-analysis. Zhonghua Yi Xue Za Zhi. 2014;94(11):836–839. [PubMed] [Google Scholar]
- 9.Jha V, Ahmed T. Modified short proximal femoral nail for intertrochanteric fractures of femur in Indian patients—Our experience. Malays Orthop. J. 2020;14(2):72–82. doi: 10.5704/MOJ.2007.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blum, L. E., Yee, M. A., Mauffrey, C., Goulet, J. A., Perdue, A. M. & Hake, M. E. Comparison of reamed long and short intramedullary nail constructs in unstable intertrochanteric femur fractures: A biomechanical study. OTA Int.3(2), e075 (2020). [DOI] [PMC free article] [PubMed]
- 11.Marmor M, Elliott IS, Marshall ST, Yacoubian SV, Yacoubian SV, Herfat ST. Biomechanical comparison of long, short, and extended-short nail construct for femoral intertrochanteric fractures. Injury. 2015;46(6):963–969. doi: 10.1016/j.injury.2015.03.005. [DOI] [PubMed] [Google Scholar]
- 12.Vaughn J, Cohen E, Vopat B, Kane P, Abbood E, Born C. Complications of short versus long cephalomedullary nail for intertrochanteric femur fractures, minimum 1 year follow-up. Eur. J. Orthop. Surg. Traumatol. 2014;25:665–670. doi: 10.1007/s00590-014-1557-2. [DOI] [PubMed] [Google Scholar]
- 13.Dunn J, Kusnezov N, Bader J, Waterman BR, Orr J, Belmont PJ. Long versus short cephalomedullary nail for trochanteric femur fractures (OTA 31–A1, A2 and A3): A systematic review. J Orthop Traumatol. 2016;17(4):361–367. doi: 10.1007/s10195-016-0405-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang Y, Zhang S, Wang S, Zhang H, Zhang W, Liu P, et al. Long and short intramedullary nails for fixation of intertrochanteric femur fractures (OTA 31–A1, A2 and A3): A systematic review and meta-analysis. Orthop. Traumatol. Surg. Res. 2017;103(5):685–690. doi: 10.1016/j.otsr.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 15.Lindskog DM, Baumgaertner MR. Unstable intertrochanteric hip fractures in the elderly. JAAOS. 2004;12(3):179–190. doi: 10.5435/00124635-200405000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Baldwin PCI, Lavender RC, Sanders R, Koval KJ. Controversies in intramedullary fixation for intertrochanteric hip fractures. J. Orthop. Trauma. 2016;30(12):635–641. doi: 10.1097/BOT.0000000000000652. [DOI] [PubMed] [Google Scholar]
- 17.Horwitz DS, Tawari A, Suk M. Nail length in the management of intertrochanteric fracture of the femur. JAAOS. 2016;24(6):e50–e58. doi: 10.5435/JAAOS-D-15-00325. [DOI] [PubMed] [Google Scholar]
- 18.Hou Z, Bowen TR, Irgit KS, Matzko ME, Andreychik CM, Horwitz DS, et al. Treatment of pertrochanteric fractures (OTA 31–A1 and A2): Long versus short cephalomedullary nailing. J. Orthop. Trauma. 2013;27(6):318–324. doi: 10.1097/BOT.0b013e31826fc11f. [DOI] [PubMed] [Google Scholar]
- 19.Dunn J, Kusnezov N, Bader J, Waterman BR, Orr J, Belmont PJ. Long versus short cephalomedullary nail for trochanteric femur fractures (OTA 31–A1, A2 and A3): A systematic review. J. Orthop. Traumatol. 2016;17(4):361–367. doi: 10.1007/s10195-016-0405-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sadeghi C, Prentice HA, Okike KM, Paxton EW. Treatment of intertrochanteric femur fractures with long versus short cephalomedullary nails. Perm. J. 2020;24:19. doi: 10.7812/TPP/19.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hulet DA, Whale CS, Beebe MJ, Rothberg DL, Gililland JM, Zhang C, et al. Short versus long cephalomedullary nails for fixation of stable versus unstable intertrochanteric femur fractures at a level 1 trauma center. Orthopedics. 2019;42(2):e202–e209. doi: 10.3928/01477447-20190118-03. [DOI] [PubMed] [Google Scholar]
- 22.Krigbaum H, Takemoto S, Kim HT, Kuo AC. Costs and complications of short versus long cephalomedullary nailing of OTA 31–A2 proximal femur fractures in U.S. veterans. J. Orthop. Trauma. 2016;30(3):125–9. doi: 10.1097/BOT.0000000000000521. [DOI] [PubMed] [Google Scholar]
- 23.Kleweno C, Morgan J, Redshaw J, Harris M, Rodriguez E, Zurakowski D, et al. Short versus long cephalomedullary nails for the treatment of intertrochanteric hip fractures in patients older than 65 years. J. Orthop. Trauma. 2014;28(7):391–397. doi: 10.1097/BOT.0000000000000036. [DOI] [PubMed] [Google Scholar]
- 24.Frisch NB, Nahm NJ, Khalil JG, Les CM, Guthrie ST, Charters MA. Short versus long cephalomedullary nails for pertrochanteric hip fracture. Orthopedics. 2017;40(2):83–88. doi: 10.3928/01477447-20161116-01. [DOI] [PubMed] [Google Scholar]
- 25.Boone C, Carlberg KN, Koueiter DM, Baker KC, Sadowski J, Wiater PJ, et al. Short versus long intramedullary nails for treatment of intertrochanteric femur fractures (OTA 31–A1 and A2) J. Orthop. Trauma. 2014;28(5):e96–e100. doi: 10.1097/BOT.0b013e3182a7131c. [DOI] [PubMed] [Google Scholar]
- 26.Guo XF, Zhang KM, Fu HB, Cao W, Dong Q. A comparative study of the therapeutic effect between long and short intramedullary nails in the treatment of intertrochanteric femur fractures in the elderly. Chin. J. Traumatol. 2015;18(6):332–335. doi: 10.1016/j.cjtee.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 27.Sellan M, Bryant D, Tieszer C, Papp S, Lawendy A, Liew A, et al. Short versus long intertan fixation for geriatric intertrochanteric hip fractures: A multicentre head-to-head comparison. J. Orthop. Trauma. 2019;33(4):169–174. doi: 10.1097/BOT.0000000000001409. [DOI] [PubMed] [Google Scholar]
- 28.Okcu G, Ozkayin N, Okta C, Topcu I, Aktuglu K. Which implant is better for treating reverse obliquity fractures of the proximal femur: A standard or long nail? Clin. Orthop. Relat. Res. 2013;471(9):2768–75. doi: 10.1007/s11999-013-2948-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hong CC, Nashi N, Makandura MC, Tan JH, Peter L, Murphy D. The long and short of cephalomedullary nails in the treatment of osteoporotic pertrochanteric fracture. Singapore Med J. 2017;58(2):85–91. doi: 10.11622/smedj.2016048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li Z, Liu Y, Liang Y, Zhao C, Zhang Y. Short versus long intramedullary nails for the treatment of intertrochanteric hip fractures in patients older than 65 years. Int. J. Clin. Exp. Med. 2015;8(4):6299–6302. [PMC free article] [PubMed] [Google Scholar]
- 31.Raval P, Ramasamy A, Raza H, Khan K, Awan N. Comparison of short vs long anti-rotation in treating trochanteric fractures. Malays. Orthop. J. 2016;10(1):22–28. doi: 10.5704/MOJ.1603.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bovbjerg PE, Larsen MS, Madsen CF, Schønnemann J. Failure of short versus long cephalomedullary nail after intertrochanteric fractures. J. Orthop. 2020;18:209–212. doi: 10.1016/j.jor.2019.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shannon SF, Yuan BJ, Cross WW, III, Barlow JD, Torchia ME, Holte PK, et al. Short versus long cephalomedullary nails for pertrochanteric hip fractures: A randomized prospective study. J. Orthop. Trauma. 2019;33(10):480. doi: 10.1097/BOT.0000000000001553. [DOI] [PubMed] [Google Scholar]
- 34.Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 35.Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Page PRJ, Poole WEC, Shah K, Upadhyay PK. Short or long intramedullary devices for hip fracture? A systematic review of the evidence. J. Orthop. 2020;22:377–382. doi: 10.1016/j.jor.2020.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang Y, Zhang S, Wang S, Zhang H, Zhang W, Liu P, et al. Long and short intramedullary nails for fixation of intertrochanteric femur fractures (OTA 31–A1, A2 and A3): A systematic review and meta-analysis. Orthop. Traumatol. Surg. Res. 2017;103(5):685–690. doi: 10.1016/j.otsr.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 38.Sohatee M, Bennet J. A systematic review of short versus long intramedullary fixation in the management of pertrochanteric fractures. Trauma. 2018;20(3):161–168. doi: 10.1177/1460408617717538. [DOI] [Google Scholar]
- 39.Rapp K, Becker C, Lamb SE, Icks A, Klenk J. Hip fractures in institutionalized elderly people: Incidence rates and excess mortality. J. Bone Miner. Res. 2008;23(11):1825–1831. doi: 10.1359/jbmr.080702. [DOI] [PubMed] [Google Scholar]
- 40.Cinque ME, Goodnough LH, Md BJS, Fithian AT, DeBaun M, Lucas JF, et al. Short versus long cephalomedullary nailing of intertrochanteric fractures: A meta-analysis of 3208 patients. Arch. Orthop. Trauma Surg. 2021 doi: 10.1007/s00402-021-03752-z. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.